Abstract
Objective:
Telephone administered therapies have emerged as an alternative method of delivery for the treatment of depression. Yet concerns persist that the use of the telephone may have a deleterious effect on therapeutic alliance. The purpose of this study was to compare therapeutic alliance in clients receiving cognitive behavioral therapy (CBT) for depression by telephone (T-CBT) or face-to-face (FtF-CBT).
Method:
325 participants were randomized to receive 18 sessions of T-CBT or FtF-CBT. The Working Alliance Inventory (WAI) was measured at weeks 4 and 14. Depression was measured during treatment and over one year post-treatment follow-up using the Hamilton Rating Scale for Depression (Ham-D) and Patient Health Questionnaire-9 (PHQ-9).
Results:
There were no significant differences in client or therapist WAI between T-CBT or FtF-CBT (Cohen’s f2 ranged from 0-.013, all ps > .05). All WAI scores predicted depression end of treatment outcomes (Cohen’s f2 ranged from .009-.06, all ps < .02). The relationship between the WAI and depression outcomes did not vary by treatment group (Cohen’s f2 ranged from 0-.004, ps > .07). The WAI did not significantly predict depression during post-treatment follow-up (all ps > .12).
Conclusions:
Results from this analysis do not support the hypothesis that the use of the telephone to provide CBT reduces therapeutic alliance relative to FtF-CBT.
Keywords: alliance, telephone therapy, CBT, depression
Depression is a common psychiatric disorder, with the general population 1-year prevalence rate of major depressive disorder (MDD) estimated to be 6.6% (Kessler et al., 2003). Most primary care patients indicate preferring psychotherapy to antidepressant medication (Dwight-Johnson, Sherbourne, Liao, & Wells, 2000), yet access barriers prevent patients from initiating and/or adhering to psychotherapy for depression (Mohr et al., 2006; Mohr et al., 2010).
The telephone has been used as a treatment delivery medium, with the intent of overcoming many of these barriers. A growing number of clinical trials have repeatedly demonstrated the efficacy of telephone-administered psychotherapy (Mohr et al., 2005; Mohr et al., 2000; Mohr, Vella, Hart, Heckman, & Simon, 2008; Simon, Ludman, Tutty, Operskalski, & Von Korff, 2004). A recent trial comparing telephone-administered cognitive behavioral therapy (T-CBT) to face-to-face (FtF) cognitive behavioral therapy (FtF-CBT) found that T-CBT produced significantly less dropout, but resulted in equivalent post-treatment outcomes in the treatment of MDD (Mohr et al., 2012).
In spite of these findings, concerns regarding the use of the telephone remain, particularly that it may negatively impact the development of the therapeutic alliance (TA; Mohr, Ho, & Siddique, 2012; Sarkar & Gupta, 2012). TA, the relationship bond that can develop between a client and therapist through collaborative work and mutual trust in establishing and reaching treatment goals (Bordin, 1979), is a core component of psychotherapy. TA has been consistently shown to predict outcomes in FtF therapy across a wide variety of disorders and treatment modalities (Arnow et al., 2013; Del Re, Flückiger, Horvath, Symonds, & Wampold, 2012; Martin, Garske, & Davis, 2000). Some research has also indicated that strong TA can exist in telephone therapy (Day, 2000; Lingely-Pottie & McGrath, 2006; Reese, Conoley, & Brossart, 2002). However, to date, TA has not been directly compared between telephone-administered and FtF psychotherapies.
The primary aim of the current study was to fill this gap in the literature by comparing the strength of TA in a trial comparing T-CBT and FtF-CBT for the treatment of MDD. A secondary aim of the current study was to examine the impact of total TA on depression outcomes for both treatments. We hypothesized that there would be no significant difference in strength of TA or in the relationship between alliance and outcome across T-CBT and FtF-CBT.
Method
This study was a planned secondary analysis of data from a randomized controlled trial comparing the efficacy and retention rates of T-CBT and FtF-CBT in a cohort of 325 depressed participants (Mohr et al., 2012).
Participants
Recruitment of participants occurred from November 2007 to December 2010 from primary care clinics located in an academic medical center in the Chicago area.
Participants were eligible for randomization if they met criteria for MDD, had a minimum score of 16 on the Hamilton Depression Rating Scale (Ham-D), were at least 18 years of age, spoke English, and were able to participate in FtF or telephone therapy. Exclusion criteria included having visual or hearing impairments preventing participation; meeting criteria for depression of an organic etiology or a severe psychiatric disorder; reporting severe alcohol or substance abuse; meeting criteria for dementia; exhibiting severe suicidality; receiving or planning to receive individual psychotherapy; or initiation of antidepressant pharmacotherapy in the previous 10 days.
In compliance with the University’s Institutional Review Board, participants were sent a consent form, which a research staff member reviewed with them over the phone prior to baseline interviews. Prior to randomization, participants signed and returned the consent form.
Treatments
Participants were randomized to either T-CBT or FtF-CBT, stratified by antidepressant status and therapist, by an independent statistician. The treatment delivery medium was the only experimental factor to vary between the two groups, with both treatments using the same CBT protocol (Beck, 1995) adapted and validated for use over the phone (Mohr et al., 2005). Main adaptations were that a workbook was developed and provided to both conditions to facilitate treatment over the phone, and instructions to ensure privacy, safety, and a distraction-free environment were given. To eliminate therapist effects, PhD-level psychologists acted as therapists for both conditions. All therapists received training and supervision from the Beck Institute for Cognitive Behavioral Therapy. All therapy sessions were recorded and 8% were randomly selected and rated by the supervisor on the Cognitive Therapy Scale (Vallis, Shaw, & Dobson, 1986) for fidelity. Further detail of therapist training and fidelity are noted elsewhere (Mohr et al., 2012).
Assessment
The Working Alliance Inventory Short Form (WAI) client version (WAI-C) and therapist version (WAI-T) was administered at weeks 4 and 14 (Hatcher & Gillaspy, 2006). Week 4 was selected to measure early TA, as this allowed sufficient time to establish an alliance (Munder, Wilmers, Leonhart, Linster, & Barth, 2010) and corresponds to the timing of outcome assessments to reduce participant burden. Week 14 was selected to measure late TA as it corresponded with the penultimate assessment point, avoiding the potential “good-bye” effects that assessment at the end of treatment might introduce. The WAI Short Form is a 12-item measure rated on a 7-point Likert scale with three subscales (Task Agreement, Goal Agreement, and Bond Development). The WAI has good predictive validity (Hatcher & Gillaspy, 2006); Cronbach’s alphas for the WAI-C and WAI-T ranged from .82-.87 and .77-.79 across administration time points, respectively.
Depression severity was measured at baseline, weeks 4, 9, 14, and 18 (end of treatment), and at 3, 6, 9, and 12 months post-treatment follow-up. Self-reported depression severity was measured using the 9-item Patient Health Questionnaire-9 (PHQ-9; Kroenke, Spitzer, & Williams, 2002), which has high internal consistency and face validity (Corson, Gerrity, & Dobscha, 2004). Cronbach’s alphas ranged from .78-.90 over the assessment time points in this trial. Interviewer based depression severity was evaluated using the 17-item Ham-D (Hamilton, 1960). To ensure interrater reliability, one audiotape of the Ham-D assessment was randomly selected every 1 to 2 weeks for calibration ratings with all evaluators. The mean interclass correlations were .96.
Data Analysis
Baseline demographic variables were compared across treatment arms using t-tests and chi-square tests of association. WAI-C and WAI-T totals and subscores were compared across demographics using mixed models incorporating ratings at 4 and 14 weeks, as well as a random subject effect nested within therapist. Missing alliance measures at week 14 were imputed based on week 4 values.
All participants that completed at least two post-baseline assessments were included in analyses examining the effects of WAI on depression. The current study fit separate mixed linear models for early response (during treatment) as well as late response (post treatment). Models adjusted for Ham-D or PHQ-9 scores at all time points prior to the assessment of alliance. Models also controlled for week of assessment of TA, covariates that were significantly related to treatment arm or WAI scores, and the random effect of client within therapist, which were used to examine the main effect of TA on end of treatment and post-treatment follow-up Ham-D and PHQ-9 scores.
Results
Participants
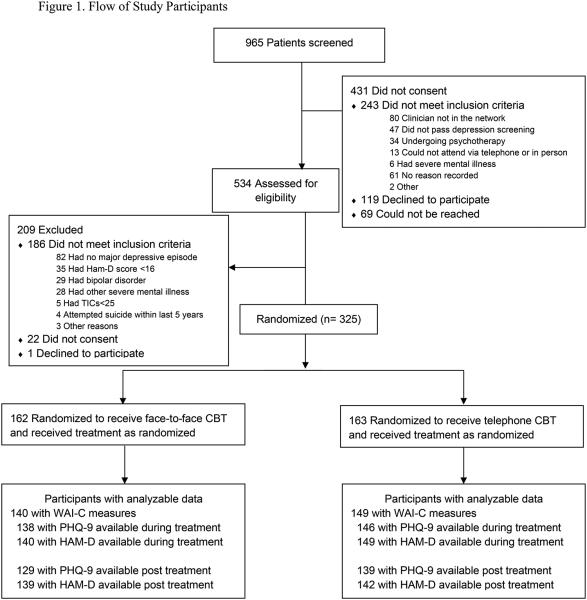
The flow of participants through this study is displayed in Figure 1. Due to failure to complete the measure, WAI-C data for 149 T-CBT and 140 FtF-CBT participants and WAI-T data for 153 T-CBT and 138 FtF-CBT participants were included. Significantly more treatment dropout occurred for FtF participants at Week 4 (Mohr et al., 2012), contributing to significant differences in assessment completion (p = .01). Participants with missing WAI data had significantly lower baseline depression scores on the PHQ-9 (p = .03), but did not differ on the Ham-D (p = .28) or any demographic variables (ps > .10). Baseline participant demographic and clinical characteristics are displayed in Table 1. Among the 325 participants entered into the trial, there were no significant differences in demographics across treatment groups.
Figure 1.
Ham-D indicates Hamilton Depression Rating Scale; TICS, Telephone Interview for Cognitive Status; PHQ-9, Patient Health Questionnaire-9; WAI-C, Working Alliance Inventory, Client version.
Table 1.
Participant Baseline Demographics and Psychiatric Characteristics
| Variable | FtF-CBT (n=162) |
T-CBT (n=163) |
p-value |
|---|---|---|---|
| Age, M (SD) | 47.5 (13.5) | 47.8 (12.6) | .87 |
| Female, n (%) | 127 (78.4) | 125(76.7) | .71 |
| Ethnicity, n (%) | |||
| Hispanic or Latino | 21 (13.0) | 23 (14.2) | .76 |
| Race, n (%) | |||
| African American | 36 (24.0) | 36 (24.3) | |
| Caucasian | 98 (65.3) | 89 (60.1) | .63 |
| More than one race | 12 (8.0) | 18 (12.2) | |
| Other | 4 (2.7) | 5 (3.4) | |
| Married/Cohabitating, n (%) | 51 (31.7) | 56 (34.4) | .61 |
| Education, n (%) | |||
| High School | 14 (8.6) | 20 (12.3) | |
| Some college | 41 (25.3) | 40 (24.5) | .57 |
| Bachelor’s Degree | 64 (39.5) | 55 (33.7) | |
| Advanced Degree | 43 (26.5) | 48 (29.4) | |
| Ham-D, M (SD) | 22.8 (4.6) | 22.9 (4.6) | .77 |
| PHQ-9, M (SD) | 16.4 (4.8) | 17.2 (4.7) | .12 |
| On active dose of antidepressant medication, n (%) |
56 (34.6) | 54 (33.1) | .78 |
Note. FtF-CBT = Face-to-Face Cognitive Behavioral Therapy; T-CBT = Telephone Cognitive Behavioral Therapy; Ham-D = Hamilton Depression Rating; PHQ-9 = Patient Health Questionnaire-9.
Therapeutic Alliance
There was a significant difference in WAI-C and subscales across gender, where female clients consistently reported higher scores for the total score and all subscales (ps between .001-.04, Cohen’s d between .13-.25). There was no difference in WAI-T by gender, nor differences in WAI-C or WAI-T by age, education, employment, household income, or race (ps > .12). The least square estimated means and standard errors for the WAI-C and WAI-T scales are displayed in Table 2. There were no significant differences in WAI-C or WAI-T total scores between T-CBT and FtF-CBT (Cohen’s f2 ranged from 0-.01, all ps > .05).
Table 2.
Comparison of treatment groups by the least square estimated means for the WAI adjusted for gender and random effect of therapist (Mean [Standard Error], unless otherwise indicated)
| Week 4 |
|||||
|---|---|---|---|---|---|
| FtF-CBT Mean (SE) |
T-CBT Mean (SE) |
Mean Difference between groups (Confidence Intervals) |
p-value | Cohen’s f2 |
|
| Therapist | n = 138 | n = 153 | |||
| Total | 66.7 (1.78) | 66.7 (1.76) | −0.03 (−2.02, 1.97) | 0.98 | <0.001 |
| Task | 21.4 (0.66) | 21.7 (0.65) | −0.25 (−1.01, 0.52) | 0.53 | 0.001 |
| Bond | 22.8 (0.59) | 22.5 (0.58) | 0.26 (−0.42, 0.94) | 0.46 | 0.002 |
| Goal | 22.5 (0.67) | 22.6 (0.67) | −0.04 (−0.73, 0.65) | 0.91 | <0.001 |
| Client | n = 140 | n = 149 | |||
| Total | 49.9 (0.64) | 49.7 (0.61) | 0.21 (−1.27, 1.68) | 0.78 | <0.001 |
| Task | 23.3 (0.36) | 23.4 (0.34) | −0.08 (−0.94, 0.78) | 0.86 | <0.001 |
| Bond | 21.9 (0.44) | 22.0 (0.42) | −0.15 (−1.11, 0.82) | 0.76 | <0.001 |
| Goal | 16.5 (0.21) | 15.9 (0.20) | 0.52 (−0.01, 1.04) | 0.053 | 0.013 |
|
|
|||||
| Week 14 |
|||||
| FtF-CBT | T-CBT | Mean Difference between groups (Confidence Intervals) |
p-value | Cohen’s f2 |
|
|
|
|||||
| Therapist | n = 138 | n = 153 | |||
| Total | 70.7 (1.68) | 70.1 (1.64) | 0.61 (−1.26, 2.48) | 0.52 | 0.002 |
| Task | 23.2 (0.64) | 22.7 (0.62) | 0.50 (−0.27, 1.26) | 0.21 | 0.007 |
| Bond | 24.1 (0.52) | 24.0 (0.50) | 0.07 (−0.55, 0.70) | 0.82 | <0.001 |
| Goal | 23.5 (0.64) | 23.5 (0.62) | 0.04 (−0.61, 0.69) | 0.91 | <0.001 |
| Client | n = 140 | n = 149 | |||
| Total | 51.6 (0.70) | 50.8 (0.65) | 0.77 (−0.84, 2.37) | 0.35 | 0.003 |
| Task | 23.9 (0.36) | 23.7 (0.33) | 0.24 (−0.63, 1.11) | 0.58 | 0.001 |
| Bond | 23.1 (0.47) | 22.7 (0.44) | 0.41 (−0.54, 1.36) | 0.40 | 0.002 |
| Goal | 16.6 (0.24) | 16.2 (0.22) | 0.38 (−0.20, 0.97) | 0.20 | 0.006 |
Note. FtF-CBT = Face-to-Face Cognitive Behavioral Therapy; T-CBT = Telephone Cognitive Behavioral Therapy; WAI = Working Alliance Inventory.
Relationship between Therapeutic Alliance and Depression Outcomes Between Treatments
The results of mixed linear models evaluating the relationship between the WAI and depression outcomes during post-treatment and follow-up are displayed in Table 3.
Table 3.
Relationship between WAI and changes in HAM-D and PHQ-9 scores during and post treatment, Ham-D or PHQ-9 scores at all time points prior to the assessment of alliance, week, and random effect of therapist
| Ham-D (WAI-C) | Ham-D (WAI-T) | PHQ-9 (WAI-C) | PHQ-9 (WAI-T) | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Time Point | Covariates | p | Cohen’s f2 | p | Cohen’s f2 | p | Cohen’s f2 | P | Cohen’s f2 |
| Treatment | Total | <0.001 | 0.018 | 0.008 | 0.016 | <0.001 | 0.029 | <0.001 | 0.021 |
| Total*Group | 0.78 | 0.000 | 0.07 | 0.004 | 0.99 | 0.000 | 0.34 | 0.002 | |
|
| |||||||||
| Post Treatment | Total | 0.55 | 0.000 | 0.48 | 0.000 | 0.12 | 0.001 | 0.60 | 0.000 |
| Follow-Up | Total*Group | 0.33 | 0.000 | 0.85 | 0.000 | 0.36 | 0.000 | 0.72 | 0.000 |
Note: Ham-D = Hamilton Depression Rating; PHQ-9 = Patient Health Questionnaire-9; WAI = Working Alliance Inventory; WAI-C = Working Alliance Inventory, client version; WAI-T = Working Alliance Inventory, therapist version. Main effect regression parameter estimates are from separate models without the interactions of Working alliance and group.
Treatment
The WAI-C total score was significantly related to reductions in depression during treatment for both the Ham-D (β = -.15, p < .001) and the PHQ-9 (β = -.12, p < .001). There were no significant interactions between the WAI-C total score with treatment for either the Ham-D (β = .001, p = .90) or the PHQ-9 (β = -.01, p = .85). Similarly, the WAI-T total score was significantly related to reductions in depression during treatment for both the Ham-D (β = -.11, p = .007) and the PHQ-9 (β = -.11, p < .001). There were no significant interactions between the WAI-T total score and treatment for the PHQ-9 (β = .05, p = .28).
Post-Treatment Follow-Up
The WAI-C total score was not significantly related to changes in depression during post-treatment follow-up for the Ham-D (β = -.01, p = .29) and the PHQ-9 (β = -.03, p = .07). There were no significant interactions between the WAI-C total score and treatment for either the Ham-D (β = -.07, p = .42) or the PHQ-9 (β = -.07, p = .33). The WAI-T total score was also not significantly related to reductions in depression during post-treatment follow-up for the Ham-D (β = -.04, p = .35) and the PHQ-9 (β = -.02, p = .52). There were no significant interactions between the WAI-T total score and treatment for either the Ham-D (β = .02, p = .76) or the PHQ-9 (β = -.00, p = .95).
Discussion
Consistent with our hypothesis, there were no significant differences in TA between telephone and FtF delivery of CBT. The findings of the present study were also consistent with previous studies showing that TA is significantly, albeit modestly related to end of treatment outcome for adults with depression receiving FtF-CBT and T-CBT. TA, however, was not a significant predictor of depression severity after the completion of treatment. Furthermore, the effect of global TA on depression outcomes did not vary by treatment delivery modality. These results were consistent for both the client and therapist perspectives of TA.
We saw no evidence of a difference between total alliance scores between FtF-CBT and T-CBT. T-CBT eliminates visual cues, but preserves non-verbal vocal cues such as prosody. Indeed, voice quality is a critical channel for conveying emotion (Eckman, Friesen, O’sullivan, & Scherer, 1980). These findings suggest that visual cues provide little additional utility above other non-verbal and verbal cues available via the telephone in supporting TA. As information and communications technologies continue to provide new media through which therapists and clients can interact, it will be important to understand how the limitations on cues provided affect the therapeutic relationship and treatment outcomes.
The primary outcome paper found that while T-CBT and FtF-CBT produced equivalent outcomes at post-treatment (Mohr et al., 2012), there was a small but statistically significant benefit for FtF-CBT over T-CBT at post-treatment follow-up. A subsequent commentary specifically suggested that differences in TA may have accounted for these differences (Sarkar & Gupta, 2012). The current findings do not support the role of TA in post-treatment differences.
To our knowledge, this is the first study to investigate the role of TA in predicting treatment outcome for an adult sample with depression receiving treatment administered FtF or by telephone. This study is also unique in its comparison of the perspectives of the therapist and client across these two methods of treatment delivery. The finding that TA and its effect on treatment outcome are not different in telephone therapy, compared to FtF therapy, is of clinical importance as telephone therapy provides an opportunity for clinicians to extend care to populations that experience barriers to initiating or adhering to treatment.
There are several limitations that should be considered in interpreting these data. First, statistical analyses are not designed to test for the null hypothesis. A non-inferiority analysis requires setting a margin that is defined by a generally accepted criterion for minimal clinical effectiveness; no such criteria exists for the WAI. However, we have provided the means and differences between treatments, which are all less than 1 point. These differences are not only statistically non-significant, but also appear to be clinically meaningless. Second, this trial examined FtF-CBT and T-CBT for depression; it is unclear how these results generalize to other forms of psychotherapy, mental health conditions, and treatment delivery media. Third, the use of the Ham-D, which has been critiqued as a weak index of depression (Gibbons, Clark, & Kupfer, 1993), is a weakness, however, the results are consistent across the Ham-D and the PHQ-9. Fourth, significant differences in assessment completion occurred between the groups. Finally, these were group analyses. We cannot exclude the possibility that there may be some individuals for whom T-CBT would not be indicated; indeed, we suspect this is the case. For example, patients with paranoid symptoms might require non-verbal cues to manage perceived ruptures in the therapeutic relationship. Future research will be needed to identify differential predictors of outcome for telephone-based and FtF treatments.
In summary, the findings of the present study indicate that there is no significant difference in TA in T-CBT, compared to FtF-CBT. TA is related to treatment outcome in CBT for depression, and this relationship does not vary whether the treatment is delivered FtF or by telephone. These findings suggest that therapists can be confident that delivering care by telephone will generally not have a negative impact on TA.
Acknowledgments
This research was supported by a grant from the National Institute of Mental Health R01 MH059708.
References
- Arnow BA, Steidtmann D, Blasey C, Manber R, Constantino MJ, Klein DN, Kocsis JH. The relationship between the therapeutic alliance and treatment outcome in two distinct psychotherapies for chronic depression. Journal of Consulting and Clinical Psychology. 2013 doi: 10.1037/a0031530. doi: 10.1037/a0031530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck JS. Cognitive Therapy: Basics and Beyond. Guilford Press; New York, NY: 1995. [Google Scholar]
- Beckner V, Vella L, Howard I, Mohr DC. Alliance in two telephone-administered treatments: relationship with depression and health outcomes. Journal of Consulting and Clinical Psychology. 2007;75(3):508–512. doi: 10.1037/0022-006X.75.3.508. doi: 10.1037/0022-006X.75.3.508. [DOI] [PubMed] [Google Scholar]
- Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research & Practice. 1979;16(3):252–260. doi: 10.1037/h0085885. [Google Scholar]
- Corson K, Gerrity MS, Dobscha SK. Screening for depression and suicidality in a VA primary care setting: 2 items are better than 1. American Journal of Managed Care. 2004;10:839–845. [PubMed] [Google Scholar]
- Daros AR, Zakzanis KK, Ruocco AC. Facial emotion recognition in borderline personality disorder. Psychological Medicine. 2012:1–11. doi: 10.1017/S0033291712002607. doi: 10.1017/S0033291712002607. [DOI] [PubMed] [Google Scholar]
- Day S. Psychotherapy using distance technology: A coparison of face-to-face, video, and audio treatments. Dissertation Abstracts International. 2000;60(11-B):5768. [Google Scholar]
- Del Re AC, Flückiger C, Horvath AO, Symonds D, Wampold BE. Therapist effects in the therapeutic alliance–outcome relationship: A restricted-maximum likelihood meta-analysis. Clinical Psychology Review. 2012;32(7):642–649. doi: 10.1016/j.cpr.2012.07.002. [DOI] [PubMed] [Google Scholar]
- Dwight-Johnson M, Sherbourne CD, Liao D, Wells KB. Treatment Preferences Among Depressed Primary Care Patients. Journal of General Internal Medicine. 2000;15(8):527–534. doi: 10.1046/j.1525-1497.2000.08035.x. doi: 10.1046/j.1525-1497.2000.08035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckman P, Friesen WV, O’Sullivan M, Scherer K. Relative importance of face, body, and speech in judgments of personality and affect. Journal of Personality and Social Psychology. 1980;38(2):270–277. [Google Scholar]
- Gibbons Robert D., Clark David C., Kupfer David J. Exactly what does the Hamilton depression rating scale measure? Journal of Psychiatric Research. 1993;27(3):259–273. doi: 10.1016/0022-3956(93)90037-3. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery & Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatcher RL, Gillaspy JA. Development and validation of a revised short version of the working alliance inventory. Psychotherapy Research. 2006;16(1):12–25. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Mrikangas KR, Wang PS. The epidemiology of major depressive disorder: Results from the national comorbidity survey replication (ncs-r) JAMA. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals. 2002;32:509–515. [Google Scholar]
- Lingely-Pottie P, McGrath PJ. A therapeutic alliance can exist without face-to-face contact. Journal of Telemedicine and Telecare. 2006;12(8):396–399. doi: 10.1258/135763306779378690. doi: 10.1258/135763306779378690. [DOI] [PubMed] [Google Scholar]
- Martin DJ, Garske JP, Davis MK. Relation of the therapeutic alliance with outcome and other variables: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2000;68(3):438–450. doi: 10.1037/0022-006x.68.3.438. [PubMed] [Google Scholar]
- Mohr DC, Hart S, Howard I, Julian L, Vella L, Catledge C, Feldman M. Barriers to psychotherapy among depressed and nondepressed primary care patients. Annals of Behavioral Medicine. 2006;32(3):254–258. doi: 10.1207/s15324796abm3203_12. doi: 10.1207/s15324796abm3203_12. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Hart SL, Julian L, Catledge C, Honos-Webb L, Vella L, Tasch ET. Telephone-administered psychotherapy for depression. Archives of General Psychiatry. 2005;62(9):1007–1014. doi: 10.1001/archpsyc.62.9.1007. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Ho J, Siddique J. Telephone vs face-to-face cognitive behavioral therapy for depression—reply. JAMA. 2012;308(11):1090–1091. doi: 10.1001/2012.jama.10723. doi: 10.1001/2012.jama.10729. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Ho J, Duffecy J, Baron KG, Lehman KA, Jin L, Reifler D. Perceived barriers to psychological treatments and their relationship to depression. Journal of Clinical Psychology. 2010;66(4):394–409. doi: 10.1002/jclp.20659. doi: 10.1002/jclp.20659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr DC, Ho J, Duffecy J, Reifler D, Sokol L, Burns MN, Siddique J. Effect of telephone-administered vs face-to-face cognitive behavioral therapy on adherence to therapy and depression outcomes among primary care patients: a randomized trial. JAMA. 2012;307(21):2278–2285. doi: 10.1001/jama.2012.5588. doi: 10.1001/jama.2012.5588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr DC, Likosky W, Bertagnolli A, Goodkin DE, Van Der Wende J, Dwyer P, Dick LP. Telephone-administered cognitive-behavioral therapy for the treatment of depressive symptoms in multiple sclerosis. Journal of Consulting and Clinical Psychology. 2000;68(2):356–361. doi: 10.1037//0022-006x.68.2.356. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Vella L, Hart S, Heckman T, Simon G. The effect of telephone-administered psychotherapy on symptoms of depression and attrition: A meta-analysis. Clinical Psychology: Science and Practice. 2008;15(3):243–253. doi: 10.1111/j.1468-2850.2008.00134.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munder T, Wilmers F, Leonhart R, Linster HW, Barth J. Working Alliance Inventory-Short Revised (WAI-SR): psychometric properties in outpatients and inpatients. Clinical Psychology and Psychotherapy. 2010;17(3):231–239. doi: 10.1002/cpp.658. doi: 10.1002/cpp.658. [DOI] [PubMed] [Google Scholar]
- Reese RJ, Conoley CW, Brossart DF. Effectiveness of telephone counseling: A field-based investigation. Journal of Counseling Psychology. 2002;49(2):233–242. doi: 10.1037/0022-0167.49.2.233. [Google Scholar]
- Sarkar S, Gupta R. Telephone vs face-to-face cognitive behavioral therapy for depression. JAMA. 2012;308(11):1090–1091. doi: 10.1001/2012.jama.10723. doi: 10.1001/2012.jama.10723. [DOI] [PubMed] [Google Scholar]
- Simon GE, Ludman EJ, Tutty S, Operskalski B, Von Korff M. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trial. JAMA. 2004;292(8):935–942. doi: 10.1001/jama.292.8.935. [DOI] [PubMed] [Google Scholar]
- Vallis TM, Shaw BF, Dobson KS. The Cognitive Therapy Scale: Psychometric properties. Journal of Consulting and Clinical Psychology. 1986;54(3):381–385. doi: 10.1037//0022-006x.54.3.381. [DOI] [PubMed] [Google Scholar]