Abstract
Purpose
To assess the impact of weight loss on health-related quality-of-life (HRQL), to describe the factors associated with improvements in HRQL after weight loss, and to assess the relationship between obesity as assessed by body mass index (BMI) and HRQL before and after weight loss.
Methods
We studied 188 obese patients with BMI ≥32 kg/m2 with one or more comorbidities or ≥35 kg/m2. All patients had baseline and follow-up assessments of BMI and HRQL using the EuroQol (EQ-5D) and its visual analog scale (VAS) before and after 6 months of medical weight loss that employed very low calorie diets, physical activity, and intensive behavioral counseling.
Results
At baseline, age was 50 ± 8 years (mean ± SD), BMI was 40. 0 ± 5.0 kg/m2, EQ-5D-derived health utility score was 0.85 ± 0.13, and VAS-reported quality-of-life was 0.67 ± 0.18. At 6 months follow-up, BMI decreased by 7.0 ± 3.2 kg/m2, EQ-5D increased by 0.06 (interquartile range (IQR) 0.06 – 0.17), and VAS increased by 0.14 (IQR 0.04 – 0.23). In multivariate analyses, improvement in EQ-5D and VAS were associated with lower baseline BMI, greater reduction in BMI at follow-up, fewer baseline comorbidities, and lower baseline HRQL. For any given BMI category, EQ-5D and VAS tended to be higher at follow-up than at baseline.
Conclusion
Measured improvements in HRQL between baseline and follow-up were greater than predicted by the reduction in BMI at follow-up. If investigators use cross-sectional data to estimate changes in HRQL as a function of BMI, they will underestimate the improvement in HRQL associated with weight loss and underestimate the cost-utility of interventions for obesity treatment.
Introduction
Cost-effectiveness analysis describes the cost per unit health outcome obtained with an experimental intervention versus usual care [1]. It provides a measure of the value obtained for the money spent and may be used to guide resource allocation. In cost-utility analysis, health outcomes are measured by quality-adjusted life-years (QALYs), a metric that adjusts length of life for quality-of-life. Quality-of-life is assessed with health utility scores, measures that reflect the general population’s preference for specific health states. Health utility scores fall on a continuum between 1.0 and 0 where 1.0 represents perfect health and 0 represents death. QALYs are calculated as the sum of the product of the number of years of life and the quality-of-life in each of those years. The goal of an experimental intervention is to maximize the number of QALYs-gained for the money spent relative to usual care.
Although conceptually straightforward, measurement of health utility scores may be difficult and time consuming [1]. To simplify the assessment of health utility scores, multi-attribute utility models have been developed [1]. The EQ-5D is a simple and widely used multi-attribute utility model that assesses 5 dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression according to 3 levels: no problems, some problems, extreme problems [2]. Patient-reported responses are weighted according to the preferences of an independent sample of judges to place the health status of the individual on a continuum between perfect health and death. The accompanying visual analog scale (VAS) records the patient’s self-reported health on a vertical scale where the endpoints are labeled “best imaginable health state” and “worst imaginable health state”. The point selected on the scale provides a quantitative measure of the health outcome as judged by the individual.
Although not without controversy, body mass index (BMI), calculated as weight in kilograms divided by the square of height in meters, is commonly used to define obesity [3,4]. An individual with BMI 18.5 to 24.9 kg/m2 is considered to be normal weight, 25.0 to 29.9 kg/m2 to be overweight, ≥30 kg/m2 to be obese, and ≥40 kg/m2 to be extremely obese. Approximately 33% of US adults are overweight, 36% are obese, and 6% are extremely obese [5]. Obesity increases the risk for many chronic conditions including type 2 diabetes and cardiovascular disease and negatively impacts quality-of-life. Although a large body of evidence has demonstrated the effectiveness of interventions for the treatment of obesity, there is less evidence to demonstrate the cost-utility of such interventions, and the published evidence has been inconsistent [6]. The degree of improvement in HRQL is a major determinant of the cost-utility of weight loss interventions and part of the inconsistency in the results of published cost-utility analyses relates to uncertainty regarding the impact of weight loss on HRQL.
Many investigators have assessed the cross-sectional relationship between body mass index (BMI) and health utility scores [7–9] and have reported changes in health utility scores for each kg/m2 unit difference in BMI [10–13] or difference in weight category [14–18]. A few investigators have prospectively assessed improvements in health utility scores for each kilogram lost [19,20] or percent of weight lost over 1 year [21]. Most previous studies have assumed that HRQL is determined by BMI and that after weight loss, an obese individual’s HRQL is the same as that for a person with the same BMI who did not lose weight [6]. To the extent that an obese individual underestimates the impact of his pre-intervention weight on HRQL, and to the extent that his HRQL after weight loss is better than predicted by his reduced BMI, cost-utility analyses will underestimate the value of obesity treatments.
In this study, we prospectively assessed the impact of a medical weight management program on HRQL, described the factors associated with improvements in HRQL after weight loss, and assessed the relationship between BMI and HRQL before and after weight loss.
Methods
We studied 188 obese patients with BMI ≥32 kg/m2 with one or more co-morbidities or ≥35 kg/m2. All patients participated in the University of Michigan Weight Management Program for at least 6 months. Patients who enrolled in the program were seen by a physician for an initial assessment, at one month, and quarterly thereafter. They were seen weekly by a dietitian during the first month, twice monthly for the next 2 months, and monthly thereafter. The initial 12 to 16 weeks of the program employed a very low calorie diet in the form of total meal replacement. Over the first 12 to 16 weeks of the program, patients were also asked to gradually increase their physical activity (low to moderate intensity) to 40 minutes per day. After 12 to 16 weeks, patients were transitioned to regular food stuffs and asked to perform 40 to 90 minutes of moderate to vigorous physical activity per day. All participants had baseline and follow-up assessments of BMI and HRQL using the EuroQoL (EQ-5D) and its visual analog scale (VAS). The study protocol was reviewed and approved by the University of Michigan Institutional Review Board and all participants provided written informed consent.
Three-hundred forty-eight patients initially met eligibility criteria and were enrolled in the weight management program between January 4, 2010 and May 30, 2012. Of those, 277 (80%) were still enrolled in the program at their scheduled 6 month visit, and 188 of them (68%) had BMI measured and EQ-5D and VAS data collected and were included in the study. Compared to persons enrolled in the program at the 6 month follow-up visit (n=277), those who dropped out before 6 months (n=71) were younger (47 ± 9 vs. 50 ± 8 years, p=0.006), had less education (39% vs. 21% <college graduate, p=0.02), and were less likely to be employed (68% vs. 80% employed, p=0.02). Compared to those who were in the program at 6 months and who had complete data (n=188), those who were missing at least one variable (n=89) had higher BMI at baseline (41.5 ± 6.4 vs. 40.0 ± 5.0, p=0.04). There were no differences between participants and nonparticipants with respect to sex, race/ethnicity, marital status, smoking, physical activity, baseline comorbidities, or number of comorbidities.
Initially, we described the percent distribution for categorical variables and the mean ± standard deviation for normally distributed, or median ± interquartile range (IQR) for non-normally distributed continuous variables. We assessed five comorbidities at baseline: hypertension, dyslipidemia, diabetes, osteoarthritis, and depression, and constructed a variable for the mean number of comorbidities as an unweighted sum of the number of comorbidities. We described the changes in BMI, weight, and HRQL from baseline to 6 months follow-up. We then explored the univariate associations among the baseline sociodemographic and clinical characteristics, comorbidities, and changes in BMI and weight, with changes in HRQL.
Next, we constructed multivariate linear regression models to assess the impact of weight loss on HRQL after adjusting for the covariates significant in the univariate analyses. We constructed two separate models, one using change in EQ-5D as the outcome and the other using change in VAS as the outcome. Both models included baseline BMI, change in BMI from baseline to 6 months follow-up, number of comorbidities at baseline, and baseline HRQL (EQ-5D or VAS as appropriate). For modeling purposes, the change in HRQL was constructed as follow-up EQ-5D or VAS minus baseline EQ-5D or VAS so that positive results indicated improvements in HRQL. Change in BMI was constructed as baseline BMI minus follow-up BMI so that positive results indicated weight loss.
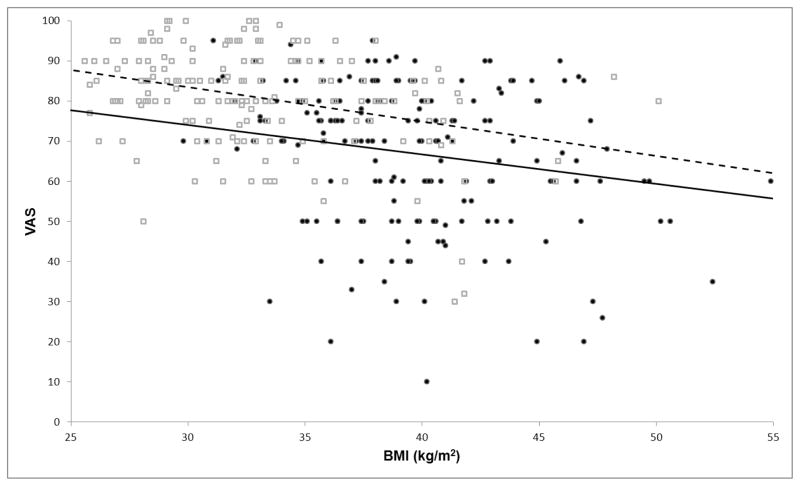
To assess the impact of weight loss on the association between HRQL and BMI, we assessed mean EQ-5D and VAS within BMI categories before and after weight loss and calculated the change in scores within categories. We also constructed scatter plots using solid circles for baseline data and open squares for follow-up data with HRQL on the y-axis and BMI on the x-axis. Because of a ceiling effect for EQ-5D-derived utility scores, we only present the scatter plot for the VAS data. We then overlaid the corresponding regression lines to visualize the association between VAS and BMI at baseline and follow-up. To test whether the two lines were different, we first tested to determine if there was a time by BMI interaction. We then used a linear regression model to determine if there was a significant difference in the association between VAS and BMI at baseline and follow-up.
Results
At baseline, mean age for the 188 participants was 50 ± 8 years (mean ± SD), 52% of the participants were women, and 87% were white (Table 1). Mean baseline BMI was 40.0 ± 5.0 kg/m2. A 5 feet 10 inch tall man with a BMI of 40 kg/m2 would weigh 278 pounds or 126 kg, and a 5 feet 4 inch tall woman with a BMI of 40 kg/m2 would weigh 233 pounds or 106 kg. Comorbidities were common: 51% of participants had hypertension, 45% had dyslipidemia, 27% had type 2 diabetes, 26% had osteoarthritis, and 18% had depression. The mean number of comorbidities was 1.7 ± 1.3. Baseline EQ-5D was 0.85 ± 0.13 and baseline VAS was 0.67 ± 0.18. At baseline, 62 (33%) of participants had EQ-5D-derived health utility scores of 1.0 but none had VAS-reported quality-of-life of 1.0.
Table 1.
Baseline characteristics of study participants* (n=188)
| Characteristics | |
|---|---|
| Age in years | 50 ± 8 |
| Female sex | 97 (52%) |
| Non-Hispanic white race/ethnicity | 163 (87%) |
| Education | |
| Some high school or high school grad | 8 (4%) |
| Vocational college or some college | 30 (16%) |
| College graduate | 80 (43%) |
| Professional or graduate degree | 70 (37%) |
| Employment | |
| Employed | 146 (78%) |
| Retired | 21 (11%) |
| Keeping house | 18 (10%) |
| Other | 3 (2%) |
| Marital status | |
| Married | 169 (90%) |
| Current smoker (missing=3) | 8 (4%) |
| Physical activity (missing=42) | |
| No physical activity weekly | 7 (5%) |
| Only light physical activity most weeks | 87 (60%) |
| Vigorous for 20 min 1–2 times per week | 22 (15%) |
| Vigorous for 20 min 3+ times per week | 30 (21%) |
| Comorbidities (missing=1) | |
| Hypertension | 96 (51%) |
| Dyslipidemia | 84 (45%) |
| Diabetes | 51 (27%) |
| Osteoarthritis | 49 (26%) |
| Depression | 33 (18%) |
| Number of comorbidities (0 to 5) (missing=1) | 1.7 ± 1.3 |
| Body mass index (kg/m2) | 40.0 ± 5.0 |
| EQ-5D | 0.85 ± 0.13 |
| VAS | 0.67 ± 0.18 |
Results are expressed as mean ± standard deviation or number (%)
At 6 months follow-up, mean weight loss was 45 ± 22 lbs (range −111 to +2 lbs) or 20.5 ± 10.1 kg (range −50.6 to +0.7 kg) and mean BMI decreased by 7.0 ± 3.2 kg/m2 (range −16.1 kg/m2 to +0.2 kg/m2). Mean increase in EQ-5D was 0.06 (IQR 0.00 to 0.17) and mean increase in VAS was 0.14 (IQR 0.4 to 0.23). At follow-up, 102 (54%) of participants had EQ-5D-derived health utility scores of 1.0 and 5 (3%) had VAS-reported quality-of-life of 1.0. Mean increase in EQ-5D was 0.004 per kilogram lost and 0.01 per unit decrease in BMI. Mean increase in VAS was 0.01 per kilogram lost and 0.03 per unit decrease in BMI.
In univariate analysis, only baseline BMI was associated with change in EQ-5D or VAS. In multivariate analyses, factors associated with increase in EQ-5D and VAS at follow-up included lower baseline BMI, greater reduction in BMI at follow-up, fewer baseline comorbidities, and lower baseline HRQL (Table 2). The models explained 48% of the variance in improvement in EQ-5D and to 60% of the variance in improvement in VAS.
Table 2.
Factors associated with change in health-related quality-of-life as assessed by the EQ-5D or visual analog scale (VAS) between baseline and 6 months follow-up.
| EQ-5D | ||
|---|---|---|
| Variable | Parameter Estimate* | P-value |
| Intercept | 0.71995 | <0.0001 |
| Baseline EQ-5D score | −0.68279 | <0.0001 |
| Baseline BMI | −0.000285 | 0.0688 |
| Baseline number of comorbidities | −0.00957 | 0.0774 |
| Change in BMI | 0.00730 | 0.0023 |
| VAS | ||
|---|---|---|
| Variable | Parameter Estimate | P-value |
| Intercept | 0.75919 | <0.0001 |
| Baseline VAS | −0.00701 | <0.0001 |
| Baseline BMI | −0.00524 | 0.0020 |
| Baseline number of comorbidities | −0.01295 | 0.0321 |
| Change in BMI | 0.01155 | <0.0001 |
A negative parameter estimate for baseline variables indicates that a lower baseline value is associated with greater improvement in HRQL at follow-up. A positive parameter estimate for change in BMI indicates that a greater reduction in BMI is associated with greater improvement in HRQL at follow-up.
To determine whether the association between BMI and HRQL differed before and after weight loss, we assessed mean EQ-5D and VAS scores within BMI categories before and after weight loss and calculated the change in scores within categories. For any given BMI category, EQ-5D and VAS tended to be higher at follow-up than at baseline (Table 3). For example, before weight loss, a BMI of 35.0 to 35.9 kg/m2 was associated with EQ-5D of 0.86 and VAS of 0.68. After weight loss, it was associated with EQ-5D of 0.89 and VAS of 0.79, differences of 0.03 and 0.11 respectively. We also constructed a scatter plot showing VAS before and after weight loss as a function of BMI. For any given BMI, VAS was significantly higher at follow-up than at baseline (Figure 1).
Table 3.
Mean BMI and HRQOL at baseline and 6 month follow-up stratified by BMI category.
| Baseline | 6 month follow-up | ||||||
|---|---|---|---|---|---|---|---|
| BMI category | N | Mean BMI | Mean EQ-5D | N | Mean BMI | Mean EQ-5D | Change in EQ-5D |
| 25.0 – 29.9 | -- | -- | -- | 57 | 28.0 | 0.94 | -- |
| 30.0 – 34.9 | 26 | 33.2 | 0.91 | 77 | 32.4 | 0.91 | + 0.00 |
| 35.0 – 39.9 | 79 | 37.6 | 0.86 | 34 | 37.1 | 0.89 | + 0.03 |
| 40.0 – 44.9 | 55 | 41.9 | 0.84 | 16 | 41.1 | 0.86 | + 0.02 |
| 45.0+ | 28 | 48.8 | 0.78 | 4 | 47.5 | 0.84 | + 0.06 |
| Baseline | 6 month follow-up | ||||||
|---|---|---|---|---|---|---|---|
| BMI category | N | Mean BMI | Mean VAS | N | Mean BMI | Mean VAS | Change in VAS |
| 25.0 – 29.9 | -- | -- | -- | 57 | 28.0 | 0.86 | -- |
| 30.0 – 34.9 | 26 | 33.2 | 0.76 | 77 | 32.4 | 0.81 | + 0.05 |
| 35.0 – 39.9 | 79 | 37.6 | 0.68 | 34 | 37.1 | 0.79 | + 0.11 |
| 40.0 – 44.9 | 55 | 41.9 | 0.63 | 16 | 41.1 | 0.69 | + 0.06 |
| 45.0+ | 28 | 48.8 | 0.61 | 4 | 47.5 | 0.73 | + 0.12 |
Fig. 1.
Scatter plot and regression lines showing association between body mass index (BMI) and visual analog scale (VAS) at baseline (solid circles and solid line) and 6 months follow-up (open squares and broken line)*
*Baseline VAS = 96.08007 – 0.734808*baseline BMI. Follow-up VAS = 109.2474 – 0.858713*follow-up BMI. There is a statistically significant difference in VAS between baseline and follow-up (p<0.0001).
Discussion
A medical weight management program that involved very low calorie diet, physical activity, and intensive behavioral counseling resulted in substantial weight loss and improved HRQL. Mean weight loss at 6 months was 45 ± 22 pounds or 20.5 ± 10.1 kg, mean improvement in EQ-5D was 0.06, and mean improvement in VAS was 0.14. Obese participants with lower baseline BMI, greater reduction in BMI from baseline to follow-up, fewer baseline comorbidities, and poorer baseline HRQL had greater improvements in HRQL at follow-up.
The relatively modest improvement in EQ-5D-derived health utility scores compared to the improvement in VAS-reported quality-of-life, and the observation that participants with poorer baseline HRQL had greater improvements in HRQL at follow-up were both likely due to a ceiling effect for the EQ-5D. At baseline and follow-up, one-third and over one-half of participants had EQ-5D of 1.0. In contrast, at baseline, no participants had VAS of 1.0 and at follow-up, only 3% had VAS of 1.0. Although simple, brief, and widely used, the EQ-5D measures only three levels of functioning in five dimensions and has been criticized for being insensitive and for having a pronounced ceiling effect [2]. The newly developed 5 level version of the EQ-5D (EQ-5D-5L) assesses the same dimensions as the EQ-5D, but each dimension has 5 levels: no problems, slight problems, moderate problems, severe problems, and extreme problems [2]. Compared to the EQ-5D, the EQ-5D-5L has better measurement properties and discriminatory power and a less pronounced ceiling effect [22]. Future studies should consider incorporating the EQ-5D-5L or a different multi-attribute utility model that assesses additional dimensions and symptoms, provides greater sensitivity and has a less pronounced ceiling effect.
Measured improvements in VAS between baseline and follow-up were greater than predicted by the reduction in BMI at follow-up. Our results confirm the results of previous studies that have suggested that the improvement in HRQL for each kilogram lost [19,20] or percent of body weight lost [21] is greater than would be predicted by assessing the cross-sectional relationship between body mass index and HRQL and assuming that an obese individuals health-related quality-of-life after weight loss is the same as that for a person with the same BMI who did not lose weight [10–13].
At baseline, patients appeared to underestimate the negative impact of obesity on HRQL and after weight loss, reported significantly better HRQL for any given BMI category. Failure to use a sensitive instrument and failure to empirically assess HRQL both before and after weight loss will underestimate the improvement in HRQL associated with weight loss and underestimate the cost-utility of interventions for obesity treatment.
There are a number of limitations to our study. First, our study was conducted in a clinical setting. Our results may not apply to the general population. Second, there was 20% dropout from our program at 6 months and a number of participants failed to have BMI measured or to complete the EQ-5D and VAS at 6 months. Fortunately, there were not substantial differences between participants and non-participants. Third, we studied a relatively small population. The limited sample size reduced our power to detect potentially important associations. Fourth, we only evaluated the impact of a medical weight management program on HRQL. We cannot determine how the individual components of the intervention (diet, physical activity, and behavioral counseling) impacted HRQL or whether changes in HRQL would be the same with pharmacologic or surgical interventions. Fifth, we assessed the impact of short-term weight loss on HRQL. The impact of weight loss on long-term HRQL might be even greater than we reported. Finally, we only assessed the impact of weight loss on HRQL. Weight gain would likely have a different impact on health utility scores than weight loss.
In conclusion, the degree of improvement in HRQL with medical weight loss is substantial and is associated with baseline BMI, the reduction in BMI, baseline comorbidities, and baseline HRQL. If investigators employ multi-attribute utility models that are more sensitive than the EQ-5D and have a less pronounced ceiling effect, measured improvements in HRQL associated with weight loss may be even larger than we observed. If investigators fail to empirically measure HRQL before and after weight loss, and instead use cross-sectional data to estimate changes in utility scores as a function of BMI alone, they will underestimate the impact of weight loss on HRQL and the cost-utility of interventions for obesity treatment.
Acknowledgments
The work was supported by Grant Number DK089503 (MNORC) and Grant Number P30DK092926 (MCDTR) from the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health. Additional support was provided by the A. Alfred Taubman Medical Institute and the Robert C. and Veronica Atkins Foundation.
References
- 1.Gold MR, Siegel JE, Russell LB, Weinstein MC, editors. Cost-Effectiveness in Health and Medicine. New York: Oxford University Press; 1996. [Google Scholar]
- 2.EQ-5D-5L User Guide. [Accessed July 17, 2013];Basic information on how to use the EQ-5D-5L instrument. Version 1.0. 2011 Apr; http://www.euroqol.org/fileadmin/user_upload/Documenten/PDF/Folders_Flyers/UserGuide_EQ-5D-5L.pdf.
- 3.Zhu SK, Wang ZM, Heshka S, Heo M, Faith MS, Heymsfield SB. Waist circumference and obesity-associated risk factors among whites in the third National Health and Nutrition Examination Survey: clinical action thresholds. Am J Clin Nutr. 2002;76:743–749. doi: 10.1093/ajcn/76.4.743. [DOI] [PubMed] [Google Scholar]
- 4.Wildman RP, Gu D, Reynolds K, Duan X, He J. Appropriate body mass index and waist circumference cutoffs for categorization of overweight and central adiposity among Chinese adults. Am J Clin Nutr. 2004;80:1129–1136. doi: 10.1093/ajcn/80.5.1129. [DOI] [PubMed] [Google Scholar]
- 5.WIN Weight-control Information Network. [Accessed July 19, 2013.];Overweight and Obesity Statistics. http://www.win.niddk.nih.gov/statistics/
- 6.Rothberg AE, Peeters A, Herman WH. The Cost-Effectiveness of Obesity Prevention and Treatment. In: Bray GA, Bouchard C, editors. Handbook of Obesity Vol 2: Clinical Applications. 4. London, England: Informa Healthcare; In press. In press. [Google Scholar]
- 7.Doyle S, Lloyd A, Moore L, Ray J, Gray A. A systematic review and critical assessment of health state utilities. Weight change and type 2 diabetes mellitus. Pharmacoeconomics. 2012;30:1133–1143. doi: 10.2165/11599420-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 8.Kortt MA, Dollery B. Association between body mass index and health-related quality of life among an Australian sample. Clin Ther. 2011;33:1466–1474. doi: 10.1016/j.clinthera.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 9.Dennett SL, Boye KS, Yurgin NR. The impact of body weight on patient utilities with or without type 2 diabetes: A review of the medical literature. Value Health. 2008;11:478–486. doi: 10.1111/j.1524-4733.2007.00260.x. [DOI] [PubMed] [Google Scholar]
- 10.Craig BM, Tseng DS. Cost-effectiveness of gastric bypass for severe obesity. Am J Med. 2002;113:491–498. doi: 10.1016/s0002-9343(02)01266-4. [DOI] [PubMed] [Google Scholar]
- 11.Hakim Z, Wolf A, Garrison LP. Estimating the effect of changes in body mass index on health state preferences. Pharmacoeconomics. 2002;20:393–404. doi: 10.2165/00019053-200220060-00004. [DOI] [PubMed] [Google Scholar]
- 12.Kortt MA, Clarke PM. Estimating utility values for health states of overweight and obese individuals using the SF-36. Qual Life Res. 2005;14:2177–2185. doi: 10.1007/s11136-005-8027-6. [DOI] [PubMed] [Google Scholar]
- 13.Soltoft F, Hammer M, Kragh N. The association of body mass index and health-related quality of life in the general population: Data from the 2003 Health Survey of England. Qual Life Res. 2009;18:1293–1299. doi: 10.1007/s11136-009-9541-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Trakas K, Oh PI, Singh S, et al. The health status of obese individuals in Canada. Int J Obes Relat Metab Disord. 2001;25:662–668. doi: 10.1038/sj.ijo.0801591. [DOI] [PubMed] [Google Scholar]
- 15.Livingston EH, Ko CY. Use of the health and activities limitation index as a measure of quality of life in obesity. Obes Res. 2002;10:824–832. doi: 10.1038/oby.2002.111. [DOI] [PubMed] [Google Scholar]
- 16.Groessl EJ, Kaplan RM, Barrett-Connor E, et al. Body mass index and quality of well-being in a community of older adults. Am J Prev Med. 2004;26:126–129. doi: 10.1016/j.amepre.2003.10.007. [DOI] [PubMed] [Google Scholar]
- 17.Macran S. The relationship between body mass index and health-related quality of life. Centre for Health Economics, University of York; 2004. [Google Scholar]
- 18.Sach TH, Barton GR, Doherty M, et al. The relationship between body mass index and health-related quality of life: Comparing the EQ-5D, EuroQol VAS and SF-6D. Int J Obes (Lond) 2007;31:189–196. doi: 10.1038/sj.ijo.0803365. [DOI] [PubMed] [Google Scholar]
- 19.Brennan A, Ara R, Sterz R, et al. Assessment of clinical and economic benefits of weight management with sibutramine in general practice in Germany. Eur J Health Econ. 2006;7:276–284. doi: 10.1007/s10198-006-0374-x. [DOI] [PubMed] [Google Scholar]
- 20.Ara R, Brennan A. The cost-effectiveness of sibutramine in non-diabetic obese patients: Evidence from four Western countries. Obes Rev. 2007;8:363–371. doi: 10.1111/j.1467-789X.2007.00352.x. [DOI] [PubMed] [Google Scholar]
- 21.Kolotkin RL, Norquist JM, Crosby RD, et al. One-year health-related quality of life outcomes in weight loss trial participants: Comparison of three measures. Health Qual Life Outcomes. 2009 doi: 10.1186/1477-7525-7-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Janssen MF, Pickard AS, Golicki D, Gudex C, Niewada M, Scalone L, Swinburn P, Busschbach J. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Qual Lfe Res. 2012 doi: 10.1007/s11136-012-0322-4. [DOI] [PMC free article] [PubMed] [Google Scholar]