Abstract
Objective
Critical Time Intervention (CTI) is a time-limited care coordination intervention designed to reduce homelessness and other adverse outcomes for persons living with serious mental illness during the transition period between institutions and community living. This study assesses whether CTI improves the quality of family relationships between family members and individuals living with serious mental illness, and examines whether changes in quality of family relationship mediated the association between the intervention and psychiatric re-hospitalization outcomes.
Method
This study utilizes data from a randomized controlled trial that assessed the effect of CTI in preventing homelessness. Following discharge from inpatient psychiatric treatment in New York City, 150 previously homeless persons living with serious mental illness were randomly assigned to receive usual services only or nine months of CTI in addition to usual services.
Results
Findings from mixed-effects regression models indicated that those assigned to the CTI group reported greater frequency of family contact and greater improvement in satisfaction with family relations than the comparison group during the 18 month follow-up period. Mediation analysis revealed that greater improvement in satisfaction with family relations mediated the effect of CTI on psychiatric re-hospitalization outcome but only at a modest level.
Conclusion and Implications for Practice
These findings suggest that a relatively brief but targeted intervention delivered at the point of hospital discharge may contribute to strengthening family relations and that improvement in perceived family relationship quality can contribute to a reduction in psychiatric re-hospitalization.
Keywords: schizophrenia, homelessness, family, Critical Time Intervention
For persons living with serious mental illness and a history of homelessness, the period following hospital discharge is one of high risk for adverse outcomes, including recurrent homelessness and psychiatric re-hospitalization (Cuffel, Held, & Goldman, 2002; Herman, Susser, Jandorf, Lavelle, & Bromet, 1998; Ilgen, Hu, Moos, & McKellar, 2008; Olfson, Mechanic, Hansell, Boyer, & Walkup, 1999). A contributing factor is thought to be the difficulty associated with accessing needed support, exacerbated by the complex and fragmented system of mental health care in many U.S. communities (Smith & Sederer, 2009).
Family caregiver can play an important role in the lives of these individuals by providing emotional and financial support, and by noticing behavior, patterns or affect that might signify possible relapse. If family members alert both the individual and any key providers to observed changes, the prospect of prompt and successful intervention increases (Lincoln, Wilhelm, & Nestoriuc, 2007; Lucksted, McFarlane, Downing, & Dixon, 2012; Rummel-Kluge, Pitschel-Walz, & Kissling, 2007). Such attention and support contributes to stability and community tenure, and is particularly important during the fragile period following hospital discharge (Postrado & Lehman, 1995; Rummel-Kluge & Kissling, 2008).
Limited or unavailable family support is a signficant problem for many persons living with serious mental illness, and those with histories of homelessness are more likely to experience low levels of assistance from family members (Brent & Giuliano, 2007; Lehman, Kernan, DeForge, & Dixon, 1995; Wu & Serper, 1999). Several factors may interfere with families’ capacity to provide support post-hospitalization. These include the immediate and cumulative emotional and financial strain associated with the mental illness of a family member, simple lack of information or understanding regarding the most effective ways to support the person in managing the illness, and limited knowledge of or access to formal resources that might serve to support the individual, the family, or both (Lucksted et al., 2012).
Critical Time Intervention (CTI) is an empirically-supported model designed to enhance continuity of support among persons living with serious mental illness during periods of transition, especially from institutions to community living. The intervention emphasizes coordinated support among caretakers, including family members who can serve as a lifeline for the person and an indispensable source for the mental health services system (Shankar & Muthuswamy, 2007). Given its focus on building support among formal and informal sources, CTI is well-positioned to identify and build family strengths, bridge differences and develop sustainable connections by applying methods drawn from family psychoeducation and other evidence based practices (Dixon et al., 2010; Pickett-Schenk, Lippincott, Bennett, & Steigman, 2008).
While our prior work showed that CTI reduced rehospitalization following discharge, the mechanism through which it operates has not been carefully studied (Tomita & Herman, 2012). This study extends our prior research by examining the effect of CTI in improving the quality of family relationships between family members and individuals living with serious mental illness, and examines whether such changes mediated the risk of psychiatric re-hospitalization.
Methods
Data Source
We used data from a randomized controlled trial that assessed the efficacy of CTI in preventing homelessness after hospital discharge (Herman et al., 2011). Participants were recruited from transitional residences located on the grounds of two state-operated psychiatric hospitals in the New York City (NYC) area to which patients with housing difficulties were referred pending discharge to the community. The inclusion criteria were: 1) DSM-IV diagnosis of psychotic disorder, 2) history of homelessness, 3) living in a transitional residence at any stage between 2002 and 2006, and 4) planned residency in NYC following discharge from the transitional residence. Individuals were excluded who: 1) did not speak English, 2) did not stay in a transitional residence for more than three week nights and 3) were unable to provide informed consent. Written informed consent from eligible participants was obtained following an approved protocol by the Columbia University Institutional Review Board. Of the 150 participants, 73 (49%) were randomly assigned to receive usual services only (USO) while 77 (51%) were assigned to receive CTI in addition to usual services. Details regarding randomization and study attrition are described in a previous publication (Herman et al., 2011).
Intervention
All participants received psychiatric treatment and discharge planning services prior to leaving the transitional residences. The USO group subsequently received standard community-based services including case management and clinical treatment. The experimental group received these services plus nine months of CTI. A trained social service worker delivered CTI, beginning to establish a relationship with the participant prior to discharge from the transitional residence. CTI workers did not help participants identify their initial housing arrangement post-discharge. To compare outcomes, both the USO and CTI participants were followed for 18 months after discharge.
CTI was delivered in three phases over nine months, with each stage lasting approximately three months. The explicit aims were to strengthen the individual’s long-term ties with various caretakers and to provide direct emotional and practical support. During the first phase, the CTI worker provided extensive support for participants, targeting areas critical for successful community transition. The CTI worker aimed to engage the participant and identify, assess, and enhance both formal service providers (i.e. residential program, mental health and medical clinic), and informal networks of community support (i.e. family and friends), including those able to provide long-term and sustainable support beyond the period of the CTI itself. During the second phase, the CTI worker still provided direct assistance, but encouraged participants and their support networks to resolve issues on their own, providing back-up support where necessary. In the final phase, the CTI worker transferred care and responsibilities to both the individual and the formal and informal caregivers, aiming to reach consensus about a viable plan that ensured collective long-term support. Thus responsibility for providing support is gradually transitioned away from the worker, in a planned way, to enduring supports within the community (Herman & Mandiberg, 2010).
Throughout the intervention, the CTI worker provides individualized and detailed arrangements critical for long-term community survival, including mobilizing family support. While family work is not the only essential element, CTI workers often served as a vital source of support for those (1) facing strained relationships, (2) coping with the influence of illegal drug use by family members, (3) challenged by safety concerns or domestic violence and (4) coping with family finance issues. CTI staff actively encouraged participants to communicate with their family, and where this broke down, to attempt to resume contact and dialogue when agreed to by the participant. To respond to family challenges, CTI workers engaged in home visits, planning, educational and informational meetings in which they discussed individual challenges and strengths (with the permission of the participant), and suggested ways to mediate conflicts and build family cohesion.
Measurement
Data were collected in hospital before discharge (baseline) and at several points during the follow-up period. Quality of family relations was assessed three times; at baseline, nine and 18 months following discharge, using two family sub-scales from the Lehman Quality of Life Interview (LQoLI). This widely utilized instrument assesses different quality of life domains among persons living with serious mental illness, and is relevant for those who are also homeless (Cramer et al., 2000; Lehman, 1988; Lehman et al., 1995). The family sub-scales, which include measures of objective and subjective quality of relationships, have been previously utlilized to assess an aspect of the quality of life related to family relationships among adults living with severe mental illness (Aschbrenner, Mueser, Bartels, & Pratt, 2011; Macias, Gold, & Jones, 2012).
The objective measure of frequency of family contact consisted of the mean ratings on two items: 1) how often the participant spoke to a family member by telephone, and 2) how often the study participant met with a family member. Responses included “not at all”, “less than once a month”, “at least once a month”, “at least once a week” or “at least once a day,” scored 1 through 5 respectively. The subjective measure of satisfaction with family relationships was based on the mean score on four items including participants’ feelings about: 1) family overall, 2) frequency of contact with family, 3) how family members acted toward each other, and 4) general quality of the family relationships. Items were rated on a scale of 1 (terrible) to 7 (delighted). Cronbach’s α for the frequency of contact and satisfaction measures ranged from 0.72–0.78 and 0.81–0.86 respectively for baseline, 9-month and 18-month assessment.
Residential history of study participants, including number of nights spent in psychiatric hospital and domiciled, was assessed via participant self-report in follow-up interviews conducted every six weeks over the 18 months. We defined psychiatric re-hospitalization as an overnight stay in either a psychiatric emergency room, psychiatric unit in a general hospital, or psychiatric hospital, and domiciled housing to be nights residing in house, room, apartment or other private housing. Psychiatric re-hospitalization during the last three six-week follow-up intervals was used as the primary outcome, consistent with our previous report (Tomita & Herman, 2012).
Baseline demographic and clinical characteristics, including information about gender, race, age, education, number of children, lifetime psychiatric diagnoses, total homeless and psychiatric hospitalization nights during the 90 days before index admission and recent substance use were collected prior to discharge from the transitional residences. Diagnoses were assessed by trained and reliable interviewers using the Structured Clinical Interview for DSM-IV (First, Spitzer, Gibbon, & Williams, 2002).
Data Analysis
We conducted two separate analyses to assess the extent to which CTI improved the quality of family relationships, and whether changes in the quality of family relationship mediated the effect of the intervention on reducing risk of psychiatric re-hospitalization. We first conducted multilevel mixed-effects linear regression to test for the effect of CTI on perceived quality of family relations (objective and subjective) over the course of the 18-month follow-up. The interaction between time (9 month and 18 month) and group assignment (USO versus CTI) was used as a measure of intervention effect. All regression models were adjusted for baseline covariates including gender, race, age, education, number of children, family relationship score, total homeless and psychiatric hospitalization nights during the 90 days before the index hospital admission, as well as psychiatric diagnosis and substance use prior to hospital admission.
Based on an approach described by MacKinnon and colleagues (2007), we next conducted binary mediation analysis (with binary outcome and two mediator variables structure) to see whether changes in objective and subjective quality of family relationship mediated the association between assignment to the intervention and psychiatric re-hospitalization. This approach was selected over structural equation modeling due to our limited sample size and model complexity(MacCallum & Austin, 2000). First we assessed the total effect (c) of assignment to CTI on psychiatric re-hospitalization but without the mediating variables, using logistic regression. We then assessed the impact of assignment to CTI based on the changes in objective (a1) and subjective (a2) quality of family relationship using OLS regressions. To account for temporal factors, change in perceived quality of family relationship was based on the difference between baseline and 18 month scores. Lastly, we assessed the direct effect (c’) of the impact of assignment to CTI on psychiatric re-hospitalization between the two groups, controlling for mediating variables, including objective (b1) and subjective (b2) quality of family relationship, using logistic regression. If the association between CTI and psychiatric re-hospitalization were mediated by changes in the family relationship, we would expect to see a significant reduction in the effect of the intervention when the mediators were controlled for in the model (c’), compared to the total effect without mediators (c). In addition, we would also anticipate a significant association between objective (b1) and subjective (b2) quality of family relationship on psychiatric re-hospitalization outcome. The total indirect effect of CTI was computed as the difference between the total effect (c) and the direct effect (c’). All regression models were adjusted for baseline demographic and clinical covariates during the 90 days before the index hospital admission, as well as psychiatric diagnosis and substance use prior to hospital admission. We also controlled for housing stability in the second analysis (operationalized as the number of days out of the 24-week period between the end of the intervention and the beginning of the final three observation intervals that the participant was domiciled), because a past study showed that it (meaning housing stability) was associated with rehospitalization risk (Schmutte, Dunn, & Sledge, 2010). The statistical significance of the mediation effect between CTI and psychiatric re-hospitalization outcome in the second sub-analysis was also assessed using the Sobel test (1982). All analyses were performed in STATA version 12.
Results
Baseline characteristics of the sample are described in Table 1. Study participants were primarily male (n=107, 71%), and African-American (n=93, 62%). Schizophrenia was the lifetime diagnosis for 61% (n=92), and 35% (n=52) had a diagnosis of schizoaffective disorder. The mean age was 37.5 years. The mean score for frequency of family contact at baseline was 2.63 and for satisfaction with family relationships was 4.47. The CTI and USO groups did not differ significantly on any baseline characteristics.
Table 1.
Comparison of baseline characteristics by groups
| Category | Group | USO (n,%) | CTI (n,%) | Statistics, p |
|---|---|---|---|---|
| Gender: | α=1.11, p=0.29 | |||
| Female | 18,25% | 25,34% | ||
| Male | 55,75% | 52,66% | ||
| Race/Ethnicity: | α=0.50, p=0.91 | |||
| Latino | 12,16% | 11,14% | ||
| African-American | 45,62% | 48,62% | ||
| White | 11,15% | 14,18% | ||
| Other | 5, 7% | 4, 5% | ||
| Age: | α=0.92, p=0.82 | |||
| 18–29 | 14,19% | 19,25% | ||
| 30–39 | 26,36% | 25,32% | ||
| 40–45 | 17,23% | 19,25% | ||
| 46+ | 16,22% | 14,18% | ||
| Education: | α=0.39, p=0.82 | |||
| Did not complete high school | 31,43% | 29,38% | ||
| Completed high school | 30,41% | 35,46% | ||
| Beyond high school | 12,16% | 12,16% | ||
| Number of children: | α=0.17, p=0.68 | |||
| At least 1 child | 27,37% | 31,40% | ||
| Psychiatric diagnosis: | α=3.04, p=0.22 | |||
| Schizophrenia | 44,60% | 48,62% | ||
| Schizoaffective | 28,38% | 24,31% | ||
| Other | 1, 1% | 5, 7% | ||
| Recent substance use: | α=1.43, p=0.49 | |||
| No history | 7, 9% | 7, 9% | ||
| No use in past month | 56,77% | 64,83% | ||
| Use in past month | 10,14% | 6, 8% | ||
| Total psychiatric hospitalization nights during the 90 days before the index hospital admission: | ||||
| Mean±SD | 7.9±19.7 | 5.8±15.9 | t=0.70, p=0.48 | |
| Total homeless nights during the 90 days before the index hospital admission: | ||||
| Mean±SD | 48.1±40.7 | 47.0±38.1 | t =0.17, p=0.87 | |
| Objective family rating: | ||||
| Mean rating±SD | 2.6±1.2 | 2.7±1.1 | t=−0.33, p=0.75 | |
| Subjective family rating: | ||||
| Mean rating±SD | 4.5±1.4 | 4.4±1.5 | t=0.38, p=0.71 | |
Diagnosis category was collapse into three categories (schizophrenia, schizoaffective and others) in this table. “Other” psychiatric diagnosis category” includes bipolar, major depression with psychosis and psychosis not otherwise specified (NOS). The Fisher’s test as opposed to the use of chi-square did not alter the result.
Sixty-seven (87%) of participants assigned to the CTI group completed the nine month follow-up period, as did 66 participants (92%) assigned to the USO group. Fifty-eight (75%) of participants assigned to the CTI completed the 18-month follow-up period, as did fifty-nine participants (81%) assigned to the USO group. There were no differences in baseline characteristics between the CTI and USO groups with respect to those lost at either the 9-month or 18-month follow-up. However, those who remained in the study after the 9-month period reported lower family contact, regardless of treatment assignment.
The results of the mixed-effects models appear in Table 2. Assignment to CTI was associated with significantly improved family contact compared to the USO group at 18 months (β=0.47, p=0.02) but not at nine months (model 1). Female participants with a diagnosis of schizophrenia and drug use at baseline reported significantly higher frequency of family contact. Assignment to CTI, as indicated in model 2, was associated with significantly improved family relationship scores compared to the USO group at nine months (β=0.66, p=0.02) and at 18 months (β=0.61, p=0.04). Study participants with schizoaffective disorder at baseline had significantly lower family relationship scores.
Table 2.
Mixed-effects regression model for frequency of family contact and perceived quality of family relationship outcomes
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| Frequency of Family Contact | Perceived Quality of Family Relationship | |||||
| b | SE | p | b | SE | p | |
| Group [USO] | 0.05 | 0.13 | 0.72 | 0.03 | 0.19 | 0.89 |
| Time [Baseline] | ||||||
| 9 Months | −0.15 | 0.15 | 0.31 | −0.39 | 0.22 | 0.07 |
| 18 Months | −0.27 | 0.15 | 0.07 | −0.23 | 0.22 | 0.30 |
| Group by time interaction | ||||||
| Treatment at 9 Months | 0.08 | 0.20 | 0.67 | 0.66 | 0.29 | 0.02 |
| Treatment at 18 Months | 0.47 | 0.20 | 0.02 | 0.61 | 0.30 | 0.04 |
| Gender [Male] | 0.23 | 0.12 | 0.04 | 0.10 | 0.15 | 0.52 |
| Age category [19–29] | ||||||
| 30–39 | −0.10 | 0.13 | 0.47 | 0.20 | 0.18 | 0.26 |
| 40–45 | −0.20 | 0.15 | 0.18 | 0.13 | 0.19 | 0.50 |
| 46+ | −0.08 | 0.16 | 0.63 | 0.27 | 0.21 | 0.21 |
| Number of children | 0.02 | 0.03 | 0.42 | −0.03 | 0.04 | 0.43 |
| Race [Latin American] | ||||||
| African-American | −0.09 | 0.13 | 0.51 | 0.32 | 0.18 | 0.07 |
| White | 0.02 | 0.18 | 0.92 | −0.12 | 0.24 | 0.61 |
| Other/Mixed | −0.18 | 0.22 | 0.43 | 0.23 | 0.29 | 0.43 |
| School [Did not complete high school] Completed high school | 0.06 | 0.11 | 0.62 | 0.16 | 0.15 | 0.29 |
| Beyond high school | 0.17 | 0.15 | 0.27 | 0.26 | 0.21 | 0.21 |
| Psychiatric diagnosis [Other] | ||||||
| Schizophrenia | 0.23 | 0.11 | 0.03 | −0.02 | 0.14 | 0.87 |
| Schizoaffective | −0.47 | 0.24 | 0.05 | −1.06 | 0.31 | <0.01 |
| Drug use [no history] | ||||||
| No use in past month | 0.22 | 0.19 | 0.27 | 0.29 | 0.26 | 0.28 |
| Use in past month | 0.52 | 0.24 | 0.03 | −0.07 | 0.32 | 0.84 |
| # of psychiatric hospitalization nights during the 90 days before the index hospital admission | <0.01 | <0.01 | 0.20 | 0.01 | <0.01 | 0.05 |
| # of homeless nights during the 90 days before the index hospital admission | <0.01 | <0.01 | 0.40 | 0.01 | <0.01 | 0.38 |
Reference in bracket. The above model controls for baseline frequency of family contact (model 1) and baseline perceived quality of family relationship (model 2).
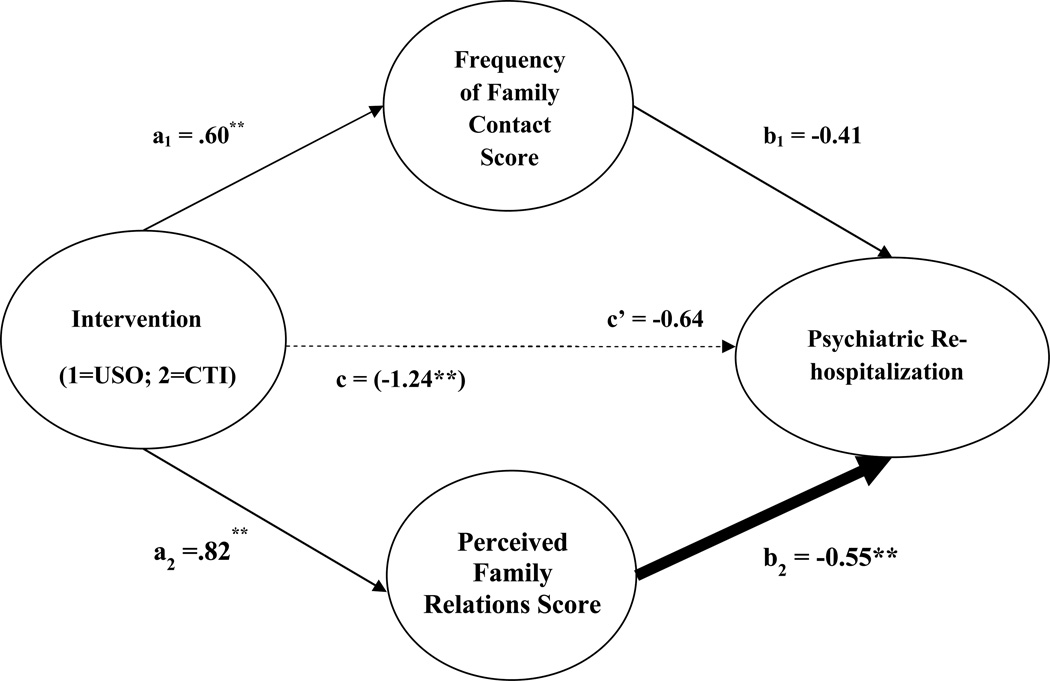
The results of the binary mediation analysis of the second sub-analysis using the two-mediator model with dichotomous outcome and continuous mediators appear in Figure 1. The total magnitude (total effect) of assignment to CTI on psychiatric re-hospitalization without the two mediating variables (c) was −1.24 (p=0.04), indicating a significant reduction in psychiatric re-hospitalization. Assignment to CTI was associated with increases in objective (β=0.60, p=0.01), and subjective (β=0.82, p=0.02) quality of family relations scores respectively (a1 and a2). The magnitude of assignment to CTI on psychiatric re-hospitalization (the direct effect), based on the full model including the two mediating variables, was −0.64 (c’) and was not significantly (p=0.32) related to outcome. The total indirect effect, which is the difference between the total effect (c) and the direct effect (c’), was −.60. The change in the subjective quality of family relationship (b2) was significantly related to the reduction in psychiatric rehospitalization (β=0.55, p = .03), but not with the objective quality of family relationship (b1). The mediation analysis showed that improvement in family relationships accounted for 52.0% of the total effect of CTI in reducing the psychiatric re-hospitalization outcome. While we found that improvement in the quality of family relationships mediated the relationship between CTI and psychiatric re-hospitalization based on the MacKinnon approach, the Sobel test indicates that the indirect effect was only modestly significant (p=0.10).
Figure 1.
Effects of CTI and Family Relationship on Psychiatric Re-Hospitalization, with Total Effects Shown in Parentheses
*p<.10; **p<.05; ***p<.01
Discussion
Our previous reports demonstrate that CTI is effective in reducing the risk of recurrent homelessness and psychiatric re-hospitalization among persons who are chronically homeless and living with serious mental illness (Susser et al., 1997; Herman et al., 2011; Tomita et al., 2012). Findings from this current study support the idea that CTI may modestly improve frequency of family contact and perceived quality of family relationship, and psychiatric re-hospitalization may be reduced through improved satisfaction with family relations. There is growing emphasis on the use of multidimensional rather than singular measures to assess outcomes among those with serious mental illness (Iyer, Rothmann, Vogler, & Spaulding, 2005). Our study contributes to these efforts by advancing knowledge about of the important function of family relations, and a possible mechanism through which CTI can help persons living with serious mental illness avoid unnecessary psychiatric re-hospitalization.
Family is an important and frequently overlooked source of potential support for people living with serious mental illness who are chronically homeless, underlined by our finding that fewer than 5% of study participants reported having no family contact during the 12 months before the index psychiatric hospitalization. However, the capacity of family members to provide ongoing support to participants following hospital discharge can be limited even when they desire to do so. Over time, cumulative stressors and limited resources can interfere with and weaken family relationships, lessening the viability of long-term family support (Brent & Giuliano, 2007). Furthermore, mental health treatment personnel often fail to engage family members in the treatment process (Mottaghipour & Bickerton, 2005). Therefore, finding new and effective ways to build partnerships between providers and family caregivers to support the person living with illness is a critical need (Leggatt, 2002).
Family-based psychosocial interventions lasting six to nine months that include psychoeducation, social support, communication and problem solving skills training are currently designated as among the core group of evidence-based practices for individuals with schizophrenia (Dixon et al., 2010; Lucksted et al., 2012). While a brief, relatively limited model such as CTI cannot substitute for intensive family intervention, our findings suggest that time-limited support from CTI workers can modestly improve the way that persons living with serious mental illness rate their level of satisfaction with family relationships and contact following hospital discharge, and reduce adverse outcome, such as psychiatric re-hospitalization. Future efforts to expand and more carefully document family interventions within the CTI model could enhance its impact, particularly regarding quality of family and other interpersonal relationships, the role of family in sustained community tenure and symptom management, self-esteem, and overall quality of life. Training and supervision of CTI workers could be expanded to include psychoeducation, stress management, crisis and meditational techniques that attend to the needs and strengths of both the individual and family.
The study has several limitations. First, we acknowledge that psychiatric re-hospitalization is merely one indicator of outcome and must be understood within the broader context of other measures of community functioning and quality of life. In this trial, the goals of CTI were rather limited—the primary one being to reduce recurrent homelessness and, to a lesser extent, re-hospitalization, during the period immediately following hospital discharge among persons seen to be at extremely high risk of adverse outcomes. Second, although mobilizing family support is an explicit element in the CTI model, we have no systematic measure of the extent to which workers intervened directly with families or the precise activities they carried out. A review of case notes revealed that CTI workers addressed family-related issues at some point during the intervention for 25 of the 66 participants. However, we had no way of knowing what, if any assistance participants assigned to the USO group received regarding family-related issues. Third, reverse causation is possible; reduced psychiatric hospitalization may be contributed to improved quality of family relationships. Finally, only the family domain from the Lehman Quality of Life Interview was available for complete longitudinal assessment, limiting our ability to examine other quality of life factors and sources of support that might help to explain the mechanisms through which CTI operates. In addition to including the full range of quality of life domains, future CTI studies should collect satisfaction data from family members and caregivers to document their perspective.
Conclusion
Our results suggest that family support provided by CTI, a relatively brief but targeted low-intensity care coordination model delivered during the period following hospital discharge, can modestly improve self-ratings of family relations and frequency of contact between individuals living with serious mental illness and their family members. The findings support the idea that CTI may be instrumental in strengthening the individual’s ties to family resources and reduce adverse outcomes, such as psychiatric re-hospitalization. As we continue to refine the model and strengthen its evidence base, we hope to further develop the guidelines for training and supervising CTI workers in family work. Part of this effort will be to identify the components of psychoeducation and other evidence-based practices that can be readily implemented within the CTI framework. This would set the stage for much needed research to systematically document and assess aspects of family intervention engaged in by CTI workers, and evaluate its immediate and long-term impact on the breadth of outcomes that reflect functioning and quality of life among persons living with serious mental illness.
Acknowledgments
This work was supported by grants F31MH082621 (PI: Tomita) and R01MH59716 (PI: Herman) from the National Institute of Mental Health.
Footnotes
All authors declare no conflict of interest.
Contributor Information
Andrew Tomita, Mailman School of Public Health, Columbia University
Ellen P. Lukens, School of Social Work, Columbia University
Daniel B. Herman, Silberman School of Social Work, Hunter College
References
- Aschbrenner KA, Mueser KT, Bartels SJ, Pratt SI. Family contact and health status among older adults with serious mental illnesses. Psychiatric Rehabilitation Journal. 2011;34(4):295–303. doi: 10.2975/34.4.2011.295.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent BK, Giuliano AJ. Psychotic-spectrum illness and family-based treatments: A case-based illustration of the underuse of family interventions. Harvard Review of Psychiatry. 2007;15(4):161–168. doi: 10.1080/10673220701532540. [DOI] [PubMed] [Google Scholar]
- Cramer JA, Rosenheck R, Xu W, Thomas J, Henderson W, Dennis S Charney for the Department of Veterans Affairs Cooperative Study Group on Clozapine in Refractory Schizophrenia. Quality of life in schizophrenia: A comparison of instruments. Schizophrenia Bulletin. 2000;26(3):659–666. doi: 10.1093/oxfordjournals.schbul.a033484. [DOI] [PubMed] [Google Scholar]
- Cuffel BJ, Held M, Goldman W. Predictive models and the effectiveness of strategies for improving outpatient follow-up under managed care. Psychiatric Services. 2002;53(11):1438–1443. doi: 10.1176/appi.ps.53.11.1438. [DOI] [PubMed] [Google Scholar]
- Dixon LB, Dickerson F, Bellack AS, Bennett M, Dickinson D, Goldberg RW, Kreyenbuhl J. The 2009 schizophrenia PORT psychosocial treatment recommendations and summary statements. Schizophrenia Bulletin. 2010;36(1):48–70. doi: 10.1093/schbul/sbp115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Herman DB, Conover S, Gorroochurn P, Hinterland K, Hoepner L, Susser ES. Randomized trial of critical time intervention to prevent homelessness after hospital discharge. Psychiatric Services. 2011;62(7):713–719. doi: 10.1176/appi.ps.62.7.713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman DB, Mandiberg J. Critical time intervention: Model description and implications for the significance of timing in social work interventions. Research on Social Work Practice. 2010;20(5):502–508. [Google Scholar]
- Herman DB, Susser ES, Jandorf L, Lavelle J, Bromet EJ. Homelessness among individuals with psychotic disorders hospitalized for the first time: findings from the Suffolk County Mental Health Project. American Journal of Psychiatry. 1998;155(1):109–113. doi: 10.1176/ajp.155.1.109. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Hu KU, Moos RH, McKellar J. Continuing care after inpatient psychiatric treatment for patients with psychiatric and substance use disorders. Psychiatric Services. 2008;59(9):982–988. doi: 10.1176/ps.2008.59.9.982. [DOI] [PubMed] [Google Scholar]
- Iyer SN, Rothmann TL, Vogler JE, Spaulding WD. Evaluating outcomes of rehabilitation for severe mental illness. Rehabilitation Psychology. 2005;50(1):43. [Google Scholar]
- Leggatt M. Families and mental health workers: the need for partnership. World Psychiatry. 2002;1(1):52–54. [PMC free article] [PubMed] [Google Scholar]
- Lehman AF. A quality of life interview for the chronically mentally ill. Evaluation and Program Planning. 1988;11(1):51–62. [Google Scholar]
- Lehman A, Kernan E, DeForge B, Dixon L. Effects of homelessness on the quality of life of persons with severe mental illness. Psychiatric Services. 1995;46(9):922–926. doi: 10.1176/ps.46.9.922. [DOI] [PubMed] [Google Scholar]
- Lincoln TM, Wilhelm K, Nestoriuc Y. Effectiveness of psychoeducation for relapse, symptoms, knowledge, adherence and functioning in psychotic disorders: A meta-analysis. Schizophrenia Research. 2007;96(1):232–245. doi: 10.1016/j.schres.2007.07.022. [DOI] [PubMed] [Google Scholar]
- Lucksted A, McFarlane W, Downing D, Dixon L. Recent developments in family psychoeducation as an evidence-based practice. Journal of Marital and Family Therapy. 2012;38(1):101–121. doi: 10.1111/j.1752-0606.2011.00256.x. [DOI] [PubMed] [Google Scholar]
- Macias RL, Gold PB, Jones DR. Age and physical health as predictors of family contact among adults with severe psychiatric illness. Psychiatric Quarterly. 2012 doi: 10.1007/s11126-012-9238-y. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58(1):593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCallum RC, Austin JT. Applications of structural equation modeling in psychological research. Annual Review of Psychology. 2000;51(1):201–226. doi: 10.1146/annurev.psych.51.1.201. [DOI] [PubMed] [Google Scholar]
- Mottaghipour Y, Bickerton A. The pyramid of family care: A framework for family involvement with adult mental health services. Advances in Mental Health. 2005;4(3):210–217. [Google Scholar]
- Olfson M, Mechanic D, Hansell S, Boyer CA, Walkup J. Prediction of homelessness within three months of discharge among inpatients with schizophrenia. Psychiatric Services. 1999;50(5):667–673. doi: 10.1176/ps.50.5.667. [DOI] [PubMed] [Google Scholar]
- Pickett-Schenk SA, Lippincott RC, Bennett C, Steigman PJ. Improving knowledge about mental illness through family-led education: the journey of hope. Psychiatric Services. 2008;59(1):49–56. doi: 10.1176/ps.2008.59.1.49. [DOI] [PubMed] [Google Scholar]
- Postrado L, Lehman A. Quality of life and clinical predictors of rehospitalization of persons with severe mental illness. Psychiatric Services. 1995;46(11):1161–1165. doi: 10.1176/ps.46.11.1161. [DOI] [PubMed] [Google Scholar]
- Rummel-Kluge C, Kissling W. Psychoeducation in schizophrenia: new developments and approaches in the field. Current Opinion in Psychiatry. 2008;21(2):168–172. doi: 10.1097/YCO.0b013e3282f4e574. [DOI] [PubMed] [Google Scholar]
- Rummel-Kluge C, Pitschel-Walz G, Kissling W. A fast, implementable psychoeducation program for schizophrenia. Psychiatric Services. 2007;58(9):1226. doi: 10.1176/ps.2007.58.9.1226. [DOI] [PubMed] [Google Scholar]
- Schmutte T, Dunn CL, Sledge WH. Predicting time to readmission in patients with recent histories of recurrent psychiatric hospitalization: A matched-control survival analysis. Journal of Nervous & Mental Disease. 2010;198(12):860–863. doi: 10.1097/NMD.0b013e3181fe726b. [DOI] [PubMed] [Google Scholar]
- Shankar J, Muthuswamy SS. Support needs of family caregivers of people who experience mental illness and the role of mental health services. Families in Society. 2007;88(2):302. [Google Scholar]
- Smith TE, Sederer LI. A new kind of homelessness for individuals with serious mental illness? The need for a "mental health home". Psychiatric Services. 2009;60(4):528–533. doi: 10.1176/ps.2009.60.4.528. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociological Methodology. 1982;13:290–312. [Google Scholar]
- Susser E, Valencia E, Conover S, Felix A, Tsai W-Y, Wyatt RJ. Preventing recurrent homelessness among mentally ill men: a "critical time" intervention after discharge from a shelter. American Journal of Public Health. 1997;87(2):256–262. doi: 10.2105/ajph.87.2.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomita A, Herman DB. The impact of critical time intervention in reducing psychiatric rehospitalization after hospital discharge. Psychiatric Services. 2012;63(9):935–937. doi: 10.1176/appi.ps.201100468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu T, Serper MR. Social support and psychopathology in homeless patients presenting for emergency psychiatric treatment. Journal of Clinical Psychology. 1999;55(9):1127–1133. doi: 10.1002/(sici)1097-4679(199909)55:9<1127::aid-jclp9>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]