Abstract
Background
Declining cognition is a risk factor for falls among older adults. The extent to which impaired judgment in performance of daily activities increases fall risk is unclear.
Objective
The aim of this study was to determine whether engagement in mobility activities in a risky manner explains the association between declining cognition and rate of falls.
Design
This study was a secondary analysis of baseline and prospective data from older adults enrolled in the intervention arm of a randomized clinical trial.
Methods
Two hundred forty-five community-dwelling older adults (79% female; mean age=79 years, SD=8.0) who were at risk for falls received physical, cognitive, and functional evaluations. Cognition was assessed with the Short Portable Mental Status Questionnaire (SPMSQ). Using interview and in-home assessment data, physical therapists determined whether participants were at risk for falls when performing mobility-related activities of daily living (ADL) and instrumental ADL (IADL). Falls were measured prospectively for 1 year using monthly falls diaries.
Results
Declining cognition was associated with increased number of mobility activities designated as risky (1.5% of mobility activities performed in a risky manner per SPMSQ point) and with increased rate of falls (rate ratio=1.16 for each unit change in SPMSQ score). Risky performance of mobility activities mediated the relationship between cognition and rate of falls.
Limitations
Risk assessment was based on the clinical judgment of experienced physical therapists. Cognition was measured with a relatively insensitive instrument, and only selected mobility activities were evaluated.
Conclusions
Engagement in mobility ADL and IADL tasks in a risky manner emerged as a link between declining cognition and increased number of falls, suggesting a mechanism through which the rate of falls may increase. Specifically, declining cognition is associated with performance of mobility activities in an unsafe manner, thereby increasing the risk for falls.
Declining cognition is known to be a risk factor for falls in older adults.1–8 Increased fall risk has been associated with a wide array of cognitive disorders found in geriatric populations, including stroke,9 Parkinson disease,10 and dementia.11 Even those with relatively mild levels of cognitive impairment exhibit increased risk for falls.6–8,12
Although the relationship between declining cognition and falls has been reliably demonstrated, the mechanisms through which declining cognition increases the rate of falls have only recently been investigated. Research has focused on executive functions, or the abilities that allow individuals to successfully perform independent, purposeful behaviors. They include planning, executing, and monitoring activities, as well as initiation, motivation, and judgment.13 Executive dysfunction has repeatedly been linked to gait variability and falls.7,8,14–16 Subtle executive dysfunction could impair the ability to plan and organize the steps of a mobility task,13 attend to competing environmental demands and key contextual cues17 (eg, ice, clutter), assess level of risk, and take appropriate precautions.18,19 For example, in a recent study, both older adults who were healthy and older adults who were at high risk for falls demonstrated difficulties with the multiple demands required by complex walking tasks, exhibiting poorer ability to flexibly allocate attention and utilize problem-solving strategies compared with younger adults17 or older adults at low fall risk.18 In addition, older adults substantially overestimated their postural capabilities and committed to performing risky mobility behaviors, suggesting that inaccurate awareness of diminished physical skills led to poor judgment.19 Judgment, or the decision-making involved in the performance of mobility activities, has received limited attention to date.
A risky mobility activity, for our purposes, was defined as an activity in which an individual engages that could lead to a potential fall based on his or her environment, physical, cognitive, or visual capabilities; need for assistive devices; and usual strategy or method of performance. Risky performance of activities is associated with higher rates of injury in younger populations with attention difficulties.20 A pattern of engagement in risky mobility activities may predispose older adults to greater numbers of falls.21 It is unknown whether risky performance of mobility activities is associated with declining cognition or mediates the association between cognitive decline and falls. We hypothesized that older adults who fall and who exhibit declining cognition may be at higher risk for falls, in part because they engage in everyday mobility activities in a hazardous way. The present study sought to examine the relationship among declining cognition, engagement in risky mobility activities, and falls.
Method
The Dane County Safety Assessment for Elders (SAFE) research study was a randomized controlled trial assessing the impact of a multifactorial falls intervention on future falls.22 Briefly, community-dwelling individuals were recruited from multiple sources, including caseworkers from the Dane County Area Agency on Aging, hospital discharge planners, home nursing agencies, senior centers, meal sites, health fairs, flu clinics, retirement facilities, meals-on-wheels organizations, and parish nurses. Inclusion criteria were: (1) residence in Dane County or surrounding counties, (2) age 65 years or older, and (3) a history of at least 2 falls in the previous year or 1 fall with self-reported injury or gait and balance problems. Older adults were excluded if they were terminally ill, resided in a nursing home or congregate living facility, or were unable to give informed consent and had no related in-home caregiver.
Initial Assessment
A registered nurse collected baseline data from the 500 individuals enrolled in the study using a structured interview, questionnaires, and physical performance measures. Interview questions assessed health status, health behaviors, mood,23 activity participation, use of mobility devices, use of eyeglasses while walking, use of psychotropic medications,24 presence of someone to provide assistance in the home, demographics (eg, age, education), and number of falls in the previous year. Physical performance measures included: the Short Physical Performance Battery (SPPB)25; the Four-Meter Walk–gait speed26; the Four-Test Balance Scale27; the Five Times Sit-to-Stand Test25; and visual acuity of the left eye, right eye, and both eyes tested at 4 m, with glasses usually worn while walking. Data also were collected for: the Activities-specific Balance Confidence (ABC) Scale28; the 12-item Short-Form Health Survey29 (SF-12); and the Short Portable Mental Screening Questionnaire (SPMSQ), a 15-item questionnaire comprising questions regarding orientation and working memory (serial sevens), on which a score of 0 indicates no error.30
Comprehensive Multifactorial Falls Assessment
Individuals were randomly assigned to either an intervention group (n=251) or a control group (n=249). In the intervention arm, a therapist visited the older adult and assessed risk with performing daily activities as part of the intervention. The control group did not have this assessment. Therefore, only participants in the intervention arm were included in these analyses. For participants in the intervention group, 1 of 3 physical therapists performed an in-home, comprehensive multifactorial falls evaluation determining individual risk factors for falls and assessing the interaction of the person and his or her environment. The goal of the evaluation was to provide participants with specific and tailored interventions and recommendations to reduce fall risk. Each physical therapist completed a 2-day training session led by the principal investigator (J.E.M.) and the co-principal investigator (T.S.). The training included use of an algorithm that contains a section on risky performance with mobility activities.31,32 The 3 therapists all evaluated the same 3 (beta) patients; then assessments and recommendations were compared for reliability. The principal investigator and co-principal investigator monitored the trained physical therapists closely in the beginning of the study and then periodically to ensure consistency in assessment and delivery of interventions.
The multifactorial assessment integrated the baseline information with additional examination, questionnaire, and interview data obtained by the physical therapist in an in-home visit. Physical examination included inspection of the participant's feet and footwear, testing for orthostatic hypotension, and testing lower extremity sensation. A comprehensive home safety assessment was performed, and participants completed the short form of the Geriatric Depression Scale.33 The physical performance assessments were: the Romberg test34; reactive balance35,36; the Modified Clinical Test of Sensory Interaction and Balance (mCTSIB)36,37; portions of the Berg Balance Scale38; the Tinetti Performance-Oriented Mobility Assessment–gait tests36; walking with horizontal head turns from the Dynamic Gait Index39; and the Timed “Up & Go” Test (TUG), with and without a cognitive task.40
The therapist obtained a detailed fall history, including the circumstances and events surrounding the participants' falls in the previous year. Participants were asked whether they performed 12 mobility-related basic activities of daily living (ADL) and instrumental ADL (IADL): stair climbing, laundry, bathing, housekeeping, shopping, toileting, car transfer, mail, yard work, answering phone/door, dressing, and meal preparation. If they did not perform the activity, the therapist recorded “not doing” and did not rate risk. If participants were performing the activity, a dichotomous score (ie, yes or no) denoting risk was recorded.
To determine the risk score, the therapist asked the participant to describe how he or she performed each activity. If a caregiver was present, his or her comments on tasks performed, method of performance, and help required were taken into account. Emphasizing the interaction of person-specific characteristics and person-specific environmental factors, the therapist rated performance of the activity as either risky or not risky. Individuals did not need to have a history of falling while performing a mobility activity to have their performance of that activity designated as risky. Risky performance of mobility activities was determined by the participant's self-report of his or her usual strategy for performing the activity, assessment of the environment in which it was performed, the availability and use of help, and evaluation of their vision, cognition, balance and mobility skills. For example, performance of bathing would be designated as risky if the person performed the activity and needed to step over the edge of a bathtub to shower but had no grab bar present, did not hold on to any other support while stepping, and had poor balance while standing on one foot. The physical therapist would recognize this combination of variables as a potential fall risk and would recommend modification of the activity to improve safety such as installing a grab bar and use of the grab bar during this task.
Follow-up Procedures
Using an algorithm developed by the principal investigator and co-principal investigator, participants were given individualized and specific recommendations to reduce fall risk based on their identified risk factors. The therapist gave recommendations to the participant's primary physician and provided referrals for additional medical or community-based interventions as indicated. The participants received a monthly phone follow-up from the physical therapist to encourage adherence to the recommendations.
Falls were assessed prospectively for 1 year using monthly falls diaries and calendars. An accidental fall was defined as “an event which results in a person coming to rest inadvertently on the ground or other lower level, and other than as a consequence of the following: sustaining a violent blow; loss of consciousness; sudden onset of paralysis, as in stroke; an epileptic seizure.”41(p5) Caregivers were asked to assist with recording of falls. Any participant who did not return a falls calendar or who reported a fall received a phone call from study personnel to confirm falls and ascertain circumstances and consequences.
Statistical Analyses
Multivariate analyses were conducted to investigate the relationships between cognition, as measured by the SPMSQ score, and falls and between cognition and risky performance of mobility behaviors. Number of falls was modeled utilizing a negative binomial (overdispersed Poisson) log-linear regression model with (log) number of days in the community as an offset term. Days and falls that transpired in a setting other than community living (ie, nursing home, hospital, or community-based residential facility) were excluded from the denominator and numerator, respectively. The SPMSQ score and proportion of behavior were the primary predictors of interest. Age, sex, psychotropic medication use, alcohol use (≥3 times per week), and mood were considered to be potentially confounding variables. Psychotropic medications included total number of scheduled and as-needed prescription antidepressants, benzodiazepines, antipsychotics, sedatives or hypnotics, and antihistamines. As-needed medications were included only if a participant took them at least once, on average, in a 2-week period. Sex, alcohol use, and mood were entered in the model as dichotomous variables, and age and number of psychotropic medications were entered as continuous variables. Proportion of mobility activities performed in a risky manner was a potential mediating variable.
To explore mediation, we fit a linear regression model for proportion of mobility activities performed in a risky manner as a function of SPMSQ score and a negative binomial model for number of falls as a function of SPMSQ score and proportion of mobility activities performed in a risky manner. Associations between (1) proportion of mobility activities performed in a risky manner and SPMSQ score and (2) numbers of falls and proportion of activities performed in a risky manner adjusting for SPMSQ score are the prerequisites for mediation.
Bivariate associations were examined between total ABC Scale score and total number of risky activities and between patients' self-reported level of confidence for specific mobility activities (car transfers and ascending/descending stairs), as assessed with the ABC Scale, and participation in these activities in a risky manner. In addition, associations were investigated between living with a supportive adult in the home and total number of risky mobility activities. All analyses were performed using SAS version 9.1 (SAS Institute Inc, Cary, North Carolina).
Results
Of 251 initial participants in the intervention arm, 6 withdrew before receiving the multifactorial falls assessment, leaving a final study population of 245 participants (193 women, 52 men). The flow diagram for the study is shown in the Figure. Baseline characteristics of the sample are presented in Table 1. Participants were elderly (mean age=79 years, SD=8), well educated (mean years of education=14.4, SD=3.9), and displayed relatively intact cognition (mean SPMSQ Scale score=0.7, SD=1.6). Sixty-two percent had fallen 2 or more times in the previous year.
Figure.
Flow diagram for the study.
Table 1.
Participant Baseline Characteristics
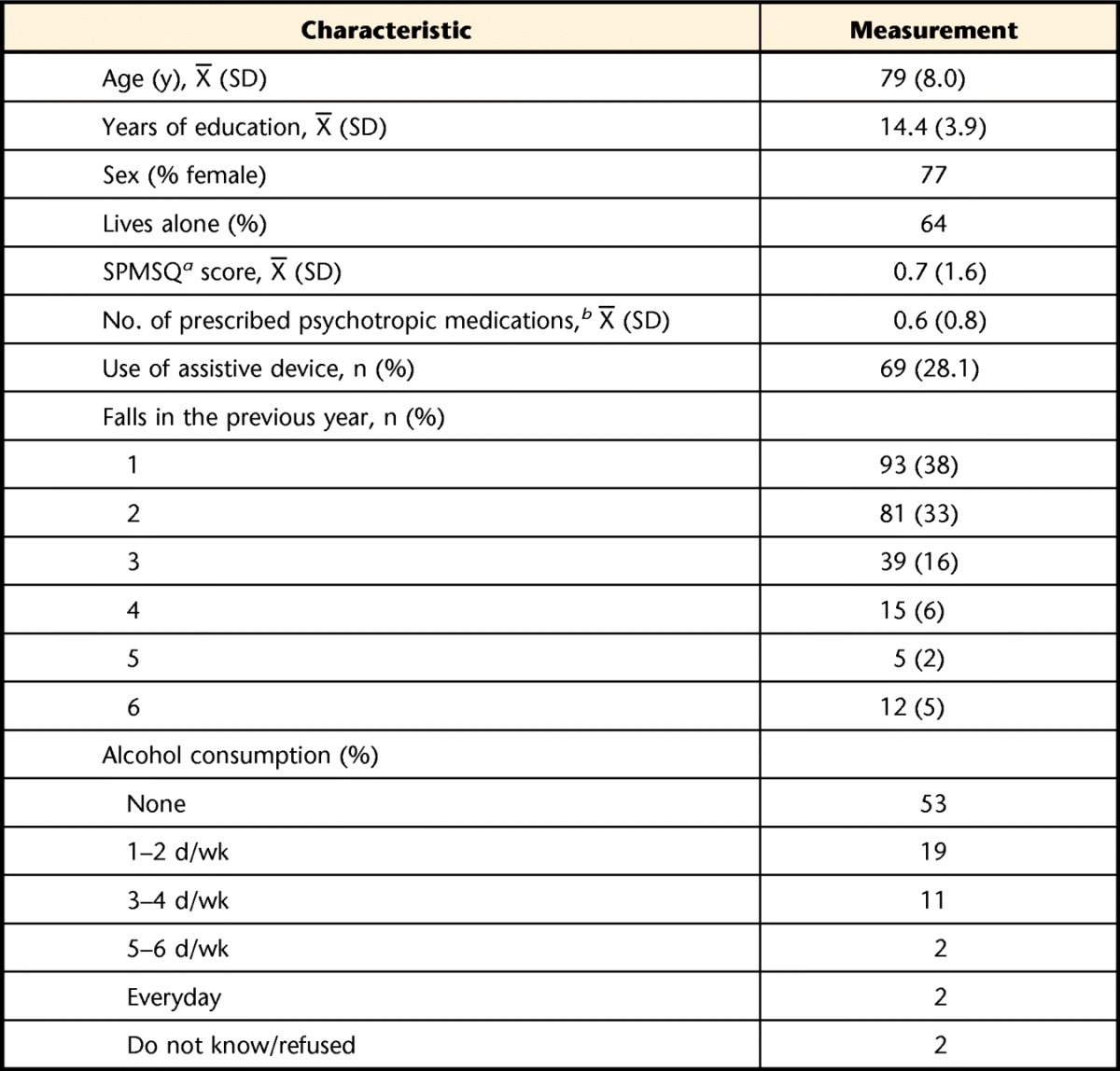
a SPMSQ=Short Portable Mental Status Questionnaire score of 0 to 2 denotes normal mental functioning. One less error is allowed if the patient has had education beyond the high school level.30
b Psychotropic medications are medications used to treat psychiatric conditions.
Table 2 presents the 12 mobility activities for which participants were rated and the percentage of respondents engaging in these activities in a manner deemed risky. The sample, as a whole, engaged in a mean of 9.43 (SD=2.51) of the 12 activities, with a mean of 0.51 (SD=0.86) of these being risky.
Table 2.
Mobility-Related Activities Performed by Older Adults at High Risk for Falls
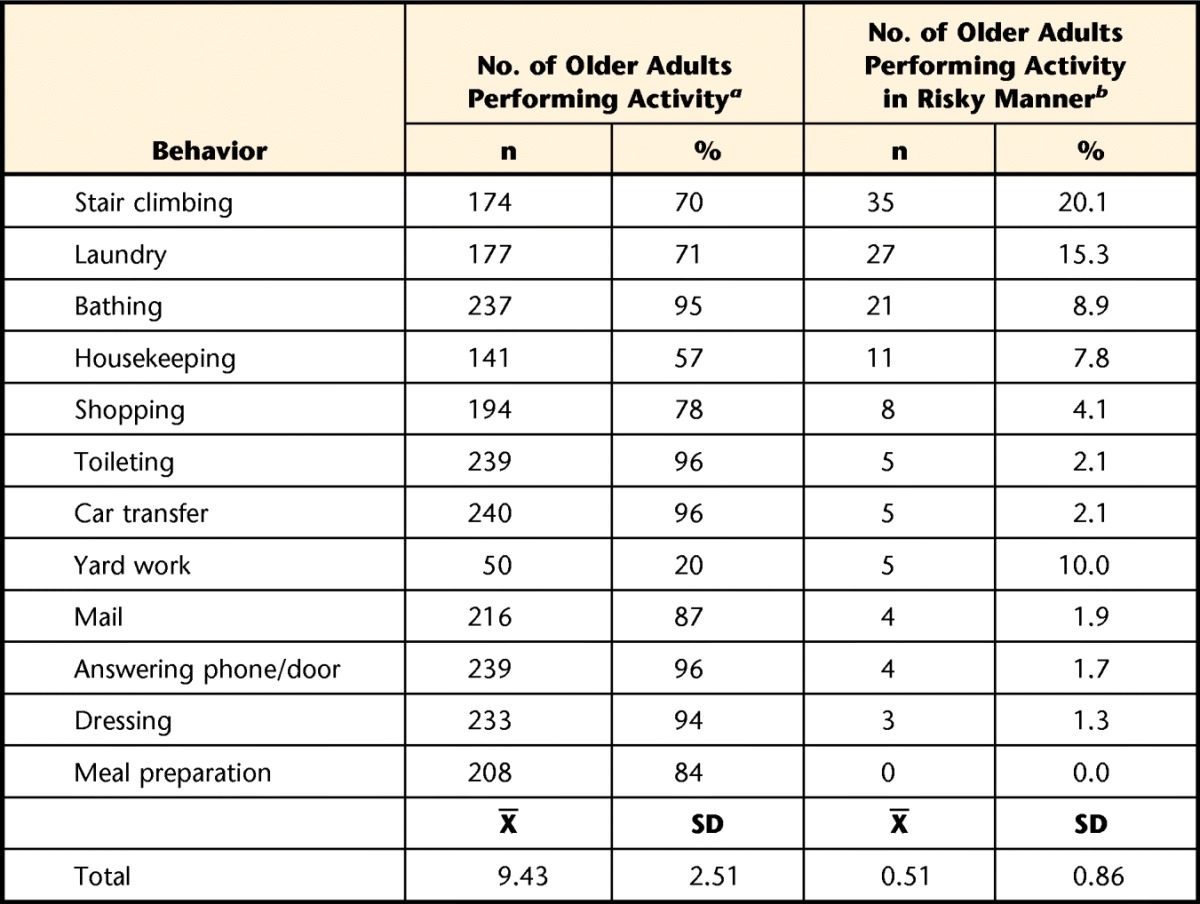
a Number of participants performing per self-report and caregiver report, if available.
b Number of participants performing in a risky manner based on physical therapist's assessment of home environment, physical and cognitive performance, and self-reported mobility behavior.
In multivariate analysis controlling for age, sex, number of psychotropic medications, alcohol use, and mood, a higher SPMSQ score (ie, declining cognition) was associated with an increased rate of falls (rate ratio=1.16 for each unit change in SPMSQ score, 95% confidence interval [95% CI]=1.03–1.32, P=.02). Higher SPMSQ scores also were associated with an increased number of mobility activities performed in a risky manner. There was an additional 1.5% of mobility activities performed in a risky manner per SPMSQ point (95% CI=0.8%–2.2%, P<.001). Because the sample, as a whole, performed 5.4% of mobility activities in a risky manner, an absolute increase of 1.5% per SPMSQ point corresponded to a relative increase of 30% per point, representing a substantial change in number of risky mobility activities (ie, 5.4% for SPMSQ score of 0, 6.9% for SPMSQ score of 1, 8.4% for SPMSQ score of 2, and so on).
Risky mobility activities mediated the relationship between SPMSQ score and fall risk. In multivariate models including both risky mobility activities and SPMSQ score, higher numbers of risky mobility activities were significantly associated with an increased rate of falls (rate ratio=1.29 for an additional 10% of mobility activities performed in a risky manner, 95% CI=1.08–1.54, P=.005), and the association between SPMSQ score and falls was attenuated (rate ratio=1.11, 95% CI=0.97–1.25, P=.15). Additional adjustment for ABC Scale score attenuated, but did not completely explain, the relationship between numbers of risky mobility behaviors and falls (rate ratio=1.20, 95% CI=1.00–1.43, P=.049).
In bivariate models examining risk with performance of specific mobility activities and self-confidence in performing those activities, low self-confidence was associated with risky performance. Poor self-confidence for car transfers was associated with risky car transfers (odds ratio [OR]=0.65, P=.002), and poor self-confidence for stairs was associated with ascending and descending stairs in a risky manner (OR=0.79, P<.001). Overall, a higher ABC Scale score (higher self-confidence) was associated with fewer risky behaviors (additional 0.9% of mobility activities performed in a risky manner per ABC Scale score point lost, P<.001). There was a significant association between living with another adult and the total number of risky behaviors performed (additional 3.2% of mobility activities performed in a risky manner with another adult in the home, P=.04). That is, individuals who lived with another adult in the home engaged in more risky behaviors compared with those who lived alone.
Discussion
In this sample of older adults at high risk for falls enrolled in the intervention arm of a multifactorial falls intervention study, mild declines in cognition were associated with an increased number of mobility activities deemed risky and a higher rate of falls. Engagement in risky mobility activities mediated the relationship between cognitive decline and falls. Altogether, these data provide support for the notion that the increased risk for falls associated with mildly declining cognition may result, in part, from judgment errors, causing the older adult to take risks when performing a mobility activity. To our knowledge, this is the first study demonstrating this relationship among declining cognition, engagement in risky mobility activities, and falls.
To understand why individuals engaged in risky mobility behaviors, we examined the contributions of confidence and living situation. We found that individuals engaging in risky mobility activities lacked confidence in their ability to perform the activity safely, implying that the decision to perform an activity in a risky way was not from overconfidence. Rather, they performed activities despite deeming them unsafe. We also examined whether having another person to provide assistance in the home influenced the likelihood that individuals would engage in risky mobility behaviors. Unexpectedly, older adults who lived with another person were more likely to perform mobility activities in a risky manner than were those who lived alone.
For physical therapists assessing fall risk and advising older adults on strategies to reduce falls, these data have several implications. First, modifying risk for falls for older adults who are cognitively compromised may require different approaches from those used with older adults who are cognitively healthy. Second, it may be important to assess risk for falls with specific activities, collating data from home evaluation, cognition, and physical examination findings. Third, older adults who lack confidence may still engage in a mobility activity in a risky manner. Thus, therapists should evaluate performance for activities where patients lack confidence, particularly for patients with declining cognition, even though declines may be mild. Fourth, therapists cannot assume that older adults living with another supportive adult are at reduced risk for falls by virtue of having someone to assist them.
Helping older adults to remain active is critical not only for physical mobility but also for quality of life.42,43 Therefore, rather than suggesting that patients limit their mobility, it may be important to suggest modifications to valued activities so that individuals may continue to function as independently as possible.44 Additionally, it may be helpful to tailor interventions specifically to a person's ability to perform mobility activities, particularly for those with declining cognition.45 Home safety modifications may reduce the risk for falls with performance of mobility ADL and IADL tasks.46 Therapists also may recommend task modifications to change a person's strategy from risky to safe.47 Moreover, it may be necessary for caregivers to take appropriate action themselves rather than simply discussing possible changes with patients.46 For example, if ascending and descending stairs is risky because clutter prevents patients from grasping handrails, caregivers may need to remove clutter themselves rather than directing patients to do so.
Preliminary evidence supports the use of individualized, multifaceted, compensatory strategies. A randomized trial of a multifactorial falls intervention that included live-in caregivers showed a significantly lower rate of falls in a subgroup of patients with cognitive impairment who lived with a caregiver compared with those who lived alone.31 Caregivers cued patients about performing mobility activities safely or themselves took over activities that the older adult could no longer perform safely.31
Our findings are consistent with the growing body of literature demonstrating the relationship among executive functioning, gait, and falls.7,8,14–16 However, to our knowledge, only one other study has specifically examined the role of judgment in performing risky mobility behaviors.19 Those findings revealed that elderly people who were healthy, but not young individuals, consistently overestimated their abilities when asked to perform potentially hazardous physical tasks. The current results provide evidence of similar judgment errors within the relevant context of individuals' home environments and demonstrate an association with declining cognition. Relative to the study by Lafargue et al,19 we utilized a larger sample (251 versus 40 participants) and observed patients performing physical, gait, and mobility tasks. A strength of Lafargue and colleagues' study was the in vivo demonstration of participants' intention to perform risky mobility behaviors.
Recent studies suggest that cognitive enhancement techniques can improve gait stability.8,48–51 However, it is not known whether these approaches will improve performance safety for everyday activities or decrease falls. Future research should establish guidelines for standardized measures of risky mobility behaviors and investigate the types of mobility activities most often associated with falls. In addition, future research should examine the specific roles of executive function and judgment in relation to performance of mobility activities. Finally, it will be important to address whether intervention studies targeting risk reduction of mobility activities due to declining cognition actually results in fewer risky mobility activities and falls.
This study had limitations. First, older adults were not observed actually performing the mobility activities on which they were rated, and it is possible that they participated in activities differently than they described. Because risk occurs within a dynamic context of individual skill, environmental demands, and approach to task, individual performance of mobility activities may range from safe to hazardous or may be inconsistent. To our knowledge, valid measures do not exist to measure fall risk with performance of mobility ADL and IADL tasks in the context of a person's environment and approach to task. Clinical judgment was used to determine risky behavior, reducing the transparency of our methods and potentially limiting the reliability and validity of our results. Our study highlights the need to develop and validate tools to assess risk when performing everyday activities in the person's own environment.
Second, cognition was measured with a relatively insensitive instrument, without specific evaluation of executive functioning. Third, we focused on the risk involved in selected common everyday activities in which older adults engage; it would not be possible to identify all possible risky activities in which a person may engage. We also did not determine whether the specific activities with hazardous performance were the activities during which a person fell during follow-up assessment, which would be unlikely given the wide range of activities performed in a year and the relative infrequency of falls. One fifth of the participants did not respond to a questionnaire item asking about the circumstances of their falls, and almost half of the respondents (46%) indicated that the circumstances of their falls did not match any of the fall categories listed. Instead, our research indicates that performance of any of these activities in a hazardous manner serves as an indicator of potential hazardous performance with other complex mobility maneuvers. The dose-response association shows that the greater the percentage of activities that are deemed risky on physical therapy assessment, the greater the future risk of falls. Fourth, all participants in this sample received a multifactorial intervention following the baseline assessment. These findings may not generalize to other populations.
Strengths of the study included its comprehensive in-home evaluation of balance, gait, and fall risk factors; its incorporation of the evaluation findings into an assessment of judgment within the context of a person's performance of everyday mobility activities; and its prospective follow-up of falls using monthly calendars. The study's focus on daily activities makes it especially relevant to the needs of older adults.
In summary, our analyses suggest that among older adults at risk for falls, declines in cognition are associated with performance of mobility activities in a manner that is risky relative to individuals' abilities. Engagement in risky mobility activities, in part, mediates the relationship between cognition and falls. Physical therapists should assess cognition, be aware that even mild cognitive declines may lead to unsafe performance of mobility tasks, and take appropriate steps to identify and limit unsafe activities to reduce fall risk. Older adults at fall risk should be assessed for cognition. Older adults with even mildly declining cognition may benefit from an assessment of their fall risk with performance of mobility ADL and IADL tasks, with the goal of improving safety through modifications in task performance.
Footnotes
Ms Shea and Dr Mahoney provided concept/idea/research design and institutional liaisons. All authors provided writing. Dr Mahoney provided data collection, project management, and fund procurement. Dr Fischer, Dr Gangnon, Dr Janczewski, and Dr Mahoney provided data analysis. Ms Shea and Dr Mahoney provided institutional liaisons. Dr Gleason provided clerical support. Dr Gleason, Dr Gangnon, Dr Janczewski, Ms Shea, and Dr Mahoney provided consultation (including review of manuscript before submission).
This work was supported by the Centers for Disease Control and Prevention, National Center for Injury Prevention and Control (grant PA #02151 to Dr Mahoney); the National Institutes of Health, National Institute on Aging (grant #K23 AG024302 to Dr Gleason); and the Alzheimer's Disease Research Center (grant #P50 AG033514 to Dr Gleason).
The University of Wisconsin School of Medicine and Public Health Institutional Review Board approved the study.
This work was presented, in part, at the American Geriatrics Society Annual Meeting; May 11–14, 2011; National Harbor, Maryland.
References
- 1. Mahoney JE, Glysch RL, Guilfoyle SM, et al. Trends, risk factors, and prevention of falls in older adults in Wisconsin. WMJ. 2005;104:22–28 [PubMed] [Google Scholar]
- 2. Hauer K, Pfisterer M, Weber C, et al. Cognitive impairment decreases postural control during dual tasks in geriatric patients with a history of severe falls. J Am Geriatr Soc. 2003;51:1638–1644 [DOI] [PubMed] [Google Scholar]
- 3. Graafmans WC, Ooms ME, Hofstee HM, et al. Falls in the elderly: a prospective study of risk factors and risk profiles. Am J Epidemiol. 1996;143:1129–1136 [DOI] [PubMed] [Google Scholar]
- 4. Tinetti ME, Gordon C, Sogolow E, et al. Fall-risk evaluation and management: challenges in adopting geriatric care practices. Gerontologist. 2006;46:717–725 [DOI] [PubMed] [Google Scholar]
- 5. Anstey KJ, Wood J, Kerr G, et al. Different cognitive profiles for single compared with recurrent fallers without dementia. Neuropsychology. 2009;23:500–508 [DOI] [PubMed] [Google Scholar]
- 6. Gleason CE, Gangnon RE, Fischer BL, Mahoney JE. Increased risk for falling associated with subtle cognitive impairment: secondary analysis of a randomized clinical trial. Dement Geriatr Cogn Disord. 2009;27:557–563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mirelman A, Herman T, Brozgol M, et al. Executive function and falls in older adults: new findings from a five-year prospective study link fall risk to cognition. PLoS One. 2012;7:e40297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Montero-Odasso M, Verghese J, Beauchet O, Hausdorff JM. Gait and cognition: a complementary approach to understanding brain function and the risk of falling. J Am Geriatr Soc. 2012;60:2127–2136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Andersson AG, Kamwendo K, Seiger A, Appelros P. How to identify potential fallers in a stroke unit: validity indexes of four test methods. J Rehabil Med. 2006;38:186–191 [DOI] [PubMed] [Google Scholar]
- 10. Hausdorff JM, Doniger GM, Springer S, et al. A common cognitive profile in elderly fallers and in patients with Parkinson's disease: the prominence of impaired executive function and attention. Exp Aging Res. 2006;32:411–429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Buchner DM, Larson EB. Transfer bias and the association of cognitive impairment with falls. J Gen Intern Med. 1988;3:254–259 [DOI] [PubMed] [Google Scholar]
- 12. Anstey KJ, von Sanden C, Luszcz MA. An 8-year prospective study of the relationship between cognitive performance and falling in very old adults. J Am Geriatr Soc. 2006;54:1169–1176 [DOI] [PubMed] [Google Scholar]
- 13. Lezak MD. Neuropsychological Assessment. New York, NY: Oxford University Press; 1976 [Google Scholar]
- 14. Holtzer R, Friedman R, Lipton RB, et al. The relationship between specific cognitive functions and falls in aging. Neuropsychology. 2007;21:540–548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Herman T, Mirelman A, Giladi N, et al. Executive control deficits as a prodrome to falls in healthy older adults: a prospective study linking thinking, walking, and falling. J Gerontol A Biol Sci Med Sci. 2010;65:1086–1092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Faulkner KA, Redfern MS, Cauley JA, et al. ; Health, Aging, and Body Composition Study Multitasking: association between poorer performance and a history of recurrent falls. J Am Geriatr Soc. 2007;55:570–576 [DOI] [PubMed] [Google Scholar]
- 17. Siu KC, Chou LS, Mayr U, et al. Does Inability to allocate attention contribute to balance constraints during gait in older adults? J Gerontol A Biol Sci Med Sci. 2008;63:1364–1369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chapman GJ, Hollands MA. Evidence that older adult fallers prioritise the planning of future stepping actions over the accurate execution of ongoing steps during complex locomotor tasks. Gait Posture. 2007;26:59–67 [DOI] [PubMed] [Google Scholar]
- 19. Lafargue G, Noel M, Luyat M. In the elderly, failure to update internal models leads to over-optimistic predictions about upcoming actions. PLoS One. 2013;8:e51218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Barkley RA. Driving impairments in teens and adults with attention-deficit/hyperactivity disorder. Psych Clin North Am. 2004;27:233–260 [DOI] [PubMed] [Google Scholar]
- 21. Studenski S, Duncan PW, Chandler J, et al. Predicting falls: the role of mobility and nonphysical factors. J Am Geriatr Soc. 1994;42:297–302 [DOI] [PubMed] [Google Scholar]
- 22. Kiehn KA, Mahoney J, Jones AN, Hansen KE. Vitamin D supplement intake in elderly fallers. J Am Geriatr Soc. 2009;57:176–177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Maloney JE, Drinka TJ, Abler R, et al. Screening for depression: single question versus GDS. J Am Geriatr Soc. 1994;42:1006–1008 [DOI] [PubMed] [Google Scholar]
- 24. Moloney JE, Palta M, Johnson J, et al. Temporal association between hospitalization and rate of falls after discharge. Arch Intern Med. 2000;160:2788–2795 [DOI] [PubMed] [Google Scholar]
- 25. Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94 [DOI] [PubMed] [Google Scholar]
- 26. Eggermont LH, Gavett BE, Volkers KM, et al. Lower-extremity function in cognitively healthy aging, mild cognitive impairment, and Alzheimer's disease. Arch Phys Med Rehabil. 2010;91:584–588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gardner MM, Buchner DM, Robertson MC, Campbell AJ. Practical implementation of an exercise-based falls prevention programme. Age Ageing. 2001;30:77–83 [DOI] [PubMed] [Google Scholar]
- 28. Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50:M28–M34 [DOI] [PubMed] [Google Scholar]
- 29. Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233 [DOI] [PubMed] [Google Scholar]
- 30. Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–441 [DOI] [PubMed] [Google Scholar]
- 31. Mahoney JE, Shea TA, Przybelski R, et al. Kenosha County falls prevention study: a randomized, controlled trial of an intermediate-intensity, community-based multifactorial falls intervention. J Am Geriatr Soc. 2007;55:489–498 [DOI] [PubMed] [Google Scholar]
- 32. Wisconsin Institute for Healthy Aging Sure Step Algorithm. 2000. Available at: https://wihealthyaging.org/sure-step
- 33. Sheikh JI, Yesavage J. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol. 1986:165–173 [Google Scholar]
- 34. Khasnis A, Gokula RM. Romberg's test. J Postgrad Med. 2003;49:169–172 [PubMed] [Google Scholar]
- 35. Horak FB, Wrisley DM, Frank J. The Balance Evaluation Systems Test (BESTest) to differentiate balance deficits. Phys Ther. 2009;89:484–498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tinetti ME. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc. 1986;34:119–126 [DOI] [PubMed] [Google Scholar]
- 37. Shumway-Cook A, Horak FB. Assessing the influence of sensory interaction on balance: suggestion from the field. Phys Ther. 1986;66:1548–1550 [DOI] [PubMed] [Google Scholar]
- 38. Berg KO, Wood-Dauphinée SL, Williams JI, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83(suppl 2):S7–S11 [PubMed] [Google Scholar]
- 39. Shumway-Cook A, Baldwin M, Polissar NL, Gruber W. Predicting the probability for falls in community-dwelling older adults. Phys Ther. 1997;77:812–819 [DOI] [PubMed] [Google Scholar]
- 40. Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;80:896–903 [PubMed] [Google Scholar]
- 41. The prevention of falls in later life: a report of the Kellogg International Work Group on the Prevention of Falls by the Elderly. Dan Med Bull. 1987;34(suppl 4):1–24 [PubMed] [Google Scholar]
- 42. Lin MR, Wolf SL, Hwang HF, et al. A randomized, controlled trial of fall prevention programs and quality of life in older fallers. J Am Geriatr Soc. 2007;55:499–506 [DOI] [PubMed] [Google Scholar]
- 43. Sodergren M. Lifestyle predictors of healthy ageing in men. Maturitas. 2013;75:113–117 [DOI] [PubMed] [Google Scholar]
- 44. Haslam RA, Sloane J, Hill LD, et al. What do older people know about safety on stairs? Ageing Soc. 2001;21:759–776 [Google Scholar]
- 45. Resnick B, Galik E, Boltz M. Function focused care approaches: literature review of progress and future possibilities. J Am Med Dir Assoc. 2013;14:313–318 [DOI] [PubMed] [Google Scholar]
- 46. Gerson LW, Camargo CA, Wilber ST. Home modification to prevent falls by older ED patients. Am J Emerg Med. 2005;23:295–298 [DOI] [PubMed] [Google Scholar]
- 47. Clemson L, Cumming RG, Kendig H, et al. The effectiveness of a community-based program for reducing the incidence of falls in the elderly: a randomized trial. J Am Geriatr Soc. 2004;52:1487–1494 [DOI] [PubMed] [Google Scholar]
- 48. Ben-Itzhak R, Giladi N, Gruendlinger L, Hausdorff JM. Can methylphenidate reduce fall risk in community-living older adults? A double-blind, single-dose cross-over study. J Am Geriatr Soc. 2008;56:695–700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Schwenk M, Zieschang T, Oster P, Hauer K. Dual-task performances can be improved in patients with dementia: a randomized controlled trial. Neurology. 2010;74:1961–1968 [DOI] [PubMed] [Google Scholar]
- 50. Silsupadol P, Shumway-Cook A, Lugade V, et al. Effects of single-task versus dual-task training on balance performance in older adults: a double-blind, randomized controlled trial. Arch Phys Med Rehabil. 2009;90:381–387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Yogev-Seligmann G, Hausdorff JM, Giladi N. The role of executive function and attention in gait. Mov Disord. 2008;23:329–342; quiz 472 [DOI] [PMC free article] [PubMed] [Google Scholar]