Abstract
Objective
To determine the prevalence and nature of residual cognitive disability after inpatient rehabilitation for children aged 7-18 years with traumatic injuries.
Study design
This retrospective cohort study included children aged 7-18 years in the Uniform Data System for Medical Rehabilitation who underwent inpatient rehabilitation for traumatic injuries in 523 facilities from 2002-2011. Traumatic injuries were identified by standardized Medicare Inpatient Rehabilitation Facility–Patient Assessment Instrument codes. Cognitive outcomes were measured by the Functional Independence Measure instrument. A validated, categorical staging system derived from responses to the items in the cognitive domain of the functional independence measure was used and consisted of clinically relevant levels of cognitive achievement from stage 1 (total cognitive disability) to stage 7 (completely independent cognitive function).
Results
There were 13 798 injured children who completed inpatient rehabilitation during the 10-year period. On admission to inpatient rehabilitation, patients with traumatic brain injury (TBI) had more cognitive disability (median stage 2) than those with spinal cord injury or other injuries (median stage 5). Cognitive functioning improved for all patients, but children with TBI still tended to have significant residual cognitive disability (median stage on discharge, 4).
Conclusions
Injured children gained cognitive functionality throughout inpatient rehabilitation. Those with TBI had more severe cognitive disability on admission and more residual disability on discharge. This is important not only for patient and family expectation setting but also for resource and service planning, as discharge from inpatient rehabilitation is a critical milestone for reintegration into society for children with serious injury.
Although injury is the leading cause of pediatric death, fatalities in injured children are rare (occurring in 5% of moderate to severe injuries1,2). Despite high survival rates, the overwhelming majority of seriously injured children suffer physical, cognitive, and quality of life impairments. These children often require inpatient rehabilitation to promote function and recovery. Although there are many outcomes that can be measured after serious injury, 2 important and commonly measured domains are physical and cognitive functionality.
We recently demonstrated that even though children aged 7-18 years with traumatic injuries uniformly had severe physical disability on admission to inpatient rehabilitation, those with traumatic brain injury (TBI) demonstrated significant improvement in physical functioning at the time of discharge.3 Other prior research has focused on cognitive disability following various injuries in children. One large meta-analysis of 28 studies from 1988-2007 summarized neurocognitive outcomes for children after TBI and found that children with moderate TBI (defined as an initial Glasgow Coma Scale score of 9-12) and severe TBI (Glasgow Coma Scale score of 3-8) had more intellectual, executive functioning, and memory deficits compared with patients with mild TBI.4 There was a dose-response whereby the symptoms of patients with mild TBI resolved over time, and the most severely injured patients had persistent neurocognitive disability >24 months after injury. This study filled an important gap in the literature by quantifying the course of recovery and the prevalence of persistent long-term deficits among children with TBI. To date, however, there are no reports of more acute cognitive outcomes in a large, contemporary cohort of injured pediatric patients at the time of discharge from inpatient rehabilitation. Although it is useful to follow injured patients serially to determine their long-term outcomes, it is important to systematically capture the functionality of patients on discharge from inpatient rehabilitation, as this is a critical stage for their recovery and reintegration into society.5 The goal of this current study was to determine the prevalence and nature of cognitive disability among severely injured children and adolescents requiring inpatient rehabilitation using a practical and clinically relevant staging system. We also wanted to examine the distribution of cognitive disability by clinically relevant groups of injuries. These findings would have implications not only for patient and family expectation setting during active rehabilitation but also for postrehabilitation planning for ongoing assistance and care.
Methods
This retrospective cohort study identified patients in the Uniform Data System for Medical Rehabilitation (UDSMR), with data from >829 rehabilitation centers, representing approximately 72% of the 1152 Centers for Medicare & Medicaid Services–designated inpatient rehabilitation facilities in the US.6 Evaluation of each inpatient in the database is completed using the Inpatient Rehabilitation Facilities–Patient Assessment Instrument (IRF-PAI)7 developed by the Centers for Medicare & Medicaid Services. The IRF-PAI includes demographic information (age, sex, race/ethnicity), hospitalization and diagnostic information (length of stay [LOS], payer, impairment codes, clinical diagnoses from International Classification of Diseases, Ninth Revision E codes), and functional status measured using the Functional Independence Measure (FIM) instrument. All UDSMR patients aged 7-18 years from 2002-2011 who completed rehabilitation immediately following an injury-related acute care hospitalization were included in the analysis.
Exposures
Individual injuries for each patient were identified using the 20 trauma-related IRF-PAI impairment codes assigned on admission to the rehabilitation center according to the injury or injuries for which each patient primarily required rehabilitation.7 The 20 codes were then grouped into the following 11 categories: TBI, TBI and multiple fracture/ amputation, TBI and spinal cord injury (SCI), quadriplegia (complete), quadriplegia (incomplete or unspecified), paraplegia (complete), paraplegia (incomplete or unspecified), other SCI, SCI and multiple fracture/amputation, burns, and other multitrauma. Further consolidation into 4 broader categories was also used: any TBI, quadriplegia, paraplegia, or other (which included combinations of TBI and SCI, TBI and multiple fracture/amputation, SCI and multiple fracture/amputation, burns, or other multitrauma). These 4 categories were created to characterize the outcomes of children with clinically meaningful subgroups of disabling injuries from multitrauma, as defined by the center-assigned IRF-PAI impairment codes, and were retained after finding differences between these groups in our study of physical functionality.3
Outcomes
Functional status of patients was assessed using the FIM instrument, 8,9 a valid and reliable measure of functionality,10,11 which has previously been used to evaluate trauma-related disability at short- and long-term intervals in children.12-14 The UDSMR database includes consistent FIM measurements documented by trained personnel on admission to and at discharge from the rehabilitation hospital. The FIM instrument is composed of 13 motor and 5 cognitive items, consisting of comprehension, expression, social interaction, problem solving, and memory. Each item can be scored from 1 to 7, with an absolute total FIM score of 18-126. Higher scores are associated with higher levels of functioning.
The primary outcome of this analysis was discharge cognitive functioning, based on a compilation of the variation in functioning across the 5 cognitive FIM items. Summary cognitive FIM scores have been categorized into a clinically relevant and previously validated staging system, consisting of 7 stages ranging from stage 1 (total cognitive disability) to stage 7 (complete cognitive independence).15,16 Each stage summarizes the variation in functioning across the 5 domains assessed into a clinically relevant set of thresholds for overall cognitive activity that the child must meet or exceed. Detailed definitions of each stage have previously been published. 16 As an example, patients with stage 1 (total assistance) can provide only 25% of the effort necessary to communicate and express needs; those with stage 4 can communicate and express most needs but may still need prompting for problem solving and memory up to 50% of the time; and those with stage 7 (complete independence) can provide 100% of required communication and expression without aid or assistance.
Statistical Analyses
Standard descriptive statistics were used to summarize demographic variables, injury characteristics, and outcomes. Derived variables included the mean Δ stage (ie, the individual patient’s average change in cognitive functioning stage from admission to discharge). ANOVA and χ2 tests were used to examine demographic differences across the major injury subgroups. A paired t-test was used to compare these mean Δ stages within each injury impairment code. The differences in median LOS values in days across the impairment codes, and over time, were examined by using the Kruskal- Wallis test.
Results
From 2002 to 2011, there were 13 798 patients aged 7-18 years who completed trauma-related inpatient rehabilitation at the 523 facilities that cared for children. Table I shows the sample demographics across the 4 major injury subgroups. Statistically significant differences were seen for all demographics among subgroup, most notably that SCI patients were more likely to be male and older.
Table I.
Demographic and rehabilitation-related sample characteristics by major injury subgroup (total N = 13 798)
| TBI | Quadriplegia | Paraplegia | Other | P value | |
|---|---|---|---|---|---|
| Age at the start of rehabilitation, mean (SD) | 16.0 (2.1) | 16.6 (1.4) | 16.5 (1.6) | 16.3 (1.9) | <.0001 |
| 7-9 y, % | 2.53 | 0.42 | 0.8 | 1.9 | <.0001 |
| 10-12 y, % | 4.34 | 0.74 | 1.61 | 3.11 | |
| 13-15 y, % | 20.09 | 17.76 | 17.28 | 15.8 | |
| 16-18 y, % | 73.05 | 81.08 | 80.31 | 79.19 | |
| Sex | <.0001 | ||||
| Male | 69.96 | 77.7 | 73.73 | 58.38 | |
| Female | 30.04 | 22.3 | 26.27 | 41.62 | |
| Race/ethnicity | <.0001 | ||||
| White, non-Hispanic | 72.87 | 65.05 | 53.07 | 75.86 | |
| Black, non-Hispanic | 11.29 | 18.49 | 25.96 | 10.17 | |
| Hispanic/Latino | 11.78 | 12.26 | 16.79 | 9.96 | |
| Other | 4.07 | 4.19 | 4.18 | 4.01 | |
| Primary payer | <.0001 | ||||
| Private | 69.19 | 65.54 | 55.63 | 70.7 | |
| Public | 21.88 | 25.16 | 31.91 | 21.43 | |
| Other | 8.92 | 9.3 | 12.46 | 7.87 | |
| Admission to rehabilitation from | <.0001 | ||||
| Acute unit of another facility | 56.39 | 53.54 | 57.32 | 57.87 | |
| Acute unit of own facility | 38.65 | 41.27 | 38.75 | 39.3 | |
| Other | 4.96 | 5.18 | 3.94 | 2.83 | |
| Discharge living setting | <.0001 | ||||
| Home | 90.01 | 82.56 | 87.38 | 90.34 | |
| Acute or subacute care | 8.27 | 12.16 | 8.84 | 7.97 | |
| Rehabilitation facility | 1.11 | 4.86 | 3.22 | 1.24 | |
| Died | 0.05 | 0 | 0 | 0.02 | |
| Other | 0.56 | 0.42 | 0.56 | 0.43 |
The Figure shows the distribution of admission and discharge stages for 4 subgroups: TBI, quadriplegia, paraplegia, and other injuries. More than 75% of children with TBI were of cognitive stage 1, 2, or 3 on admission, with >33% still at these stages on discharge. These stages correspond to the most severe disability in the domains of comprehension, expression, social interaction, problem solving, and memory. Children with quadriplegia and paraplegia as their main IRF-PAI code had higher levels of cognitive functionality on admission compared with the TBI group. Median admission stage of functioning for these patients was 6, and the majority of these patients improved to stage 7 on discharge. The majority of the TBI group had severe cognitive disability on admission and improved to only moderate disability on discharge. Table II shows the median admission and discharge stages with IQRs, the average difference between the stages, and the mean LOS for the 11 grouped impairment codes. Even though all injury groups demonstrated improvements in stage on discharge from rehabilitation (P < .0001 for each), children with TBI had more severe discharge cognitive disability compared with those with SCI, burns, or multiple injuries. As reported in our prior work, patients with SCI had longer LOS values than those without SCI (P < .0001). When examining trends over time, there was an overall slight decrease in LOS (median 15 days in 2002 [IQR 5-29] to median 13 days in 2011 [IQR 8-25 days], P = .02). The discharge cognitive stages over time have remained stable (median 5 [IQR 4-6]) for 2002-2011.
Figure.
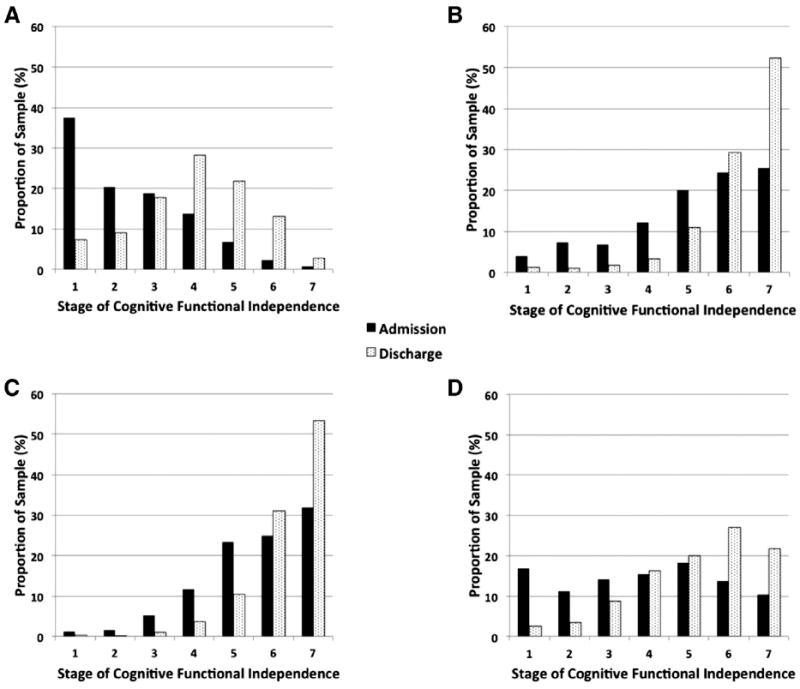
The proportion of the study population at each cognitive stage* at admission and discharge from inpatient rehabilitation by major injury subgroup. A, TBI (n = 6297). B, quadriplegia (n = 946). C, paraplegia (n = 1244). D, other injuries (n = 5311).
*Disability stages range from stage 1 (severe cognitive disability) to stage 7 (complete cognitive function).
Table II.
Distribution of admission and discharge stages for functional independence and length of inpatient rehabilitation
| Injury impairment code | N | % | Cognitive stage
|
Median LOS, d† | ||
|---|---|---|---|---|---|---|
| Median admit cognitive stage (IQR) | Median discharge cognitive stage (IQR) | Mean paired difference between admit and discharge stage* | ||||
| TBI | 6297 | 45.6 | 2 (1-3) | 4 (3-5) | 1.6 | 20 |
| TBI + multiple fracture/amputation | 3001 | 21.8 | 3 (1-4) | 5 (4-6) | 1.5 | 13 |
| Other multitrauma | 1379 | 10.0 | 5 (4-6) | 6 (5-7) | 0.9 | 9 |
| Paraplegia, Complete | 683 | 5.0 | 6 (5-7) | 7 (6-7) | 0.7 | 29 |
| Paraplegia, incomplete or unspecified | 561 | 4.1 | 6 (5-7) | 7 (6-7) | 0.7 | 21 |
| Quadriplegia, incomplete or unspecified | 532 | 3.9 | 6 (5-7) | 7 (6-7) | 0.9 | 33 |
| Quadriplegia, vomplete | 414 | 3.0 | 5 (4-6) | 6 (6-7) | 1.3 | 46 |
| TBI + SCI | 330 | 2.4 | 4 (2-5) | 5 (4-6) | 1.5 | 23 |
| Other SCI | 244 | 1.8 | 6 (5-7) | 7 (6-7) | 0.8 | 11 |
| SCI + multiple fracture/amputation | 188 | 1.4 | 5 (4-6) | 6 (5-7) | 0.8 | 18 |
| Burns | 169 | 1.2 | 6 (5-7) | 6 (5-7) | 0.7 | 12 |
P < .0001 for all individual mean, paired Δ stages.
P < .0001 for LOS across various impairment codes.
Discussion
As a group, children with TBI had very poor cognitive functioning on admission to inpatient rehabilitation, improved during the rehabilitation hospitalization, and were discharged with significant residual cognitive disability. Specifically, the majority of patients with TBI had an admission stage of 1, 2, or 3 (corresponding to moderate to complete difficulty with comprehension, expression, social interaction, problem solving, and memory) and a discharge stage of 3, 4, or 5 (corresponding to mild to moderate difficulties with these domains). In contrast, fewer patients with SCI and other injuries had clinically important cognitive disability on admission, with the vast majority of patients with SCI improving by discharge to be able to demonstrate complete or near-complete independence with cognitive function. Of note, patients with other injuries or multitrauma (eg, TBI and SCI, extremity injuries with TBI or SCI, burns) had a more equal distribution of outcomes across the 7 stages on discharge. This is in direct contrast to our prior work that assessed physical disability with this same cohort, where patients with SCI had more severe disability and less recovery following inpatient rehabilitation.
This study builds on prior work assessing the cognitive functioning of children following disabling injuries. Older studies used the National Pediatric Trauma Registry, maintained from1985 through 2001. One analysis modeled recovery of children from disabling TBI and found that, of those without preexisting cognitive deficit, intubation, coma at admission to the trauma center, or an injury severity score of >27, 96% would achieve cognitive independence by discharge from the trauma center.14 Another National Pediatric Trauma Registry study of children with multitrauma but without significant head injury showed much higher rates of physical disability on discharge from the acute care hospitalization compared with those with cognitive disability.12 Two additional recent prospective, multicenter studies of school-age children and younger adolescents with TBI showed more residual cognitive disability in moderate and severely injured patients with TBI at 3 and 12 months following injury compared with those with mild TBI.17,18 As demonstrated with the existing literature, functional disability can be measured at various milestones along the course of recovery, from the point of discharge from acute care to years following the injury. There is evidence to show that some children with TBI may continue to have neurocognitive recovery ≥10 years following injury and that the “final” assessment of outcomes may be most appropriately made in adulthood.19,20 Additionally, there is often attrition of patients in longitudinal studies of severely injured patients, which may bias the sample and lead to an inaccurate assessment of the spectrum of outcomes.20,21 The distinct advantage of measuring functional outcomes at the end of inpatient rehabilitation is that it marks a critical point in recovery for the most severely injured children. This information can be used to establish reasonable expectations for patients’ families for the rehabilitation phase of care. Additionally, understanding the differences between injury patterns and various outcomes is critical for predicting the type and level of support necessary on discharge from inpatient rehabilitation. As an example, patients with SCI require more technology-based assistance, and patients with TBI need programmatic and educational services.22,23 Patients with TBI could benefit from comprehensive outcomes testing specifically assessing cognitive function, school district assessments of patients and implementation of accommodations, ongoing outpatient cognitive rehabilitation, and psychoeducation of patients with concomitant mental health comorbidities following their injury.
Although 2 recent studies used the UDSMR and absolute FIM scores to study postrehabilitation outcomes in children and adults with TBI24 and SCI,25 they did not specifically focus on children, include patients with other injuries, or use the more clinically relevant cognitive stages of functioning that we used in this analysis. Total, absolute FIM scores may be less helpful in understanding the functional needs of populations across the physical and cognitive domains. 3 For example, we know that children who achieve FIM cognitive stage 4 (the median stage reached by those with TBI by rehabilitation discharge) will be able to communicate and express most needs but may still need prompting for problem solving and memory up to 50% of the time. Although this analysis focused on cognitive functionality, the interaction of cognitive and physical disability must also be considered, as completing cognitive tasks can influence performance on physical tasks when performed in tandem compared with their independent assessment.26
Several limitations should be noted. First, the database may not be completely representative of all severely injured patients discharged from acute care; there may have been individuals with financial or geographic barriers to rehabilitation. However, the large size and geographic diversity of the sample suggest that findings are likely broadly generalizable to seriously injured children who would be referred for inpatient rehabilitation. Additionally, there were no consistently documented International Classification of Diseases, Ninth Revision E codes for injury mechanism, which precluded analyses associating outcomes with injury causation, which would have contributed to priority setting for efforts to prevent injuries from specific causes. In addition, there was limited information on the actual rehabilitation care provided, which prevented assessment of important quality of care measures.27 Another limitation is that many children in this age range continue to have ongoing neurodevelopment and/or spontaneous recovery, so assessment of functionality at discharge from rehabilitation may not reflect long-term function or assistive needs. However, this point of transition from inpatient rehabilitation to reemersion into society is important to anticipate the level of assistance necessary for certain injuries. Additionally, considering the main outcome in the 4 broad injury groups may have reduced the granularity of the analyses, particularly in the “other” category that included a heterogeneous cohort of multitrauma and other trauma. As an example, patients with multitrauma or non-TBI/non-SCI injuries could have poor cognitive outcomes because of secondary effects from other factors not measured, such as pain, concentration, and psychological sequelae. Finally, the FIM scores provide a gross assessment of functionality and not a comprehensive evaluation of cognitive ability, quality of life, behavior, decision making, or other outcomes, although the FIM staging system used is clinically relevant for rehabilitation goals.16
Acknowledgments
We thank Paulette M. Niewczyk, MPH, PhD, and the staff at the UDSMR at the University of Buffalo, State University of New York, for use of the data, and Huaqing Zhao, PhD, for assistance with data analysis.
Supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (1K08HD073241-01 to M.Z.). The views presented are those of the authors and not necessarily the views of the National Institutes of Health.
Glossary
- FIM
Functional Independence Measure
- IRF-PAI
Inpatient Rehabilitation Facilities–Patient Assessment Instrument
- LOS
Length of stay
- SCI
Spinal cord injury
- TBI
Traumatic brain injury
- UDSMR
Uniform Data System for Medical Rehabilitation
Footnotes
The authors declare no conflicts of interest.
References
- 1.Centers for Disease Control and Prevention, National Centers for Injury Prevention and Control. Ten leading causes of death and injury. [December 2, 2011]; http://www.cdc.gov/injury/wisqars/LeadingCauses.html.
- 2.Burd RS, Madigan D. The impact of injury coding schemes on predicting hospital mortality after pediatric injury. Acad EmergMed. 2009;16:639–45. doi: 10.1111/j.1553-2712.2009.00446.x. [DOI] [PubMed] [Google Scholar]
- 3.Zonfrillo MR, Durbin DR, Winston FK, Zhao H, Stineman MG. Physical disability after injury-related inpatient rehabilitation in children. Pediatrics. 2013;131:e206–13. doi: 10.1542/peds.2012-1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Babikian T, Asarnow R. Neurocognitive outcomes and recovery after pediatric TBI: meta-analytic review of the literature. Neuropsychology. 2009;23:283–96. doi: 10.1037/a0015268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jaffe KM. Pediatric trauma rehabilitation: a value-added safety net. J Trauma Inj Infect Crit Care. 2008;64:819–23. doi: 10.1097/TA.0b013e318165f177. [DOI] [PubMed] [Google Scholar]
- 6.Uniform Data System for Medical Rehabilitation (UDSMR) [December 15, 2011]; http://www.udsmr.org.
- 7.Centers for Medicare & Medicaid Services (CMS) Inpatient Rehabilitation Facility (IRF) Patient Assessment Instrument (PAI) [March 29, 2012]; http://www.cms.gov/InpatientRehabFacPPS/04_IRFPAI.asp.
- 8.Keith RA, Granger CV, Hamilton BB, Sherwin FS. The functional independence measure: a new tool for rehabilitation. Adv Clin Rehabil. 1987;1:6–18. [PubMed] [Google Scholar]
- 9.Hamilton BB, Granger CV, Sherwin FS, Zielezny M, Tashman JS. A uniform national data system for medical rehabilitation. In: Fuhrer M, editor. Rehabilitation outcomes: Analysis and measurement. Baltimore, MD: Brookes; 1987. pp. 137–47. [Google Scholar]
- 10.Heinemann AW, Linacre JM, Wright BD, Hamilton BB, Granger C. Relationships between impairment and physical disability as measured by the functional independence measure. Arch Phys Med Rehabil. 1993;74:566–73. doi: 10.1016/0003-9993(93)90153-2. [DOI] [PubMed] [Google Scholar]
- 11.Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 1996;77:1226–32. doi: 10.1016/s0003-9993(96)90184-7. [DOI] [PubMed] [Google Scholar]
- 12.Aitken ME, Jaffe KM, DiScala C, Rivara FP. Functional outcome in children with multiple trauma without significant head injury. Arch Phys Med Rehabil. 1999;80:889–95. doi: 10.1016/s0003-9993(99)90079-5. [DOI] [PubMed] [Google Scholar]
- 13.Willis CD, Gabbe BJ, Butt W, Cameron PA. Assessing outcomes in paediatric trauma populations. Injury. 2006;37:1185–96. doi: 10.1016/j.injury.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 14.Wechsler B, Kim H, Gallagher PR, DiScala C, Stineman MG. Functional status after childhood traumatic brain injury. J Trauma Inj Infect Crit Care. 2005;58:940–9. doi: 10.1097/01.ta.0000162630.78386.98. [DOI] [PubMed] [Google Scholar]
- 15.Stineman MG, Ross RN, Fiedler R, Granger CV, Maislin G. Functional independence staging: conceptual foundation, face validity, and empirical derivation. Arch Phys Med Rehabil. 2003;84:29–37. doi: 10.1053/apmr.2003.50061. [DOI] [PubMed] [Google Scholar]
- 16.Stineman MG, Ross RN, Fiedler R, Granger CV, Maislin G. Staging functional independence validity and applications. Arch Phys Med Rehabil. 2003;84:38–45. doi: 10.1053/apmr.2003.50060. [DOI] [PubMed] [Google Scholar]
- 17.McCarthy ML, MacKenzie EJ, Durbin DR, Aitken ME, Jaffe KM, Paidas CN, et al. Health-related quality of life during the first year after traumatic brain injury. Arch Pediatr Adolesc Med. 2006;160:252–60. doi: 10.1001/archpedi.160.3.252. [DOI] [PubMed] [Google Scholar]
- 18.Rivara FP, Koepsell TD, Wang J, Temkin N, Dorsch A, Vavilala MS, et al. Disability 3, 12, and 24 months after traumatic brain injury among children and adolescents. Pediatrics. 2011;128:e1129–38. doi: 10.1542/peds.2011-0840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson V, Godfrey C, Rosenfeld JV, Catroppa C. Predictors of cognitive function and recovery 10 years after traumatic brain injury in young children. Pediatrics. 2012;129:e254–61. doi: 10.1542/peds.2011-0311. [DOI] [PubMed] [Google Scholar]
- 20.Horneman G, Emanuelson I. Cognitive outcome in children and young adults who sustained severe and moderate traumatic brain injury 10 years earlier. Brain Inj. 2009;23:907–14. doi: 10.1080/02699050903283239. [DOI] [PubMed] [Google Scholar]
- 21.Anderson V, Catroppa C, Morse S, Haritou F, Rosenfeld JV. Intellectual outcome from preschool traumatic brain injury: a 5-year prospective, longitudinal study. Pediatr. 2009;124:e1064–71. doi: 10.1542/peds.2009-0365. [DOI] [PubMed] [Google Scholar]
- 22.Henderson S, Skelton H, Rosenbaum P. Assistive devices for children with functional impairments: impact on child and caregiver function. Dev Med Child Neurol. 2008;50:89–98. doi: 10.1111/j.1469-8749.2007.02021.x. [DOI] [PubMed] [Google Scholar]
- 23.Glang A, Todis B, Thomas CW, Hood D, Bedell G, Cockrell J. Return to school following childhood TBI: who gets services? Neurorehabil. 2008;23:477–86. [PubMed] [Google Scholar]
- 24.Granger CV, Markello SJ, Graham JE, Deutsch A, Reistetter TA, Ottenbacher KJ. The Uniform Data System for Medical Rehabilitation: report of patients with traumatic brain injury discharged from rehabilitation programs in 2000-2007. Am J Phys Med Rehabil. 2010;89:265–78. doi: 10.1097/PHM.0b013e3181d3eb20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Granger CV, Karmarkar AM, Graham JE, Deutsch A, Niewczyk P, Divita MA, et al. The Uniform Data System for Medical Rehabilitation: report of patients with traumatic spinal cord injury discharged fromrehabilitation programs in 2002-2010. AmJ PhysMed Rehabil. 2012;91:289–99. doi: 10.1097/PHM.0b013e31824ad2fd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Katz-Leurer M, Rotem H, Keren O, Meyer S. Effect of concurrent cognitive tasks on gait features among children post-severe traumatic brain injury and typically-developed controls. Brain Inj. 2011;25:581–6. doi: 10.3109/02699052.2011.572943. [DOI] [PubMed] [Google Scholar]
- 27.Rivara FP, Ennis SK, Mangione-Smith R, Mackenzie EJ, Jaffe KM. Quality of care indicators for the rehabilitation of children with traumatic brain injury. Arch Phys Med Rehabil. 2012;93:381–5.e9. doi: 10.1016/j.apmr.2011.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]


