Abstract
Valve replacement is typically the most appropriate option for treating aortic valve stenotic insufficiency. However, neither mechanical nor bioprosthetic replacement components preserve the circumferential expansion and contraction of a native aortic annulus during the cardiac cycle, because the prosthetic ring is affixed to the annulus.
A 64-year-old man presented with a bicuspid and stenotic aortic valve, and the native annulus was too small to accommodate a porcine replacement valve. We fashioned new aortic leaflets from bovine pericardium with use of a template, and we affixed the sinotubular junction with use of inner and outer stabilization rings. Postoperative echocardiograms revealed coaptation of the 3 new leaflets with no regurgitation. At the patient's 5.5-year follow-up examination, echocardiograms showed flexible leaflet movement with a coaptation height of 7 mm, and expansion and contraction of the aortic annulus similar to that of a normal native annulus. The transvalvular pressure gradient was insignificant. If long-term durability of the new leaflets is confirmed, this method of leaflet replacement and fixation of the sinotubular junction might serve as an acceptable alternative to valve replacement in the treatment of aortic valve stenosis. We describe the patient's case and present our methods and observations.
Key words: Aortic valve/physiology/surgery, aortic valve stenosis/surgery, biomechanics, heart valve prosthesis implantation, prosthesis design, treatment outcome
More aortic valve diseases are treated by means of valve replacement than by valve repair. Replacement, whether with a mechanical or bioprosthetic valve, does not preserve the dynamic changes of the native aortic annulus during the cardiac cycle, because the prosthetic ring is affixed to the annulus. In addition, leaflet motion and area are limited by the 3 stent-posts of a tissue valve or by the ring of a mechanical valve. Consequently, prosthetic valves retain only the opening-and-closing function of the leaflets, and not annular contraction or expansion, during the cardiac cycle. If leaflet replacement alone is performed in the treatment of aortic valve disease, the dynamic functioning of the aortic annulus is expectedly preserved. In a patient who had a bicuspid and stenotic aortic valve, we performed leaflet replacement that involved the use of bovine pericardium and fixation of the sinotubular junction (STJ). We examined leaflet movement and annular dynamic capability during a 5.5-year follow-up period, and we report the case and our findings.
Case Report
A 64-year-old man presented at our hospital with palpitations, easily induced fatigue, and dyspnea on exertion. Echocardiograms revealed moderately severe mitral stenotic insufficiency, moderate tricuspid regurgitation, chronic atrial fibrillation, and a calcified and bicuspid aortic valve with moderate stenotic insufficiency. The patient's left ventricular ejection fraction (LVEF) was 0.56, and his left atrial internal diameter was 53 mm.
In March 2007, the patient underwent corrective surgery. He was placed under moderately hypothermic cardiopulmonary bypass with use of cold-blood cardioplegic solution. We performed mitral valve replacement with a 27-mm Epic™ porcine valve (St. Jude Medical, Inc.; St. Paul, Minn), tricuspid annuloplasty, and the Cox maze III procedure for chronic atrial fibrillation. After the aortic valve was excised through a transverse aortotomy 1 cm above the commissures, we found that the annulus was too small to accommodate a 19-mm porcine replacement valve. We marked the tops of the 3 commissures with a medical pen, including an imaginary commissure between the fused right and left native leaflets. Even though the annulus was small (<20 mm), the size of the prospective STJ was 26 mm—reasonable for our patient (body surface area, 1.58 m2).1 We tailored 3 new leaflets from a bovine pericardial patch with use of a commercially available 26-mm C-Leafcon® template (ScienCity; Seoul, Republic of Korea) (Fig. 1A). The new pericardial leaflets were sutured to the annulus with continuous 5-0 polypropylene sutures. During suturing, the central two thirds of the pericardial leaflet was plicated in a 1.5:1 ratio to the annulus, and the lateral third closest to the commissure was sutured evenly (Fig. 1B). Fixation of the STJ was achieved with a 26-mm inner ring and a 30-mm outer ring® (ScienCity) and 18 interrupted mattress sutures of 4-0 polypropylene.2 The inner ring, which is made of Dacron and is a flexible but inelastic flat ring 5 mm wide, was placed inside the STJ to maintain a consistent dimension. The thicker and softer outer ring was placed outside the STJ and supported the role of the inner ring. The lower margin of the inner ring was placed more than 5 mm above both coronary ostia. Total cardiopulmonary bypass time was 235 min and aortic cross-clamping time was 198 min.
Fig. 1.
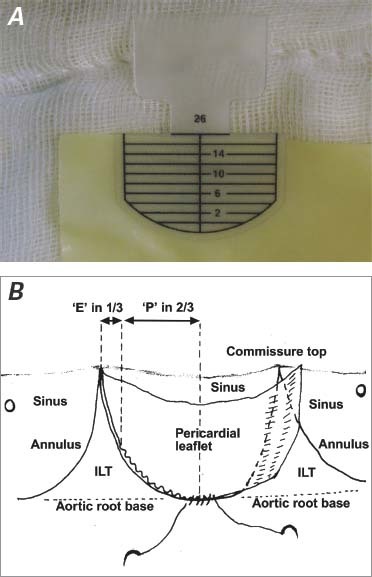
A) Photograph shows a 26-mm C-Leafcon® template, used to tailor bovine pericardium into new aortic leaflets. The template's length corresponds with the upper margin of the new leaflet patch, whose length is the diameter of the sinotubular junction. Leaflet size is calculated as follows: the height of the leaflet is 67% of the length of the upper margin; the template adds an extra 2 mm in width to the calculated leaflet size to allow for sutures. B) During suturing, the central two thirds of the suture margin of the pericardial leaflet was plicated in a 1.5:1 ratio (‘P’), and the lateral third of the leaflet was evenly attached to the annulus (‘E’).
ILT = interleaflet triangle
Postoperative echocardiograms revealed accurate coaptation of the 3 aortic valve leaflets, with no regurgitation. At 5.5 postoperative years, the aortic valve had flexible leaflet movement and a coaptation height of 7 mm. The average transvalvular pressure gradient was 2 mmHg at the annular level and 17 mmHg at the STJ level. In the echocardiographic parasternal long-axis view, the annulus was largest during ejection (17 mm) and smallest during isovolumic relaxation (12.5 mm) (Fig. 2). The patient's LVEF was 0.61, and his left atrial internal diameter was 40 mm. As of December 2013, he was doing well and had improved to New York Heart Association functional class I.
Fig. 2.
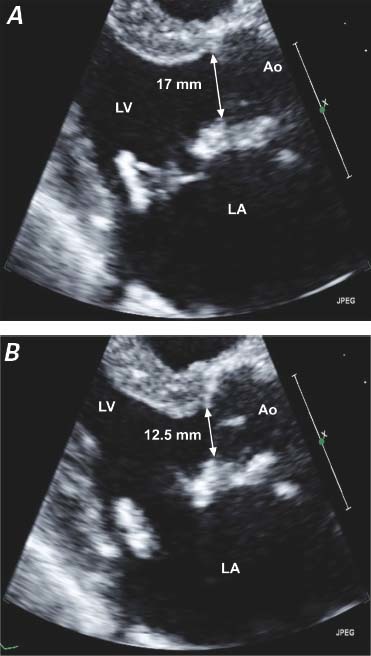
Postoperative transthoracic Doppler echocardiograms (parasternal long-axis views) at the end of the patient's 5.5-year follow-up period. A) During ejection, the aortic valve opens fully, and annular dimension increases to 17 mm. B) During isovolumic relaxation, the aortic valve closes with a 7-mm coaptation height, and annular dimension decreases to 12.5 mm.
Ao = ascending aorta; LA = left atrium; LV = left ventricle
Discussion
During the cardiac cycle, the aortic annulus is a dynamic structure.3 Valve replacement is the gold standard for treating aortic valve stenosis. However, mechanical and bioprosthetic valves compare unfavorably with native aortic valves in several ways: loss of annular dynamic capabilities due to fixation to the prosthetic ring, comparatively reduced leaflet area, and the placement of artificial material such as stents and sewing rings. In treating aortic diseases that involve valvular lesions only, leaflet replacement can be sufficient, even in patients who have a relatively small annulus. Our leaflet replacement procedure was introduced as part of the CARVAR technique,2 a comprehensive repair method for aortic valve and root diseases. A similar technique has been used in the treatment of pulmonary valve regurgitation.4 The leaflet replacement procedure has 3 important technical advantages: the new leaflet can be ideally sized for individual patients, the suturing technique changes a flat pericardial patch into a scoop-shaped leaflet, and the fixation of the STJ with the inner and outer rings maintains the coaptation capabilities of the new leaflets.
Unlike valve replacement, leaflet replacement preserves the anatomy of the aortic annulus and the native valve orifice and maintains their dynamic capabilities. In our patient, we observed dynamic contraction and expansion of the annulus in the same echocardiographic plane. Using small prosthetic valves frequently results in a significant transvalvular pressure gradient.5 However, after leaflet replacement, the gradient was insignificant in our patient, who had a small annulus. The new pericardial leaflets opened fully during systole, comparing favorably with the typically limited leaflet openings amidst the struts of bioprosthetic valves. After 5.5 years, the movement of the patient's new valve was strikingly similar to that of a normal native valve, and the valve leaflets had not thickened or become stenotic. The ring fixation of the STJ induced accurate coaptation of the new leaflets, preventing STJ dilation and subsequent coaptation failure.2 The dimensions of our patient's new STJ remained within the normal range of aortic root dimensions.1 Whereas the aortic annulus is a dynamic structure that exhibits substantial dimensional changes during the cardiac cycle,6 the area change at the STJ level is considerably less than the area changes in a patient's coronary sinuses and aortic annulus.7 Therefore, the fixed STJ might not significantly affect the hemodynamic conditions in the annulus.
During ejection, the maximal expansion of our patient's aortic annulus resulted in a transvalvular pressure gradient low enough to minimize turbulent damage to the aortic cusps.8 As a result, we anticipate that the new leaflets will remain durable. Our patient's 5.5-year postoperative results were good, and we are continuing his long-term monitoring. If further durability of the new leaflets is confirmed, this method of leaflet replacement and fixation of the STJ might prove to be an acceptable alternative to valve replacement in the treatment of aortic valve stenosis.
Acknowledgment
We gratefully acknowledge Meong Gun Song, MD (Song Meong Gun Heart Institute at Konkuk University Medical Center; Seoul, Republic of Korea) for editorial assistance with the manuscript, particularly in describing the surgical techniques.
References
- 1.Lin FY, Devereux RB, Roman MJ, Meng J, Jow VM, Jacobs A. Assessment of the thoracic aorta by multidetector computed tomography: age- and sex-specific reference values in adults without evident cardiovascular disease. J Cardiovasc Comput Tomogr. 2008;2(5):298–308. doi: 10.1016/j.jcct.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 2.Hahm SY, Choo SJ, Lee JW, Seo JB, Lim TH, Song JK. Novel technique of aortic valvuloplasty. Eur J Cardiothorac Surg. 2006;29(4):530–6. doi: 10.1016/j.ejcts.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 3.Cheng A, Dagum P, Miller DC. Aortic root dynamics and surgery: from craft to science. Philos Trans R Soc Lond B Biol Sci. 2007;362(1484):1407–19. doi: 10.1098/rstb.2007.2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jung TE, Baek JH, Lee DH. Pulmonary valve leaflet extension with bovine pericardium for treatment of pulmonary insufficiency. Tex Heart Inst J. 2011;38(1):68–70. [PMC free article] [PubMed] [Google Scholar]
- 5.Tanigawa K, Eishi K, Yamachika S, Hashizume K, Tada S, Yamane K. Comparison of the effects of aortic valve replacement using 19-mm Carpentier-Edwards Perimount bioprosthesis and 19-mm Medtronic Mosaic bioprosthesis. Ann Thorac Cardiovasc Surg. 2008;14(2):81–7. [PubMed] [Google Scholar]
- 6.de Heer LM, Budde RP, Mali WP, de Vos AM, van Herwerden LA, Kluin J. Aortic root dimension changes during systole and diastole: evaluation with ECG-gated multidetector row computed tomography. Int J Cardiovasc Imaging. 2011;27(8):1195–204. doi: 10.1007/s10554-011-9838-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lansac E, Lim HS, Shomura Y, Lim KH, Rice NT, Goetz W. A four-dimensional study of the aortic root dynamics. Eur J Cardiothorac Surg. 2002;22(4):497–503. doi: 10.1016/S1010-7940(02)00405-0. [DOI] [PubMed] [Google Scholar]
- 8.Dagum P, Green GR, Nistal FJ, Daughters GT, Timek TA, Foppiano LE. Deformational dynamics of the aortic root: modes and physiologic determinants. Circulation. 1999;100(19 Suppl):II54–62. doi: 10.1161/01.cir.100.suppl_2.ii-54. [DOI] [PubMed] [Google Scholar]


