Abstract
We investigated the overall success rate of percutaneous coronary intervention (PCI) as a treatment for coronary chronic total occlusion and sought to determine the predictive factors of technical success and of one-year major adverse cardiac events (MACE). These factors have not been conclusively defined.
Using data from our single-center PCI registry, we enrolled 269 consecutive patients (mean age, 56.13 ± 10.72 yr; 66.2% men) who underwent first-time PCI for chronic total occlusion (duration, ≥3 mo) from March 2006 through September 2010. We divided them into 2 groups: procedural success and procedural failure. We compared occurrences of in-hospital sequelae and one-year MACE between the groups, using multivariate models to determine predictors of technical failure and one-year clinical outcome.
Successful revascularization was achieved in 221 patients (82.2%). One-year MACE occurred in 13 patients (4.8%), with a predominance of target-vessel revascularization (3.7%). The prevalence of MACE was significantly lower in the procedural-success group (1.8% vs 18.8%; P <0.001). In the multivariate model, technical failure was the only predictor of one-year MACE. The predictors of failed procedures were lesion location, multivessel disease, the occurrence of dissection, a Thrombolysis In Myocardial Infarction flow grade of 0 before PCI, the absence of tapered-stump arterial structure, and an increase in serum creatinine level or lesion length.
In our retrospective, observational study, PCI was successful in a high percentage of chronic total occlusion patients and had a low prevalence of complications. This suggests its safety and effectiveness as a therapeutic option.
Key words: Angioplasty, balloon, coronary/methods; chronic disease/therapy; coronary occlusion/therapy; disease-free survival; heart diseases/prevention & control; multivariate analysis; myocardial revascularization; patient selection; retrospective studies; treatment outcome
As a treatment for coronary chronic total occlusion (CTO), percutaneous coronary intervention (PCI) is widely considered to be one of the most complex procedures in interventional cardiology. The low overall success rate of PCI is predominantly attributable to an inability to cross occlusions with an interventional guidewire.1–1 The overall prevalence of CTO on diagnostic angiograms is 15% to 30%. The results of recent studies show that one third to one half of patients with angiographically significant coronary artery disease have at least one CTO.6–8 On the basis of the available data, PCI is performed in only 10% to 15% of CTO angioplasty procedures2—most patients with CTO are referred for coronary artery bypass grafting (CABG) or are prescribed medical therapy.
New techniques and dedicated devices and improved operator experience have markedly increased the procedural success rate for occlusion recanalization. Investigators conducting large studies in different settings have reported short- and long-term survival advantages associated with successful PCI of chronic occlusions in comparison with failed procedures and have tried to identify clinical and procedural predictors of the success and outcome of PCI.1,9–12 However, debate continues in regard to whether the benefits of occlusion recanalization outweigh the risks and challenges. The specific factors that might enable the best choice of treatment for patients with CTO (PCI vs CABG or medical therapy) have not been conclusively identified.3,8,11
In the present retrospective study, we investigated the overall success rate of PCI in CTO patients. We sought to determine the in-hospital and one-year outcomes of patients undergoing the procedure, and identify factors that adversely influence the success rate of PCI and the occurrence of one-year major adverse cardiac events (MACE).
Patients and Methods
We extracted our data from the Tehran Heart Center Registry of Interventional Cardiology, a single-center registry in which all adult patients who undergo PCI are enrolled without any specific exclusionary criteria. Detailed data on demographic and clinical characteristics, procedures, complications, and clinical outcomes are documented in the registry. As a routine practice, follow-up data are obtained from all patients upon their discharge from the hospital, and then 1, 6, and 12 months after PCI during organized clinical visits or through telephone contact by trained research physicians and nurses.
Study Population
We identified all patients with CTO of a coronary artery (duration, ≥3 mo) who underwent first-time PCI at Tehran Heart Center from March 2006 through September 2010. Chronic occlusions of bypassed vessels, patients treated solely by means of plain old balloon angioplasty, and occlusions of estimated durations shorter than 3 months were excluded. Of 283 patients who met the inclusionary criteria, 14 had been lost to follow-up and were excluded from analysis; complete follow-up was achieved in 269 (95.05%) of the patients. We enrolled these 269 consecutive patients (mean age, 56.13 ± 10.72 yr; 66.2% men) into either of 2 groups on the basis of procedural success or failure. The protocol for this retrospective, observational study was approved by our institutional review board.
Definitions
Chronic total occlusion was defined as vessel continuity completely interrupted by an atherosclerotic lesion in a native coronary artery, with a Thrombolysis In Myocardial Infarction (TIMI) flow grade of 0 or 1 for 3 months or longer; or as the presence of bridging collateral vessels.13 The duration of occlusion was estimated by clinical events such as myocardial infarction (MI) or the sudden onset or worsening of ischemic symptoms, or it was proved by the patients’ previous angiographic reports and the presence of bridging collateral vessels on angiograms. Technical success was defined as the ability to cross an occluded segment and successfully open the artery (restoration of a TIMI flow grade of 2 or 3) with a residual stenosis of less than 30% in all views.14,15
Multivessel disease was defined as stenosis of ≥70% in more than one major coronary artery. Lesions distal to 2 bends of >75° were considered to have moderate-to-severe tortuosity. Moderate-to-severe calcification was defined as readily apparent densities within the vascular wall at the site of the stenosis. The angiographic structure of the occlusion was defined as “tapered-stump” if the artery ended in a funnel shape. Intracoronary microchannels at the site of the occlusion were considered to be bridging collateral vessels that established the chronicity of the occlusion.16 Contralateral injection, performed in some cases, was defined as simultaneous dye injection to show the distal portion of the vessel after the occlusion site (filled via collateral vessels) and to estimate the length of the occlusion.17
Postprocedural MI was defined as an elevation of creatine kinase-MB mass to at least 3 times the upper limit of normal after the procedure (our laboratory's normal limit of creatine kinase-MB is 6.73 ng/mL for men and 3.77 ng/mL for women). In patients who had a postprocedural MI that was related to the target lesion, the development of new Q waves in the electrocardiographic leads indicated a Q-wave MI.18
The study endpoint was the occurrence of MACE during the follow-up period: cardiac death, nonfatal MI, target-lesion revascularization, or target-vessel revascularization (TVR). Target-lesion revascularization was defined either as repeat percutaneous or surgical revascularization for a lesion anywhere within the stent or within 5-mm borders proximal or distal to the stent. Target-vessel revascularization was defined as PCI or CABG for chest pain or positive noninvasive-test results (exercise stress test, stress echocardiogram, or radionuclide study showing reversible defects) for ischemia consequent to a lesion in the same epicardial vessel.
Evaluation Protocol
One independent reviewer retrospectively evaluated all angiograms and angioplasty films, and all reported data arose from that reviewer's decisions. A different independent reviewer reviewed the images from a randomly selected 15% of the patients. The level of agreement between the reviewers was 93.5%. In the evaluation of bridging collateral vessels and moderate-to-severe calcification, interobserver variability was 6.5% and 3.2%, respectively.
Interventional Procedure
Before PCI, all patients were given aspirin orally (325 mg), a clopidogrel loading dose (600 mg, at least 2 hr before), and weight-adjusted unfractionated heparin (80–100 U/kg) intravenously. The technical approach and procedural devices were chosen by the interventional cardiologists. The antegrade approach was routinely used, and, depending on procedural progress, different strategies and the use of stiffer wires were considered. Contralateral injection was performed in some patients.
In the successful-procedure group, clopidogrel (75 mg/d) was prescribed for 12 months to patients who received a drug-eluting stent (DES) and for at least 3 months to patients who received a bare-metal stent (BMS). The patients with a DES were discharged from the hospital with instructions to take 325 mg/d of aspirin for at least 3 months; the patients with a BMS were instructed to take that dose of aspirin for at least 1 month. Thereafter, 80 mg/d of aspirin was prescribed for an indefinite period after PCI.
Statistical Analysis
Results are presented as mean ± SD for numerical variables and as number and percentage for categorical variables. The Student t or Mann-Whitney U test was used to compare continuous variables, and the χ2 or Fisher exact test was used to compare categorical variables. For one-year MACE-free outcome, survival curves were estimated by means of the Kaplan-Meier method (the standard estimator of the survival function) and were compared between the 2 groups by means of the log-rank test.
Variables with a univariate P value <0.15 were candidates for inclusion in the multivariate analyses. We constructed a multivariate Cox proportional hazards model with a backward elimination method for identifying variables associated with one-year MACE-free survival outcome. Associations are expressed as hazard ratio (HR) with 95% confidence interval (CI). The overall fit of the final model was checked with use of Cox-Snell residuals, and checks were performed to identify departures from proportional-hazard assumption.
We established a multivariate backward logistic regression model for factors predicting procedural failure. Associations between the independent predictors and procedural failure in the final model are expressed as odds ratio (OR) with 95% CI. We used the area under the receiver operating characteristic curve to measure model discrimination and used the Hosmer-Lemeshow goodness-of-fit statistic to estimate model calibration (higher P values imply that the model better fits the observed data). P values ≤0.05 were considered statistically significant. We used SPSS software version 15.0 for Windows (IBM Corporation; Armonk, NY) for the statistical analyses.
Results
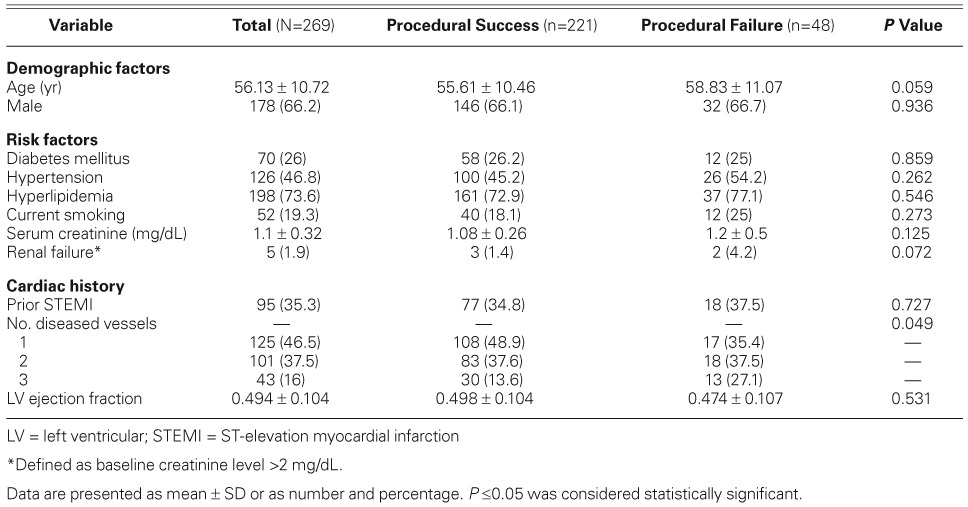
Table I shows the baseline demographic and clinical characteristics of the study population. Revascularization was successful in 221 of the 269 patients (82.2%). Almost half the patients had hypertension (46.8%), and 73.6% had hyperlipidemia. The only significant difference between the groups in baseline characteristics was the prevalence of multivessel disease, which was significantly higher in the procedural-failure group (64.6% vs 51.1%, P=0.049).
TABLE I.
Baseline Demographic and Clinical Characteristics of the Patients
Angiographic and Procedural Characteristics
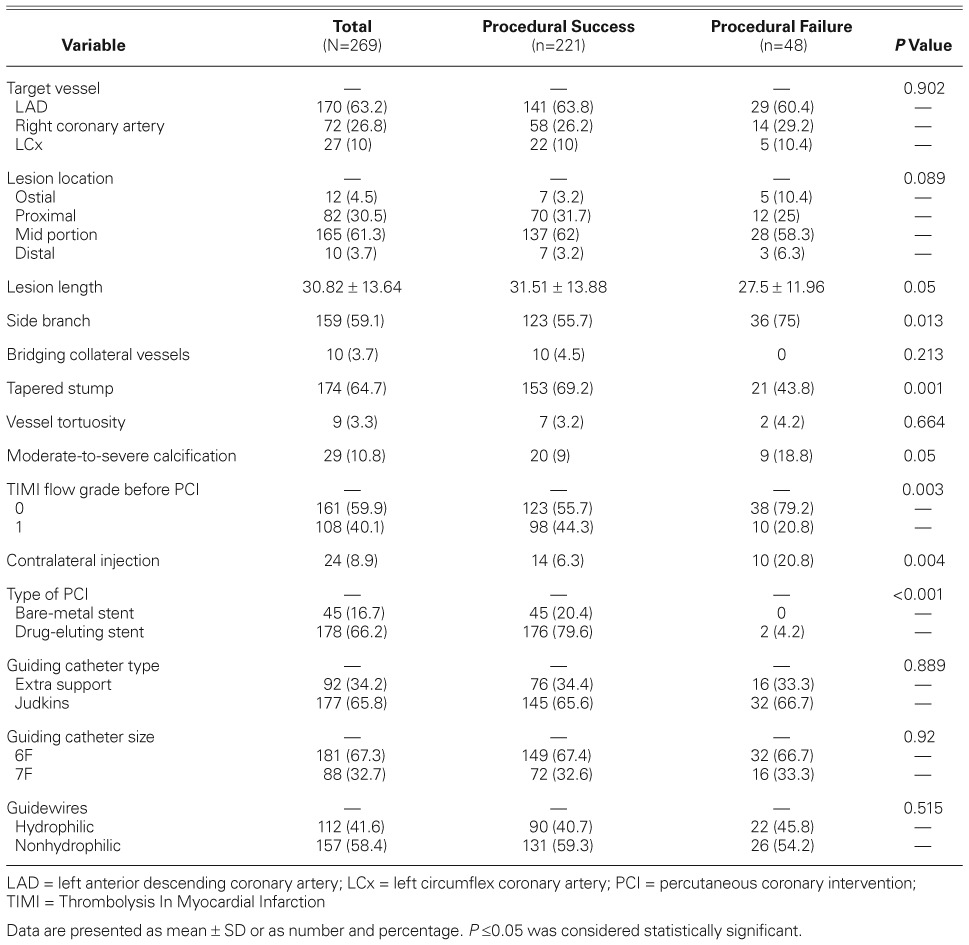
Table II shows the angiographic and procedural characteristics. In 63.2% of the patients, the left anterior descending coronary artery was the chronically occluded target vessel. The procedures performed on lesions with tapered stumps were significantly more successful than those on lesions that lacked that tapered structure. The presence of at least one side branch arising at the site of the occlusion, the finding of moderate-to-severe calcification, and the need for contralateral injection were significantly higher in the procedural-failure group. Most patients in the failure group presented with a TIMI flow grade of 0 before PCI (P=0.003). A DES was deployed in 178 patients (66.2%) and a BMS in 45 patients (16.7%).
TABLE II.
Angiographic and Procedural Characteristics
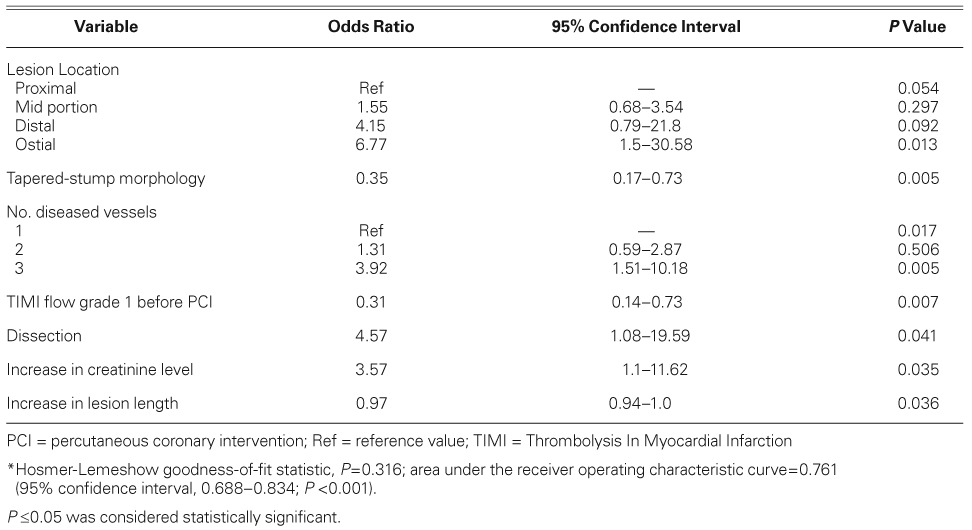
According to the multivariate analysis, independent predictors of technical failure were the location of the lesion, 3-vessel coronary artery disease, the absence of tapered-stump morphology, a TIMI flow grade of 0 before PCI, the occurrence of dissection, and an increase in serum creatinine level or lesion length. As Table III shows, PCI for ostial lesions was the most powerful predictor of technical failure (OR=6.77; 95% CI, 1.5–30.58; P=0.013). The area under the receiver operating characteristic curve was 0.761 (95% CI, 0.688–0.834; P <0.001), implying the model's ability to discriminate between failed and successful procedures.
TABLE III.
Multivariate Predictors of Technical Failure*
Procedural and In-Hospital Complications
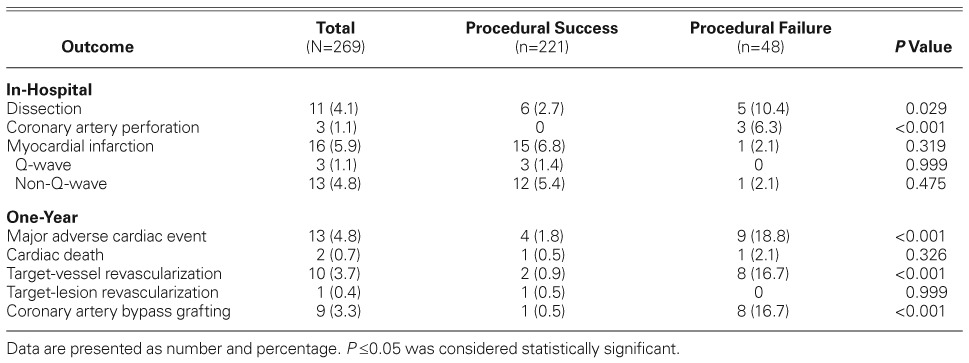
Technical success was achieved in 82.2% of the patients; inability to pass the guidewire was the reason for technical failure. Table IV shows the in-hospital and one-year complications. In 11 patients with coronary artery dissection, 2 had a non-Q-wave MI and one had a Q-wave MI. Mild or minimal pericardial effusion developed in 2 patients without progressing to cardiac tamponade. There were no relevant clinical sequelae in the remaining patients in whom coronary dissection or arterial perforation occurred. In 3 patients who developed postprocedural MI, new Q waves were detected in the electrocardiographic leads related to the target lesion. No emergent CABG was required and no deaths occurred during hospitalization. Except for dissection and perforation, which were significantly more frequent in the procedural-failure group, there was no significant difference between the 2 groups with respect to procedural and in-hospital complications.
TABLE IV.
In-Hospital and One-Year Clinical Outcomes
One-Year Occurrence of Major Adverse Cardiac Events
Complete follow-up was achieved in 95.05% of the patients (mean duration, 15.06 ± 3.15 mo). Table IV shows that one-year MACE occurred in 13 patients (4.8%), with a predominance of TVR (3.7%). The overall prevalence of MACE was significantly lower in the patients who underwent successful PCI (1.8% vs 18.8% in the failure group; P <0.001). One patient in the success group underwent TVR (PCI in the same vessel) and target-lesion revascularization (repeat PCI because of in-stent restenosis) during the follow-up period. Procedural failure was significantly associated with more frequent need for TVR and CABG during the follow-up period (Table IV). Figure 1 shows the Kaplan-Meier cumulative MACE-free and CABG-free survival estimates. Included in the multivariate model were all the variables that had a significant relationship with one-year MACE in the univariate analysis (P <0.15, results not shown)—side branches, presence of bridging collateral vessels, number of diseased vessels, vascular site of chronic occlusion, absence of tapered-stump structure, moderate-to-severe calcification, TIMI flow grade of 1 before PCI, hypertension, age, creatinine level, lesion length, and technical success. Only technical success was powerfully associated with a lower incidence of one-year MACE (HR=0.09; 95% CI, 0.03–0.30; P <0.001).
Fig. 1.
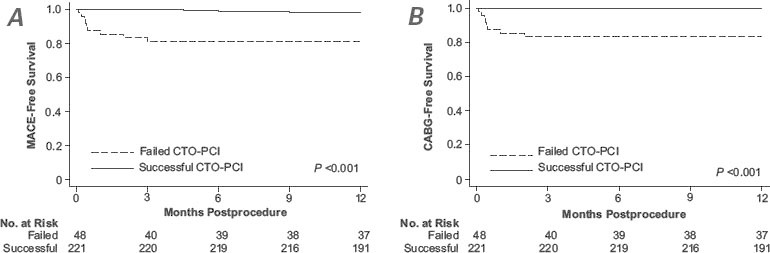
Kaplan-Meier cumulative A) MACE-free and B) CABG-free survival estimates in patients who underwent successful and failed percutaneous coronary intervention for chronic occlusion.
CABG = coronary artery bypass grafting; CTO = chronic total occlusion; MACE = major adverse coronary event; PCI = percutaneous coronary intervention
Discussion
The results of our study support PCI as an effective and safe therapeutic option in properly selected CTO patients because of the high success rate (82.2%) and the low prevalence of complications. Upon multivariate analysis, the most powerful predictors of technical failure were PCI for ostial lesions, the number of diseased vessels, and the occurrence of dissection during the procedure. Other independent predictors of technical failure were the absence of tapered-stump structure, a TIMI flow grade of 0 before PCI, and an increase in serum creatinine level or lesion length. One-year MACE occurred in 13 patients (4.8%), with a predominance of TVR (3.7%). Upon multivariate analysis, the only independent predictor of MACE was the technical failure of PCI.
Our technical success rate was within the range reported in several single-center studies (51%–85%).1,9–12,19 No in-hospital deaths occurred among the patients in our study, and no emergent CABG was necessary during their hospitalization. These results, which agree with those previously reported,1,8,11 imply that PCI for chronic occlusion is a safe procedure for the patients.
Because evaluating potential success is important before attempting PCI in chronically occluded lesions, investigators have designed various studies to identify influential factors.1,2,8,12,19,20 Despite the reported findings, debate continues in regard to the impact of different clinical and angiographic variables on technical success and long-term clinical outcome.3 Several angiographic factors, including the absence of tapered-stump structure,21–26 the presence of bridging collateral vessels,23 and the presence of a side branch at the occlusion site,23,24 have been reported as predictors of technical failure. Severe tortuosity and moderate-to-severe calcification have also been reported as predictors of technical failure.8,21,25–27 Still other investigators have concluded that multivessel disease and lesion lengths >15 mm predict technical failure.1,8,11,19,21 Our results confirm some of the aforementioned conclusions but not others. For instance, calcification, bridging collateral vessels, and side branches at the occlusion site—identified as negative predictors of success in previous studies—had no predictive value in our study. This incongruity might be explained by variation in definitions and durations of chronic occlusion in previous studies. In addition, some large studies did not include information about important variables such as angiographic structure.8,12,28
Our study is one of the few to evaluate predictors of one-year MACE in patients who have undergone PCI as treatment for CTO. In line with previous investigations, our results confirmed the importance of technical success as a predictor of MACE-free survival. Initially successful PCI was the only predictor of one-year MACE-free survival in a large, multicenter, observational study.1 In a retrospective study,2 multivessel disease was the most powerful predictor of 5-year MACE; other independent predictors were successful recanalization and lack of stent implantation.
Previous investigators have emphasized the predictive impact of lesion lengths >15 mm on technical success.1,11,19 Although lesion length had predictive value for technical failure in our study, its impact was less than in the aforementioned studies. This finding might be a consequence of improved devices, techniques, and operator experience, which decreases the negative impact of lesion length on technical success. Further studies are necessary for confirmation.
Limitations of the Study
The number of cases in our failure group was relatively small and was 3 times lower than the number in the success group, which can affect the power of our study and our findings. Because the reported success rates of PCI in CTO vary from 51% to 85%, such a problem has been observed in previous observational studies. However, in our study, the frequencies of most variables that were not significantly different between the 2 groups of patients were very close together (Tables I and II), and the results would not seem to change if the sample size were larger. A second limitation is that no predictor for death, MI, or CABG could be identified in this analysis. The present study's retrospective nature with observational analysis of outcome is another limitation. For instance, some advanced technical approaches and new devices were not available in our center at the time of the study. Finally, detailed data about postprocedural medication were not available in our registry.
Conclusion
In properly selected patients who have coronary CTO, we conclude that PCI can be an effective and safe therapeutic option, with a high success rate and low prevalence of complications. Nonetheless, inconsistencies persist in regard to predictors of procedural success and long-term outcome. This suggests that large, prospective, multicenter studies with accurate inclusionary criteria and long-term follow-up periods are necessary to clarify these predictive factors. When the predictors are identified conclusively, they might aid the selection of patients and lesions for PCI, and contribute to the development of new methods and technologies designed to improve the procedural success rate of PCI in patients who have CTO.
References
- 1.Olivari Z, Rubartelli P, Piscione F, Ettori F, Fontanelli A, Salemme L. Immediate results and one-year clinical outcome after percutaneous coronary interventions in chronic total occlusions: data from a multicenter, prospective, observational study (TOAST-GISE) J Am Coll Cardiol. 2003;41(10):1672–8. doi: 10.1016/S0735-1097(03)00312-7. [DOI] [PubMed] [Google Scholar]
- 2.Hoye A, van Domburg RT, Sonnenschein K, Serruys PW. Percutaneous coronary intervention for chronic total occlusions: the Thoraxcenter experience 1992–2002. Eur Heart J. 2005;26(24):2630–6. doi: 10.1093/eurheartj/ehi498. [DOI] [PubMed] [Google Scholar]
- 3.Joyal D, Afilalo J, Rinfret S. Effectiveness of recanalization of chronic total occlusions: a systematic review and meta-analysis. Am Heart J. 2010;160(1):179–87. doi: 10.1016/j.ahj.2010.04.015. [DOI] [PubMed] [Google Scholar]
- 4.Stone GW, Reifart NJ, Moussa I, Hoye A, Cox DA, Colombo A. Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: part II. Circulation. 2005;112(16):2530–7. doi: 10.1161/CIRCULATIONAHA.105.583716. [DOI] [PubMed] [Google Scholar]
- 5.Stone GW, Kandzari DE, Mehran R, Colombo A, Schwartz RS, Bailey S. Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: part I. Circulation. 2005;112(15):2364–72. doi: 10.1161/CIRCULATIONAHA.104.481283. [DOI] [PubMed] [Google Scholar]
- 6.Srinivas VS, Brooks MM, Detre KM, King SB, 3rd, Jacobs AK, Johnston J, Williams DO. Contemporary percutaneous coronary intervention versus balloon angioplasty for multivessel coronary artery disease: a comparison of the National Heart, Lung and Blood Institute Dynamic Registry and the Bypass Angioplasty Revascularization Investigation (BARI) study. Circulation. 2002;106(13):1627–33. doi: 10.1161/01.CIR.0000031570.27023.79. [DOI] [PubMed] [Google Scholar]
- 7.Christofferson RD, Lehmann KG, Martin GV, Every N, Caldwell JH, Kapadia SR. Effect of chronic total coronary occlusion on treatment strategy. Am J Cardiol. 2005;95(9):1088–91. doi: 10.1016/j.amjcard.2004.12.065. [DOI] [PubMed] [Google Scholar]
- 8.Rathore S, Matsuo H, Terashima M, Kinoshita Y, Kimura M, Tsuchikane E. Procedural and in-hospital outcomes after percutaneous coronary intervention for chronic total occlusions of coronary arteries 2002 to 2008: impact of novel guidewire techniques. JACC Cardiovasc Interv. 2009;2(6):489–97. doi: 10.1016/j.jcin.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 9.Mehran R, Claessen BE, Godino C, Dangas GD, Obunai K, Kanwal S. Long-term outcome of percutaneous coronary intervention for chronic total occlusions. JACC Cardiovasc Interv. 2011;4(9):952–61. doi: 10.1016/j.jcin.2011.03.021. [DOI] [PubMed] [Google Scholar]
- 10.Jones DA, Weerackody R, Rathod K, Behar J, Gallagher S, Knight CJ. Successful recanalization of chronic total occlusions is associated with improved long-term survival. JACC Cardiovasc Interv. 2012;5(4):380–8. doi: 10.1016/j.jcin.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 11.Noguchi T, Miyazaki M, Morii I, Daikoku S, Goto Y, Nonogi H. Percutaneous transluminal coronary angioplasty of chronic total occlusions. Determinants of primary success and long-term clinical outcome. Catheter Cardiovasc Interv. 2000;49(3):258–64. doi: 10.1002/(SICI)1522-726X(200003)49:3<258::AID-CCD7>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 12.Suero JA, Marso SP, Jones PG, Laster SB, Huber KC, Giorgi LV. Procedural outcomes and long-term survival among patients undergoing percutaneous coronary intervention of a chronic total occlusion in native coronary arteries: a 20-year experience. J Am Coll Cardiol. 2001;38(2):409–14. doi: 10.1016/S0735-1097(01)01349-3. [DOI] [PubMed] [Google Scholar]
- 13.The Thrombolysis in Myocardial Infarction (TIMI) trial. Phase I findings. TIMI Study Group. N Engl J Med. 1985;312(14):932–6. doi: 10.1056/NEJM198504043121437. [DOI] [PubMed] [Google Scholar]
- 14.Thompson CA, Jayne JE, Robb JF, Friedman BJ, Kaplan AV, Hettleman BD. Retrograde techniques and the impact of operator volume on percutaneous intervention for coronary chronic total occlusions: an early U.S. experience. JACC Cardiovasc Interv. 2009;2(9):834–42. doi: 10.1016/j.jcin.2009.05.022. [DOI] [PubMed] [Google Scholar]
- 15.Paul GA, Connelly K, Dick AJ, Strauss BH, Wright GA. Assessment of left ventricular function with cardiac MRI after percutaneous coronary intervention for chronic total occlusion [abstract] Heart. 2011;97(Suppl 1):A22–3. doi: 10.1136/heartjnl-2011-300198.31. [DOI] [Google Scholar]
- 16.Popma JJ. Coronary arteriography. In: Bonow RO, Mann DL, Zipes DP, Libby P, editors. Braunwald's heart disease: a textbook of cardiovascular medicine. 9th ed. Philadelphia: Elsevier Saunders; 2012. pp. 406–32. [DOI] [Google Scholar]
- 17.Tsuchikane E, Katoh O, Suzuki T, Nakamura S, Nguyen TN, Saito S. Chronic total occlusion. In: Nguyen TN, Colombo A, Hu D, Grines CL, Saito S, editors. Practical handbook of advanced interventional cardiology: tips and tricks. 3rd ed. Malden (MA): Blackwell Publishing, Inc.; 2008. p. 176. [Google Scholar]
- 18.Popma JJ, Bhatt DL. Percutaneous coronary intervention. In: Bonow RO, Mann DL, Zipes DP, Libby P, editors. Braunwald's heart disease: a textbook of cardiovascular medicine. 9th ed. Philadelphia: Elsevier Saunders; 2012. pp. 1270–89. [DOI] [Google Scholar]
- 19.Dong S, Smorgick Y, Nahir M, Lotan C, Mosseri M, Nassar H. Predictors for successful angioplasty of chronic totally occluded coronary arteries. J Interv Cardiol. 2005;18(1):1–7. doi: 10.1111/j.1540-8183.2005.00390.x. [DOI] [PubMed] [Google Scholar]
- 20.Piscione F, Galasso G, Maione AG, Pisani A, Golino P, Leosco D. Immediate and long-term outcome of recanalization of chronic total coronary occlusions. J Interv Cardiol. 2002;15(3):173–9. doi: 10.1111/j.1540-8183.2002.tb01052.x. [DOI] [PubMed] [Google Scholar]
- 21.Morino Y, Abe M, Morimoto T, Kimura T, Hayashi Y, Muramatsu T. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 2011;4(2):213–21. doi: 10.1016/j.jcin.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 22.Maiello L, Colombo A, Gianrossi R, Mutinelli MR, Bouzon R, Thomas J, Finci L. Coronary angioplasty of chronic occlusions: factors predictive of procedural success. Am Heart J. 1992;124(3):581–4. doi: 10.1016/0002-8703(92)90262-T. [DOI] [PubMed] [Google Scholar]
- 23.Tan KH, Sulke N, Taub NA, Watts E, Karani S, Sowton E. Determinants of success of coronary angioplasty in patients with a chronic total occlusion: a multiple logistic regression model to improve selection of patients. Br Heart J. 1993;70(2):126–31. doi: 10.1136/hrt.70.2.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ishizaka N, Issiki T, Saeki F, Ishizaka Y, Ikari Y, Abe J. Angiographic follow-up after successful percutaneous coronary angioplasty for chronic total coronary occlusion: experience in 110 consecutive patients. Am Heart J. 1994;127(1):8–12. doi: 10.1016/0002-8703(94)90503-7. [DOI] [PubMed] [Google Scholar]
- 25.Bufe A, Haltern G, Dinh W, Wolfertz J, Schleiting H, Guelker H. Recanalisation of coronary chronic total occlusions with new techniques including the retrograde approach via collaterals. Neth Heart J. 2011;19(4):162–7. doi: 10.1007/s12471-011-0091-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li CG, Liu XB, Ge L, Qian JY, Shen Y, Dai YX. Determinants of success percutaneous coronary intervention in patients with chronic total coronary artery occlusion [in Chinese] Zhonghua Xin Xue Guan Bing Za Zhi. 2011;39(1):30–4. [PubMed] [Google Scholar]
- 27.Garcia-Garcia HM, Brugaletta S, van Mieghem CA, Gonzalo N, Diletti R, Gomez-Lara J. CRosser As First choice for crossing Totally occluded coronary arteries (CRAFT Registry): focus on conventional angiography and computed tomography angiography predictors of success. EuroIntervention. 2011;7(4):480–6. doi: 10.4244/EIJV7I4A78. [DOI] [PubMed] [Google Scholar]
- 28.Bell MR, Berger PB, Bresnahan JF, Reeder GS, Bailey KR, Holmes DR., Jr Initial and long-term outcome of 354 patients after coronary balloon angioplasty of total coronary artery occlusions. Circulation. 1992;85(3):1003–11. doi: 10.1161/01.CIR.85.3.1003. [DOI] [PubMed] [Google Scholar]


