Abstract
Purpose
We examine overweight/obesity management in primary care in relation to body mass index (BMI), documentation of weight status, and comorbidities.
Methods
This analysis of baseline data from the Cholesterol Education and Research Trial included 2,330 overweight and obese adult primary care patients from southeastern New England. Data were obtained via a telephone interview and abstraction of subjects’ medical record. BMI (kg/m2) was calculated from measured height and weight. Management of overweight/obesity included advice to lose weight, physical activity recommendations, dietary recommendations, and referral for nutrition counseling.
Results
Documentation of weight status was more common with increasing BMI (13% of overweight patients, 39% of mildly obese, and 77% of moderately/severely obese). Documentation of overweight/obesity was associated with increased behavioral treatment; the biggest increase was seen for advice to lose weight (ORs were 7.2 for overweight patients, 3.3 for patients with mild obesity, and 4.0 for moderate/severe obesity). While weight-related comorbidities were associated with increased overweight/obesity management at all BMIs, the biggest increase in odds was for patients with moderate/severe obesity.
Conclusions
Documentation of weight management was more common among patients with documented overweight/obesity and with weight-related comorbidities. These insights may help in designing new interventions in primary care setting for overweight and obese patients.
Introduction
The two-thirds of U.S. adults who are overweight or obese(1) are at increased risk for hypertension, dyslipidemia, Type II diabetes, cardiovascular disease, osteoarthritis, sleep apnea, some cancers, depression, and reduced life expectancy.(2-6) Current practice guidelines recommend that adult patients in primary care be screened for overweight and obesity.(7, 8) Primary care physicians reach most segments of the population and their expertise is highly regarded by patients, placing them in a unique position to motivate and counsel overweight or obese patients about the health benefits of moderate weight loss, improved diet, and increased physical activity.(9) Yet despite this “epidemic of obesity”, there is mounting evidence that many primary care providers are not adequately addressing overweight/obesity.(10-20)
Many studies assessing the recognition and management of obesity in primary care have not differentiated levels of obesity.(15-19) Additionally, few studies included overweight patients(14, 15) yet there is strong clinical trial evidence that modest weight loss in this group can delay or prevent the development of diabetes, hypertension, and dyslipidemia.(21-23) Additionally, overweight patients with comorbidities have greater mortality risks than those with obesity without comorbid conditions.(2, 6) Given the increasing health consequences with increasing BMI(17) and the benefits of weight loss among overweight individuals, differentiating between overweight and classes of obesity is important to better understand overweight/obesity management in primary care and to better translate evidence-based guidelines into clinical practice. In this study, we examine two factors that may influence overweight/obesity management in the primary care setting: documentation of overweight/obesity and presence of weight-related comorbidities. Understanding current overweight/obesity management practices could inform future education efforts and interventions to promote successful treatment in the primary care setting.
Methods
This study uses baseline data from the Cholesterol Education and Research Trial (CEART), a randomized cluster quality improvement trial testing the effectiveness of translating the Adult Treatment Panel III guidelines into clinical practice. The Memorial Hospital of Rhode Island Institutional Review Board approved the study. Thirty representative non-academic primary care practices (15 Internal Medicine and 15 Family Practice; 15 group and 15 solo practices) were recruited from Rhode Island and Massachusetts. Patients eligible for CEART (aged 20 to 80 years, spoke English, and had at least once physician visit in the past two years) received letters signed by their physicians inviting them to participate in the study. A random sample of 20 to 120 patients per practice was selected from patients who provided informed consent. Participants completed a short computer-assisted telephone interview and research assistants abstracted medical records from May 25, 2004 through August 18, 2005. After exclusion of patients who were pregnant (n = 18), missing weight (n = 83) or height (n = 770), or underweight (BMI < 18.5 kg/m2; n = 41) or normal weight (18.5 kg/m2 BMI ≤ 25 kg/m2, n = 1017) the present sample included 2,330 overweight or obese primary care patients.
BMI was calculated from the most recent weight and height recorded in the medical record and patients were classified as overweight (25 kg/m2 BMI ≤ 30 kg/m2), mildly obese (30 kg/m2 BMI ≤ 35 kg/m2), or moderately/severely obese (35 kg/m2 ≤ BMI).(7) Because primary care physicians may record overweight even when the patient is clinically obese, we considered documentation of either overweight or obesity. Documentation included information abstracted from the patient’s problem list and/or any notation indicating the patient’s weight status (e.g., “patient is obese”). Research assistants reviewed medical records for advice to lose weight, physical activity and dietary recommendations, and referral for nutrition counseling within the previous two years. Evidence of physical activity or dietary recommendations included any notation of advice. Documentation of four common weight-related comorbidities (diabetes, lipid disorders, hypertension, and cardiovascular disease) required the diagnosis or documentation on the problem list and was not based solely upon medication usage, laboratory data, or blood pressure readings. Diabetes included both Type I and Type II diabetes but excluded gestational diabetes. During the telephone interview, patients reported their date of birth, gender, marital status, education, and smoking status. Patients who reported smoking at least one cigarette during the past month were considered smokers.
We compared the characteristics of patients and measures of overweight/obesity management across degrees of overweight/obesity. We then compared patterns of overweight/obesity management in relation to documentation of overweight/obesity and presence of weight-related comorbidities, within each group (overweight, mild obesity, and moderate/severe obesity). Next, we estimated odds ratios using generalized linear mixed models with a logit link function in order to adjust for the clustering of patients within medical practices.(24, 25) We evaluated each model for confounding by age, gender, smoking status, race/ethnicity, education, and marital status.(1, 10-12, 15-18) Potential confounders that changed the estimate of association by at least 10% were retained in each model. Models were fit separately for each measure of overweight/obesity management within each weight category. Variables included in each model are indicated in table footnotes. Analyses were conducted with SAS 9.1.3 for Windows (SAS Institute Inc., Cary, NC).
Results
Patients with higher BMIs were, on average, more likely to be female and less likely to be married or cohabitating (Table 1). Documentation of overweight/obesity was more common with increasing BMI. Overweight or obesity was documented in 13% of overweight patients’ charts, 39% of mildly obese patients’ charts, and 77% of moderately/severely obese patients’ charts (Table 1; p < 0.01 for linear trend across BMI categories). The prevalence of each comorbidity increased with increasing BMI, as did the proportion of patients with at least one of these comorbid conditions (Table 1). All four measures of overweight/obesity management increased with increasing degree of overweight/obesity (p < 0.01 for linear trend for each measure).
Table 1.
Characteristics of overweight or obese primary care patients
| Overweight (n = 1236) | Mild obesity (n = 661) | Moderate or severe obesity (n = 433) | |
|---|---|---|---|
|
| |||
| Female (%) | 51 | 54 | 66 |
|
| |||
| Age, years (mean (SE)) | 54.5 (0.8) | 53.9 (0.9) | 54.7 (0.9) |
|
| |||
| Marital status (%) | |||
| - Married/cohabitating | 74 | 72 | 62 |
| - Single | 11 | 13 | 16 |
| - Widowed/divorced/separated | 14 | 14 | 21 |
|
| |||
| Non-Hispanic White (%) | 94 | 94 | 93 |
|
| |||
| Education (%) | |||
| - High school or less | 33 | 34 | 39 |
| - Technical/junior/some college | 21 | 26 | 24 |
| - College graduate | 27 | 24 | 24 |
| - Post-grad/professional degree | 19 | 17 | 13 |
|
| |||
| Current smoker (%) | 13 | 16 | 15 |
|
| |||
| Overweight or obesity documented (%) | 13 | 39 | 77 |
|
| |||
| Comorbidities (%) | |||
| - Diabetes | 8 | 14 | 26 |
| - Lipid disorder | 61 | 63 | 68 |
| - Hypertension | 42 | 56 | 69 |
| - Cardiovascular disease | 10 | 11 | 15 |
|
| |||
| At least one comorbidity (%) | 71 | 78 | 88 |
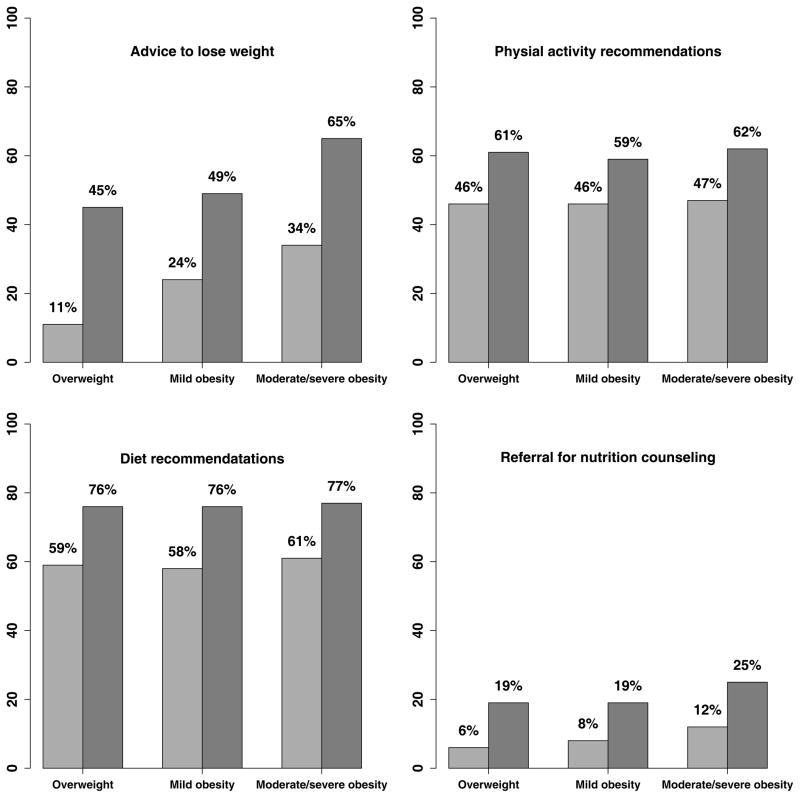
All four measures of overweight/obesity management were more common among those with higher BMIs (Figure 1). While physical activity and diet recommendations were common among all patients, for only patients with moderate/severe obesity that was documented by their physician was the prevalence of advice to lose weight more than 50%, and less than a quarter of overweight and obese patients received referrals for nutrition counseling (Figure 1). We found increased odds of overweight/obesity management in relation to documentation of overweight/obesity within each BMI category; odds ratios ranged from 1.9 to 7.2, depending on the measure of management and BMI category (Table 2). Documentation of overweight/obesity in the progress note or problem list had a much greater impact on advice to lose weight among overweight patients compared to those with mild or moderate/severe obesity (OR’s: 7.2 versus 3.3 and 4.0; Table 2).
Figure 1.
Management of overweight/obesity by documentation of overweight/obesity and degree of overweight/obesity
The light grey bars represent patients without documented overweight/obesity and the dark grey bars represent patients with documented overweight/obesity.
Table 2.
Management of overweight/obesity among primary care patients by documentation of overweight/obesity and degree of overweight/obesity (adjusted OR (95% CI))
| Documentation of overweight and/or obesity | Overweight | Mild obesity | Moderate or severe obesity | |
|---|---|---|---|---|
|
| ||||
| Advise to lose weight | Yes | 7.2 (4.8 – 10.6) * | 3.3 (2.3 – 4.6) | 4.0 (2.4 – 6.6) |
| No | (Referent) | (Referent) | (Referent) | |
|
| ||||
| Physical activity recommendations | Yes | 2.3 (1.5 – 3.4) | 1.9 (1.3 – 2.8) | 2.2 (1.3 – 3.7) |
| No | (Referent) | (Referent) | (Referent) | |
|
| ||||
| Diet recommendations | Yes | 2.9 (1.8 – 4.7) | 3.2 (2.1 – 4.9) | 2.5 (1.5 – 4.3) |
| No | (Referent) | (Referent) | (Referent) | |
|
| ||||
| Referral for nutrition counseling | Yes | 3.3 (2.1 – 5.4) † | 2.5 (1.6 – 4.0) | 2.7 (1.4 – 5.2) ‡ |
| No | (Referent) | (Referent) | (Referent) | |
Adjusted for sex
Adjusted for age
Adjusted for education
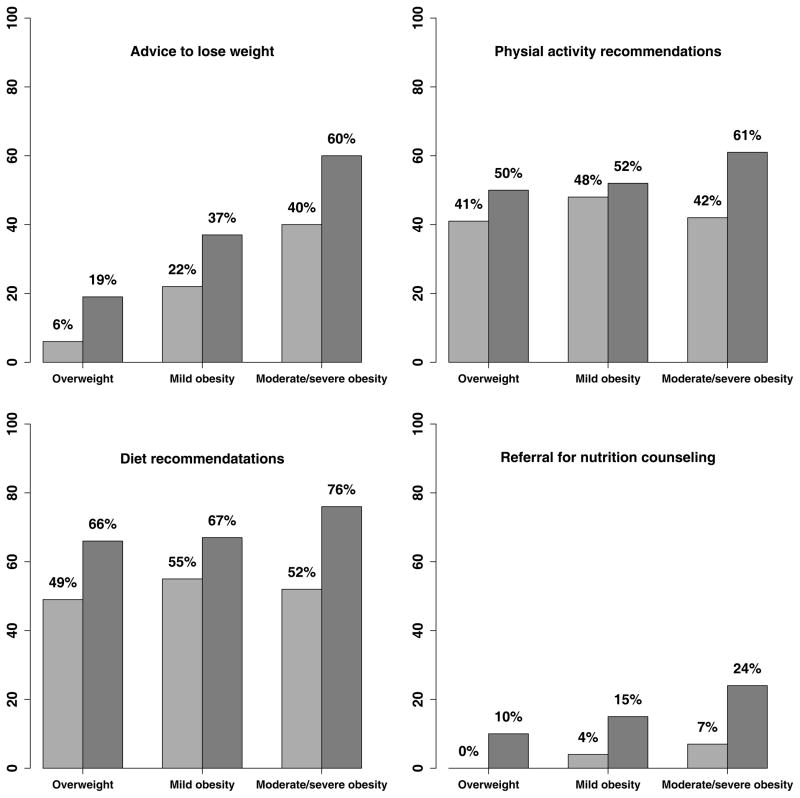
A similar pattern of overweight/obesity management practices was observed for overweight and obese primary care patients in relation to presence of weight-related comorbidities (Figure 2). We found increased odds of overweight/obesity management in relation to presence of weight-related comorbidities within each BMI category; odds ratios ranged from 1.2 to 4.8, depending on the measure of management and BMI category (Table 3). While weight-related comorbidities were associated with similar increase in odds of referrals for nutrition counseling for patients with differing levels of overweight/obesity, weight-related comorbidities had a greater impact on advice to lose weight, physical activity recommendations, and diet recommendations among patients with moderate/severe obesity (Table 3).
Figure 2.
Management of overweight/obesity by presence of at least one weight-related comorbidity and degree of overweight/obesity
The light grey bars represent patients without selected weight-related comorbidities (diabetes, lipid disorders, hypertension, or cardiovascular disease) and the dark grey bars represent patients with at least one of these weight-related comorbidities.
Table 3.
Management of overweight/obesity among primary care patients by presence of at least one weight-related comorbidity and degree of overweight/obesity (adjusted OR (95% CI))
| At least one weight-related comorbidity | Overweight | Mild obesity | Moderate or severe obesity | |
|---|---|---|---|---|
|
| ||||
| Advice to lose weight | Yes | 2.3 (1.5 – 3.4) * | 2.0 (1.4 – 3.0) | 3.4 (1.9 – 6.2)* |
| No | (Referent) | (Referent) | (Referent) | |
|
| ||||
| Physical activity recommendations | Yes | 1.5 (1.1 – 1.9) | 1.2 (0.8 – 1.7) | 2.9 (1.5 – 5.4)* |
| No | (Referent) | (Referent) | (Referent) | |
|
| ||||
| Dietary recommendations | Yes | 2.4 (1.8 – 3.2) | 2.0 (1.3 – 3.0) | 4.8 (2.4 – 9.6)*† |
| No | (Referent) | (Referent) | (Referent) | |
|
| ||||
| Referral for nutrition counseling | Yes | 3.4 (1.8 – 6.4)* | 3.1 (1.6 – 6.1) | 3.3 (1.4 – 7.6) |
| No | (Referent) | (Referent) | (Referent) | |
Adjusted for age
Adjusted for sex
Discussion
In this study of overweight and obese primary care patients, we found that documentation of weight status and behavioral interventions were more common among patients with increasing BMIs and that overweight/obesity management occurred more frequently among patients with documented weight status and those with weight-related comorbidities.
Our study confirms previous findings that overweight/obesity management occurs more frequently with increasing BMI(10, 12, 16-19) and the rates of physical activity and dietary recommendations in our population are similar to those found in previous studies.(13, 19, 26) In the present study, referral for nutrition counseling was the least common treatment strategy. Patients with moderate/severe obesity and weight-related comorbidities were the most likely to receive a referral for nutrition counseling (24%).
Behavioral interventions were more frequent among patients with documented overweight or obesity.(10, 11, 14, 16, 18, 27) Documentation of overweight/obesity was associated with similarly increased odds of physical activity and dietary recommendations and referrals for nutrition counseling across degrees of overweight/obesity. However, documentation of overweight/obesity was associated with higher increased odds of advice to lose weight among overweight patients compared to patients with mild or moderate/severe obesity. Because modest weight loss could shift overweight patients into a healthy weight category, perhaps physicians may be more likely to both document overweight and provide weight loss advice for the subset of overweight patients they believe may successfully achieve weight loss. Alternatively, some overweight patients may initiate conversations about weight with their physicians, leading to both documentation of their weight status and their physician recommending weight loss.
Although there are multiple potential explanations, this finding suggests that increasing documentation of overweight might lead to increased management activities. Although those with comorbid conditions may be more likely to receive advice to lose weight,(12, 15) studies have found that only about half of obese patients with comorbidities received advice to lose weight from their physician.(11, 16) We found that at all levels of overweight/obesity, those with comorbidities were more likely to have documented behavioral interventions for overweight/obesity..(10, 12, 15, 17) The increase in odds associated with presence of weight-related comorbidities was greatest for advice to lose weight and physical activity and dietary recommendations. Frequency of lifestyle advice in relation to weight-related comorbidities has not been investigated in such a way by previous studies.(14-16)
This study has several strengths and limitations. We differentiated between mild and moderate/severe obesity and included overweight individuals, resulting in greater understanding of overweight/obesity management. We were unable to differentiate between moderate and severe obesity due to limited numbers of patients in these weight categories. While BMI does not differentiate between lean and fat mass, BMI is highly correlated with waist circumference and is similarly related to total and abdominal fat(28) and is recommended for the classification of overweight and obesity in adults by national evidence-based clinical guidelines.(7, 8) The primary care providers in this study included general internists and family physicians from a spectrum of practice types. While many previous studies have assessed management of overweight and obesity from care provided at a single office visit(11, 29, 30) or patient self-reports of care,(12, 16-18) we reviewed two years of documented care, which better reflects the longitudinal nature of primary care. The design of the chart abstraction limits our ability to establish a temporal relationship between weight status and documentation and management of overweight/obesity. However, in this sample, on average, patients’ weight classification did not change over the course of twelve to eighteen months (unpublished data). Because this sample comes from southeastern New England and was predominantly non-Hispanic white, our findings may not be generalizable to primary care patients from other regions of the country or of other races/ethnicities.
A common limitation of data obtained from chart reviews is the potential discrepancy between conversations and documentation of these conversations. While documentation of weight status indicates recognition, a lack of documentation does not necessarily imply a lack of recognition. Therefore, it is possible that physicians discussed weight with their patients or made behavioral recommendations yet did not document these conversations in the patient’s chart. It is unknown whether this likely underestimate occurred differentially across BMI categories. Because practice guidelines suggest lifestyle modifications for the weight-related comorbidities studied, we are unable to determine whether behavioral recommendations were made to manage these health conditions or for weight control. Additionally, we were not able to assess whether conversations were initiated by physicians or patients. This is a problem common to many studies exploring the management of overweight/obesity in the primary care(14, 26) and there is evidence that both patients and clinicians initiate conversations about weight control.(20, 31)
Practice guidelines(8) recommend more intensive counseling than may be feasible in the context of a primary care visit. Reported challenges in effectively treating obesity in the primary care setting include lack of time, inadequate training on how to counsel patients, lack of insurance reimbursement, patient noncompliance, inadequate teaching materials, and low confidence.(17, 27, 32-35) While some physicians may feel that patients would not want to discuss their weight, many overweight and obese patients feel that their excess weight is unhealthy and would feel comfortable discussing weight with their physician.(17, 19, 30)
Because primary care providers’ advice can have an impact on patients’ behavior(12, 18, 26) and on patients’ confidence and motivation to change their behavior,(30) there is need to devise approaches that may help primary care clinicians balance visit constraints and the need for intensive lifestyle counseling to treat overweight and obesity in their patients. Electronic medical records (EMRs) offer the potential for the automatic calculation of BMI at point-of-service, which has been found to increase documentation of weight status and treatment in obese patients’ charts.(36) Websites can provide patients with tailored and interactive health information.(37) Some research has found patients to have positive experiences and attitudes with electronic health records and electronic communication with their providers about their care.(38) Group medical visits (GMVs) facilitated by physicians and other primary care professionals may provide a venue for increased patient education and understanding about their health. Newly implemented group medical visit programs have had positive responses from patients.(39, 40) However, many team-focused approaches may require reformed payment approaches to primary care.(41, 42)
In our study, documentation of weight management was more common for patients with documented overweight/obesity and among patients with weight-related comorbidities. Advice to lose weight was documented for a minority of overweight and mildly obese patients, yet these patients may have the greatest chance of obtaining a healthy weight. Triggers or office system approaches may be helpful in the management of overweight/obesity in the primary care setting. Research is needed to explore strategies to help primary care physicians balance time constraints and competing demands to provide the more intensive behavioral interventions needed to combat the obesity epidemic.
Acknowledgments
Data collection was supported by grant 1 R01 HL070804-01: Translating ATPIII Cholesterol Management Guidelines into Primary Care Practice (PI: Charles Eaton). We would like to thank the participating practices and the research assistants who conducted the medical record abstractions.
Footnotes
Conflicts of interest:
The authors have no conflicts of interest. Dr. Eaton is a member of the National Committee for Quality Assurance’s (NCQA’s) Adult Obesity panel.
References
- 1.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the united states, 1999–2004. JAMA. 2006 Apr 5;295(13):1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Pi-Sunyer FX. Medical hazards of obesity. Ann Intern Med. 1993;119(7 Pt 2):655–60. doi: 10.7326/0003-4819-119-7_part_2-199310011-00006. [DOI] [PubMed] [Google Scholar]
- 3.Hu FB, Manson JE, Stampfer MJ, Colditz G, Liu S, Solomon CG, Willett WC. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med. 2001;345(11):790–7. doi: 10.1056/NEJMoa010492. [DOI] [PubMed] [Google Scholar]
- 4.Eckel RH. Obesity and heart disease: A statement for healthcare professionals from the nutrition committee, american heart association. Circulation. 1997;96(9):3248–50. doi: 10.1161/01.cir.96.9.3248. [DOI] [PubMed] [Google Scholar]
- 5.Onyike CU, Crum RM, Lee HB, Lyketsos CG, Eaton WW. Is obesity associated with major depression? results from the third national health and nutrition examination survey. Am J Epidemiol. 2003;158(12):1139–47. doi: 10.1093/aje/kwg275. [DOI] [PubMed] [Google Scholar]
- 6.Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A, Bonneux L. Obesity in adulthood and its consequences for life expectancy: A life-table analysis. Ann Intern Med. 2003;138(1):24–32. doi: 10.7326/0003-4819-138-1-200301070-00008. [DOI] [PubMed] [Google Scholar]
- 7.National Institutes of Health. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. Baton Rouge, LA: North American Association for the Study of Obesity; 1998. p. 51. Report No.: 6 Suppl 2. [Google Scholar]
- 8.U S. Preventive Services Task Force. Screening for obesity in adults: Recommendations and rationale. Ann Intern Med. 2003;139(11):930–2. doi: 10.7326/0003-4819-139-11-200312020-00012. [DOI] [PubMed] [Google Scholar]
- 9.Hiddink GJ, Hautvast JG, van Woerkum CM, Fieren CJ, Van’t Hof MA. Consumers’ expectations about nutrition guidance: The importance of primary care physicians. Am J Clin Nutr. 1997;65(6 Suppl):1974S–9S. doi: 10.1093/ajcn/65.6.1974S. [DOI] [PubMed] [Google Scholar]
- 10.Simkin-Silverman LR, Gleason KA, King WC, Weissfeld LA, Buhari A, Boraz MA, Wing RR. Predictors of weight control advice in primary care practices: Patient health and psychosocial characteristics. Prev Med. 2005;40(1):71–82. doi: 10.1016/j.ypmed.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 11.Stafford RS, Farhat JH, Misra B, Schoenfeld DA. National patterns of physician activities related to obesity management. Arch Fam Med. 2000;9(7):631–8. doi: 10.1001/archfami.9.7.631. [DOI] [PubMed] [Google Scholar]
- 12.Galuska DA, Will JC, Serdula MK, Ford ES. Are health care professionals advising obese patients to lose weight? JAMA. 1999;282(16):1576–8. doi: 10.1001/jama.282.16.1576. [DOI] [PubMed] [Google Scholar]
- 13.Wadden TA, Anderson DA, Foster GD, Bennett A, Steinberg C, Sarwer DB. Obese women’s perceptions of their physicians’ weight management attitudes and practices. Arch Fam Med. 2000;9(9):854–60. doi: 10.1001/archfami.9.9.854. [DOI] [PubMed] [Google Scholar]
- 14.Bardia A, Holtan SG, Slezak JM, Thompson WG. Diagnosis of obesity by primary care physicians and impact on obesity management. Mayo Clin Proc. 2007;82(8):927–32. doi: 10.4065/82.8.927. [DOI] [PubMed] [Google Scholar]
- 15.Jackson JE, Doescher MP, Saver BG, Hart LG. Trends in professional advice to lose weight among obese adults, 1994 to 2000. Journal of General Internal Medicine. 2005;20(9):814–8. doi: 10.1111/j.1525-1497.2005.0172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sciamanna CN, Tate DF, Lang W, Wing RR. Who reports receiving advice to lose weight? results from a multistate survey. Archives of Internal Medicine. 2000;160(15):2334–9. doi: 10.1001/archinte.160.15.2334. [DOI] [PubMed] [Google Scholar]
- 17.Potter MB, Vu JD, Croughan-Minihane M. Weight management: What patients want from their primary care physicians. J Fam Pract. 2001;50(6):513–8. [PubMed] [Google Scholar]
- 18.Loureiro ML, Nayga RM. Obesity, weight loss, and physician’s advice. Social Science & Medicine. 2006;62(10):2458–68. doi: 10.1016/j.socscimed.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 19.Davis NJ, Emerenini A, Wylie-Rosett J. Obesity management: Physician practice patterns and patient preference. The Diabetes Educator. 2006;32(4):557–61. doi: 10.1177/0145721706290437. [DOI] [PubMed] [Google Scholar]
- 20.Flocke SA, Clark A, Schlessman K, Pomiecko G. Exercise, diet, and weight loss advice in the family medicine outpatient setting. Fam Med. 2005;37(6):415–21. [PubMed] [Google Scholar]
- 21.Stevens VJ, Obarzanek E, Cook NR, Lee I, Appel LJ, West DS, Mias NC, Mattfeldt-Beman M, Belden L, Bragg C, Millstone M, Raczynski J, Brewer A, Singh B, Cohen J for the Trials of Hypertension Prevention Research Group. Long-term weight loss and changes in blood pressure: Results of the trials of hypertension prevention, phase II. Ann Intern Med. 2001;134(1):1–11. doi: 10.7326/0003-4819-134-1-200101020-00007. [DOI] [PubMed] [Google Scholar]
- 22.Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, Stevens VJ, Vollmer WM, Lin P, Svetkey LP, Young DR Writing Group of the PREMIER Collaborative Research Group. Effects of comprehensive lifestyle modification on blood pressure control: Main results of the PREMIER clinical trial. JAMA. 2003;289(16):2083–93. doi: 10.1001/jama.289.16.2083. [DOI] [PubMed] [Google Scholar]
- 23.Knowler WC, Barett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murray DM, Varnell SP, Biltstein JL. Design and analysis of group-randomized trials: A review of recent methodological developments. American Journal of Public Health. 2004;94(3):423–32. doi: 10.2105/ajph.94.3.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parker DR, Evangelou E, Eaton CB. Intraclass correlation coefficients for cluster randomized trials in primary care: The cholesterol education and research trial (CEART) Contemporary Clinical Trials. 2005;26(2):260. doi: 10.1016/j.cct.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 26.Taira DA, Safran DG, Seto TB, Rogers WH, Tarlov AR. The relationship between patient income and physician discussion of health risk behaviors. JAMA. 1997;278(17):1412–7. [PubMed] [Google Scholar]
- 27.Eaton CB, Goodwin MA, Stange KS. Direct observation of nutrition counseling in community family practice. Am J Prev Med. 2002;23(3):174–9. doi: 10.1016/s0749-3797(02)00494-4. [DOI] [PubMed] [Google Scholar]
- 28.Janssen I, Heymsfield SB, Allison DB, Kotler DP, Ross R. Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal, subcutaneous, and visceral fat. Am J Clin Nutr. 2002;75:683–8. doi: 10.1093/ajcn/75.4.683. [DOI] [PubMed] [Google Scholar]
- 29.Mellen PB, Palla SL, Goff DC, Bonds DE. Prevalence of nutrition and exercise counseling for patients with hypertension, united states, 1999 to 2000. JGIM. 2004;19:917–24. doi: 10.1111/j.1525-1497.2004.30355.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Greiner KA, Born W, Hall S, Hou Q, Kimminau KS, Ahluwalia JS. Discussing weight with obese primary care patients: Physician and patient perspectives. J Gen Intern Med. 2008;23(5):581–7. doi: 10.1007/s11606-008-0553-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pollak KI, Ostbye T, Alexander SC, Gradison M, Bastian LA, Brouwer Namenek, Rebecca J, Lyna P. Empathy goes a long way in weight loss discussions. J Fam Pract. 2007;56(12):1031–6. [PubMed] [Google Scholar]
- 32.Hiddink GJ, Hautvast JG, van Woerkum CM, Fieren CJ, van’t Hof MA. Nutrition guidance by primary-care physicians: Perceived barriers and low involvement. Eur J Clin Nutr. 1995;49(11):842–51. [PubMed] [Google Scholar]
- 33.Kushner RF. Barriers to providing nutrition counseling by physicians: A survey of primary care practitioners. Prev Med. 1995;24(6):546–52. doi: 10.1006/pmed.1995.1087. [DOI] [PubMed] [Google Scholar]
- 34.Park ER, Wolfe TJ, Gokhale M, Winickoff JP, Rigotti NA. Perceived preparedness to provide preventive counseling: Reports of graduating primary care residents at academic health centers. J Gen Intern Med. 2005;20:386–91. doi: 10.1111/j.1525-1497.2005.0024.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Foster GD, Wadden TA, Makris AP, Davidson D, Sanderson RS, Allison DB, Kessler A. Primary care physicians’ attitudes about obesity and its treatment. Obes Res. 2003;11(10):1168–77. doi: 10.1038/oby.2003.161. [DOI] [PubMed] [Google Scholar]
- 36.Bordowitz R, Morland K, Reich D. The use of an electronic medical record to improve documentation and treatment of obesity. Fam Med. 2007;39(4):274–9. [PubMed] [Google Scholar]
- 37.Woolf SH, Krist AH, Johnson RE, Wilson DB, Rothemich SF, Norman GJ, Devers KJ. A practice-sponsored web site to help patients pursue healthy behaviors: An ACORN study. Ann Fam Med. 2006;4(2):148–52. doi: 10.1370/afm.522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hassol A, Walker JM, Kidder D, Rokita K, Young D, Pierdon S, Deitz D, Kuck S, Ortiz E. Patient experiences and attitudes about access to a patient electronic health care record and linked web messaging. J Am Med Inform Assoc. 2004;11(6):505–13. doi: 10.1197/jamia.M1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barud S, Marcy T, Armor B, Chonlahan J, Beach P. Development and implementation of group medical visits at a family medicine center. Am J Health-Syst Pharm. 2006;63:1448–52. doi: 10.2146/ajhp050266. [DOI] [PubMed] [Google Scholar]
- 40.Miller D, Zantop V, Hammer H, Faust S, Grumbach K. Group medical visits for low-income women with chronic disease: A feasability study. Journal of Women’s Health. 2004;13(2):217–25. doi: 10.1089/154099904322966209. [DOI] [PubMed] [Google Scholar]
- 41.Bodenheimer T. Transforming practice. N Engl J Med. 2008;359(20):2086–9. doi: 10.1056/NEJMp0805631. [DOI] [PubMed] [Google Scholar]
- 42.Fiscella K, Epstein RM. So much to do, so little time: Care for the socially disadvantaged and the 15-minute visit. Arch Internal Med. 2008;168(17):1843–52. doi: 10.1001/archinte.168.17.1843. [DOI] [PMC free article] [PubMed] [Google Scholar]