Abstract
Background: Cognitive impairment is among the most debilitating outcomes of multiple sclerosis (MS). Although several neuropsychological tests and self-report cognitive measures have been used to assess cognitive impairment, they may not be sensitive to change over time, or may not be feasible to administer in a clinical setting. The purpose of this study was to assess the reliability and validity of the 8-item PROMIS Cognitive Abilities and Cognitive Concerns Scales in a large community-based sample of people with MS. The PROMIS Cognitive Abilities and Cognitive Concerns Scales derive from the National Institutes of Health–funded Patient Reported Outcomes Measurement Information System (PROMIS), an item repository that capitalizes on recent psychometric advances to produce short, psychometrically sound health measures.
Methods: Mailed survey data were collected from 322 individuals recruited from two National Multiple Sclerosis Society chapters in a southwestern state.
Results: Both cognitive scales demonstrated high internal consistency reliability and were moderately correlated with self-reported depressive symptoms, self-efficacy, barriers to health promotion, health, and functional status (all correlation coefficients >0.35). In hierarchical regression analysis, the PROMIS Cognitive Concerns score added significant unique variance to the prediction of MS Incapacity Status after controlling for self-reported depressive symptoms, exercise, spiritual growth, and global health. Those who were unemployed owing to their disabilities had significantly lower PROMIS Cognitive Abilities scores and higher Cognitive Concerns scores than those who were working or those who were retired or not working for other reasons.
Conclusions: The PROMIS Cognitive Abilities and Cognitive Concerns Scales are short, psychometrically sound measures that assess an important dimension of functioning and health for people with MS.
Cognitive impairment is a major source of concern for people with multiple sclerosis (MS); its impact on major areas of life functioning, including employment, can be profound.1–7 Cognitive impairment has been observed early in the MS trajectory, making timely clinical assessment key to effective disease management. However, underdiagnosis is a problem,8 and clinicians need more effective methods to screen quickly for cognitive impairment and monitor cognitive functioning over time.
Previous research has found a relationship between cognitive functioning and other constructs such as depression,5,9–11 social participation,1,12 and coping11 among those with MS. In particular, Arnett and colleagues13 reported that the relationship between cognitive impairment and depression was higher among those who were not using active coping strategies. To the extent that health-promotion activities might be considered an active coping mechanism for people with MS, we might expect a positive relationship between frequency of reported health-promotion behaviors and cognitive abilities, and a negative relationship with cognitive concerns. Perceived barriers to health-promoting behaviors might in turn relate positively to cognitive concerns, but negatively to cognitive abilities. Because people with MS have indicated that cognitive limitations made them feel less competent and less confident when performing tasks,4 the construct of self-efficacy might also be hypothesized to relate in a positive direction to cognitive abilities and in a negative direction to cognitive concerns. Finally, cognitive abilities might be expected to relate positively to global perceptions of health status, while perceived health status might relate negatively to cognitive concerns.
Both neuropsychological tests and self-report measures have been used to quantify the degree of cognitive impairment experienced by people with MS.1,8 While neurocognitive measures are considered the most precise way of diagnosing impairment, self-report measures add key information about the impact of cognitive functioning on the individual’s daily life. Some measures, designed primarily for research purposes, may be less applicable to clinical situations and have not been shown to be sensitive to change over time following exposure to interventions designed to build cognitive skills. Moreover, many of these studies have been conducted in small samples recruited from one clinical setting.8,14
In an earlier study, we observed that the short forms of the PROMIS Cognitive Abilities and Cognitive Concerns Scales demonstrated good internal consistency reliability and were sensitive to change following a cognitive skills–building intervention in a small sample of 29 individuals with MS.15 These measures were derived from the Patient Reported Outcomes Measurement Information System (PROMIS), an initiative of the National Institutes of Health (NIH) designed to provide an item repository of commonly assessed physical and mental functioning outcomes.16
The aim of the current study was to examine the reliability and validity of the PROMIS cognitive scales in a larger community-based sample of people with MS, all of whom had been diagnosed more than 15 years earlier. The specific research questions were as follows:
What is the reliability of the PROMIS cognitive scales in a large community-based sample of individuals with MS?
What is the evidence for construct and criterion validity of the PROMIS cognitive scales as measures of perceived cognitive functioning in people with MS?
Methods
Data-Collection Procedures
The data for these analyses are from the 16th year of data collection in an ongoing longitudinal study of people with MS recruited for a study of health-promoting behaviors. Following receipt of institutional review board approval from the authors’ university, the sample was originally recruited from a large mailing to the members of two National Multiple Sclerosis Society chapters in a southwestern state (Texas). Some of those participating in year 16 mailings have since moved to 23 other states, and the sample is now more diverse in location even though a majority still live in Texas. Recruitment procedures for the original sample are documented elsewhere.17,18
The mailing to individuals in the 2012 spring cohort of the longitudinal study (N = 375) included a letter introducing the survey, which was also enclosed, and a postage-paid return envelope. Completed surveys were checked for omissions, and a letter with any missing responses was sent back to the respondents. This helped control the amount of missing information. Respondents were thanked for their participation, and a small gift of $30 was offered for their time.
Instruments
The PROMIS version 1.0 short-form subscales of Cognitive Abilities and Cognitive Concerns each contain 8 items. The Cognitive Abilities items target positive self-assessments of cognitive functioning such as “My memory has been as good as usual” and “I have been able to concentrate.” The Cognitive Concerns items are worded negatively and express concerns in the same areas. Two examples are “My thinking has been slow” and “I have had trouble shifting back and forth between different activities that require thinking.” Items on both subscales use a 5-point rating from “not at all” to “very much.” Items are summed to create a total score for each subscale. These relatively short scales were derived from an intensive item analysis using Item Response Theory and qualitative analysis to produce short but reliable measures.16 In the previous study,15 Cronbach α coefficients of 0.94 were reported for both scales. The test-retest correlation coefficients over a 2-month period were 0.83 for Cognitive Concerns and 0.80 for Cognitive Abilities.
The 16-item Incapacity Status Scale (ISS)19 measures functional limitations related to MS in the areas of personal activity and care, such as mobility, bowel and bladder function, sensory or cognitive impairments, emotional distress, bathing, dressing, and feeding. The predominantly physical functioning items were endorsed by the International Federation of Multiple Sclerosis Societies for use in MS research, and Kurtzke19 has presented data to support the scale’s validity. Items are rated on a 5-point scale, with higher scores indicating greater inability to perform activities. Total scores can range from 0 to 64. The Cronbach α coefficient for the ISS in this study was 0.90.
The Center for Epidemiological Studies Depression Scale–10 (CESD-10) was used to measure depressive symptoms.20 Respondents rated how frequently they have experienced ten depressive symptoms, each on a 4-point scale. The CESD-10 has demonstrated good reliability and validity with various populations, including people with chronic and disabling conditions.21,22 For this study, the Cronbach α coefficient of the CESD-10 was 0.85.
Health-promoting behavior was measured by the Health-Promoting Lifestyle Profile II (HPLP-II).23 Self-reported frequency of behavior on the 52-item HPLP-II yields scores on six subscales (Physical Activity, Health Responsibility, Spiritual Growth, Interpersonal Relations, Nutrition, and Stress Management). Reliability and validity of the HPLP-II have been supported in multiple studies.24,25 For this study, the Cronbach α coefficient for HPLP-II subscales ranged from 0.81 to 0.90.
The Global Health Self-Rating is a single question that asks for an overall health rating “at the present time.” The four response categories range from excellent (4) to poor (1). The developers have demonstrated its reliability and validity in previous research.26
The Barriers to Health Promoting Activities scale for people who are disabled27 is designed to address intrapersonal (eg, not interested), interpersonal (eg, difficulty with communication), and environmental barriers (eg, bad weather). It includes 18 items rated on a 4-point scale (from never to routinely). Higher total scores indicate greater perceived barriers. Its reliability and validity have been documented in previous research.25 The Cronbach α reliability coefficient was 0.88 in this study.
The Sherer et al.28 measure of General Self-Efficacy was used as a measure of general self-confidence to affect outcomes in various situations. Respondents rated 17 items on a 5-point scale from “disagree strongly” to “agree strongly,” with a choice of “neither agree nor disagree” offered. Those responses were summed to create a general self-efficacy score. Higher General Self-Efficacy scores indicate greater self-confidence in one’s abilities. Sherer et al. reported a Cronbach α coefficient of 0.86.28 Construct validity is evidenced by the confirmation of predicted correlations with other psychological constructs, as well as success in vocational, educational, and military settings. Previous studies by Stuifbergen and Becker29 and Stuifbergen30 reported Cronbach α coefficients of 0.87 and 0.86, respectively, and moderate correlation coefficients with the HPLP-II. The Cronbach α reliability coefficient in this study was 0.90.
Data-Analysis Plan
All analyses were performed using IBM SPSS Statistics, version 19. Cronbach α coefficients were computed to assess internal consistency reliability (Research Question 1). Descriptive statistics were computed to profile the sample and to provide means and standard deviations for all major study variables.
Bivariate correlation analysis was performed to explore the relationships between PROMIS Cognitive Abilities and PROMIS Cognitive Concerns Scales and other health-related measures. To further understand the unique contribution of PROMIS scores to the prediction of functional impairment, a hierarchical regression was performed to determine how much variance in the prediction of Incapacity Status was explained by PROMIS Cognitive Concerns scores after taking into account other health measures. The advantage of hierarchical regression analysis is that it allows researchers to examine the change in R2 when key variables are added to a model, once the effects of other related variables have been held constant. Before conducting multiple regression analysis, multiple regression assumptions such as multicollinearity and outliers were checked. To avoid problems with issues of multicollinearity and suppression,31 only one of the PROMIS scales (Cognitive Concerns) and two subscales of the HPLP-II were chosen as predictors. Thus, the predictors used in the first step of the regression analysis were restricted to the 1-item Global Health Self-Rating, the CESD-10 measure of depressive symptoms, and two subscales of the HPLP-II: Physical Activity and Spiritual Growth (representing the physical and emotional aspects of health promotion most highly correlated with the ISS). The PROMIS Cognitive Concerns Scale was then entered on the second step of the analysis to predict Incapacity Status scores. The R2 for change was examined to determine whether there was a significant change in the amount of variance accounted for in the model when the PROMIS Cognitive Concerns Scale was added.
To assess criterion validity using known groups, the sample was divided into three groups: those employed full time or part time (n = 62), those who indicated that they were unemployed owing to their disability (n = 100), and those unemployed for other reasons, primarily retirement (n = 160). One-way analysis of variance (ANOVA) with post hoc analysis was then performed to determine whether those who reported being unemployed owing to disability had significantly different PROMIS scores than the other two groups (at P < .05).
Results
The data were entered into SPSS for the 322 completed surveys, which represented an 86% response rate. A sample of 17% of the single-entered cases were double-checked against the actual survey responses by research staff not involved in the initial data entry. The error rate was less than 0.5%. Almost all respondents answered all the items that they were asked. When a couple of items were missed on a scale, mean substitution was used. If a participant missed more than 15% of items for a scale, however, the participant’s responses were deleted.
Sample Description
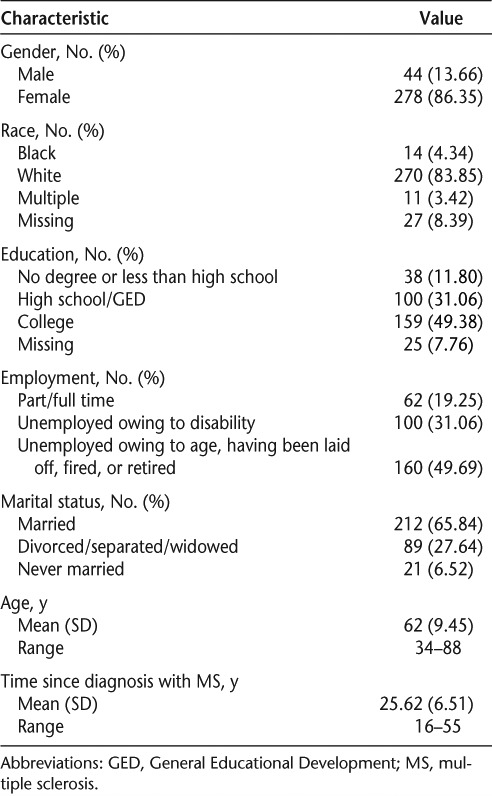
As shown in Table 1, participants’ ages ranged from 34 to 88 years, with an average age of 62 (SD 9.45). The average time since diagnosis was 25.62 years (SD 6.51), and 72% had taken at least two courses of steroids. The sample was predominantly married non-Hispanic white females. About half of them had a college degree. Only 19% were employed for pay (either full time or part time), and 31% (n = 100) reported being unemployed owing to their disability. The average quality of life rating on a 10-point scale (1 = very poor; 10 = very good) was 7.25 (SD 2.14). Forty percent rated their health as fair or poor.
Table 1.
Study sample background characteristics (N = 322)
Descriptive Information About the PROMIS Scales
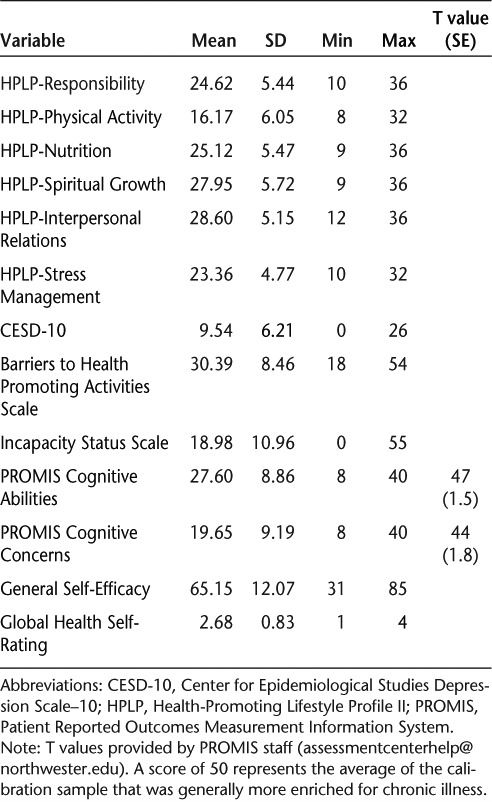
Means, standard deviations, and score ranges for all scale scores are shown in Table 2. Corresponding T scores are shown for the PROMIS Cognitive Abilities and Cognitive Concerns average scores. The calibration sample is described by the PROMIS assessment center as “generally enriched for chronic illness.” The T scores for this MS sample are slightly below the T score average (44 and 47 for Cognitive Concerns and Cognitive Abilities, respectively).
Table 2.
Descriptive statistics for PROMIS cognitive scales and other health-related measures (N = 322)
Internal Consistency Reliability
The PROMIS Cognitive Abilities and Cognitive Concerns Scales demonstrated high internal consistency reliability, with Cronbach α coefficients of 0.97 for both.
Construct Validation
Correlations with Related Construct
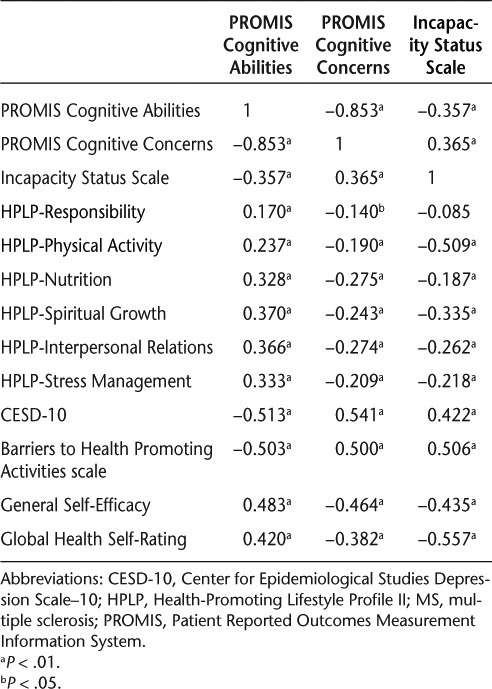
The PROMIS scales were strongly correlated with each other (r = −0.85) and moderately correlated with a number of health-related measures (Table 3). As expected, both cognitive scales were moderately to highly correlated in opposite directions with the CESD measure of depressive symptoms, Sherer’s self-efficacy measure, and the Barriers to Health Promoting Activities scale (all correlation coefficients >0.40). In addition, the Cognitive Abilities score had a moderate relationship with the Global Health Self-Rating item, but only low to moderate correlations with the subscales of the HPLP-II. Both scales were moderately correlated with the ISS (r = 0.37 for Cognitive Concerns and −0.36 for Cognitive Abilities).
Table 3.
Correlation coefficients among PROMIS Cognitive Abilities Scale, PROMIS Cognitive Concerns Scale, Incapacity Status Scale, and Other Health Measures (N = 322)
Hierarchical Regression Analysis
To further explore the construct validity of the PROMIS Cognitive Concerns scale, a hierarchical regression was performed to determine how much variance in the prediction of Incapacity Status, a measure of functional impairment, was explained by PROMIS Cognitive Concerns after taking into account other health measures. To avoid problems with issues of multicollinearity and suppression,24 the predictors used in the first step of the regression analysis were restricted to the 1-item Global Health Self-Rating, the CESD measure of depressive symptoms, and two subscales of the HPLP-II: Physical Activity and Spiritual Growth (representing the physical and emotional aspects of health promotion most highly correlated with the ISS). The PROMIS Cognitive Concerns Scale was then entered on the second step of the analysis to predict Incapacity Status scores. The unstandardized regression coefficients (b) and intercept, the standardized regression coefficients (β), and confidence intervals for the full model are reported in Table 4.
Table 4.
Multiple hierarchical regression analysis to predict incapacity status (n = 319)
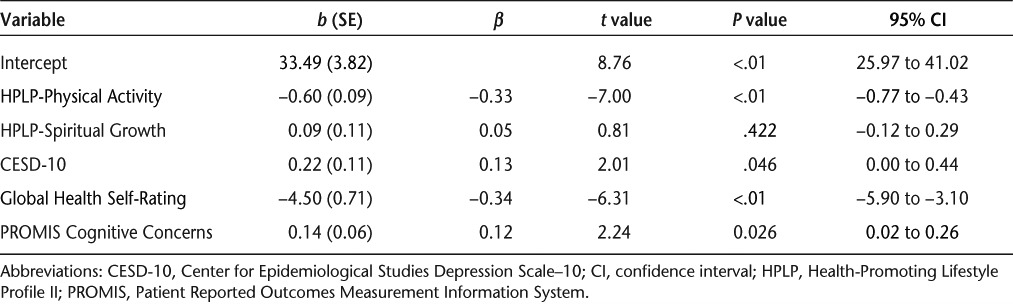
The results of step 1 indicated that the variance accounted for (R2) with the first four independent variables (HPLP two subscales, Global Health Self-Rating, CESD) was 0.44 (adjusted R2 = 0.43) and it was significantly different from zero (F4,315 = 60.53, P < .001). In the first step, the HPLP Physical Activity Scale, the CESD, and the Global Health Self-Rating were significant predictors of Incapacity Status scores (Physical Activity, b = −0.60, P < .001; CESD-10, b = 0.22, P < .01; health self-rating, b = −4.50, P < .01). In step 2, the PROMIS Cognitive Concerns score was entered into the regression equation. The change in variance accounted for (ΔR2) was equal to 0.01, which was associated with significant change (F for change1,314 = 5.03, P < .05). That is, the PROMIS Cognitive Concerns score added significant variance to the prediction of functional impairment, after controlling for all other health variables. Incapacity Status scores increase, on average, by 0.14 point for each 1-point Cognitive Concerns score increase, holding constant health-promoting behavior subscales (Physical Activity, Spiritual Growth), depressive symptoms, and self-rated health status. The adjusted R2 for the final model was 0.44.
Known Group Validation with Employment Status
There were statistically significant differences in PROMIS Cognitive Abilities (F2,319 = 6.38, P < .01) and PROMIS Cognitive Concerns scores by employment status (F2,319 = 5.70, P < .01). Post hoc analyses indicated that those unemployed owing to their disability reported significantly poorer cognitive abilities and more cognitive concerns than those who were working or those who were unemployed for other reasons.
Discussion
To our knowledge, this is the first exploration of the PROMIS cognitive scales in a large sample of individuals with MS. The PROMIS Cognitive Abilities and Cognitive Concerns Scales not only capitalize on recent advances in psychometric theory, but also facilitate comparisons of cognitive functioning among people with other chronic conditions. The Cronbach α coefficients suggest that the internal consistency reliabilities are impressive for 8-item scales and reflect the careful development process undertaken by the PROMIS research team.
As expected, scores on the two PROMIS scales were highly related in opposite directions (r = −0.85). The moderate to strong correlation coefficients between PROMIS cognitive scales and the other health measures examined here suggest that for people with MS, their perceptions of their cognitive functioning are highly related to their perceptions of depressive symptoms, self-efficacy, barriers to health promotion, and functional impairment and perceived health status. These findings support the construct validity of the PROMIS scales among people with MS. While the relationships were less strong with the various dimensions of health promotion measured by the HPLP-II, the moderate-strength correlations between PROMIS Cognitive Abilities and four of the six HPLP-II subscales suggest that future research should explore the impact of cognitive function on health promotion. The pattern of results reveals that Cognitive Concerns scores, which present negatively stated items, were more strongly correlated with other negatively oriented scales (Incapacity Status, depressive symptoms), while Cognitive Abilities scores had higher numeric correlation coefficients with other measures that focus on abilities rather than limitations or deficits. This pattern of results may reflect the influence of cognitive response set on the measurement of the construct under investigation and suggests that the answers obtained are related not only to the questions asked but also to their positive or negative valence.
Among the set of predictors in the hierarchical regression, the self-reported exercise behaviors and global health self-rating were the strongest predictors of functional limitations as reflected in the ISS. However, cognitive concerns contributed significant unique variance to the prediction of functional limitations, after measures of physical activity, spirituality, depressive symptoms, and general health self-rating were controlled for. This finding suggests that self-perceived cognitive limitations, as measured by the PROMIS Cognitive Concerns scale, are associated with perceived functional incapacity independent of the relationship functional incapacity has to other health factors.
Consistent with previous research,1,2,4,6 PROMIS cognitive scale scores differed by employment status. Because there were many retired individuals in our older sample (average age, 62 years), we divided the unemployed group into those who reported being employed owing to disability and those unemployed for other reasons. The fact that we found that those who were unemployed owing to disability reported poorer cognitive functioning than either those who were working or those who were unemployed for other reasons suggests that future researchers should consider differentiating those who are unemployed owing to disability from those who are unemployed for other reasons. As expected, those who were unemployed for various reasons other than disability were older than the other two groups. Those unemployed owing to disability were more similar in age to those who were working, so the observed differences in perceived cognitive function between these two groups do not appear to be due to age differences.
As has been observed in other studies,5,9–11,32,33 cognitive scores were moderately correlated with a measure of depressive symptoms. Whether cognitive impairment leads to depression or both result directly from the brain deterioration caused by MS, the results of the hierarchical regression analysis performed here suggest that both contribute independently to perceived MS functional limitations, as measured by the ISS.
These data are subject to the biases commonly found with self-report measures such as social desirability and response set. Because the analyses presented here are cross-sectional in nature, causal inferences cannot be made. Moreover, the findings are based on a convenience sample of individuals originally recruited through the MS society in one state, although a number have now moved to other states. The results may not generalize to people with MS who are not members of this MS society—or chose not to participate in this study. Future studies should be undertaken with more diverse samples recruited using other sampling strategies. In addition, it should be noted that the ISS is heavily weighted toward mobility impairment. Future studies should investigate the relationship of the PROMIS Cognitive Abilities and Cognitive Concerns scores to other measures of functional status.
The findings do suggest that the PROMIS Cognitive Abilities and Cognitive Concerns scales can provide clinicians with short yet psychometrically sound measures of self-reported cognitive functioning. Because each scale contains only eight items, they reduce patient burden relative to longer cognitive measures. Future studies should be undertaken in clinical sites to test their utility in those settings.
PracticePoints.
Patients with MS and their health-care providers would benefit from short, psychometrically sound measures of cognitive functioning that are feasible to administer in clinical settings.
The 8-item PROMIS Cognitive Abilities and Cognitive Concerns Scales demonstrated good internal consistency reliability in a sample of 322 people with MS.
Scores on the PROMIS Cognitive Abilities and Cognitive Concerns Scales were strongly related to scores on self-reported measures of self-efficacy, depressive symptoms, barriers to health promotion, health, and functional status, including employment.
Footnotes
Financial Disclosures: The authors have no conflicts of interest to disclose.
Funding/Support: This project was supported by a grant from the National Institute of Nursing Research (Grant 5 R01 NR003195-11A1), Alexa Stuifbergen, Principal Investigator.
References
- 1.Rao SM, Leo GJ, Ellington L. Cognitive dysfunction in multiple sclerosis. II. Impact on employment and social functioning. Neurology. 1991;41:692–696. doi: 10.1212/wnl.41.5.692. et al. [DOI] [PubMed] [Google Scholar]
- 2.Amato MP, Ponziani G, Rossi F. Quality of life in multiple sclerosis: the impact of depression, fatigue and disability. Mult Scler. 2001;7:340–344. doi: 10.1177/135245850100700511. et al. [DOI] [PubMed] [Google Scholar]
- 3.Benedict RH, Cookfair D, Gavett R. Validity of the Minimal Assessment of Cognitive Function in Multiple Sclerosis (MACFIMS) J Int Neuropsychol Soc. 2006;12:549–558. doi: 10.1017/s1355617706060723. et al. [DOI] [PubMed] [Google Scholar]
- 4.Shevil E, Finlayson M. Perceptions of persons with multiple sclerosis on cognitive changes and their impact on daily life. Disabil Rehabil. 2006;28:779–788. doi: 10.1080/09638280500387013. [DOI] [PubMed] [Google Scholar]
- 5.Figved N, Benedict R, Klevan G. Relationship of cognitive impairment to psychiatric symptoms in multiple sclerosis. Mult Scler. 2008;14:1084–1090. doi: 10.1177/1352458508092262. et al. [DOI] [PubMed] [Google Scholar]
- 6.Messmer Uccelli M, Specchia C, Battaglia A, Miller DM. Factors that influence the employment status of people with multiple sclerosis: a multi-national study. J Neurol. 2009;256:1989–1996. doi: 10.1007/s00415-009-5225-0. [DOI] [PubMed] [Google Scholar]
- 7.Stuifbergen AK, Becker H, Perez F. A randomized controlled trial of a cognitive rehabilitation intervention for persons with multiple sclerosis. Clin Rehabil. 2012;26:882–893. doi: 10.1177/0269215511434997. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benedict RH, Munschauer F, Linn R. Screening for multiple sclerosis cognitive impairment using a self-administered 15-item questionnaire. Mult Scler. 2003;9:95–101. doi: 10.1191/1352458503ms861oa. et al. [DOI] [PubMed] [Google Scholar]
- 9.Stuifbergen AK, Phillips LJ. The influence of metamemory on the quality of life of persons with multiple sclerosis. J Neurosci Nurs. 2006;38:428–434. doi: 10.1097/01376517-200612000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Julian L, Merluzzi NM, Mohr DC. The relationship among depression, subjective cognitive impairment, and neuropsychological performance in multiple sclerosis. Mult Scler. 2007;13:81–86. doi: 10.1177/1352458506070255. [DOI] [PubMed] [Google Scholar]
- 11.Goretti B, Portaccio E, Zipoli V. Coping strategies, cognitive impairment, psychological variables and their relationship with quality of life in multiple sclerosis. Neurol Sci. 2010;31:S227–230. doi: 10.1007/s10072-010-0372-8. et al. [DOI] [PubMed] [Google Scholar]
- 12.Pierson SH, Griffith N. Treatment of cognitive impairment in multiple sclerosis. Behav Neurol. 2006;17:53–67. doi: 10.1155/2006/545860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arnett PA, Higginson CI, Voss WD, Randolph JJ, Grandey AA. Relationship between coping, cognitive dysfunction and depression in multiple sclerosis. Clin Neuropsychol. 2002;16:341–355. doi: 10.1076/clin.16.3.341.13852. [DOI] [PubMed] [Google Scholar]
- 14.Amato MP, Zipoli V. Clinical management of cognitive impairment in multiple sclerosis: a review of current evidence. Int MS J. 2003;10:72–83. [PubMed] [Google Scholar]
- 15.Becker H, Stuifbergen AK, Morrison J. Promising new approaches to assess cognitive functioning in people with multiple sclerosis. Int J MS Care. 2012;14:71–76. doi: 10.7224/1537-2073-14.2.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cella D, Riley W, Stone A. Initial item banks and first wave testing of the Patient-Reported Outcomes Measurement Information System (PROMIS) network: 2005–2008. J Clin Epidemiol. 2010;63:1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stuifbergen AK, Roberts G. Health promotion practices of women with multiple sclerosis. Arch Phys Med Rehabil. 1997;78(suppl 5):S3–S9. doi: 10.1016/s0003-9993(97)90215-x. [DOI] [PubMed] [Google Scholar]
- 18.Harrison T, Stuifbergen A, Adachi E. Marriage, impairment, and acceptance in persons with multiple sclerosis. West J Nurs Res. 2004;26:266–285. doi: 10.1177/0193945903260188. et al. [DOI] [PubMed] [Google Scholar]
- 19.Kurtzke JF. A proposal for a uniform minimal record of disability in multiple sclerosis. Acta Neurol Scand. 1981;64(suppl 87):110–129. [Google Scholar]
- 20.Andresen EM, Malmgren JA, Carter WB. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10:77–84. et al. [PubMed] [Google Scholar]
- 21.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 22.Stuifbergen AK, Seraphine A, Roberts G. An explanatory model of health promotion and quality of life in chronic disabling conditions. Nurs Res. 2000;49:122–129. doi: 10.1097/00006199-200005000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Walker SN, Sechrist KR, Pender NJ. The Health Promoting Lifestyle Profile: development and psychometric characteristics. Nurs Res. 1987;36:76–81. [PubMed] [Google Scholar]
- 24.Berger AM, Walker SN. An explanatory model of fatigue in women receiving adjuvant breast cancer chemotherapy. Nurs Res. 2001;50:43–54. doi: 10.1097/00006199-200101000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Stuifbergen AK, Becker H, Blozis S. A randomized clinical trial of a wellness intervention for women with multiple sclerosis. Arch Phys Med Rehabil. 2003;84:467–476. doi: 10.1053/apmr.2003.50028. et al. [DOI] [PubMed] [Google Scholar]
- 26.Lawton MP, Moss M, Fucomer M. A research and service oriented multilevel assessment instrument. J Gerontol. 1982;37:91–99. doi: 10.1093/geronj/37.1.91. et al. [DOI] [PubMed] [Google Scholar]
- 27.Becker H, Stuifbergen AK, Sands D. Development of a scale to measure barriers to health promotion activities among persons with disabilities. Am J Health Promot. 1991;5:449–454. doi: 10.4278/0890-1171-5.6.449. [DOI] [PubMed] [Google Scholar]
- 28.Sherer M, Maddux J, Mercandante B. The self-efficacy scale: construction and validation. Psychol Rep. 1982;51:663–671. et al. [Google Scholar]
- 29.Stuifbergen AK, Becker H. Predictors of health-promoting lifestyles in persons with disabilities. Res Nurs Health. 1994;17:3–13. doi: 10.1002/nur.4770170103. [DOI] [PubMed] [Google Scholar]
- 30.Stuifbergen AK. Health-promoting behaviors and quality of life among individuals with multiple sclerosis. Sch Inq Nurs Pract. 1995;9:31–50. [PubMed] [Google Scholar]
- 31.Bobko P. Correlation and Regression: Applications for Industrial Organizational Psychology and Management. Thousand Oaks, CA: Sage Publications; 2001. [Google Scholar]
- 32.Arnett PA, Barwick FH, Beeney JE. Depression in multiple sclerosis: review and theoretical proposal. J Int Neuropsychol Soc. 2008;14:691–724. doi: 10.1017/S1355617708081174. [DOI] [PubMed] [Google Scholar]
- 33.Barwick FH, Arnett PA. Relationship between global cognitive decline and depressive symptoms in multiple sclerosis. Clin Neuropsychol. 2011;25:193–209. doi: 10.1080/13854046.2010.538435. [DOI] [PubMed] [Google Scholar]


