Abstract
Background: Despite recent efforts to educate multiple sclerosis (MS) health-care providers about the importance of pelvic floor disorders (urinary, bowel, and sexual dysfunction), no data are currently available to assess outcomes of these efforts in terms of patient satisfaction.
Methods: As part of the fall 2010 North American Research Committee on Multiple Sclerosis survey, we conducted a prospective, survey-based cohort study (N = 14,268) to evaluate patient satisfaction with the current evaluation and treatment of pelvic floor disorders. Patients were queried about 1) bother from bladder, bowel, or sexual symptoms; 2) whether they had been evaluated by a health-care provider for pelvic floor issues in the last 12 months; and 3) satisfaction with the evaluation and treatment they received, on a 5-point Likert scale. Patients were also asked whether these treatments had affected their quality of life (7-point Likert scale).
Results: A total of 9397 responses were received (response rate of 65.9%); respondents were primarily white (89%) and female (77.4%). Moderate-to-severe pelvic floor symptoms were reported by one-third of patients (bladder, 41%; bowel, 30%; sexual, 42%). Most respondents had been asked about bladder (61%) or bowel (50%) issues by their health-care providers, but only 20% had been queried about sexual dysfunction. Most respondents were moderately to very satisfied with the management of their bladder and bowel disorders but significantly less satisfied with that of sexual dysfunction.
Conclusions: While MS patients are generally satisfied with current management of bladder and bowel dysfunction, improvement is needed in that of sexual dysfunction.
Multiple sclerosis (MS) is well known to have significant detrimental effects on bowel, bladder, and sexual function. In recent years, several organizations have attempted to educate health-care providers on the importance of pelvic floor disorders in order to improve patient care. In 1999, the Multiple Sclerosis Council for Clinical Practice Guidelines drafted recommendations for the management of urinary dysfunction in patients with MS, setting the first standards for the management of these problems.1 More recently, the Consortium of Multiple Sclerosis Centers (CMSC) published consensus guidelines for the management of bowel and urinary symptoms, which included treatment algorithms to guide patients, families, and health-care providers and reflected advances in patient care in a variety of related fields.2
A previous study demonstrated the significant undertreatment of overactive bladder (OAB) symptoms among patients with MS.3 Sixty-five percent of respondents to the fall 2005 North American Research Committee on Multiple Sclerosis (NARCOMS) questionnaire reported at least one moderate-to-severe urinary symptom, including urinary frequency, urgency, leakage of any kind, and nocturia. Among respondents with moderate-to-severe OAB symptoms, only 55% had ever undergone urologic evaluation for these complaints, and only 51% had ever been treated with an anticholinergic medication. Among those who had been treated, the treatments used tended to be older (characterized as being less well tolerated and having greater side effects compared with newer medications) and not in line with those used in the general population. Longer disease duration was significantly correlated with worsening OAB symptoms, as represented by a higher urinary symptom score (r = 0.135, P < .001).
Given the inadequate treatment and evaluation of bladder-related dysfunction demonstrated in previous research, we sought to determine the experience of MS patients with pelvic floor disorders in general, including bladder, bowel, and sexual problems. Although significant effort has been put forth to educate both patients and health-care providers on the importance of evaluating and treating these problems, pelvic floor disorders remain embarrassing and difficult to discuss, resulting in their frequent neglect in the course of routine patient care. Furthermore, patient-based outcomes reflecting the impact of these educational efforts have not been assessed to date.
The goal of this study was to assess patient satisfaction with the care received for pelvic floor disorders—including bowel, bladder, and sexual dysfunction symptoms—using a large database of community-dwelling patients with MS. Patient history of evaluation and treatment and association with degree of physical disability were also assessed.
Methods
The NARCOMS Registry, a project of the CMSC (www.mscare.org), is the largest registry in North America of patients with MS. Consisting of MS patients who volunteered to participate in research-related activities, it captures self-reported demographic and clinical information from MS patients at enrollment in the registry and semiannually thereafter through questionnaires administered either online or by mail, in accordance with participant preference. The registry is the largest self-report database of patients with MS worldwide, with more than 14,000 active participants, and is approved by the Western Institutional Review Board (IRB) and the IRB at the University of Alabama at Birmingham. We obtained an exemption from the University Hospitals Case Medical Center IRB for this study. De-identified data from the fall 2010 questionnaire were supplied for analysis by NARCOMS in the form of an Excel (Microsoft, Redmond, WA) spreadsheet with a data dictionary.
At enrollment in NARCOMS, participants provide demographic information and clinical information, including age at MS onset. Each semiannual NARCOMS questionnaire includes an assessment of disability status and quality of life (QOL). The Patient-Determined Disease Steps (PDDS) measures disability based on self-report and has been validated in large MS populations against the physician-scored Expanded Disability Status Scale (EDSS).4–6 It is scored from 0 to 8, with 0 defined as no disability and 8 as bed-bound.7 Respondents are also evaluated for bladder and spasticity-related disability using standardized questionnaires.
In the fall of 2010, we collaborated with the NARCOMS staff to create a two-page questionnaire on pelvic floor disorders for inclusion in the fall 2010 survey. Specifically, patients were asked to report their degree of bother from bladder, bowel, and sexual problems on a 4-point scale (1 = not at all bothered, 4 = severely bothered). Respondents were given a choice of “not applicable” for each of the pelvic floor disorder types if they did not have these symptoms. Patients were asked whether their health-care providers had inquired about each type of pelvic floor disorder in the last 12 months (yes or no). Patients were also asked to rate on a 5-point Likert scale (1 = not at all, 5 = completely) their degree of satisfaction with the care they received for each problem. Finally, they were asked whether their QOL had changed with treatment (7-point Likert scale; 1 = much better, 7 = much worse). Medication use, evaluation by a urologist, and correlation with disability as measured by PDDS score were also evaluated.
Data analysis used descriptive statistics, χ2 tests for comparisons between genders, calculation of correlation coefficients, and 95% confidence intervals (CIs). Data analysis was performed with SAS, version 9.2 (SAS Institute Inc, Cary, NC).
Results
In the fall of 2010, the biannual NARCOMS questionnaire was delivered to 14,268 participants; a total of 9397 questionnaires were returned, for a response rate of 65.9%. Respondents were primarily white (89%) and female (77.4%), with an average (SD) age of 55 (10.5) years. Significant disability, defined as a PDDS score of at least 3 (representing gait disability or worse), was reported by 6070 respondents (64.6%; 95% CI, 63.6–65.5). Moderate-to-severe bladder disability scores were reported by 2743 respondents (29.2%; 95% CI, 28.3–30.1), with 281 (3%; 95% CI, 2.7–3.4) reporting total loss of bowel and bladder control.
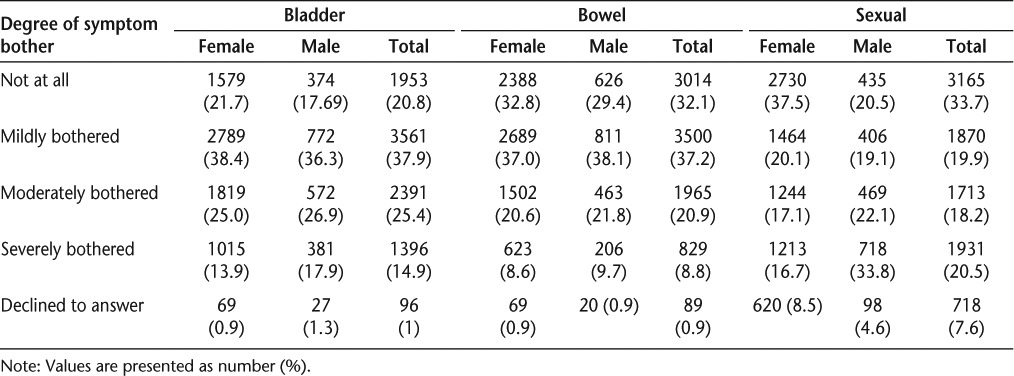
Moderate-to-severe pelvic floor symptoms, defined as a Likert scale score of 3 or higher, were reported by a large number of respondents (Table 1). Moderate-to-severe bother from bladder symptoms was reported by 3787 respondents (40.3%; 95% CI, 39.3–41.3): 2834 females (39.8%) versus 953 males (44.8%) (P < .001). Moderate-to-severe bowel symptoms were reported by 2794 respondents (29.7%; 95% CI, 28.8–30.7): 2125 females (29.8%) versus 669 males (31.5%) (P = .039). Despite a large number of respondents who opted not to answer questions about sexual dysfunction (718 respondents, or 7.6%), a sizeable number reported moderate-to-severe sexual problems (3644 respondents, or 38.8%; 95% CI, 37.8–39.8), with results differing significantly by gender: 2457 females (34.5%) versus 1187 males (55.8%) (P < .001).
Table 1.
Degree of bother from pelvic floor symptoms reported by respondents (N = 9397)
Increased disability as gauged by the PDDS was significantly correlated with the presence of bladder (r = 0.483; 95% CI, 0.468–0.498), bowel (r = 0.364; 95% CI, 0.347–0.381), and sexual dysfunction (r = 0.140; 95% CI, 0.120–0.159) (all P < .001). The presence of bladder dysfunction significantly increased the likelihood of concurrent bowel (r = 0.505; 95% CI, 0.490–0.520; P < .001) and sexual dysfunction (r = 0.240; 95% CI, 0.221–0.259; P < .001).
Respondents were much more likely to have been asked about bladder and bowel dysfunction than about sexual dysfunction by their health-care providers in the last year. Overall, 61.3% (5763 respondents; 95% CI, 60.3–62.3) had been queried about bladder dysfunction in the last year: 4430 (60.9%) female patients and 1333 (62.7%) male patients (P = .245). Fifty percent (4733 respondents; 95% CI, 49.4–51.4) had been asked about bowel problems: 3573 (49.1%) females and 1160 (54.6%) males (P < .001). In contrast, only 20.1% overall (1892 respondents; 95% CI, 19.3–20.9) recalled being asked about sexual dysfunction issues in the last year by their health-care providers. This differed significantly by gender, with 1202 (16.5%) females versus 690 (32.4%) males responding positively (P < .001).
Patients with significant pelvic floor symptoms were more likely to have been assessed for pelvic floor disorders than were respondents as a whole. In patients with moderate-to-severe bladder symptoms, 2630 of 3787 patients (69.4%; 95% CI, 68.0–70.9) reported evaluation of this issue by their current MS health-care providers: 1958 of 2834 (69.1%) females and 672 of 953 (70.5%) males (P = .557). For patients with moderate-to-severe bowel symptoms, 1638 of 2794 (58.6%; 95% CI, 56.8–60.5) reported undergoing evaluation for their symptoms: 1217 of 2125 (57.3%) females and 421 of 669 (62.9%) males (P = .014). And among patients with moderate-to-severe sexual problems, only 870 of 3644 (23.9%; 95% CI, 22.5–25.3) reported evaluation for these symptoms in the last year. There was a significant difference by gender, with only 455 of 2457 (18.5%) females reporting such evaluation, compared with 415 of 1187 (35.0%) males (P < .001).
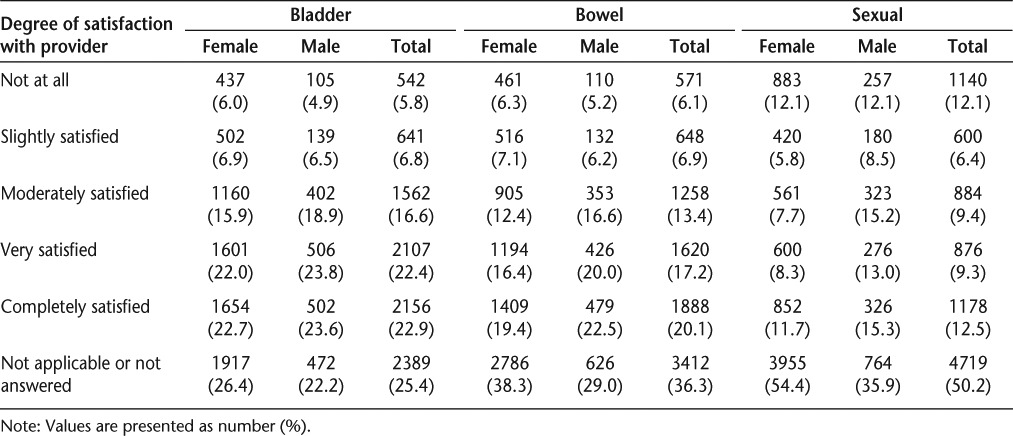
Despite low-to-moderate rates of questioning about pelvic floor issues, patients were generally satisfied with the evaluation and treatment of bladder and bowel complaints, but less satisfied with the management of sexual dysfunction, by their health-care providers (Table 2). Respondents were most pleased with the management of bladder symptoms (urinary incontinence or retention), with 5825 of 7008 patients overall (83.1%; 95% CI, 82.2–84.0), 4415 of 5354 (82.5%) females, and 1410 of 1654 (85.2%) males reporting moderate-to-complete satisfaction. Respondents were comparably satisfied with the evaluation and treatment of bowel symptoms (fecal incontinence, diarrhea, and constipation), with 4766 of 5985 patients overall (79.6%; 95% CI, 78.6–80.6) reporting moderate-to-complete satisfaction: 3508 of 4485 (78.2%) females and 1258 of 1500 (83.9%) males. Satisfaction was much lower, however, among those responding to questions about sexual dysfunction. Many patients opted not to answer these questions (50%, or 4719 respondents). Of the 4768 patients who did respond, only 2938 (61.6%; 95% CI, 60.2–63.0) reported moderate-to-complete satisfaction with their care: 2013 of 3316 (60.7%) females versus 925 of 1362 (67.9%) males (P < .001). Thirty-seven percent of respondents were “not at all” to “slightly” satisfied with the care received for sexual dysfunction. Increased bother from bladder, bowel, or sexual problems was inversely correlated with satisfaction with provider evaluation and treatment (bladder: r = –0.206; 95% CI, –0.228 to –0.184; bowel: r = –0.339; 95% CI, –0.361 to –0.317; sexual: r = –0.400; 95% CI, –0.423 to –0.376; all P < .001).
Table 2.
Patient satisfaction with provider evaluation and treatment of bladder, bowel, and sexual problems (N = 9397)
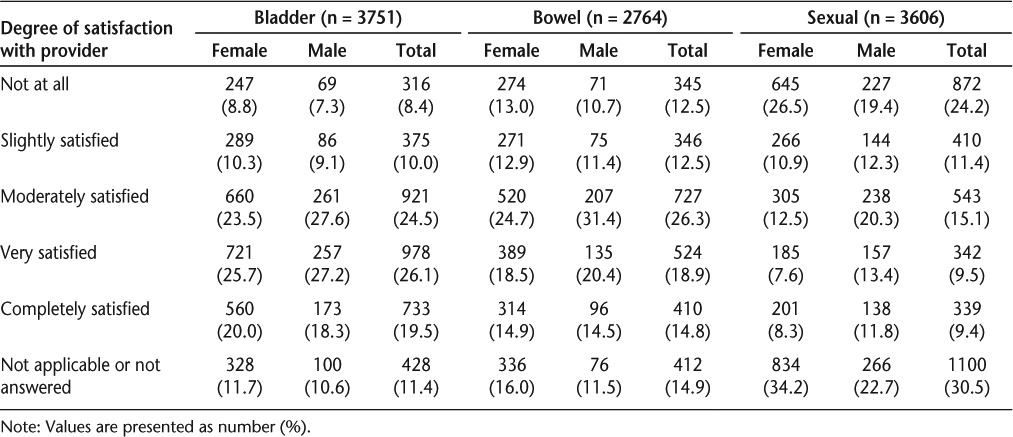
Among patients with moderate-to-severe pelvic floor problems, rates of satisfaction with care were higher among those with bowel and bladder symptoms than among those with sexual dysfunction (Table 3). Although no difference was found regarding the care of urinary symptoms, men tended to be more satisfied than women with the care of bowel and sexual problems. Of patients with moderate-to-severe bladder symptoms, 70.2% (2632; 95% CI, 68.7–71.6) of respondents reported moderate-to-complete satisfaction with their evaluation and care: 69.2% of females and 73.0% of males (P = .025). Among those with moderate-to-severe bowel symptoms, 60% (1661; 95% CI, 58.3–61.9) reported moderate-to-complete satisfaction: 58.1% of females and 66.4% of males (P < .001). In contrast, of respondents with moderate-to-severe sexual dysfunction, only 33.9% (95% CI, 32.4–35.5) were moderately to completely satisfied with their care, while 24.2% (95% CI, 22.8–25.6) were “not at all satisfied”: 26.5% of females and 19.4% of males (P < .001). Age did not affect patient satisfaction with the management of their pelvic floor problems.
Table 3.
Satisfaction with provider evaluation and treatment of pelvic floor problems among patients with moderate-to-severe symptoms only
For the majority of patients, treatment of pelvic floor dysfunction had either a positive effect or no effect on QOL. Although the results were skewed by the large number of patients who chose not to respond to this question, of the 5134 who did respond, 43% reported no effect on QOL and 47% reported an improvement, ranging from “a little better” to “much better” on a 7-point Likert scale. Nine percent (467 respondents) believed that treatment of their pelvic floor problems had negatively affected their QOL.
Discussion
Despite significant efforts to educate patients, families, and health-care providers on the importance of bowel, bladder, and sexual dysfunction in MS patients, the impact of these efforts remains unclear. In a previous study, we demonstrated that 65% of men and women with MS reported moderate-to-severe urinary symptoms and that the majority of these patients had not been evaluated or treated for these problems.3 Those patients who had received treatment were often given older and significantly more morbid therapeutic options than members of the general population. Given these findings, we sought to explore the prevalence of bladder, bowel, and sexual dysfunction in a large sampling of the MS population. Most importantly, we sought to determine whether the significant educational efforts by MS organizations were having any effect on the satisfaction of MS patients with the care they receive for pelvic floor problems and the impact of this care on QOL.
Our results demonstrate that moderate-to-severe pelvic floor symptoms are extremely common among MS patients, with 41% reporting bladder, 30% reporting bowel, and 42% reporting sexual dysfunction. Our results may be skewed by selection bias. The sampling of patients participating in the NARCOMS Registry may not be representative of the general population of MS patients. Although patients who agree to participate in NARCOMS surveys may tend to be more willing to discuss their medical and personal issues, a significant number of patients opted not to answer questions about sexual dysfunction. Bladder and bowel symptoms as well as sexual dysfunction remain difficult topics to discuss, and our limited questionnaire responses may reflect widespread discomfort even in an anonymous format.
Selection bias and differences in symptom measures may also explain why only 41% of respondents reported moderate-to-severe bladder symptoms in the fall 2010 survey, compared with 65% in the survey administered in the fall of 2005. Patients who had previously completed the fall 2005 questionnaire may have opted not to answer similar questions in the 2010 survey. In addition, different tools were used in the two questionnaires to measure symptom severity, with the validated Urinary Distress Index used in 2005 versus a self-described Likert scale in 2010.8 The resulting difference in the definition of “moderate-to-severe” pelvic floor symptoms may significantly contribute to the variation in our results.
Despite the large numbers of patients who chose not to answer questions on sexual dysfunction, a significant number of respondents did report such dysfunction (42%). Sexual dysfunction appears to be a significant concern for both men and women with MS. Men reported significantly higher rates of moderate-to-severe sexual dysfunction. Again, selection bias may hinder our ability to accurately estimate the prevalence of these complaints. Were patients with severe sexual dysfunction simply not comfortable answering these questions (suggesting that the true incidence is higher)? No evidence suggests this to be the case. Or were the patients with the most severe symptoms the ones most likely to respond (suggesting that the true incidence is much lower)? In addition, the elective nature of sexual activity versus the universal need to urinate and defecate may further skew our results. Nonetheless, our findings serve as a good starting point for determining the true rates of sexual and all pelvic floor disorders in MS patients. Although further studies are needed, men seem to be more bothered by sexual dysfunction than women. Further research is required to establish the true prevalence of these symptoms in the MS population.
Respondents reported being asked about bowel and bladder complaints more frequently than sexual complaints within the last year by a health-care provider. Bladder (61%) and bowel (50%) symptoms were discussed with a health-care provider within the last year by at least half of respondents. Given recent significant educational efforts, however, we had hoped that these percentages would be higher. Unfortunately, only 20% of respondents had been asked about sexual dysfunction issues, although 40% reported moderate-to-severe symptoms. Pelvic floor issues may not be a high priority in the often-complicated medical care of MS patients as their disease progresses. Although increased bladder, bowel, and sexual dysfunction may be routinely acknowledged signs of worsening MS, our study is the first to demonstrate a clear correlation between worsening pelvic floor symptoms and MS progression. Health-care providers should not ignore these important issues, no matter what stage of disease the patient exhibits.
Rates of patient satisfaction with the care received from health-care providers and its impact on QOL were surprising. Despite relatively low rates of evaluation of pelvic floor symptoms, most patients reported moderate-to-complete satisfaction with the care received (70%). Although patients with the most severe symptoms tended to be less satisfied with their care, minor attention to these issues appeared to adequately satisfy most patients. In general, female respondents tended to be less satisfied with the care received for pelvic floor problems than male respondents, although the difference did not always reach statistical significance. Although male respondents reported higher rates of moderate-to-severe sexual dysfunction, men were generally more satisfied than women with the care they received for these issues. In general, male sexual dysfunction is more easily treated, with excellent pharmacologic options available, while treatments for women are limited, possibly explaining this difference.
Despite relatively high rates of satisfaction with evaluation and treatment of pelvic floor disorders overall, such treatment did not have a clear impact on patient QOL for the majority of respondents. Although these results may be surprising, they may indicate that pelvic floor issues are not a major concern for most of our respondents, and perhaps for MS patients in general.
Finally, our survey did not involve screening for depression or other psychosocial issues. As a result, the potential significant impact of these factors on satisfaction with the care of pelvic floor disorders, especially sexual dysfunction, and QOL was not assessed. Psychosocial factors are well known to affect female sexual function in general; these unassessed factors may contribute to the lower rates of satisfaction with sexual dysfunction care among female respondents.9,10 Further studies examining this complex relationship would strengthen our understanding of these issues.
This study demonstrates significant patient satisfaction with current levels of evaluation and treatment of bladder and bowel dysfunction in MS. Recent efforts to increase patient, family, and clinician awareness of the importance of pelvic floor issues appear to have made some impact on the QOL of MS patients. However, these results are not universal; with regard to sexual dysfunction, outcomes remain poor. Many patients do not appear to receive adequate care from their health-care providers for these issues, nor are they satisfied with the care they do get. Future efforts must also be directed at more aggressive identification and treatment of sexual dysfunction among men and women with MS.
PracticePoints.
Although educational efforts have led to significant improvements in the management of bowel and bladder dysfunction among men and women with MS, treatments for sexual dysfunction remain inadequate.
Many patients are very satisfied with the care they receive for their urinary and bowel symptoms but are dissatisfied with the treatment of sexual dysfunction issues associated with MS.
Acknowledgments
The authors would like to acknowledge the Consortium of Multiple Sclerosis Centers (CMSC) and its Foundation for their support of NARCOMS; and Robert Fox, MD, Tuula Tyry, PhD, MAED, and Kerry Grimberg, PhD, for their assistance with the editing of this manuscript.
Footnotes
Financial Disclosures: The authors have no conflicts of interest to disclose.
References
- 1.Seland P. 1999 Paper presented at: “Urinary Dysfunction and Multiple Sclerosis: Evidence-Based Management Strategies for Urinary Dysfunction in Multiple Sclerosis” (conference of the Multiple Sclerosis Council for Clinical Practice Guidelines [MSCCPG]) Washington, DC. [Google Scholar]
- 2.Namey M. Elimination dysfunction in multiple sclerosis: proceedings of a consensus conference. Int J MS Care. 2012;14(suppl 1):1–26. et al. [Google Scholar]
- 3.Mahajan S, Patel P, Marrie R. The undertreatment of overactive bladder symptoms in women with multiple sclerosis: an ancillary analysis of the NARCOMS patient registry. J Urol. 2010;183:1432–1437. doi: 10.1016/j.juro.2009.12.029. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz C, Vollmer T, Lee H, North American Research Consortium on Multiple Sclerosis Outcomes Study Group Reliability and validity of two self-report measures of impairment and disability for MS. Neurology. 1999;52:63–71. doi: 10.1212/wnl.52.1.63. [DOI] [PubMed] [Google Scholar]
- 5.Hohol M, Orav E, Weiner H. Disease steps in multiple sclerosis: a simple approach to evaluate disease progression. Neurology. 1995;45:251–255. doi: 10.1212/wnl.45.2.251. [DOI] [PubMed] [Google Scholar]
- 6.Hohol M, Orav E, Weiner H. Disease steps in multiple sclerosis: a longitudinal study comparing disease steps and EDSS to evaluate disease progression. Mult Scler. 1999;5:349–354. doi: 10.1177/135245859900500508. [DOI] [PubMed] [Google Scholar]
- 7.Kurtzke J. Rating disability in multiple sclerosis: an expanded disability status scale (EDSS) Neurology. 1983;33:144. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- 8.Uebersax J, Wyman JF, Shumaker SA, McClish DK, Fantl JA, Continence Program for Women Research Group Short forms to assess life quality and symptom distress for urinary incontinence in women: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Neurourol Urodyn. 1995;14:131–139. doi: 10.1002/nau.1930140206. [DOI] [PubMed] [Google Scholar]
- 9.Orasanu B, Wyman A, Mahajan S. Sexual dysfunction in patients with multiple sclerosis. Mult Scler Relat Disord. 2013;2:117–123. doi: 10.1016/j.msard.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 10.Crayton H, Rossman H. Managing the symptoms of multiple sclerosis: a multimodal approach. Clin Ther. 2006;28:445–460. doi: 10.1016/j.clinthera.2006.04.005. [DOI] [PubMed] [Google Scholar]


