Abstract
Previous research has documented that individuals exposed to more stressors during disasters and their immediate aftermath (immediate stressors) are at risk of experiencing longer-term postdisaster stressors. Longer-term stressors, in turn, have been found to play a key role in shaping postdisaster psychological functioning. Few studies have simultaneously explored the links from immediate to longer-term stressors, and from longer-term stressors to psychological functioning, however. Additionally, studies have inadequately explored whether postdisaster psychological symptoms influence longer-term stressors. In the current study, we aimed to fill these gaps. Participants (N = 448) were from population-based study of Hurricane Ike survivors and completed assessments 2–5 months (Wave 1), 5–9 months (Wave 2) and 14–18 months (Wave 3) postdisaster. Through path analysis, we found that immediate stressors, assessed at Wave 1, were positively associated with Wave 2 and Wave 3 stressors, which in turn were positively associated with Wave 2 and Wave 3 posttraumatic stress and depressive symptoms. Wave 2 posttraumatic stress symptoms were positively associated with Wave 3 stressors, and Wave 1 depressive symptoms were positively associated with Wave 2 stressors. The findings suggest that policies and interventions can reduce the impact of disasters on mental health by preventing and alleviating both immediate and longer-term postdisaster stressors.
Research has amply documented elevated rates of many psychological disorders, including posttraumatic stress and major depression, in the aftermath of disasters (e.g., Neria, Nandi, & Galea, 2008). In the initial months after disaster, there is a clear dose-response relationship between exposure to stressors experienced during the disaster and its immediate aftermath (immediate stressors, e.g., property loss and damage) and psychological symptoms, with the highest levels of symptoms among those who experienced the most stressors (e.g., Galea et al., 2007). Although some studies suggest that immediate stressors continue to have significant effects on psychological symptoms over longer periods of time (e.g., Paxson, Fussell, Rhodes, & Waters, 2012), others have suggested that their influence on symptoms weakens and that they could even contribute to positive psychological outcomes, including posttraumatic growth (e.g., Norris, Perilla, Riad, Kaniasty & Lavizzo, 1999; Xu & Liao, 2011). Instead, longer-term stressors (e.g., more persistent disruptions in employment, relationship problems) are thought to play a more important role in determining longer-term symptoms (e.g., Norris et al., 1999).
Conservation of resources (COR) theory (Hobfoll, 1989) provides a framework for understanding how immediate and longer-term stressors contribute to postdisaster psychological responses. COR theory conceptualizes stressors as losses of resources, including objects (e.g., housing), conditions (e.g., relationships), and energies (e.g., money). Individuals who experience initial resource loss are prone to further losses through a process termed “loss spirals” (Hobfoll, 1989). It follows that disaster survivors who experience more immediate stressors would be prone to experience more longer-term stressors. Studies to date have demonstrated this association, for example, showing immediate stressors to be predictive of longer-term displacement, unemployment, and declines in social support (e.g., Blaze & Shwalb, 2009; Elliot & Pais, 2006; Kaniasty & Norris, 2009). Evident in these findings is that initial losses can lead to subsequent losses within the same domain as well as in different domains. For example, a housing-related loss (e.g., property damage) could lead to both further housing-related stressors (e.g., residential instability) and other stressors (e.g., difficulties finding employment, disruptions in relationships).
These loss spirals, or longer-term stressors triggered by immediate stressors, are thought to heighten risk for persistent mental health problems (Hobfoll, 1989), and research to date has indeed detected associations between longer-term stressors and postdisaster psychopathology. For example, increases in stressors (e.g., unemployment, relationship conflicts) in the aftermath of Hurricane Andrew were predictive of increases in posttraumatic stress and depressive symptoms beyond immediate hurricane exposure (Norris et al., 1999). Other studies have focused on specific longer-term stressors, including relocation, family-related stressors, and declines in social support, and found positive associations with psychological symptoms, again controlling for exposure to immediate disaster-related stressors (e.g., Najarian, Goenjian, Pelcovitz, Mandel, & Najarian, 2001; Rowe, La Greca, & Alexandersson, 2010).
Taken together, the literature suggests that immediate stressors increase the likelihood of longer-term stressors, heightening the risk of postdisaster mental health problems. Few studies, however, have simultaneously explored these pathways. One exception is a study of flood survivors that found that the degree of flood exposure was associated with greater losses in psychosocial resources (e.g., time with loved ones, sense of optimism), which in turn were associated with greater increases in psychological distress (Smith & Freedy, 2000). Another study found that Hurricane Katrina survivors who endured more immediate stressors experienced greater pre- to postdisaster declines in social support, which in turn were associated with greater pre- to postdisaster increases in psychological distress (Lowe, Chan, & Rhodes, 2010).
Also lacking in the literature is how postdisaster symptoms might contribute to loss spirals. Research on stress generation indicates that depressed individuals select into more stressful experiences, particularly those of an interpersonal nature (Hammen, 2006). Posttraumatic stress symptoms have likewise been linked to increased risk for subsequent trauma exposure (Cougle, Resnick, & Kilpatrick, 2009), and it is possible that this is also true for subsequent stressor exposure. More generally, the functional impairment rendered by depressive and posttraumatic stress symptoms, including difficulties in employment activities and relationships, suggests that they could induce further stressors (e.g.,Amaya-Jackson et al., 1999; Kessler et al., 2003).
In the current study, we aimed to test a path model reflective of the complex processes that contribute to longer-term postdisaster posttraumatic stress and depressive symptoms. Data were from a 3-wave population-based study of Hurricane Ike survivors, spanning from 2–18 months postdisaster. Based on prior theory and research, we hypothesized that (a) more immediate stressors would be associated more longer-term stressors, (b) both immediate and longer-term stressors would be associated with more posttraumatic stress and depressive symptoms, and (c) more posttraumatic stress and depressive symptoms at one wave would be associated with more longer-term stressors at subsequent waves.
Method
Participants and Procedure
Participants were part of the 3-wave Galveston Bay Recovery Study, a population-based study of mental health in the after-math of Hurricane Ike (Tracy, Norris, & Galea, 2011). Hurricane Ike made landfall over Galveston, Texas on September 13, 2008, as a Category 2 storm and led to an estimated 3.4 billion dollars in property damage (Federal Emergency Management Agency, 2008). In the current study, adults (aged 18 years or older) who lived in Galveston and Chambers counties in south-eastern Texas at least 1 month prior to the hurricane were recruited. Wave 1 interviews were conducted from November 7, 2008 to March 24, 2009 (2–5 months postdisaster; median date: January 9, 2009); 658 participants were surveyed, representing a baseline response rate of 40%. Participants were reinterviewed twice: 529 of the 658 (80.4%) Wave 1 participants completed the Wave 2 interview between February 6, 2009 and June 29, 2009 (5–9 months postdisaster; median date: April 14, 2009); and 487 of the 658 Wave 1 participants (74.0% overall; 84.6% of those who participated in both Waves 1 and 2) completed the Wave 3 interview between November 19, 2009 and April 13, 2010 (14–18 months postdisaster; median date: December 14, 2009). After the study was described to participants at each time point, oral informed consent was obtained. Institutional review boards of the University of Michigan, Dartmouth College, and Yale University approved the study. In the current study, we included participants who completed all three waves (N = 448).
Measures
Demographic variables
We included a variety of demographic variables as covariates in the analyses based on previous research (e.g., Neria et al., 2008; Norris et al., 2002). We included dummy codes for male gender (48.5%), racial/ethnic minority groups (non-Hispanic Black: 13.6%;Hispanic: 18.5%; and other race: 4.2%), whether the participant was a parent of a child under 18 years old at Wave 1 (34.0%), and Wave 1 marital status (single: 25.1%; divorced, separated, or widowed: 18.3%; married: 56.6% [reference group]). Age was included as a continuous variable (M = 45.76 years, SD = 16.88). Two ordinal variables were included as indicators of socioeconomic status. First, participants reported their highest level of education at Wave 1, from 1 = less than high school to 5 = graduate work (M = 2.68, SD = 1.11). Second participants reported their household income in the year prior to Hurricane Ike at Wave 1, from 1 = less than $10,000 to 7 = $100,000 or more (M = 4.40, SD = 1.96).
Posttraumatic stress
The PTSD Checklist-Specific Version (PCL-S; Blanchard, Jones-Alexander, Buckley, & Forneris, 1996) assessed posttraumatic stress related to Hurricane Ike. Whereas the PCL-S is typically asked in reference to the prior month, the instructions were modified for the current study such that at Wave 1, questions were asked in reference to the period since Hurricane Ike, and at Wave 2 and Wave 3, to the period since the previous interview. The scale included 17 items (e.g., “repeated, disturbing thoughts or memories of Hurricane Ike,” “avoiding activities or situations because they reminded you of Hurricane Ike”) assessing symptoms of PTSD from the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR; American Psychological Association, 2000). Participants rated the extent to which they were bothered by each symptom from 1 = not at all to 5 = extremely. PCL-S scores were created by summing responses to all items, with a possible range of 17–85. The PCL-S has been shown to have excellent internal consistency and substantial agreement with PTSD diagnosis and symptom ratings (e.g., Blanchard et al., 1996). Cronbach’s α for the PCL-S scale ranged from .92 to .96 in the current study (Wave 1: M = 26.52, SD = 12.71, range=17–85; Wave 2: M = 23.17, SD = 9.52, range = 17–82; Wave 3: M = 24.22, SD = 11.13, range = 17–85).
On the PCL-S, participants are classified as having probable PTSD if they rate “moderately” or above one or more re-experiencing symptoms (Criterion B), three or more avoidance symptoms (Criterion C), and two or more arousal symptoms (Criterion D), as well as if they reported feeling terrified or helpless at the time of the event (Criterion A), had symptoms that lasted more than 30 days (Criterion E), and had significant distress or impairment (Criterion F; Weathers, Litz, Herman, Huska, & Keane, 1993); 10.0% of participants met these criteria at Wave 1, 5.6% at Wave 2, and 6.0% at Wave 3.
Depression
The Patient Health Questionnaire-9 (PHQ-9; Kroenke & Spitzer, 2002) assessed past-month symptoms of depression at each wave. Participants were asked whether there was ever a 2-week period during which they were bothered by nine symptom (e.g., “feeling down, depressed, or hopeless,” “feeling tired or having little energy”) and, if so, how often they were bothered, from 0 = not at all to 3 = nearly everyday, and whether this occurred in the prior month. Past-month PHQ-9 scores were created by summing ratings for symptoms reported to have occurred in the past month, with a possible range of 0–27. Previous studies have found the PHQ-9 to have excellent internal consistency, test-retest reliability, and construct validity (e.g., Kroenke, Spitzer, & Williams, 2001). Cronbach’s α for the PHQ-9 scale ranged from .79 to .89 in the current study (Wave 1: M = 1.78, SD = 3.96, range = 0–24; Wave 2: M = 1.64, SD = 3.37, range = 0–23;Wave 3: M = 2.18, SD = 4.52, range = 0–27).
At each time point, participants completed an additional item assessing whether symptoms seemed to occur together. Participants with scale scores of 10 or greater and who indicated that symptoms occurred together were classified as having probable past-month depression, criteria that has been shown to be significantly predictive of a depression diagnosis from a mental health professional (Kroenke et al., 2001); at each wave, 6.3% of participants met these criteria.
Predisaster mental health
Previous research indicates significant associations between pre- and postdisaster psychological symptoms (e.g., Norris et al., 2002). Diagnoses of probable predisaster PTSD and major depression were therefore established at Wave 1 and included as dummy-coded variables. To assess predisaster PTSD, participants indicated whether they had experienced other traumatic events (e.g., rape, car accident) prior to Hurricane Ike. Participants then completed a modified version of the PCL-S in which they rated the extent to which they were ever bothered by symptoms related to the event they considered the “worst”; 10.3% of participants met the afore-mentioned criteria for probable predisaster PTSD based on this assessment.
For predisaster depression, participants completed the PHQ-9 at Wave 1, with items asked in reference to any 2-week period in the participants’ lifetime, and the item assessing whether symptoms seemed to occur together. Additionally, participants indicated their age of onset and if the same as their current age, whether this was prior to Hurricane Ike. Those who met criteria for lifetime depression, and whose age of onset was prior to Hurricane Ike, were coded as having probable predisaster major depression; 17.6% of participants met these criteria.
Immediate stressors
At Wave 1, participants indicated whether they had experienced seven stressors as a result of Hurricane Ike: (a) displacement for over a week, (b) lack of any resource (e.g., food, shelter, electricity) for over a week, (c) loss of or damage to personal property, (d) loss of or damage to sentimental possessions (e.g., photographs), (e) health problem of self or household member, (f) financial loss (including job loss or income decline), and (g) increased relationship demands or problems. A count of affirmative responses was computed. The items were modified from scales used in the aftermath of other disasters, and were used in a population-based study of Hurricane Katrina survivors (Galea, Tracy, Norris, & Coffey, 2008; M = 2.97, SD = 1.61, range = 0–7).
Longer-term stressors
At Waves 2 and 3, participants completed a 12-item stressors inventory (modified from Boardman, Finch, Ellison, Williams, & Jackson, 2001). Participants indicated whether, since the last interview, they had experienced each stressor: (a) mental illness of someone close, (b) parent with problem with drugs or alcohol, (c) other family member with problem with drugs or alcohol, (d) divorce or breakup, (e) lost job, (f) life-threatening physical illness of someone close, (g) seen or heard physical fighting between caregivers, (h) serious illness or injury, (i) serious legal problems, (j) unemployed for at least 3 months, (k) serious financial problems, and (l) problems getting access to adequate health care. A count of affirmative responses was computed. Previous studies have found this scale to be significantly associated with both posttraumatic stress and depression (Beard et al., 2009; Galea et al., 2008; Wave 2: M = .97, SD = 1.42, range = 0–6;Wave 3: M = 1.58, SD = 1.77, range = 0–9).
Data Analysis
As mentioned above, only participants who completed all three waves were included in the study. A series of Bonferroni-corrected t tests and χ2 tests examined differences between completers (n = 448) and noncompleters (n = 210); no significant differences were detected. Among the variables included, nine had missing data: (a) age, (b) marital status, (c) race, (d) predisaster household income, (e) highest level of education, (f) predisaster probable PTSD, (g) predisaster probable depression, (h) Wave 1 posttraumatic stress, and (i) Wave 1 depression. The missing rate ranged from 0.0% to 11.2%, and the overall rate of missingness was 1.6%. We examined differences between participants with complete data (79.0%, n = 354) and participants missing data on any of the variables included in the current study (21.0%, n = 94) using Bonferroni-corrected t tests and χ2 tests. One significant difference was detected: Complete cases had significantly higher education than cases with missing data. Missing data were imputed using the sequential regression imputation method implemented in IVEWARE (Raghunathan, Solenberger, & Van Hoewyk, 2002). Data were imputed based on variables collected prior to or at the same time as the variable with missing data. Five imputed datasets were created, and results represent an average of the five separate analyses with Rubin’s (1987) correction of standard error. Prior to conducting statistical analyses, the distributions of each variable were carefully examined and assumptions of normality were met. Analyses were weighted to account for differential sampling probabilities across the five study strata, probabilities of selection within households, nonresponse, and attrition during the follow-up period. An additional poststratification weight was calculated to account for sociodemographic differences between the sample and the population in Galveston and Chambers counties according to the 2005–2007 American Community Survey (U.S. Census Bureau, 2007). Analyses were conducted in Mplus 6.0 (Muthén & Muthén, 1998–2010) to account for the complex survey design and multiple imputation.
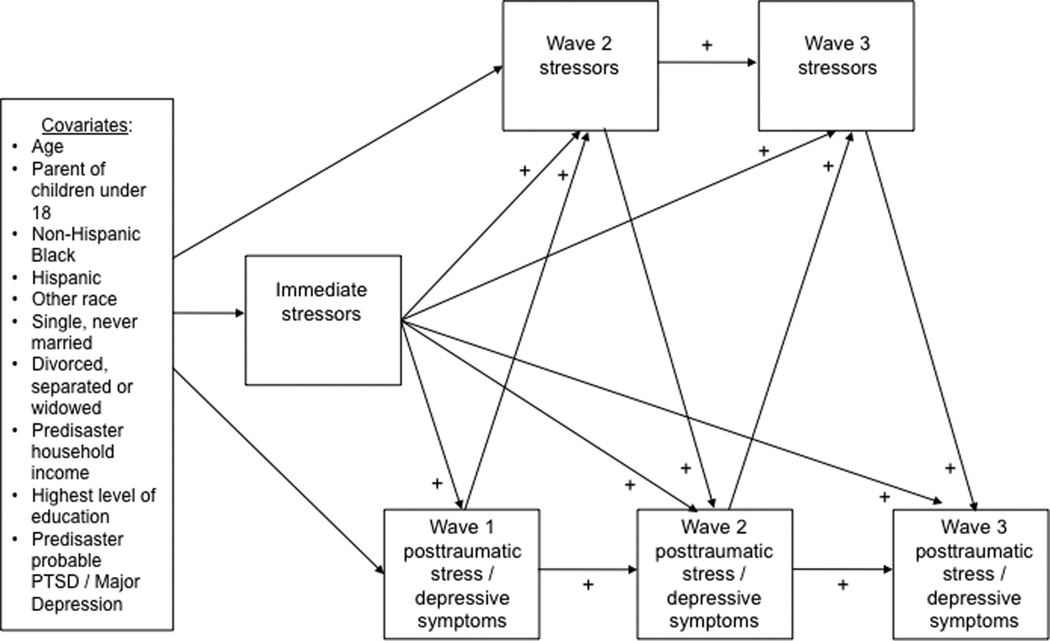
The hypothesized path analytic model is shown in Figure 1. We hypothesized that immediate stressors would be positively associated with posttraumatic stress and depressive symptoms at each time point, and with Wave 2 and Wave 3 stressors. Additionally, we hypothesized that Wave 2 and Wave 3 stressors would be positively associated with Wave 2 and Wave 3 symptoms, respectively, and that Wave 1 and Wave 2 symptoms would be positively associated with Wave 2 and Wave 3 stressors, respectively. We also included autoregressive paths for stressors and symptoms, and demographic covariates and predisaster mental health status variables as predictors of immediate stressors, Wave 1 symptoms, and Wave 2 stressors. Prior to testing the hypothesized model, we conducted bivariate analysis to determine whether relationships between the variables were significant in the expected direction. Next, a path analysis was conducted. Following the recommendations of Hu and Bentler (1998), we set the cutoff of acceptable model fit at <.08 for root mean square error of approximation (RMSEA) and > .90 for comparative fit index (CFI). In cases of poor model fit, modification indices were inspected and models with additional, nonhypothesized paths were tested. Paths with p > .10 were trimmed from final models.
Figure 1.
Hypothesized path analytic model. A plus sign indicates a hypothesized positive relationship; a minus sign indicates a hypothesized negative relationship. Paths from covariates to immediate stressors, Wave 1 posttraumatic stress/depression, and Wave 2 stressors were included.
Results
All of the correlation coefficients corresponding to the hypothesized paths in the model were significant in the expected direction at p < .001 (Table 1).
Table 1.
Means, Standard Deviations, and Zero-Order Correlations Among Variables
| M /% | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Immediate stressors | 2.97 | 1.61 | – | |||||||||||||||
| 2. | Wave 2 stressors | 0.97 | 1.42 | .24*** | – | ||||||||||||||
| 3. | Wave 3 stressors | 1.58 | 1.77 | .31*** | .64*** | – | |||||||||||||
| 4. | Wave 1 posttraumatic stress | 26.52 | 12.71 | .44*** | .21*** | .40*** | – | ||||||||||||
| 5. | Wave 2 posttraumatic stress | 23.17 | 9.52 | .40*** | .30*** | .39*** | .78*** | – | |||||||||||
| 6. | Wave 3 posttraumatic stress | 24.22 | 11.13 | .32*** | .30*** | .50*** | .58*** | .74*** | – | ||||||||||
| 7. | Wave 1 depression | 1.78 | 3.96 | .18*** | .28*** | .45*** | .53*** | .47*** | .40*** | – | |||||||||
| 8. | Wave 2 depression | 1.64 | 3.37 | .17*** | .51*** | .44*** | .39*** | .44*** | .44*** | .52*** | – | ||||||||
| 9. | Wave 3 depression | 2.18 | 4.52 | .22*** | .35*** | .51*** | .48*** | .53*** | .59*** | .64*** | .63*** | – | |||||||
| 10. | Age | 45.76 | 16.88 | .01 | −.01 | −.08 | .02 | .10* | .18*** | .10* | .15** | .16*** | – | ||||||
| 11. | Male | 48.5% | – | .11* | .08 | −.02 | −.13** | −.08 | −.03 | −.13** | −.02 | −.05 | .02 | – | |||||
| 12. | Parent of children < 18 years | 34.0% | – | −.12* | −.06 | −.04 | −.03 | −.03 | −.05 | −.01 | .10* | −.06 | −.39*** | −.14** | – | ||||
| 13. | Non–Hispanic Black | 13.6% | – | .09 | .04 | .23*** | .19*** | .15** | .28*** | .22*** | .15** | .27*** | −.02 | −.16*** | −.03 | – | |||
| 14. | Hispanic | 18.5% | – | .01 | .04 | .02 | .18*** | .21*** | .20*** | .06 | .10* | .06 | −.19*** | .05 | .15** | −.19*** | – | ||
| 15. | Other race | 4.2% | – | −.02 | .23*** | .14** | .02 | −.01 | −.04 | −.03 | .01 | −.04 | −.07 | .03 | .14** | −.08 | −.10* | – | |
| 16. | Married | 56.6% | – | −.05 | −.29*** | −.32*** | −.09 | −.15** | −.24*** | −.16*** | −.18*** | −.19*** | .15** | −.03 | .03 | −.33*** | −.11* | −.14** | – |
| 17. | Single | 25.1% | – | .08 | .26*** | .21*** | −.05 | .02 | .11* | −.05 | .04 | −.02 | −.42*** | .16*** | .01 | .22*** | .07 | .14** | −.66*** |
| 18. | Predisaster household income | 4.40 | 1.96 | −.08 | −.25*** | −.21*** | −.23*** | −.27*** | −.37*** | −.18*** | −.23*** | −.24*** | −.10* | .10* | −.09 | −.26*** | −.30*** | −.12* | .35*** |
| 19. | Level of education | 2.68 | 1.11 | −.06 | −.17*** | −.20*** | −.17*** | −.20*** | −.36*** | −.12* | −.17*** | −.17*** | −.20*** | −.06 | .05 | −.21*** | −.22*** | −.02 | .26*** |
| 20. | Predisaster probable PTSD | 10.3% | – | .04 | .14** | .05 | .09 | −.01 | .05 | .10* | .16*** | .12* | .09 | −.07 | −.05 | −.07 | −.07 | −.06 | .01 |
| 21. | Predisaster probable major depression | 17.6% | – | .12* | .15** | .19*** | .09 | .17*** | .05 | .42*** | .26*** | .35*** | .09 | −.11* | .05 | .01 | −.12* | −.06 | .11* |
Note. Values in bold indicate main paths in hypothesized path analytic model. N = 448. PTSD = posttraumatic stress disorder.
p < .05.
p < .01.
p < .001.
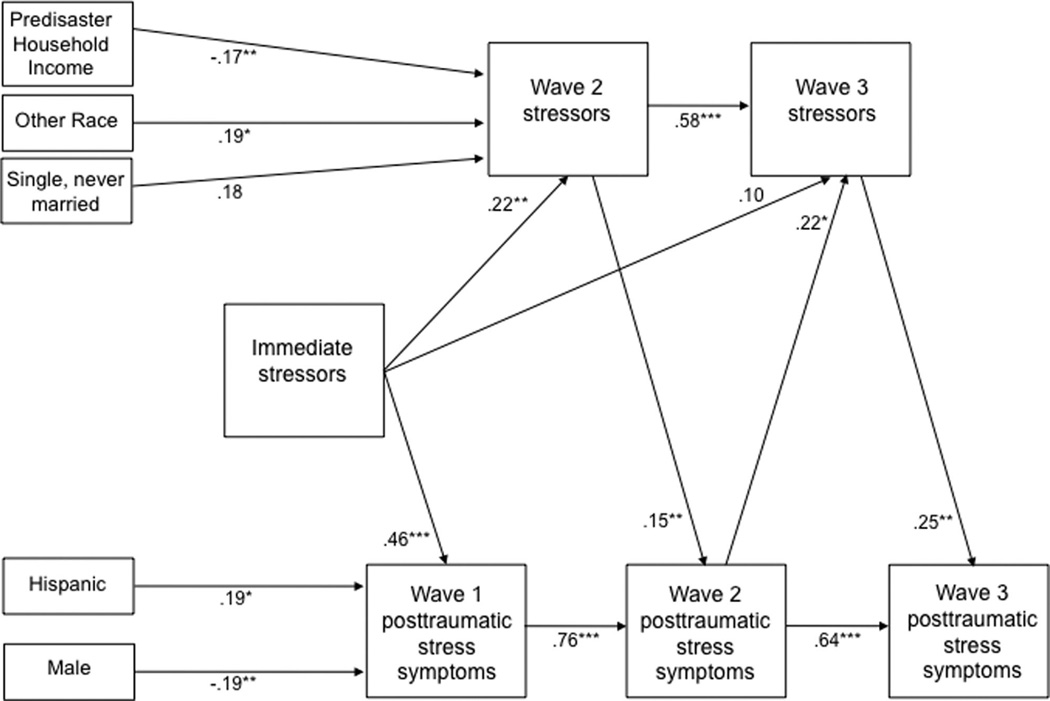
The final model predicting posttraumatic stress is shown in Figure 2. The model had acceptable fit with the data (RMSEA = .04, CFI = .95). The following hypothesized paths were trimmed from the final model (all p > .10): (a) immediate stressors to Wave 2 posttraumatic stress, (b) immediate stressors to Wave 3 posttraumatic stress, and (c) Wave 1 posttraumatic stress to Wave 2 stressors. All other paths were significant in the expected direction, except for the paths from immediate stressors to Wave 3 stressors, which was marginally significant. For the covariates, we found significantly higher Wave 1 posttraumatic stress among female and Hispanic participants, significantly higher Wave 2 stressors among other race and lower predisaster household income participants, and marginally significantly higher Wave 2 stressors among single, never-married participants.
Figure 2.
Final path model predicting postdisaster posttraumatic stress symptoms. Numbers represent standardized path coefficients. N = 448. *p < .05. **p < .01. ***p < .001.
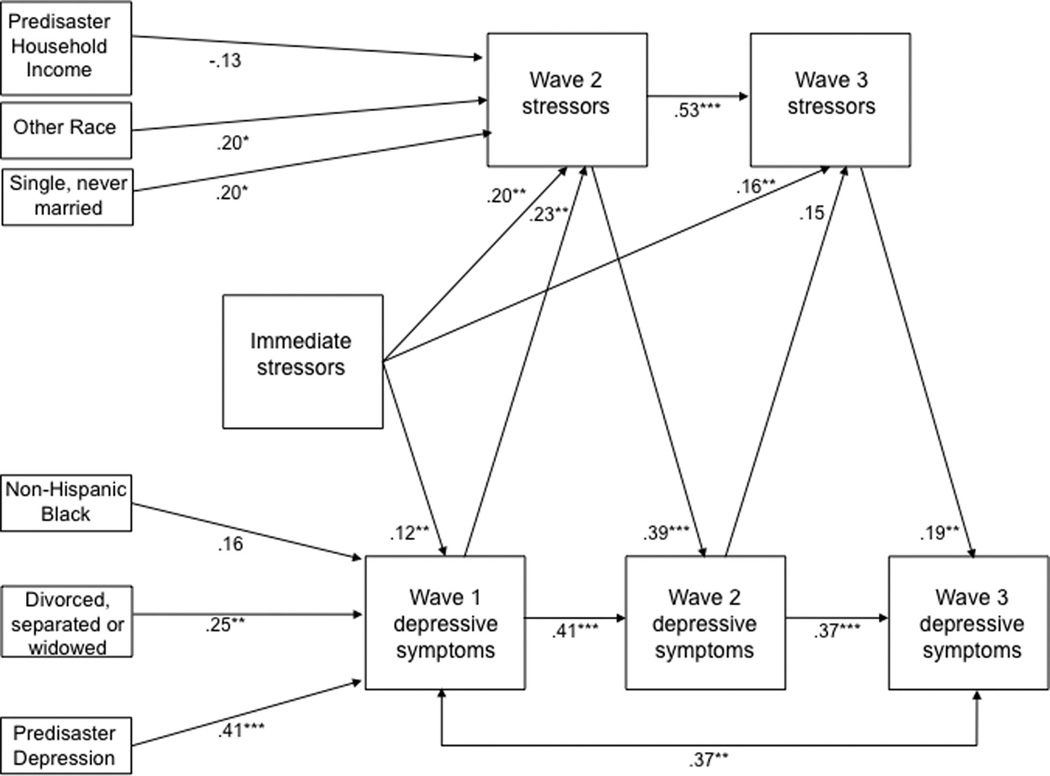
The final model predicting symptoms of depression is shown in Figure 3. The model had acceptable fit with the data (RMSEA = .04, CFI = .92). Inspection of modification led to the addition of path from Wave 1 depression to Wave 3 depression. The following hypothesized paths were trimmed from the final model (all p > .10): (a) immediate stressors to Wave 2 depression, and (b) immediate stressors to Wave 3 depression. All other paths were significant in the expected direction, except for the path from Wave 2 depression to Wave 3 stressors, which was marginally significant. For the covariates, we found significantly higher Wave 1 depression among participants with probable predisaster depression and participants who were divorced, separated, or widowed at baseline, and marginally significantly higher levels among non-Hispanic Black participants. In addition, we found significantly higher Wave 2 stressors among other race, single, never married, and lower predisaster household income participants.
Figure 3.
Final path model predicting postdisaster depressive symptoms. Numbers represent standardized path coefficients. N = 448. *p < .05. **p < .01. ***p < .001.
Discussion
The current study drew on data from a 3-wave population-based study of Hurricane Ike survivors to examine the processes contributing to postdisaster loss spirals and posttraumatic stress and depressive symptoms. The results of path analysis generally supported our hypotheses. First, more stressors endured during the hurricane and its immediate aftermath were associated more stressors at subsequent waves. Second, immediate stressors were positively associated with Wave 1 posttraumatic stress and depressive symptoms, whereas the hypothesized paths from immediate stressors to Wave 2 and Wave 3 symptoms did not reach statistical significance. However, Wave 2 and Wave 3 stressors were positively associated with Wave 2 and Wave 3 symptoms, respectively. Third, we found evidence that posttraumatic stress and depressive symptoms contributed to loss spirals. Whereas the path from Wave 1 posttraumatic stress to Wave 2 stressors did not reach statistical significance, more Wave 2 posttraumatic stress symptoms were associated with more Wave 3 stressors. In contrast, more Wave 1 depressive symptoms were significantly associated with more Wave 2 stressors, and more Wave 2 depressive symptoms were marginally associated with Wave 3 stressors.
Taken together, the results suggest that immediate stressors contribute to longer-term postdisaster psychological symptoms through a complex and dynamic process. Immediate stressors led to disruptions in survivors’ daily lives, as indicated by longer-term stressors. It is likely that some of these stressors stem directly from hurricane-related experiences (e.g., illnesses or injuries) and losses (e.g., financial problems, persistent unemployment). Other longer-term stressors could reflect the indirect and more pervasive toll of disasters on survivors’ and their families’ functioning (e.g., mental illness of someone close, divorce, or break-up).
In this regard, our findings demonstrated the role of postdisaster psychological symptoms in the process of loss spirals. It seems that posttraumatic stress and depressive symptoms perpetuate themselves by leading to more longer-term stressors. Notably, the paths from symptoms to stressors differed between the posttraumatic stress and depressive symptom models, such that between the first two waves, the path from depressive symptoms to stressors was significant, whereas between the second two waves, the path from posttraumatic stress symptoms to stressors was significant. One possibility is that depressive symptoms (e.g., lack of energy and motivation) could hinder a disaster survivors’ ability to take action in addressing immediate stressors thereby turning them into longer-term stressors. In contrast, the effects of posttraumatic stress symptoms on survivors’ daily lives could be more likely to manifest over time. Future research is needed to better understand the potentially different roles of posttraumatic stress and depression in postdisaster loss spirals.
The results of the study were consistent with previous research documenting the paths from immediate to longer-term stressors and from longer-term stressors to postdisaster psychological symptoms separately (e.g., Blaze & Shwalb, 2009; Norris et al., 1999), as well as the few studies exploring them simultaneously (e.g., Smith & Freedy, 2000). An additional contribution of the study was that we also demonstrated paths from symptoms to stressors. Although these paths were supported by previous research and theory, to our knowledge they have not been examined in a disaster context.
Importantly, the significant pathways held when controlling for demographic variables previously associated with postdisaster psychological outcomes. We also controlled for retro-spective assessments of predisaster mental health. Predisaster probable major depressive disorder (MDD) was associated with higher postdisaster depression, whereas predisaster probable posttraumatic stress disorder (PTSD) was not associated with postdisaster posttraumatic stress. It is possible that predisaster MDD is more likely to shape postdisaster psychopathology than predisaster PTSD. An alternative explanation is that assessments of predisaster MDD were more prone to retrospective bias than assessments of predisaster PTSD, thus leading to a relative inflation of the path from predisaster MDD to postdisaster depression. Another possibility is that significant associations would have been detected between predisaster PTSD and postdisaster posttraumatic stress if assessments were not linked to a specific index event. Given these considerations, the findings should be interpreted with caution and replicated in studies with access to predisaster data.
The results of the study have implications for research, policy, and practice. Future research could extend further into the postdisaster period, for example, to determine whether the association between immediate and longer-term stressors holds years after the disaster. Additional psychological outcomes (e.g., generalized anxiety, substance use) could be explored, as could factors that might protect against the pernicious effect of longer-term stressors on psychological outcomes and vice versa (e.g., adaptive coping, mental health service utilization).
The results suggest that policies targeting both postdisaster stressors and psychological symptoms are needed, particularly among survivors who experienced a high degree of immediate stressors. For example, resources that connect survivors with permanent housing options or assist survivors in facilitating repair of their predisaster homes, as well as job training and placement programs for unemployed survivors, would promote longer-term psychological well-being (e.g., Bell, 2008; Jones-DeWeever, 2008). Rapid deployment of postdisaster mental health services and identification of survivors in need would also reduce acute psychological symptoms and their potential contribution to longer-term stressors.
The results also suggest the importance of clinicians’ attunement to the interrelations between longer-term stressors and survivors’ mental health. For example, a behavioral activation approach (Dimidjian, Martell, Addis, & Herman-Dunn, 2008) could address the ways in which psychological symptoms contribute to stressors, and reduce them both through encouragement of active coping. Other interventions could focus more directly on stressors, such as couples and family-based interventions to alleviate relationship tensions and mitigate their effects on mental health (e.g., Jacobson & Christensen, 1998). Clinicians could also forge connections with services that address postdisaster stressors (e.g., those assisting survivors in securing housing and employment), both to facilitate referrals for patients in need and to connect to distressed survivors who might not otherwise seek mental health services.
There are several notable limitations to this study. Although our longer-term stressors scale included a range of experiences that have been associated with postdisaster outcomes, it assumed that each had equal valence. Other measures that take into account the number, frequency, duration, and appraisal of stressors would provide more precise estimates of associations between longer-term stressors and mental health indices. In addition, we excluded other aspects of disaster exposure that could account for psychological outcomes, such as perceived life threat, injuries, and bereavement. The assessments of longer-term stressors and psychological symptoms also occurred at the same time point. Survivors reported on longer-term stressors in reference to the time since the previous interview, but could have been influenced by current psychopathology. In a similar vein, the measure of posttraumatic stress was administered in reference to the time since the prior interview, whereas the measure of depression was administered in reference to the past month, and it is possible that the patterns would have been different had the same timeframe been used for both classes of symptoms. Lastly, as mentioned previously, there also may have been retrospective bias in our assessment of predisaster mental health, especially predisaster MDD.
Despite these limitations, the results suggest that stressors experienced during disasters and their immediate aftermath influence longer-term postdisaster posttraumatic stress and depressive symptoms in two ways. First, they increase the likelihood of subsequent stressors, which are associated with more postdisaster symptoms. Second, they are associated with higher short-term psychological symptoms that perpetuate themselves by leading to contributing longer-term stressors. Interventions and policies that target acute symptoms and postdisaster stressors would reduce the longer-term impact of disasters on mental health.
Acknowledgments
This research was supported by the National Institute of Mental Health (P60MH082598 and T32MH013043).
References
- Amaya-Jackson L, Davidson JR, Hughes DC, Swartz M, Reynolds V, George LK, Blazer DG. Functional impairment and utilization of services associated with posttraumatic stress in the community. Journal of Traumatic Stress. 1999;12:709–724. doi: 10.1023/A:1024781504756. [DOI] [PubMed] [Google Scholar]
- American Psychological Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 2000. text rev. [Google Scholar]
- Beard JR, Cerdá M, Blaney S, Ahem J, Vlahov D, Galea S. Neighborhood characteristics and change in depressive symptoms among older residents of New York City. American Journal of Public Health. 2009;99:1308–1314. doi: 10.2105/AJPH.2007.125104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell H. Case management with displaced survivors of Hurricane Katrina: A case study of one host community. Journal of Social Service Research. 2008;34:15–27. [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behavior Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Blaze JT, Shwalb DW. Resource loss and relocation: A follow-up study of adolescents two years after Hurricane Katrina. Psychological Trauma: Theory, Research, Practice, and Policy. 2009;1:312–322. [Google Scholar]
- Boardman JD, Finch BK, Ellison CG, Williams DR, Jackson JS. Neighborhood disadvantage, stress, and drug use among adults. Journal of Health and Social Behavior. 2001;42:151–165. [PubMed] [Google Scholar]
- Cougle JR, Resnick H, Kilpatrick DG. A prospective examination of PTSD symptoms as risk factors for subsequent exposure to potentially traumatic events among women. Journal of Abnormal Psychology. 2009;118:405–411. doi: 10.1037/a0015370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimidjian S, Martell CR, Addis ME, Herman-Dunn R. Behavioral activation for depression. In: Barlow DH, editor. Clinical handbook of psychological disorders: A step-by-step treatment manual. 4th ed. New York, NY: Guilford Press; 2008. pp. 328–364. [Google Scholar]
- Elliot JR, Pais J. Race, class, and Hurricane Katrina: Social differences in human response to disaster. Social Science Research. 2006;35:295–321. [Google Scholar]
- Federal Emergency Management Agency. Hurricane Ike impact report. 2008 Retrieved from http://www.fema.gov/pdf/hazard/hurricane/2008/ike/impact_report.pdf.
- Galea S, Brewin CR, Gruber M, Jones RT, King DW, King LA, Kessler RC. Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Archives of General Psychiatry. 2007;64:1427–1434. doi: 10.1001/archpsyc.64.12.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Tracy M, Norris F, Coffey SF. Financial and social circumstances and the incidence and course of PTSD in Mississippi during the first two years after Hurricane Katrina. Journal of Traumatic Stress. 2008;21:357–368. doi: 10.1002/jts.20355. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress generation in depression: Reflection on its origins, research, and future directions. Journal of Clinical Psychology. 2006;62:1065–1082. doi: 10.1002/jclp.20293. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE. Conservation of resources: A new attempt at conceptualizing stress. American Psychologist. 1989;44:513–524. doi: 10.1037//0003-066x.44.3.513. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3:424–453. [Google Scholar]
- Jacobson NS, Christensen A. Acceptance and change in couple therapy: A therapist’s guide to transforming relationships. New York, NY: Norton; 1998. [Google Scholar]
- Jones-DeWeever A. Women in the wake of the storm: Examining the post-Katrina realities of the women of New Orleans and the Gulf Coast. Washington, DC: Institute for Women’s Policy Research; 2008. [Google Scholar]
- Kaniasty K, Norris FH. Distinctions that matter: Received social support, perceived social support and social embeddedness after disasters. In: Neria Y, Galea S, Norris F, editors. Mental health consequences of disasters. New York, NY: Cambridge University Press; 2009. pp. 175–200. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Wang PS. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R) Journal of the American Medical Association. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer R. The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals. 2002;32:1–9. Retrieved from http://www.healio.com/psychiatry. [Google Scholar]
- Kroenke K, Spitzer R, Williams J. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe SR, Chan CS, Rhodes JE. Pre-hurricane perceived social support protects against psychological distress: A longitudinal analysis of low-income mothers. Journal of Consulting and Clinical Psychology. 2010;78:551–560. doi: 10.1037/a0018317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus (Version 6.0) [Computer software] Los Angeles, CA: Author; 1998–2010. [Google Scholar]
- Najarian LM, Goenjian AK, Pelcovitz D, Mandel F, Najarian B. The effect of relocation after a natural disaster. Journal of Traumatic Stress. 2001;14:511–526. doi: 10.1023/A:1011108622795. [DOI] [PubMed] [Google Scholar]
- Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: A systematic review. Psychological Medicine. 2008;38:467–480. doi: 10.1017/S0033291707001353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris FH, Perilla JL, Riad JK, Kaniasty K, Lavizzo EA. Stability and change in stress, resources, and psychological distress following natural disaster: Findings from Hurricane Andrew. Anxiety, Stress, and Coping. 1999;12:363–396. doi: 10.1080/10615809908249317. [DOI] [PubMed] [Google Scholar]
- Norris F, Friedman M, Watson P, Byrne C, Diaz E, Kaniasty K. 60,000 disaster victims speak. Part I: An empirical review of the empirical literature, 1981–2001. Psychiatry. 2002;65:207–239. doi: 10.1521/psyc.65.3.207.20173. [DOI] [PubMed] [Google Scholar]
- Paxson C, Fussell E, Rhodes J, Waters M. Five years later: Recovery from post traumatic stress and psychological distress among low-income mothers affected by Hurricane Katrina. Social Science & Medicine. 2012;74:150–157. doi: 10.1016/j.socscimed.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raghunathan TE, Solenberger PW, Van Hoewyk J. IVEware: Imputation and variance estimation software: User guide. Ann Arbor, MI: University of Michigan; 2002. [Google Scholar]
- Rowe CL, La Greca AM, Alexandersson A. Family and individual factors associated with substance involvement and PTS symptoms among adolescents in Greater New Orleans after Hurricane Katrina. Journal of Consulting and Clinical Psychology. 2010;78:806–817. doi: 10.1037/a0020808. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Multiple imputation for non-response in surveys. New York, NY: Wiley; 1987. [Google Scholar]
- Smith BW, Freedy JR. Psychosocial resource loss as a mediator of the effects of flood exposure on psychological distress and physical symptoms. Journal of Traumatic Stress. 2000;13:349–357. doi: 10.1023/A:1007745920466. [DOI] [PubMed] [Google Scholar]
- Tracy M, Norris FH, Galea S. Differences in the determinants of posttraumatic stress disorder and depression after a mass traumatic event. Depression and Anxiety. 2011;28:666–675. doi: 10.1002/da.20838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, Keane T. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the Annual Meeting of the International Society of Traumatic Stress Studies; San Antonio, TX. 1993. Oct, [Google Scholar]
- U.S. Census Bureau. American Community Survey 2005–2007 estimates. 2007 Retrieved from http://www.census.gov/acs/www/data_documentation/data_main/
- Xu J, Liao Q. Prevalence and predictors of posttraumatic growth among adult survivors one year following 2008 Sichuan earthquake. Journal of Affective Disorders. 2011;133:274–280. doi: 10.1016/j.jad.2011.03.034. [DOI] [PubMed] [Google Scholar]