Abstract
Although street-based female sex workers (FSWs) are highly vulnerable to HIV, they often lack access to needed health services and medical care. This paper reports the results of a recently completed randomized intervention trial for FSWs in Miami, Florida, which tested the relative efficacy of two case management interventions that aimed to link underserved FSWs with health services and to reduce risk behaviors for HIV. Participants were recruited using targeted sampling strategies and were randomly assigned to: a Strengths-Based/Professional Only (PO) or a Strengths-Based/Professional-Peer condition (PP). Follow-up data were collected 3 and 6 months post-baseline. Outcome analyses indicated that both intervention groups displayed significant reductions in HIV risk behaviors and significant increases in services utilization; the Professional-Peer condition provided no added benefit. HIV seropositive FSWs responded particularly well to the interventions, suggesting the utility of brief strengths-based case management interventions for this population in future initiatives.
Keywords: female sex workers, HIV interventions, service utilization, peers, drug use
INTRODUCTION
Female sex workers (FSWs) are severely impacted by HIV/AIDS in many parts of the world [1,2]. In low and middle income countries, overall HIV seroprevalence among FSWs is estimated to be 12%, and exceeds 30% in countries with high background prevalence [3]. This concentrated disease burden is attributable to many factors, including extensive high-risk sexual behaviors with multiple partners [4–13], high prevalence of sexually transmitted infections (STIs) [1], and structural dynamics that indirectly exacerbate risk for HIV [3].
Street-based female sex workers are particularly impacted by structural challenges, including poverty and unstable housing, violence, social isolation, stigma, and discrimination [12,14–16]. Owing to the unregulated or criminalized status of sex work in many parts of the world, street sex workers tend to operate informally and are generally without recourse to any type of workplace enforcement or legal protection [17,18]. As a result, street-based FSWs have limited power to negotiate sexual encounters [19], and are more likely to be HIV positive than their venue-based counterparts [20], yet they are often dissuaded from accessing preventive health care, as well as HIV/STI services and treatment [2,3]. For many FSWs, fear of discrimination, arrest, and stigma inhibits health services utilization [21–25].
Despite these challenges, there is a growing body of evidence documenting successful intervention programs for female sex workers in Asia, Mexico, South Africa, Kenya, and elsewhere [26–31]. Randomized trials of behavioral interventions to reduce the transmission of HIV in low- and middle- income countries have reported significant reductions in HIV/STI incidence and unprotected sex behaviors, as well as increases in consistent condom use and HIV testing among FSWs [1,2,29,32–35]. Though neither widely implemented nor evaluated, structural-level and microenterprise interventions for FSWs have also demonstrated initial successes in increasing alternative economic opportunities, reducing reliance on sex work, reducing risk environments, and increasing their power to engage in protected sex [17,36–38].
With few exceptions, however, FSWs in the U.S. have not been a focus of HIV intervention trials, and are a largely understudied population [39]. A resulting irony is that critical prevalence and incidence data on HIV infection among U.S.-based sex workers are generally unavailable [40,41]. Isolated published reports indicate that HIV disease burden among this population is at a level comparable to that observed in the developing world, with 11% seroprevalence noted among FSWs in New York City jails [42] and 25% prevalence documented among drug-involved African American FSWs in South Florida [40]. Published HIV intervention outcomes for U.S.-based FSWs are equally scarce, although one recent randomized trial conducted by the authors demonstrated significant changes in drug use and sexual risk behaviors after exposure to a brief, 2-session peer-delivered intervention [43].
This paper reports the results of a recently completed randomized intervention trial for FSWs in Miami, Florida, which tested the relative efficacy of two case management interventions that aimed to link underserved FSWs with needed health services, and, to reduce risk behaviors for HIV. The intervention focus was informed by prior research, which indicated extremely low levels of services utilization among street-based FSWs, despite myriad health and social problems [14,18]. It was theorized that the inability to access and receive needed health services contributed to the perpetuation of substance abuse, sex work, and HIV risk among this vulnerable population. Linkage with health services was conceived as a mechanism to reduce drug use, reduce women’s dependence on sex work for survival, and ultimately reduce the burden of HIV in this community.
To this end, we implemented a brief strengths-based case management (SBCM) intervention [44] in a highly vulnerable sample of drug-involved street-based FSWs, and compared its’ efficacy relative to a SBCM intervention enhanced by the addition of a peer case manager. SBCM has previously demonstrated efficacy in linking substance abusers with treatment and reducing drug use [44–46]; and linking HIV-positive individuals to care [47,48]; but appears to work best among populations already seeking treatment or those who are less marginalized – stably housed, more educated, non-crack users, non-sex traders, less severe alcohol problems, older age groups, and Latinos compared to African Americans [44,47,48]. The present study targeted a street-based population of African-American FSWs who were disconnected from health services, and who also had very high levels of competing needs. As such, we hypothesized that the addition of a peer case manager would increase the efficaciousness of the SBCM intervention for this high risk group of women. Peer educators have been used successfully in a variety of health promotion initiatives with vulnerable populations, including reducing high risk sexual behaviors among young gay men [49], increasing needle cleaning in injection drug user networks [50], and promoting adherence to antiretroviral therapy among HIV-infected individuals [51]. Our prior work also demonstrated a beneficial impact of peers as HIV educators among street-based FSWs [62]. As such, the overall goal of the study was to examine the value added of the peer in effecting health service linkages and reducing risk for HIV among this highly marginalized population of FSWs.
METHODS
Target Population and Study Eligibility
The target population for this trial was drug-using African American FSWs in Miami-Dade County, Florida. Study inclusion was limited to African American women based on the authors’ prior research, which indicated that African-Americans were nearly two times more likely than sex workers of other racial/ethnic groups to test HIV-positive [12]. Eligible clients were African American women ages 18 to 50 who had: a) traded sex for money or drugs at least 3 times in the past 30 days; and, b) used cocaine, crack, or heroin 3 or more times a week in the past 30 days. Women who reported current participation in a formal substance abuse treatment program were excluded.
Study Recruitment
Participants in the study were located through targeted sampling strategies [52], which are useful for studying hard-to-reach populations. Targeted sampling is a purposeful, systematic sampling method by which specified populations within geographical districts are identified, and detailed plans are constructed to recruit specified numbers of individuals within each of the target areas.
Based on existing indicator data related to sex work activity and information from community key informants, recruitment efforts centered on the primary street sex work areas to the north of downtown Miami, along the main thoroughfares of Biscayne Boulevard (from N.E. 14th St. to N.E. 85th St.), 54th, 62nd and 79th Streets (from N.E. 10th Ave. to N.W. 32nd Ave.), and Miami Avenue (from N.W. 10th St. to N.W. 30th St.). These “strolls” directly overlay the areas of the county with the highest concentration of African American residents, the highest prevalence of HIV, and the highest poverty rates, making them ideal locations for study recruitment [53,54].
Primary recruitment was carried out by professional outreach workers. The outreach staff was female, indigenous to the target recruitment areas, and several members of the team had prior experience conducting outreach for local community service agencies. Female outreach teams recruited from different sections of the primary sex work strolls on an at least weekly basis over the three year study recruitment period. As specific areas became saturated or unproductive (e.g. failing to yield new, eligible recruits), the team rotated to other identified street sex work locations within the target areas. The use of active sex workers as secondary recruiters also broadened our access to less visible sex work locations (e.g. small motels, apartment buildings, parking lots) within the target areas and broadened recruitment efforts to include non-traditional, late-night hours.
Field Site
Based on the study’s targeted sampling plan, the project office was established near two of the major sex work “strolls” in the Miami area. This area was also easily reachable by public transportation, bicycle, or on foot. The project was known in the community as “Women Protecting Women,” because it was designed exclusively for women sex workers and was fully staffed by women.
Study Interventions
Participants were randomly assigned to either: 1) a Strengths-Based/Professional-Only (PO) Condition, in which a professional case manager partnered with the participant to set, plan and achieve goals from a strengths perspective; or, 2) a Strengths-Based/Professional-Peer (PP) Condition in which a team composed of a professional case manager and a recovering addict/former sex worker peer facilitator worked with the participant from a strengths perspective to develop service goals and achieve service linkage.
The strengths approach centers on the identification and utilization of the participants’ own skills and assets as mechanisms for service acquisition [55]. This model promotes the primacy of the client-case manager relationship, and provides an active, assertive form of advocacy for participants [56]. Strengths-Based case management is rooted in the concept that change is best supported through recognition and acceptance of the participant’s current beliefs, rather than direct confrontation that may inhibit the development of a therapeutic relationship. Case managers use non-directive techniques and emphasize the self-efficacy of the participant in goal setting. In line with this approach, intervention goals in the trial reported here were entirely participant-driven. All intervention staff (site manager, case managers, and peers) participated in formal Strengths-Based case management training, led by a licensed clinical social worker with more than two decades of experience in this approach.
Both intervention arms provided the participant with five structured strengths-based case management sessions over an eight week period, and field visits by project staff were offered as needed. The first session emphasized relationship building and engagement, regardless of the participant’s present attitude about linking with treatment or other services. The session included an explanation of the goals and objectives of the intervention, discussion of the participant’s interest in, or hesitancy about, linking with services, and, emphasized the participant’s ability to make appropriate decisions about her own life. Each session involved the use of a contact plan to summarize goals, steps to achieving them, and possible barriers. Active referrals were made at each session for any services desired by the participant. The second session was devoted to the systematic identification of participant strengths as a method for furthering relationship building and establishing the participant’s awareness of her own self-efficacy. The standardized strengths assessment process was oriented to help participants identify skills that would be useful for dealing with barriers to service linkage. The third session centered on barrier identification and a reinforcement of strengths. During this contact case managers became more assertive in helping participants identify multi-layered barriers to linkage and possible solutions. Whereas many of the barriers discussed in early sessions were expected to be of a tangible nature (e.g., lack of stable housing, lack of identification), session three was devoted to the exploration of more subtle barriers that the individual had not verbalized, such as fear of failing in treatment, stigma related to sex work, or lack of social support. The fourth session summarized progress, reviewing strengths that had been identified, barriers that still existed and possible solutions to those barriers. Participants were reminded of the time-limited nature of the intervention and the importance of their ownership of decisions related to health service linkage. The fifth session centered on disengagement, ensuring that the participant had all the information necessary to follow through with treatment or other service linkage at a later time. Case managers worked with participants to create a final contact plan to summarize future steps that the participant might take to facilitate their linkage with needed services. Participants received a $25 stipend for attendance at each intervention session. The provision of incentives was aimed at reducing practical and financial barriers to intervention attendance; this allowed highly marginalized FSWs, many of whom lack access to basic resources and transportation [57], to participate fully in the intervention process without incurring personal expense.
The Professional-Peer Condition followed the same 5 session structure and content described above, with the exception that the peer facilitator participated in the intervention sessions and remained in contact with their cases throughout the entire six month study participation period, providing ongoing support for service linkage. The specific tasks of the peer facilitator included: 1) orienting participants to the project, and engaging the client in the case management process; 2) coordinating appointments with the case manager; 3) operating as an active member of the case management team; 4) participating in the strengths assessment in support of the case manager to establish a comfortable environment for the participant; 5) providing social support for the participant while she and the case manager work on service plans; 6) contacting service locations by telephone and/or field visit; making referral appointments and assisting participants in communicating with referral sites; 7) accompanying participants to appointments as needed to assist and serve as an advocate; and, 8) participating with case manager in sessions, wrap ups, and case reviews of progress and accomplishments.
Study Procedures
Study recruiters made contact with potential participants in various street locations in accordance with the targeted sampling plan. Potential participants were given contact information for the project intervention center, and were asked to participate in telephone screening for eligibility. Those meeting project eligibility requirements were scheduled for appointments at the project intervention center, where they were re-screened. After eligibility was confirmed, informed consent was obtained, followed by saliva drug testing. The baseline interview was then conducted, which took approximately one hour to complete. Participants were paid a $25 stipend upon completion of the baseline interview and received a hygiene kit containing a variety of risk reduction materials.
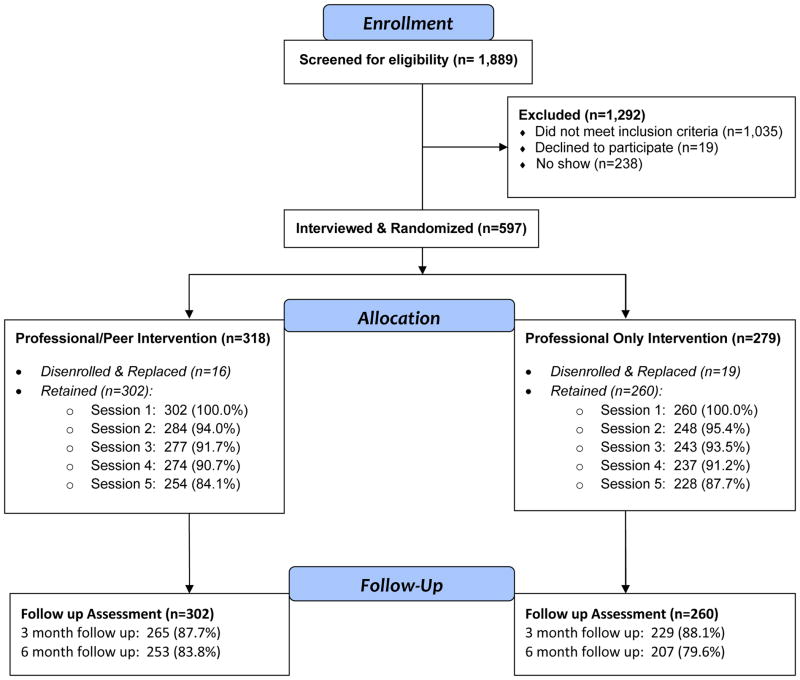
Immediately following the baseline interview participants were randomly assigned to one of the two intervention conditions described above (see Figure 1). The site manager conducted the random assignment procedure using a computerized urn randomization program, which stratified by three factors: HIV status; current homelessness; and, current crack cocaine use. Each of these factors was thought to have potentially significant influence on service linkage and HIV risk, and as such, balance on these covariates across intervention arms was important to achieve. A priori, the allocation ratio was adjusted to assign approximately 250 participants to the Professional-Only condition and 300 to the Professional-Peer condition (clinicaltrials.gov; NCT 00780260). This was done in order to allow sufficient statistical power to examine a priori study hypotheses pertinent only to the Professional-Peer intervention arm (e.g. primary crack cocaine users will benefit proportionately more from the Professional-Peer strengths-based case management condition compared to primary users of other drugs). Our hypotheses were rooted in prior research demonstrating that SBCM worked less well for crack users compared to non-crack users [48]; thus, it was expected that primary crack users would benefit from the addition of the peer case manager.
Figure 1.
Study Flow Diagram
Post-randomization, a small number of participants (n=35) failed to attend the initial session of their assigned intervention. Given that they received no exposure to the study interventions, they were dis-enrolled and replaced. All who attended session one were retained in the trial, regardless of further compliance (see Figure 1). This approach was established a priori in order to examine study outcomes among those actually exposed to one of the two study interventions.
Follow-up assessments were conducted at 3 and 6 months post-baseline. Participants were paid a $25 stipend upon completion of each interview. All project staff completed the requirements for National Institutes of Health (NIH) web-based certification for protection of human subjects. Study protocols were approved by the University of Delaware’s (predecessor institution) and Nova Southeastern University Institutional Review Boards. A Certificate of Confidentiality from the National Institutes of Health was also obtained.
Data Collection and Measures
Trained female interviewers conducted computer-assisted personal interviews (CAPI). The Global Appraisal of Individual Needs (GAIN, v. 5.4; [58]) was the primary component of the standardized baseline and follow-up assessments. The GAIN captures information on demographics, homelessness, physical and mental health status, services utilization, violence, substance use, and sexual risk behaviors.
Demographic information gathered on study participants included age, level of education, and health insurance status. In addition, housing status was assessed with one item: When was the last time, if ever, you considered yourself to be homeless? This variable was dichotomized to “within the past 90 days” or “not within the past 90 days.”
Given the vulnerabilities of the sample, we also examined the prevalence of substance dependence, violent victimization, mental health problems, and HIV infection.
Substance Dependence
Dependence was assessed using the TCU Drug Screen II [59], which consists of nine items measuring past year drug problem severity. Endorsement of three or more items (e.g. using more or longer than intended, using in unsafe situations) approximates DSM-IV-R criteria for dependence [59]. The alpha reliability coefficient for the TCU Drug Screen was 0.8.
Violence
Participants answered four dichotomous (yes/no) items measuring lifetime physical, sexual, and emotional abuse. Recent violence was measured by 11 items of past 90 day violent episodes (including physical and sexual assault) by paying partners or other perpetrators. These were restructured into a dichotomous variable indicating the presence or absence of any violence in the specified time period.
Mental health
Participants were asked “When was the last time, if ever, your life was significantly disturbed by nerve, mental or psychological problems?” This variable was dichotomized to “within the past 90 days” or not within the 90 day period prior to interview, in order to correspond to the 90 day measurement window of other descriptive study variables.
HIV Status
Participants responded to a single item “What was the result of your last HIV test?” At baseline, twenty eight participants did not respond to this item. Using imputation from HIV status data reported at follow-up (e.g. from a report of sero-negative status at either follow-up point we imputed baseline sero-negative status), only three participants remained missing on this item.
Outcome Measures
The study was designed to recruit a sample of 550 participants, and assumed 15% attrition over the 6 month study period. Using an α= .05 level of significance, the study had .80 power to detect a relative difference between intervention groups of 11% or more. Outcome measures for this study were of two types: 1) HIV risk reduction outcomes, assessed by temporal changes in: days of alcohol use; days of crack cocaine use; numbers of unprotected vaginal sex acts; and, numbers of male sexual partners; and, 2) service utilization outcomes, assessed by temporal changes in: participation in self-help for substance problems; HIV testing; medical care access; and, HIV care.
HIV Risk Outcomes
Substance Use
Detailed substance use histories were collected that included current (past 90 day) use of alcohol and a variety of illicit substances (including crack and powder cocaine, heroin, and methamphetamine) as well as prescription drugs used non-medically (i.e. when was the last time, if ever, you used prescription painkillers without a prescription?). For each substance endorsed, participants reported days of use during the past 90 day period. As expected, alcohol and crack cocaine were by far the most prevalent drugs in the sample, endorsed by 88.4% and 70.8%, of participants, respectively, in the past 90 days. Alcohol and crack were examined as primary outcomes given their elevated prevalence in the sample; in addition, our focus on crack cocaine was driven by the distinctive constellation of risk factors that often accompanies its use among FSWs (including homelessness, HIV-positive status, and unprotected sexual behavior [60]), which is especially pertinent when examining HIV transmission/acquisition risk. We assessed changes in the number of days using alcohol and crack cocaine at each wave.
Sexual Risk Behaviors
Sexual behavior measures at each contact included total counts of past 90 day vaginal sex, counts of protected and unprotected vaginal sex, and numbers of male sexual partners, both paying and non-paying. We assessed changes in numbers of male sexual partners and numbers of unprotected vaginal sex acts across waves.
Service Utilization Outcomes
Self-help
This study examined participation in diverse treatment modalities over time, including self-help groups (AA/NA/CA) and formal residential/outpatient psychosocial treatment programs. For the present analysis, we limited our examination to self-help participation due to the fact that study eligibility criteria prohibited formal substance abuse treatment participation at baseline, and as such, effect sizes could not be calculated. Admission to formal substance abuse treatment was significantly correlated with participation in addiction self-help groups at 6 month follow-up (r=.45; p<.001); as such, we examined self-help participation as a proxy for exposure to both formal and informal treatment services. At each wave, participation in self-help for substance use problems was assessed by the following item: “During the past 90 days, on how many days have you attended one or more self-help groups meetings (such as AA, NA, CA)?”
HIV testing
Participants were asked a single item “When was your last HIV test for which you received the results?” We calculated the time elapsed since the last HIV test relative to the baseline and follow-up interview dates, and dichotomized the resulting variable as “HIV tested in the prior 3 months,” yes or no. We assessed changes in HIV testing uptake at each data collection wave for seronegative participants.
Regular source of medical care
Participants responded to one item designed to measure connection to the health care system, “Do you have a physician who you consider to be your doctor or a clinic you consider your regular source of medical care?” Temporal changes in care access were assessed at each wave.
HIV treatment
At each interview point, HIV positive participants were asked “Are you currently receiving medical care for your HIV infection?” We examined changes in uptake of HIV treatment at each wave.
Data Analysis
Study participants who were randomized but subsequently failed to receive at least one treatment exposure were excluded and replaced; as such, our analysis was guided by a modified intent to treat approach. Study recruitment began in May, 2007, and through June 2010, 562 eligible clients had been randomized and retained in the study. Follow-up interviews were completed in January, 2011. Outcomes analyses included all of the data available for each follow-up wave. For baseline to three month outcomes, there were 494 cases available for analysis; and for baseline to 6 months, 460 cases (see Figure 1).
Data from the interview questionnaires were analyzed using Stata/SE 12.1 for Windows. Descriptive statistics were calculated to describe the baseline sample by intervention condition in terms of demographics; HIV serostatus; past 90 day substance use and past year substance dependence; sexual risk behaviors; mental distress; and victimization history.
The initial step in the outcome analysis was to explore the potential for differential attrition by examining the baseline characteristics of those retained in the study versus those lost to follow-up. In this regard, we compared the baseline characteristics of women who completed the 6 month follow-up assessment and their lost to follow-up counterparts using t-test and chi-square comparisons. These analyses indicated that follow-up completers: were slightly older on average than non-completers; had higher baseline crack cocaine use than non-completers; were less likely to be homeless than non-completers; and were more likely to be HIV positive than non-completers. Importantly, however, no significant differences were noted on primary outcomes (services utilization, drug use, sexual risk behaviors) between participants retained in the study and those lost to follow-up.
All of the continuous level outcome measures (days of alcohol use, days of crack use, number of sexual partners, times unprotected vaginal sex, days in self-help) had skewed distributions; as such, these measures were log transformed for the longitudinal analyses. Baseline differences and longitudinal effect sizes for these measures are reported for the log-transformed measures. Binary level outcomes (HIV testing, regular source of medical care, HIV treatment) were not transformed.
To examine the extent of change over time in the eight primary and secondary outcomes, we constructed multilevel non-linear growth models (MLM) for repeated measures, controlling for intervention group, and intervention group * time interaction, age, age * time interaction, HIV serostatus, HIV serostatus * time interaction, homeless status, and homeless status* time interaction. We included age, HIV status, housing status and their respective interactions with time as covariates in the MLMs as prior research among FSWs has associated these factors with differing levels of HIV risk [12,61]. Models were centered using the mean age of the sample. These models make use of all available measurement points, and quantify the slope and rate of the change curves at the two follow-up points. In addition to differences in behavior change by intervention condition, the models indicate whether there were significant differences in outcomes and rates of behavior change by demographic variables (e.g., age, HIV serostatus). We also report outcome results within study conditions, including the Cohen’s d effect size statistic and related 95% confidence intervals. For binary outcomes, effect sizes were calculated by converting the odds ratios to Cohen’s d [62].
RESULTS
Table I presents the demographic and health characteristics of the sample at baseline, compared across intervention groups. As expected, the sample reported very high levels of health and social problems. More than half (54.8%) reported homelessness in the past 90 days, and a substantial proportion (41.1%) reported violent victimization in the same time period. Substance use problems were prevalent, with 90.6% of the sample meeting criteria for past year dependence. High levels of current health problems were endorsed by the sample of FSWs as well, with 59.4% reporting significant mental health dysfunction in the past 90 days. Limited access to health services was indicated by low rates of insurance (33%), and significant proportions without a regular source of healthcare (43%). Study randomization procedures appeared to function well, with minimal differences between intervention groups on virtually all demographic, drug use, and health measures. The exception was length of sex work history, with women in the Professional/Peer intervention reporting on average 1.7 additional years in sex work compared to their counterparts in the Professional Only intervention (p=.03).
Table I.
Baseline Sample Characteristics by Intervention Group, N=562
| Prof/Peer | (N=302) | Prof Only | (N=260) | Chi-square or t-statistic | P | |
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Demographics | ||||||
| Age, mean (SD) | 39.3 | (8.6) | 39.3 | (8.4) | −0.07 | 0.94 |
| Homeless in past 90 days, n % | 164 | 54.3 | 144 | 55.4 | 0.07 | 0.79 |
| Less than HS education, n % | 162 | 53.6 | 130 | 50.0 | 0.74 | 0.39 |
| Has a regular doctor/source of care, n % | 177 | 58.6 | 145 | 55.8 | 0.46 | 0.49 |
| Has health insurancea, n % | 97 | 32.1 | 89 | 34.4 | 0.32 | 0.57 |
| Substance Use | ||||||
| Days using alcohol, past 90, mean (SD) | 43.8 | (35.4) | 46.5 | (34.0) | −0.89 | 0.37 |
| Days using crack, past 90, mean (SD) | 44.2 | (38.1) | 47.4 | (36.7) | −0.99 | 0.32 |
| DSM substance dependence, n % | 273 | 90.4 | 236 | 90.8 | 0.02 | 0.88 |
| Prior treatment admissionsa, mean (SD) | 2.2 | (3.9) | 2.1 | (3.8) | 0.33 | 0.74 |
| Sexual behaviors | ||||||
| 90 day paying partners, mean (SD) | 20.6 | (46.7) | 17.2 | (32.9) | 0.98 | 0.33 |
| Years in sex workb, mean (SD) | 15.4 | (9.2) | 13.7 | (9.2) | 2.21 | 0.03 |
| 90 day unprotected vaginal sexc, n % | 153 | 51.5 | 117 | 45.3 | 2.10 | 0.15 |
| 90 day unprotected oral sexd, n % | 163 | 63.4 | 127 | 60.5 | 0.43 | 0.51 |
| Health factors | ||||||
| Lifetime abuse history, n % | 264 | 87.4 | 230 | 88.5 | 0.14 | 0.71 |
| 90 day violencea, n % | 127 | 42.2 | 103 | 39.6 | 0.38 | 0.54 |
| 90 day mental health problemsa, n% | 177 | 58.8 | 157 | 60.4 | 0.15 | 0.70 |
| HIV-positivee, n % | 50 | 16.6 | 52 | 20.2 | 1.26 | 0.26 |
Note:
n=561;
n=560;
n=555 – 7 participants did not engage in vaginal sex;
n=467 – 95 participants did not engage in oral sex;
n=559 – 3 participants had missing data.
Study Outcomes
Table II displays the results of the MLMs of longitudinal changes in the outcome measures, controlling for intervention group, age, HIV serostatus, homelessness, and their interactions with time. Results for the continuous outcome measures are displayed on the first page of the table, followed by dichotomous outcomes on page 2. The observed decrease in days of crack use was significant at the p<.001 level for the entire sample of FSWs. There was a significant difference in crack use frequency by age at baseline, with 10% higher crack use for every year of additional age (p<.001); older women also decreased their crack use to a greater extent over time, an additional 3% reduction was observed at each follow-up point (p<.001). HIV status also indicated a significant effect over time, with HIV positive FSWs demonstrating a 25% greater reduction in crack use frequency over time compared to HIV negatives (p<.05). There was no difference by intervention group or homeless status in the rate of change for crack cocaine use over time.
Table II.
| Multilevel model of longitudinal change in past 90 day outcomes (log-transformed) (N=559)
| ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Column | 1 | 2 | 3 | 4 | 5 | |||||
|
| ||||||||||
| Variable | Days of crack use | Days of alcohol use | Number of sex partners | Unprotected vaginal sex times | Days in self-help | |||||
| Estimate | S.E. | Estimate | S.E. | Estimate | S.E. | Estimate | S.E. | Estimate | S.E. | |
| Fixed Effects: | ||||||||||
| Intercept | 2.85† | .12 | 3.09† | .12 | 2.16† | .07 | 1.30† | .11 | .36† | .09 |
| Time | −.98† | .07 | −.91† | .07 | −.71† | .05 | −.14 | .08 | .47† | .06 |
| Group (ref. prof. only) | −.19 | .14 | −.18 | .14 | .10 | .08 | .17 | .12 | .08 | .10 |
| Group* Time | .11 | .08 | .12 | .08 | −.04 | .05 | −.06 | .08 | −.09 | .06 |
| Age | .10† | .01 | .01 | .01 | −.01** | .00 | .01 | .01 | .00 | .01 |
| Age* Time | −.03† | .00 | −.01 | .00 | .01* | .00 | −.02† | .01 | .00 | .00 |
| HIV status (ref.neg) | .18 | .19 | −.39** | .18 | .01 | .10 | −.30 | .16 | .12 | .14 |
| HIVstatus* Time | −.25* | .10 | −.05 | .10 | −.14* | .07 | −.25* | .11 | −.02 | .08 |
| Homeless (ref. homeless) | −.28 | .14 | .11 | .14 | −.21** | .08 | −.04 | .13 | −.05 | .11 |
| Homeless* Time | .12 | .08 | .06 | .08 | .08 | .05 | .14 | .09 | −.20** | .06 |
| Random Variance: | ||||||||||
| Intercept | 1.49† | .13 | 1.24† | .11 | .28† | .03 | .65† | .08 | .68† | .06 |
| Residual | 1.51† | .07 | 1.51† | .07 | .65† | .03 | 1.74† | .08 | .98† | .04 |
| Multilevel model of longitudinal change in dichotomous past 90 day outcomes (N=559)
| ||||||
|---|---|---|---|---|---|---|
| Column | 1 | 2 | 3 | |||
|
| ||||||
| Variable | HIV Testinga | HIV Careb | Regular Source of Medical Care | |||
| OR | S.E. | OR | S.E. | OR | S.E | |
| Fixed Effects: | ||||||
| Intercept | .78 | .14 | 1.25 | .81 | .47** | .13 |
| Time | 1.49* | .25 | 2.61 | 1.86 | 3.37† | .85 |
| Group (ref. prof. only) | .89 | .19 | 2.57 | 1.77 | 1.42 | .47 |
| Group* time | 1.10 | .21 | .83 | .52 | 1.07 | .27 |
| Age | .99 | .01 | 1.01 | .05 | 1.00 | .02 |
| Age* Time | .97** | .01 | 1.04 | .05 | .99 | .02 |
| HIV status (ref.neg) | 23.02† | 13.34 | ||||
| HIV status* Time | 1.91 | .99 | ||||
| Homeless (ref. homeless) | .61* | .14 | 5.79* | 4.19 | 5.88† | 2.09 |
| Homeless* Time | 1.14 | .22 | .95 | .62 | .57* | .15 |
| Random Variance: | ||||||
| Intercept | .95 | .18 | 1.54 | .56 | 2.43* | .27 |
| Linear slope (Time) | .75 | .23 | 1.12 | .74 | 1.16 | .32 |
Note. SE=standard error;
All parameter entries are restricted maximum likelihood estimates fitted using Stata/SE12.1 xtmixed
p=<.05;
p<.01;
p<.001
All parameter entries are restricted maximum likelihood estimates fitted using Stata/SE12.1 xtmelogit
p=<.05;
p<.01;
p<.001;
Only HIV negative participants at baseline were included in this analysis.
Only HIV positive participants at baseline were included in this analysis.
Alcohol use days (column 2) displayed a significant temporal decrease at the p<.001 level for the entire sample. Baseline HIV status also had a significant effect, with HIV positive FSWs 39% lower on alcohol use at study entry compared to HIV negative women (p<.01). There was no difference by intervention group, age, HIV status or homeless status in the rate of change for alcohol use over time.
Sexual risk behavior outcomes are shown in the third and fourth columns of Table II. There was a significant reduction in the number of male sexual partners over time (p<.001), and small age effects were also present both at baseline and over time. HIV status had a significant impact on change over time, with HIV positive FSWs reporting a 14% greater reduction in the number of sexual partners compared to HIV negatives. There was no difference by intervention group or homeless status in the rate of change for numbers of sexual partners over time, though non-homeless FSWs reported significantly fewer sexual partners at baseline (p <.01). For unprotected vaginal sex frequency (shown in column 4), neither intervention group nor time reached statistical significance. There was a significant effect of HIV status, with HIV positive FSWs decreasing their unprotected sex frequency 25% more than HIV negatives.
Column 5 displays the first service utilization outcome, specifically, frequency of participation in AA/NA/CA. Time was significant for the entire sample, with a 47% increase observed in self-help attendance days (p<.001). Housing status also predicted frequency of self-help attendance over time, with homeless FSWs increasing their participation 20% more than their non-homeless counterparts (p<.01). No significant differences in self-help participation between intervention conditions were noted.
As noted above, the second page of Table II displays the MLM results for the dichotomous outcomes. Column 1 presents the results for past 90 day participation in HIV testing. Time was significant for the entire sample, with 1.49 times higher odds of HIV testing observed at follow-up (p<.05). Housing status predicted testing behavior at baseline, with lower odds of recent testing among non-homeless FSWs (p<.05), but homelessness was unrelated to uptake of testing over time. Age was associated with HIV testing over time, with older women displaying lower odds of testing uptake at follow-up (p<.01). No significant differences were detected in HIV testing between intervention conditions. Column 2 displays the results for HIV care among seropositive FSWs. For this outcome, no significant changes were observed over time, though at baseline non-homeless FSWs had nearly 6 times higher odds of being in current medical care for HIV infection (p<.05). Finally, column 3 contains the results for having a regular source of medical care. Time was significant for the entire sample, with 3.37 times higher odds of access to a regular source of care at follow-up (p<.001). At baseline, both housing stability and HIV seropositive status were significantly associated with higher odds of having a regular source of medical care. No significant differences were detected in access to a regular source of medical care between intervention conditions.
Wave by wave changes in the mean values of continuous-level outcomes and prevalence of dichotomous outcomes are shown in Table III. Effect sizes for the changes between baseline and 6 month follow-up by intervention group are also displayed in Table III.
Table III.
| Baseline to 6 month effect sizes for HIV risk and service linkage outcomes (continuous outcomes)
| |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| BL | 3 Mo FU | 6 Mo. FU | BL-6 Mo | p | Effect Size1 | CI for E.S. Difference | |||||
| Mean (sd) | Mean (sd) | Mean (sd) | Mean Difference | Lower | Upper | ||||||
| Days of crack use | |||||||||||
| Professional Only (n=207): | 50.51 | 36.03 | 18.62 | 30.95 | 15.22 | 29.38 | 35.29 | <.01 | 1.05 | 0.85 | 1.26 |
| Professional/Peer (n=253): | 44.79 | 37.77 | 18.26 | 31.19 | 13.87 | 28.11 | 30.92 | <.01 | 0.92 | 0.73 | 1.10 |
| Days of alcohol use | |||||||||||
| Professional Only (n=207): | 47.25 | 34.57 | 18.77 | 28.65 | 17.44 | 27.88 | 29.81 | <.01 | 0.94 | 0.73 | 1.14 |
| Professional/Peer (n=253): | 44.53 | 35.39 | 20.54 | 30.29 | 16.96 | 27.48 | 27.57 | <.01 | 0.87 | 0.68 | 1.05 |
| Number of sex partners | |||||||||||
| Professional Only (n=207): | 18.41 | 34.72 | 5.61 | 22.87 | 3.60 | 19.27 | 14.81 | <.01 | 1.17 | 0.96 | 1.38 |
| Professional/Peer (n=253): | 21.68 | 47.83 | 3.58 | 10.31 | 3.53 | 11.34 | 18.15 | <.01 | 1.18 | 1.00 | 1.38 |
| Unprotected vag. sex times | |||||||||||
| Professional Only (n=207): | 18.49 | 51.41 | 9.81 | 25.09 | 10.54 | 25.75 | 7.95 | .03 | 0.15 | −0.03 | 0.36 |
| Professional/Peer (n=251): | 17.35 | 38.77 | 12.58 | 33.52 | 12.80 | 30.53 | 4.55 | .01 | 0.18 | 0.01 | 0.36 |
| Days in self-help | |||||||||||
| Professional Only (n=207): | 1.29 | 5.98 | 9.35 | 21.78 | 9.17 | 20.28 | −7.88 | <.01 | −0.48 | −0.67 | −0.28 |
| Professional/Peer (n=253): | 2.40 | 9.77 | 9.37 | 21.53 | 11.17 | 24.39 | −8.77 | <.01 | −0.39 | −0.55 | −0.20 |
| Baseline to 6 month effect sizes for HIV risk and service linkage outcomes (dichotomous outcomes)
| |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| BL | 3 Mo FU | 6 Mo. FU | BL-6 Mo Difference | p | Effect Size | CI for E.S. Difference | |||||
| n | % | n | % | n | % | Lower | Upper | ||||
| HIV testing2 | |||||||||||
| Professional Only (n=154): | 59 | 38.3 | 89 | 57.8 | 79 | 51.3 | 13.0% | .02 | −0.33 | −0.62 | −0.04 |
| Professional/Peer (n=195): | 61 | 31.3 | 111 | 56.9 | 99 | 50.8 | 19.5% | <.01 | −0.54 | −0.83 | −0.27 |
| Regular source of medical care | |||||||||||
| Professional Only (n=207): | 117 | 56.5 | 135 | 65.2 | 152 | 73.4 | 16.9% | <.01 | −0.75 | −1.16 | −0.39 |
| Professional/Peer: (n=253): | 152 | 60.1 | 186 | 73.5 | 195 | 77.1 | 17.0% | <.01 | −0.78 | −1.14 | −0.45 |
| HIV Care3 | |||||||||||
| Professional Only (n=43): | 32 | 74.4 | 36 | 83.7 | 37 | 86.0 | 11.6% | .18 | −0.69 | −1.96 | 0.22 |
| Professional/Peer (n=43): | 34 | 79.1 | 37 | 86.0 | 37 | 86.0 | 6.9% | .51 | −0.38 | −1.39 | 0.47 |
Effect Size (Cohen’s d) and related 95% confidence intervals are for log-transformed measures
HIV testing includes only baseline seronegative participants;
HIV care includes only baseline seropositive participants.
Effect sizes were large across several outcomes, including days of alcohol use (0.94 in the Professional group vs. 0.87 in the Professional/Peer group) crack use (1.05 vs. 0.92), numbers of sexual partners (1.17 vs. 1.18), and having a regular source of medical care (−0.75 vs. −0.78). Effect sizes were moderate for other service utilization outcomes, including days in self help (−0.48 vs. −0.39), HIV testing (−0.33 vs. −0.54), and HIV care (−0.69 vs. −0.38). A small effect was detected for unprotected sex in both groups (0.15 vs. 0.18); however, the confidence interval for the effect size estimate in the Professional Only condition contains 0. Thus, we cannot rule out that the true effect is zero.
DISCUSSION
This randomized trial documented that participation in a SBCM intervention produced significant changes in HIV risk behavior and service utilization outcomes among a sample of highly vulnerable drug-involved FSWs. Although SBCM has been implemented successfully with drug abusing populations in a variety of settings, this approach has been utilized almost exclusively among individuals already seeking treatment or other services, rather than among street-based drug users who have not initiated service contact [44,63,64]. As such, the effort reported here is unique in its application of SBCM to a population that is largely disconnected from formal health care systems and confronted by multiple and layered barriers that impede even initial steps toward service seeking. Within this context, the demonstration of strong and significant pre-post intervention effects indicates that SBCM is a viable and useful approach to intervention with marginalized street-based FSWs. The high intervention attendance and study retention rates we achieved also support the acceptability of the SBCM approach to FSWs.
Despite the positive impact demonstrated by the SBCM interventions overall, significant differences by intervention condition (Professional Only vs. Professional/Peer) were largely absent. Although we hypothesized that the addition of a peer case manager to the intervention team would produce robust differences in outcomes, it is not entirely unexpected that SBCM alone produced significant pre-post intervention effects. Brief SBCM has been proven efficacious as an intervention for effecting linkages among treatment seekers in both central intake units and needle exchange programs [44,65]. Within the context of this strong intervention, the inclusion of peer case managers appeared to provide no added benefit for risk reduction or services utilization among our sample of FSWs. This study adds to the literature on peer-based HIV interventions, which have shown mixed results [66]. HIV system navigation approaches have demonstrated positive effects of peer health navigators, including eliminating barriers to HIV treatment and improving HIV primary medical care engagement and retention [67], as well as improving engagement of the most hard to reach patients [68]. In contrast, RCTs testing peer intervention models relative to controls have shown no added benefit on ART adherence, viral load, or access to care among HIV infected patients [69,70]. This body of findings suggests that peer-driven approaches have potential utility for HIV-related interventions, but are not a panacea; the utility of peer-based activities may be selective, fitting better with specific intervention structures, intensities, tasks, and goals. Clearly these are empirical questions; further research is warranted to identify the most productive avenues for peer contributions to HIV prevention/interventions.
In our outcome models, we demonstrated that age, housing stability, and HIV status are important covariates impacting both baseline level of risk, as well as change over time. In this regard, HIV status displayed a strong and consistent association with change over time that warrants mentioning. On three of the four risk behavior outcomes examined (days of crack use, number of sex partners, and unprotected vaginal sex times) baseline HIV positive status was associated with significantly greater risk reductions over time, ranging from 14% to 25% by outcome. Importantly, these were not newly diagnosed FSWs, as status was determined by baseline self-report and diagnosis was typically many years prior. As such, this study documents that exposure to a brief SBCM intervention can be an important tool for engaging or re-engaging HIV positive FSWs who remain entrenched in risky, street-based lifestyles. Interestingly, the successful reduction of risk behaviors also bears out the hypothesis that indirect intervention approaches can be efficacious; this study documents that reducing service barriers and affording health care access does have a measurable impact on individuals’ drug use, sexual risk behaviors, and HIV-related services utilization. As such, SBCM should be considered as a potential component of combination behavioral and biomedical prevention/intervention approaches for highly vulnerable FSWs going forward.
Limitations
This study has limitations which should be noted. First, although study data were gathered from a large sample of FSWs, those who participated are likely not representative of all street-based sex workers in Miami. Recruitment was limited to drug-involved African American women, and targeted specific geographic areas with visible indicators of drug use and sex work. As well, the focus on informal, unregulated street sex work locations likely yielded a sample very much different from venue-based sex workers, and as a consequence generalizability to other sex worker populations is cautioned. An additional limitation involves the reliance on self-report data and the potential for reporting biases. The existing evidence for the validity of self-reported health services utilization is mixed; some studies indicate high levels of correspondence between self-report and medical record data, while others document fairly large discrepancies [71–73]. We acknowledge that reliance on self-report behavioral measures is not ideal, as both recall problems and social desirability can lead to response bias. To lessen recall problems, our follow-up data collection was limited to 90 day reporting, which is more accurate than periods of longer duration [72]. Care was taken to reduce the potential for socially desirable reporting in outcomes, as there was complete separation of interviewer and case manager/peer roles; participants were assured that their interview data were not available to intervention staff, and interview staff were likewise unaware of intervention session content. Nevertheless, this limitation warrants attention in the interpretation of results. As a final point, there were specific weaknesses in the study design that should be mentioned. First, the lack of a true control group precluded examination of potential enrollment or assessment effects on changes in risk behavior and services utilization over time. In addition, our modified intent to treat design limited our outcome analysis to those participants receiving at least one treatment exposure.
CONCLUSION
The data in this study document the importance of pursuing HIV intervention initiatives among FSWs in the United States, who exhibit prevalence levels in line with FSWs in much of the developing world. We found that an individual level SBCM intervention model was acceptable and engaging to a street-based population of FSWs, and also produced significant effects on risk behaviors for HIV infection and transmission. From a public health perspective, reducing HIV transmission in a sex work context may have considerable impact on the epidemic, and prevention monies focused on initiatives for this population would appear to be an efficient use of scarce resources. Nevertheless, interventions for FSWs going forward should address structural level challenges, in addition to individual level barriers. Successful approaches in the longer-term must include intervention models that can engage and retain vulnerable individuals such as SBCM, yet inroads must also be made to improve the viability of connections to the health service system. Individuals with high levels of competing needs, and particularly substance abuse, may have limited windows of opportunity for service linkage when motivation is high, but service acquisition can involve lengthy admissions or eligibility screening procedures or waiting lists that span months [74,75]. Those most in need often disengage or are lost in this critical time period; to bridge this gap it is essential that interventions going forward build capacity for ongoing support networks for FSWs (advocacy groups, self-help networks, support groups) to fill these voids in the formal service delivery system.
Acknowledgments
This research was supported by Grant # R01DA013131 from the National Institute Drug Abuse. NIDA had no further role in study design; in the collection, analysis and interpretation of data; in the writing of this report; or in the decision to submit the paper for publication.
References
- 1.Wariki WMV, Ota E, Mori R, et al. Behavioral interventions to reduce the transmission of HIV infection among sex workers and their clients in low-and middle-income countries. Cochrane Database Syst Rev. 2012:2. doi: 10.1002/14651858.CD005272.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chersich MF, Luchters S, Ntaganira I, et al. Priority interventions to reduce HIV transmission in sex work settings in sub-Saharan African and the delivery of these services. J Int AIDS Soc. 2013;16:17980. doi: 10.7448/IAS.16.1.17980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baral S, Beyrer C, Muessig K, et al. Burden of HIV among female sex workers in low-income and middle-income countries: A systematic review and meta-analysis. The Lancet Infect Dis. 2012;12:538–549. doi: 10.1016/S1473-3099(12)70066-X. [DOI] [PubMed] [Google Scholar]
- 4.Baseman J, Ross M, Williams M. Sale of Sex for Drugs and Drugs for Sex: An Economic Context of Sexual Risk Behaviors for STDs. Sex Transm Dis. 1999 Sep;26(8):444–449. doi: 10.1097/00007435-199909000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Deren S, Sanchez J, Shedlin M, et al. HIV Risk Behaviors Among Dominican Brothel and Street Prostitutes in New York City. AIDS Educ Prev. 1996 Oct;8(5):444–456. [PubMed] [Google Scholar]
- 6.Goudreau R. Prostitutes’ ‘Status’ Seen as a Factor: Dade Study Shows Sharp Differences. Miami Herald. 1987 Jun 4;:14A. [Google Scholar]
- 7.Hansen H, Lopez-Iftikhar MM, Alegría MJ. The Economy of Risk and Respect: Accounts by Puerto Rican Sex Workers of HIV Risk Taking. J Sex Res. 2002 Nov;39(4):292–301. doi: 10.1080/00224490209552153. [DOI] [PubMed] [Google Scholar]
- 8.Kwiatkowski CF, Booth RE. Differences in HIV Risk Behaviors Among Women Who Exchange Sex for Drugs, Money, or Both Drugs and Money. AIDS Behav. 2000 Sep;4(3):233–240. [Google Scholar]
- 9.Booth RE, Kwiatkowski CF, Weissman G. Health-Related Service Utilization and HIV Risk Behaviors Among HIV Infected Injection Drug Users and Crack Smokers. Drug Alcohol Depend. 1999;55:69–78. doi: 10.1016/s0376-8716(98)00179-3. [DOI] [PubMed] [Google Scholar]
- 10.McKeganey NP. Prostitution and HIV: What Do We Know and Where Might Research Be Targeted in the Future? AIDS. 1994 Sep;8(9):1215–1226. doi: 10.1097/00002030-199409000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Porter J, Bonilla L. Drug Use, HIV, and the Ecology of Street Prostitution. In: Weitzer R, editor. Sex for Sale: Prostitution, Pornography, and the Sex Industry. New York: Routledge; 2000. pp. 103–121. [Google Scholar]
- 12.Surratt HL, Inciardi JA. HIV Risk, Seropositivity and Predictors of Infection Among Homeless and Non-Homeless Women Sex Workers in Miami, Florida, USA. AIDS Care. 2004;16(5):594–604. doi: 10.1080/09540120410001716397. [DOI] [PubMed] [Google Scholar]
- 13.Wojcicki JM, Malala J. Condom Use, Power and HIV/AIDS Risk: Sex-Workers Bargain for Survival in Hillbrow/Joubert Park/Berea, Johannesburg. Soc Sci Med. 2001 Jul;53(1):99–121. doi: 10.1016/s0277-9536(00)00315-4. [DOI] [PubMed] [Google Scholar]
- 14.Kurtz SP, Surratt HL, Kiley MC, Inciardi JA. Barriers to Health and Social Services for Street-Based Sex Workers. J Health Care Poor Underserved. 2005;16(2):345–361. doi: 10.1353/hpu.2005.0038. [DOI] [PubMed] [Google Scholar]
- 15.Wechsberg WM, Lam WKK, Zule W, et al. Violence, Homelessness, and HIV Risk Among Crack-Using African-American Women. Subst Use Misuse. 2003;38(3–6):669–700. doi: 10.1081/ja-120017389. [DOI] [PubMed] [Google Scholar]
- 16.King EJ, Maman S, Bowling JM, Moracco KE, Dudina V. The influence of stigma and discrimination on female sex workers’ access to HIV services in St. Petersburg, Russia. AIDS Behav. 2013 doi: 10.1007/s10461-013-0447-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Odek WO, Busza J, Morris CN, et al. Effects of micro-enterprise services on HIV risk behaviour among female sex workers in Kenya’s urban slums. AIDS Behav. 2009;13:449–461. doi: 10.1007/s10461-008-9485-y. [DOI] [PubMed] [Google Scholar]
- 18.Surratt HL, Inciardi JA, Kurtz SP, Kiley MC. Sex Work and Drug Use in a Subculture of Violence. Crime & Delinquency. 2004;50(1):43–59. [Google Scholar]
- 19.Surratt HL, Kurtz SP, Weaver JC, Inciardi JA. The Connections of Mental Health Problems, Violent Life Experiences, and the Social Milieu of the “Stroll” with the HIV Risk Behaviors of Female Street Sex Workers. Journal of Psychology and Human Sexuality. 2005;17(1/2):23–44. [Google Scholar]
- 20.Manopaiboon C, Prybylski D, Subhachaturas W, et al. Unexpectedly high HIV prevalence among female sex workers in Bangkok, Thailand in a respondent-driven sampling survey. Int J STD AIDS. 2013 doi: 10.1177/0956462412472300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beattie TSH, Bhattacharjee P, Suresh M, et al. Personal, interpersonal and structural challenges to accessing HIV testing, treatment and care services among female sex workers, men who have sex with men, and transgenders in Karnataka state, South India. J Epidemiol Community Health. 2012;66:ii42–ii48. doi: 10.1136/jech-2011-200475. [DOI] [PubMed] [Google Scholar]
- 22.Flynn MB, McKeever JL, Spda T, Gordon-Garofalo V. Active Client Participation: An Examination of Self-Empowerment in HIV/AIDS Case Management with Women. Journal of the Association of Nurses in AIDS Care. 2000 May-Jun;11(3):59–68. doi: 10.1016/S1055-3290(06)60276-8. [DOI] [PubMed] [Google Scholar]
- 23.Shedlin MG. AIDS and Intravenous Drug Use: Future Directions for Community-Based Prevention Research [NIDA Research Monograph] Vol. 93. Rockville, MD: National Institute on Drug Abuse; 1990. An Ethnographic Approach to Understanding HIV High-risk Behaviors: Prostitution and Drug Abuse; pp. 134–149. DHHS Publication No. (ADM) 90-1627. [PubMed] [Google Scholar]
- 24.Weiner A. Understanding the Social Needs of Streetwalking Prostitutes. Soc Work. 1996 Jan;41(1):97–105. doi: 10.1093/sw/41.1.97. [DOI] [PubMed] [Google Scholar]
- 25.Overs C. The tide cannot be turned without us: HIV epidemics amongst key affected populations. Paper presented at: XIX International AIDS Conference; July 26, 2012; Washington, DC. [Google Scholar]
- 26.Wechsberg WM, Luseno WK, Lam WKK, Parry CDH, Morojele NK. Substance use, sexual risk, and violence: HIV prevention intervention with sex workers in Pretoria. AIDS Behav. 2006;10(2):131–137. doi: 10.1007/s10461-005-9036-8. [DOI] [PubMed] [Google Scholar]
- 27.Rou K, Wu Z, Sullivan SG, et al. A five-city trial of a behavioural intervention to reduce sexually transmitted disease/HIV risk among sex workers in China. AIDS. 2007;21(Suppl 8):S95–S101. doi: 10.1097/01.aids.0000304703.77755.c7. [DOI] [PubMed] [Google Scholar]
- 28.Morisky DE, Stein JA, Chiao C. Impact of a social infuence intervention on condom use and sexually transmitted infections among establishment-based female sex workers in the Philippines: A multilevel analysis. Health Psychol. 2006;25(5):595–603. doi: 10.1037/0278-6133.25.5.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Patterson TL, Mausbach B, Lozada R, et al. Efficacy of a brief behavioral intervention to promote condom use among female sex workers in Tijuana and Ciudad Juarez, Mexico. Am J Public Health. 2008;98(11):2051–2057. doi: 10.2105/AJPH.2007.130096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rojanapithayakorn W. The 100% condom use program in Asia. Reprod Health Matters. 2006;14(28):41–53. doi: 10.1016/S0968-8080(06)28270-3. [DOI] [PubMed] [Google Scholar]
- 31.Luchters S. Impact of five years of peer-mediated interventions on sexual behavior and sexually transmitted infections among female sex workers in Mombasa, Kenya. BMC Public Health. 2008;8:143. doi: 10.1186/1471-2458-8-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Markosyan K, Lang DL, Salazar LF, et al. A randomized control trial of am HIV prevention intervention for street-based female sex workers in Yerevan, Armenia: Preliminary evidence of efficacy. AIDS Behav. 2010;14:530–537. doi: 10.1007/s10461-010-9689-9. [DOI] [PubMed] [Google Scholar]
- 33.Chiao C, Morisky DE, Ksobiech K, Malow RM. Promoting HIV testing and condom use among Filipina commerical sex workers: Findings from a quasi-experimental intervention study. AIDS Behav. 2009;13:892–901. doi: 10.1007/s10461-008-9418-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wechsberg WM, Zule WA, Luseno WK, et al. Effectiveness of an adapted evidence-based woman-focused intervention for sex workers and non-sex workers: The Women’s Health CoOp in South Africa. Journal of Drug Issues. 2011;41(2):233–252. [Google Scholar]
- 35.Strathdee S, Abramovitz D, Remedios L, et al. Reductions in HIV/STI incidence and sharing of injection equipment among female sex workers who inject drugs: Results from a randomized controlled trial. PLoS ONE. 2013;8(6):e65812. doi: 10.1371/journal.pone.0065812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Swenderman D, Basu I, Das S, Jana S, Rotheram-Borus MJ. Empowering sex workers in India to reduce vulnerability to HIV and sexually transmitted diseases. Soc Sci Med. 2009;69(8):1157–1166. doi: 10.1016/j.socscimed.2009.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sherman SG, Srikrishnan AK, Rivett KA, et al. Acceptability of a microenterprise intervention among female sex workers in Chennai, India. AIDS Behav. 2010;14:649–657. doi: 10.1007/s10461-010-9686-z. [DOI] [PubMed] [Google Scholar]
- 38.Basu I, Jana S, Rotheram-Borus MJ, et al. HIV prevention among sex workers in India. J J Acquir Immune Defic Syndr. 2004;36(3):845–852. doi: 10.1097/00126334-200407010-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Beyrer C, Baral S, Kerrigan D, et al. Expanding the Space: inclusion of most-at-risk populations in HIV prevention, treatment, and care services. J Acquir Immune Defic Syndr. 2011;57(Supplement 2):S96–S98. doi: 10.1097/QAI.0b013e31821db944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Inciardi JA, Surratt HL, Kurtz SP. HIV, HBV, and HCV Infections Among Drug-involved, Inner-City, Street Sex Workers in Miami, Florida. AIDS Behav. 2006;10(2):137–147. doi: 10.1007/s10461-005-9049-3. [DOI] [PubMed] [Google Scholar]
- 41.Scaccabarrozzi L. Sex workers and HIV. [Accessed October 29 2012];AIDS Community Research Initiate of America Update. 2006 15(1):1–27. http://img.thebody.com/legacyAssets/41/40/winter06.pdf#page=1. [Google Scholar]
- 42.Parvez F, Katyal M, Alper H, Leibowitz R, Venters H. Female sex workers incarcerated in New York City jails: Prevalence of sexually transmitted infections and associated risk behaviors. Sex Transm Infect. 2013;89:280–284. doi: 10.1136/sextrans-2012-050977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Surratt HL, Inciardi JA. An effective HIV risk reduction reduction protocol for drug-using women sex workers. J Prev Interv Community. 2010;38:118–131. doi: 10.1080/10852351003640732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rapp RC, Otto AL, Lane DT, et al. Improving linkage with substance abuse treatment using brief case management and motivational interviewing. Drug Alcohol Depend. 2008;94(1–3):172–182. doi: 10.1016/j.drugalcdep.2007.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rapp RC, Siegal HA, Li L, Saha P. Predicting Post-Primary Treatment Services and Drug Use Outcome: A Multivariate Analysis. American Journal of Alcohol and Drug Abuse. 1998;24(4):603–615. doi: 10.3109/00952999809019610. [DOI] [PubMed] [Google Scholar]
- 46.Hesse M, Vanderplasschen W, Rapp R, Broekaert E, Fridell M. Case management for persons with substance use disorders (Review) Cochrane Database Syst Rev. 2011;(10) doi: 10.1002/14651858.CD006265.pub2. http://web.ebscohost.com.ezproxylocal.library.nova.edu/ehost/pdfviewer/pdfviewer?vid=3&sid=ed64213e-7466-43c1-a156-b8653ff53f67%40sessionmgr4003&hid=4104. [DOI] [PubMed]
- 47.Craw JA, Gardner LI, Marks G, et al. Brief strengths-based case management promotes entry into HIV medical care: Results of the antiretroviral treatment access study-II. J Acquir Immune Defic Syndr. 2008;47(5):597–606. doi: 10.1097/QAI.0b013e3181684c51. [DOI] [PubMed] [Google Scholar]
- 48.Gardner EM, Metsch LR, Anderson-Mahoney P, et al. Efficacy of a brief case management intervention to link recently diagnosed HIV-infected persons to care. AIDS. 2005;19:423–431. doi: 10.1097/01.aids.0000161772.51900.eb. [DOI] [PubMed] [Google Scholar]
- 49.Hays RB, Peterson JL. HIV Prevention for Gay and Bisexual Men in Metropolitan Cities. In: DiClemente RJ, Peterson JL, editors. Preventing AIDS: Theories and Methods of Behavioral Interventions. New York: Plenum Press; 1994. pp. 267–296. [Google Scholar]
- 50.Latkin CA. Outreach in Natural Setting: The Use of Peer Leaders for HIV Prevention Among Drug Users’ Networks. Public Health Rep. 1998;113(Suppl 1):151–159. [PMC free article] [PubMed] [Google Scholar]
- 51.Broadhead RS, Heckathorn DD, Altice FL, et al. Increasing drug users’ adherence to HIV treatment: Results of a peer-driven intervention study. Soc Sci Med. 2002;55(2):235–246. doi: 10.1016/s0277-9536(01)00167-8. [DOI] [PubMed] [Google Scholar]
- 52.Watters JK, Biernacki P. Targeted sampling: Options for the study of hidden populations. Soc Probl. 1989 Oct;36(4):416–430. [Google Scholar]
- 53.Miami Dade County Department of Health. [Accessed August 29, 2013];Miami-Dade County Reported HIV (Not AIDS) Cases Through 2012. 2012 http://www.dadehealth.org/downloads/2012%20HIV%20Reported.pdf.
- 54.Miami Dade County Department of Health. [Accessed December 6, 2013];Where black non-hispanics live, 2010. 2010 http://www.miamidade.gov/housing/library/reports/caper-2011-attachment-02.pdf.
- 55.Rapp RC. Strengths-based case management: Enhancing treatment for persons with substance abuse problems. In: Saleebey D, editor. The strengths perspective in social work practice (fourth edition) Boston: Allyn and Bacon; 2006. [Google Scholar]
- 56.Modrcin M, Rapp C, Chamberlain R. Case Management with Physically Disabled Individuals: Curriculum and Training Program. Lawrence, KS: University of Kansas School of Social Welfare; 1985. [Google Scholar]
- 57.Buttram ME, Surratt HL, Kurtz SP. Resilience and Syndemic Risk Factors among African American Female Sex Workers. Psychology, Health and Medicine. 2013 doi: 10.1080/13548506.2013.824595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dennis ML, Titus JC, White MK, Unsicker JI, Hodgkins D. Global Appraisal of Individual Needs - Initial (GAIN-I) Bloomington, IL: Chestnut Health Systems; 2002. [Google Scholar]
- 59.Institute of Behavioral Research. [Accessed July 5, 2013];TCU Drug Screen II. 2006 http://www.ibr.tcu.edu/pubs/datacoll/Forms/ddscreen-95.pdf.
- 60.Inciardi JA, Lockwood D, Pottieger AE. Women and Crack-Cocaine. New York: Macmillan; 1993. [Google Scholar]
- 61.Inciardi JA, Surratt HL, Kurtz SP, Weaver JC. The Effect of Serostatus on HIV Risk Behavior Change among Women Sex Workers in Miami, Florida. AIDS Care. 2005;17(Suppl 1):S88–S101. doi: 10.1080/09540120500121011. [DOI] [PubMed] [Google Scholar]
- 62.Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat Med. 2000;19:3127–3131. doi: 10.1002/1097-0258(20001130)19:22<3127::aid-sim784>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 63.Siegal HA, Rapp RC, Kelliher CW, et al. The Strengths Based Perspective of Case Management: A Promising Inpatient Substance Abuse Treatment Enhancement. J Psychoactive Drugs. 1995;27(1):67–72. doi: 10.1080/02791072.1995.10471674. [DOI] [PubMed] [Google Scholar]
- 64.Siegal HA, Rapp RC, Li L, Saha P, Kirk K. The Role of Case Management in Retaining Clients in Substance Abuse Treatment: An Exploratory Analysis. Journal of Drug Issues. 1997;27(4):821–831. [Google Scholar]
- 65.Strathdee SA, Ricketts EP, Huettner S, et al. Facilitating entry into drug treatment among injection drug users referred from a needle exchange program: Results from a community-based behavioral intervention trial. Drug Alcohol Depend. 2006;83:225–232. doi: 10.1016/j.drugalcdep.2005.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cunningham CO, Sohler NL, Cooperman NA, et al. Strategies to improve access to and utilization of health care services and adherence to antiretroviral therapy among HIV-infected drug users. Subst Use Misuse. 2011;46(2–3):218–232. doi: 10.3109/10826084.2011.522840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bradford JB, Coleman S, Cunningham W. HIV system navigation: An emerging model to improve HIV care access. AIDS Patient Care STDS. 2007;21(Supp 1):S-49–S-58. doi: 10.1089/apc.2007.9987. [DOI] [PubMed] [Google Scholar]
- 68.Hallum-Montes R, Manoloudis T, D’Souza R, et al. Results of a peer navigation pilot program to link HIV positive clients of harm reduction services with Ryan White clinical service providers. Journal of Public Health and Epidemiology. 2013;5(2):56–58. [Google Scholar]
- 69.Simoni JM, Pantalone DW, Plummer MD, Huang B. A randomized controlled trial of a peer support intervention targeting antiretroviral medication adherence and depressive symptomatology in HIV-positive men and women. Health Psychol. 2007;26(4):488–495. doi: 10.1037/0278-6133.26.4.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Purcell DW, Latka MH, Metsch LR, et al. Results from a randomized controlled trial of a peer-mentoring intervention to reduce HIV transmission and increase access to care and adherence to HIV medications among HIV-seropositive injection drug users. J Acquir Immune Defic Syndr. 2007;46(Supp 2):S35–S47. doi: 10.1097/QAI.0b013e31815767c4. [DOI] [PubMed] [Google Scholar]
- 71.Sohler NL, Coleman SM, Cabral H, et al. Does self-report data on HIV primary care utilization agree with medical record data for socially marginalized populations in the United States? AIDS Patient Care STDs. 2009;23(10):837–843. doi: 10.1089/apc.2009.0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Short ME, Goetzel RZ, Pei X, et al. How accurate are self-reports? An analysis of self-reported healthcare utilization and absence when compared to administrative data. Journal of Occupational & Environmental Medicine. 2009;51(7):786–796. doi: 10.1097/JOM.0b013e3181a86671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Reijneveld SA, Stronks K. The validity of self-reported use of health care across socioeconomic strata: A comparison of survey and registration data. Int J Epidemiol. 2001;30(6):1407–1414. doi: 10.1093/ije/30.6.1407. [DOI] [PubMed] [Google Scholar]
- 74.Carr CJA, Xu J, Redko C, et al. Individual and system influences on waiting time for substance abuse treatment. J Subst Abuse Treat. 2008;34(2):192–201. doi: 10.1016/j.jsat.2007.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Andrews CM, Shin HC, Marsh JC, Cao D. Client and program characteristics associated with wait time to substance abuse treatment entry. American Journal of Alcohol Abuse. 2013;39(1):61–68. doi: 10.3109/00952990.2012.694515. [DOI] [PubMed] [Google Scholar]