Abstract
Background
Prevalence of childhood overweight/obesity has increased considerably in recent years. The transition to higher rates of overweight/obesity has been well documented in high income countries; however, consistent or representative data from lower income countries is scarce. It is therefore pertinent to assess if rates of overweight/obesity are also increasing in lower income countries, to inform public health efforts.
Objective
This systematic review aimed to investigate the evidence for an overweight/obesity transition occurring in school-aged children and youth in Sub Saharan Africa.
Methods
Studies were identified by searching the MEDLINE, Embase, Africa Index Medicus, Global Health, Geobase, and EPPI-Centre electronic databases. Studies that used subjective or objective metrics to assess body composition in apparently healthy or population-based samples of children and youth aged 5 to 17 years were included.
Results
A total of 283 articles met the inclusion criteria, and of these, 68 were used for quantitative synthesis. The four regions (West, Central, East, and South) of Sub Saharan Africa were well represented, though only 11 (3.9%) studies were nationally representative. Quantitative synthesis revealed a trend towards increasing proportions of overweight/obesity over time in school-aged children in this region, as well as a persistent problem of underweight. Weighted averages of overweight/obesity and obesity for the entire time period captured were 10.6% and 2.5% respectively. Body composition measures were found to be higher in girls than boys, and higher in urban living and higher socioeconomic status children compared to rural populations or those of lower socioeconomic status.
Conclusions
This review provides evidence for an overweight/obesity transition in school-aged children in Sub Saharan Africa. The findings of this review serve to describe the region with respect to the growing concern of childhood overweight/obesity, highlight research gaps, and inform interventions.
PROSPERO Registration Number
CRD42013004399
Introduction
Worldwide populations are facing “modern” health risks due to increasing prevalence of overweight and obesity (overweight/obesity), physical inactivity, and sedentary behaviours, which are associated with obesogenic environments. This has caused a shift in the major causes of death from “traditional” health risks associated with poverty such as undernutrition, unsafe water, and poor sanitation, to a growing burden of modifiable non-communicable diseases (NCDs) [1]. The World Health Organization (WHO) classifies overweight/obesity as the fifth leading cause of global mortality, and one of the greatest health challenges and determinants for various chronic diseases such as heart disease, hypertension, diabetes, and psychosocial problems, in the 21st century [1], [2]–[6]. This growing population health threat has garnered much attention in view of the declaration and global campaign on the prevention and control of NCDs signed by the United Nations in 2011 [7].
While the health benefits of maintaining healthy body weights and an active lifestyle are well established [6], consumption of calorie-dense foods, declines in habitual physical activity, and increases in sedentary behaviour have been on the rise across developing nations [8]. Traditional practices such as walking long distances, and habitual physical labour have been replaced by motorized transport, and sedentary activities, particularly in urban settings [9]. Furthermore, in many Sub Saharan Africa (SSA) countries, an increased level of body fat is associated with beauty, prosperity, health, and prestige, while in contrast, thinness is perceived to be a sign of ill health or poverty [9]. These factors are now leading to increases in the occurrence of overweight/obesity and related risk factors for NCDs in SSA's children and youth [1], [9].
The health risks associated with overweight/obesity are particularly problematic in children due to the potential for long-term health concerns. A growing body of evidence has shown that overweight/obesity in childhood is significantly associated with increased risk of obesity, physical morbidity, and premature mortality in adulthood [10], [11], [12]. Fortunately, children who are able to attain a normal weight by adolescence have better cardiovascular disease risk factor profiles when compared to those that remain overweight [10]. Childhood is therefore a crucial time to learn basic life skills, including proper nutrition, and how to accumulate sufficient levels of activity in order to attain healthy body weights.
While we must recognise the diversity of populations in SSA, there are certain long-term developmental problems in this region that tend to adversely affect most or all of its countries and peoples [13]. Being the poorest continent in the world, with the highest population growth rate, the concern for an immense double burden of disease due to persistent infectious diseases and modern risks such as an overweight/obesity transition is troubling. The need for population wide interventions to reduce or prevent the adoption of less healthy lifestyles and body weights, particularly for children in SSA has never been greater [9], [14].
The objective of this systematic review was to determine if SSA is indeed undergoing an overweight/obesity transition. Specifically, this review aimed to examine time trends in the proportions of overweight/obesity in school-aged children and youth in SSA, thereby highlighting any research gaps and identifying areas of need for healthy active living interventions.
Methods
Study inclusion criteria
Studies were included if they reported using either subjective (e.g., parent or self-report questionnaires) or objective (e.g., directly measured) measures of body composition (weight, height, body mass index, waist/hip circumference, skin-folds, or body image assessment) in children aged 5–17 years. No date or language limits were set, but due to feasibility, only studies presented in either English or French were included. In addition, only studies of populations from SSA countries were included.
Study exclusion criteria
All published, peer-reviewed studies were eligible for inclusion; however, in order to obtain information on a general population living under ordinary conditions, intervention programs and studies were excluded unless they conducted baseline assessments. Studies done on children with chronic conditions were excluded.
Search strategy
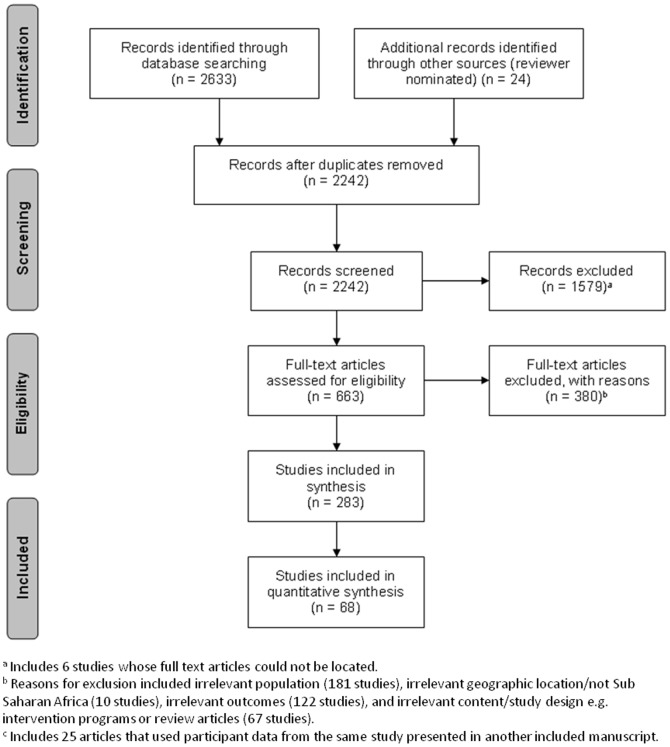
Studies were identified using the following electronic databases: Ovid MEDLINE (1948 to May, Week 4, 2013), Ovid Embase (1974 to Week 21, 2013), Africa Index Medicus (database dates not available, latest search on June 3, 2013), Global Health (1973 to June 3, 2013, through the CAB direct interface), Geobase (1884-June 3, 2013 through the Engineering Village interface), and EPPI-Centre database of health promotion research (Bibliomap) (dates of coverage not available, latest search on June 3, 2013). In addition, several open access journals relevant to SSA were identified and those journal web sites were searched for additional relevant papers. The search strategy for this systematic review was completed in tandem with a sister publication examining the evidence for a physical activity, sedentary behaviour, and physical fitness transition among school-age children and youth in SSA; hence, the inclusion of these terms in the search strategy. The search strategy was created and run by MS. The complete search strategy used for MEDLINE is presented in table 1 . The PRISMA flow chart in figure 1 accounts for the number of articles included to inform this systematic review. References were exported, de-duplicated and reviewed using Reference Manager Software (Version 11, Thompson Reuters, San Francisco, CA). Titles and abstracts of potentially relevant articles were screened by two independent reviewers (SKM and one of CEF or LJW), and full text copies were obtained for articles meeting initial screening criteria. Full text articles were screened in duplicate for inclusion in the review (SKM and one of CEF or LJW), and any discrepancies were discussed and resolved by the reviewers. This review is registered with the international prospective register of systematic reviews PROSPERO network (registration number: CRD42013004399); available at http://www.crd.york.ac.uk/prospero/.
Table 1. MEDLINE search strategy; Ovid interface.
| 1 | exp “Africa South of the Sahara”/ |
| 2 | (sub-sahar* or east afric* or south afric* or keny* or (south adj3 sahar*)).mp. |
| 3 | 1 or 2 |
| 4 |

|
| 5 | Sedentary Lifestyle/ |
| 6 | ((chair or sitting or car or automobile or auto or bus or indoor or in-door or screen or computer) adj time).tw. |
| 7 | low energy expenditure.tw. |
| 8 | (computer game* or video game* or ((television adj watch*) or tv watch*)).tw. |
| 9 | television/or computers/or video games/ |
| 10 | (screen based entertainment or screen-based entertainment or screen time).tw. |
| 11 | physical inactivit*.tw. |
| 12 | bed rest.mp. |
| 13 | sitting.tw. |
| 14 | exp obesity/ |
| 15 | (obesit* or obese).tw. |
| 16 | exp overweight/ |
| 17 | (overweight or over weight).tw. |
| 18 | exp Body Fat Distribution/ |
| 19 | exp body composition/ |
| 20 | Waist Circumference/ |
| 21 | waist circumference.tw. |
| 22 | Skinfold Thickness/ |
| 23 | (skin folds or skin fold*).tw. |
| 24 | (body composition* or BMI or body mass index).tw. |
| 25 | exp “body weights and measures”/ |
| 26 | (bio-impedance analysis or BIA).tw. |
| 27 | Absorptiometry, Photon/ |
| 28 | (absorptiometery or densitometry or photodensitometry or DXA or DEXA).tw. |
| 29 | Physical Fitness/ |
| 30 | (physical conditioning or physical fitness).tw. |
| 31 | musculoskeletal fitness.tw. |
| 32 | physical endurance/ |
| 33 | cardiovascular fitness.tw. |
| 34 | motor 
|
| 35 | physical exertion/ |
| 36 | aerobic exercise.tw. |
| 37 | exp sports/ |
| 38 | play/ |
| 39 | exp physical education/ |
| 40 | musculoskeletal physiological processes/or exercise/or movement/or locomotion/or running/or swimming/or walking/or motor activity/ |
| 41 | or/4-40 |
| 42 | (child* or adolescent* or youth* or pediatric* or paediatric*).tw. |
| 43 | 3 and 41 and 42 |
Note: The search strategy for this systematic review was completed in tandem with a sister publication examining the evidence for a physical activity, sedentary behaviour, and physical fitness transition among school-age children and youth in Sub Saharan Africa; hence, the inclusion of these terms in the search strategy.
Figure 1. PRISMA flow chart of search strategy results.
Data extraction, quality assessment, and synthesis
Data extraction was completed using a standardized data extraction template (SKM, CEF, AGL, and LJW). Study quality was assessed by SKM and CEF using a modified Downs and Black instrument [15]. Due to limitations in study design, questions selected from the Downs and Black quality assessment instrument excluded any questions that referred to intervention and trial study methodology. Ten out of the possible 27 questions were used for quality assessment as represented in table 2 . Table 3 provides the score out of ten for all studies included in this systematic review. Due to heterogeneity in study methodology and cut-points used to categorize samples into under, healthy, overweight, and obese, we were unable to carry out a meta-analysis in this review. However, quantitative syntheses were conducted by calculating the weighted averages (by sample size) of the prevalence of overweight/obesity. Our goal was to examine time trends and thereafter compute an overall prevalence of overweight/obesity in the region, by comparing the crude rates or prevalence of overweight/obesity in the individual populations or samples. As such, we attempted to standardize the crude rates by acknowledging and adjusting with respect to the sample sizes in each of the included studies, and indicating graphically the sample size upon which a particular data point was based. Findings from the quantitative synthesis were also complemented with narrative syntheses of the included studies.
Table 2. Modified Downs and Black checklist (Downs & Black, 1998).
| Reporting | |
| Objective Clearly Stated | Question 1 from full checklist (Y = 1/N = 0) |
| Main Outcomes Clearly Described | Question 2 (Y = 1/N = 0) |
| Patient Characteristics Clearly Defined | Question 3 (Y = 1/N = 0) |
| Main Findings Clearly Defined | Question 6 (Y = 1/N = 0) |
| Random Variability in Estimates Provided | Question 7 (Y = 1/N = 0) |
| Actual Probability Values Reported | Question 10 (Y = 1/N = 0) |
| External Validity | |
| Sample Targeted Representative of Population | Question 11 (Y = 1/N = 0) |
| Sample Recruited Representative of Population | Question 12 (Y = 1/N = 0) |
| Internal Validity/Bias | |
| Statistical Tests Used Appropriately | Question 18 (Y = 1/N = 0) |
| Primary Outcomes Valid/Reliable | Question 20 (Y = 1/N = 0) |
Table 3. Descriptive characteristics of included studies.
| First Author | Year | Study Design | Country | Sample Size | Age Range (Years) | Body Composition Measure or Categorization System | D&B Score |
| Prinsloo [104] | 1964 | Cross sectional | South Africa | 261 | 5–6 | Weight, height | 7 |
| Sloan [105] | 1967 | Cross sectional | South Africa | 393 | 15–17 | Weight, height | 7 |
| Smit [106] | 1967 | Cross sectional | South Africa | 2250 | 6–15 | Weight, height, skin fold measures | 7 |
| Leary [107] | 1969 | Cross sectional | South Africa | 301 | 7–15 | Weight, height | 7 |
| Areskog [108] | 1969 | Cross sectional | Ethiopia | 153 | 9–14 | Weight, height, skin fold measures | 7 |
| Fisher [109] | 1970 | Cross sectional | Zambia | 195 | 7–16 | Weight, height | 7 |
| Davies [266] | 1971 | Cross sectional | Rhodesia (now Zimbabwe) | 252 | 7–15 | Harvard standards | 7 |
| Davies [111] | 1973 | Cross sectional | Tanzania | 141 | 7–17 | Weight, height | 7 |
| Davies [110] | 1974 | Cross sectional | Tanzania | 1038 | 7–16 | Weight, height | 7 |
| Walker [112] | 1974 | Cross sectional | South Africa | 400 | 16–17 | Weight, height | 5 |
| Margo [268] | 1976 | Cross sectional | South Africa | 195 | 5–16 | None OW/OB | 7 |
| Booyens [113] | 1977 | Cross sectional | South Africa | 488 | 6–7 | Weight, height | 6 |
| Richardson [267] | 1977 | Cross sectional | South Africa | 804 | 17 | Harvard standards | 7 |
| Richardson [270] | 1977 | Cross sectional | South Africa | 6598 | 7–17 | None OW/OB | 6 |
| Richardson [271] | 1977 | Cross sectional | South Africa | 4655 | 7, 12 and 17 | None OW/OB | 7 |
| van Rensburg [272] a | 1977 | Cross sectional | South Africa | 488 | 6–7 | None OW/OB | 6 |
| Clegg [114] | 1978 | Cross sectional | Ethiopia | 203 | 5–16 | Weight, height | 6 |
| Coovadia [269] | 1978 | Cross sectional | South Africa | 5743 | 5–12 | Weight, height | 3 |
| Walker [273] | 1978 | Cross sectional | South Africa | 705 | 10–12 | None OW/OB | 7 |
| Sukkar [274] a | 1979 | Cross sectional | Sudan | 855 | 5–13 | Tanner et al., 1966 | 7 |
| Haller [154] | 1980 | Cross sectional | Côte d'Ivoire | 430 | 5–15 | None OW/OB | 6 |
| Walker [115] | 1980 | Cross sectional | South Africa | 1240 | 16–17 | Weight, height | 7 |
| Grassivaro [116] b , c | 1980 | Cross sectional | Somalia | 1206 | 6–17 | Weight, height | 9 |
| Rao [117] b | 1981 | Cross sectional | Zambia | 2487 | 5–17 | Weight, height | 7 |
| Carswell [275] | 1981 | Cross sectional | Tanzania | 238 | 10–14 | Tanner et al., 1966 | 6 |
| Singer [118] | 1981 | Cross sectional | Namibia | 306 | 5–17 | Weight, height | 7 |
| Oyemade [276] | 1981 | Cross sectional | Nigeria | 353 | 6–14 | None OW/OB | 7 |
| Griffin [277] | 1982 | Cross sectional | Kenya | 109 | 7–13 | Other NCHS based system | 7 |
| Nnanyelugo [155] | 1982 | Cross sectional | Nigeria | 1347 | 6–15 | Weight, height | 7 |
| Kulin [119] | 1982 | Cross sectional | Kenya | 656 | 10–17 | Weight, height | 7 |
| Sukkar [278] | 1982 | Mixed | Sudan | 1864 | 5–14 | Harvard standards | 7 |
| Power [279] b , c | 1982 | Cross sectional | South Africa | 790 | 6–8 | Other NCHS based system | 9 |
| Richardson [280] b , c | 1983 | Cross sectional | South Africa | 1337 | 8, 11, 14, and 17 | Harvard standards | 9 |
| Akesode [281] | 1983 | Cross sectional | Nigeria | 394 | 6–17 | Other categorization system | 7 |
| Little [120] | 1983 | Cross sectional | Kenya | 265 | 5–17 | Weight, height | 7 |
| Ng'andu [282] | 1984 | Cross sectional | Zambia | 374 | 7–14 | Other WHO based system | 6 |
| Rekart [121] | 1985 | Cross sectional | Sudan | 227 | 13–17 | Weight, height | 6 |
| Stephenson [122] | 1985 | Cross sectional | Kenya | 12 | 7–15 | Weight, height, skin fold measures | 7 |
| Ndamba [123] | 1986 | Cross sectional | Zimbabwe | 147 | 8–15 | Weight, height | 7 |
| Ogunranti [124] | 1986 | Cross sectional | Nigeria | 1165 | 5–12 | Weight | 7 |
| Corlett [125] | 1986 | Cross sectional | Botswana | 721 | 6–14 | Weight, height | 7 |
| Adams-Campbell [126] | 1987 | Cross sectional | Nigeria | 254 | 6–17 | BMI | 7 |
| Wagstaff [243] | 1987 | Longitudinal | South Africa | 864 | 5–14 | NCHS reference | 6 |
| Villiers [244] | 1987 | Cross sectional | South Africa | 375 | 10–17 | NCHS reference | 7 |
| Ogunranti [127] | 1987 | Cross sectional | Nigeria | 600 | 5–10 | Mid upper arm circumference | 5 |
| Corlett [128] | 1988 | Cross sectional | Botswana | 612 | 7–12 | Weight, height | 7 |
| Corlett [129] | 1988 | Cross sectional | Botswana | 483 | 7–14 | Weight, height | 7 |
| Adeniran [130] | 1988 | Cross sectional | Nigeria | 18 | 13–17 | Weight, height, body fat % | 7 |
| Adeniran [131] | 1988 | Cross sectional | Nigeria | 23 | 13–17 | Weight, height, body fat % | 7 |
| Jacobs [283] | 1988 | Cross sectional | South Africa | 430 | 5–10 | Other NCHS based system | 6 |
| Sigman [16] | 1989 | Longitudinal | Kenya | 138 | 7 and 8 | Weight z-scores | 7 |
| Prazuck [132] b , c | 1989 | Cross sectional | Mali | 844 | 15–17 | Weight, height | 9 |
| Ekpo [17] | 1990 | Cross sectional | Nigeria | 1552 | 5–16 | BMI | 6 |
| Walker [284] b , c | 1991 | Cross sectional | South Africa | 1015 | 14–17 | Other NCHS based system | 7 |
| Neumann [18] | 1992 | Cross sectional | Kenya | 133 | 7–9 | Weight, height | 7 |
| Ng'andu [133] | 1992 | Cross sectional | Zambia | 372 | 7–16 | BMI | 7 |
| Benefice [19] | 1992 | Cross sectional | Senegal | 100 | 9–14 | BMI | 7 |
| Goduka [134] | 1992 | Cross sectional | South Africa | 300 | 5–6 | Weight, height | 7 |
| Adams-Campbell [20] | 1992 | Longitudinal | Nigeria | 208 | 6–17 | Skin fold measures | 7 |
| Williams [21] | 1992 | Cross sectional | Kenya and Nigeria | 350 | 10–15 | BMI | 6 |
| Ng'andu [285] | 1992 | Cross sectional | Zambia | 800 | 12–17 | Nominal/adjusted classification system | 7 |
| Oli [135] | 1994 | Cross sectional | Ethiopia | 1850 | 7–14 | Weight, height | 7 |
| McDonald [22] | 1994 | Longitudinal | Kenya | 138 | 7–8 | Weight z-scores | 8 |
| Lawless [23] | 1994 | Longitudinal | Kenya | 86 | 6–11 | Weight z-scores | 7 |
| Mabrouk [136] | 1995 | Cross sectional | Sudan | 400 | 7–12 | Weight, height | 7 |
| Dufetel [137] | 1995 | Cross sectional | Senegal | 72 | 8–14 | Weight, height | 7 |
| Walker [156] b , c | 1996 | Cross sectional | Nigeria | 1192 | 6–12 | None OW/OB | 8 |
| Proctor [24] | 1996 | Cross sectional | Cameroon | 119 | 9–14 | BMI | 7 |
| Benefice [25] | 1996 | Cross sectional | Senegal | 348 | 5–13 | Weight, height, skin fold measures | 7 |
| Pettifor [26] | 1997 | Cross sectional | South Africa | 651 | 6–17 | BMI z-scores | 8 |
| Brabin [138] | 1997 | Cross sectional | Nigeria | 914 | 14–17 | Weight, height | 7 |
| Cole [286] | 1997 | Cross sectional | Nigeria | 22 | 11–17 | Ketz 1990 system | 7 |
| Owa [287] | 1997 | Cross sectional | Nigeria | 904 | 5–15 | US reference sample | 8 |
| Longo-Mbenza [27] | 1998 | Cross sectional | Zaire (now Democratic Republic of Congo - DRC) | 4848 | 5–16 | BMI | 6 |
| Benefice [157] | 1998 | Cross sectional | Senegal | 348 | 5–13 | None OW/OB | 7 |
| Prista [158] | 1998 | Cross sectional | Mozambique | 593 | 8–15 | None OW/OB | 8 |
| Benefice [28] | 1999 | Cross sectional | Senegal | 221 | 12–13 | BMI | 8 |
| Oelofse [159] | 1999 | Cross sectional | South Africa | 131 | 5–11 | None OW/OB | 6 |
| Levitt [29] | 1999 | Prospective Cohort Study | South Africa | 818 | 5 | BMI | 7 |
| Monyeki [245] | 1999 | Cross sectional | South Africa | 1149 | 5–10 | NCHS reference | 8 |
| Nyirongo [160] | 1999 | Cross sectional | Zimbabwe | 930 | 5–16 | None OW/OB | 8 |
| Akinkugbe [139] | 1999 | Cross sectional | Nigeria | 1076 | 11–15 | Weight, height | 8 |
| Sellen [30] a | 1999 | Cross sectional | Tanzania & Kenya | 234 | 5–17 | BMI | 7 |
| Hamidu [140] | 2000 | Cross sectional | Nigeria | 1712 | 5–16 | Weight, height | 7 |
| Sellen [288] | 2000 | Cross sectional | Tanzania | 169 | 5–12 | Seoane & Latham 1971 | 8 |
| Dibba [141] | 2000 | Cross sectional | Gambia | 160 | 8–11 | Weight, height | 8 |
| Zverev [161] | 2001 | Cross sectional | Malawi | 493 | 6–17 | None OW/OB | 7 |
| Garnier [31] | 2001 | Cross sectional | Senegal | 80 | 13–15 | BMI | 8 |
| Benefice [32] a | 2001 | Cross sectional | Senegal | 40 | 13 | BMI | 8 |
| Benefice [33] a | 2001 | Cross sectional | Senegal | 40 | 13 | BMI | 8 |
| Jinabhai [246] a | 2001 | Cross sectional | South Africa | 579 | 8–10 | NCHS reference | 7 |
| Beasley [162] | 2002 | Cross sectional | Chad | 1024 | 6–15 | None OW/OB | 7 |
| Pawloski [34] | 2002 | Cross sectional | Mali | 1056 | 10–17 | Weight z-scores | 7 |
| Perzanowski [142] | 2002 | Cross sectional | Kenya | 265 | 8–15 | Weight, height, body fat % | 6 |
| Underhay [187] a , b | 2002 | Cross sectional | South Africa | 1242 | 10–15 | IOTF categories | 9 |
| Bhargava [35] | 2003 | Longitudinal | Kenya | 100 | 6–9 | BMI | 6 |
| Eckhardt [36] | 2003 | Cross sectional | South Africa | 86 | 6–16 | BMI | 7 |
| Garnier [37] | 2003 | Cross sectional | Senegal | 331 | 14–16 | Weight z-scores | 8 |
| Grillenberger [38] | 2003 | Cross sectional | Kenya | 110 | 7 | Weight z-scores | 7 |
| Mabalia-Babela [289] | 2003 | Cross sectional | DRC | 1087 | 6–13 | BMI percentiles per Rolland-Cachera 1994 | 8 |
| Mukundi [163] | 2003 | Cross sectional | Kenya | 851 | 10–17 | None OW/OB | 7 |
| Prista [247] | 2003 | Cross sectional | Mozambique | 2316 | 6–17 | NCHS reference | 8 |
| Leman [39] | 2003 | Cross sectional | Nigeria | 39 | 5–8 | BMI | 7 |
| Jinabhai [184] b , c , d | 2003 | Cross sectional | South Africa | 29535 | 8–11 | WHO and IOTF categories | 9 |
| Schutte [40] a , b | 2003 | Cross sectional | South Africa | 1244 | 10–15 | BMI | 9 |
| Gray [143] | 2004 | Cross sectional | Kenya | 183 | 5–16 | Weight, height | 7 |
| Micklesfield [290] | 2004 | Cross sectional | South Africa | 198 | 7–11 | US reference sample | 7 |
| Larsen [41] | 2004 | Cross sectional | Kenya | 11 | 15–17 | BMI | 7 |
| Benefice [188] | 2004 | Cross sectional | Senegal | 507 | 16 | IOTF categories | 6 |
| Benefice [42] | 2004 | Cross sectional | Senegal | 40 | 13–15 | Weight z-scores | 7 |
| Monyeki [43] | 2004 | Longitudinal | South Africa | 85 | 7 | BMI | 8 |
| McVeigh [44] a | 2004 | Cross sectional | South Africa | 386 | 9 | BMI | 7 |
| Cameron [144] a | 2004 | Cross sectional | South Africa | 214 | 9 | Body fat % | 7 |
| Mukuddem-Petersen [164] a , b | 2004 | Cross sectional | South Africa | 1257 | 10–15 | None OW/OB | 9 |
| Prista [45] | 2005 | Cross sectional | Mozambique | 2271 | 16–17 | BMI | 8 |
| Agyemang [189] b , c | 2005 | Cross sectional | Ghana | 1277 | 8–16 | IOTF categories | 9 |
| Garnier [165] | 2005 | Longitudinal | Senegal | 1806 | 5–17 | CDC categories | 7 |
| Calvert [291] | 2005 | Cross sectional | South Africa | 393 | 8–12 | BMI z-score | 8 |
| Monyeki [292] | 2005 | Longitudinal | South Africa | 855 | 7–14 | US reference sample | 8 |
| Benefice [46] | 2005 | Cross sectional | Senegal | 99 | 10–13 | BMI | 8 |
| Friedman [47] | 2005 | Cross sectional | Kenya | 272 | 10–13 | BMI z-score | 8 |
| Jinabhai [190] b , c , d | 2005 | Secondary analysis | South Africa | 643 | 8–11 | IOTF categories | 9 |
| Steyn [248] b , c , d | 2005 | Secondary analysis | South Africa | 544 | 7–8 | NCHS reference | 10 |
| Underhay [192] a , b | 2005 | Cross sectional | South Africa | 1242 | 10–15 | IOTF categories | 9 |
| Monyeki [191] a | 2006 | Longitudinal | South Africa | 1884 | 6–13 | IOTF categories | 8 |
| Zerfu [249] | 2006 | Cross sectional | Ethiopia | 1208 | 9–17 | NCHS reference | 6 |
| Armstrong [193] b , c , d | 2006 | Cross sectional | South Africa | 10195 | 6–13 | IOTF categories | 10 |
| Kruger [194] b | 2006 | Cross sectional | South Africa | 1257 | 10–15 | IOTF categories | 9 |
| Aandstad [48] | 2006 | Cross sectional | Tanzania | 156 | 9–10 | BMI | 7 |
| Munday [49] | 2006 | Longitudinal | Gambia | 62 | 5–10 | BMI z-scores | 7 |
| Djarova [50] | 2006 | Cross sectional | Zimbabwe | 49 | 6–14 | BMI | 6 |
| Onyewadume [51] | 2006 | Cross sectional | Botswana | 30 | 11–14 | BMI | 8 |
| Nyati [145] a | 2006 | Cross sectional | South Africa | 369 | 9 | Weight, height | 8 |
| Vidulich [52] a | 2006 | Cross sectional | South Africa | 476 | 10 | BMI | 7 |
| Micklesfield [146] | 2007 | Cross sectional | South Africa | 64 | 9 | Weight, height | 7 |
| Micklesfield [53] | 2007 | Cross sectional | South Africa | 400 | 9 | BMI | 8 |
| Ben-Bassey [54] | 2007 | Cross sectional | Nigeria | 1504 | 12–17 | BMI | 8 |
| Longo-Mbenza [250] | 2007 | Cross sectional | DRC | 1535 | 5–17 | NCHS reference | 6 |
| Rohner [166] | 2007 | Cross sectional | Côte d'Ivoire (Ivory Coast) | 281 | 5–15 | None OW/OB | 7 |
| Jinabhai [195] b , c , d | 2007 | Cross sectional | South Africa | 5322 | 13–17 | IOTF categories | 10 |
| Madhavan [167] | 2007 | Cross sectional | South Africa | 117 | 5–14 | None OW/OB | 7 |
| Vidulich [55] | 2007 | Cross sectional | South Africa | 476 | 10 | BMI | 7 |
| Monyeki [56] | 2007 | Longitudinal | South Africa | 702 | 7–14 | Weight z-score | 8 |
| Semproli [196] | 2007 | Cross sectional | Kenya | 1,383 | 5–17 | IOTF categories | 7 |
| Andries [57] | 2007 | Longitudinal | South Africa | 702 | 7–14 | Weight z-score | 7 |
| Bovet [197] b , c , d | 2007 | Cross sectional | Seychelles | 4343 | 12–15 | IOTF categories | 9 |
| Goon [147] | 2007 | Cross sectional | Nigeria | 2015 | Body fat % | 8 | |
| Travill [293] | 2007 | Cross sectional | South Africa | 720 | 8–17 | Waterlow et al., 1977 | 7 |
| Makgae [198] a | 2007 | Longitudinal | South Africa | 1902 | 6–13 | IOTF categories | 8 |
| Ejike [58] | 2008 | Cross sectional | Nigeria | 923 | 10–17 | BMI | 8 |
| Ekpo [168] | 2008 | Cross sectional | Nigeria | 228 | 5–15 | None OW/OB | 8 |
| Anyiam [169] b , c | 2008 | Cross sectional | Nigeria | 3802 | 5–13 | None OW/OB | 10 |
| Nienaber [59] | 2008 | Cross sectional | South Africa | 195 | 15 | BMI | 8 |
| Olivieri [170] | 2008 | Cross sectional | Zimbabwe | 982 | 6–17 | None OW/OB | 7 |
| Monyeki [199] | 2008 | Longitudinal | South Africa | 1817 | 7–13 | IOTF categories | 7 |
| Jeremiah [294] | 2008 | Cross sectional | Nigeria | 144 | 5–8 | Other WHO based system | 7 |
| Funke [60] | 2008 | Cross sectional | Nigeria | 315 | 10–17 | BMI | 7 |
| Lennox [61] | 2008 | Cross sectional | South Africa | 318 | 15 | BMI | 8 |
| Goon [62] a | 2008 | Cross sectional | Nigeria | 2015 | 9–12 | BMI | 8 |
| Alaofe [251] | 2009 | Cross sectional | Benin | 180 | 12–17 | NCHS reference | 7 |
| Prista [227] | 2009 | Cross sectional | Mozambique | 256 | 6–16 | WHO categories | 8 |
| Micklesfield [63] | 2009 | Cross sectional | South Africa | 400 | 9 | BMI | 8 |
| Demerath [64] | 2009 | Secondary analysis | South Africa | 196 | 9 | Other NCHS based system | 8 |
| Cameron [65] | 2009 | Secondary analysis | South Africa | 227 | 8–11 | BMI | 7 |
| Hawley [66] | 2009 | Secondary analysis | South Africa | 1164 | 9–11 | Weight z-scores | 6 |
| Berntsen [67] | 2009 | Cross sectional | Tanzania | 190 | 9–10 | BMI | 8 |
| Dapi [255] | 2009 | Cross sectional | Cameroon | 581 | 12–16 | CDC categories | 7 |
| Ayoola [171] | 2009 | Cross sectional | Nigeria | 349 | 7–16 | None OW/OB | 7 |
| Senbanjo [68] | 2009 | Cross sectional | Nigeria | 392 | 5–14 | BMI | 8 |
| Padez [228] | 2009 | Cross sectional | Mozambique | 1417 | 9–17 | WHO categories | 7 |
| Mulugeta [148] | 2009 | Cross sectional | Ethiopia | 413 | 10–15 | BMI z-scores | 7 |
| Naiho [69] | 2009 | Cross sectional | Nigeria | 200 | 5–10 | BMI | 6 |
| Adegoke [70] | 2009 | Cross-sectional | Nigeria | 704 | 6–17 | BMI | 8 |
| Amuta [172] | 2009 | Cross sectional | Nigeria | 600 | 6–17 | None OW/OB | 6 |
| Poopedi [74] b , c | 2009 | Cross sectional | South Africa | 385 | 10 | BMI | 10 |
| Kimani-Murage [252] b , c | 2010 | Cross sectional | South Africa | 1914 | 5–14 | IOTF categories | 9 |
| Bamidele [173] | 2010 | Cross sectional | Nigeria | 139 | 5–15 | Other WHO based system | 7 |
| Omigbodun [229] | 2010 | Cross sectional | Nigeria | 1503 | 10–17 | WHO categories | 7 |
| Harmse [72] | 2010 | Cross sectional | South Africa | 221 | 13–17 | BMI | 7 |
| Senbanjo [256] | 2010 | Cross sectional | Nigeria | 392 | 5–14 | CDC categories | 8 |
| Goon [73] | 2010 | Cross sectional | Nigeria | 563 | 12–17 | BMI | 7 |
| Mosha [230] | 2010 | Cross sectional | Tanzania | 428 | 6–12 | WHO categories | 5 |
| Olumakaiye [174] | 2010 | Cross sectional | Nigeria | 315 | 10–17 | Other NCHS based system | 8 |
| Goon [186] | 2010 | Cross sectional | Nigeria | 2015 | 9–12 | CDC and IOTF categories | 8 |
| Goon [200] | 2010 | Cross sectional | Nigeria | 219 | 7–14 | IOTF categories | 7 |
| Opara [231] | 2010 | Cross sectional | Nigeria | 770 | 5–14 | WHO categories | 7 |
| Ejike [253] | 2010 | Cross sectional | Nigeria | 563 | 10–17 | NCHS reference | 7 |
| Truter [254] | 2010 | Cross sectional | South Africa | 280 | 9–13 | NCHS reference | 7 |
| Ansa [75] | 2010 | Cross sectional | Nigeria | 964 | 10–17 | BMI | 8 |
| Bogale [175] | 2010 | Cross sectional | Ethiopia | 100 | 5 | None OW/OB | 7 |
| Mulugeta [176] | 2010 | Cross sectional | Ethiopia | 413 | 10–15 | None OW/OB | 8 |
| Hawkesworth [295] | 2010 | Cross sectional | Gambia | 171 | 5–10 | BMI | 8 |
| Poopedi [71] | 2011 | Cross sectional | South Africa | 385 | 10 | BMI | 7 |
| Micklesfield [76] | 2011 | Cross sectional | South Africa | 471 | 13 | BMI | 7 |
| Salman [257] | 2011 | Cross sectional | Sudan | 304 | 6–12 | CDC categories | 7 |
| Nagwa [232] | 2011 | Cross sectional | Sudan | 1138 | 10–17 | WHO categories | 7 |
| Griffiths [77] | 2011 | Mixed | South Africa | 281 | 9–10 | BMI | 7 |
| Dabone [233] | 2011 | Cross sectional | Burkina Faso | 649 | 7–14 | WHO categories | 7 |
| Henry-Unaeze [78] b , c | 2011 | Cross sectional | Nigeria | 200 | 12–17 | BMI | 9 |
| Hadley [79] b , c | 2011 | Cross sectional | Ethiopia | 1943 | 13–17 | BMI | 8 |
| Odenigbo [258] | 2011 | Cross sectional | Nigeria | 119 | 6–12 | CDC categories | 7 |
| Thrandrayen [80] b , c | 2009 | Retrospective longitudinal | South Africa | 672 | 10 and 15 | BMI z-scores | 8 |
| Goon [81] | 2012 | Cross sectional | South Africa | 1136 | 9–13 | BMI | 7 |
| Kruger [82] b , c | 2012 | Cross sectional | South Africa | 582 and 462 | 7–9 | Weight z-scores | 6 |
| Semproli [83] | 2011 | Cross sectional | Kenya | 1383 | 5–17 | BMI z-scores | 7 |
| Koueta [201] | 2011 | Cross sectional | Burkina Faso | 204 | 13–16 | IOTF categories | 7 |
| Stevens [84] | 2011 | Cross sectional | Ghana | 181 | 9–16 | BMI | 7 |
| Peltzer [202] d | 2011 | Secondary analysis | Ghana & Uganda | 5613 | 13–15 | IOTF categories | 9 |
| Goon [234] a , b , c | 2011 | Cross sectional | Nigeria | 2015 | 9–12 | WHO categories | 9 |
| Nwizu [85] | 2011 | Cross sectional | Nigeria | 728 | 10–17 | BMI | 7 |
| Naude [86] | 2011 | Cross sectional | South Africa | 162 | 12–16 | BMI z-scores | 5 |
| Abolarin [87] | 2011 | Cross sectional | Nigeria | 560 | 6–12 | BMI | 8 |
| Abrahams [88] | 2011 | Cross sectional | South Africa | 717 | 10–12 | BMI z-scores | 8 |
| Motswagole [89] | 2011 | Cross sectional | South Africa | 919 | 9–15 | BMI | 8 |
| Croteau [259] | 2011 | Cross sectional | Kenya | 72 | 8–12 | CDC categories | 8 |
| Fetuga [226] | 2011 | Cross sectional | Nigeria | 1690 | 6–16 | CDC categories | 7 |
| Rankin [149] | 2011 | Cross sectional | South Africa | 81 | 13–16 | Weight | 7 |
| Larbi [260] | 2011 | Cross sectional | Ghana | 1482 | 6–15 | CDC categories | 8 |
| Mchiza [90] | 2011 | Secondary analysis | South Africa | 201 | 9–12 | BMI | 6 |
| Armstrong [203] b , c , d | 2011 | Secondary analysis | South Africa | 30365 | 8–11 | IOTF categories | 10 |
| Benefice [91] | 2011 | Cross sectional | Senegal | 791 | 5–15 | BMI | 8 |
| Kimani-Murage [204] | 2011 | Cross sectional | South Africa | 944 | 10–14 | IOTF categories | 7 |
| Dapi [92] | 2011 | Cross sectional | Cameroon | 227 | 12–16 | BMI | 8 |
| Vidulich [150] | 2011 | Cross sectional | South Africa | 419 | 10 | Weight, height | 8 |
| Faye [296] b , c | 2011 | Cross sectional | Senegal | 2356 | 11–17 | Rolland-Cachera et al., 1991 | 8 |
| Fetuga [235] | 2011 | Cross sectional | Nigeria | 1016 | 6–10 | WHO categories | 8 |
| Cameron [93] | 2011 | Cross sectional | South Africa | 119 | 9–10 | BMI | 6 |
| Goon [151] b | 2011 | Cross sectional | South Africa | 1136 | 9–13 | Weight, height | 9 |
| Amusa [205] | 2011 | Cross sectional | South Africa | 409 | 7–13 | IOTF categories | 8 |
| Ramos [177] | 2011 | Cross sectional | Kenya | 215 | 9–10 | None OW/OB | 7 |
| Puckree [236] | 2011 | Cross sectional | South Africa | 120 | 10–12 | WHO categories | 7 |
| Armstrong [94] a , d | 2011 | Cross sectional | South Africa | 10295 | 6–13 | BMI | 10 |
| Adamo [206] a | 2011 | Cross sectional | Kenya | 179 | 9–13 | IOTF categories | 7 |
| Goon [261] | 2011 | Cross sectional | Nigeria | 553 | 12–1 7 | CDC categories | 7 |
| Kamau [237] b , c | 2011 | Cross sectional | Kenya | 5325 | 10–15 | WHO categories | 9 |
| Ojofeitimi [297] | 2011 | Cross sectional | Nigeria | 280 | 10–14 | Other similar study | 8 |
| Kemp [207] b , c | 2011 | Cross sectional | South Africa | 816 | 6–7 | IOTF categories | 10 |
| Oldewage-Theron [238] | 2011 | Cross sectional | South Africa | 97 | 6–13 | WHO categories | 7 |
| Okoh [262] | 2012 | Cross sectional | Nigeria | 1302 | 6–12 | CDC categories | 7 |
| Naidoo [263] | 2012 | Cross sectional | South Africa | 170 | 7–10 | CDC categories | 7 |
| Ene-Obong [209] | 2012 | Cross sectional | Nigeria | 1,599 | 5–9 | IOTF categories | 7 |
| Prentice [152] | 2012 | Longitudinal | Gambia | 80 | 8–16 | Weight, height | 7 |
| Kramoh [239] | 2012 | Cross sectional | Côte d'Ivoire | 2038 | 12 | WHO categories | 7 |
| Musa [95] | 2012 | Cross sectional | Nigeria | 3243 | 9–15 | BMI | 7 |
| Adesina [96] | 2012 | Cross sectional | Nigeria | 884 | 10–17 | BMI | 8 |
| Cordeiro [178] b , c | 2012 | Cross sectional | Tanzania | 670 | 10–15 | None OW/OB | 9 |
| Monyeki [210] a | 2012 | Longitudinal | South Africa | 256 | 14 | IOTF categories | 8 |
| Griffiths [211] | 2012 | Cross sectional | South Africa | 358 | 16 | IOTF categories | 7 |
| Onywera [185] | 2012 | Cross sectional | Kenya | 169 | 9–12 | WHO categories | 7 |
| Bafor [97] | 2012 | Cross sectional | Nigeria | 369 | 5–10 | BMI | 7 |
| Reddy [212] b , c , d | 2012 | Secondary analysis | South Africa | 9522 and 9371 | 14–17 | IOTF categories | 9 |
| Opare-Addo [240] | 2012 | Cross sectional | Ghana | 720 | 7–17 | WHO categories | 8 |
| Ojiambo [98] | 2012 | Cross sectional | Kenya | 200 | 12–16 | BMI z-scores | 7 |
| Chinedu [264] | 2012 | Cross sectional | Nigeria | 926 | 6–16 | CDC categories | 5 |
| Craig [179] | 2012 | Cross sectional | South Africa | 1519 | 7, 11, and 15 | None OW/OB | 5 |
| Amare [180] | 2012 | Cross sectional | Ethiopia | 100 | 5–15 | None OW/OB | 8 |
| Moselakgomo [213] | 2012 | Cross sectional | South Africa | 1172 | 10–16 | IOTF categories | 8 |
| Micklesfield [214] | 2012 | Cross sectional | South Africa | 381 | 11–15 | IOTF categories | 6 |
| Monyeki [215] | 2012 | Cross sectional | South Africa | 256 | 14 | IOTF categories | 8 |
| Monyeki [298] | 2012 | Cross sectional | South Africa | 153 | 14–15 | Not indicated | 8 |
| Truter [216] | 2012 | Cross sectional | South Africa | 280 | 9–13 | IOTF categories | 7 |
| Musa [217] | 2012 | Cross sectional | Nigeria | 3240 | 9–16 | IOTF categories | 8 |
| Bovet [218] b , c | 2012 | Cross sectional | Seychelles | 8462 | 9–16 | IOTF categories | 9 |
| Fetuga [299] | 2012 | Cross sectional | Nigeria | 1557 | 5–11 | Weight standard deviation scores | 8 |
| Girma [100] | 2012 | Cross sectional | Ethiopia | 116 | 7–9 | Weight z-scores | 6 |
| Motswagole [241] | 2012 | Cross sectional | South Africa | 2111 | 6–15 | WHO categories | 7 |
| Wolff [101] | 2012 | Cross sectional | Madagascar | 1236 | 6–15 | BMI | 8 |
| Toriola [265] a | 2012 | Cross sectional | South Africa | 1172 | 10–16 | CDC categories | 7 |
| Wolff [102] a | 2012 | Cross sectional | Madagascar | 1236 | 6–15 | BMI | 7 |
| Goon [153] a , b , c | 2012 | Cross sectional | Nigeria | 2015 | 9–12 | Weight, height | 10 |
| Toriola [219] | 2012 | Longitudinal | South Africa | 283 | 14 | IOTF categories | 8 |
| Feeley [208] | 2013 | Longitudinal | South Africa | 1298 | 13, 15, and 17 | IOTF categories | 7 |
| Wilson [220] b , c , d | 2013 | Secondary analysis | Seychelles | 580 | 11–17 | IOTF categories | 8 |
| Ginsburg [221] | 2013 | Cross sectional | South Africa | 1613 | 15 | IOTF categories | 7 |
| Senbanjo [103] | 2013 | Cross sectional | Nigeria | 548 | 5–17 | BMI | 7 |
| Malete [222] | 2013 | Cross sectional | Botswana | 756 | 13–16 | IOTF categories | 7 |
| Neumann [181] | 2013 | Cross sectional | Kenya | 910 | 6–14 | None OW/OB | 7 |
| Degarege [182] | 2013 | Cross sectional | Ethiopia | 403 | 5–15 | None OW/OB | 8 |
| Puoane [242] | 2013 | Cross sectional | South Africa | 162 | 10–15 | WHO categories | 7 |
| Amare [183] | 2013 | Cross sectional | Ethiopia | 405 | 9–14 | None OW/OB | 8 |
| Mang'eni [223] a | 2013 | Cross sectional | Kenya | 200 | 13–16 | IOTF categories | 7 |
| Onywera [224] a | 2013 | Cross sectional | Kenya | 179 | 9–13 | IOTF categories | 7 |
| Heroux [225] a | 2013 | Cross sectional | Kenya | 179 | 9–13 | IOTF categories | 7 |
| Average (D&B) score | 7.4 |
Acronyms: D & B score (Downs & Black score); None OW/OB (none were overweight/obese); BMI (Body Mass Index); CDC-NCHS (Centers for Disease Control and Prevention – National Center for Health Statistics); WHO (World Health Organization); IOTF (International Obesity Task Force).
= Identical study sample as used in another included manuscript (not included in quantitative synthesis) [n = 27].
= Article indicated targeting a sample size representative of the population of interest [n = 38].
= Article indicated recruiting a sample size representative of the population of interest [n = 31].
= Article indicated that the sample size was nationally representative [n = 11].
Results
Figure 1 shows the PRISMA flow chart with numbers of included and excluded articles at each step of the review process, while table 3 provides a summary of all studies that met the inclusion criteria. A total of 2657 records were identified through database searches and other sources. Following de-duplication, 2242 articles were screened for eligibility, and 663 articles were selected for a full-text review. Of these, 283 articles met the inclusion criteria, and 68 of the studies (comprising 190,149 participants) were used in quantitative synthesis. Reasons for exclusion included: ineligible population (e.g., studies that did not involve children 5–17 years of age with no pre-existing condition) (n = 181); ineligible country (e.g., population living in a country/region outside of SSA) (10); ineligible outcome (n = 122); or ineligible study design (n = 67). It is important to note that all the studies included in this review were found to have used objective methods of collecting body composition data.
Regional representation
As shown in table 3 , which includes a summary of the 283 studies included in the review, the four regions of SSA were well represented, with 91 (32.1%) from West African countries - with Nigeria represented in 60 of these records; 7 (2.5%) from Central African countries; 75 (26.5%) from East African countries - with Kenya represented in 28 of these records; 108 (38.2%) from South African countries - with South Africa represented in 102 of these records; and 2 (0.7%) that were East and West combined. In total, 27 countries were captured in this review.
Publication rate
The earliest relevant record captured was published in 1964. There was a marked increase in the publishing rate from the earliest to the current studies: 5 articles between 1960 and 1969, 15 from 1970–1979, 32 from 1980–1989, 31 from 1990–1999, 92 from 2000–2009, and 108 articles from 2010 to May/June 2013.
Data quality assessment
The average modified Downs and Black score out of ten for all studies included in this systematic review was 7.4; indicative that data quality was fairly high among the included records, within the prescribed limitations of study designs included in this review. The majority of studies used in the quantitative synthesis scored 7 or higher. As presented in table 3 , the scoring process further revealed that only 38 (13.4%) of 283 included articles targeted a sample that was representative of their population of interest, and 31 (11.0%) recruited a sample that was representative of their population of interest. Only 11 (3.9%) articles explicitly mentioned using a nationally representative sample, one of which used the same study sample as that of another already included study.
Body composition measures
Of the 283 included studies, 88 (31.1%) articles [16]–[103] reported on mean BMI, BMI-z-score, and/or weight z-scores of the sample population, 50 (17.7%) articles [104]–[153] reported on body fat percentage, waist circumference, skin fold measures, and/or weight and height measures, and a total of 30 (10.6%) articles [154]–[183] reported finding no prevalence of overweight/obesity in their study samples. Of the remaining 115 (40.6%) records, 82 articles [184]–[265] used the more widely accepted international cut-points (namely, the International Obesity Task Force (IOTF), the Centers for Disease Control and Prevention (CDC), and the most recent WHO cut-points) to further categorize their samples into underweight, normal-weight, and overweight/obese. The other 33 articles [266]–[298] mentioned using one of a number of other cut-points and reference standard groups including but not limited to Tanner et al., 1966, Seoane & Latham, 1971, Frisancho 1990, Rosner et al., 1998, Harvard Standards, Waterlow 1972/77, and various US and UK reference samples. Of the 30 studies reporting no prevalence of overweight/obesity, a majority had not used the more widely accepted international cut-points, while the reminder did not provide the required prevalence estimates to be included in the quantitative synthesis.
Quantitative synthesis
Of the 82 articles that used more widely accepted international cut-points, 11 studies [187], [191], [192], [198], [206], [215], [224], [225], [234], [246], [265] were removed due to having an identical study sample as an already included study, and 3 studies [214], [218], [264] were removed for having not indicated the sample sizes in the age range of interest. As represented in table 4 , the remaining 68 (24.0%) articles [184]–[186], [188]–[190], [193]–[197], [199]–[205], [207]–[213], [216], [217], [219]–[223], [226]–[233], [235]–[245], [247]–[263] were used in quantitative synthesis. Of these, the largest proportion (44.1%) used the IOTF cut-points [299], 30.9% used CDC cut-points [300], and 25.0% used the most recent WHO cut-points [301] for weight status. Briefly, the IOTF methodology involved obtaining the body mass index for children from six large nationally representative cross sectional surveys on growth from Brazil, Great Britain, Hong Kong, the Netherlands, Singapore, and the United States. Thereafter, centile curves for body mass index were constructed for each dataset by sex, and passed though the widely used cut off points of 25 and 30 kg/m2 for adult overweight and obesity at age 18 years. The resulting curves were averaged to provide age and sex specific cut off points for children 2–18 years of age [299]. In the case of the CDC cut-points, growth charts were developed based on data from five national health examination surveys conducted in the United States, including limited supplemental data. Smoothed percentile curves were created by first smoothing selected empirical percentiles, then creating parameters obtain the final curves, additional percentiles, and z-scores [300]. Finally, the WHO cut-points were developed after data from the 1977 National Center for Health Statistics (NCHS)/WHO growth reference for 1–24 years, were merged with data from the under-fives growth standards' cross-sectional sample to smooth the transition between the two samples. The new curves filled the gap in growth curves and provided an appropriate reference for the 5 to 19 years age group [301].
Table 4. Proportions of overweight/obesity as reported by studies used in quantitative synthesis.
| Sample Size (n) | Proportions in Males | Proportions in Females | Proportions in Both Males and Females | ||||||||||||||||
| First Author | Year | Country | Cut Off | Age Range (years) | M | F | Total | UW | NW | OW | OB | UW | NW | OW | OB | UW | NW | OW | OB |
| Villiers [244] | 1987 | South Africa | 1 | 14–15 | 57 | 57 | 1.8 | 1.8 | |||||||||||
| Wagstaff [243] | 1987a (1981) | South Africa | 1 | 5–14 | 937 | 27.3 | 3.9 | 3.4 | |||||||||||
| Wagstaff [243] | 1987a (1983) | South Africa | 1 | 5–14 | 864 | 21.9 | 7.1 | 4.0 | |||||||||||
| Monyeki [245] | 1999 | South Africa | 1 | 5–10 | 595 | 557 | 1152 | 0.5 | 0.7 | 0.6 | |||||||||
| Prista [247] | 2003 | Mozambique | 1 | 6–17 | 1094 | 1222 | 2316 | 21.9 | 4.8 | 10.0 | 7.7 | 15.6 | 6.3 | ||||||
| Jinabhai [184] | 2003 | South Africa | 2 | 8–11 | 17351 | 12025 | 29376 | 3.0 | 0.7 | 4.5 | 1.2 | 3.6 | 0.9 | ||||||
| Benefice [188] | 2004 | Senegal | 3 | 16 | 188 | 319 | 507 | 50.0 | 0.0 | 0.0 | 17.9 | 1.6 | 0.0 | 29.8 | 1.0 | 0.0 | |||
| Agyemang [189] | 2005 | Ghana | 3 | 8–16 | 616 | 661 | 1277 | 3.1 | 6.4 | 4.8 | |||||||||
| Jinabhai [190] | 2005 | South Africa | 3 | 8–11 | 292 | 351 | 643 | 5.1 | 0.6 | ||||||||||
| Steyn [248] | 2005 | South Africa | 1 | 7–8 | 544 | 6.4 | 85.4 | 5.0 | 3.3 | ||||||||||
| Zerfu [249] | 2006 | Ethiopia | 1 | 9–17 | 918 | 23.8 | 3.5 | ||||||||||||
| Armstrong [193] | 2006 | South Africa | 3 | 6–13 | 5603 | 4680 | 10283 | 10.8 | 3.2 | 13.0 | 4.9 | 11.8 | 4.0 | ||||||
| Kruger [194] | 2006 | South Africa | 3 | 10–15 | 608 | 649 | 1257 | 4.1 | 1.5 | 8.3 | 1.7 | 6.3 | 1.6 | ||||||
| Longo-Mbenza [250] | 2007 | DRC | 1 | ≥12 | 362 | 124 | 486 | 24.0 | 68.5 | 35.5 | |||||||||
| Jinabhai [195] | 2007 | South Africa | 3 | 13–17 | 2398 | 2924 | 5322 | 18.4 | 4.2 | 2.6 | 20.9 | 9.7 | 13.4 | ||||||
| Semproli [196] | 2007 | Kenya | 3 | 5–17 | 702 | 681 | 1383 | 10.6 | 6.3 | 3.2 | |||||||||
| Bovet [197] | 2007 | Seychelles | 3 | 12–15 | 2202 | 2141 | 4343 | 8.1 | 3.1 | 13.1 | 4.4 | 10.6 | 3.7 | ||||||
| Monyeki [199] | 2008 | South Africa | 3 | 7–13 | 938 | 879 | 1817 | 1.1 | 2.1 | 1.6 | |||||||||
| Alaofe [251] | 2009 | Benin | 1 | 12–17 | 180 | 180 | 8.0 | 81.0 | 8.0 | 3.0 | 8.0 | 81.0 | 8.0 | 3.0 | |||||
| Prista [227] | 2009 | Mozambique | 2 | 6–16 | 139 | 117 | 256 | 1.1 | 0.0 | ||||||||||
| Dapi [255] | 2009 | Cameroon | 1 | 12–16 | 248 | 333 | 581 | 6.0 | 4.0 | 1.0 | 14.0 | 3.0 | 10.0 | ||||||
| Padez [228] | 2009 | Mozambique | 2 | 9–17 | 298 | 400 | 698 | 0.7 | 0.0 | 1.3 | 0.3 | 1.0 | 0.2 | ||||||
| Goon [186] | 2010 | Nigeria | 1 | 9–12 | 979 | 1036 | 2015 | 87.1 | 2.1 | 1.6 | 3.2 | 2.8 | 2.7 | 2.2 | |||||
| Kimani-Murage [252] | 2010 | South Africa | 3 | 5–14 | 1884 | 6.5 | 5.0 | 1.5 | |||||||||||
| Omigbodun [229] | 2010 | Nigeria | 2 | 10–17 | 763 | 740 | 1503 | 22.3 | 1.2 | 15.5 | 3.9 | 19.0 | 2.5 | ||||||
| Senbanjo [256] | 2010 | Nigeria | 1 | 5–14 | 202 | 190 | 392 | 37.1 | 61.9 | 1.0 | 23.2 | 74.7 | 2.1 | 30.4 | 68.1 | 1.5 | |||
| Mosha [230] | 2010 | Tanzania | 2 | 6–9 | 60 | 145 | 205 | 21.4 | 68.8 | 5.8 | 4.0 | ||||||||
| Goon [200] | 2010 | Nigeria | 3 | 7–14 | 107 | 112 | 219 | 2.7 | 1.0 | ||||||||||
| Odenigbo [258] | 2010 | Nigeria | 1 | 6–12 | 119 | 29.4 | 63.0 | 6.7 | 0.8 | ||||||||||
| Opara [231] | 2010 | Nigeria | 2 | 5–12.5 | 378 | 29.1 | 10.3 | ||||||||||||
| Ejike [253] | 2010 | Nigeria | 1 | 10–17 | 337 | 226 | 563 | 5.3 | 23.7 | 2.7 | 7.2 | 4.3 | 17.1 | ||||||
| Salman [257] | 2010 | Sudan | 1 | 6–12 | 68 | 236 | 304 | 82.4 | 11.8 | 5.9 | 75.0 | 14.0 | 11.0 | 76.7 | 13.5 | 9.9 | |||
| Truter [254] | 2010 | South Africa | 1 | 9–12 | 128 | 152 | 280 | 78.9 | 15.6 | 5.5 | 77.6 | 15.1 | 7.2 | 78.2 | 15.4 | 6.4 | |||
| Nagwa [232] | 2011 | Sudan | 2 | 10–17 | 526 | 612 | 1138 | 17.7 | 61.0 | 9.9 | 11.4 | 10.6 | 69.6 | 11.6 | 8.2 | 13.9 | 65.6 | 10.8 | 9.7 |
| Dabone [233] | 2011 | Burkina Faso | 2 | 7–14 | 312 | 337 | 649 | 13.7 | 2.3 | ||||||||||
| Koueta [201] | 2011 | Burkina Faso | 3 | 13–16 | 204 | 3.9 | |||||||||||||
| Peltzer [202] | 2011 | Ghana & Uganda | 3 | 13–15 | 2738 | 2875 | 5613 | 2.7 | 0.5 | 9.5 | 0.9 | 6.2 | 0.7 | ||||||
| Croteau [259] | 2011 | Kenya | 1 | 8–12 | 29 | 43 | 72 | 11.1 | 84.7 | 4.2 | |||||||||
| Fetuga [226] | 2011 | Nigeria | 2 | 6–16 | 821 | 669 | 1690 | 2.5 | 3.3 | 2.5 | |||||||||
| Larbi [290] | 2011 | Ghana | 1 | 6–15 | 706 | 776 | 1482 | 7.9 | 78.7 | 13.4 | |||||||||
| Kimani-Murage [204] | 2011 | South Africa | 3 | 10–14 | 944 | 7.5 | |||||||||||||
| Fetuga [235] | 2011 | Nigeria | 2 | 6–10 | 479 | 537 | 1016 | 23.8 | 3.8 | 20.8 | 3.3 | 22.2 | 3.5 | ||||||
| Amusa [205] | 2011 | South Africa | 3 | 7–13 | 193 | 216 | 409 | 2.6 | 2.9 | 2.8 | |||||||||
| Puckree [236] | 2011 | South Africa | 2 | 10–12 | 48 | 72 | 120 | 66.2 | 28.8 | 5.0 | |||||||||
| Goon [261] | 2011 | Nigeria | 1 | 12–17 | 0 | 553 | 553 | 5.4 | 77.0 | 11.1 | 5.4 | 5.4 | 77.0 | 11.1 | 5.4 | ||||
| Kamau [237] | 2011 | Kenya | 2 | 10–15 | 2620 | 2705 | 5325 | 6.5 | 2.6 | 10.9 | 3.6 | 8.7 | 3.1 | ||||||
| Kemp [207] | 2011 | South Africa | 3 | 6–7 | 419 | 397 | 816 | 90.2 | 6.4 | 3.3 | 86.4 | 9.3 | 4.3 | 88.4 | 7.8 | 3.8 | |||
| Oldewage-Theron [238] | 2011 | South Africa | 2 | 6–13 | 43 | 54 | 97 | 4.7 | 90.7 | 2.3 | 2.3 | 5.7 | 90.5 | 3.8 | 0.0 | 5.2 | 90.7 | 3.1 | 1.0 |
| Armstrong [203] | 2011a (1994) | South Africa | 3 | 8–11 | 17756 | 12609 | 30365 | 1.1 | 1.4 | 1.2 | 0.2 | ||||||||
| Armstrong [203] | 2011a (2004) | South Africa | 3 | 8–11 | 17756 | 12609 | 30365 | 9.5 | 2.2 | 16.5 | 4.4 | 12.4 | 3.1 | ||||||
| Okoh [262] | 2012 | Nigeria | 1 | 6–12 | 585 | 717 | 1302 | 11.7 | 76.7 | 5.7 | 5.9 | ||||||||
| Naidoo [263] | 2012 | South Africa | 1 | 7–10 | 70 | 100 | 170 | 54.3 | 11.4 | 34.3 | 55.0 | 16.0 | 29.0 | 54.7 | 14.1 | 31.2 | |||
| Ene-Obong [209] | 2012 | Nigeria | 3 | 5–9 | 706 | 19.0 | 68.7 | 9.5 | 2.8 | ||||||||||
| Kramoh [239] | 2012 | Côte d'Ivoire | 2 | 12 | 856 | 1182 | 2038 | 1.8 | 6.8 | 64.0 | 27.0 | 4.0 | 5.0 | ||||||
| Monyeki [210] | 2012 | South Africa | 3 | 14 | 100 | 156 | 256 | 44.0 | 48.0 | 8.0 | 30.7 | 51.9 | 17.3 | 35.9 | 50.4 | 13.7 | |||
| Griffiths [211] | 2012 | South Africa | 3 | 16 | 190 | 168 | 358 | 6.3 | 3.7 | 22.2 | 8.4 | 13.3 | 5.7 | ||||||
| Onywera [185] | 2012 | Kenya | 2 | 9–12 | 85 | 84 | 169 | 6.8 | 16.7 | 12.0 | |||||||||
| Opare-Addo [240] | 2012 | Ghana | 2 | 7–17 | 0 | 720 | 720 | 6.0 | 74.6 | 10.4 | 8.9 | ||||||||
| Moselakgomo [213] | 2012 | South Africa | 3 | 10–16 | 541 | 631 | 1172 | 4.6 | 80.8 | 9.1 | 5.5 | 5.2 | 79.4 | 11.0 | 4.4 | 4.9 | 80.0 | 10.1 | 4.9 |
| Truter [216] | 2012 | South Africa | 3 | 9–13 | 128 | 152 | 280 | 15.6 | 5.5 | 15.1 | 7.2 | 15.5 | 6.5 | ||||||
| Musa [217] | 2012 | Nigeria | 3 | 9–16 | 1526 | 1,714 | 3240 | 88.5 | 9.7 | 1.8 | |||||||||
| Motswagole [241] | 2012 | South Africa | 2 | 6–15 | 2111 | 34.2 | 0.6 | ||||||||||||
| Toriola [219] | 2012 | South Africa | 3 | 14 | 111 | 172 | 283 | 34.2 | 48.6 | 17.1 | 26.2 | 41.0 | 32.4 | 29.3 | 44.0 | 26.4 | |||
| Reddy [212] | 2012a (2002) | South Africa | 3 | 14–17 | 4184 | 5338 | 9522 | 6.3 | 1.6 | 24.3 | 5.0 | 16.4 | 3.5 | ||||||
| Reddy [212] | 2012a (2008) | South Africa | 3 | 14–17 | 4565 | 4806 | 9371 | 11.0 | 3.3 | 29.0 | 7.5 | 20.2 | 5.5 | ||||||
| Feeley [208] | 2013 | South Africa | 3 | 13–17 | 607 | 616 | 1223 | 8.1 | 27.0 | 17.6 | |||||||||
| Wilson [220] | 2013 | Seychelles | 3 | 11–17 | 278 | 302 | 580 | 13.4 | 15.6 | 7.7 | |||||||||
| Ginsburg [221] | 2013 | South Africa | 3 | 15 | 773 | 840 | 1613 | 20.3 | 71.8 | 5.4 | 2.5 | 9.6 | 65.4 | 17.5 | 7.5 | 14.2 | 68.5 | 11.7 | 5.1 |
| Malete [222] | 2013 | Botswana | 3 | 13–16 | 464 | 292 | 756 | 5.0 | 78.4 | 11.6 | 5.1 | ||||||||
| Puoane [242] | 2013 | South Africa | 2 | 10–15 | 0 | 162 | 162 | 2.4 | 61.4 | 36.2 | |||||||||
| Mang'eni [223] | 2013 | Kenya | 3 | 13–16 | 98 | 102 | 200 | 5.0 | |||||||||||
| 95885 | 84455 | 190149 | 25.0 | 68.0 | 5.6 | 2.0 | 8.3 | 68.6 | 11.5 | 3.9 | 17.6 | 68.5 | 8.1 | 2.5 | |||||
| Sample totals | (M) – weighted averages | (F) – weighted averages | (T) – weighted averages | ||||||||||||||||
Acronyms: M (male); F (female); UW (underweight); NW (normal weight); OW (overweight); OB (obese).
Weighted averages: Proportions may not add up to 100% for M, F, and T since some of the included studies did not report in each of the UW, NW, OW, and, OB categories.
Year of publication (year that corresponding data was collected included in brackets).
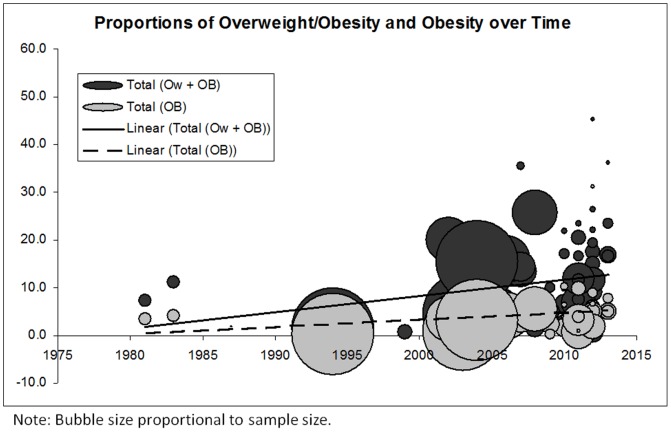
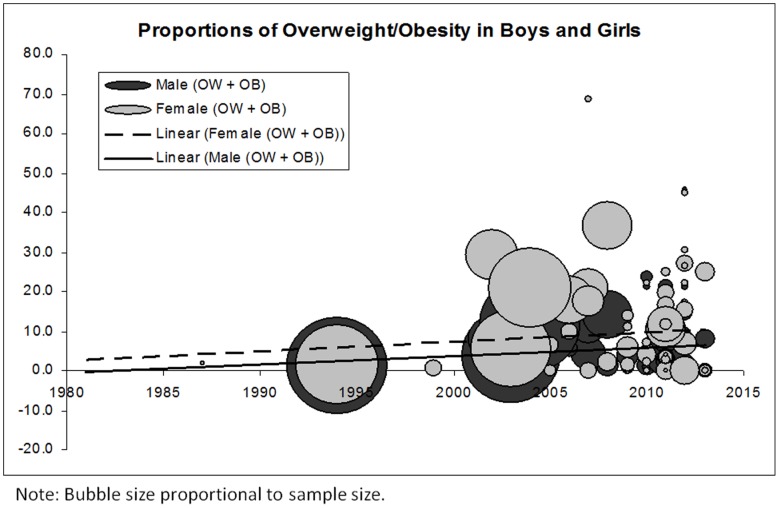
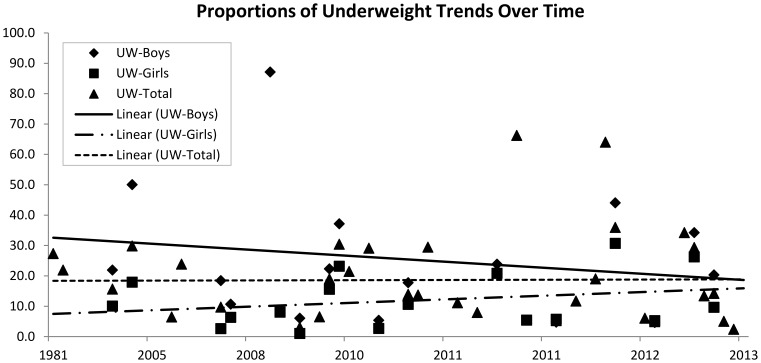
Figure 2 shows a distinctive time trend towards increasing proportions of overweight/obesity in school-aged children in SSA. The figure also shows a similar but less prominent trend towards increasing proportions of obesity over time. Figure 3 , shows increasing trends in proportions of overweight/obesity over time for both boys and girls; however, the proportions are consistently higher in girls than in boys. To determine the robustness of these findings, we examined the trends in overweight/obesity over time using the few studies that indicated having recruited a representative sample of the population. We similarly found a trend towards increasing proportions of overweight/obesity among school-aged children in this region. The findings were also similar when boys and girls were assessed separately. While not the focus of this manuscript, as shown in Figure 4 , we also examined trends in underweight over time for the included studies that had also reported this proportion. We found a trend towards decreasing proportions of underweight over time in boys, a trend towards increasing proportions over time in girls, and a largely unaltered trend over time - at approximately 20% - when boys and girls were considered together.
Figure 2. Proportions of overweight/obesity (combined) and obesity over time in Sub Saharan Africa.
Figure 3. Proportions of overweight/obesity (combined) in Sub Saharan Africa's boys and girls.
Figure 4. Proportions of underweight over time in Sub Saharan Africa.
The weighted averages (for the entire time period and all studies included in the quantitative analysis) of overweight/obesity proportions in boys and girls were calculated as 7.6% and 15.4% respectively. Weighted averages of obesity alone for boys and girls were 2.0% and 3.9% respectively. Weighted averages of overweight/obesity and obesity proportions for boys and girls combined were 10.6% and 2.5%. Weighted proportion of underweight was calculated as 25.0% for boys, 8.3% for girls, and 17.6% for boys and girls combined.
Narrative synthesis
Narrative descriptions of the relationship between body composition and age, sex, socioeconomic status (SES), and urban/rural differences are discussed below based largely on the studies not included in the quantitative synthesis:
Sex differences
Of the 96 studies [16]–[18], [20], [24]–[26], [29], [36], [39], [40], [43], [45], [46], [48], [51], [53]–[56], [59]–[61], [63]–[68], [70]–[72], [74], [76]–[80], [83], [85], [86], [89], [91], [92], [95], [96], [98], [103]–[105], [107], [109]–[114], [116]–[120], [123], [124], [126], [128], [129], [132], [133], [135], [136], [140], [143], [147], [149]–[152], [163], [169], [170], [214], [215], [218], [225], [281], [287], [289], [292], [293], [295] that reported their data by sex, 31 articles [20], [25], [29], [40], [45], [59], [67], [68], [70], [71], [74], [76], [78], [79], [85], [86], [89], [92], [95], [96], [103], [107], [124], [126], [132], [147], [151], [163], [170], [214], [215] reported that girls had higher body composition measures than boys, while 5 articles [265], [267], [289], [292], [293] reported that boys had higher body composition measures than girls. The remaining studies either found no significant difference or did not report a difference between boys and girls.
Urban/rural differences
Thirty-three articles compared body composition measures in urban and rural populations. Of these, 29 studies (including 7 studies used in the quantitative synthesis) [17, 24, 27, 31, 34, 37, 54, 58, 79, 84, 87, 98, 119, 128, 129, 138, 156, 163, 206, 212, 282, 298, (185, 189, 200, 217, 233, 240, 260)] reported significantly higher body composition measures in the urban compared to the rural sample, with the remaining studies [110], [111], [140], [280] reporting no significant difference between the two populations.
Socioeconomic status (SES) differences
Twenty four articles reported on outcomes of interest by some measure of socioeconomic status (e.g., income quartile, public/private school attendance). Of these, 19 articles (including 8 studies used in the quantitative synthesis) [45, 54, 61, 68, 75, 77, 84, 92, 99, 101, 156, 163, 169, 218, 296, 297, (212, 228, 231, 237, 247, 250, 255, 256)] reported that higher SES was associated with higher body composition measures, whilst the remaining articles [54], [75], [92], [169], [256] found no significant association of SES on body composition.
Age differences
Of the articles that reported on body composition measures by age, 15 studies found a largely positive relationship with age [287], [170], [70], [147], [103], [95], [151], [20], [42], [242], [256], [229], [230], [199], [297], while 7 studies found a largely negative relationship with age [83], [264], [233], [19], [190], [196], [245]. In some cases, the relationship between age and body composition measures differed between sexes; as such, we may conclude that there was no convincing or consistent evidence of an independent age effect.
Discussion
To our knowledge, this systematic review is the first to comprehensively examine if there is evidence supporting an overweight/obesity transition in school-aged children and youth in SSA.
An overweight/obesity transition
Due to vast heterogeneity in types of measurement, classification, and analysis, both narrative and quantitative analyses (weighted proportions and bubble plots of overweight/obesity) were presented in this review. Quantitative synthesis was completed using 68 studies that categorized children and youth based on internationally accepted cut-points for weight status. The weighted averages of overweight/obesity proportions in boys and girls was 7.6% and 15.4% respectively, while obesity proportions in boys and girls was 2.0% and 3.9% respectively. Weighted averages of overweight/obesity, and obesity for the total population were 10.6% and 2.5%. Current evidence revealed a clear transition of increasing proportions of overweight/obesity in school-aged children in SSA, and a similar, but less prominent trend towards increasing proportions of obesity over time. This transition to higher proportions of overweight/obesity is similar to observed trends in developed countries; however, the weighted averages fall far below proportions in various high income countries. For example, in Canada, research has shown that the prevalence of overweight/obesity has more than doubled (14% to 29%) and the obesity rate has tripled (3% to 9%) over the last 25 years in children and youth 5 to 17 years of age [302], [303]. In the USA, 33% of children and youth 6–19 years are considered to be overweight/obesity, and 18% are considered to obese [304].
It is important to note that across all age groups, WHO cut-points yield higher proportions of boys and girls classified as overweight/obesity than do the IOTF, or CDC cut-points [305]. While studies that used any of the three cut-points were analysed together in this review, when interpreting prevalence estimates of overweight/obesity, it is important to consider the choice of cut-point used in each study. With the largest proportion of included studies using IOTF cut-points, it could be argued that this may “dilute” the weighted average of the proportions of overweight/obesity calculated for SSA. Nonetheless, these results indicate that while there is an imminent threat of continued increases in levels of childhood overweight/obesity in SSA, implementing viable population health interventions may mitigate the associated health risks in these earlier stages.
Persistence of underweight
In discussing an overweight/obesity transition, it is important to recognize that child under-nutrition remains one of SSA's most fundamental challenge for improved human development [306], [307], [308]. This is particularly concerning when considering the school-aged child population as malnutrition affects their education outcomes, and consequently opportunities for success in later years [306]. Inadequate access to food and health services as a result of poverty and broader social determinants of health are some of the underlying determinants of child under-nutrition. The underweight trend over time was largely unaltered at approximately 20% for boys and girls combined, providing the evidence of a persisting underweight problem among SSA's children and youth, and substantiating the emergence of a public health double-edged sword. This persistence in underweight coupled with an overweight/obesity transition may place undue strain on the limited healthcare resources in SSA countries [14]. As such, frameworks for interventions to improve the nutritional status of SSA children will have to account for broader concepts such as societal organization, economic structures, and political ideologies [306]. We would however like to caution the reader that describing an underweight trend was not an objective of this systematic review; as such, pertinent articles reporting on underweight may have been omitted during the literature search thereby skewing these results.
Sex differences
Both quantitative and narrative synthesis revealed that there were increasing trends in proportions of overweight/obesity over time for both boys and girls; however, body composition measures and the proportions of overweight/obesity were proportionally higher in girls than in boys. In contrast, in North America, obesity is more common in boys than in girls, with the most significant differences observed among younger children 5–11 years [304], [309]. Higher proportions of overweight/obesity in SSA girls may be related to differences in gender roles particularly those requiring higher physical exertion (e.g., boys participating in higher energy expending roles/activities); and, cultural desirability whereby being overweight (i.e., “rounder”) is an admired trait and seen as a sign of wealth and prestige, particularly in girls.
Urban/rural and SES differences
Narrative synthesis revealed higher body composition measures in the urban compared to the rural population. In addition, higher SES was associated with higher body composition measures, pointing to a positive SES relationship. Factors associated with overweight/obesity span various behavioural, social, environmental, and biological constructs making them difficult to ascertain; however, urban residence and higher SES may be positively associated with overweight/obesity in SSA owing to improved access to governance, health care, education, employment and income, in addition to increased availability of packaged foods high in saturated fats and sugars and increased sedentary behaviour, all of which are more accessible to and/or affordable for those of higher SES or individuals living in urban areas.
Strengths, limitations, and future directions
The main strength of this review was the use of high quality standards to conceptualize and conduct the methodology and synthesis. Further, as many decisions as possible were made a priori to limit possible bias, and all levels of the review process were conducted in duplicate, ensuring a higher level of accuracy. Our assessment indicated that the quality of included studies was relatively high. The main limitation of this study lies in the vast heterogeneity in study methodology. The variety in the types of body composition measurements, analyses, definitions of SES, and reference standards limited our interpretation and presentation of the results. Quantitative synthesis was limited to those using the more widely accepted cut-points to further categorise study samples by weight status. It is also unclear if any material relevant for this review may have been published in un-indexed journals and hence not captured by the literature search.
Recognizing that future studies may increasingly employ WHO cut-points, since they represent a more robust criterion-based standard, we recommend that studies use the WHO cut-points for categorizing childhood overweight/obese in SSA, as this would allow for improved comparability and time trend analyses as attempted in this paper. A repository of studies, particularly those that are representative may be set up to this end, to allow for periodic comparative analysis for the whole of SSA. Measurements on more population representative samples are also required e.g., a multi-country survey using common measurement techniques and sampling procedures would be most desirable.
Conclusion
This systematic review provides evidence for an overweight/obesity transition in school-aged children in SSA. While the weighted averages of overweight/obesity in SSA are lower, this transition to higher proportions of overweight/obesity is similar to findings in various developed countries. The weighted average of overweight/obesity was higher in girls than in boys, and higher in those with higher SES. The review also revealed a persisting problem of underweight in the region, underpinning a double burden of risk factors. Findings of this review indicate that more nationally representative studies are needed to strengthen this field of research, and that interventions and strategies to address the growing threat of childhood overweight/obesity should focus on the higher SES and urban populations, with greater attention placed on girls.
Acknowledgments
The authors are grateful to Alison McFarlane and Afekwo Mbonu for their contributions towards locating the full text articles and for assistance with manuscript formatting.
Supporting Information
PRISMA checklist.
(DOC)
Funding Statement
The authors have no support or funding to report.
References
- 1.World Health Organization (2009) Global health risks: mortality and burden of disease attributable to selected major risks. Geneva, Switzerland.
- 2. Alamian A, Paradis G (2009) Correlates of multiple chronic disease behavioral risk factors in Canadian children and adolescents. Am J Epidemiol 170: 1279–1289. [DOI] [PubMed] [Google Scholar]
- 3. Batty D, Lee I (2004) Physical activity and coronary heart disease. BMJ 328: 1089–1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ross R, Janssen I (2007) Physical activity, fitness, and obesity. In: Bouchard C, Blair S, Haskell W, editors. Physical activity and health. Champaign, III: Human Kinetics Inc. pp. 173–190.
- 5. Tanuseputro P, Manuel D, Leung M, Nguyen K, Johansen H (2003) Risk factors for cardiovascular disease in Canada. Can J Cardiol 19: 1249–1259. [PubMed] [Google Scholar]
- 6.US Department of Health and Human Services (1996) Physical activity and health: a report of the Surgeon General. Atlanta, Georgia: National Center for Chronic Disease Prevention and Health Promotion.
- 7.United Nations News Center (2011) UN launches global campaign to curb death toll from non-communicable diseases. Available: www.un.org/news/. Accessed 19 September 2011.
- 8.World Health Organization (2004) Global strategy on diet, physical activity and health. Geneva, Switzerland.
- 9.Steyn K, Damasceno A (2006) Lifestyle and related risk factors for chronic diseases. In: Jamison DT, Feachem RG, Makgoba MW, et al., editors. Disease and mortality in Sub-Saharan Africa. 2nd edition.Washington, DC: World Bank. Available: http://www.ncbi.nlm.nih.gov/books/NBK2290/. Accessed 24 June 2013.
- 10. Lawlor D, Benfield L, Logue J, Tilling K, Howe L, et al. (2010) Association between general and central adiposity in childhood, and change in these, with cardiovascular risk factors in adolescence: prospective cohort study. BMJ 341: c6224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Reilly J, Kelly J (2011) Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes (Lond) 35: 891–898. [DOI] [PubMed] [Google Scholar]
- 12. The NS, Suchindran C, North KE, Popkin BM, Gordon-Larsen P (2010) Association of adolescent obesity with risk of severe obesity in adulthood. JAMA 304: 2024–2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McNamara RS (1985) the challenges for Sub-Saharan Africa: Sir John Crawford memorial lecture, presidential speech.Washington, DC: World Bank. Available: http://documents.worldbank.org/curated/en/1985/11/438287/challenges-sub-saharan-africa. Accessed 24 June 2013.
- 14. Unwin N, Setel P, Rashid S, Mugusi F, Mbanya J, et al. (2001) Noncommunicable diseases in sub-Saharan Africa: where do they feature in the health research agenda? Bull World Health Organ 79: 947–953. [PMC free article] [PubMed] [Google Scholar]
- 15. Downs SH, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 52: 377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sigman M, Neumann C, Jansen AA, Bwibo N (1989) Cognitive abilities of Kenyan children in relation to nutrition, family characteristics, and education. Child Dev 60: 1463–1474. [PubMed] [Google Scholar]
- 17. Ekpo EB, Udofia O, Andy JJ (1990) A disappearing urban/rural blood pressure difference in Nigerian children: an evaluation of possible determining factors. Ann Trop Paediatr 10: 211–219. [DOI] [PubMed] [Google Scholar]
- 18. Neumann C, McDonald MA, Sigman M, Bwibo N (1992) Medical illness in school-age Kenyans in relation to nutrition, cognition, and playground behaviors. J Dev Behav Pediatr 13: 392–398. [PubMed] [Google Scholar]
- 19. Benefice E (1992) Physical activity and anthropometric and functional characteristics of mildly malnourished Senegalese children. Ann Trop Paediatr 12: 55–66. [DOI] [PubMed] [Google Scholar]
- 20. ms-Campbell LL, Ukoli FA, Silverman JA, Omene JA, Nwankwo MU, et al. (1992) Tracking of blood pressure and anthropometric measures in Nigerian children. J Hum Hypertens 6: 47–51. [PubMed] [Google Scholar]
- 21. Williams CL, Wyinder EL (1992) Cardiovascular risk factors in children from fifteen countries. Cardiovascular Risk Factors 2: 45–55. [Google Scholar]
- 22. McDonald MA, Sigman M, Espinosa MP, Neumann CG (1994) Impact of a temporary food shortage on children and their mothers. Child Dev 65: 404–415. [PubMed] [Google Scholar]
- 23. Lawless JW, Latham MC, Stephenson LS, Kinoti SN, Pertet AM (1994) Iron supplementation improves appetite and growth in anemic Kenyan primary school children. J Nutr 124: 645–654. [DOI] [PubMed] [Google Scholar]
- 24. Proctor MH, Moore LL, Singer MR, Hood MY, Nguyen US, et al. (1996) Risk profiles for non-communicable diseases in rural and urban schoolchildren in the Republic of Cameroon. Ethn Dis 6: 235–243. [PubMed] [Google Scholar]
- 25. Benefice E, Malina R (1996) Body size, body composition and motor performances of mild-to-moderately undernourished Senegalese children. Ann Hum Biol 23: 307–321. [DOI] [PubMed] [Google Scholar]
- 26. Pettifor JM, Moodley GP (1997) Appendicular bone mass in children with a high prevalence of low dietary calcium intakes. J Bone Miner Res 12: 1824–1832. [DOI] [PubMed] [Google Scholar]
- 27. Longo-Mbenza B, Bayekula M, Ngiyulu R, Kintoki VE, Bikangi NF, et al. (1998) Survey of rheumatic heart disease in school children of Kinshasa town. Int J Cardiol 63: 287–294. [DOI] [PubMed] [Google Scholar]
- 28. Benefice E, Cames C (1999) Physical activity patterns of rural Senegalese adolescent girls during the dry and rainy seasons measured by movement registration and direct observation methods. Eur J Clin Nutr 53: 636–643. [DOI] [PubMed] [Google Scholar]
- 29. Levitt NS, Steyn K, de WT, Morrell C, Edwards R, et al. (1999) An inverse relation between blood pressure and birth weight among 5 year old children from Soweto, South Africa. J Epidemiol Community Health 53: 264–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sellen DW (1999) Growth patterns among seminomadic pastoralists (Datoga) of Tanzania. Am J Phys Anthropol 109: 187–209. [DOI] [PubMed] [Google Scholar]
- 31. Garnier D, Benefice E (2001) Habitual physical activity of Senegalese adolescent girls under different working conditions, as assessed by a questionnaire and movement registration. Ann Hum Biol 28: 79–97. [DOI] [PubMed] [Google Scholar]
- 32. Benefice E, Garnier D, Ndiaye G (2001) High levels of habitual physical activity in West African adolescent girls and relationship to maturation, growth, and nutritional status: results from a 3-year prospective study. Am J Human Biol 13: 808–820. [DOI] [PubMed] [Google Scholar]
- 33. Benefice E, Garnier D, Ndiaye G (2001) Assessment of physical activity among rural Senegalese adolescent girls: influence of age, sexual maturation, and body composition. J Adolesc Health 28: 319–327. [DOI] [PubMed] [Google Scholar]
- 34. Pawloski LR (2002) Growth and development of adolescent girls from the Segou Region of Mali (West Africa). Am J Phys Anthropol 117: 364–372. [DOI] [PubMed] [Google Scholar]
- 35. Bhargava A, Fox-Kean M (2003) The effects of maternal education versus cognitive test scores on child nutrition in Kenya. Econ Hum Biol 1: 309–319. [DOI] [PubMed] [Google Scholar]
- 36. Eckhardt CL, Adair LS, Caballero B, Avila J, Kon IY, et al. (2003) Estimating body fat from anthropometry and isotopic dilution: a four-country comparison. Obes Res 11: 1553–1562. [DOI] [PubMed] [Google Scholar]
- 37. Garnier D, Simondon KB, Hoarau T, Benefice E (2003) Impact of the health and living conditions of migrant and non-migrant Senegalese adolescent girls on their nutritional status and growth. Public Health Nutr 6: 535–547. [DOI] [PubMed] [Google Scholar]
- 38. Grillenberger M, Neumann CG, Murphy SP, Bwibo NO, van't VP, et al. (2003) Food supplements have a positive impact on weight gain and the addition of animal source foods increases lean body mass of Kenyan schoolchildren. J Nutr 133: 3957S–3964S. [DOI] [PubMed] [Google Scholar]
- 39. Leman CR, Adeyemo AA, Schoeller DA, Cooper RS, Luke A (2003) Body composition of children in south-western Nigeria: validation of bio-electrical impedance analysis. Ann Trop Paediatr 23: 61–67. [DOI] [PubMed] [Google Scholar]
- 40. Schutte AE, Huisman HW, van Rooyen JM, de Ridder JH, Malan NT (2003) Associations between arterial compliance and anthropometry of children from four ethnic groups in South Africa: the THUSA BANA Study. Blood Press 12: 97–103. [DOI] [PubMed] [Google Scholar]
- 41. Larsen HB, Christensen DL, Nolan T, Sondergaard H (2004) Body dimensions, exercise capacity and physical activity level of adolescent Nandi boys in western Kenya. Ann Hum Biol 31: 159–173. [DOI] [PubMed] [Google Scholar]
- 42. Benefice E, Garnier D, Ndiaye G (2004) Nutritional status, growth and sleep habits among Senegalese adolescent girls. Eur J Clin Nutr 58: 292–301. [DOI] [PubMed] [Google Scholar]
- 43. Monyeki MA, Toriola AL, Monyeki KD, Brits SJ, Pienaar AE (2004) Body size, body composition and physical fitness of 7-years-old Ellisras rural children, South Africa: Ellisras Longitudinal Study (ELS). African Journal for Physical, Health Education, Recreation and Dance 10: 154–162. [Google Scholar]
- 44. McVeigh JA, Norris SA, Cameron N, Pettifor JM (2004) Associations between physical activity and bone mass in black and white South African children at age 9 yr. J Appl Physiol 97: 1006–1012. [DOI] [PubMed] [Google Scholar]
- 45. Prista A, Maia AJ, Saranga S, Nhantumbo L, Marques AT, et al. (2005) Somatic growth of a school-aged population from Mozambique: trend and biosocial meaning. Hum Biol 77: 457–470. [DOI] [PubMed] [Google Scholar]
- 46. Benefice E, Ndiaye G (2005) Relationships between anthropometry, cardiorespiratory fitness indices and physical activity levels in different age and sex groups in rural Senegal (West Africa). Ann Hum Biol 32: 366–382. [DOI] [PubMed] [Google Scholar]
- 47. Friedman JF, Phillips-Howard PA, Mirel LB, Terlouw DJ, Okello N, et al. (2005) Progression of stunting and its predictors among school-aged children in western Kenya. Eur J Clin Nutr 59: 914–922. [DOI] [PubMed] [Google Scholar]
- 48. Aandstad A, Berntsen S, Hageberg R, Klasson-Heggebo L, Anderssen SA (2006) A comparison of estimated maximal oxygen uptake in 9 and 10 year old schoolchildren in Tanzania and Norway. BJSM online 40: 287–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Munday K, Ginty F, Fulford A, Bates CJ (2006) Relationships between biochemical bone turnover markers, season, and inflammatory status indices in prepubertal Gambian boys. Calcif Tissue Int 79: 15–21. [DOI] [PubMed] [Google Scholar]
- 50. Djarova T, Dube S, Tivchev G, Chivengo A (2006) Nutritional profiles, physical development and daily activities of African children in Zimbabwe with insulin-dependent diabetes mellitus. South African Journal of Science 102: 4–6. [Google Scholar]
- 51.Onyewadume IU (2006) Fitness of Black African early adolescents with and without mild mental retardation. Adapted Physical Activity Quarterly 23: unpaginated.
- 52. Vidulich L, Norris SA, Cameron N, Pettifor JM (2006) Differences in bone size and bone mass between black and white 10-year-old South African children. Osteoporos Int 17: 433–440. [DOI] [PubMed] [Google Scholar]
- 53. Micklesfield LK, Norris SA, Nelson DA, Lambert EV, van der ML, et al. (2007) Comparisons of body size, composition, and whole body bone mass between North American and South African children. J Bone Miner Res 22: 1869–1877. [DOI] [PubMed] [Google Scholar]
- 54. Ben-Bassey UP, Oduwole AO, Ogundipe OO (2007) Prevalence of overweight and obesity in Eti-Osa LGA, Lagos, Nigeria. Obes Rev 8: 475–479. [DOI] [PubMed] [Google Scholar]
- 55. Vidulich L, Norris SA, Cameron N, Pettifor JM (2007) Infant programming of bone size and bone mass in 10-year-old black and white South African children. Paediatr Perinat Epidemiol 21: 354–362. [DOI] [PubMed] [Google Scholar]
- 56. Monyeki MA, Koppes LL, Monyeki KD, Kemper HC, Twisk JW (2007) Longitudinal relationships between nutritional status, body composition, and physical fitness in rural children of South Africa: The Ellisras longitudinal study. Am J Human Biol 19: 551–558. [DOI] [PubMed] [Google Scholar]
- 57. Andries MM, Koppes LLJ, Monyeki KD, Kemper HCG, Twisk JWR (2007) Longitudinal relationships between nutritional status, body composition, and physical fitness in rural children of South Africa: The Ellisras longitudinal study. Am J Human Biol 19: 551–558. [DOI] [PubMed] [Google Scholar]
- 58. Ejike CE, Ugwu CE, Ezeanyika LU, Olayemi AT (2008) Blood pressure patterns in relation to geographic area of residence: a cross-sectional study of adolescents in Kogi state, Nigeria. BMC Public Health 8: 411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Nienaber C, Pieters M, Kruger SH, Stonehouse W, Vorster HH (2008) Overfatness, stunting and physical inactivity are determinants of plasminogen activator inhibitor-1activity, fibrinogen and thrombin-antithrombin complex in African adolescents. Blood Coagul Fibrinolysis 19: 361–368. [DOI] [PubMed] [Google Scholar]
- 60. Funke OM (2008) Prevalence of underweight: A matter of concern among adolescents in Osun State, Nigeria. Pakistan Journal of Nutrition 7: 503–508. [Google Scholar]
- 61. Lennox A, Pienaar AE, Wilders C (2008) Physical fitness and the physical activity status of 15-year-old adolescents in a semi-urban community. South African Journal for Research in Sport, Physical Education and Recreation 30: 59–73. [Google Scholar]
- 62. Goon DT, Toriola AL, Shaw BS, Amusa LO, Musa DI (2008) Sex Differences In Anthropometric Characteristics Of Nigerian School Children Aged 9-12 Years. African Journal for Physical, Health Education, Recreation and Dance 14: 130–142. [Google Scholar]
- 63. Micklesfield LK, Norris SA, van der ML, Lambert EV, Beck T, Pettifor JM (2009) Comparison of site-specific bone mass indices in South African children of different ethnic groups. Calcif Tissue Int 85: 317–325. [DOI] [PubMed] [Google Scholar]
- 64. Demerath EW, Jones LL, Hawley NL, Norris SA, Pettifor JM, et al. (2009) Rapid infant weight gain and advanced skeletal maturation in childhood. J Pediatr 155: 355–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Cameron N, Jones LL, Griffiths PL, Norris SA, Pettifor JM (2009) How well do waist circumference and body mass index reflect body composition in pre-pubertal children? Eur J Clin Nutr 63: 1065–1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Hawley NL, Rousham EK, Norris SA, Pettifor JM, Cameron N (2009) Secular trends in skeletal maturity in South Africa: 1962-2001. Ann Hum Biol 36: 584–594. [DOI] [PubMed] [Google Scholar]
- 67. Berntsen S, Lodrup Carlsen KC, Hageberg R, Aandstad A, Mowinckel P, et al. (2009) Asthma symptoms in rural living Tanzanian children; prevalence and the relation to aerobic fitness and body fat. Allergy 64: 1166–1171. [DOI] [PubMed] [Google Scholar]
- 68. Senbanjo IO, Njokanma OF, Oshikoya KA (2009) Waist circumference values of Nigerian children and adolescents. Ann Nutr Metab 54: 145–150. [DOI] [PubMed] [Google Scholar]
- 69. Naiho AO, Ebite LE, Aloamaka CP, Nwangwa KE (2009) The effect of crude oil exploration on growth and peak expiratory flow rate of children. Biomedical and Pharmacology Journal 2: 467–468. [Google Scholar]
- 70. Adegoke SA, Olowu WA, Adeodu OO, Elusiyan JBE, Dedeke IOF (2009) Prevalence of overweight and obesity among children in Ile-ife, south-western Nigeria. West Afr J Med 28: 216–221. [PubMed] [Google Scholar]
- 71. Poopedi MA, Norris SA, Pettifor JM (2011) Factors influencing the vitamin D status of 10-year-old urban South African children. Public Health Nutr 14: 334–339. [DOI] [PubMed] [Google Scholar]
- 72. Harmse B, Kruger HS (2010) Significant differences between serum CRP levels in children in different categories of physical activity: the PLAY study. Cardiovasc 21: 316–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Goon DT, Toriola AL, Uever J, Wuam S, Toriola OM (2010) Growth status and menarcheal age among adolescent school girls in Wannune, Benue State, Nigeria. BMC Pediatr 10: 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Poopedi MA, Norris SA, Pettifor JM (2009) Factors influencing the vitamin D status of 11 year old urban South Africa children. Bone Conference: 5th International Conference on Childrens Bone Health Cambridge United Kingdom. Conference Start: 20090623 Conference End: 20090626. Conference Publication: S84.
- 75. Ansa VO, Anah MU, Odey FA, Mbu PN, Agbor EI (2010) Relationship between parental socio-economic status and casual blood pressure in coastal Nigerian adolescents. West Afr J Med 29: 146–152. [DOI] [PubMed] [Google Scholar]
- 76. Micklesfield LK, Norris SA, Pettifor JM (2011) Determinants of bone size and strength in 13-year-old South African children: The influence of ethnicity, sex and pubertal maturation. Bone 48: 777–785. [DOI] [PubMed] [Google Scholar]
- 77. Griffiths PL, Rousham EK, Norris SA, Pettifor JM, Cameron N (2008) Socio-economic status and body composition outcomes in urban South African children. Arch Dis Child 93: 862–867. [DOI] [PubMed] [Google Scholar]
- 78. Henry-Unaeze HN, Okonkwo CN (2011) Food consumption pattern and calcium status of adolescents in Nnewi, Nigeria. Pakistan Journal of Nutrition 10: 317–321. [Google Scholar]
- 79. Hadley C, Belachew T, Lindstrom D, Tessema F (2011) The shape of things to come? Household dependency ratio and adolescent nutritional status in rural and urban Ethiopia. Am J Phys Anthropol 144: 643–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Thandrayen K, Norris S, Pettifor J (2009) Heterogeneity in fracture pathogenesis of urban South African children: The birth to twenty cohort. Bone Conference: 5th International Conference on Childrens Bone Health Cambridge United Kingdom. Conference Start: 20090623 Conference End: 20090626. Conference Publication: S100.
- 81. Goon DT, Toriola AL, Shaw BS (2012) Using receiver operating characteristic curve analysis in detecting excess adiposity in 9-13-year old South African children. West Indian Med J 61: 670–673. [PubMed] [Google Scholar]
- 82. Kruger HS, Steyn NP, Swart EC, Maunder EM, Nel JH, et al. (2012) Overweight among children decreased, but obesity prevalence remained high among women in South Africa, 1999-2005. Public Health Nutr 15: 594–599. [DOI] [PubMed] [Google Scholar]
- 83. Semproli S, Canducci E, Ricci E, Gualdi-Russo E (2011) Nutrient intake in 5-17-year-old African boys and girls in a rural district of Kenya. Nutr Hosp 26: 765–774. [DOI] [PubMed] [Google Scholar]
- 84. Stevens W, ddo-Yobo E, Roper J, Woodcock A, James H, et al. (2011) Differences in both prevalence and titre of specific immunoglobulin E among children with asthma in affluent and poor communities within a large town in Ghana. Clin Exp Allergy 41: 1587–1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Nwizu SE, Njokanma OF, Okoromah CA, David NA (2011) Relationship between bioelectrical impedance analysis and body mass index in adolescent urban Nigerians. West Afr J Med 30: 99–103. [PubMed] [Google Scholar]
- 86. Naude CE, Senekal M, Laubscher R, Carey PD, Fein G (2011) Growth and weight status in treatment-naive 12-16 year old adolescents with alcohol use disorders in Cape Town, South Africa. Nutr J 10: 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Abolarin TO, Aiyegbusi AI, Tella BA, Akinbo SR (2011) Relationship between selected anthropometric variables and prevalence of flatfoot among urban and rural school children in south west Nigeria. Niger 21: 135–140. [PubMed] [Google Scholar]
- 88. Abrahams Z, de VA, Steyn NP, Fourie J, Dalais L, et al. (2011) What's in the lunchbox? Dietary behaviour of learners from disadvantaged schools in the Western Cape, South Africa. Public Health Nutr 14: 1752–1758. [DOI] [PubMed] [Google Scholar]
- 89. Motswagole BS, Kruger HS, Faber M, van Rooyen JM, de Ridder JH (2011) The sensitivity of waist-to-height ratio in identifying children with high blood pressure. Cardiovasc 22: 208–211. [DOI] [PubMed] [Google Scholar]
- 90. McHiza ZJ, Goedecke JH, Lambert EV (2011) Intra-familial and ethnic effects on attitudinal and perceptual body image: a cohort of South African mother-daughter dyads. BMC Public Health 11: 433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Benefice E, Luna Monrroy SJ, Lopez Rodriguez RW, Ndiaye G (2011) Fat and muscle mass in different groups of pre-pubertal and pubertal rural children. Cross-cultural comparisons between Sahelian (rural Senegal) and Amazonian (Beni River, Bolivia) children. Ann Hum Biol 38: 500–507. [DOI] [PubMed] [Google Scholar]
- 92. Dapi LN, Hornell A, Janlert U, Stenlund H, Larsson C (2011) Energy and nutrient intakes in relation to sex and socio-economic status among school adolescents in urban Cameroon, Africa. Public Health Nutr 14: 904–913. [DOI] [PubMed] [Google Scholar]
- 93.Cameron N, Johnson W, Anderson EL (2011) Rapid growth (>1.33SDS) rather than catch-up growth (>0.67 to <1.33 SDS) during infancy is associated with significantly greater risk for obesity in childhood. Obesity (Silver Spring) Conference: 29th Annual Scientific Meeting of the Obesity Society, Obesity 2011 Orlando, FL United States. Conference Start: 20111001 Conference End: 20111005. Conference Publication: S220.
- 94. Armstrong ME, Lambert EV, Lambert MI (2011) Physical fitness of South African primary school children, 6 to 13 years of age: discovery vitality health of the nation study. Percept Mot Skills 113: 999–1016. [DOI] [PubMed] [Google Scholar]
- 95. Musa DI, Williams CA (2012) Cardiorespiratory fitness, fatness, and blood pressure associations in Nigerian youth. Med Sci Sports Exerc 44: 1978–1985. [DOI] [PubMed] [Google Scholar]
- 96. Adesina AF, Peterside O, Anochie I, Akani NA (2012) Weight status of adolescents in secondary schools in port Harcourt using Body Mass Index (BMI). Ital 38: 31. Bafor A, Omota B, Ogbemudia AO (2012) Correlation between clinical tibiofemoral angle and body mass index in normal Nigerian children. Int Orthop 36: 1247–1253.22183152 [Google Scholar]
- 97. Bafor A, Omota B, Ogbemudia AO (2012) Correlation between clinical tibiofemoral angle and body mass index in normal Nigerian children. Int Orthop 36: 1247–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Ojiambo RM, Easton C, Casajus JA, Konstabel K, Reilly JJ, et al. (2012) Effect of urbanization on objectively measured physical activity levels, sedentary time, and indices of adiposity in Kenyan adolescents. J Phys Act Health 9: 115–123. [DOI] [PubMed] [Google Scholar]
- 99.Fetuga B, Olanrewaju D, Ogunlesi T, Jonsson B, bertsson-Wikland K (2012) Growth in prepubertal Nigerian children is highly socio-economy dependent. Hormone Research in Paediatrics Conference: 51st Annual Meeting of the European Society for Paediatric Endocrinology, ESPE 2012 Leipzig Germany. Conference Start: 20120920 Conference End: 20120923. Conference Publication: 213.
- 100.Girma M, Loha E, Bogale A, Stoecker BJ (2012) Child nutritional status and cognitive performance in Hawassa Town, Southern Ethiopia. FASEB Journal Conference: Experimental Biology 2012, EB San Diego, CA United States. Conference Start: 20120421 Conference End: 20120425. Conference Publication.
- 101. Wolff PT, Arison L, Rahajamiakatra A, Raserijaona F, Niggemann B (2012) High asthma prevalence and associated factors in urban malagasy schoolchildren. Journal of Asthma 49: 575–580. [DOI] [PubMed] [Google Scholar]
- 102.Wolff PT, Arison L, Rahasamiakatra A, Raserisaona F, Niggemann B (2012) Bronchial asthma in urban malagasy children: The vavanystudy. Journal of Allergy and Clinical Immunology Conference: 2012 Annual Meeting of the American Academy of Allergy, Asthma and Immunology, AAAAI 2012 Orlando, FL United States. Conference Start: 20120302 Conference End: 20120306. Conference Publication: AB166.
- 103. Senbanjo IO, Oshikoya KA, Olutekunbi OA, Njokanma OF (2013) Body fat distribution of children and adolescents in Abeokuta, Southwest Nigeria. Am J Phys Anthropol 150: 647–654. [DOI] [PubMed] [Google Scholar]
- 104. Prinsloo JG (1964) Heights and Weights of White Nursery-School Children in Pretoria. SAMJ, S Suid-Afrikaanse Tydskrif Vir Geneeskunde. 38: 601–606. [PubMed] [Google Scholar]
- 105. Sloan AW, Wiggett R (1967) Inter-racial comparison of tests of physical fitness on high school children at Cape Town. J Sports Med Phys Fitness 7: 192–197. [PubMed] [Google Scholar]
- 106. Smit PJ, Potgieter JF, Neser ML, Fellingham SA (1967) Sex, age and race variations in the body measurements of white, Bantu, Coloured and Indian children aged 7-15 years. SAMJ, S Suid-Afrikaanse Tydskrif Vir Geneeskunde 41: 422–426. [PubMed] [Google Scholar]
- 107. Leary PM (1969) The use of percentile charts in the nutritional assessment of children from primitive communities. SAMJ , S Suid-Afrikaanse Tydskrif Vir Geneeskunde 43: 1165–1169. [PubMed] [Google Scholar]
- 108. Areskog NH, Selinus R, Vahlquist B (1969) Physical work capacity and nutritional status in Ethiopian male children and young adults. Am J Clin Nutr 22: 471–479. [DOI] [PubMed] [Google Scholar]
- 109. Fisher M, Davison W (1970) Growth curves for some Zambian school children. J Trop Pediatr 16: 103–111. [DOI] [PubMed] [Google Scholar]
- 110. Davies CTM (1973) Physiological responses to exercise in East African children. I. Normal values for rural and urban boys and girls aged 7-15 years. Journal of Tropical Pediatrics and Environmental Child Health 19: 110–114. [DOI] [PubMed] [Google Scholar]
- 111. Davies CT, Mbelwa D, Dore C (1974) Physical growth and development of urban and rural East African children, aged 7-16 years. Ann Hum Biol 1: 257–268. Amuta EU, Houmsou RS (2009) Assessment of nutritional status of school children in Makurdi, Benue State. Pakistan Journal of Nutrition 8: 691–694. [DOI] [PubMed] [Google Scholar]
- 112. Walker ARP (1974) Studies on sugar intake and overweight in South African black and white schoolchildren. SAMJ, S 48: 1650–1654. [PubMed] [Google Scholar]
- 113. Booyens J, Luitingh ML, Edwards H, van Rensburg CF (1977) Skinfold thickness measurements in assessment of nutritional status of Indian and White schoolchildren. SAMJ, S Suid-Afrikaanse Tydskrif Vir Geneeskunde 52: 1044–1048. [PubMed] [Google Scholar]
- 114. Clegg EJ, Pawson IG (1978) The influence of family characteristics on the heights, weights and skinfolds of highland and lowland children in Ethiopia. Ann Hum Biol 5: 139–146. [DOI] [PubMed] [Google Scholar]
- 115. Walker AR, Walker BF, Daya L, Ncongwane J (1980) Blood pressures of South African Black adolescents aged 16 to 17 years. Trans R Soc Trop Med Hyg 74: 595–600. [DOI] [PubMed] [Google Scholar]
- 116. Grassivaro GP, Franceschetti MM (1980) Growth of children in Somalia. Hum Biol 52: 547–561. [PubMed] [Google Scholar]
- 117. Rao UK, Katzarski M, Mehta L, Brady K (1981) Growth of Zambian children. Med J Zambia 15: 87–91. [PubMed] [Google Scholar]
- 118. Singer R, Kimura K (1981) Body height, weight, and skeletal maturation in Hottentot (Khoikhoi) children. Am J Phys Anthropol 54: 401–413. [DOI] [PubMed] [Google Scholar]
- 119. Kulin HE, Bwibo N, Mutie D, Santner SJ (1982) The effect of chronic childhood malnutrition on pubertal growth and development. Am J Clin Nutr 36: 527–536. [DOI] [PubMed] [Google Scholar]
- 120. Little MA, Galvin K, Mugambi M (1983) Cross-sectional growth of nomadic Turkana pastoralists. Hum Biol 55: 811–830. [PubMed] [Google Scholar]
- 121. Rekart ML, Plastino J, Carr C (1985) Health status of teenage school boys in eastern Sudan. East Afr Med J 62: 54–59. [PubMed] [Google Scholar]
- 122. Stephenson LS, Latham MC, Kurz KM, Miller D, Kinoti SN, et al. (1985) Urinary iron loss and physical fitness of Kenyan children with urinary schistosomiasis. Am J Trop Med Hyg 34: 322–330. [DOI] [PubMed] [Google Scholar]
- 123. Ndamba J (1986) Schistosomiasis: its effects on the physical performance of school children in Zimbabwe. Cent Afr J Med 32: 289–293. [PubMed] [Google Scholar]
- 124. Ogunranti JO (1986) Weight of contemporary Nigerian growing children in clinical anthropology. J Trop Pediatr 32: 218–224. [DOI] [PubMed] [Google Scholar]
- 125. Corlett JT (1986) Growth of urban schoolchildren in Botswana. Ann Hum Biol 13: 73–82. [DOI] [PubMed] [Google Scholar]
- 126. ms-Campbell LL, Ukoli F, Young MP, Omene J, Nwankwo M, et al. (1987) An epidemiological assessment of blood pressure determinants in an adolescent population of Nigerians. J Hypertens 5: 575–580. [DOI] [PubMed] [Google Scholar]
- 127. Ogunranti JO (1987) The mid-arm circumference in healthy eastern Nigerian children. A nutritional-clinical anthropometric parameter. Child Care Health Dev 13: 59–67. [DOI] [PubMed] [Google Scholar]
- 128. Corlett JT (1988) Strength development of Tswana children. Hum Biol 60: 569–577. [PubMed] [Google Scholar]
- 129. Corlett JT, Woollard E (1988) Growth patterns of rural children in the Kgalagadi region of Botswana. Ann Hum Biol 15: 153–159. [DOI] [PubMed] [Google Scholar]
- 130. Adeniran SA, Toriola AL (1988) Effects of different running programmes on body fat and blood pressure in schoolboys aged 13-17 years. Journal of Sports Medicine and Physical Fitness 28: 267–273. [PubMed] [Google Scholar]
- 131. Adeniran SA, Toriola AL (1988) Effects of continuous and interval running programmes on aerobic and anaerobic capacities in schoolgirls aged 13 to 17 years. Journal of Sports Medicine and Physical Fitness 28: 260–266. [PubMed] [Google Scholar]
- 132. Prazuck T, Fisch A, Pichard E, Sidibe Y, Gentilini M (1989) Growth of adolescents in Mali (West Africa). J Trop Pediatr 35: 52–54. [DOI] [PubMed] [Google Scholar]
- 133. Ng'andu NH (1992) Blood pressure levels of Zambian rural adolescents and their relationship to age, sex, weight, height and three weight-for-height indices. Int J Epidemiol 21: 246–252. [DOI] [PubMed] [Google Scholar]
- 134. Goduka IN, Poole DA, otaki-Phenice L (1992) A comparative study of black South African children from three different contexts. Child Dev 63: 509–525. [DOI] [PubMed] [Google Scholar]
- 135. Oli K, Tekle-Haimanot R, Forsgren L, Ekstedt J (1994) Blood pressure patterns and its correlates in schoolchildren of an Ethiopian community. J Trop Pediatr 40: 100–103. [DOI] [PubMed] [Google Scholar]
- 136. Mabrouk AA, Ibrahim SA (1995) Normal values for lung function tests in Sudanese children. East Afr Med J 72: 258–262. [PubMed] [Google Scholar]
- 137. Dufetel P, Wazni A, Gaultier C, Derossi G, Cisse F, et al. (1995) [Growth and ventilatory function in Black children and adolescents]. [French]. Rev Mal Respir 12: 135–143. [PubMed] [Google Scholar]
- 138. Brabin L, Ikimalo J, Dollimore N, Kemp J, Ikokwu-Wonodi C, et al. (1997) How do they grow? A study of south-eastern Nigerian adolescent girls. Acta Paediatr 86: 1114–1120. [DOI] [PubMed] [Google Scholar]
- 139. Akinkugbe FM, Akinwolere AO, Kayode CM (1999) Blood pressure patterns in Nigerian adolescents. West Afr J Med 18: 196-202. Hamidu LJ, Okoro EO, Ali MA (2000) Blood pressure profile in Nigerian children. East Afr Med J 77: 180–184. [PubMed] [Google Scholar]
- 140. Hamidu LJ, Okoro EO, Ali MA (2000) Blood pressure profile in Nigerian children. East Afr Med J 77: 180–184. [DOI] [PubMed] [Google Scholar]
- 141. Dibba B, Prentice A, Ceesay M, Stirling DM, Cole TJ, et al. (2000) Effect of calcium supplementation on bone mineral accretion in gambian children accustomed to a low-calcium diet. Am J Clin Nutr 71: 544–549. [DOI] [PubMed] [Google Scholar]
- 142. Perzanowski MS, Ng'Ang'A LW, Carter MC, Odhiambo J, Ngari P, et al. (2002) Atopy, asthma, and antibodies to Ascaris among rural and urban children in Kenya. J Pediatr 140: 582–588. [DOI] [PubMed] [Google Scholar]
- 143. Gray SJ, Wiebusch B, Akol HA (2004) Cross-sectional growth of pastoralist Karimojong and Turkana children. Am J Phys Anthropol 125: 193–202. [DOI] [PubMed] [Google Scholar]
- 144. Cameron N, Griffiths PL, Wright MM, Blencowe C, Davis NC, et al. (2004) Regression equations to estimate percentage body fat in African prepubertal children aged 9 y. Am J Clin Nutr 80: 70–75. [DOI] [PubMed] [Google Scholar]
- 145. Nyati LH, Norris SA, Cameron N, Pettifor JM (2006) Effect of ethnicity and sex on the growth of the axial and appendicular skeleton of children living in a developing country. Am J Phys Anthropol 130: 135–141. [DOI] [PubMed] [Google Scholar]
- 146. Micklesfield LK, Levitt NS, Carstens MT, Dhansay MA, Norris SA, et al. (2007) Early life and current determinants of bone in South African children of mixed ancestral origin. Ann Hum Biol 34: 647–655. [DOI] [PubMed] [Google Scholar]
- 147. Goon DT, Toriola AL, Shaw BS (2007) Sex differences in body fatness in Nigerian children. African Journal for Physical, Health Education, Recreation and Dance 13: 294–305. [Google Scholar]
- 148.Mulugeta A, Gebre M, Abdulkadir M, Gtsadik A, Gyesus A, et al.. (2009) Micronutrient deficiencies among school girls from tigray, northern Ethiopia. The FASEB Journal Conference: Experimental Biology.
- 149. Rankin D, Ellis SM, Macintyre UE, Hanekom SM, Wright HH (2011) Dietary intakes assessed by 24-h recalls in peri-urban African adolescents: validity of energy intake compared with estimated energy expenditure. Eur J Clin Nutr 65: 910–919. [DOI] [PubMed] [Google Scholar]
- 150. Vidulich L, Norris SA, Cameron N, Pettifor JM (2011) Bone mass and bone size in pre- or early pubertal 10-year-old black and white South African children and their parents. Calcif Tissue Int 88: 281–293. [DOI] [PubMed] [Google Scholar]
- 151. Goon DT, Toriola AL, Shaw BS, Amusa LO (2011) Centripetal fat patterning in South African children. Pakistan Journal of Medical Sciences 27: 832–836. [Google Scholar]
- 152. Prentice A, Dibba B, Sawo Y, Cole TJ (2012) The effect of prepubertal calcium carbonate supplementation on the age of peak height velocity in Gambian adolescents. Am J Clin Nutr 96: 1042–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Goon DT, Toriola AL, Shaw BS (2012) Stature and body mass of Nigerian children aged 9-12 years. Minerva Pediatr 64: 325–331. [PubMed] [Google Scholar]
- 154. Haller L, Lauber E (1980) [Health of school children on the Ivory Coast. Development of anthropometric parameters of 5- to 15-year-old children and the effect of parasitic diseases on their growth]. [French]. Acta Trop 37: 63–73. [PubMed] [Google Scholar]
- 155. Nnanyelugo DO (1982) Anthropometric indices and measurements on primary school children of contrasting parental occupations. Growth 46: 220–237. [PubMed] [Google Scholar]
- 156. Walker MB, Omotade OO, Walker O (1996) Height and weight measurements of Ibadan school children. Afr J Med Med Sci 25: 273–276. [PubMed] [Google Scholar]
- 157.Benefice E (1998) Growth and motor performances of rural Senegalese children. 117–131.
- 158.Prista A (1998) Nutritional status, physical fitness and physical activity in children and youth in Maputo (Mozambique). 94–104.
- 159. Oelofse A, Faber M, Benade JG, Benade AJ, Kenoyer DG (1999) The nutritional status of a rural community in KwaZulu-Natal, South Africa: the Ndunakazi project. Cent Afr J Med 45: 14–19. [DOI] [PubMed] [Google Scholar]
- 160. Nyirongo LO, Chideme-Maradzika J, Woelk G, Chapman GN, Siziya S (1999) A comparison of nutritional indices of children in Chitungwiza, Zimbabwe, with the international reference standard.[Erratum appears in Can Afr J Med 1999 Oct;45(10):281]. Cent Afr J Med 45: 198–203. [DOI] [PubMed] [Google Scholar]
- 161. Zverev Y, Gondwe M (2001) Growth of urban school children in Malawi. Ann Hum Biol 28: 384–394. [DOI] [PubMed] [Google Scholar]
- 162. Beasley M, Brooker S, Ndinaromtan M, Madjiouroum EM, Baboguel M, et al. (2002) First nationwide survey of the health of schoolchildren in Chad. Trop Med Int Health 7: 625–630. [DOI] [PubMed] [Google Scholar]
- 163. Mukudi E (2003) Nutrition status, education participation, and school achievement among Kenyan middle-school children. Nutrition 19: 612–616. [DOI] [PubMed] [Google Scholar]
- 164. Mukuddem-Petersen J, Kruger HS (2004) Association between stunting and overweight among 10-15-y-old children in the North West Province of South Africa: the THUSA BANA Study. Int J Obes Relat Metab Disord 28: 842–851. [DOI] [PubMed] [Google Scholar]
- 165. Garnier D, Simondon KB, Benefice E (2005) Longitudinal estimates of puberty timing in Senegalese adolescent girls. Am J Human Biol 17: 718–730. [DOI] [PubMed] [Google Scholar]
- 166. Rohner F, Zimmermann MB, Wegmueller R, Tschannen AB, Hurrell RF (2007) Mild riboflavin deficiency is highly prevalent in school-age children but does not increase risk for anaemia in Cote d'Ivoire. Br J Nutr 97: 970–976. [DOI] [PubMed] [Google Scholar]
- 167.Madhavan S, Townsend N (2007) The social context of children's nutritional status in rural South Africa. Scand J Public Health Suppl Supplement. 69: 107–117. [DOI] [PMC free article] [PubMed]
- 168. Ekpo UF, Omotayo AM, Dipeolu MA (2008) Changing lifestyle and prevalence of malnutrition among settled pastoral Fulani children in Southwest Nigeria. Ann Agric Environ Med 15: 187–191. [PubMed] [Google Scholar]
- 169. Anyiam JO, Ogala WN, Onuora CU (2008) Body mass index of healthy Nigerian children. Niger J Med 17: 407–413. [DOI] [PubMed] [Google Scholar]
- 170. Olivieri F, Semproli S, Pettener D, Toselli S (2008) Growth and malnutrition of rural Zimbabwean children (6-17 years of age). Am J Phys Anthropol 136: 214–222. [DOI] [PubMed] [Google Scholar]
- 171. Ayoola O, Ebersole K, Omotade OO, Tayo BO, Brieger WR, et al. (2009) Relative height and weight among children and adolescents of rural southwestern Nigeria. Ann Hum Biol 36: 388–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Amuta EU, Houmsou RS (2009) Assessment of nutritional status of school children in Makurdi, Benue State. Pakistan Journal of Nutrition 8: 691–694. [Google Scholar]
- 173. Bamidele JO, Abodunrin OL, Olajide FO, Oke YF (2010) Prevalence and determinants of anemia among primary school pupils of a peri-urban community in Osun State, Nigeria. Int J Adolesc Med Health 22: 461–468. [DOI] [PubMed] [Google Scholar]
- 174. Olumakaiye MF, Atinmo T, Olubayo-Fatiregun MA (2010) Food consumption patterns of Nigerian adolescents and effect on body weight. J Nutr Educ Behav 42: 144–151. [DOI] [PubMed] [Google Scholar]
- 175.Bogale A, Stoecker BJ, Kennedy T, Hubbs-Tait L, Thomas D, et al.. (2010) Anthropometric measures and cognitive performance of mother-child pairs from Sidama, Southern Ethiopia. FASEB Journal Conference: Experimental Biology 2010, EB Anaheim, CA United States. Conference Start: 20100424 Conference End: 20100428. Conference Publication.
- 176.Mulugeta A, Gebre M, Abdelkadir M, Tsadik AG, yesus A, et al.. (2010) Iron deficiency in adolescent school girls from tigray, northern ethiopia. FASEB Journal Conference: Experimental Biology 2010, EB Anaheim, CA United States. Conference Start: 20100424 Conference End: 20100428. Conference Publication.
- 177.Ramos EM, Munoz JS, Sanchez JCP, Santana ER, Garcia MCV, et al.. (2011) Nutritional assessment in an elementary school in Kenya. Tropical Medicine and International Health Conference: 7th European Congress on Tropical Medicine and International Health Barcelona Spain. Conference Start: 20111003 Conference End: 20111006. Conference Publication: 307.
- 178. Cordeiro LS, Wilde PE, Semu H, Levinson FJ (2012) Household food security is inversely associated with undernutrition among adolescents from Kilosa, Tanzania. J Nutr 142: 1741–1747. [DOI] [PubMed] [Google Scholar]
- 179.Craig EM, Reilly JJ, Bland RM (2012) How best to assess unhealthy weight status? Arch Dis Child Conference: Annual Conference of the Royal College of Paediatrics and Child Health, RCPCH 2012 Glasgow United Kingdom. Conference Start: 20120522 Conference End: 20120524. Conference Publication: A45–A46.
- 180.Amare B, Moges B, Fantahun B, Tafess K, Woldeyohannes D, et al.. (2012) Micronutrient levels and nutritional status of school children living in Northwest Ethiopia. Nutr J 11. [DOI] [PMC free article] [PubMed]
- 181. Neumann CG, Jiang L, Weiss RE, Grillenberger M, Gewa CA, et al. (2013) Meat supplementation increases arm muscle area in Kenyan schoolchildren. Br J Nutr 109: 1230–1240. [DOI] [PubMed] [Google Scholar]
- 182. Degarege A, Erko B (2013) Association between intestinal helminth infections and underweight among school children in Tikur Wuha Elementary School, Northwestern Ethiopia. Journal of Infection and Public Health 6: 125–133. [DOI] [PubMed] [Google Scholar]
- 183.Amare B, Ali J, Moges B, Yismaw G, Belyhun Y, et al.. (2013) Nutritional status, intestinal parasite infection and allergy among school children in Northwest Ethiopia. BMC Pediatr 13. [DOI] [PMC free article] [PubMed]
- 184. Jinabhai CC, Taylor M, Sullivan KR (2003) Implications of the prevalence of stunting, overweight and obesity amongst South African primary school children: a possible nutritional transition? Eur J Clin Nutr 57: 358–365. [DOI] [PubMed] [Google Scholar]
- 185. Onywera VO, Adamo KB, Sheel AW, Waudo JN, Boit MK, et al. (2012) Emerging evidence of the physical activity transition in Kenya. J Phys Act Health 9: 554–562. [DOI] [PubMed] [Google Scholar]
- 186. Goon DT, Toriola AL, Shaw BS (2010) Screening for body-weight disorders in Nigerian children using contrasting definitions. Obes Rev 11: 508–515. [DOI] [PubMed] [Google Scholar]
- 187.Underhay C, De Ridder JH, Van Rooyen JM, Kruger HS (2002) Obesity, blood pressure and physical activity among 10-15 year-old children: The Thusa Bana study. African Journal for Physical, Health Education, Recreation and Dance 8.
- 188. Benefice E, Caius N, Garnier D (2004) Cross-cultural comparison of growth, maturation and adiposity indices of two contrasting adolescent populations in rural Senegal (West Africa) and Martinique (Caribbean). Public Health Nutr 7: 479–485. [DOI] [PubMed] [Google Scholar]
- 189. Agyemang C, Redekop WK, Owusu-Dabo E, Bruijnzeels MA (2005) Blood pressure patterns in rural, semi-urban and urban children in the Ashanti region of Ghana, West Africa. BMC Public Health 5: 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Jinabhai CC, Taylor M, Sullivan KR (2005) Changing patterns of under- and over-nutrition in South African children-future risks of non-communicable diseases. Ann Trop Paediatr 25: 3–15. [DOI] [PubMed] [Google Scholar]
- 191. Monyeki KD, Kemper HC, Makgae PJ (2006) The association of fat patterning with blood pressure in rural South African children: the Ellisras Longitudinal Growth and Health Study. Int J Epidemiol 35: 114–120. [DOI] [PubMed] [Google Scholar]
- 192. Underhay JDR, Van Rooyen JM, Kruger HS (2005) Ethnicity and prevalence of obesity and high blood pressure among 10–15 year-old South African children. African Journal for Physical, Health Education, Recreation and Dance 11: 121–131. [Google Scholar]
- 193. Armstrong ME, Lambert MI, Sharwood KA, Lambert EV (2006) Obesity and overweight in South African primary school children — the Health of the Nation Study. SAMJ , S Suid-Afrikaanse Tydskrif Vir Geneeskunde 96: 439–444. [PubMed] [Google Scholar]
- 194. Kruger R, Kruger HS, Macintyre UE (2006) The determinants of overweight and obesity among 10- to 15-year-old schoolchildren in the North West Province, South Africa - the THUSA BANA (Transition and Health during Urbanisation of South Africans; BANA, children) study. Public Health Nutr 9: 351–358. [DOI] [PubMed] [Google Scholar]
- 195. Jinabhai CC, Reddy P, Taylor M, Monyeki D, Kamabaran N, et al. (2007) Sex differences in under and over nutrition among school-going Black teenagers in South Africa: an uneven nutrition trajectory. Trop Med Int Health 12: 944–952. [DOI] [PubMed] [Google Scholar]
- 196. Semproli S, Gualdi-Russo E (2007) Childhood malnutrition and growth in a rural area of Western Kenya. Am J Phys Anthropol 132: 463–469. [DOI] [PubMed] [Google Scholar]
- 197. Bovet P, Auguste R, Burdette H (2007) Strong inverse association between physical fitness and overweight in adolescents: a large school-based survey. International Journal of Behavioral Nutrition and Physical Activity 4: 05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198. Makgae PJ, Monyeki KD, Brits SJ, Kemper HC, Mashita J (2007) Somatotype and blood pressure of rural South African children aged 6-13 years: Ellisras longitudinal growth and health study. Ann Hum Biol 34: 240–251. [DOI] [PubMed] [Google Scholar]
- 199. Monyeki KD, Kemper HC, Makgae PJ (2008) Relationship between fat patterns, physical fitness and blood pressure of rural South African children: Ellisras Longitudinal Growth and Health Study. J Hum Hypertens 22: 311–319. [DOI] [PubMed] [Google Scholar]
- 200. Goon DT, Toriola AL, Musa DI, Akusu S, Wuam S, et al. (2010) Cardiorespiratory fitness of 7–14 year-old Andibila children in Oju, Nigeria. Gazzetta Medica Italiana Archivio per le Scienze Mediche 169: 287–295. [Google Scholar]
- 201. Koueta F, Dao L, Dao F, Djekompte S, Sawadogo J, et al. (2011) [Factors associated with overweight and obesity in children in Ouagadougou (Burkina Faso)]. [French]. Sante 21: 227–231. [DOI] [PubMed] [Google Scholar]
- 202. Peltzer K, Pengpid S (2011) Overweight and obesity and associated factors among school-aged adolescents in Ghana and Uganda. Int J Environ Res Public Health 8: 3859–3870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Armstrong ME, Lambert MI, Lambert EV (2011) Secular trends in the prevalence of stunting, overweight and obesity among South African children (1994-2004). Eur J Clin Nutr 65: 835–840. [DOI] [PubMed] [Google Scholar]
- 204. Kimani-Murage EW, Kahn K, Pettifor JM, Tollman SM, Klipstein-Grobusch K, et al. (2011) Predictors of adolescent weight status and central obesity in rural South Africa. Public Health Nutr 14: 1114–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205. Amusa LO, Goon DT (2011) Blood pressure among overweight children aged 7-13 years in 10 rural communities in South Africa: The Tshannda Longitudinal Study. Pakistan Journal of Medical Sciences 27: 664–667. [Google Scholar]
- 206. Adamo KB, Sheel AW, Onywera V, Waudo J, Boit M, et al. (2011) Child obesity and fitness levels among Kenyan and Canadian children from urban and rural environments: a KIDS-CAN Research Alliance Study. Int J Pediatr Obes 6: e225–e232. [DOI] [PubMed] [Google Scholar]
- 207.Kemp C, Pienaar AE, Schutte A (2011) The prevalence of hypertension and the relationship with body composition in Grade 1 learners in the North West Province of South Africa. South African Journal of Sports Medicine; Vol 23, No 4 (2011).
- 208. Feeley AB, Musenge E, Pettifor JM, Norris SA (2013) Investigation into longitudinal dietary behaviours and household socio-economic indicators and their association with BMI Z-score and fat mass in South African adolescents: the Birth to Twenty (Bt20) cohort. Public Health Nutr 16: 693–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209. Ene-Obong H, Ibeanu V, Onuoha N, Ejekwu A (2012) Prevalence of overweight, obesity, and thinness among urban school-aged children and adolescents in southern Nigeria. Food Nutr Bull 33: 242–250. [DOI] [PubMed] [Google Scholar]
- 210. Monyeki MA, Neetens R, Moss SJ, Twisk J (2012) The relationship between body composition and physical fitness in 14 year old adolescents residing within the Tlokwe local municipality, South Africa: the PAHL study. BMC Public Health 12: 374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211. Griffiths PL, Sheppard ZA, Johnson W, Cameron N, Pettifor JM, et al. (2012) Associations between household and neighbourhood socioeconomic status and systolic blood pressure among urban South African adolescents. J Biosoc Sci 44: 433–458. [DOI] [PubMed] [Google Scholar]
- 212. Reddy SP, Resnicow K, James S, Funani IN, Kambaran NS, et al. (2012) Rapid increases in overweight and obesity among South African adolescents: comparison of data from the South African National Youth Risk Behaviour Survey in 2002 and 2008. Am J Public Health 102: 262–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213. Moselakgomo VK, Toriola AL, Shaw BS, Goon DT, Akinyemi O (2012) Body mass index, overweight, and blood pressure among adolescent schoolchildren in Limpopo province, South Africa. Revista Paulista de Pediatria 30: 562–569. [Google Scholar]
- 214.Micklesfield L, Pedro T, Twine R, Kinsman J, Pettifor J, et al.. (2012) Physical activity patterns and determinants in rural South African adolescents. Journal of Science and Medicine in Sport Conference: Be Active 2012 Sydney, NSW Australia. Conference Start: 20121031 Conference End: 20121103. Conference Publication: S251.
- 215.Monyeki M, Neetens R, Moss S, Twisk J (2012) Therelationship ofbodycomposition with physical fitness in the 14 years adolescents residing within the Tlokwe Local Municipality, South Africa: The PAHL-Study. Journal of Science and Medicine in Sport Conference: Be Active 2012 Sydney, NSW Australia. Conference Start: 20121031 Conference End: 20121103. Conference Publication: S170–S171.
- 216. Truter L, Pienaar AE, Du TD (2012) The relationship of overweight and obesity to the motor performance of children living in South Africa. South African Family Practice 54: 429–435. [Google Scholar]
- 217. Musa DI, Toriola AL, Monyeki MA, Lawal B (2012) Prevalence of childhood and adolescent overweight and obesity in Benue State, Nigeria. Tropical Medicine and International Health 17: 1369–1375. [DOI] [PubMed] [Google Scholar]
- 218. Bovet P, Paccaud F, Chiolero A (2012) Socio-economic status and obesity in children in Africa. Obes Rev 13: 1080. [DOI] [PubMed] [Google Scholar]
- 219. Toriola OM, Monyeki MA (2012) Health-related fitness, body composition and physical activity status among adolescent learners: The PAHL study. African Journal for Physical, Health Education, Recreation and Dance 18: 795–811. [Google Scholar]
- 220. Wilson ML, Viswanathan B, Rousson V, Bovet P (2013) Weight Status, Body Image and Bullying among Adolescents in the Seychelles. Int J Environ Res Public Health 10: 1763–1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221. Ginsburg C, Griffiths PL, Richter LM, Norris SA (2013) Residential mobility, socioeconomic context and body mass index in a cohort of urban South African adolescents. Health Place 19: 99–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Malete L, Motlhoiwa K, Shaibu S, Wrotniak BH, Maruapula SD, et al.. (2013) Body image dissatisfaction is increased in male and overweight/obese adolescents in Botswana. Journal of Obesity 2013 , 2013. Article Number: 763624. Date of Publication: 2013. [DOI] [PMC free article] [PubMed]
- 223. Mang'eni OR, Maguta K, Thairu K, Takahashi R, Wilunda C (2013) The relation between physical activity and indicators of body fatness in Kenyan adolescents. J Appl Med Sciences 2: 43–59. [Google Scholar]
- 224. Onywera VO, Heroux M, Jaureguiulloa E, Adamo KB, Taylor JL, et al. (2013) Adiposity and physical activity among children in countries at different stages of the physical activity transition: Canada, Mexico and Kenya. AJPHERD 19: 132–142. [Google Scholar]
- 225.Heroux M, Onywera VO, Tremblay MS, Adamo KB, Taylor JL, et al. (2013) The relation between aerobic fitness, muscular fitness, and obesity in children from three countries at different stages of the physical activity transition. ISRN Obesity http://dx.doi.org/10.1155/2013/134835doci. [DOI] [PMC free article] [PubMed]
- 226. Fetuga MB, Ogunlesi TA, Adekanmbi AF, Alabi AD (2011) Growth pattern of schoolchildren in Sagamu, Nigeria using the CDC standards and 2007 WHO standards. Indian Pediatr 48: 523–528. [DOI] [PubMed] [Google Scholar]
- 227. Prista A, Nhantumbo L, Silvio S, Lopes V, Maia J, et al. (2009) Physical activity assessed by accelerometry in rural African school-age children and adolescents. Pediatr Exerc Sci 21: 384–399. [DOI] [PubMed] [Google Scholar]
- 228. Padez C, Varela-Silva MI, Bogin B (2009) Height and relative leg length as indicators of the quality of the environment among Mozambican juveniles and adolescents. Am J Human Biol 21: 200–209. [DOI] [PubMed] [Google Scholar]
- 229. Omigbodun OO, Adediran KI, Akinyemi JO, Omigbodun AO, Adedokun BO, et al. (2010) Gender and rural-urban differences in the nutritional status of in-school adolescents in south-western Nigeria. J Biosoc Sci 42: 653–676. [DOI] [PubMed] [Google Scholar]
- 230. Mosha TC, Fungo S (2010) Prevalence of overweight and obesity among children aged 6-12 years in Dodoma and Kinondoni municipalities, Tanzania. Tanzan J Health Res 12: 6–16. [DOI] [PubMed] [Google Scholar]
- 231. Opara DC, Ikpeme EE, Ekanem US (2010) Prevalence of stunting, underweight and obesity in school aged children in Uyo, Nigeria. Pakistan Journal of Nutrition 9: 459–466. [Google Scholar]
- 232. Nagwa MA, Elhussein AM, Azza M, Abdulhadi NH (2011) Alarming high prevalence of overweight/obesity among Sudanese children. Eur J Clin Nutr 65: 409–411. [DOI] [PubMed] [Google Scholar]
- 233.Dabone C, Delisle HF, Receveur O (2011) Poor nutritional status of schoolchildren in urban and peri-urban areas of Ouagadougou (Burkina Faso). Nutr J 10. [DOI] [PMC free article] [PubMed]
- 234. Goon DT, Toriola AL, Shaw BS, Amusa LO, Monyeki MA, et al. (2011) Anthropometrically determined nutritional status of urban primary schoolchildren in Makurdi, Nigeria. BMC Public Health 11: 769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235. Fetuga MB, Ogunlesi TA, Adekanmbi AF, Alabi AD (2011) Nutritional status of semi-urban Nigerian school children using the 2007 WHO reference population. West Afr J Med 30: 331–336. [PubMed] [Google Scholar]
- 236. Puckree T, Naidoo P, Pill P, Naidoo T (2011) Underweight and Overweight in Primary School Children in eThekwini District in KwaZulu-Natal, South Africa. African Journal of Primary Health Care & Family Medicine 3: 1–6. [Google Scholar]
- 237.Kamau JW, Wanderi MP, Njororai WWS, Wamukoya EK (2011) Prevalence of overweight and obesity among primary school children in Nairobi province, Kenya. African Journal for Physical, Health Education, Recreation and Dance 17.. [Google Scholar]
- 238. Oldewage-Theron W, Napier C, Egal A (2011) Dietary fat intake and nutritional status indicators of primary school children in a low-income informal settlement in the Vaal region. South African Journal of Clinical Nutrition 24: 99–104. [Google Scholar]
- 239. Kramoh KE, N'goran YN, ke-Traboulsi E, Boka BC, Harding DE, et al. (2012) [Prevalence of obesity in school children in Ivory Coast]. [French]. Ann Cardiol Angeiol (Paris) 61: 145–149. [DOI] [PubMed] [Google Scholar]
- 240. Opare-Addo PM, Stowe M, nkobea-Kokroe F, Zheng T (2012) Menarcheal and pubertal development and determining factors among schoolgirls in Kumasi, Ghana. J Obstet Gynaecol 32: 159–165. [DOI] [PubMed] [Google Scholar]
- 241.Motswagole BS, Kruger HS, Faber M, Monyeki KD (2012) Body composition in stunted, compared to non-stunted, black South African children, from two rural communities. South African Journal of Clinical Nutrition 25.. [Google Scholar]
- 242. Puoane TR, Fourie JM, Tsolekile L, Nel JH, Temple NJ (2013) What Do Black South African Adolescent Girls Think About Their Body Size? Journal of Hunger and Environmental Nutrition 8: 85–94. [Google Scholar]
- 243. Wagstaff L, Reinach SG, Richardson BD, Mkhasibe C, de VG (1987) Anthropometrically determined nutritional status and the school performance of black urban primary school children. Hum Nutr Clin Nutr 41: 277–286. [PubMed] [Google Scholar]
- 244. de Villiers FP (1987) The growth pattern of adolescent Tswana schoolchildren. J Trop Pediatr 33: 143–152. [DOI] [PubMed] [Google Scholar]
- 245. Monyeki KD, van Lenthe FJ, Steyn NP (1999) Obesity: does it occur in African children in a rural community in South Africa? Int J Epidemiol 28: 287–292. [DOI] [PubMed] [Google Scholar]
- 246. Jinabhai CC, Taylor M, Coutsoudis A, Coovadia HM, Tomkins AM, et al. (2001) A health and nutritional profile of rural school children in KwaZulu-Natal, South Africa. Ann Trop Paediatr 21: 50–58. [PubMed] [Google Scholar]
- 247. Prista A, Maia JA, Damasceno A, Beunen G (2003) Anthropometric indicators of nutritional status: implications for fitness, activity, and health in school-age children and adolescents from Maputo, Mozambique. Am J Clin Nutr 77: 952–959. [DOI] [PubMed] [Google Scholar]
- 248. Steyn NP, Labadarios D, Maunder E, Nel J, Lombard C, et al. (2005) Secondary anthropometric data analysis of the National Food Consumption Survey in South Africa: the double burden. Nutrition 21: 4–13. [DOI] [PubMed] [Google Scholar]
- 249. Zerfu M, Mekasha A (2006) Anthropometric assessment of school age children in Addis Ababa. Ethiop Med J 44: 347–352. [PubMed] [Google Scholar]
- 250. Longo-Mbenza B, Lukoki LE, M'Buyamba-Kabangu JR (2007) Nutritional status, socio-economic status, heart rate, and blood pressure in African school children and adolescents. Int J Cardiol 121: 171–177. [DOI] [PubMed] [Google Scholar]
- 251. Alaofe H, Zee J, Dossa R, O'Brien HT (2009) Impact of socioeconomic and health related factors on the iron status of adolescent girls from two boarding schools in Southern Benin. Int J Adolesc Med Health 21: 545–554. [DOI] [PubMed] [Google Scholar]
- 252. Kimani-Murage EW, Kahn K, Pettifor JM, Tollman SM, Dunger DB, et al. (2010) The prevalence of stunting, overweight and obesity, and metabolic disease risk in rural South African children. BMC Public Health 10: 158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253. Chukwunonso Ejike ECC, Chidi UE, Lawrence Ezeanyika US (2010) Physical growth and nutritional status of a cohort of semi-urban Nigerian adolescents. Pakistan Journal of Nutrition 9: 392–397. [Google Scholar]
- 254. Truter L, Pienaar AE, Toit D (2010) Relationships between overweight, obesity and physical fitness of nine- to twelve-year-old South African children. South African Family Practice 52: 227–233. [Google Scholar]
- 255. Dapi LN, Janlert U, Nouedoui C, Stenlund H, Haglin L (2009) Socioeconomic and gender differences in adolescents' nutritional status in urban Cameroon, Africa. Nutr Res 29: 313–319. [DOI] [PubMed] [Google Scholar]
- 256. Senbanjo IO, Oshikoya KA (2010) Physical activity and body mass index of school children and adolescents in Abeokuta, Southwest Nigeria. World J Pediatr 6: 217–222. [DOI] [PubMed] [Google Scholar]
- 257. Salman Z, Kirk GD, Deboer MD (2010) High Rate of Obesity-Associated Hypertension among Primary Schoolchildren in Sudan. Int J Hypertens 2011: 629492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258. Odenigbo UM, Nkwoala CC, Okpala OC (2010) Impact of birth weight on the nutritional status and academic performance of school age children. Pakistan Journal of Nutrition 9: 1157–1161. [Google Scholar]
- 259. Croteau K, Schofield G, Towle G, Suresh V (2011) Pedometer-determined physical activity of Western Kenyan children. J Phys Act Health 8: 824–828. [DOI] [PubMed] [Google Scholar]
- 260. Larbi IA, Klipstein-Grobusch K, Amoah AS, Obeng BB, Wilson MD, et al. (2011) High body mass index is not associated with atopy in schoolchildren living in rural and urban areas of Ghana. BMC Public Health 11: 469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261. Goon DT, Toriola AL, Uever JN, Wuam S, Toriola OM (2011) Prevalence of body weight disorders among adolescent school girls in Tarka, Nigeria. Minerva Pediatr 63: 467–471. [PubMed] [Google Scholar]
- 262. Okoh BA, Alikor EA, Akani N (2012) Prevalence of hypertension in primary school-children in Port Harcourt, Nigeria. Paediatr Int Child Health 32: 208–212. [DOI] [PubMed] [Google Scholar]
- 263. Naidoo T, Konkol K, Biccard B, Dudose K, McKune AJ (2012) Elevated salivary C-reactive protein predicted by low cardio-respiratory fitness and being overweight in African children. Cardiovasc 23: 501–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264. Chinedu SN, Eboji OK, Emiloju OC (2012) Trends in weight abnormality of school children and adolescents in Nigeria. Journal of Medical Sciences (Faisalabad) 12: 239–243. [Google Scholar]
- 265.Toriola AL, Moselakgomo VK, Shaw BS, Goon DT (2012) Overweight, obesity and underweight in rural black South African children. South African Journal of Clinical Nutrition 25.
- 266. Davies JC (1971) A screening programme for rural school-children in Rhodesia: pilot study. Dev Med Child Neurol 13: 779–783. [DOI] [PubMed] [Google Scholar]
- 267. Richardson BD, Wadvalla M (1977) The bearing of height, weight and skinfold thickness on obesity in four South African ethnic groups of school pupils of 17 years. Trop Geogr Med 29: 82–90. [PubMed] [Google Scholar]
- 268. Margo G, Baroni Y, Brindley M, Green R, Metz J (1976) Protein energy malnutrition in coloured children in Western Township, Johannesburg. Part II. Prevalence and severity. SAMJ, S Suid-Afrikaanse Tydskrif Vir Geneeskunde. 50: 1241–1245. [PubMed] [Google Scholar]
- 269. Coovadia HM, Adhikari M, Mthethwa D (1978) Physical growth of Negro children in the Durban area. Trop Geogr Med 30: 373–381. [PubMed] [Google Scholar]
- 270. Richardson BD (1977) Underweight, stunting and wasting in black and white South African schoolchildren: malnutrition or adaptation? Trans R Soc Trop Med Hyg 71: 210–216. [DOI] [PubMed] [Google Scholar]
- 271. Richardson BD (1977) Underweight - a nutritional risk? SAMJ, S Suid-Afrikaanse Tydskrif Vir Geneeskunde 51: 42–48. [PubMed] [Google Scholar]
- 272. van Rensburg CF, Booyens J, Gathiram P, Khan J, Luitingh ML, et al. (1977) The relationship between scholastic progress and nutritional status. Part I. A study of 488 school beginners. SAMJ, S Suid-Afrikaanse Tydskrif Vir Geneeskunde 52: 644–649. [PubMed] [Google Scholar]
- 273. Walker AR, Bhamjee D, Walker BF, Richardson BD (1978) Growth, school attendance, and serum albumin levels in South African black children of 10-12 years. J Trop Med Hyg 81: 2–8. [PubMed] [Google Scholar]
- 274. Sukkar MY, Kemm JR, Makeen AM, Khalid MH (1979) Anthropometric survey of children in rural Khartoum, Sudan. Ann Hum Biol 6: 147–158. [DOI] [PubMed] [Google Scholar]
- 275. Carswell F, Hughes AO, Palmer RI, Higginson J, Harland PS, et al. (1981) Nutritional status, globulin titers, and parasitic infections of two populations of Tanzanian school children. Am J Clin Nutr 34: 1292–1299. [DOI] [PubMed] [Google Scholar]
- 276. Oyemade A, Olugbile A, Janes MD (1981) Health of Nigerian rural school children. J Trop Pediatr 27: 101–105. [DOI] [PubMed] [Google Scholar]
- 277. Griffin L, Fast M (1982) A preliminary study on poly-parasitism and the size of primary school children in Kenya. Cent Afr J Med 28: 219–222. [PubMed] [Google Scholar]
- 278. Sukkar MY, Kemm JR, Kardesh M (1982) Age-independent anthropometry: an examination of data from rural Khartoum, Sudan. Ann Hum Biol 9: 265–275. [DOI] [PubMed] [Google Scholar]
- 279. Power DJ (1982) An anthropometric study of young schoolchildren in an area of Cape Town. SAMJ, S Suid-Afrikaanse Tydskrif Vir Geneeskunde 61: 303–305. [PubMed] [Google Scholar]
- 280. Richardson BD, Laing PM, Rantsho JM, Swinel RW (1983) The bearing of diverse patterns of diet on growth and menarche in four ethnic groups of South African girls. J Trop Med Hyg 86: 5–12. [PubMed] [Google Scholar]
- 281. Akesode FA, Ajibode HA (1983) Prevalence of obesity among Nigerian school children. Soc Sci Med 17: 107–111. [DOI] [PubMed] [Google Scholar]
- 282. Ng'andu NH (1984) Growth of urban and rural children in Zambia (a limited study). Med J Zambia 18: 30–35. [PubMed] [Google Scholar]
- 283. Jacobs M, Joubert G, Hoffman M (1988) Anthropometric assessment of children in Mamre. SAMJ, S Suid-Afrikaanse Tydskrif Vir Geneeskunde. 74: 341–343. [PubMed] [Google Scholar]
- 284. Walker AR, Walker BF, Locke MM, Cassim FA, Molefe O (1991) Body image and eating behaviour in interethnic adolescent girls. J R Soc Health 111: 12–16. [DOI] [PubMed] [Google Scholar]
- 285. Ng'andu NH, Watts TE, Siziya S (1992) Age at menarche and the weight-for-height index. SAMJ, S Suid-Afrikaanse Tydskrif Vir Geneeskunde. 81: 408–411. [PubMed] [Google Scholar]
- 286. Cole AH, Taiwo OO, Nwagbara NI, Cole CE (1997) Energy intakes, anthropometry and body composition of Nigerian adolescent girls: a case study of an institutionalized secondary school in Ibadan. Br J Nutr 77: 497–509. [DOI] [PubMed] [Google Scholar]
- 287. Owa JA, Adejuyigbe O (1997) Fat mass, fat mass percentage, body mass index, and mid-upper arm circumference in a healthy population of Nigerian children. J Trop Pediatr 43: 13–19. [DOI] [PubMed] [Google Scholar]
- 288. Sellen DW (2000) Age, sex and anthropometric status of children in an African pastoral community. Ann Hum Biol 27: 345–365. [DOI] [PubMed] [Google Scholar]
- 289. Mabalia-Babela JR, Massamba A, Ntsila R, Senga P (2003) [Nutritional status of school-age children in Brazzaville: effects of environmental factors]. [French]. Arch Pediatr 10: 732–733. [DOI] [PubMed] [Google Scholar]
- 290. Micklesfield LK, Zielonka EA, Charlton KE, Katzenellenbogen L, Harkins J, et al. (2004) Ultrasound bone measurements in pre-adolescent girls: interaction between ethnicity and lifestyle factors. Acta Paediatr 93: 752–758. [DOI] [PubMed] [Google Scholar]
- 291. Calvert J, Burney P (2005) Effect of body mass on exercise-induced bronchospasm and atopy in African children. J Allergy Clin Immunol 116: 773–779. [DOI] [PubMed] [Google Scholar]
- 292. Monyeki MA, Koppes LL, Kemper HC, Monyeki KD, Toriola AL, et al. (2005) Body composition and physical fitness of undernourished South African rural primary school children. Eur J Clin Nutr 59: 877–883. [DOI] [PubMed] [Google Scholar]
- 293. Travill AL (2007) Growth and physical fitness of socially disadvantaged boys and girls aged 8-17 years living in the Western Cape, South Africa. African Journal for Physical, Health Education, Recreation and Dance 13: 279–293. [Google Scholar]
- 294. Jeremiah ZA, Uko EK, Usanga EA (2008) Relation of nutritional status, sickle cell trait, glucose-6-phosphate dehydrogenase deficiency, iron deficiency and asymptomatic malaria infection in the Niger Delta, Nigeria. Journal of Medical Sciences 8: 269–274. [Google Scholar]
- 295. Hawkesworth S, Sawo Y, Fulford AJ, Goldberg GR, Jarjou LM, et al. (2010) Effect of maternal calcium supplementation on offspring blood pressure in 5- to 10-y-old rural Gambian children. Am J Clin Nutr 92: 741–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296. Faye J, Diop M, Gati OR, Seck M, Mandengue SH, et al. (2011) [Prevalence of child and teenage obesity in schools in Dakar]. [French]. Bull Soc Pathol Exot 104: 49–52. [DOI] [PubMed] [Google Scholar]
- 297. Olubanji Ojofeitimi E, Iyanuoluwa Olugbenga-Bello A, debode Adekanle D, Adeomi AA (2011) Pattern and determinants of obesity among adolescent females in private and public schools in olorunda local government area of osun state, Nigeria: a comparative study. Journal of Public Health in Africa 2: e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Monyeki M, Mamabolo R (2012) Relationships between physical activity with BMI and percentage body fat among girls by locality in Tlokwe Local Municipality, South Africa: The PAHL-Study. Journal of Science and Medicine in Sport Conference: Be Active 2012 Sydney, NSW Australia. Conference Start: 20121031 Conference End: 20121103. Conference Publication: S42.
- 299. Cole TJ, Bellizzi MC, Flegal KM, Dietz WH (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320: 1240–1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300. Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, et al. (2002) CDC Growth Charts for the United States: methods and development. Vital Health Stat 11 246: 1–190. [PubMed] [Google Scholar]
- 301. de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J (2007) Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 85: 660–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302. Shields M (2005) Overweight Canadian children and adolescents. Health Rep 17: 27–42. [PubMed] [Google Scholar]
- 303. Tremblay M, Katzmarzyk P, Willms J (2002) Temporal trends in overweight and obesity in Canada, 1981-1996. Int J Obes Relat Metab Disord 26: 538–543. [PubMed] [Google Scholar]
- 304. Ogden CL, Carroll MD, Kit BK, Flegal KM (2012) Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 307: 483–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305. Shields M, Tremblay MS (2010) Canadian obesity estimates based on WHO, IOTF and CDC cut-points. Int J Pediatr Obes 3: 265–73. [DOI] [PubMed] [Google Scholar]
- 306.Benson T, Shekar M. (2006) Trends and issues in child undernutrition. In: Jamison DT, Feachem RG, Makgoba MW, Bos ER, Baingana FK, Hofman KJ, et al., editors. Disease and mortality in Sub-Saharan Africa. 2nd edition. Washington, DC: World Bank. Available: http://www.ncbi.nlm.nih.gov/books/NBK2301/. Accessed 24 June 2013.
- 307. de Onis M, Blössner M, Borghi E, Morris R, Frongillo EA (2004) Methodology for estimating regional and global trends of child malnutrition. Int J Epidemiol 33: 1260–1270. [DOI] [PubMed] [Google Scholar]
- 308.World Health Organization (2003) Global database on child growth and malnutrition. Geneva, Switzerland. [DOI] [PubMed]
- 309. Roberts KC, Shields M, de Groh M, Aziz A, Gilbert JA (2012) Over weight and obesity in children and adolescents: results from the 2009 to 2011 Canadian Health Measures Survey. Health Rep 23: 37–41. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA checklist.
(DOC)