Abstract
Purpose
To evaluate the detectability of urinary stones on virtual nonenhanced images generated at pyelographic-phase dual-energy computed tomography (CT).
Materials and Methods
This retrospective HIPAA-compliant study was institutional review board approved. All included patients had previously consented to the use of their medical records for research. Sixty-two patients (38 men, 24 women; age range, 35–91 years) had undergone CT urography, which consisted of nonenhanced and pyelographic-phase dual-energy CT performed by using a dual-source scanner. Commercial software was used to create virtual nonenhanced images by suppressing the iodine signal from the pyelographic-phase dual-energy CT scans. Two radiologists, in consensus, evaluated the virtual nonenhanced images for the presence of stones. Sensitivity for detecting stones was calculated on a per-stone basis. Sensitivity, specificity, and accuracy were also calculated on a per–renal unit (defined as the intrarenal collecting system and ureter of one kidney) basis. The true nonenhanced scan was considered the reference standard. A jackknife method was used because any patient may have multiple stones.
Results
Of 62 patients with 122 renal units, 21 patients with 25 renal units had a total of 43 stones (maximal transverse diameter range, 1–24 mm; median, 3 mm). The overall sensitivity for detecting stones was 63% (27 of 43 stones) per stone. Sensitivities were 29% (four of 14 stones) for 1–2-mm stones, 64% (nine of 14 stones) for 3–4-mm stones, 83% (five of six stones) for 5–6-mm stones, and 100% (nine of nine stones) for 7-mm or larger (7, 7, 7, 8, 8, 9, 11, 15, and 24 mm) stones. All three ureteral stones (3, 4, and 8 mm) were correctly identified. The sensitivity, specificity, and accuracy for detecting stones on a per–renal unit basis were 65% (17 of 26 renal units), 92% (88 of 96 renal units), and 86% (105 of 122 renal units), respectively.
Conclusion
Virtual nonenhanced images generated at pyelographic-phase dual-energy CT enabled the detection of urinary stones with moderate accuracy. The detection of small (1–2-mm) stones was limited.
© RSNA, 2010
Introduction
The characterization of materials with use of dual-energy computed tomography (CT) was first described in the late 1970s (1,2), but the technique was not adopted widely for clinical use because it required two separate CT examinations at different energies. With the introduction of dual-source, dual-energy CT technology, two scans with two different energy x-ray spectra could be obtained simultaneously, eliminating misregistration due to patient motion (3,4). Dual-energy CT has been shown to be useful for determining the composition of urinary stones (5) and subtracting bone or calcium plaques at CT angiography (3,6,7). In addition, the virtual nonenhanced technique of subtracting iodine from contrast material–enhanced dual-energy CT acquisitions shows promise as a substitute for nonenhanced CT scanning. The virtual nonenhanced technique previously has been applied for the evaluation of endoleaks after abdominal aortic aneurysm repair (8,9), pulmonary nodules (10), and renal masses (11,12).
Nonenhanced CT is the reference standard for the detection of urinary stones, which are often obscured by high-attenuating iodinated contrast material in the renal parenchyma or collecting system (13). With use of a phantom model, the dual-energy CT iodine-subtraction virtual nonenhanced technique was shown to be capable of depicting urinary stones submerged in iodine solutions (14). Investigators in an earlier clinical study also demonstrated that virtual nonenhanced images reconstructed from nephrographic-phase scans may be helpful for detecting urinary stones (15).
CT urography consists of nonenhanced scanning followed by pyelographic-phase scanning after the administration of iodinated contrast material. Nonenhanced scans are obtained mainly to determine the presence or absence of urinary stones, whereas pyelographic-phase scans are obtained to determine the presence or absence of urothelial abnormalities (primarily transitional cell carcinoma) (16–19). With the creation of virtual nonenhanced CT scans from pyelographic-phase images, one of the main purposes of nonenhanced CT during CT urography could be achieved without obtaining a true nonenhanced scan for the detection of urinary stones. The purpose of our investigation was to evaluate the detectability of urinary stones with virtual nonenhanced images generated at pyelographic-phase dual-energy CT.
Materials and Methods
Three authors (A.N.P., J.G.F., C.H.M.) received partial funding from Siemens Healthcare (Forchheim, Germany), the manufacturer of the CT scanner used in this study, and one author (A.N.P.) is currently employed by Siemens Healthcare. The other authors had control over the data and information submitted for publication.
Patient Population
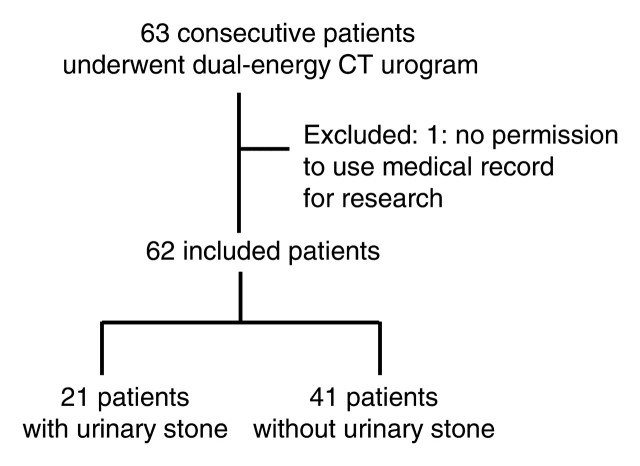
This retrospective Health Insurance Portability and Accountability Act–compliant study was approved by our institutional review board. Of the 63 consecutive patients who underwent dual-energy CT urography between February 2008 and October 2008, 62 (mean age, 66.1 years; age range, 35–91 years) had data that were included in the study. There were 38 men (mean age, 66.0 years; age range, 42–83 years) and 24 women (mean age, 66.2 years; age range, 35–91 years) (overall mean body weight, 79 kg; weight range, 49–115 kg). One patient did not give permission for the use of medical records for research and thus was excluded (Fig 1). No other patient was excluded. All other patients had previously consented to have their medical records used for research purposes. At our institution, dual-energy scanning is routinely performed when patients are scheduled on a dual-source CT scanner for clinically indicated abdominal or pelvic CT. This is because dual-energy CT images (with blending of low– and high–kilovolt peak images) are equivalent in image quality to single-energy CT images, given that the same radiation dose is administered to the patient (20). Dual-energy CT has the potential for added value—for example, in differentiating uric acid from non–uric acid stones or improving the conspicuity of iodinated contrast material (20). Due to tube current limitations of the low-tube-potential setting, we generally acquire single-energy scans rather than dual-energy scans in our practice for patients who weigh more than 110 kg. Thus, only one patient in our study population had a body weight of more than 110 kg. Indications for CT urography included hematuria (n = 42), known or history of urinary stone disease (n = 12), work-up of urinary tract malignancy (n = 7), and bladder outlet obstruction (n = 1).
Figure 1:
Flowchart of patient exclusion and inclusion for dual-energy CT urography and the presence or absence of urinary tract stones.
CT Protocol
All CT images were obtained with a dual-source CT scanner (Somatom Definition DS, software version VA20; Siemens Healthcare). Fifty-three patients underwent split-bolus two-phase (nonenhanced and combined nephrographic-pyelographic phases) CT urography, and nine underwent single-bolus three-phase (nonenhanced, nephrographic, and pyelographic phases) CT urography. One of the two protocols was chosen according to our standard clinical practice. At our institution, split-bolus two-phase CT urography is generally used for patients with a relatively low risk of malignancy, and single-bolus three-phase CT urography is generally used for patients with a relatively high risk of malignancy, those with renal insufficiency, and those requiring simultaneous evaluation of renal parenchymal or other solid organ lesions. For the split-bolus two-phase CT urography protocol, nonenhanced scanning was initially performed from the kidneys to the bladder. Then, 50 mL of intravenous contrast material (iohexol, Omnipaque 300; GE Healthcare, Milwaukee, Wis) was administered at a rate of 4 mL/sec and followed by 200 mL of saline administered at the same rate by using a power injector. After a 10-minute delay, an additional 90 mL of contrast material was administered at 4 mL/sec. Contrast-enhanced scanning through the abdomen and pelvis was performed 70 seconds after the second bolus of contrast material. For the single-bolus three-phase CT urography protocol, nonenhanced scanning was initially performed from the kidneys to the bladder. Contrast-enhanced scans through the abdomen and pelvis were then obtained 70 seconds after 100–140 mL of intravenous contrast material was administered at a rate of 4 mL/sec by using a power injector. After acquisition of the nephrographic scan, 200 mL of saline was administered. After a 10-minute delay from the start of contrast material administration, a second contrast-enhanced scan through the abdomen and pelvis was obtained. Abdominal compression was used for the pyelographic phase in 60 patients as previously described (17). Abdominal compression was not used in two patients because of a known obstructive renal stone or abdominal aortic aneurysm. Nonenhanced and pyelographic-phase scans were obtained by using the dual-energy mode (140 kVp and 80 kVp) with a collimation of 14 × 1.2 mm. Automatic exposure control (CareDose4D; Siemens Healthcare) was used with quality reference amperage values of 80 mAs for 140-kVp tubes and 340 mAs for 80-kVp tubes. The scanning parameters were set such that the radiation dose for dual-energy CT, as reflected by the volume CT dose index, was comparable to the dose for single-energy CT at our institution, nominally 18 mGy. The ratio of the amperage values for 80- and 140-kVp tubes was chosen to result in similar noise levels on the 80- and 140-kVp images. Nonenhanced images were reconstructed with 5-mm-thick sections and a 2.5-mm reconstruction increment, and pyelographic-phase scans were reconstructed with 1.5-mm-thick sections and 1.5-mm reconstruction increments.
Iodine-Subtraction Virtual Nonenhanced Image Processing
Iodine-subtraction virtual nonenhanced images were generated from the pyelographic-phase CT scans at an independent workstation (Syngo Multi Modality Workplace; Siemens Healthcare) by using commercially available software (Syngo, Dual Energy Viewer; Siemens Healthcare). Dual-energy processing took less than 1 minute per patient. The default dual-energy ratio (2.0), defined as the ratio of CT attenuation values of iodine measured on 80- and 140-kVp scans, was used to generate virtual nonenhanced images. Images were generated with 1.5-mm-thick sections.
Image Interpretation
The virtual nonenhanced images generated from pyelographic-phase images obtained in all patients were reviewed in consensus by two radiologists (T.J.V., A.K., 16 and 19 years experience in abdominal radiology, respectively) at a workstation (Advantage Window 4.2; GE Healthcare). Pyelographic-phase images without iodine subtraction were also presented and were used to verify the location of the calcification identified on the virtual nonenhanced images and to determine if the calcifications were inside or outside the urinary tract. The readers were blinded to other imaging and clinical information. The default display window width and level settings were 450 and 40 HU, respectively, but the readers were allowed to change the window settings as necessary. When readers identified a urinary stone, its anatomic location and section position were recorded. A third radiologist (N.T., 10 years experience in abdominal radiology) reviewed the pyelographic-phase images without iodine subtraction and evaluated the presence of a urinary tract stone. This reviewer also was blinded to other imaging and clinical information. The default display window width and level settings were 2000 and 300 HU, respectively, but the reviewer was allowed to change the window settings as necessary. The location of the stone(s) was similarly recorded. At a different session, the third radiologist reviewed the true nonenhanced images, which were used as the reference standard, and identified urinary tract stones. The maximal diameter of the stones in the transverse plane was measured (N.T.) by using electronic calipers on the true nonenhanced images and virtual nonenhanced images at two different sessions. The urinary stones identified on the virtual nonenhanced images were matched to the stones identified on the true nonenhanced images. Potential reasons for the false-negative and false-positive findings on the virtual nonenhanced images were also identified (N.T.) by comparing the virtual nonenhanced images and true nonenhanced images.
Statistical Analyses
Statistical software (S-PLUS, version 8.01; Insightful, Seattle, Wash) was used for statistical analyses. The sensitivity in the detection of urinary stones on virtual nonenhanced images was calculated per stone. Sensitivities were also calculated for separate ranges of stone size. Sensitivity, specificity, and accuracy were calculated on a per–renal unit basis. Renal unit was defined as the intrarenal collecting system and ureter of one kidney. The 95% confidence interval (CI) was also calculated. A jackknife method was used because any patient may have multiple stones. When the sensitivity was 100%, the 95% CI was calculated on the basis of binomial distribution. The sensitivity in the detection of a urinary stone on pyelographic-phase images without iodine subtraction was also calculated. Maximal diameters of the stones were compared between the true nonenhanced and virtual nonenhanced images.
Results
Of 62 patients with 122 renal units, 21 patients had a total of 43 stones (40 in the kidney, three in the ureter; maximal diameter, 1–24 mm; median diameter, 3 mm) in 25 renal units. The overall sensitivity for stone detection on a per-stone basis was 63% (27 of 43 stones; 95% CI: 42.8%, 82.8%) with use of the virtual nonenhanced images generated from the pyelographic-phase scans (Fig 2). Sensitivities were 29% (four of 14 stones; 95% CI: 3.8%, 53.4%) for 1–2-mm stones, 64% (nine of 14 stones; 95% CI: 30.5%, 98.1%) for 3–4-mm stones, 83% (five of six stones; 95% CI: 42.8%, 100%) for 5–6-mm stones, and 100% (nine of nine stones; 95% CI: 66.4%, 100%) for 7-mm or larger (stone sizes: 7, 7, 7, 8, 8, 9, 11, 15, and 24 mm) stones. All three ureteral stones (3, 4, and 8 mm) were correctly identified (Fig 3). The sensitivity, specificity, and accuracy for detecting stones on a per–renal unit basis were 65% (17 of 26 renal units; 95% CI: 45.3%, 85.5%), 92% (88 of 96 renal units; 95% CI: 85.6%, 97.8%), and 86% (105 of 122 renal units; 95% CI: 79.9%, 92.3%), respectively. With use of pyelographic-phase images without iodine subtraction, the sensitivity for stone detection on a per-stone basis was 9% (four of 43 stones).
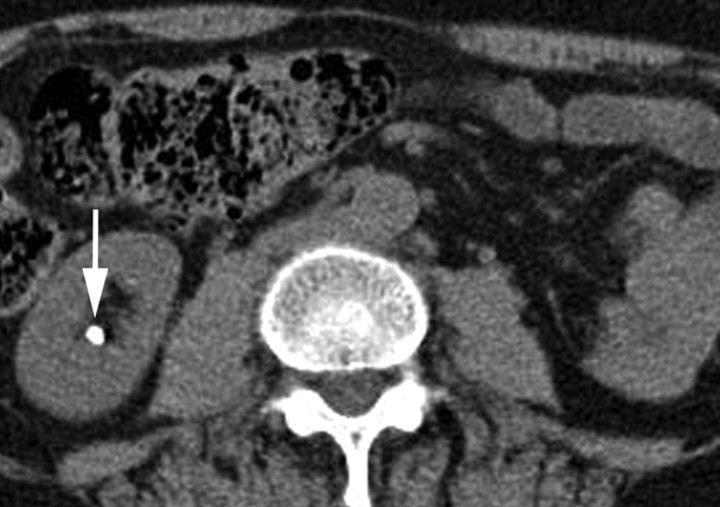
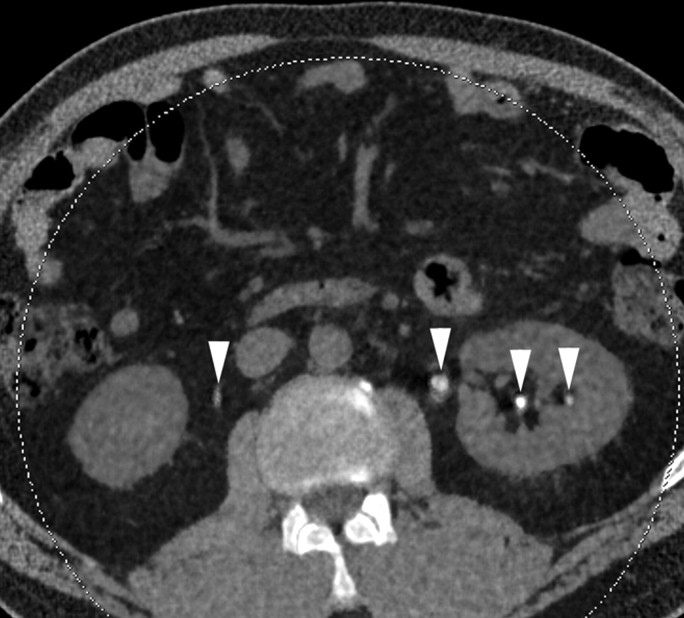
Figure 2a:
Transverse CT images in 61-year-old woman with multiple renal stones. (a, b) True nonenhanced scans show 2-mm (a) and 5-mm (b) calyceal stones (arrow) in lower pole of right kidney. (c, d) Corresponding pyelographic-phase images show iodinated contrast material (arrowheads) in collecting systems, obscuring renal stones. (e, f) Corresponding virtual nonenhanced images created from pyelographic-phase scans show removal of iodine signal from collecting systems. The 5-mm stone (arrow in f) in right kidney is visible as high-attenuating material, but the 2-mm stone is not identifiable in e owing to oversubtraction of stone signal.
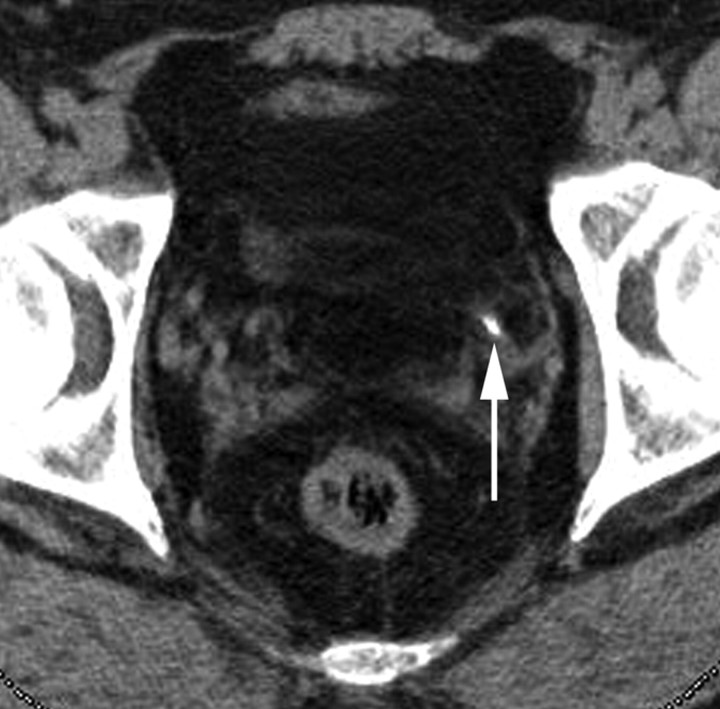
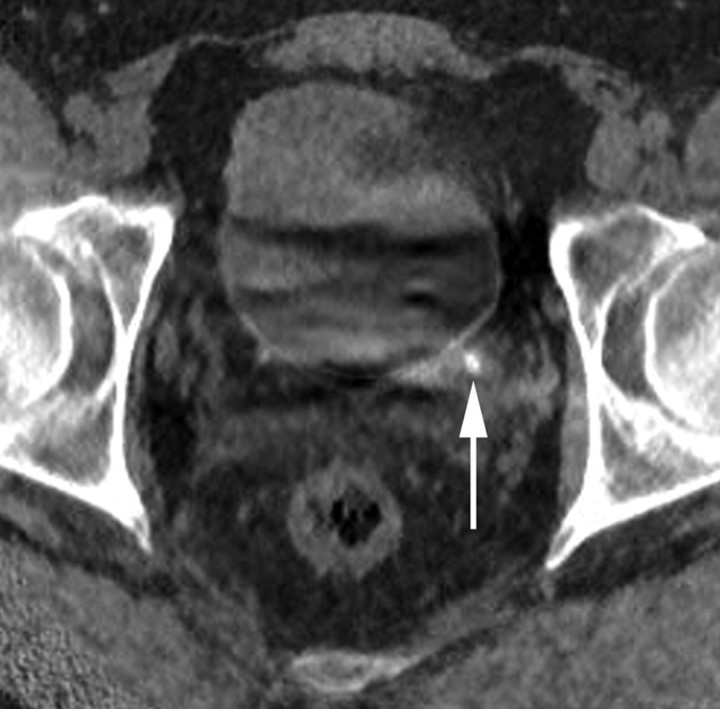
Figure 3a:
Transverse CT images in 44-year-old man with left distal ureteral stone. (a) True nonenhanced scan shows 3-mm stone (arrow) in distal left ureter. (b) Pyelographic-phase image shows iodinated contrast material in ureters and bladder, obscuring nonobstructing ureteral stone. (c) Virtual nonenhanced image created from pyelographic-phase scan shows removal of iodine signal from ureters and bladder. Left distal ureteral stone (arrow) is visible as high-attenuating material.
Figure 2b:
Transverse CT images in 61-year-old woman with multiple renal stones. (a, b) True nonenhanced scans show 2-mm (a) and 5-mm (b) calyceal stones (arrow) in lower pole of right kidney. (c, d) Corresponding pyelographic-phase images show iodinated contrast material (arrowheads) in collecting systems, obscuring renal stones. (e, f) Corresponding virtual nonenhanced images created from pyelographic-phase scans show removal of iodine signal from collecting systems. The 5-mm stone (arrow in f) in right kidney is visible as high-attenuating material, but the 2-mm stone is not identifiable in e owing to oversubtraction of stone signal.
Figure 2c:
Transverse CT images in 61-year-old woman with multiple renal stones. (a, b) True nonenhanced scans show 2-mm (a) and 5-mm (b) calyceal stones (arrow) in lower pole of right kidney. (c, d) Corresponding pyelographic-phase images show iodinated contrast material (arrowheads) in collecting systems, obscuring renal stones. (e, f) Corresponding virtual nonenhanced images created from pyelographic-phase scans show removal of iodine signal from collecting systems. The 5-mm stone (arrow in f) in right kidney is visible as high-attenuating material, but the 2-mm stone is not identifiable in e owing to oversubtraction of stone signal.
Figure 2d:
Transverse CT images in 61-year-old woman with multiple renal stones. (a, b) True nonenhanced scans show 2-mm (a) and 5-mm (b) calyceal stones (arrow) in lower pole of right kidney. (c, d) Corresponding pyelographic-phase images show iodinated contrast material (arrowheads) in collecting systems, obscuring renal stones. (e, f) Corresponding virtual nonenhanced images created from pyelographic-phase scans show removal of iodine signal from collecting systems. The 5-mm stone (arrow in f) in right kidney is visible as high-attenuating material, but the 2-mm stone is not identifiable in e owing to oversubtraction of stone signal.
Figure 2e:
Transverse CT images in 61-year-old woman with multiple renal stones. (a, b) True nonenhanced scans show 2-mm (a) and 5-mm (b) calyceal stones (arrow) in lower pole of right kidney. (c, d) Corresponding pyelographic-phase images show iodinated contrast material (arrowheads) in collecting systems, obscuring renal stones. (e, f) Corresponding virtual nonenhanced images created from pyelographic-phase scans show removal of iodine signal from collecting systems. The 5-mm stone (arrow in f) in right kidney is visible as high-attenuating material, but the 2-mm stone is not identifiable in e owing to oversubtraction of stone signal.
Figure 2f:
Transverse CT images in 61-year-old woman with multiple renal stones. (a, b) True nonenhanced scans show 2-mm (a) and 5-mm (b) calyceal stones (arrow) in lower pole of right kidney. (c, d) Corresponding pyelographic-phase images show iodinated contrast material (arrowheads) in collecting systems, obscuring renal stones. (e, f) Corresponding virtual nonenhanced images created from pyelographic-phase scans show removal of iodine signal from collecting systems. The 5-mm stone (arrow in f) in right kidney is visible as high-attenuating material, but the 2-mm stone is not identifiable in e owing to oversubtraction of stone signal.
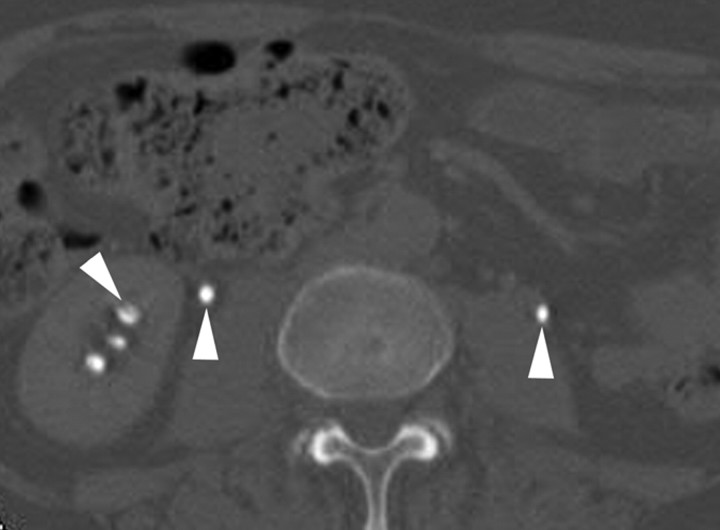
Figure 3b:
Transverse CT images in 44-year-old man with left distal ureteral stone. (a) True nonenhanced scan shows 3-mm stone (arrow) in distal left ureter. (b) Pyelographic-phase image shows iodinated contrast material in ureters and bladder, obscuring nonobstructing ureteral stone. (c) Virtual nonenhanced image created from pyelographic-phase scan shows removal of iodine signal from ureters and bladder. Left distal ureteral stone (arrow) is visible as high-attenuating material.
Figure 3c:
Transverse CT images in 44-year-old man with left distal ureteral stone. (a) True nonenhanced scan shows 3-mm stone (arrow) in distal left ureter. (b) Pyelographic-phase image shows iodinated contrast material in ureters and bladder, obscuring nonobstructing ureteral stone. (c) Virtual nonenhanced image created from pyelographic-phase scan shows removal of iodine signal from ureters and bladder. Left distal ureteral stone (arrow) is visible as high-attenuating material.
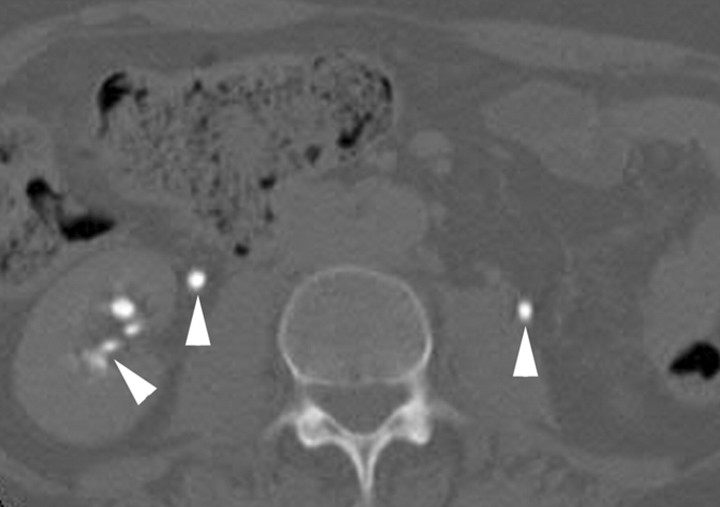
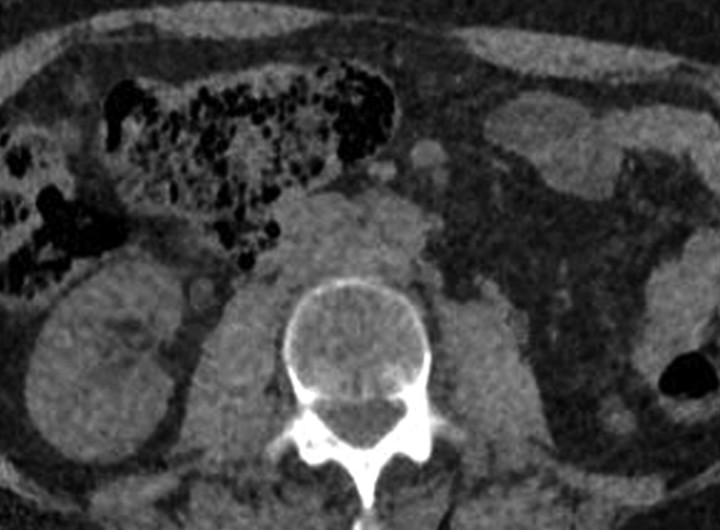
There were 16 false-negative stones on the virtual nonenhanced scans. Ten of these stones were 1–2 mm in size and were undetectable, even in retrospect, on the virtual nonenhanced scan; presumably, this was mainly due to subtraction of the stone signal (oversubtraction). Five missed stones were 3–4 mm in size, and three were undetectable, even in retrospect, on the virtual nonenhanced scan—again presumably owing to subtraction of the stone signal (oversubtraction). Two stones were detectable in retrospect. A 5-mm stone was not detectable; diffuse nonsubtracted iodine signal (undersubtraction) in the urinary tract obscured the stone (Fig 4). This presumably occurred because the CT attenuation value of urine was high, reaching the maximal measurable attenuation of 3070 HU on 80-kVp images and resulting in failed iodine subtraction. There were 10 regions where a small, 1–2-mm area of nonsubtracted iodine signal (undersubtraction) in the calyces was mistaken for small stones, resulting in eight false-positive renal units.
Figure 4:
Transverse virtual nonenhanced CT image created from pyelographic-phase scan in 51-year-old man with left renal stone shows iodinated contrast material (arrowheads) in renal collecting system and ureter due to failed iodine signal removal. Stone in left kidney is not detectable because of nonsubtracted iodine signal (not shown).
Of the 29 identifiable stones on the virtual nonenhanced images, 19 had a maximal diameter that was 1–2 mm smaller on the virtual nonenhanced images than on the true nonenhanced images, nine stones were equal in size, and one stone was 1 mm larger.
Discussion
Iodine-subtraction virtual nonenhanced images created from dual-energy pyelographic-phase CT scans enabled the detection of urinary stones with a sensitivity of 63% (27 of 43 stones) on a per-stone basis. The sensitivity for the detection of 3-mm or larger stones was 79% (23 of 29 stones). All three ureteral stones, which were clinically most important, were detectable.
Scheffel et al (15) found that virtual nonenhanced CT scans created from nephrographic-phase CT images enabled the detection of urinary stones, with a sensitivity of 74% (26 of 35 stones) on a per-stone basis. However, the original nephrographic-phase CT images without iodine subtraction had a sensitivity of 94% (33 of 35 stones) (15). Thus, virtual nonenhanced CT images did not have added value to the original nephrographic-phase CT scans. In our study, virtual nonenhanced CT scans were created from pyelographic-phase CT images. The original pyelographic-phase CT images without iodine subtraction had a sensitivity of 9% (four of 43 stones). Hence, the dual-energy CT virtual nonenhanced CT images improved stone detection.
Two typical CT urography protocols include single-bolus three-phase (nonenhanced, nephrographic, and pyelographic phases) protocols and split-bolus two-phase (nonenhanced and combined nephrographic-pyelographic phases) protocols. At our institution, most of our CT urography studies are performed by using the split-bolus two-phase protocol to decrease the radiation dose to the patient (21). Nephrographic and pyelographic phases are combined with this protocol; thus, virtual nonenhanced CT images could not be created from pure nephrographic-phase CT images as in the previous study (15). Therefore, we evaluated virtual nonenhanced CT images created from the pyelographic-phase dual-energy CT scans in this study.
Most stones detected appeared slightly smaller on the virtual nonenhanced images than on the true nonenhanced images. This was probably due to subtraction of some stone signal from the stone periphery along with the iodine signal. In addition, collimation of the dual-energy pyelographic-phase scans was 1.2 mm compared with 0.6 mm for the single-energy CT urograms obtained at our institution. The relatively low z-axis resolution probably did not allow separation of the small stones and iodine in the urinary tract because of volume averaging. This probably explains the low rate of detecting 1–2-mm stones (28%).
One 5-mm stone was not detectable in this study because of inadequate iodine subtraction, presumably due to the high CT attenuation of urine. In a phantom study, poor subtraction of iodine occurred when the attenuation of the iodine solution was extremely high, causing breakdown of the subtraction algorithm (14).
Even though most ureteral stones smaller than 3 mm pass spontaneously (22), the detection of such stones is often clinically important. Small intrarenal stones seldom cause symptoms, but they can be the cause of microscopic hematuria. Thus, it is unlikely that, with use of the current dual-energy CT technology and algorithms, virtual nonenhanced CT images created from pyelographic-phase scans can replace true nonenhanced CT images in patients with hematuria or those suspected of having urinary stone disease. However, this technique may be useful for selected patients in whom the clinical effect of detecting small urinary stones is low.
Dual-energy CT performed after the administration of iodinated contrast material also has the potential to enable characterization of renal mass enhancement with use of the virtual nonenhanced technique (11,12). Therefore, virtual nonenhanced images reconstructed from dual-energy pyelographic-phase CT scans have the potential to depict urinary stones and help characterize renal masses without the use of true nonenhanced CT. Depending on the acquisition techniques, the elimination of nonenhanced CT from CT urography acquisitions could lead to a 20%–50% reduction in the overall radiation dose to the patient (21). The radiation dose with dual-energy scanning at 80–140 kVp is comparable to the dose with single-energy scanning at 120 kVp to achieve a similar image quality or noise level (4,23).
Dual-energy CT technology continues to evolve. One of the recent advances includes the use of a tin filter applied to the high-energy x-ray tube. The separation of the high- and low-energy x-ray spectra has improved, allowing better material characterization (24). The other recent improvement is an increase in the maximal field of view of dual-energy iodine-subtraction virtual nonenhanced images, which has facilitated a decreased risk of missing relevant urinary anatomy. The second detector of the dual-source CT scanner used in this study has a maximal field of view of 26 cm, whereas the primary detector has a 50-cm field of view. Thus, the virtual nonenhanced images have a maximal field of view of 26 cm, requiring careful positioning of patients in the CT scanner to ensure full coverage of the urinary system.
Our study had a number of limitations. The study was retrospective. In addition, the virtual nonenhanced images were reviewed by two radiologists in consensus; thus, interobserver variability was not assessed. The section thickness for the true nonenhanced images was 5 mm, whereas that for the pyelographic-phase and virtual nonenhanced images was 1.5 mm. One radiologist evaluated the true nonenhanced images, measured the size of stones on the true nonenhanced and virtual nonenhanced images, and identified potential reasons for the false-negative and false-positive findings. This may have led to bias in our results. Finally, only one patient weighing more than 110 kg was included in our study. We generally use the single-energy mode when a patient weighs more than 110 kg because the image quality of the 80-kVp tube for obese patients is often compromised because the CT system is not able to generate sufficient tube currents (20). We do not know the performance of this technique in larger patients.
In conclusion, dual-energy iodine-subtraction virtual nonenhanced images generated from pyelographic-phase CT scans can depict urinary stones. Recent advances in the dual-energy iodine-subtraction CT technique require further investigation.
Advances in Knowledge.
-
•.
Virtual nonenhanced images generated at pyelographic-phase dual-energy CT enable the detection of urinary stones with an accuracy of 86% on a per–renal unit basis.
-
•.
Stone detection rates were 29% for 1–2-mm stones, 64% for 3–4-mm stones, 83% for 5–6-mm stones, and 100% for 7-mm or larger stones.
Implication for Patient Care.
-
•.
Virtual nonenhanced images generated at pyelographic-phase dual-energy CT are potential substitutes for nonenhanced CT scans in select patients in whom the clinical effect of detecting small urinary stones is small.
Acknowledgments
We thank Patrick D. Fitz-Gibbon, BS, and Jay Mandrekar, PhD, for statistical support.
Received August 7, 2009; revision requested September 25; revision received November 23; accepted January 11, 2010; final version accepted February 3.
See Materials and Methods for pertinent disclosures.
Abbreviation:
- CI
- confidence interval
References
- 1.Millner MR, McDavid WD, Waggener RG, Dennis MJ, Payne WH, Sank VJ. Extraction of information from CT scans at different energies. Med Phys 1979;6(1):70–71. [DOI] [PubMed] [Google Scholar]
- 2.Chiro GD, Brooks RA, Kessler RM, et al. Tissue signatures with dual-energy computed tomography. Radiology 1979;131(2):521–523. [DOI] [PubMed] [Google Scholar]
- 3.Johnson TR, Nikolaou K, Wintersperger BJ, et al. Dual-source CT cardiac imaging: initial experience. Eur Radiol 2006;16(7):1409–1415. [DOI] [PubMed] [Google Scholar]
- 4.Johnson TR, Krauss B, Sedlmair M, et al. Material differentiation by dual energy CT: initial experience. Eur Radiol 2007;17(6):1510–1517. [DOI] [PubMed] [Google Scholar]
- 5.Primak AN, Fletcher JG, Vrtiska TJ, et al. Noninvasive differentiation of uric acid versus non-uric acid kidney stones using dual-energy CT. Acad Radiol 2007;14(12):1441–1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lell MM, Kramer M, Klotz E, Villablanca P, Ruehm SG. Carotid computed tomography angiography with automated bone suppression: a comparative study between dual energy and bone subtraction techniques. Invest Radiol 2009;44(6):322–328. [DOI] [PubMed] [Google Scholar]
- 7.Brockmann C, Jochum S, Sadick M, et al. Dual-energy CT angiography in peripheral arterial occlusive disease. Cardiovasc Intervent Radiol 2009;32(4):630–637. [DOI] [PubMed] [Google Scholar]
- 8.Chandarana H, Godoy MC, Vlahos I, et al. Abdominal aorta: evaluation with dual-source dual-energy multidetector CT after endovascular repair of aneurysms—initial observations. Radiology 2008;249(2):692–700. [DOI] [PubMed] [Google Scholar]
- 9.Stolzmann P, Frauenfelder T, Pfammatter T, et al. Endoleaks after endovascular abdominal aortic aneurysm repair: detection with dual-energy dual-source CT. Radiology 2008;249(2):682–691. [DOI] [PubMed] [Google Scholar]
- 10.Chae EJ, Song JW, Seo JB, Krauss B, Jang YM, Song KS. Clinical utility of dual-energy CT in the evaluation of solitary pulmonary nodules: initial experience. Radiology 2008;249(2):671–681. [DOI] [PubMed] [Google Scholar]
- 11.Brown CL, Hartman RP, Dzyubak OP, et al. Dual-energy CT iodine overlay technique for characterization of renal masses as cyst or solid: a phantom feasibility study. Eur Radiol 2009;19(5):1289–1295. [DOI] [PubMed] [Google Scholar]
- 12.Graser A, Johnson TR, Hecht EM, et al. Dual-energy CT in patients suspected of having renal masses: can virtual nonenhanced images replace true nonenhanced images? Radiology 2009;252(2):433–440. [DOI] [PubMed] [Google Scholar]
- 13.Smith RC, Rosenfield AT, Choe KA, et al. Acute flank pain: comparison of non-contrast-enhanced CT and intravenous urography. Radiology 1995;194(3):789–794. [DOI] [PubMed] [Google Scholar]
- 14.Takahashi N, Hartman RP, Vrtiska TJ, et al. Dual-energy CT iodine-subtraction virtual unenhanced technique to detect urinary stones in an iodine-filled collecting system: a phantom study. AJR Am J Roentgenol 2008;190(5):1169–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scheffel H, Stolzmann P, Frauenfelder T, et al. Dual-energy contrast-enhanced computed tomography for the detection of urinary stone disease. Invest Radiol 2007;42(12):823–829. [DOI] [PubMed] [Google Scholar]
- 16.McNicholas MM, Raptopoulos VD, Schwartz RK, et al. Excretory phase CT urography for opacification of the urinary collecting system. AJR Am J Roentgenol 1998;170(5):1261–1267. [DOI] [PubMed] [Google Scholar]
- 17.Chow LC, Sommer FG. Multidetector CT urography with abdominal compression and three-dimensional reconstruction. AJR Am J Roentgenol 2001;177(4):849–855. [DOI] [PubMed] [Google Scholar]
- 18.Kawashima A, Glockner JF, King BF. CT urography and MR urography. Radiol Clin North Am 2003;41(5):945–961. [DOI] [PubMed] [Google Scholar]
- 19.Nolte-Ernsting C, Cowan N. Understanding multislice CT urography techniques: many roads lead to Rome. Eur Radiol 2006;16(12):2670–2686. [DOI] [PubMed] [Google Scholar]
- 20.Fletcher JG, Takahashi N, Hartman R, et al. Dual-energy and dual-source CT: is there a role in the abdomen and pelvis? Radiol Clin North Am 2009;47(1):41–57. [DOI] [PubMed] [Google Scholar]
- 21.Vrtiska TJ, Hartman RP, Kofler JM, Bruesewitz MR, King BF, McCollough CH. Spatial resolution and radiation dose of a 64-MDCT scanner compared with published CT urography protocols. AJR Am J Roentgenol 2009;192(4):941–948. [DOI] [PubMed] [Google Scholar]
- 22.Takahashi N, Kawashima A, Ernst RD, et al. Ureterolithiasis: can clinical outcome be predicted with unenhanced helical CT? Radiology 1998;208(1):97–102. [DOI] [PubMed] [Google Scholar]
- 23.Yu L, Primak AN, Liu X, McCollough CH. Image quality optimization and evaluation of linearly mixed images in dual-source, dual-energy CT. Med Phys 2009;36(3):1019–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Primak AN, Ramirez Giraldo JC, Liu X, Yu L, McCollough CH. Improved dual-energy material discrimination for dual-source CT by means of additional spectral filtration. Med Phys 2009;36(4):1359–1369. [DOI] [PMC free article] [PubMed] [Google Scholar]