Abstract
♦ Introduction: Peritonitis remains the main cause of peritoneal dialysis (PD) technique failure worldwide, despite significant reductions in infection rates observed over the past decades. Several studies have described risk factors for peritonitis, technique failure and mortality. However, there are scarce data regarding predictors of complications during and after a peritonitis episode. The aim of our study was to analyze predictors of peritonitis-related outcome in the Brazilian Peritoneal Dialysis study (BRAZPD) cohort.
♦ Methods: All adult incident patients recruited in the BRAZPD Study between December 2004 and October 2007, who remained at least 90 days on PD and presented their first peritonitis episode (n = 474 patients) were included in the study. The endpoints analyzed were non-resolution, death due to a peritonitis episode and long-term technique survival after a peritonitis episode.
♦ Results: In the multivariable regression, non-resolution was independently associated with older age (odds ratio (OR) 1.02; p < 0.01), collagenosis as the primary renal disease (OR 4.6; p < 0.05) and Pseudomonas spp as etiological agent (OR 2.9; p < 0.05). Patients who were transferred from APD to CAPD during peritonitis therapy presented a higher risk of non-response (OR 2.5; p < 0.05). The only factor associated with death during a peritonitis episode was older age (OR 1.04; p < 0.05). Exposure to vancomycin and male gender were the independent predictors of long-term technique failure (OR 2.2; p < 0.01).
♦ Conclusion: Apart from confirming previous observations of the negative impact of older age and Pseudomonas spp peritonitis on outcomes, we observed that collagenosis may negatively impact response to treatment and exposure to vancomycin may possibly reduce long-term technique survival. It is important to emphasize that the association of vancomycin with technique failure does not prove causality. These findings shed light on new factors predicting outcome when peritonitis is diagnosed.
Keywords: Peritoneal dialysis, peritonitis, BRAZPD, clinical outcomes
Although hemodialysis (HD) and peritoneal dialysis (PD) present similar outcomes in terms of patient survival, PD therapy is associated with significantly lower technique survival. This holds true despite the reduction in peritonitis rates observed over the past decades (1). Not surprisingly, PD-related peritonitis has been extensively studied, and risk factors for peritonitis are well established, including in large cohort studies based in heterogeneous geographic areas in developing countries (2). Of concern, even when properly treated, approximately 20% of all episodes are refractory to treatment (3,4). Furthermore, prolonged efforts to treat refractory peritonitis can lead to extended hospitalization time, ultrafiltration failure due to peritoneal membrane damage, increased risk of fungal peritonitis, and mortality in a small but not negligible proportion of cases (4,5). However, other than microbiological issues that were studied in the past, little has been published about factors associated with refractory peritonitis and which patients are at higher risk to die after a peritonitis episode (6). Moreover, among those successfully treated for a peritonitis episode, the factors associated with technique failure remain to be investigated. Thus, the aim of this study is to identify factors predicting non-resolution and peritonitis-related mortality, as well as the risk factors for long-term technique failure after the first peritonitis episode.
Methods
This study was performed in accordance with the Declaration of Helsinki and all participants signed written informed consent before the enrollment.
Patient Population
The study included all incident patients 18 years or older, who remained at least 90 days on PD and presented their first peritonitis episode (n = 474) during the follow-up, from 114 PD centers reporting monthly to the BRAZPD, a multicenter Brazilian cohort study, from December 2004 through October 2007 (7). Data were obtained using software specifically designed to collect data in each participating clinic (PDNet), which were transferred to a central database.
During the follow-up period, patients were evaluated monthly by nephrologists and nurses at the PD clinic. Data collection included age (years), gender, race, cause of end-stage renal disease (ESRD), previous hemodialysis (HD), PD modality at the time of peritonitis episode (CAPD or APD), body mass index (kg/m2), BP (mmHg), serum albumin (g/dl), hemoglobin levels (g/dl), PD indication (medical, patient’s option, or only option), previous nephrology referral, family income (minimum wages [MW] per month: no income, 0 to 2, 3 to 5, 6 to 10, 11 - 20, > 20), education level (illiteracy, elementary, secondary, and higher), distance from dialysis center (< 25, 25 to 50, > 50 km), region where patients live and its Human Development Index (HDI), number of treated patients per center, microbiological characteristics of peritonitis, and total follow-up period (months). The HDI is an annual index published by the United Nations Development Program to measure national development. The presence of comorbid conditions (collagenosis, malignancy, cardiopathy, left ventricular hypertrophy, and diabetes) was registered as present or absent.
Definitions and Clinical Management
The definition of peritonitis followed the recommendations of the International Society for Peritoneal Dialysis (ISPD) guidelines (4). Non-resolution was defined as refractoriness to treatment that leads the patient to be transferred to HD or death as a consequence of the first peritonitis episode. Death related to peritonitis episode was defined as death of a patient with active peritonitis, or admitted with peritonitis, or within 2 weeks of a peritonitis episode (8,9). Technique failure was defined as the patients’ transfer to HD for any reason. Death, loss of follow-up, renal transplantation and recovery of renal function were considered censored data. Empirical antibiotic prescription was based on the patient’s clinical conditions according to each center’s protocol and the patients were hospitalized whenever necessary.
Statistical Analysis
Outcomes evaluated were non-resolution, death due to a peritonitis episode and long-term technique survival after a peritonitis episode. Clinical, demographic, dialysis-related, geographic, and socioeconomic variables were included in all analyses. For all outcomes assessed, multicollinearity between variables was double checked through analysis of the variance inflation factor (VIF) scores and a correlation of estimates. A subgroup analysis of APD patients was also performed including an additional variable as “switch to CAPD during the treatment (Yes or No)”.
Logistic regression was used to assess predictors of non-resolution and death related to the first peritonitis episode. All assumptions to logistic regression were checked and met. Discrete variables were converted into a set of dichotomous variables by dummy variable coding (10). The method utilized was stepwise backward deletion, in which, after being evaluated one at a time, those variables that did not contribute significantly were deleted. In addition, all variables with a p level lower than 0.20 in the univariate analysis were included in the multivariate model. The multivariable regression analysis is suitable here since we excluded the possibility of any center-related effects running a hierarchical model (i.e., random effects for treating units).
For long-term technique failure analysis, the Kaplan-Meier survival curve was calculated for all variables and if a p value < 0.20 was obtained in the long rank test the corresponding variable was included in the Cox proportional hazard regression model. Patients who died or were transferred to HD at the time of the peritonitis episode were excluded from this analysis as well as those with fungal peritonitis. Statistical significance was defined as p < 0.05. The statistical software packages utilized were SPSS 11.01.1 and MLwin version 2.26.
Results
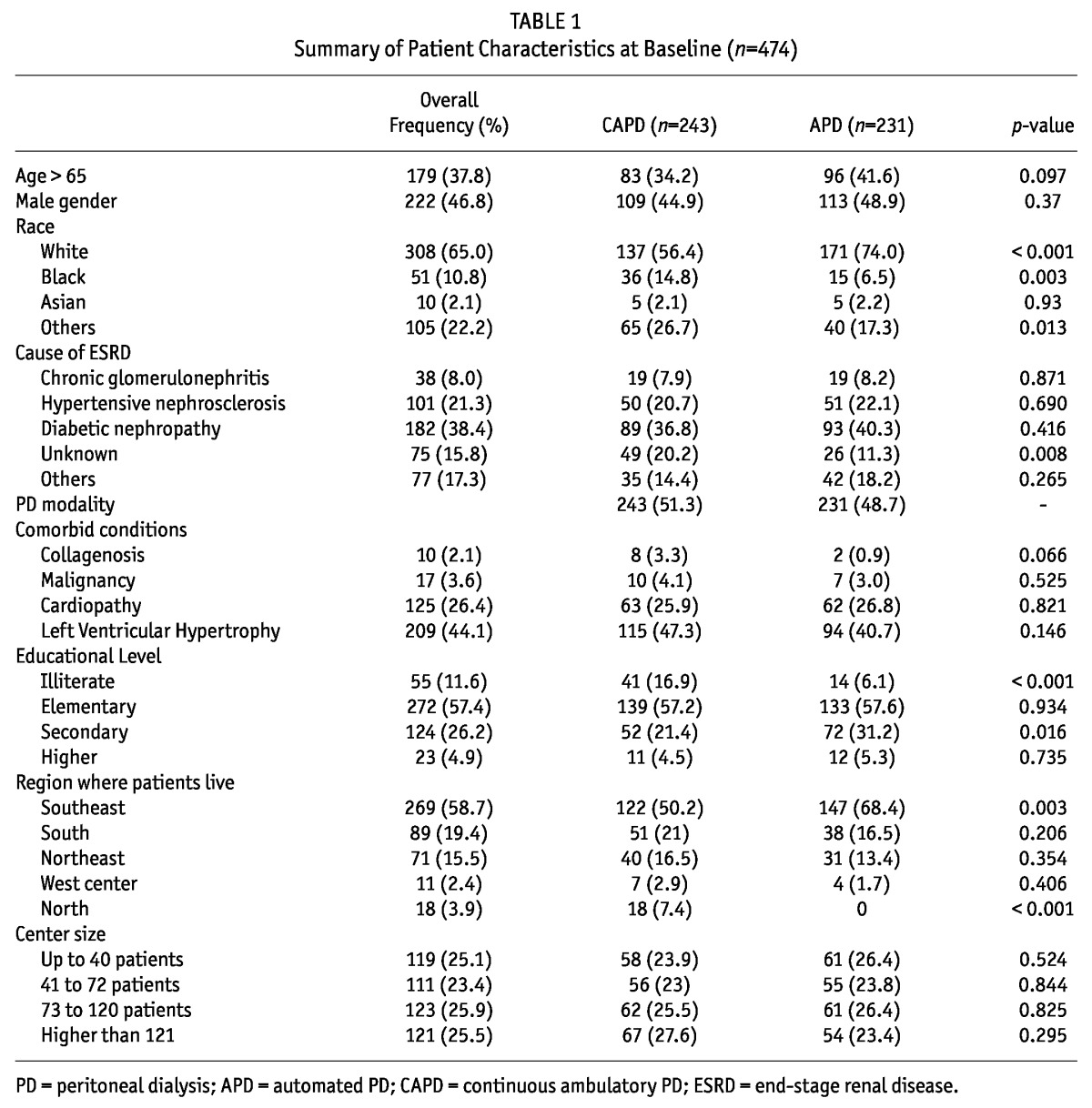
Between December 2004 and October 2007, 474 patients from a cohort of 2,032 incident adult PD patients presented a first peritonitis episode. Patient characteristics at baseline, including the characteristics of patients on APD and CAPD, are described in Table 1. The description of the whole cohort characteristics is described elsewhere (7).
TABLE 1.
Summary of Patient Characteristics at Baseline (n=474)
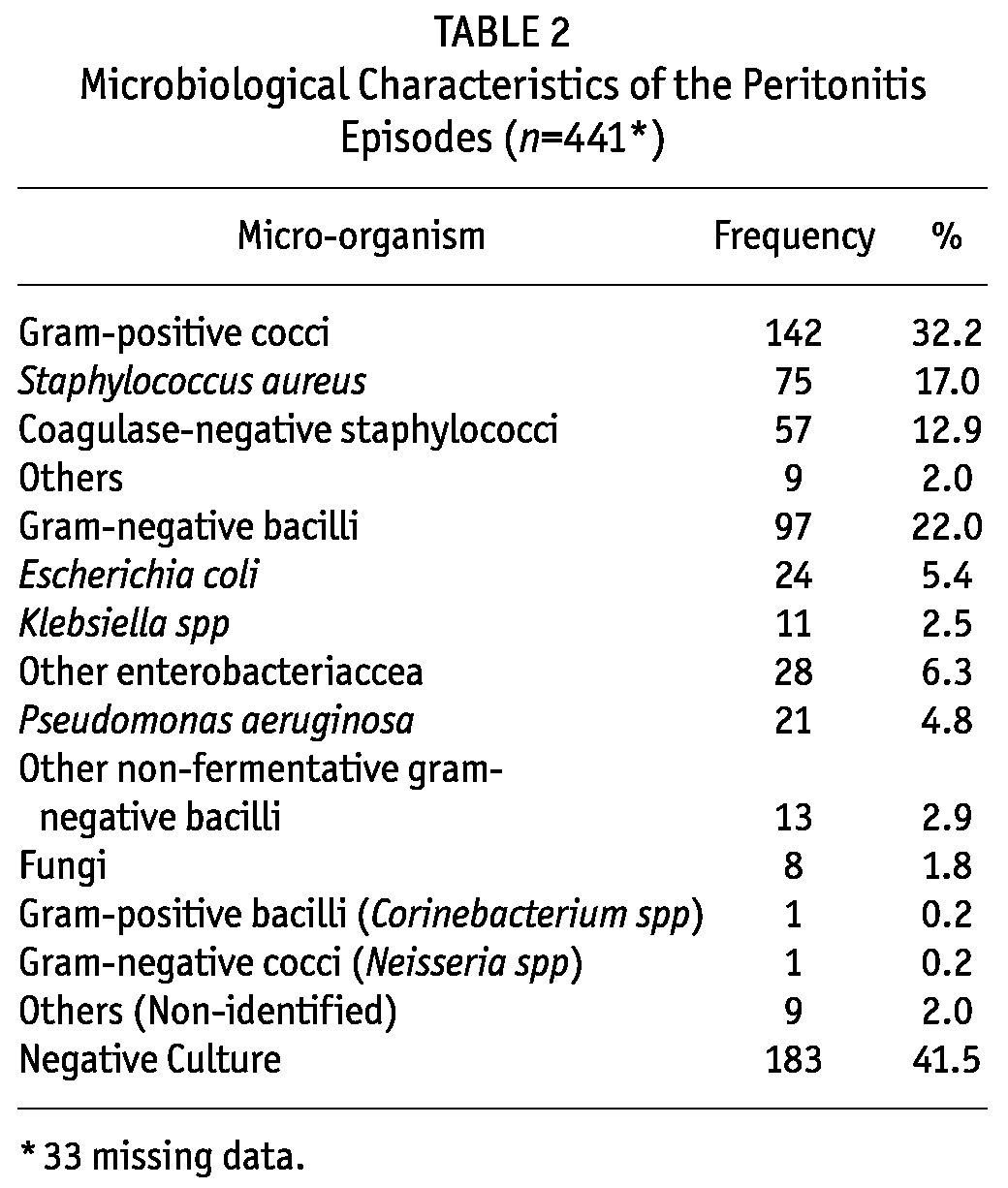
Negative culture was observed in 183 (41.5%) episodes and 33 episodes did not present the description of the culture results. The culture negative episodes were homogeneously distributed between all centers. In the 258 cases of peritonitis with a causative organism identified, 142 (32%) were due to gram-positive bacteria, 97 (22%) to gram-negatives, and eight (1.8%) to fungi. Detailed microbiological information is shown in Table 2.
TABLE 2.
Microbiological Characteristics of the Peritonitis Episodes (n=441*)
Regarding treatment, the main antibiotic used to cover gram-positive bacteria was a first generation cephalosporin in 295 episodes, followed by vancomycin in 154. For gram-negative bacteria, gentamicin was the most prescribed antibiotic, in 201 episodes, followed by a third generation cephalosporin in 122 and quinolones in 90 patients.
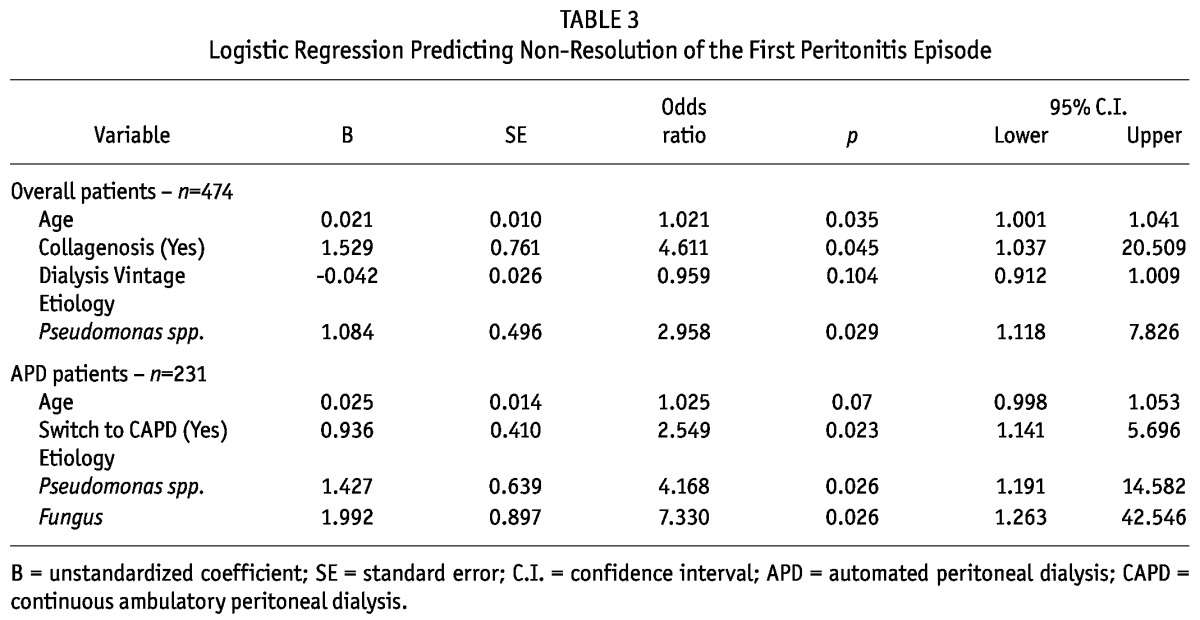
Predictors of Non-Resolution of the First Peritonitis Episode
The treatment of 67 patients failed, yielding a non-resolution rate of 14.1%. Age (p = 0.04), dialysis vintage (p = 0.06), collagenosis as a comorbid condition (p = 0.16), gender (p = 0.16), Pseudomonas etiology (p = 0.01) and fungal peritonitis (p = 0.10) presented a p value lower than 0.2 and were included in the multivariate analysis. In the multiple regression model, age, presence of collagenosis, and Pseudomonas spp etiology remained independently associated with non-resolution. No specific antibiotic treatment was found to have influenced the resolution rate. In the subgroup of APD patients, those who transiently switch to CAPD during the infectious treatment presented a higher non-resolution rate; indeed, in this subgroup, Pseudomonas and fungal etiologies were associated with non-resolution (Table 3). There was no independent predictor for non-resolution in the CAPD sub-group of patients.
TABLE 3.
Logistic Regression Predicting Non-Resolution of the First Peritonitis Episode
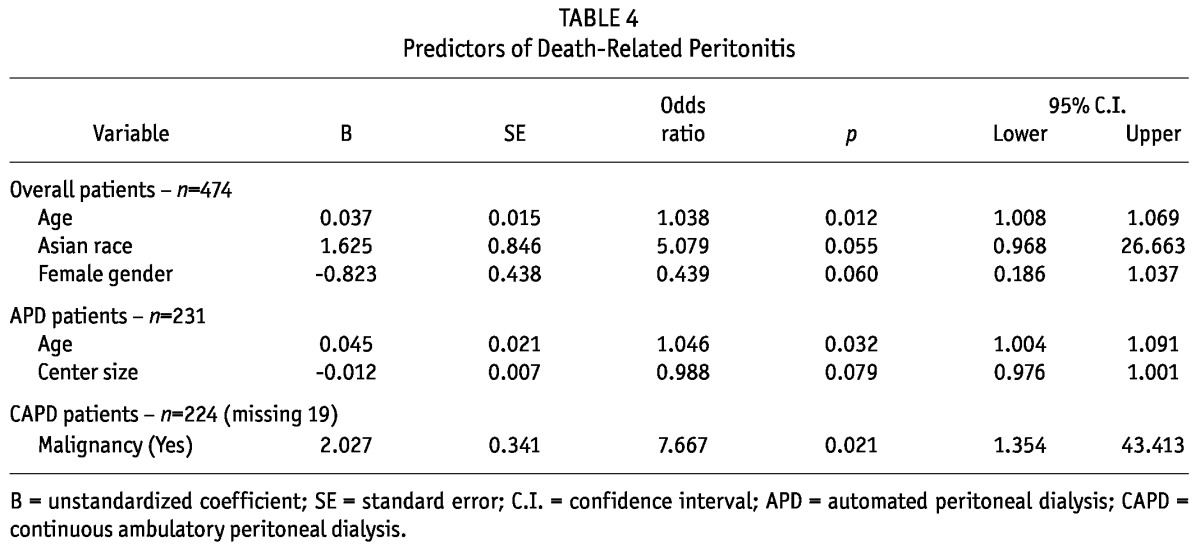
Predictors of Death Related to Peritonitis
Mortality related to the first peritonitis episode was 5.7% (n = 27). Variables included in the multivariate model were gender (p = 0.06), center size (p = 0.09), educational level (illiterate) (p = 0.08), cardiopathy (p = 0.08), age (p = 0.01), malignancy (p = 0.51) and non-White race (p = 0.05). As shown in Table 4, age was the only independent risk factor for death related to the first peritonitis episode. In the subgroup of APD patients, age remained the only predictor of death, while in CAPD only malignancy was independently associated with death risk (Table 4).
TABLE 4.
Predictors of Death-Related Peritonitis
Long-Term Technique Failure Following the First Peritonitis
All the patients whose first peritonitis episode evolved into resolution were included in this analysis. Of a total of 399 patients, 81 were transferred to HD. Peritonitis was the main cause of technique failure in 46.9% of the cases while UF failure was responsible for 29.6%. Technique survival after the first year of the initial infectious episode was 73.2%, dropping to 49.9% at 2 years.
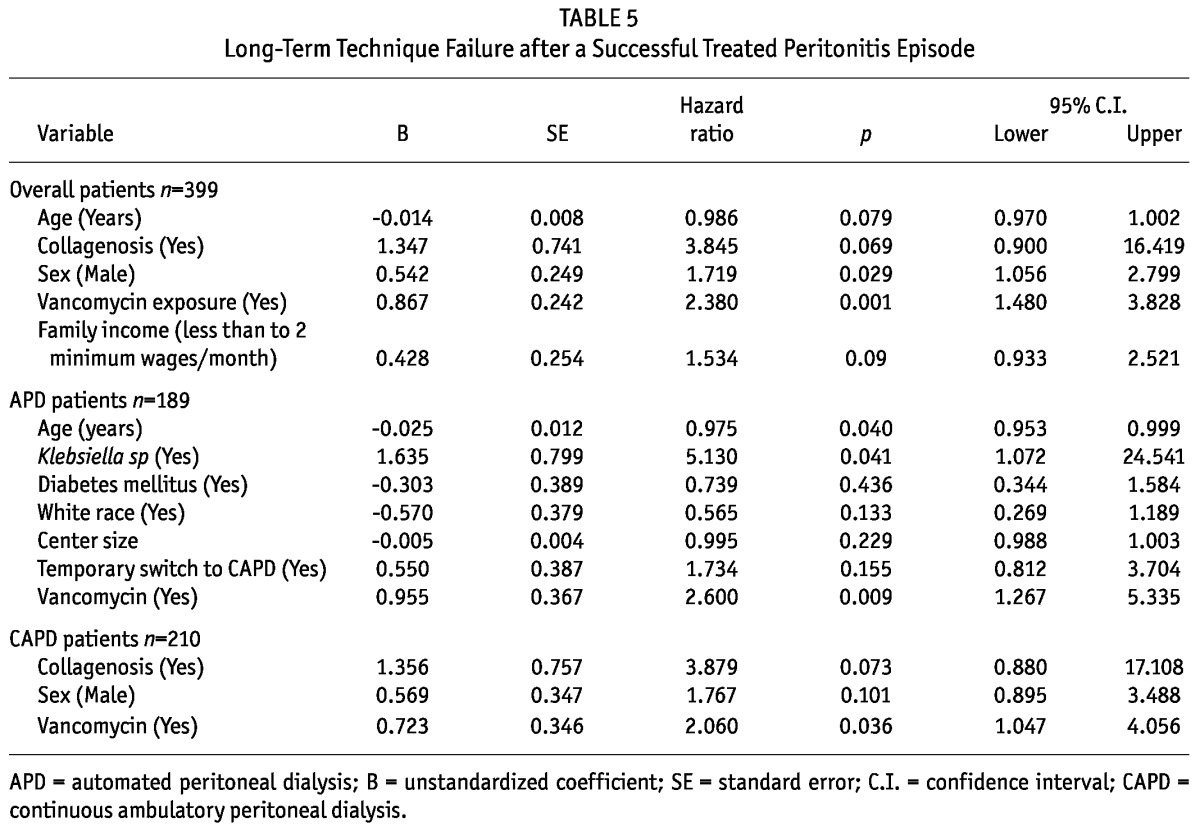
By univariate analysis no associations were found between bacterial etiologies, subsequent peritonitis episodes and technique failure, while there were associations between presence of collagenosis (p = 0.19), gender (p = 0.11), exposure to vancomycin (p < 0.01), age (p = 0.04), and family income (p = 0.08) and the endpoint; these variables were included in the Cox model. The multivariate Cox analysis found that the independent predictors of technique failure were exposure to vancomycin and male gender (Table 5). Among APD patients, the variables included in the Cox model were age (p < 0.01), Klebsiella peritonitis (p = 0.08), center size (p = 0.04), transient switch do CAPD (p < 0.01), exposure to vancomycin (p < 0.01), and white race (p = 0.09). In this subgroup, vancomycin exposure, Klebsiella peritonitis, and lower age were independently associated with the endpoint (Table 5). In contrast, the CAPD subgroup model included collagenosis (p = 0.09), female gender (p = 0.10) and vancomycin (p = 0.08); exposure to vancomycin was the only independent risk factor for technique failure.
TABLE 5.
Long-Term Technique Failure after a Successful Treated Peritonitis Episode
Discussion
Although risk factors for peritonitis have been extensively studied in the literature, only a small number of them reported clinical and demographic predictors of outcomes following a peritonitis episode. In fact, to the best of our knowledge, there is only one large prospective cohort study describing factors such associations (11). The main results of the present study were that factors other than the etiology of peritonitis, namely older age, presence of collagenosis, and clinical practice pattern (use of vancomycin and transfer of APD patients to CAPD during peritonitis) were associated with clinical outcome.
Peritonitis non-resolution rates have been described to be approximately 20% or higher in different series with a mortality rate of approximately 10% (1,12-15). In the current study, the non-resolution rate was lower (14.1%) than previously described. As expected, Pseudomonas spp etiology was an independent predictor of non-resolution, but surprisingly S. aureus was not. This finding could be possibly explained by a low methicillin resistance rate among S. aureus. Unfortunately data on bacterial resistance were not available in the BRAZPD database. In addition, we found that culture-negative peritonitis was not associated with the endpoint, in disagreement with the majority of previous reports (16-19), including the largest case series, published by Fahim et al. (19), which have reported higher resolution rate. Culture-negative PD peritonitis episodes in general correspond to infectious causes that fail to reach the threshold of microbiological detection, as coagulase-negative staphylococci and viruses associated with benign clinical course (16). A large prevalence of culture-negative episodes was described in the present study that suggest suboptimal culture techniques in the country. These episodes could be caused by several etiologies that potentially influence the outcome.
A few patient conditions, such as older age and collagenosis, were identified as predictors of non-resolution. Nevertheless, the increased mortality in the elderly was the reason for age as a significant predictor of non-resolution. Although collagenosis was previously reported as a risk factor for peritonitis, technique failure, and mortality (20,21), this is the first association between this comorbidity and non-resolution. This observation is to be expected, since those are chronic inflammatory conditions, which are commonly treated by immunosuppression that leads to immune dysfunction. In addition, previous studies showed an important association between chronic inflammation, assessed by baseline levels of C-reactive protein, and peritonitis refractoriness (11). Information about immunosuppressive treatment in this group of patients would be interesting, but it was not available in the database.
In the present cohort, PD modality was not a predictor of any outcomes, which is in agreement with previous reports (1,22). However, transference to CAPD is a common practice in our country due to concerns of adequate antibiotic dosing during APD and the subgroup of APD patients who were transiently transferred to CAPD for peritonitis treatment presented a higher non-resolution rate. This novel finding was not associated with center size or any other covariable. The most plausible possibilities to explain this finding are: (a) APD patients could face technique difficulties in performing manual exchanges when they are subtly forced to transfer to CAPD (such issues could be a consequence of either patients that were never trained to perform manual exchanges — starting PD on APD — or if such training occurred a long time ago), or (b) volume overload due to UF failure in high-transporter patients transferred to CAPD. This is an important finding that could reduce permanent transference to HD and deserves further study. CAPD technique should be revised periodically or, if not possible, immediately before transferring to CAPD for peritonitis treatment.
Death is an uncommon occurrence in PD-related peritonitis and has been reported in less than 10% of all episodes. In the present study the peritonitis-related mortality rate was 5.7% and older age was the only risk factor for death. This is in agreement with previous studies, and the immune dysfunction related to aging is likely an important causative factor (1,15,23,24). Nevertheless, the severity of medical disease observed in these patients, as well as possible residual confounders, must also be taken into account when trying to explain the association of collagenosis and peritonitis-related mortality.
Contrary to previous studies, no etiological agents were associated with higher mortality rate. The lack of association between fungal peritonitis and mortality is probably related to the small number of cases caused by this agent, since this study only took into account the first episode of peritonitis. Interestingly, this relationship between fungal peritonitis and mortality has been observed mainly when associated with multiple previous peritonitis episodes. This observation may imply that, at least in part, the high mortality observed in fungal peritonitis may be related to previous clinical infectious events. Our study presents a high prevalence of negative cultures and similarly with previous reports that were highlighted in the ISPD guideline, the culture negative peritonitis did not influenced any of the outcomes.
We further evaluated, in successfully treated patients, whether or not conditions related to their first peritonitis episode would influence long-term technique survival. Two variables were independent risk factors for technique failure: male gender and prescription of vancomycin to treat the initial peritonitis episode (Figure 1). The influence between gender and outcomes in PD is not well established, for example previous reports from both a large retrospective Canadian cohort and a North American cohort of incident patients, associated higher PD technique survival with female gender (25,26). Herein several factors can possibly act as a confounder, from genetic characteristics to cultural and socioeconomic aspects.
Figure 1 —
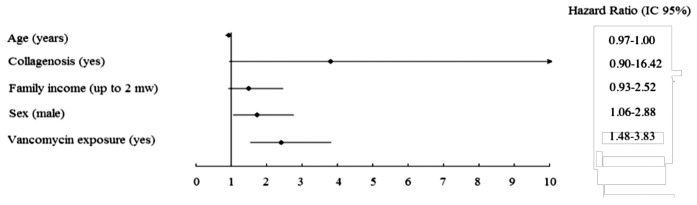
Independent risk factors for technique failure.
One of the most interesting findings in this study was that exposure to vancomycin predicted technique failure. It is known that vancomycin can potentially affect residual renal function (RRF). Indeed, Herget-Rosenthal et al. described in a cohort of 71 incident patients that vancomycin, as a part of a composite variable, was a risk factor for RRF declining (27). However, to the best of our knowledge, this is the first time that vancomycin is reported as an independent factor for technique failure in PD. Unfortunately, longitudinal information about RRF to further investigate the effect of vancomycin on this variable was not available. Alternatively, the lower technique survival rate associated with vancomycin use could be a consequence of its prescription in high-risk patients with more severe peritoneal infections, which could have a negative impact on peritoneal membrane preservation. In agreement with this possibility, Fahim et al. showed that vancomycin prescription was associated with a higher risk for permanent transfer to HD (28). Yet the characteristics between patients exposed and not exposed to vancomycin were similar, although criteria regarding antibiotic choice were not available in our database.
A sub-analysis of outcomes according to PD modality (APD vs. CAPD) confirmed that vancomycin was an important risk factor for technique failure specifically in APD patients. Moreover, particularly in APD patients, Klebsiella spp and lower age emerged as independent risk factors, while in CAPD, no new factor appeared. As Klebsiella spp are of enteric origin, we can speculate that a possible association between these germs and gastrointestinal diseases could eventually lead to worse outcomes. The reasons for these clustered findings in APD remain to be elucidated.
Regarding the protective effect of older age on technique failure, information in the literature is controversial (29-30). The greater risk of technique failure in elderly patients could be attributed to reasons such as an inability to perform PD because of cognitive or mechanical reasons; however, similar to the present results Lim et al. (25), in a large Australia and New Zealand cohort, reported that compared to younger patients, elderly patients presented a higher risk of peritonitis-related mortality, but a lower risk of technique failure. In agreement, Perl et al. (31), comparing three large Canadian incident cohorts of PD patients who initiated dialysis during 1995 - 2000, 2001 - 2005, and 2006 - 2009, reported that patients under 65 years old showed no reduction in technique failure over time, while those above 65 years of age had a lower risk of technique failure in 2001 - 2005 and 2006 - 2009 relative to 1995 - 2000. According to Lim et al. (25) it is possible that, to maintain their independence, elderly patients may prefer to persist with PD regardless of PD-related complications, while Perl et al. (31) suggested the role of the increasing use of home-assisted PD for older patients as a reason for the improvement of clinical outcome in these patients. These explanations are plausible to explain the present results; unfortunately, our database does not provide enough information to examine these questions.
This study has limitations. First, our database did not include data on bacterial antibiotic resistance, inflammatory markers, and dialysate cells count during peritonitis, which are conditions previously associated with infection resolution (1,32). Second, the prevalence of negative culture was higher than current recommendations. Third, the strong association of vancomycin and technique failure does not mean a cause-effect relationship but only an association that deserves additional study. And finally, there are no data on RRF, an important risk factor for technique failure. Nevertheless, this study has important strengths: it is a large multicenter cohort analysis of incident PD patients, and provides important clinical, demographic, and microbiological factors not analyzed until the present. Finally, this study uses a national based, large cohort in a country with very heterogeneous geographic and socio-economic variables.
In summary, the main contributions of this study were to shed light on new factors predicting outcome when a peritonitis episode is diagnosed. We confirmed that the treatment response for peritonitis caused by Pseudomonas spp is challenging, but has no impact on mortality. In contrast, S. aureus peritonitis did not add risk, and collagenosis as a cause of renal disease was for the first time described as a risk factor for peritonitis non-resolution. We also provide original associations between temporary transferring of APD patients to CAPD for antibiotic-therapy treatment and poor outcomes. In addition, aging was the only independent factor associated with mortality. Finally, a strong association between vancomycin and poor technique survival for those successfully treated was described although this does not prove causality. This novel information can serve as useful tools to guide specific and more intensive strategies in the treatment of patients with those characteristics, as well as serve as an important reference for the design of future studies.
Disclosures
Thyago Proença de Moraes has received speakers’ honoraria and travel sponsorship from Baxter. Marcia Olandoski, Jacqueline Caramori, Luis Cuadrado Martin, and Pasqual Barretti declare no conflicts of interest. Jose Carolino Divino Filho was a full-time employee of Baxter Healthcare during data collection. Roberto Pecoits-Filho and Natalia Fernandes received consulting fees from Baxter Healthcare.
Acknowledgments
Baxter Healthcare provided financial support for this project.
References
- 1. Davenport A. Peritonitis remains the major clinical complication of peritoneal dialysis: the London, UK, peritonitis audit 2002-2003. Perit Dial Int 2009; 29:297–302 [PubMed] [Google Scholar]
- 2. Martin LC, Caramori JC, Fernandes N, Divino-Filho JC, Pecoits-Filho R, Barretti P. Geographic and educational factors and risk of the first peritonitis episode in Brazilian Peritoneal Dialysis study (BRAZPD) patients. Clin J Am Soc Nephrol; 6:1944–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Krishnan M, Thodis E, Ikonomopoulos D, Vidgen E, Chu M, Bargman JM, et al. Predictors of outcome following bacterial peritonitis in peritoneal dialysis. Perit Dial Int 2002; 22:573–81 [PubMed] [Google Scholar]
- 4. Blake PG. Peritonitis and catheter guidelines—a 2010 update. Perit Dial Int; 30:391–2 [DOI] [PubMed] [Google Scholar]
- 5. Blake PG, Bargman JM, Brimble KS, Davison SN, Hirsch D, McCormick BB, et al. Clinical practice guidelines and recommendations on peritoneal dialysis adequacy 2011. Perit Dial Int; 31:218–39 [DOI] [PubMed] [Google Scholar]
- 6. van Esch S, Krediet RT, Struijk DG. Prognostic factors for peritonitis outcome. Contrib Nephrol 2012; 178: 264–70 [DOI] [PubMed] [Google Scholar]
- 7. Fernandes N, Bastos MG, Cassi HV, Machado NL, Ribeiro JA, Martins G, et al. The Brazilian Peritoneal Dialysis Multicenter Study (BRAZPD): characterization of the cohort. Kidney Int Suppl 2008; 108:S145–51 [DOI] [PubMed] [Google Scholar]
- 8. Piraino B, Bailie GR, Bernardini J, Boeschoten E, Gupta A, Holmes C, et al. ISPD Ad Hoc Advisory Committee. Peritoneal dialysis-related infections recommendations: 2005 update. Perit Dial Int 2005; 25:107–31 [PubMed] [Google Scholar]
- 9. Li PK, Szeto CC, Piraino B, Bernardini J, Figueiredo AE, Gupta A, et al. Peritoneal dialysis-related infections recommendations: 2010 update. Perit Dial Int; 30:393–23 [DOI] [PubMed] [Google Scholar]
- 10. Ho R. Multiple Regression. In: Handbook of Univariate and Multivariate Data Analysis and Interpretation with SPSS. Boca Raton: Chapman & Hall/CRC; 2006. [Google Scholar]
- 11. Zalunardo NY, Rose CL, Ma IW, Altmann P. Higher serum C-reactive protein predicts short and long-term outcomes in peritoneal dialysis-associated peritonitis. Kidney Int 2007; 71:687–92 [DOI] [PubMed] [Google Scholar]
- 12. Barretti P, Bastos KA, Dominguez J, Caramori JC. Peritonitis in Latin America. Perit Dial Int 2007; 27:332–9 [PubMed] [Google Scholar]
- 13. Brown MC, Simpson K, Kerssens JJ, Mactier RA. Peritoneal dialysis-associated peritonitis rates and outcomes in a national cohort are not improving in the post-millennium (2000-2007). Perit Dial Int 2011; 31:639–50 [DOI] [PubMed] [Google Scholar]
- 14. Ghali JR, Bannister KM, Brown FG, Rosman JB, Wiggins KJ, Johnson DW, et al. Microbiology and outcomes of peritonitis in Australian peritoneal dialysis patients. Perit Dial Int 2011; 31:651–62 [DOI] [PubMed] [Google Scholar]
- 15. Oliveira LG, Luengo J, Caramori JC, Montelli AC, Cunha MD, Barretti P. Peritonitis in recent years: clinical findings and predictors of treatment response of 170 episodes at a single Brazilian center. Int Urol Nephrol 2012. February 3 Epub ahead of print [DOI] [PubMed] [Google Scholar]
- 16. Bunke M, Brier ME, Golper TA. Culture-negative CAPD peritonitis: the Network 9 Study. Adv Perit Dial 1994; 10:174–8 [PubMed] [Google Scholar]
- 17. Szeto CC, Wong TY, Chow KM, Leung CB, Li PK. The clinical course of culture-negative peritonitis complicating peritoneal dialysis. Am J Kidney Dis 2003; 42:567–74 [DOI] [PubMed] [Google Scholar]
- 18. Chen KH, Chang CT, Weng SM, Yu CC, Fang JT, Huang JY, et al. Culture-negative peritonitis: a fifteen-year review. Ren Fail 2007; 29:177–81 [DOI] [PubMed] [Google Scholar]
- 19. Fahim M, Hawley CM, McDonald SP, Brown FG, Rosman JB, Wiggins KJ, et al. Culture-negative peritonitis in peritoneal dialysis patients in Australia: predictors, treatment, and outcomes in 435 cases. Am J Kidney Dis 2010; 55:690–7 [DOI] [PubMed] [Google Scholar]
- 20. Huang JW, Hung KY, Yen CJ, Wu KD, Tsai TJ. Systemic lupus erythematosus and peritoneal dialysis: outcomes and infectious complications. Perit Dial Int 2001; 21:143–7 [PubMed] [Google Scholar]
- 21. Siu YP, Leung KT, Tong MK, Kwan TH, Mok CC. Clinical outcomes of systemic lupus erythematosus patients undergoing continuous ambulatory peritoneal dialysis. Nephrol Dial Transplant 2005; 20:2797–802 [DOI] [PubMed] [Google Scholar]
- 22. Ruger W, van Ittersum FJ, Comazzetto LF, Hoeks SE, ter Wee PM. Similar peritonitis outcome in CAPD and APD patients with dialysis modality continuation during peritonitis. Perit Dial Int 2011; 31(1):39–47 [DOI] [PubMed] [Google Scholar]
- 23. Ongradi J, Stercz B, Kovesdi V, Vertes L. Immunosenescence and vaccination of the elderly, I. Age-related immune impairment. Acta Microbiol Immunol Hung 2009; 56:199–210 [DOI] [PubMed] [Google Scholar]
- 24. Donowitz GR, Cox HL. Bacterial community-acquired pneumonia in older patients. Clin Geriatr Med 2007; 23:515–34 [DOI] [PubMed] [Google Scholar]
- 25. Lim WH, Dogra GK, McDonald SP, Brown FG, Johnson DW. Compared with younger peritoneal dialysis patients, elderly patients have similar peritonitis-free survival and lower risk of technique failure, but higher risk of peritonitis-related mortality. Perit Dial Int 2011; 31:663–71 [DOI] [PubMed] [Google Scholar]
- 26. Shen JI, Mitani AA, Saxena AB, Goldstein BA, Winkelmayer WC. Determinants of peritoneal dialysis technique failure in incident US patients. Perit Dial Int 2012. October 2 Epub ahead of print [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Herget-Rosenthal S, von Ostrowski M, Kribben A. Definition and risk factors of rapidly declining residual renal function in peritoneal dialysis: an observational study. Kidney Blood Press Res 2012; 35(4):233–41 [DOI] [PubMed] [Google Scholar]
- 28. Fahim M, Hawley CM, McDonald SP, Brown FG, Rosman JB, Wiggins KJ, et al. Coagulase-negative staphylococcal peritonitis in Australian peritoneal dialysis patients: predictors, treatment and outcomes in 936 cases. Nephrol Dial Transplant 2010; 25(10):3386–92 [DOI] [PubMed] [Google Scholar]
- 29. Yang X, Fang W, Kothari J, Khandelwal M, Naimark D, Jassal SV, et al. Clinical outcomes of elderly patients undergoing chronic peritoneal dialysis: experiences from one center and a review of the literature. Int Urol Nephrol 2007; 39:1295–302 [DOI] [PubMed] [Google Scholar]
- 30. Kolesnyk I, Dekker FW, Boeschoten EW, Krediet RT. Time-dependent reasons for peritoneal dialysis technique failure and mortality. Perit Dial Int 2010; 30:170–7 [DOI] [PubMed] [Google Scholar]
- 31. Perl J, Wald R, Bargman JM, Na Y, Jassal SV, Jain AK, et al. Changes in patient and technique survival over time among incident peritoneal dialysis patients in Canada. Clin J Am Soc Nephrol 2012; 7:1145–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Yang CY, Chen TW, Lin YP, Lin CC, Ng YY, Yang WC, et al. Determinants of catheter loss following continuous ambulatory peritoneal dialysis peritonitis. Perit Dial Int 2008; 28(4):361–70 [PubMed] [Google Scholar]


