Abstract
Background
Laparoendoscopic single site (LESS) surgery may have perceived benefits of reduced visible scarring compared to conventional laparoscopic (LAP) totally extraperitoneal (TEP) hernia repairs. We reviewed the literature to compare LESS TEP inguinal hernia repairs with LAP TEP repairs.
Methods
We searched electronic databases for research published between January 2008 and January 2012.
Results
A total of 13 studies reported on 325 patients. The duration of surgery was 40–98 minutes for unilateral hernia and 41–121 minutes for bilateral repairs. Three studies involving 287 patients compared LESS TEP (n = 128) with LAP TEP (n = 159). There were no significant differences in operative duration for unilateral hernias (p = 0.63) or bilateral repairs (p = 0.29), and there were no significant differences in hospital stay (p > 0.99), intraoperative complications (p = 0.82) or early recurrence rates (p = 0.82). There was a trend toward earlier return to activity in the LESS TEP group (p = 0.07).
Conclusion
Laparoendoscopic single site surgery TEP hernia repair is a relatively new technique and appears to be safe and effective. Advantages, such as less visible scarring, mean patients may opt for LESS TEP over LAP TEP. Further studies with clear definitions of outcome measures and robust follow-up to assess patient satisfaction, return to normal daily activities and recurrence are needed to strengthen the evidence.
Abstract
Contexte
La chirurgie laparoendoscopique à orifice unique (LESS) a comme avantage perçu une réduction des cicatrices apparentes comparativement aux réparations laparoscopiques (LAP) classiques totalement extrapéritonéales (TEP) des hernies. Nous avons passé en revue la littérature afin de comparer les réparations des hernies inguinales par chirurgie LESS TEP et par LAP TEP.
Méthodes
Nous avons interrogé les bases de données électroniques pour y recenser la recherche publiée entre janvier 2008 et janvier 2012.
Résultats
En tout, 13 études ont porté sur 325 patients. La durée de la chirurgie a été de 40 à 98 minutes pour les réparations de hernies unilatérales et de 41 à 121 minutes pour les réparations de hernies bilatérales. Trois études regroupant 287 patients ont comparé la technique LESS TEP (n = 128) à la technique LAP TEP (n = 159). On n’a observé aucune différence significative quant à la durée de la chirurgie des réparations de hernies unilatérales (p = 0,63) ou bilatérales (p = 0,29) et aucune différence significative de durée des séjours hospitaliers (p > 0,99), de complications peropératoires (p = 0,82) ou de taux de récurrences précoces (p = 0,82). On a noté une tendance à un retour plus rapide aux activités dans le groupe soumis à la technique LESS TEP (p = 0,07).
Conclusion
La réparation de hernie par chirurgie TEP laparoendoscopique à un seul orifice est une technique relativement nouvelle et semble sécuritaire et efficace. Ses avantages, par exemple des cicatrices moins apparentes, pourraient pousser les patients à opter pour la technique LESS TEP plutôt que LAP TEP. Il faudra procéder à d’autres études fondées sur des définitions paramétriques claires et comportant un suivi robuste pour évaluer la satisfaction des patients, la reprise des activités quotidiennes normales et les taux de récurrences afin de consolider les preuves.
Inguinal hernias are a common problem and concern in the population with more than 80 000 new diagnoses1 leading to more than 70 000 repairs between 2010 and 2011 in the UK;2 20 million repairs are performed worldwide every year.3,4 Open inguinal hernia repairs are well-established procedures5 with good postoperative outcomes. Since the early 1990s6,7 laparoscopic techniques have become more popular. Some studies report an increase from 6% in 1992 to more than 40% in 2008 of hernias being repaired laparoscopically;8 this rapid rise in use may be because of less pain, faster recovery and better long-term outcomes.9–11 Furthermore, the minimally invasive procedures (typically the transperitoneal approach, but also the extraperitoneal approach if the midline raphe is crossed) offer the ability to examine the contralateral side,12 which may reveal an incipient or obvious hernia in up to 20% of patients.13,14 The proportion of laparosopic repairs has increased markedly over the last 20 years.15 The 2 recognized types of laparoscopic approaches are totally extraperitoneal preperitoneal (TEPP) or transabdominal preperitoneal (TAPP). Although both techniques are safe16 and offer advantages, totally extraperitoneal (TEP) repairs may be associated with a lower incidence of port site hernias, bowel-related complications, less pain and greater patient satisfaction; conversely, TEP may be associated with an increased likelihood of conversion.17–19
Greater patient education and demand for better cosmesis after surgical procedures have led to increased interest in laparoendoscopic single site surgery (LESS). Initially there was reluctance to adopt the technique owing to lack of technical facilitation; however, new or innovative port types20 and newer instruments have led to its application in a variety of surgical specialities.21 Laparoendoscopic single site TEP may be performed using conventional instruments, although articulating or curved instruments are in use.22 Although patients have good outcomes after conventional laparoscopic techniques, some authors suggest that there is a preference for LESS,23 which may be because of less postoperative pain24,25 or possible better cosmesis. Some have argued there is no advantage to single port surgery.26 We hypothesized that LESS TEP may be superior to conventional laparoscopic TEP (LAP TEP) because of fewer incisions, which may lead to less pain, and because the single incision in the umbilicus may result in a hidden scar with a better cosmetic appearance.
We reviewed the literature examining the role of LESS TEP for inguinal hernias. We aimed to compare LESS TEP with LAP TEP. Our main summative outcome measures were duration of surgery, hospital stay, cosmesis and return to activity.
Methods
Searching and selection
We identified all studies examining the role of LESS TEP for hernia repairs or comparing LESS TEP with LAP TEP that were published between January 2008 and January 2012. We searched the Medline, Embase and CINAHL databases available through the National Health Service National Library of Health website, the Cochrane library and PubMed. A range of key words are available to describe LESS techniques, and we used these terms to search for relevant material.27 The main key words “single port,” “single site surgery,” “laparoendoscopic single site,” “single port access,” “single incision,” “multiport” and “totally extraperitoneal hernia repair” were used in combination with the medical subject headings “hernia” and “inguinal hernia.” Articles, reviews and meta-analyses that we considered irrelevant based on the titles and abstracts were excluded. Relevant articles referenced in these publications were obtained, and we searched the references of identified studies to identify any further studies. No language restriction was applied.
Quality assessment
Two authors (M.R.S.S. and M.K.) independently assessed the methodological quality of the trials included for meta-analysis using standardized reference tools.28–31
Data extraction
Articles were included according to our review criteria (all noncomparative studies reporting on LESS TEP, all studies comparing LESS TEP with LAP TEP for groin hernias, all comparative or randomized studies, all elective cases, trials involving adults of any sex) and were reviewed by 2 researchers (M.R.S.S. and M.K.). This was performed independently, and if any conflict arose resolution was through discussion with the authors prior to analysis. Only papers examining the role of LESS TEP for hernias in adults and studies comparing LESS TEP with LAP TEP were included.
Our main outcome measures were duration of surgery for unilateral and bilateral hernias, hospital stay, complications, pain and concerns raised at follow up.
Statistical analysis
Statistical analyses were performed using Review Manager 5.0.23 (RevMan; Cochrane Collaboration).32 A value of p < 0.05 was chosen as the significance level for outcome measures. For continuous data (duration of surgery, hospital stay, return to activity), the inverse variance method was used for the combination of standardized mean differences (SMD). Binary data (intraoperative complications and recurrence) were summarized as risk ratios (RR) and combined using the Mantel–Haenszel method.33 Heterogeneity of the studies was assessed according to Q and I2 statistics. We used a random-effects method if the heterogeneity was significant; otherwise a fixed-effects method was used. In a sensitivity analysis, 1 was added to each cell frequency for trials in which no event occurred, according to the method recommended by Deeks and colleagues.34 When standard deviations were not reported, we estimated them either from ranges or p values. Forest plots were used for the graphical display.
Results
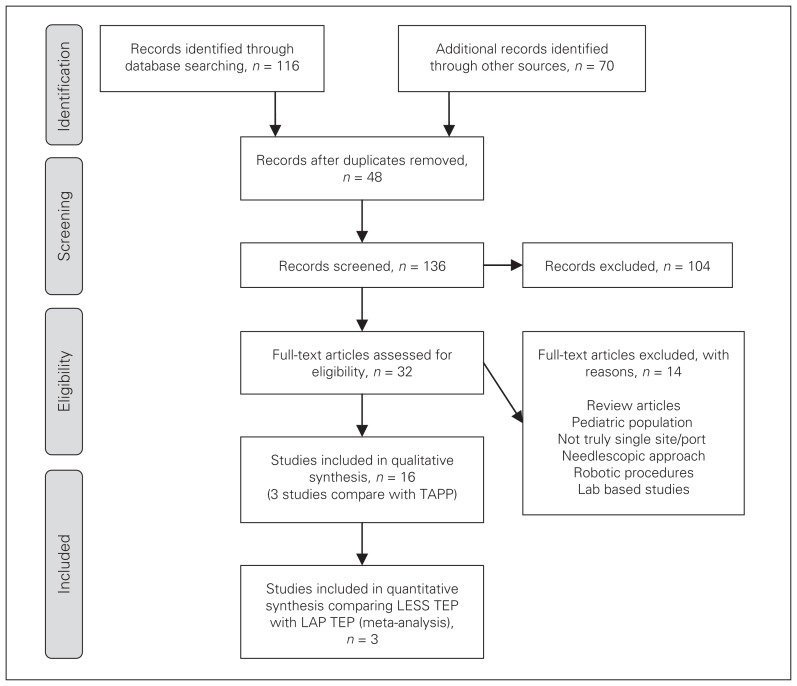
A total of 136 articles were screened for relevance. On further scrutiny, 16 articles15,19,22,35–47 were used in our literature review and 3 studies comparing LESS TEP with LAP TEP were found to have useful data for the summative outcome. One study commented on a previous report.37 Three studies22,40,45 compared LESS TEP with LAP TEP and were combined to produce a summative outcome. A flow chart of the literature search according to PRISMA guidelines48 is shown in Figure 1. Characteristics of each article are given in Tables 1 and 2.
Fig. 1.
Study selection. LAP = laparoscopic; LESS = laparoendoscopic single site surgery; TAPP = transabdominal preperitoneal; TEP = totally extraperitoneal.
Table 1.
Characteristics of studies included in our review and meta-analysis
| Characteristic | Cugura et al.35,37 | Jacob et al.38 | Bucher et al.36 | Surgit et al.41 | Agrawal et al.39 | Tran15 | Do et al.19 | Chung et al.42 | He et al.43 | Tai et al.44* | Shih et al.47 | Kim et al.46 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of patients | 1 | 3 | 4 | 23 | 16 | 68 | 10 | 100 | 3 | 7 | 30 | 60 |
| Age, yr (range) | 60 | NR | NR | 48.4 (23–67) | 65.5 (21–87) | 44 (18–83) | 43.7 (28–64) | 48 (18–82) | 64.6 (49–73) | 46.5 (21–80)* | NR | 58.5 (24–85) |
| Sex, male:female | 1:0 | 2:1 | — | 18:5 | 16:0 | 66:2 | 10:0 | 85:15 | 3:0 | — | — | 58:2 |
| Surgical technique | ||||||||||||
| Preperitoneal spacemaker | Balloon | Balloon | No balloon | Balloon | No balloon | Balloon | Balloon | Balloon | No balloon | Balloon | Balloon | No balloon |
| Ports | 3 ports via 1 incision | Single port device | Single port device | Single port device | Single port device | Single port device | Single port device | 3 ports via 1 incision | Single port device | 3 ports via 1 incision* | 3 ports via 1 incision | 3 ports via 1 incision |
| Camera | — | 45° | — | 30° | — | 30° | 30° | 30° | 30° | 30°* | 0° | 30° |
| Instruments | Standard straight | Standard straight | Standard straight | Articulating/standard | Standard straight | Curved | Curved/standard | Standard straight | Standard straight | Standard straight* | Curved, manually bent | Standard straight |
| Incision length, cm (range) | 2.5 | 2.5 | Larger than standard TEP | 2 | 3 (2.5–4.5) | 2.5 | 2.8 (2.3–3.2) | 2 | 2 | 1.5* | 2 | 2–2.5 |
| Fixed | Yes | Tacks | — | Tacks | Tacks | Tacks, glue | No fixation | Tacks | — | Tacks* | Tacks | Tacks |
| Duration of surgery; n, min (range) or min ± SD | 60 (52–64) | 64.2 (40–175) | ||||||||||
| Unilateral hernia | n = 1, 90 | NA | n = 3 | n = 19, 48.4 (32–62) | n = 13, 40 (25–75) | n = 36, 50 (35–90) | n = 10, 53.6 (45–65) | n = 83 | NA | 60 | n = 24, 98.3 ± 26.7 | n = 57; indirect: 65.2 (33–150), direct: 52.6 (32–80) |
| Bilateral hernias | NA | n = 3, 79.3 | n = 1 | n = 4, 96.7 (85–120) | n = 3, 70 (60–75) | n = 32, 80 (60–125) | NA | n = 17 | n = 3, 41 (26–65) | 78.5 (52–110) | n = 6, 121.4 ± 13.5 | n = 3, 77 (66–90) |
| Hospital stay, d (range) | 2 | 1, not recorded for 2 patients | — | 1.17 (1–2) | < 1 | 1 overnight patient | 2 | 1.54 (1–11) | 3 | 1.4 | 1.85 | 2.15 |
| Conversion | 0 | 0 | 1, bleeding; 1 extra port inserted | 1, large hernia and adhesions; 2 extra ports inserted | 0 | 1, unable to deploy port; 2 extra ports inserted | 0 | 2, peritoneal tear and adhesions; LESS TAPP performed | 0 | 0 | 0 | 1, omental incarceration, conversion to TAPP |
| Intraoperative complications, no. | 0 | 0 | 1, bleeding | 0 | 0 | — | 0 | 1, peritoneal tear | — | No major complications | 0 | 0 |
| Postoperative recovery | Uneventful | Uneventful | Uneventful | Uneventful | Uneventful | Uneventful | Uneventful | 2 had urinary retention | Uneventful | 1 had ileus and seroma | 2 had seroma | 2: 1 had seroma, 1 had urinary retention |
| Patient satisfaction (scale: 1–5) | — | — | — | — | — | None were dissatisfied | — | — | — | 87.5% satisfied* | — | — |
| Pain | — | — | — | — | n = 1, transient pain in testicle postoperatively | Most patients stopped analgesics within 48 h | No complaints of pain | 5 patients had groin ache | Minimal pain at discharge | — | — | — |
| Return to activity, d | — | — | — | — | — | 7–14 | — | 5.6 (1–30) | — | — | — | — |
| Other follow-up | No wound complications | Early complications: 1 epididymitis, 1 wound infection, 1 wound dehiscience, 11 seroma/haematoma | No wound complications | No wound complications reported | ||||||||
| 2 wk | — | No complications | — | — | — | — | — | — | ||||
| 1 mo | — | n = 1, no complications | — | — | — | — | — | — | ||||
| 2–3 mo | — | — | — | — | n = 2, minor wound complications | — | — | — | ||||
| 10–14 mo | — | — | — | — | — | — | — | — | ||||
| Recurrence, no. | — | None at 2 wk | None at 14 wk | None at 1 mo | None at 2–3 mo | None at 1–10 mo | None at 1 mo | 1 and 10 mo | None at 1 mo | — | None at 6 mo | — |
NR = not reported; SD = standard deviation; TAPP = transabdominal preperitoneal; TEP = totally extraperitoneal.
Results combined with TAPP hernia repairs.
Table 2.
Characteristics of studies comparing LESS TEP with LAP TEP
| Characteristic | Sherwinter et al.40 | Tai et al.45 | Cugura et al.22 | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| LAP TEP | LESS TEP | LAP TEP | LESS TEP | LAP TEP | LESS TEP | |
| No. of patients | 52 | 52 | 22 | 22 | 85 | 54 |
|
| ||||||
| Age, yr (range) or yr ± SD | 33.7 ± 11.3 | 37.5 ± 11.9 | 58.5 (17–79) | 55 (20–84) | 56.4 | 46.9 |
|
| ||||||
| Surgical technique | Preperitoneal space formed with balloon 1 × 11 mm, 2 × 5 mm ports (through single incision for LESS TEP), mesh fixed | Preperitoneal space formed with balloon 1 × 10 mm, 2 × 5 mm ports (through single incision via glove for LESS TEP), 30° camera and straight or curved instruments, mesh fixed | Preperitoneal space formed with balloon 1 × 10 mm, 2 × 5 mm ports (through single incision for LESS TEP), 0/30° camera and straight instruments, mesh fixed in majority of cases | |||
|
| ||||||
| Duration of surgery; n, min ± SD | ||||||
|
| ||||||
| Unilateral hernia | n = 39, 48.2 ± 10.8 | n = 43, 51.7 ± 15.1 | n = 19, 40 ± 21.6 | n = 15, 50 ± 14.2 | n = 18, 58.6 ± 23.4 | n = 11, 82.3 ± 39.3 |
|
| ||||||
| Bilateral hernias | n = 13, 85.9 ± 8.2 | n = 9, 85.8 ± 16.5 | n = 3, 60 ± 15.3 | n = 7, 60 ± 24.8 | n = 67, 62.6 ± 26.7 | n = 43, 68.3 ± 18.3 |
|
| ||||||
| Hospital stay, d ± SD | 0.19 ± 0.07 | 0.19 ± 0.06 | 2.0 ± 1.6 | 2.0 ± 1.3 | 1.7 ± 0.8 | 1.7 ± 1.5 |
|
| ||||||
| Intraoperative complications, no. | — | — | 0 | 0 | 0 | 0 |
|
| ||||||
| Length of incision(s), cm (range) | — | — | 3.5 (2.5–4.5) | 2 (1.5–2.5) | Umbilical incision: 1.5 cm | Umbilical incision: 1.5 cm |
|
| ||||||
| Patient satisfaction, scale: 1–5 ± SD | — | — | — | — | 4.1 ± 0.8 | 3.9 ± 0.7 |
|
| ||||||
| Pain, | ||||||
|
| ||||||
| 24 hr | — | — | — | — | 3.4 ± 1.7 | 3.6 ± 2.1 |
|
| ||||||
| 1 wk | — | — | — | — | 1.57 ± 2.31 | 0.29 ± 0.66 |
|
| ||||||
| Return to activity, d ± SD | 11.88 ± 6.07 | 10.94 ± 5.7 | — | — | 3.8 ± 1.2 | 3.4 ± 1.5 |
|
| ||||||
| Recurrence, no. | 0 | 0 | 0 | 1 mesh displacement | 0 | 0 |
LAP = laparoscopic; LESS = laparoendoscopic single site; SD = standard deviation; TEP = totally extraperitoneal.
Demographic characteristics of patients undergoing LESS TEP
Thirteen studies15,19,35–39,41–44,46,47 reported on 325 patients undergoing the LESS TEP procedure. The patient age range was 18–85 years,15,19,35,37–39,41–44,46 and 90% of patients were men.15,19,35,37–39,41–43,46
Surgical technique
Nine studies reported on the use of a balloon to create a preperitoneal space.15,19,35,37,38,41,42,44,47 Seven studies used a single port access device.15,19,36,38,39,41,43 Other techniques included the use of 3 ports through a single incision.35,37,42,44,46,47 A range of 0–45° cameras and straight, curved, articulating or manually bent instruments were used.15,19,35–39,41–44,46,47 Two studies36,43 did not report their mesh fixation method and 1 did not use any form of fixation.19
Outcomes after the LESS TEP approach
Perioperative data
The mean duration of surgery was 40–98 minutes for unilateral hernia repairs15,19,35–37,39,41,42,44,46,47 and 41–121 minutes for bilateral hernia repairs.15,36,38,39,41–44,46,47 Six patients required conversion, although no conversions were to a formal open procedure.15,36,41,42,46 There were only 2 reported intraoperative complications involving bleeding or a peritoneal tear.36,42 Hospital stay ranged from less than a day to 2.15 days.15,19,35,37–39,41–44,46,47 Postoperative recovery was uneventful all but 7 patients: seroma developed in 5 patients, 1 went into ileus and 1 experienced urinary retention).42,44,46,47
Follow-up
Follow-up ranged from 2 weeks to 14 months. Patients reported only minimal discomfort or ache.15,39,42,43 There were only minor complications: epididymitis, wound infection, dehiscience and seroma/hematomas.39,42 Two studies reported on return to activities after a range of 5–14 days.15,42 There were no recurrences reported up to 14 months after the operation.15,19,36,38,39,41–43,47
Comparison with LAP TEP approach
Three studies22,40,45 reported on a total of 128 patients in the LESS TEP group and 159 in the LAP TEP group.
Duration of surgery
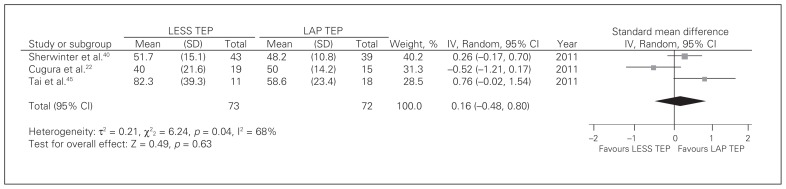
Unilateral hernia repairs
Three studies22,40,45 contributed to a summative outcome. There was significant heterogeneity among trials (Q2 = 6.24, p = 0.040, I2 = 68); therefore the fixed-effects model was inappropriate. There was no difference in duration of surgery between LESS TEP and LAP TEP (random-effects model: SMD = 0.16, 95% confidence interval [CI] −0.48 to 0.80, z = 0.49, p = 0.63; Fig. 2).
Fig. 2.
Duration of surgery for unilateral hernias. CI = confidence interval; IV = inverse variance; LAP = laparoscopic; LESS = laparoendoscopic single site surgery; SD = standard deviation; TEP = totally extraperitoneal.
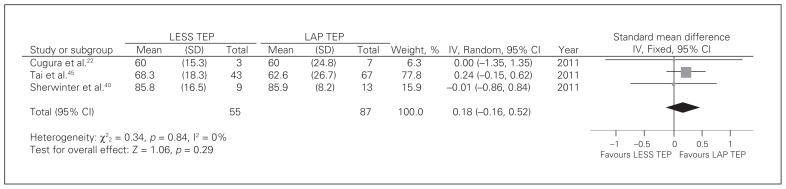
Bilateral hernia repairs
Three studies22,40,45 contributed to a summative outcome. There was no significant heterogeneity among trials (Q2 = 0.34, p = 0.84, I2 = 0). There was no difference in duration of surgery between LESS TEP and LAP TEP (fixed-effects model: SMD = 0.18, 95% CI −0.16 to 0.52, z = 1.06, p = 0.29; Fig. 3).
Fig. 3.
Duration of surgery for bilateral hernias. CI = confidence interval; IV = inverse variance; LAP = laparoscopic; LESS = laparoendoscopic single site surgery; SD = standard deviation; TEP = totally extraperitoneal.
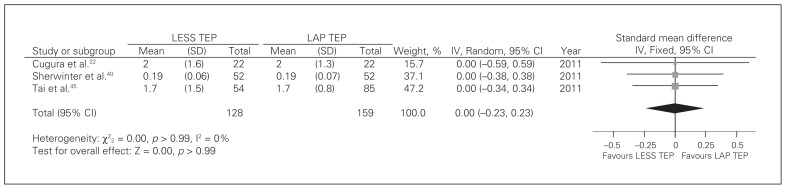
Hospital stay
Three studies22,40,45 reported on hospital stay. There was no significant heterogeneity among trials (Q2 = 0.00, p > 0.99, I2 = 0). There was no difference between groups [fixed-effects model: SMD = 0.00, 95% CI −0.23 to 0.23, z = 0.00, p > 0.99; Fig. 4).
Fig. 4.
Hospital stay. CI = confidence interval; IV = inverse variance; LAP = laparoscopic; LESS = laparoendoscopic single site surgery; SD = standard deviation; TEP = totally extraperitoneal.
Intraoperative complications and conversions
There was no significant heterogeneity among trials (Q1 = 0.05, p = 0.82, I2 = 0). There was no difference between techniques according to the studies included22,45 (fixed-effects model: RR = 1.25, 95% CI 0.18–8.51, z = 0.23, p = 0.82). None of the patients required conversions.22,40,45
Cosmesis and follow-up
The length of the incision in the umbilicus was similar in both techniques (1.5–2 cm);22,45 however, the total length of all incisions was slightly less in the LESS TEP group than the LAP TEP group (2 cm v. 3.5 cm, respectively).22 This difference did not appear to translate into less satisfaction in the LAP TEP group.45
One study40 reported 5 and 6 minor complciations in the LAP TEP and LESS TEP groups, respectively. There were 4 patients with seromas and 1 patient with bladder dysfunction after LAP TEP, and there were 3 patients with seromas and 3 with bladder dysfunction after LESS TEP.
Pain
Only 1 study45 reported on pain. After 24 hours, there appeared to be no difference between techniques; however, after 1 week patients who underwent LESS TEP had significantly less pain. One study40 reported on analgesic use, and although patients undergoing LESS TEP required painkillers for less time than those in the LAP TEP group, the difference was not significant.
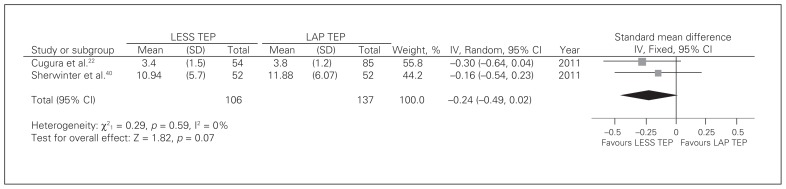
Return to activity
Two studies22,40 reported on return to activity. There was no significant heterogeneity among trials (Q1 = 0.29, p = 0.59, I2 = 0). Patients in the LESS TEP group restarted activity earlier, and this difference approached statistical significance (fixed-effects model: SMD = −0.16, 95% CI −0.49 to 0.02, z = 1.82, p = 0.07; Fig. 5).
Fig. 5.
Return to activity. CI = confidence interval; IV = inverse variance; LAP = laparoscopic; LESS = laparoendoscopic single site surgery; SD = standard deviation; TEP = totally extraperitoneal.
Recurrence
There was no significant heterogeneity among trials (Q1 = 0.05, p = 0.82, I2 = 0). There was no difference between techniques according to the studies included22,45 (fixed-effects model: RR = 1.25, 95% CI 0.18–8.51, z = 0.23, p = 0.82).
Discussion
The nature of surgery has led to developments in techniques to reduce the postoperative stress response and improvement in cosmesis. These include robotic laparoscopy, natural orifice translumenal endoscopic surgery (NOTES) and, increasingly, minimally invasive and LESS surgery.49,50 One of the main challenges to robotic surgery is cost;51 NOTES may be unacceptable to certain groups of patients, whereas LESS may be the most preferred approach.23
Main findings
This paper examined the role of LESS TEP for inguinal hernia repairs and compared it with LAP TEP. Duration of surgery for unilateral and bilateral repairs showed a great variation but appeared comparable to conventional TEP performed by surgeons on different points of their learning curve.52,53 The conversion rate was low (0.02%) and no conversions were to a formal open technique; surgeons preferred to convert to TAPP or add further ports. Postoperative recovery was largely uneventful, and very few complications were noted. No recurrence was noted up to 14 months after surgery, and most patients returned to activity within 2 weeks.
Formal comparison with LAP TEP showed no significant difference in duration of surgery, hospital stay, intraoperative complications, conversions or recurrence. The LESS TEP procedure had a slightly smaller total incision length than LAP TEP. There are equivocal results in relation to pain and analgesic requirements. There was a trend for patients in the LESS TEP group to return to activity earlier, but the difference did not achieve statistical significance (p = 0.07); this result is consistent with the literature showing faster recovery in other settings.54
Importance
The importance of these findings is that for patients with inguinal hernias, a range of safe and effective options is available and may be used to treat dual pathologies.55 Furthermore the LESS technique may offer patients the ability to return to activity earlier, which may be especially important for those who are self-employed.56 This article also suggests that current evidence is strong enough to warrant further trials to establish the role of this technique. Although some articles suggest cosmesis may be better with LESS TEP, LAP TEP is an acceptable technique with good postoperative outcomes.57
Appraisal of evidence
Owing to investment in newer or different instruments or ports, some suggest that LESS techniques are more expensive than conventional laparoscopic techniques; however, recent studies have shown comparability between the 2 techniques.58,59 There is a learning curve associated with LESS techniques; however, it may not be as steep as initially perceived60,61 and depends on a number of factors, including the type of port used for access.62 Nonetheless, experienced surgeons ought to perform or supervise these procedures to ensure adequate training. Furthermore, in the initial stages there may be a higher rate of postoperative complications until such time that the learning curve has reached a plateau.63 Technical challenges include access,64 poor triangulation and lack of space leading to instrument clash,65 which may be overcome by the use of 30° cameras.22 Instrument control may also be less intuitive.41 One disadvantage to LAP TEP is that if complications arise conversion to either LAP TAP or open surgery may be the only options, whereas with LESS TEP conversion to conventional LAP TEP is also an option.
Future advances include robotic surgery; however, recent studies have shown similar durations of surgery, and although remote operating is a definite advantage, costs may be prohibitive.51
From a patient perspective, single incision surgery is more appealing presumably owing to potential cosmetic benefits; however, this should be in the context of an appropriate safety profile.66 The cosmetic concern may be greater in children, with recent studies showing good outcomes.67,68 One factor regarding cosmesis is the position of the scar, with some reports suggesting an intraumbilical or crescenteric incision giving the best outcomes.15,22
Heterogeneity
The literature varied greatly in terms of specifics involved with the LESS TEP technique. In our literature review, some authors used a balloon15,19,35,38,41,42,44,47 to create the preperitoneal space, whereas others used blunt dissection.25,39,43,46 A range and combination of straight or curved and articulating instruments and 0°–45° cameras were used. Only 1 study reported no mesh fixation.19
In our pooled analysis comparing LESS TEP with LAP TEP, there was significant heterogeneity in the duration of surgery for unilateral repairs. This may be related to slightly different technique variations and differences in learning curve. This finding is in keeping with the lack of heterogeneity in duration of bilateral repair, reflecting progression in the number of procedures performed. However, most of the included studies did not state where the bilateral hernias were in relation to their learning curve. There was no significant heterogeneity in relation to hospital stay, recurrence, intraoperative complications or return to activity, which probably reflects similar clinical and follow-up protocols among the centres. Although there was no significanct heterogeneity, there were some clinical differences in the type of technique used (Table 2). For example, some authors used a homemade port,45 some used different cameras and 1 group did not fix the mesh in all patients.22 Only 1 study reported the type of analgesics used and their discharge protocols.40 The activities to which patients returned were not clearly identified, and convalescence may have been very different depending on age, sex and type of employment.56 Other limitations to our study include the use of assessments of the papers according to set criteria. Although this may give an indication to the strength of the study, it may not highlight potential weaknesses, including detailed differences that were not documented in the studies, such as site of pain (umbilical v. pubic due to tacks) or sequelae of complications.
The degree of clinical heterogeneity means firm conclusions for practice need to be made with caution.
Quality assessment
We did not formally assess the quality of the studies included in our initial review. This was generally because of the small numbers in the series and because of the relative paucity of studies in the literature. In our early meta-analysis there was only 1 study22 that stated it was a randomized controlled trial of moderate quality; however, the study did not detail sample size calculations, allocation concealment or analysis based on intention to treat, which may lead to significant bias in reporting outcomes. Furthermore, this same trial did not specifically state it was double-blind. The remaining 2 studies were comparative studies, and 1 was a comparison with a historical cohort, which presents inherent weaknesses. One study45 did not report inclusion or exclusion criteria; the other study40 did not state clearly their diagnostic criteria or identify standardized outcome forms. It is too early to comment on publication bias.
Future studies
Further prospective randomized studies focusing on cosmesis, postoperative pain, analgesic requirements and return to activity are required to assess whether LESS TEP has an advantage over LAP TEP.69 Clear definitions of pain and return to activity should be given with examination of the type of job conducted, as it may be that LESS TEPP may benefit particular groups of workers. Studies should consider the learning curve of the surgeon to ensure appropriate comparisons with LAP TEP in relation to duration of surgery and hospital stay. Our review highlights the need for a multicentre randomized controlled trial with appropriate follow up.
Conclusion
The LESS TEP hernia repair is a relatively new technique and appears to be safe and effective. Advantages, such as less visible scarring, mean patients may opt for LESS TEP over LAP TEP. Further studies with clear definitions of outcome measures and robust follow up to assess patient satisfaction, return to normal daily activities and recurrence are required to strengthen the evidence.
Footnotes
Competing interests: None declared.
Contributors: M.R.S. Siddiqui, M. Kovzel, O. Priest, S.R. Preston and Y. Soon designed the study. M.R.S. Siddiqui and M. Kovzel acquired the data, which M.R.S. Siddiqui, M. Kovzel and S. Brennan analyzed. M.R.S. Siddiqui and M. Kovzel wrote the article, which all authors reviewed and approved for publication.
References
- 1.Health & Social Care Information Centre. Primary diagnosis. [accessed 2012 Feb. 27]. Available: www.hscic.gov.uk/searchcatalogue?productid=13264&q=hospital+episode+statistics&sort=Relevance&size=10&page=1#top.
- 2.Health & Social Care Information Centre. Main procedures and interventions. [accessed 2012 Feb. 27]. Available: www.hscic.gov.uk/searchcatalogue?productid=13264&q=hospital+episode+statistics&sort=Relevance&size=10&page=1#top.
- 3.Kingsnorth AN, LeBlanc KA. Management of abdominal hernias. 3rd ed. London: Edward Arnold; 2003. pp. 40–47. [Google Scholar]
- 4.Kingsnorth A, LeBlanc KA. Hernias: inguinal and incisional. Lancet. 2003;362:1561–71. doi: 10.1016/S0140-6736(03)14746-0. [DOI] [PubMed] [Google Scholar]
- 5.Lichtenstein IL, Shulman AG, Amid PK, et al. The tension-free hernioplasty. Am J Surg. 1989;157:188–93. doi: 10.1016/0002-9610(89)90526-6. [DOI] [PubMed] [Google Scholar]
- 6.Spaw AT, Ennis BW, Spaw LP. Laparoscopic hernia repair: the anatomic basis. J Laparoendosc Surg. 1991;1:269–77. doi: 10.1089/lps.1991.1.269. [DOI] [PubMed] [Google Scholar]
- 7.Corbitt JD., Jr Laparoscopic herniorrhaphy. Surg Laparosc Endosc. 1991;1:23–5. [PubMed] [Google Scholar]
- 8.Zendejas B, Ramirez T, Jones T, et al. Trends in the utilization of inguinal hernia repair techniques: a population-based study. Am J Surg. 2012;203:313–7. doi: 10.1016/j.amjsurg.2011.10.005. discussion 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eklund A, Montgomery A, Bergkvist L, et al. Chronic pain 5 years after randomized comparison of laparoscopic and Lichtenstein inguinal hernia repair. Br J Surg. 2010;97:600–8. doi: 10.1002/bjs.6904. [DOI] [PubMed] [Google Scholar]
- 10.Hamza Y, Gabr E, Hammadi H, et al. Four-arm randomized trial comparing laparoscopic and open hernia repairs. Int J Surg. 2010;8:25–8. doi: 10.1016/j.ijsu.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 11.Karthikesalingam A, Markar SR, Holt PJ, et al. Meta-analysis of randomized controlled trials comparing laparoscopic with open mesh repair of recurrent inguinal hernia. Br J Surg. 2010;97:4–11. doi: 10.1002/bjs.6902. [DOI] [PubMed] [Google Scholar]
- 12.Pawanindra Lal, Philips P, Chander J, et al. Is unilateral laparoscopic TEP inguinal hernia repair a job half done? The case for bilateral repair. Surg Endosc. 2010;24:1737–45. doi: 10.1007/s00464-009-0841-4. [DOI] [PubMed] [Google Scholar]
- 13.Duvie SO. One-stage bilateral inguinal herniorrhaphy in the adult. Can J Surg. 1984;27:192–3. [PubMed] [Google Scholar]
- 14.Sayad P, Abdo Z, Cacchione R, et al. Incidence of incipient contralateral hernia during laparoscopic hernia repair. Surg Endosc. 2000;14:543–5. doi: 10.1007/s004640000101. [DOI] [PubMed] [Google Scholar]
- 15.Tran H. Safety and efficacy of single incision laparoscopic surgery for total extraperitoneal inguinal hernia repair. JSLS. 2011;15:47–52. doi: 10.4293/108680811X13022985131174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kucuk C. Single-incision laparoscopic transabdominal preperitoneal herniorrhaphy for recurrent inguinal hernias: preliminary surgical results. Surg Endosc. 2011;25:3228–34. doi: 10.1007/s00464-011-1698-x. [DOI] [PubMed] [Google Scholar]
- 17.Krishna A, Misra MC, Bansal VK, et al. Laparoscopic inguinal hernia repair: transabdominal preperitoneal (TAPP) versus totally extraperitoneal (TEP) approach: a prospective randomized controlled trial. Surg Endosc. 2012;26:639–49. doi: 10.1007/s00464-011-1931-7. [DOI] [PubMed] [Google Scholar]
- 18.McCormack K, Wake BL, Fraser C, et al. Transabdominal preperitoneal (TAPP) versus totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair: a systematic review. Hernia. 2005;9:109–14. doi: 10.1007/s10029-004-0309-3. [DOI] [PubMed] [Google Scholar]
- 19.Do M, Liatsikos E, Beatty J, et al. Laparoendoscopic single-site extraperitoneal inguinal hernia repair: initial experience in 10 patients. J Endourol. 2011;25:963–8. doi: 10.1089/end.2010.0696. [DOI] [PubMed] [Google Scholar]
- 20.Wen KC, Lin KY, Chen Y, et al. Feasibility of single-port laparoscopic cholecystectomy using a homemade laparoscopic port: a clinical report of 50 cases. Surg Endosc. 2011;25:879–82. doi: 10.1007/s00464-010-1287-4. [DOI] [PubMed] [Google Scholar]
- 21.Hirano D, Minei S, Yamaguchi K, et al. Retroperitoneoscopic adrenalectomy for adrenal tumors via a single large port. J Endourol. 2005;19:788–92. doi: 10.1089/end.2005.19.788. [DOI] [PubMed] [Google Scholar]
- 22.Cugura JF, Kirac I, Kulis T, et al. Comparison of single incision laparoscopic totally extraperitoneal and laparoscopic totally extraperitoneal inguinal hernia repair: initial experience. J Endourol. 2012;26:63–6. doi: 10.1089/end.2011.0352. [DOI] [PubMed] [Google Scholar]
- 23.Rao A, Kynaston J, MacDonald ER, et al. Patient preferences for surgical techniques: Should we invest in new approaches? Surg Endosc. 2010;24:3016–25. doi: 10.1007/s00464-010-1078-y. [DOI] [PubMed] [Google Scholar]
- 24.Ahmed I, Paraskeva P. A clinical review of single-incision laparoscopic surgery. Surgeon. 2011;9:341–51. doi: 10.1016/j.surge.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 25.Bucher P, Pugin F, Buchs NC, et al. Randomized clinical trial of laparoendoscopic single-site versus conventional laparoscopic cholecystectomy. Br J Surg. 2011;98:1695–702. doi: 10.1002/bjs.7689. [DOI] [PubMed] [Google Scholar]
- 26.Lee J, Baek J, Kim W. Laparoscopic transumbilical single-port appendectomy: initial experience and comparison with three-port appendectomy. Surg Laparosc Endosc Percutan Tech. 2010;20:100–3. doi: 10.1097/SLE.0b013e3181d84922. [DOI] [PubMed] [Google Scholar]
- 27.Tsai AY, Selzer DJ. Single-port laparoscopic surgery. Adv Surg. 2010;44:1–27. doi: 10.1016/j.yasu.2010.05.017. [DOI] [PubMed] [Google Scholar]
- 28.Rangel SJ, Kelsey J, Colby CE, et al. Development of a quality assessment scale for retrospective clinical studies in pediatric surgery. J Pediatr Surg. 2003;38:390–6. doi: 10.1053/jpsu.2003.50114. [DOI] [PubMed] [Google Scholar]
- 29.SIGN guidelines. [accessed 2013 Jan. 18]. Available: www.sign.ac.uk/guidelines/fulltext/50/checklist3.htm.
- 30.Chalmers TC, Smith H, Jr, Blackburn B, et al. A method for assessing the quality of a randomized control trial. Control Clin Trials. 1981;2:31–49. doi: 10.1016/0197-2456(81)90056-8. [DOI] [PubMed] [Google Scholar]
- 31.Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 32.Manager R. (RevMan) [computer program], (2008) version 5.0. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; [Google Scholar]
- 33.Egger M, Smith GD, Altman DG. Systematic reviews in healthcare. London (UK): BMJ Publishing; 2006. [Google Scholar]
- 34.Deeks JJ, Altman DG, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. In: Group BP, editor. Systematic reviews in health care: meta-analysis in context. 2nd ed. London (UK): BMJ Publishing; 2001. [Google Scholar]
- 35.Cugura JF, Kirac I, Kulis T, et al. First case of single incision laparoscopic surgery for totally extraperitoneal inguinal hernia repair. Acta Clin Croat. 2008;47:249–52. [PubMed] [Google Scholar]
- 36.Bucher P, Pugin F, Morel P. Single port totally extraperitoneal laparoscopic inguinal hernia repair. Re: Single incision total extraperitoneal (one SITE) laparoscopic inguinal hernia repair using a single access port device, B. P. Jacob et al. (2009) Hernia. 2009;13:667–8. doi: 10.1007/s10029-009-0564-4. [DOI] [PubMed] [Google Scholar]
- 37.Filipovic-Cugura J, Kirac I, Kulis T, et al. Single-incision laparoscopic surgery (SILS) for totally extraperitoneal (TEP) inguinal hernia repair: first case. Surg Endosc. 2009;23:920–1. doi: 10.1007/s00464-008-0318-x. [DOI] [PubMed] [Google Scholar]
- 38.Jacob BP, Tong W, Reiner M, et al. Single incision total extraperitoneal (one SITE) laparoscopic inguinal hernia repair using a single access port device. Hernia. 2009;13:571–2. doi: 10.1007/s10029-009-0521-2. [DOI] [PubMed] [Google Scholar]
- 39.Agrawal S, Shaw A, Soon Y. Single-port laparoscopic totally extraperitoneal inguinal hernia repair with the TriPort system: initial experience. Surg Endosc. 2010;24:952–6. doi: 10.1007/s00464-009-0663-4. [DOI] [PubMed] [Google Scholar]
- 40.Sherwinter DA. Transitioning to single-incision laparoscopic inguinal herniorrhaphy. JSLS. 2010;14:353–7. doi: 10.4293/108680810X12924466007485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Surgit O. Single-incision laparoscopic surgery for total extraperitoneal repair of inguinal hernias in 23 patients. Surg Laparosc Endosc Percutan Tech. 2010;20:114–8. doi: 10.1097/SLE.0b013e3181d848c3. [DOI] [PubMed] [Google Scholar]
- 42.Chung SD, Huang CY, Wang SM, et al. Laparoendoscopic single-site totally extraperitoneal adult inguinal hernia repair: initial 100 patients. Surg Endosc. 2011;25:3579–83. doi: 10.1007/s00464-011-1761-7. [DOI] [PubMed] [Google Scholar]
- 43.He K, Chen H, Ding R, et al. Single incision laparoscopic totally extraperitoneal inguinal hernia repair. Hernia. 2011;15:451–3. doi: 10.1007/s10029-010-0674-z. [DOI] [PubMed] [Google Scholar]
- 44.Tai HC, Ho CH, Tsai YC. Laparoendoscopic single-site surgery: adult hernia mesh repair with homemade single port. Surg Laparosc Endosc Percutan Tech. 2011;21:42–5. doi: 10.1097/SLE.0b013e31820ad65a. [DOI] [PubMed] [Google Scholar]
- 45.Tai HC, Lin CD, Chung SD, et al. A comparative study of standard versus laparoendoscopic single-site surgery (LESS) totally extraperitoneal (TEP) inguinal hernia repair. Surg Endosc. 2011;25:2879–83. doi: 10.1007/s00464-011-1636-y. [DOI] [PubMed] [Google Scholar]
- 46.Kim JH, Park SM, Kim JJ, et al. Initial experience of single port laparoscopic totally extraperitoneal hernia repair: nearly-scarless inguinal hernia repair. J Korean Surg Soc. 2011;81:339–43. doi: 10.4174/jkss.2011.81.5.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shih TY, Wen KC, Lin KY, et al. Transumbilical, single-port, totally extraperitoneal, laparoscopic inguinal hernia repair using a homemade port and a conventional instrument: an initial experience. J Laparoendosc Adv Surg Tech A. 2012;22:162–4. doi: 10.1089/lap.2011.0235. [DOI] [PubMed] [Google Scholar]
- 48.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Menenakos C, Kilian M, Hartmann J. Single-port access in laparoscopic bilateral inguinal hernia repair: first clinical report of a novel technique. Hernia. 2010;14:309–12. doi: 10.1007/s10029-009-0534-x. [DOI] [PubMed] [Google Scholar]
- 50.Rane A, Ahmed S, Kommu SS, et al. Single-port ‘scarless’ laparoscopic nephrectomies: the United Kingdom experience. BJU Int. 2009;104:230–3. doi: 10.1111/j.1464-410X.2009.08399.x. [DOI] [PubMed] [Google Scholar]
- 51.Tran H. Robotic single-port hernia surgery. JSLS. 2011;15:309–14. doi: 10.4293/108680811X13125733356198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Haidenberg J, Kendrick ML, Meile T, et al. Totally extraperitoneal (TEP) approach for inguinal hernia: the favorable learning curve for trainees. Curr Surg. 2003;60:65–8. doi: 10.1016/S0149-7944(02)00657-8. [DOI] [PubMed] [Google Scholar]
- 53.Choi YY, Kim Z, Hur KY. Learning curve for laparoscopic totally extraperitoneal repair of inguinal hernia. Can J Surg. 2012;55:33–6. doi: 10.1503/cjs.019610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ahmed K, Wang TT, Patel VM, et al. The role of single-incision laparoscopic surgery in abdominal and pelvic surgery: a systematic review. Surg Endosc. 2011;25:378–96. doi: 10.1007/s00464-010-1208-6. [DOI] [PubMed] [Google Scholar]
- 55.Huang CP, Huang CY, Chang CH, et al. Single-incision laparoscopic surgery for vesical diverticulectomy with total extraperitoneal hernioplasty for bladder diverticulum concomitant with right inguinal hernia-a case report. Int J Urol. 2010;17(S1):A318. [Google Scholar]
- 56.Siddiqui MR, Barry J, Lodha K, et al. Age and sex differences in complications and convalescence after laparoscopic cholecystectomy. Magy Seb. 2011;64:193–201. doi: 10.1556/MaSeb.64.2011.4.3. [DOI] [PubMed] [Google Scholar]
- 57.Froghi F, Sodergren MH, Darzi A, et al. Single-incision laparoscopic surgery (SILS) in general surgery: a review of current practice. Surg Laparosc Endosc Percutan Tech. 2010;20:191–204. doi: 10.1097/SLE.0b013e3181ed86c6. [DOI] [PubMed] [Google Scholar]
- 58.Love KM, Durham CA, Meara MP, et al. Single-incision laparoscopic cholecystectomy: a cost comparison. Surg Endosc. 2011;25:1553–8. doi: 10.1007/s00464-010-1433-z. [DOI] [PubMed] [Google Scholar]
- 59.Ayloo SM, Buchs NC, Addeo P, et al. Traditional versus single-site placement of adjustable gastric banding: a comparative study and cost analysis. Obes Surg. 2011;21:815–9. doi: 10.1007/s11695-010-0259-z. [DOI] [PubMed] [Google Scholar]
- 60.Park YH, Baik KD, Lee YJ, et al. Learning curve analysis for laparoendoscopic single-site radical nephrectomy. J Endourol. 2012;26:494–8. doi: 10.1089/end.2011.0473. [DOI] [PubMed] [Google Scholar]
- 61.Gawart M, Dupitron S, Lutfi R. Laparoendoscopic single-site gastric bands versus standard multiport gastric bands: a comparison of technical learning curve measured by surgical time. Am J Surg. 2012;203:327–9. doi: 10.1016/j.amjsurg.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 62.Brown-Clerk B, de Laveaga AE, LaGrange CA, et al. Laparoendoscopic single-site (LESS) surgery versus conventional laparoscopic surgery: comparison of surgical port performance in a surgical simulator with novices. Surg Endosc. 2011;25:2210–8. doi: 10.1007/s00464-010-1524-x. [DOI] [PubMed] [Google Scholar]
- 63.Irwin BH, Cadeddu JA, Tracy CR, et al. Complications and conversions of upper tract urological laparoendoscopic single-site surgery (LESS): multicentre experience: results from the NOTES Working Group. BJU Int. 2011;107:1284–9. doi: 10.1111/j.1464-410X.2010.09663.x. [DOI] [PubMed] [Google Scholar]
- 64.Ross SB, Clark CW, Morton CA, Rosemurgy AS. Access for laparoendoscopic single site surgery. Diagn Ther Endosc. 2010;2010:943091. doi: 10.1155/2010/943091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fader AN, Levinson KL, Gunderson CC, et al. Laparoendoscopic single-site surgery in gynaecology: a new frontier in minimally invasive surgery. J Minim Access Surg. 2011;7:71–7. doi: 10.4103/0972-9941.72387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chow A, Purkayastha S, Dosanjh D, et al. Patient reported outcomes and their importance in the development of novel surgical techniques. Surg Innov. 2012;19:327–34. doi: 10.1177/1553350611426011. [DOI] [PubMed] [Google Scholar]
- 67.Yamoto M, Morotomi Y, Yamamoto M, et al. Single-incision laparoscopic percutaneous extraperitoneal closure for inguinal hernia in children: an initial report. Surg Endosc. 2011;25:1531–4. doi: 10.1007/s00464-010-1430-2. [DOI] [PubMed] [Google Scholar]
- 68.Rothenberg SS, Shipman K, Yoder S. Experience with modified single-port laparoscopic procedures in children. J Laparoendosc Adv Surg Tech A. 2009;19:695–8. doi: 10.1089/lap.2009.0148. [DOI] [PubMed] [Google Scholar]
- 69.Podolsky ER, Curcillo PG., II Single port access (SPA) surgery — a 24-month experience. J Gastrointest Surg. 2010;14:759–67. doi: 10.1007/s11605-009-1081-6. [DOI] [PubMed] [Google Scholar]