Abstract
Objective
To examine the magnitude of explicit and implicit weight biases compared to biases against other groups; and identify student factors predicting bias in a large national sample of medical students.
Design and Methods
A web-based survey was completed by 4732 1st year medical students from 49 medical schools as part of a longitudinal study of medical education. The survey included a validated measure of implicit weight bias, the implicit association test, and 2 measures of explicit bias: a feeling thermometer and the anti-fat attitudes test.
Results
A majority of students exhibited implicit (74%) and explicit (67%) weight bias. Implicit weight bias scores were comparable to reported bias against racial minorities. Explicit attitudes were more negative toward obese people than toward racial minorities, gays, lesbians, and poor people. In multivariate regression models, implicit and explicit weight bias was predicted by lower BMI, male sex, and non-Black race. Either implicit or explicit bias was also predicted by age, SES, country of birth, and specialty choice.
Conclusions
Implicit and explicit weight bias is common among 1st year medical students, and varies across student factors. Future research should assess implications of biases and test interventions to reduce their impact.
Keywords: Weight bias, stigma, medical students, BMI, stereotyping, education
Introduction
A growing body of research suggests healthcare providers’ explicit and implicit biases about patients’ stigmatized social characteristics can influence the quality and content of the care they provide.[1–3] The majority of this research has focused on the impact of implicit and explicit racial bias. Explicit biases are intentional and conscious and are assessed using self-report measures. Implicit biases are automatically activated, may occur unconsciously, and are typically measured using response-latency tasks like the Implicit Association Task (IAT), which measure the strength of association between social categories and attitudes. Implicit and explicit racial bias are only modestly related [4, 5] and independently predict discrimination.[5] Within the medical context, implicit and explicit racial bias have been linked to disparities in provider decision-making,[3, 5] communication quality,[6] and patient ratings of care.[1]
The impact of implicit and explicit attitudes about obese patients on provider behavior has received less study, although healthcare providers [7–11] have been found to hold explicit negative attitudes, including stereotypes of obese people as lazy, unmotivated, noncompliant, and unhealthy. Healthcare providers display less respect for obese patients. [12, 13] Because lower respect predicts less positive affective communication and information giving,[14] these findings have significant implications for interpersonal processes of care. Common stereotypes of obese people as lazy or unmotivated may undermine interpersonal behavior given findings that physicians engage in less patient-centered communication with patients they believe will not comply with recommendations.[15] The few extant studies that directly examine the impact of provider attitudes toward obese patients support these concerns. In one study, physicians who read patient vignettes expressed less desire to help obese patients and rated them as a greater waste of time.[12] Other studies have found that physicians spend less time educating obese patients about their health and building rapport.[16, 17] Obese patients may sense these attitudes, and have reported experiencing stigma while seeking healthcare. [18–20] At least partially as a result of these experiences, obese patients are more likely to avoid follow-up and preventive care. [18, 20–22]
Understanding provider weight bias is especially important given the large and growing prevalence of obesity in the US. Although the medical profession attracts people who are highly committed to helping others, those pursuing the profession are still susceptible to societal biases against obese people. Little is known about what factors protect providers from this bias; thus it is critical to understand the attitudes of individuals entering the medical profession in order to inform curricula to reduce biases and ensure high-quality, equitable care. If biases are not formally addressed in medical school, informal influences in the medical school environment, such as faculty biases [23] or derogatory humor about obese people [24] may reinforce or increase bias.
Also unknown are the student factors associated with weight bias. For example, students who enter primary care specialties that require more patient communication may have less negative attitudes toward stigmatized groups.[2] As a result, we have little evidence to guide the timing and targets of interventions to reduce weight bias among medical students. This study represents a first step in addressing this evidence gap by 1) examining the prevalence and intensity of explicit and implicit weight bias among incoming medical students, and 2) identifying student characteristics that predict weight bias.
Method
Sample
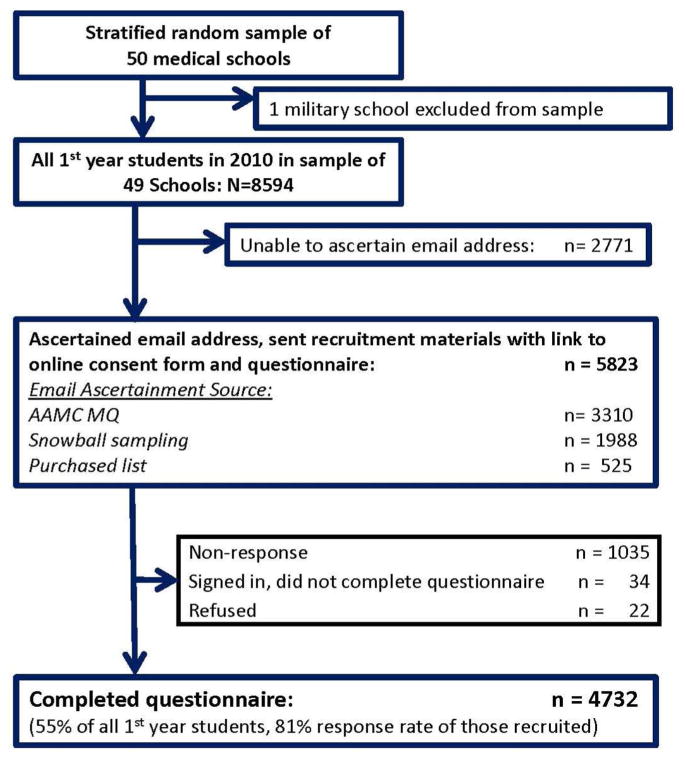
This study uses baseline data collected as part of the Medical Student Cognitive Habits and Growth Evaluation Study (CHANGES), a longitudinal study of medical students who matriculated in US medical schools in the fall of 2010. CHANGES is designed to examine changes in medical students’ well-being, experiences and attitudes during medical school. This research study was approved by the IRBs of Mayo Clinic, the University of Minnesota, and Yale University. We randomly selected 50 medical schools from strata of public/private schools and 6 regions of the country using sample proportional to strata size methodology. One sampled school had highly unique characteristics (military school) that would have limited the generalizability of our study findings and was excluded, leaving a sample of 49 schools. Since there are no comprehensive lists of 1st year students (MS1) available early-mid fall, we used the following methods to ascertain as many of the 8594 MS1 attending the 49 schools as possible (see figure 1).
Figure 1.
Flowchart showing ascertainment strategies and number of participants enrolled with each strategy
The AAMC inserted a question into their voluntary Matriculation Questionnaire, sent to all incoming students, asking respondents to provide an email address to learn more about our study.
We purchased a list (as stated above, incomplete) of MS1 from an AMA-licensed vendor.
We used snowball sampling to ascertain additional MS1. When MS1 completed the web-based measures they received study information to forward to classmates. MS1 who contacted us were screened for eligibility and invited to participate.
We ascertained and invited 5823 students (68% of all MS1 attending sampled schools) to participate in the web-based survey. The sample (n=4732) consists of 81% of those sent an invitation and 55% of the entire pool of MS1, which is comparable to other published studies of medical students.[25] The sample had similar gender and race distributions to the population of all MS1 in study schools. All students completed the survey during their first semester of medical school.
Data Collection and Integrity
Students identified as MS1 in a sampled school were sent an email or letter with a link to the informed consent page. Those who consented were linked to an online questionnaire. Time spent on each page of the questionnaire and total time to completion were recorded. If participants attempted to move to the next page with an unanswered question on the current screen, a warning directed them back to the unanswered question. If they chose not to answer that question, they had to click on a button to indicate their desire to skip the question. This protected participants’ right to skip questions while eliminating time-saving incentives for doing so. After students completed the questionnaire they completed two Implicit Associations Tests (IATs). All participants were given the Race IAT and 50% were randomly assigned to either the anti-fat (n=2370) or another IAT. Upon completing the IATs, participants provided their name and address to receive a $50.00 cash incentive. This allowed us to identify and eliminate duplicates, and confirm that snowball-sampled respondents were MS1 at the school they identified. Responses were examined for indications of systematic response bias (e.g. clicking the same response option to move rapidly through the questionnaire). Invalid or incomplete questionnaires were omitted (n=32).
Measures
Common survey questions were used to measure age, sex, race, Hispanic/Latino ethnicity, country of birth, height, and weight. Respondents who identified multiple race/ethnic groups were categorized into one of those groups in the following order: black, Hispanic, South Asian, East Asian, white. Body mass index (BMI) was calculated. Students reported both parents’ education, and we created SES categories based on the highest education attained by either parent: doctoral degree, master’s degree, bachelor’s degree, or no college degree. Students recruited via the AAMC questionnaire were asked if we could link their survey responses to the AAMC Matriculation Questionnaire. Those who declined (n=316) and those who were recruited via another strategy received additional items assessing intended medical specialization. Students who chose family practice, internal medicine, preventative medicine, or pediatrics were considered primary care track students.
Implicit weight bias was measured with the fat-thin IAT. The IAT is a validated measure of automatic, unconscious attitudes that compares the time required to categorize images of fat and thin people together with positive and negative words.[4, 5] We categorized the IAT difference scores according to commonly-used cutpoints for slight, moderate, and strong bias.
Explicit weight bias was measured using a validated “feeling thermometer” strategy in which participants indicated their feelings toward obese people by moving a slider along a thermometer.[26] Numbers along the thermometer ranged from 0–100 degrees, by 10s, with ends labeled “very warm or favorable” and “very cold or unfavorable.” Participants completed several feeling thermometers for different groups, and raw thermometer scores toward obese people and members of other social groups were subtracted from thermometer scores toward white people. This allowed us to consider feelings toward obese people relative to a non-stigmatized majority group, and account for differences in the respondent’s likelihood to cluster scores around any specific point.
Explicit attitudes about obese people and obesity were measured with items selected from Crandall’s anti-fat attitudes questionnaire (AFAT) (Table 3).[27] All items were measured on a 7-point scale from strongly disagree to strongly agree. Using principal components analysis, three subscales were identified that are consistent with previous studies. 1) Dislike of fat people (3 items, Cronbach’s alpha=.86). 2) Willpower/blame (2 items, alpha= .79). 3) Fear of fat (2 items, alpha=.79).
Table 3. Prevalence of Explicit Anti-fat Attitudes.
Table 3 shows the wording of the explicit bias measure items, and the proportion of the sample who agree slightly, moderately or strongly with each item. Also included is the proportion who agrees moderately or strongly with at least one scale item.
| % (n) slightly agreeing with the item | % (n) moderately or strongly agreeing with the item | |
|---|---|---|
| Dislike | ||
| I really don’t like fat people much. | 11.4% (521) | 4.7% (221) |
| I have a hard time taking fat people seriously | 10.2% (473) | 3.2% (149) |
| Fat people make me feel somewhat uncomfortable | 14.8% (681) | 3.5% (162) |
| ≥ 1 scale item | 6.9% (316) | |
| Blame | ||
| Fat people tend to be fat pretty much through their own fault | 21.8% (1020) | 14.8% (696) |
| Some people are fat because they have no will power | 34.2% (1578) | 25.8% (1210) |
| ≥ 1 scale item | 29.8% (1392) | |
| Fear | ||
| I feel disgusted with myself when I gain weight | 28.8% (1346) | 32.5% (1489) |
| I worry about becoming fat | 28.4% (1325) | 39.6% (1823) |
| ≥ 1 scale item | 45.8% (2109) |
Analysis
Analyses were adjusted for complex sampling probabilities. We calculated descriptive statistics for sample characteristics and attitudes; and calculated correlations between bias and attitude measures. Then, we performed analyses of variance (ANOVAs) or simple linear regression to assess associations between attitude/bias scores and student characteristics. Characteristics that predict weight bias in other populations, [23, 28, 29] and/or have implications for clinical care, were selected for modeling. We used results of these bivariate models to choose reference categories for independent variables in multivariate models, and calculated 5 multivariate general linear models, simultaneously adjusted for all student and school characteristics to control for confounding. We report beta coefficients and p-values from global adjusted F-tests and individual parameter t-tests. Because students from different race groups may rate whites differently, we used an additional multivariate model to assess the association between race and raw “obese people” feeling thermometer score as a sensitivity analysis.
Results
Sample characteristics are presented in table 1. Table 2 shows that implicit bias was weakly correlated with explicit bias, dislike of fat people, and beliefs that obese people have low willpower. Explicit bias was strongly correlated with dislike and blame, and moderately correlated with fear of fat.
Table 1. Sample Characteristics and Bivariate Associations with Weight Bias and Attitudes (N=4732).
Table 1 shows the descriptive information about the sample, as well as the bivariate relationships between demographic and other descriptors of the sample and implicit and explicit weight bias
| Descriptive | Implicit Bias | Explicit Bias | Explicit Attitudes | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Continuous Predictors | IAT | Thermometer | Dislike | Willpower | Fear | |
|
| ||||||
| Age | Mean= 23.9 | beta= −.002 | beta= −.51 | beta= −.02 | beta= −.02 | beta= −.03 |
| p-value for F-test | SE=.06 | p=.53 | p<.001 | p=.001 | p=.02 | p=.001 |
|
| ||||||
| BMI | Mean= 23.3 | beta= −.01 | beta= −.41 | beta= −.02 | beta= .02 | beta= .10 |
| p-value for F-test | SE=.06 | p=.003 | p<.001 | p<.001 | p=.01 | p<.001 |
|
| ||||||
| Categorical Predictors | % (n) | Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) |
|
| ||||||
| Sex | ||||||
| Female | 50 (2363) | .40 (.01) | 15.68 (.36) | 2.20 (.03) | 3.66 (.03) | 4.96 (.04) |
| Male | 50 (2369) | .43 (.01) | 16.86 (.47) | 2.38 (.03) | 4.26 (.03) | 4.15 (.03) |
| p-value for F-test | .12 | .03 | <.001 | <.001 | <.001 | |
|
| ||||||
| Race/Ethnicity | ||||||
| Black | 6 (301) | .29 (.03) | 8.62 (1.15) | 1.72 (.05) | 3.43 (.08) | 4.03 (.09) |
| Hispanic | 6 (269) | .44 (.03) | 14.55 (1.36) | 2.18 (.06) | 3.82 (.07) | 4.67 (.10) |
| East Asian | 14 (640) | .39 (.02) | 15.47 (.61) | 2.48 (.05) | 3.73 (.05) | 4.54 (.07) |
| South Asian | 10 (479) | .35 (.03) | 12.57 (.69) | 2.15 (.05) | 3.68 (.06) | 4.60 (.07) |
| White | 65 (2913) | .44 (.01) | 18.12 (.37) | 2.34 (.03) | 4.13 (.03) | 4.60 (.03) |
| p-value for F-test | <.001 | <.001 | <.001 | <.001 | <.001 | |
|
| ||||||
| Born in USA | ||||||
| Yes | 84 (3927) | .43 (.01) | 16.79 (.35) | 2.31 (.02) | 4.01 (.03) | 4.59 (.03) |
| No | 16 (729) | .34 (.02) | 13.82 (.64) | 2.22 (.04) | 3.76 (.05) | 4.37 (.05) |
| p-value for F-test | .001 | <.001 | .08 | <.001 | <.001 | |
|
| ||||||
| Parent’s Highest Degree | ||||||
| Doctoral | 38 (1760) | .39 (.01) | 17.34 (.46) | 2.34 (.03) | 3.95 (.03) | 4.51 (.03) |
| Masters | 25 (1178) | .43 (.01) | 17.12 (.58) | 2.34 (.03) | 3.98 (.04) | 4.65 (.04) |
| Bachelors | 22 (1023) | .44 (.02) | 15.68 (.56) | 2.24 (.04) | 4.00 (.05) | 4.57 (.04) |
| < Bachelor | 16 (721) | .44 (.02) | 13.31 (.73) | 2.17 (.04) | 3.96 (.05) | 4.48 (.06) |
| p-value for F-test | .03 | .001 | .001 | .84 | .03 | |
|
| ||||||
| Anticipated Specialty | ||||||
| Primary Care | 36 (1558) | .43 (.01) | 14.02 (.42) | 2.14 (.03) | 3.77 (.04) | 4.51 (.04) |
| Specialty | 64 (2746) | .42 (.01) | 17.79 (.48) | 2.38 (.03) | 4.09 (.03) | 4.60 (.03) |
| p-value for F-test | .74 | <.001 | <.001 | <.001 | .09 | |
Table 2. Correlations, Means, and Standard Deviations of Weight Bias and Attitude Measures.
Table 2 shows the means and standard errors of each measure of explicit and implicit bias in this sample, as well as the correlation coefficients between each measure.
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. Implicit Bias | 1.00 | ||||
| 2. Explicit Bias | .13 | 1.00 | |||
| 3. Dislike for Fat People | .11 | .51 | 1.00 | ||
| 4. Blame/lack willpower | .10 | .35 | .42 | 1.00 | |
| 5. Fear of Fat | .01 | .13 | .19 | .19 | 1.00 |
| Mean | .42 | 16.27 | 2.29 | 3.96 | 4.55 |
| Standard Error | .01 | .33 | .02 | .02 | .02 |
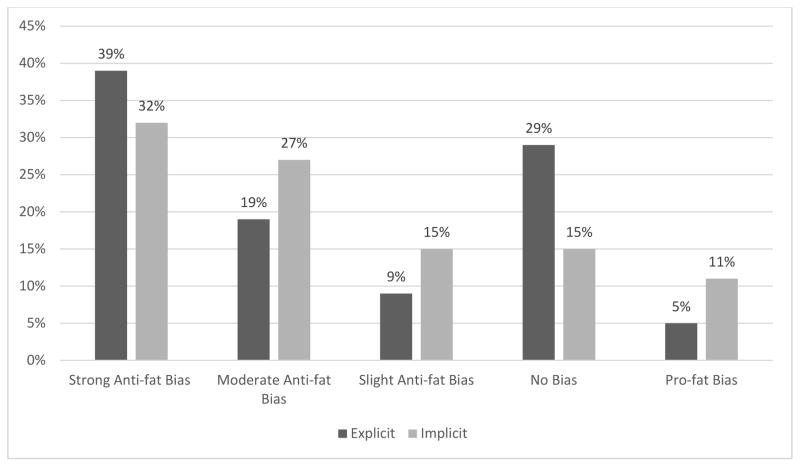
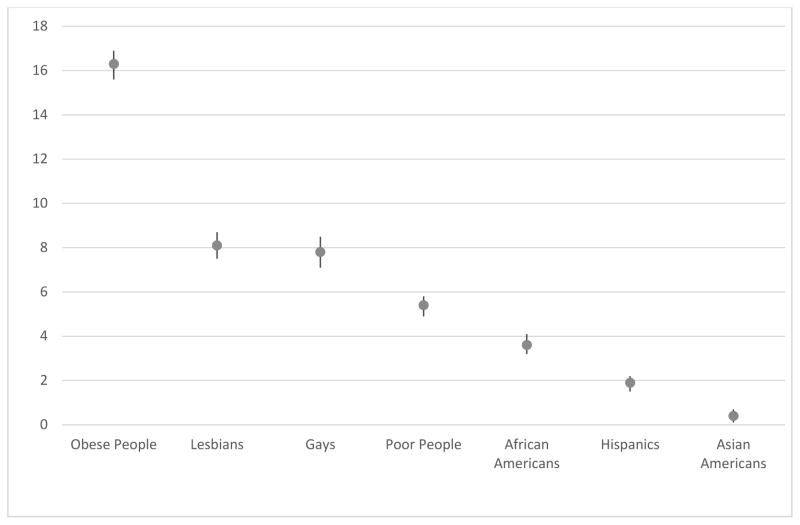
The mean IAT score was .42 (Table 2), representing moderate bias against obese people. Figure 2 shows the distribution of categorized IAT scores and explicit bias scores. Strong, moderate or slight bias was demonstrated by 74%, with 32% showing strong bias. Explicit bias was similarly prevalent; 67% of students explicitly rated obese people less positively than whites. Figure 3 depicts positivity toward several groups relative to whites. All race and ethnic groups, gays, lesbian, and poor people are clustered within 8 degrees of ratings of whites. Obese people were rated an average of 16.3 degrees lower than white people.
Figure 2. Distribution of explicit and implicit weight bias in a national sample of medical students.
An IAT score ≥ .65 was considered strong; a score < .65 and ≥ .35, moderate; and a score <.35 and ≥.15, slight anti-fat bias. A score > −.15 and <.15 was considered no bias, and a score ≤ −.15 was considered pro-fat bias. For explicit bias, a difference between feeling thermometer scores for Whites and obese people > 15 was considered strong; a difference between 6 and 15, moderate; and difference between 1 and 5, slight anti-fat bias. A difference of 0 was no bias, and a difference < 0 was pro-fat bias.
Figure 3. Explicit bias against people who are obese and other stigmatized/minority groups relative to Whites.
The dots represent the sample mean of each participant’s rating of whites minus their rating of obese people on feeling thermometers. Higher numbers indicate lower warmth toward the group relative to Whites. The bars represent the 95% confidence intervals
The mean explicit dislike score was 2.29, with 7% moderately or strongly agreeing with at least 1 item (Table 3). The mean blame/lack of willpower score was 3.96, with 30% moderately or strongly agreeing with at least 1 item. The mean fear of fat score was 4.55, with 46% moderately or strongly agreeing with at least 1 item.
Several student characteristics predicted implicit and explicit bias and attitudes in bivariate models (table 1). Implicit and explicit weight bias, and each explicit attitude, was associated with lower BMI and differed across race groups, with blacks consistently displaying the least bias. Implicit and explicit weight bias, blame, and fear of fat were greater among students born in the US. Implicit weight bias was associated with lower parental education. Explicit weight bias was associated with male sex, younger age, higher parent education, and plans to specialize in a non-primary care field. Younger age was associated with dislike, blame, and fear of fat. Men endorsed more dislike and blame, though women experienced more fear of fat. Higher parental education was associated with fear of fat and dislike. Primary care track students endorsed less dislike and blame.
In multivariate models (Table 4) several student characteristics predicted implicit bias, explicit bias, or attitudes. Implicit bias was associated with lower BMI; male sex; white or Hispanic race/ethnicity (compared to black race); being U.S.-born, and being in the lowest SES group. Explicit bias was associated with younger age; lower BMI; male sex; white, Hispanic, or East Asian race/ethnicity (compared to black race); higher SES; and intending to pursue a career in specialty care. In the sensitivity analysis of the adjusted association between race and feeling thermometer score, Hispanic ethnicity was not associated with explicit bias, relative to Black race. Dislike was associated with younger age, lower BMI; male sex; white, Hispanic, East Asian, or South Asian race/ethnicity (compared to black race); highest SES; and intending to pursue a career in specialty care. Belief that fat people lack willpower was associated with younger age, male sex; white, Hispanic, or East Asian race/ethnicity (compared to black race); and intending to choose a career in specialty care. Fear of becoming fat was associated with younger age; higher BMI; female sex; white, Hispanic, East Asian, or South Asian race/ethnicity (compared to black race); and intending to choose a career in specialty care.
Table 4. Multivariate Associations between Student and School Factors and Weight Bias/Attitudes (N=4732).
Table 4 shows the results of multivariate linear models predicting implicit and explicit bias measures. Beta coefficients, global p-values and p-values for each level of categorical variables are presented.
| Model 1: Implicit Bias | Model 2: Explicit Bias | Model 3: Dislike | Model 4: Blame | Model 5: Fear | |
|---|---|---|---|---|---|
|
| |||||
| Beta (p-value) | Beta (p-value) | Beta (p-value) | Beta (p-value) | Beta (p-value) | |
|
| |||||
| Age | −.001 (p=.86) | −.44 (p<.001) | −.01 (p=.04) | −.02 (p<.01) | −.04 (p<.001) |
|
| |||||
| BMI | −.01 (p<.001) | −.43 (p<.001) | −.03 (p<.001) | −.01 (p=.15) | .16 (p<.001) |
|
| |||||
| Sex | |||||
| Male | .06 (p=.001) | 1.57 (p = .01) | .23 (p<.001) | .58 (p<.001) | −1.14 (p<.001) |
| Female | ref | ref | ref | ref | ref |
| p-value for Wald F | .001 | .01 | <.001 | <.001 | <.001 |
|
| |||||
| Race/Ethnicity | |||||
| White | .11 (p < .01) | 7.47 (p<.001) | .54 (p<.001) | .58 (p<.001) | .93 (p<.001) |
| Hispanic | .13 (p <.01) | 4.25 (p = .02)* | .42 (p<.001) | .29 (p= <.01) | .95 (p<.001) |
| East Asian | .07 (p = .09) | 4.33 (p<.01) | .66 (p<.001) | .24 (p= <.01) | 1.00 (p<.001) |
| South Asian | .02 (p = .67) | 1.71 (p = .17) | .33 (p<.001) | .13 (p= .19) | 1.03 (p<.001) |
| Black | ref | ref | ref | ref | ref |
| p-value for Wald F | .001 | <.001 | p<.001 | p<.001 | <.001 |
|
| |||||
| Born in USA | |||||
| Yes | .07 (p < .01) | .76 (p = .35) | .05 (p=.41) | .04 (p= .60) | .04 (p=.40) |
| No | ref | ref | ref | ref | ref |
| p-value for Wald F | <.01 | .35 | .41 | .60 | .30 |
|
| |||||
| Parent’s Highest Degree | |||||
| Doctoral | −.06 (p = .03) | 2.73 (p<.01) | .11 (p=.04) | −.04 (p= .45) | .04 (p=.55) |
| Masters | −.003 (p = .90) | 2.44 (p = .02) | .13 (p=.05) | .02 (p= .69) | .10 (p=.19) |
| Bachelors | −.016 (p = .59) | .71 (p = .43) | .02 (p=.75) | .02 (p=.77) | .05 (p=.39) |
| Less than Bachelor | ref | ref | ref | ref | ref |
| p-value for Wald F | .02 | .<.01 | .046 | .58 | .49 |
|
| |||||
| Anticipated Specialty | |||||
| Specialty | .01 (p = .50) | 3.47 (p<.001) | .22 (p<.001) | .22 (p<.001) | .11 (p=.04) |
| Primary Care | ref | ref | ref | ref | ref |
| p-value for Wald F | .50 | <.001 | <.001 | <.001 | .04 |
Not significantly different than Black race (pt-test=.16) in sensitivity model of raw “obese people” thermometer scores.
Discussion
We measured the magnitude of explicit and implicit weight bias and the relationship between implicit weight bias, explicit weight bias, and explicit anti-fat attitudes, and identified the student characteristics that are associated with each type of attitude. The mean IAT score was .42, which is considered moderate bias against obese people; 59% of students displayed either moderate or strong implicit bias. This is consistent with attitudes observed in studies of healthcare providers,[30–32] though direct comparison is limited by the use of different measures in those studies. Implicit weight bias was more prevalent than previously reported in a sample of 3rd-year students from one medical school.[33] It is also comparable to the mean IAT score of .40 found among individuals who self-identified as MDs.[23]
The magnitude of implicit weight bias held by medical students is comparable to the magnitude of documented implicit anti-black bias held by healthcare providers and medical students. One study of medical students at a single institution found the mean race IAT score to be .32,[34] and studies of physicians’ implicit race bias have found mean D scores to range from .18 to .39.[1, 3, 35]
Consistent with prior research, [4, 5, 33] implicit and explicit bias were weakly correlated (r=.13). It has been observed that race bias in healthcare providers follows a pattern of high implicit bias and low explicit bias, which has been labeled aversive prejudice because feelings of racial bias are aversive to consciously egalitarian individuals.[36] By contrast, the distributions of implicit and explicit weight bias (Figure 2) suggest that explicit weight bias is more prevalent than explicit bias against racial minorities. The differences between the patterns of implicit and explicit bias for race and weight suggest that interventions to reduce race bias would need to be tailored to address the high prevalence of explicit bias as well as the high prevalence of implicit bias. Sixty-seven percent of students explicitly rated obese people less favorably than white people, and the mean explicit weight bias score was more than double the mean explicit bias score for lesbians, gays, poor people, or members of any race group (figure 3). Additionally, 16% agreed with the statement “I don’t like fat people very much.” Thirty percent moderately or strongly agreed with at least 1 item from the scale of blame for obesity; and 45% moderately or strongly agreed with at least 1 item measuring fear of fat.
This relatively high level of explicit weight bias may result from low internal or external pressure to appear unbiased against obese people. These data suggest that medical students, who in most cases hold egalitarian beliefs, believe it is acceptable to hold negative attitudes about obese patients. Indeed, obesity is an independent risk factor for chronic disease, so some medical students may blur the line between dislike for obesity (the disease which may contribute to poor patient outcomes) and obese patients. However, in one qualitative study of medical students, obese people were identified as the most common target of derogatory humor, [24] supporting the supposition that explicit negativity toward obese people is acceptable among healthcare providers in a way that race and other prejudices are not.
The significant minority of medical students (29.8%) who endorsed items in the blame/willpower scale represents a challenge for ensuring care quality for obese patients. Healthcare providers use less patient-centered verbal communication with patients they believe will not be adherent, and adherence to behavior change recommendations would likely require the willpower that many students believe is lacking. Thus, providers who believe that obese patients lack willpower may be less likely to discuss health behaviors such as physical activity, that lower chronic disease risk regardless of body size.[37, 38] To promote more equitable care for obese patients, medical schools might focus efforts to educate students on this topic.
We identified several factors that predicted implicit and explicit bias and anti-fat attitudes. Consistent with prior research,[23] lower BMI was associated with more negative implicit and explicit bias and dislike of fat people. Blame did not differ significantly across BMI, suggesting that obese students may blame themselves for their weight. Furthermore, greater BMI was associated with fear of fat, which may have implications for the body image and self-esteem of obese students.
With the exception of fear of fat, men exhibited more negative implicit and explicit attitudes than women. This is consistent with prior studies.[23, 33] Black students had the most positive implicit and explicit weight-related attitudes. Whites and Hispanics had greater implicit and explicit bias, and more negative explicit attitudes than blacks; although in sensitivity analysis, Hispanics did not have greater explicit bias than blacks. Due to these inconsistent findings, black-Hispanic differences in explicit bias should be interpreted with caution. East Asian students exhibited more explicit bias and stronger explicit anti-fat attitudes; and South Asian students endorsed more blame and fear of fat. These race differences may result from cultural differences in ideal body types that have been noted in prior research.[39] Independent of race, being U.S.-born predicted implicit bias, possibly reflecting U.S. cultural attitudes toward personal responsibility.[28] Students whose parents had advanced degrees had stronger explicit bias, whereas those whose parents had less than a college degree had greater implicit bias. Differences in explicit bias could be explained by class differences in the prevalence of obesity and subsequent familiarity and positive interactions with obese people. However, the marginally significant association between implicit bias and lower parental education is inconsistent with this interpretation. Additional research might examine the replicability of this effect and investigate different factors that may help account for it.
Students who planned to choose a primary care specialty endorsed less explicit bias, dislike, and blame than those on a track toward specialty careers. This finding may have implications for the quality of specialty care. On an absolute scale, primary care students also endorsed strong implicit and explicit anti-fat attitudes, which are significant because primary care providers have frequent contact with patients, and may address health behaviors and body weight. The U.S. Preventive Services Task force recommends that primary care providers screen for obesity at every contact. These frequent discussions of weight with biased individuals may lead to frequent stigmatizing experiences.
Limitations to the study include the potential for participation bias. However, we were able to attain a high response rate and a sample that resembled the population of matriculating students. Another limitation is our use of a difference score between attitudes toward obese people and whites to assess explicit weight bias. Though there are benefits of using this measure, race differences in attitudes toward whites complicate the interpretation of associations between student race and explicit attitudes. However, this study is the first to explore implicit and explicit bias and anti-fat attitudes in a national sample of medical students, and provides strong evidence that bias is prevalent in 1st year students.
The high level of implicit and explicit bias found in this sample underscores the need to develop and implement interventions early in medical school to reduce bias and limit its impact on patient care. Recent studies have found that providing students with information about genetic or environmental causes of obesity that are outside the control of the individual can reduce implicit and explicit weight bias. [30] Other promising research has demonstrated that providing information challenging the consensus of anti-fat attitudes can reduce explicit bias.[40] Because this kind of bias is currently socially acceptable, interventions might be modeled after strategies to improve attitudes toward other groups for which social norms generally allow the expression of bias (e.g., people with mental illness or people living with AIDS). Medical school curricula often include cultural competency instruction to reduce the impact of race bias and improve healthcare quality for members of minority race groups. Given the comparatively high level of implicit and explicit weight bias demonstrated here, similar efforts to reduce weight bias may be necessary inclusions in medical school curricula.
What is Known About the Subject
Weight bias is prevalent among health care providers, including physicians.
Moderate weight bias has been found in medical student samples at single schools.
Women and people with higher BMIs tend to have lower weight bias.
What This Study Adds
Weight bias prevalence estimates from a large national sample of 1st year medical students from 49 schools are presented
Explicit weight bias is stronger than explicit bias against blacks, Hispanics, 0ays, lesbians, and poor people; and implicit weight bias scores are similar to those reported for race bias
Less implicit and explicit bias observed among black students, female students, older students, and students with higher BMIs; less implicit bias demonstrated by students born outside the US, and less explicit bias demonstrated by students from lower SES backgrounds, and students intending to enter a primary care specialty.
Acknowledgments
SP, MvR, RP, and JD planned and carried out analyses for this manuscript. All authors were involved in interpreting findings, writing the paper, and had final approval.
Dr. Phelan is supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under award K01DK095924. Other support for this research was provided by the National Heart, Lung, and Blood Institute under award R01HL085631.
Footnotes
Conflicts of Interest
Drs. Phelan, Dovidio, Puhl, Burgess, Nelson, Yeazel, Perry, and van Ryn and Ms. Hardeman do not report any conflicts of interest.
Contributor Information
Sean M. Phelan, Division of Health Care Policy and Research, Mayo Clinic, Rochester, MN, USA.
John F. Dovidio, Department of Psychology, Yale University, New Haven, CT, USA.
Rebecca M. Puhl, Rudd Center for Food Policy and Obesity, Yale University, New Haven, CT, USA.
Diana J. Burgess, Center for Chronic Disease Outcomes Research, Minneapolis VAMC & Department of Medicine, University of Minnesota, Minneapolis, MN, USA.
David B. Nelson, Center for Chronic Disease Outcomes Research, Minneapolis VAMC & Department of Medicine, University of Minnesota, Minneapolis, MN, USA.
Mark W. Yeazel, Department of Family Medicine and Community Health, University of Minnesota, Minneapolis, MN, USA.
Rachel Hardeman, Division of Health Policy and Management, University of Minnesota, Minneapolis, MN, USA.
Sylvia Perry, Department of Psychology, Yale University, New Haven, CT, USA.
Michelle van Ryn, Division of Health Care Policy and Research, Mayo Clinic, Rochester, MN, USA.
References
- 1.Cooper L, et al. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. American Journal of Public Health. 2012;102(5):979–987. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Penner LA, et al. Aversive Racism and Medical Interactions with Black Patients: A Field Study. J Exp Soc Psychol. 2010;46(2):436–440. doi: 10.1016/j.jesp.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Green AR, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22(9):1231–8. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hofmann W, et al. A meta-analysis on the correlation between the implicit association test and explicit self-report measures. Personality and Social Psychology Bulletin. 2005;31(1):1369–1385. doi: 10.1177/0146167205275613. [DOI] [PubMed] [Google Scholar]
- 5.Greenwald AG, et al. Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97(1):17–41. doi: 10.1037/a0015575. [DOI] [PubMed] [Google Scholar]
- 6.Dovidio J, Kawakami K, Gaertner S. Implicit and explicit prejudice and interracial interaction. Journal of Personality and Social Psychology. 2002;82(1):62–68. doi: 10.1037//0022-3514.82.1.62. [DOI] [PubMed] [Google Scholar]
- 7.Budd GM, et al. Health care professionals’ attitudes about obesity: An integrative review. Appl Nurs Res. 2009;24(3):127–37. doi: 10.1016/j.apnr.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 8.Brown I. Nurses’ attitudes towards adult patients who are obese: literature review. J Adv Nurs. 2006;53(2):221–32. doi: 10.1111/j.1365-2648.2006.03718.x. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz MB, et al. Weight bias among health professionals specializing in obesity. Obes Res. 2003;11(9):1033–9. doi: 10.1038/oby.2003.142. [DOI] [PubMed] [Google Scholar]
- 10.Agell G, Rothblum ED. Effects of clients’ obesity and gender on the therapy judgments of psychologists. Professional Psychology, Research and Practice. 1991;22(3):223–229. [Google Scholar]
- 11.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring) 2009;17(5):941–64. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 12.Hebl MR, Xu J. Weighing the care: physicians’ reactions to the size of a patient. Int J Obes Relat Metab Disord. 2001;25(8):1246–52. doi: 10.1038/sj.ijo.0801681. [DOI] [PubMed] [Google Scholar]
- 13.Huizinga MM, et al. Physician respect for patients with obesity. J Gen Intern Med. 2009;24(11):1236–9. doi: 10.1007/s11606-009-1104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beach MC, et al. Are physicians’ attitudes of respect accurately perceived by patients and associated with more positive communication behaviors? Patient Educ Couns. 2006;62(3):347–54. doi: 10.1016/j.pec.2006.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Street RL, Jr, Gordon H, Haidet P. Physicians’ communication and perceptions of patients: is it how they look, how they talk, or is it just the doctor? Soc Sci Med. 2007;65(3):586–98. doi: 10.1016/j.socscimed.2007.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bertakis KD, Azari R. The impact of obesity on primary care visits. Obes Res. 2005;13(9):1615–23. doi: 10.1038/oby.2005.198. [DOI] [PubMed] [Google Scholar]
- 17.Gudzune KA, et al. Physicians build less rapport with obese patients. Obesity. 2013;21(10):2146–52. doi: 10.1002/oby.20384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Amy NK, et al. Barriers to routine gynecological cancer screening for White and African-American obese women. Int J Obes (Lond) 2006;30(1):147–55. doi: 10.1038/sj.ijo.0803105. [DOI] [PubMed] [Google Scholar]
- 19.Aldrich T, Hackley B. The impact of obesity on gynecologic cancer screening: an integrative literature review. J Midwifery Womens Health. 2010;55(4):344–56. doi: 10.1016/j.jmwh.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 20.Rosen AB, Schneider EC. Colorectal cancer screening disparities related to obesity and gender. J Gen Intern Med. 2004;19(4):332–8. doi: 10.1111/j.1525-1497.2004.30339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cohen SS, et al. Obesity and screening for breast, cervical, and colorectal cancer in women: a review. Cancer. 2008;112(9):1892–904. doi: 10.1002/cncr.23408. [DOI] [PubMed] [Google Scholar]
- 22.Drury CA, Louis M. Exploring the association between body weight, stigma of obesity, and health care avoidance. J Am Acad Nurse Pract. 2002;14(12):554–61. doi: 10.1111/j.1745-7599.2002.tb00089.x. [DOI] [PubMed] [Google Scholar]
- 23.Sabin JA, Marini M, Nosek BA. Implicit and Explicit Anti-Fat Bias among a Large Sample of Medical Doctors by BMI, Race/Ethnicity and Gender. PLoS One. 2012;7(11):e48448. doi: 10.1371/journal.pone.0048448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wear D, et al. Making fun of patients: Medical students’ perceptions and use of derogatory and cynical humor in clinical settings. Academic Medicine. 2006;81(5):454–462. doi: 10.1097/01.ACM.0000222277.21200.a1. [DOI] [PubMed] [Google Scholar]
- 25.Dyrbye LN, et al. The learning environment and medical student burnout: a multicentre study. Med Educ. 2009;43(3):274–82. doi: 10.1111/j.1365-2923.2008.03282.x. [DOI] [PubMed] [Google Scholar]
- 26.Alwin D. Feeling thermometers versus 7-point scales: Which are better? Sociological Methods and Research. 1997;25:318–340. [Google Scholar]
- 27.Crandall CS. Prejudice against fat people: ideology and self-interest. J Pers Soc Psychol. 1994;66(5):882–94. doi: 10.1037//0022-3514.66.5.882. [DOI] [PubMed] [Google Scholar]
- 28.Crandall CS, et al. An Attribution-Value model of prejudice: Anti-fat attitudes in six nations. Personality and Social Psychology Bulletin. 2001 Jan;27(1):30–37. 2001. [Google Scholar]
- 29.Miller DP, Jr, et al. Are Medical Students Aware of Their Anti-obesity Bias? Academic medicine : journal of the Association of American Medical Colleges. 2013;88(7):978–982. doi: 10.1097/ACM.0b013e318294f817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O’Brien KS, et al. Reducing anti-fat prejudice in preservice health students: a randomized trial. Obesity (Silver Spring) 2010;18(11):2138–44. doi: 10.1038/oby.2010.79. [DOI] [PubMed] [Google Scholar]
- 31.Schwartz M, et al. Weight bias among health professionals specializing in obesity. Obesity Research. 2003;11(9):1033–9. doi: 10.1038/oby.2003.142. [DOI] [PubMed] [Google Scholar]
- 32.Teachman BA, Brownell KD. Implicit anti-fat bias among health professionals: is anyone immune? Int J Obes Relat Metab Disord. 2001;25(10):1525–31. doi: 10.1038/sj.ijo.0801745. [DOI] [PubMed] [Google Scholar]
- 33.Miller DP, Jr, et al. Are Medical Students Aware of Their Anti-obesity Bias? Acad Med. 2013 doi: 10.1097/ACM.0b013e318294f817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haider AH, et al. Association of unconscious race and social class bias with vignette-based clinical assessments by medical students. JAMA. 2011;306(9):942–51. doi: 10.1001/jama.2011.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sabin J, et al. Physicians’ implicit and explicit attitudes about race by MD race, ethnicity, and gender. J Health Care Poor Underserved. 2009;20(3):896–913. doi: 10.1353/hpu.0.0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gaertner SL, Dovidio JF. The aversive form of racism. In: Dovidio JF, Gaertner SL, editors. Prejudice, Discrimination, and Racism. Academic Press; Orlando, FL: 1986. pp. 61–89. [Google Scholar]
- 37.Fogelholm M. Physical activity, fitness and fatness: relations to mortality, morbidity and disease risk factors. A systematic review. Obesity Reviews. 2010;11(3):202–21. doi: 10.1111/j.1467-789X.2009.00653.x. [DOI] [PubMed] [Google Scholar]
- 38.Weinstein AR, et al. Relationship of physical activity vs body mass index with type 2 diabetes in women. JAMA. 2004;292(10):1188–94. doi: 10.1001/jama.292.10.1188. [DOI] [PubMed] [Google Scholar]
- 39.Kemper KA, et al. Black and white females’ perceptions of ideal body size and social norms. Obes Res. 1994;2(2):117–26. doi: 10.1002/j.1550-8528.1994.tb00637.x. [DOI] [PubMed] [Google Scholar]
- 40.Puhl RM, Schwartz MB, Brownell KD. Impact of perceived consensus on stereotypes about obese people: A new approach for reducing bias. Health Psychology. 2005;24(5):517–525. doi: 10.1037/0278-6133.24.5.517. [DOI] [PubMed] [Google Scholar]