Abstract
A 74-year-old woman underwent replacement of the ascending aorta for acute type A aortic dissection. The patient suffered from bacteremia postoperatively and repeated computed tomography showed an increasing diameter of pseudoaneurysms at the site of the proximal anastomosis due to graft infection. Re-mechanical Bentall operation and arch replacement were therefore performed using a composite graft of a rifampicin-bonded gelatin-sealed 24-mm woven Dacron graft and a mechanical valve. The postoperative course was uneventful. We report the successful in situ reconstruction using the above-mentioned Dacron graft and describe the preparation of the rifampicin solution using a surfactant.
Keywords: prosthetic graft infection, rifampicin-bonded gelatin-sealed woven Dacron graft, rifampicin solution
Introduction
Prosthetic graft infection is one of the most life-threatening complications of vascular surgery. In situ replacement with a rifampicin-bonded graft has been performed after an initial report had been published in 1991.1) In particular, rifampicin is not completely water-soluble, which maintains its anti-infectivity; however, the preparation of the rifampicin solution is not yet standardized. We performed in-situ reconstruction with a rifampicin-bonded gelatin-sealed 24-mm woven Dacron graft for prosthetic graft infection and achieved promising results. We herein report the case and describe the preparation of the rifampicin solution.
Case Report
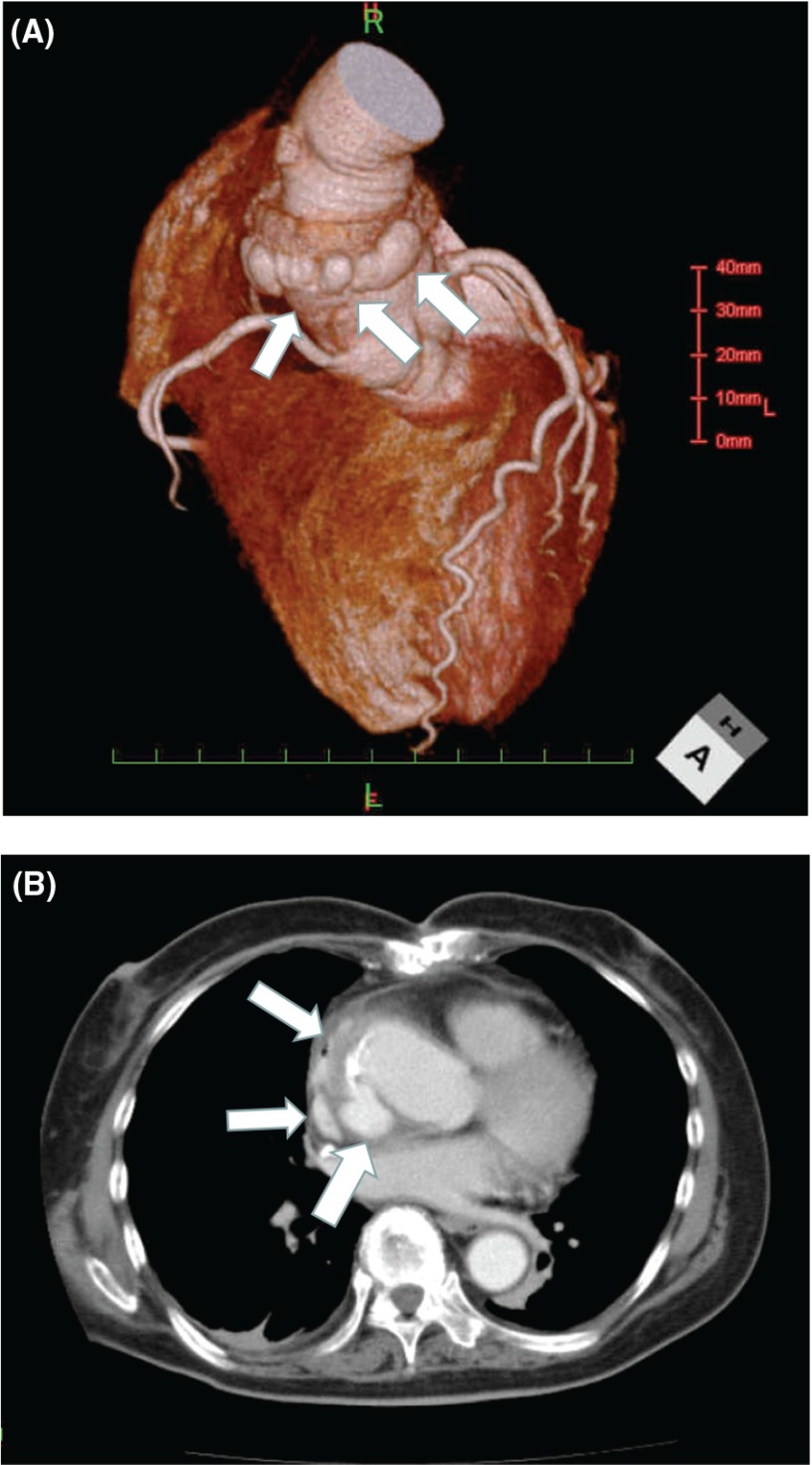
A 74-year-old woman underwent replacement of the ascending aorta using a 28-mm woven Dacron graft (J Graft Shield Neo; Junken Medical Co., Ltd., Chiba, Japan) for acute type A dissection because of continuous pain in spite of strict antihypertensive treatment and bed rest (Fig. 1). On postoperative day 10, the patient suffered from bacteremia caused by methicillin-sensitive Staphylococcus aureus (MSSA). Thus, we initiated cefazolin sodium infusion at 6 g/day and vacuum assisted closure therapy. Repeated computed tomography (CT) showed an increasing diameter of pseudoaneurysms at the site of the proximal anastomosis due to graft infection (Fig. 2A and 2B). During the deterioration of her physical condition, her body temperature, heart rate, and blood pressure were 38.6°C, 94 bpm, and 158/82 mmHg, respectively. Blood examination revealed maximum leukocyte and C-reactive protein values of 33700/mm3 and 32.8 mg/dL, respectively.
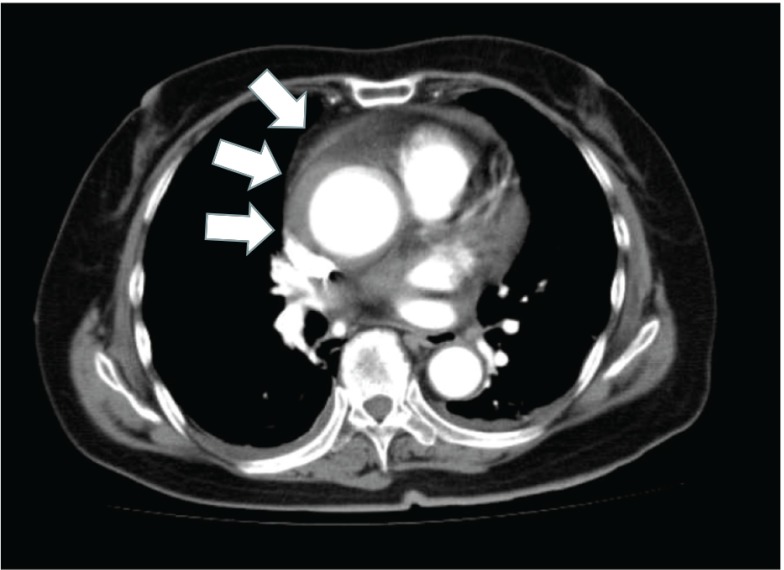
Fig. 1.
Initial contrast-enhanced computed tomography image showing thrombosed type A aortic dissection.
Fig. 2.
Preoperative systemic computed tomography angiography showing pseudoaneurysms surrounding the proximal anastomosis site (A) and one of the psedoaneurysms enhanced in the axial section (B).
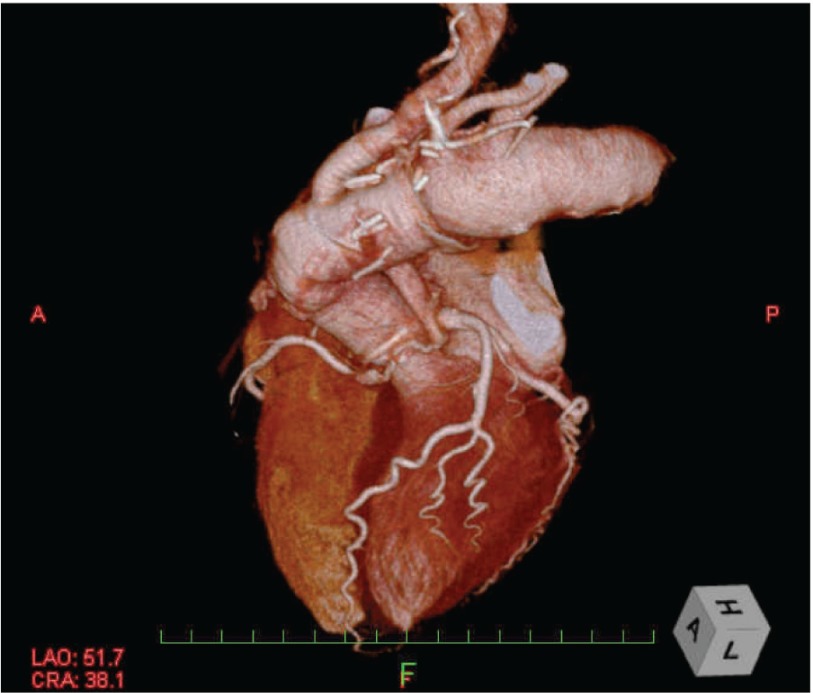
Re-sternotomy was performed and cardiopulmonary bypass was established through the femoral artery and two-staged venous cannula from the right atrium. Under circulatory arrest with selective cerebral perfusion at a rectal temperature of 25.0°C, the aortic root and arch were replaced. The composite graft of a rifampicin-bonded gelatin-sealed 24-mm woven Dacron graft (J Graft Shield Neo; Junken Medical Co., Ltd., Japan) and a 21-mm SJM Regent valve (St. Jude Medical, Inc., St. Paul, Minnesota, USA) were used. Postoperative CT angiography showed no pseudoaneurysm in the aortic root and complete resection of the lesion (Fig. 3).
Fig. 3.
Postoperative computed tomography angiography showing no pseudoaneurysm in the aortic root and complete resection of the lesion.
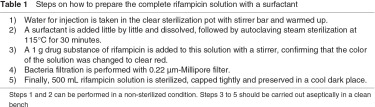
For the in-situ reconstruction, we prepared the rifampicin solution as follows. Water for injection was obtained from a clear sterilization pot with a stirrer bar and warmed up. Fifty grams of the surfactant Polysorbate 80 (Tween 80; NOF Corp., Tokyo, Japan) was added and dissolved, followed by autoclaving steam sterilization at 115°C for 30 min. A 1-gram drug substance of rifampicin was added to the solution with a stirrer, confirming that the color of the solution was changed to clear red. Bacterial filtration was performed with a 0.22-µm Millipore filter (Vented Millex-GS 0.22 µm; Merck Millipore, Darmstadt, Germany). Finally, 500 mL of the prepared rifampicin solution was sterilized, capped tightly, and preserved in a cool dark place (4°C) (Table 1).
Cefazolin sodium was administered intravenously at 6 g/day for 8 weeks postoperatively and then cephalexin was given orally (capsule form) at 1000 mg/day for chronic suppression. The patient was discharged with no major complication.
Discussion
Prosthetic graft infection is one of the most life-threatening complications of vascular surgery, the incidence of which ranges from less than 1% to 6% in published series.2–7) The infection is difficult to treat and is associated with high mortality and morbidity rates.
Several approaches to treat infected aortic prosthetic grafts have been reported using cryopreserved homografts,8) autologous veins for the abdomen,9) or omentum wrapping.10)
We performed in-situ re-Bentall operation in our case using a rifampicin-bonded gelatin-sealed 24-mm woven Dacron graft, which has been reported to be effective, and we anticipate that more institutions will be able to prepare the rifampicin solution in conjunction with the use of this graft in the near future.11,12) Rifampicin, which was originally developed for use in the oral form, has recently been used in the solution form for the therapy of various diseases. As rifampicin is only slightly soluble in water, rifampicin in this study was dissolved in water using a surfactant to increase its solubility and produce a sufficiently stable rifampicin solution.
It is difficult to prepare a cryopreserved homograft in an emergency situation. After the initial experimental report of the use of a rifampicin-bonded gelatin-sealed Dacron graft by Goëau-Brissonnière, et al.13) and the first clinical report of the use of a rifampicin-bonded graft by Strachen, et al.14) rifampicin has been used and shown to be an effective antibiotic for graft infection. Moreover, rifampicin can maintain its anti-infectivity for at least 3 days by binding with gelatin.15) It is highly essential to maintain anti-infectivity for several days when performing reoperation for an infected prosthetic graft. Furthermore, rifampicin is relatively water-insoluble and therefore it does not readily dissolve in the blood. Accordingly, we treated the graft infection caused by MSSA successfully by dissolving rifampicin completely using a surfactant and soaking the composite graft in the rifampicin solution for 30 min.
Recently, Uchida, et al.16) reported excellent results with the use of a rifampicin-bonded graft and omental pedicle grafting. They prepared rifampicin solution in a similar manner as ours. The differences in their procedure were that they used the rifampicin-bonded graft for mycotic aneurysms, not for postoperative graft infection, and that they performed omental pedicle grafting together with the in-situ replacement of rifampicin-bonded grafting.
In summary, in addition to the complete preparation of the rifampicin solution, determining the affinity between rifampicin and gelatin-sealed woven Dacron may contribute to the maintenance of the local drug concentration and play a critical role in the successful reoperation for an infected prosthetic graft. As we successfully treated only one patient this time using this method, a meticulous follow-up is mandatory and the accumulation of therapeutic experiences will be needed.
Acknowledgement
We are indebted to Associate Professor Edward F. Barroga (PhD) of the Department of International Medical Communications of Tokyo Medical University for his editorial review of the English manuscript.
Disclosure Statement
Yasunori Iida and other co-authors have no conflict of interest.
References
- Quick CR, Vassallo DJ, Colin JF, et al. Conservative treatment of major aortic graft infection. Eur J Vasc Surg 1990; 4: 63-7 [DOI] [PubMed] [Google Scholar]
- Hoffert PW, Gensler S, Haimovici H. Infection complicating arterial grafts: personal experience with 12 cases and review of the literature. Arch Surg 1965; 90: 427-35 [DOI] [PubMed] [Google Scholar]
- Szilagyi DE, Smith RF, Elliott JP, et al. Infection in arterial reconstruction with synthetic grafts. Ann Surg 1972; 176: 321-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenstern L. Postoperative jaundice. An approach to a diagnostic dilemma. Am J Surg 1974; 128: 255-61 [PubMed] [Google Scholar]
- Lorentzen JE, Nielsen OM, Arendrup H, et al. Vascular graft infection: an analysis of sixty-two graft infections in 2411 consecutively implanted synthetic vascular grafts. Surgery 1985; 98: 81-6 [PubMed] [Google Scholar]
- Earnshaw JJ. Infection after vascular reconstruction-hard graft for surgeons. Surg Infect 1991; 3: 4-6 [Google Scholar]
- O’Hara PJ, Hertzer NR, Beven EG, et al. Surgical anagement of infected abdominal aortic grafts: review of a 25-year experience. J Vasc Surg 1986; 3: 725-31 [PubMed] [Google Scholar]
- Vogt PR, Turina MI. Management of infected aortic grafts: development of less invasive surgery using cryopreserved homografts. Ann Thorac Surg 1999; 67: 1986-9; discussion 1997-8 [DOI] [PubMed] [Google Scholar]
- Lorentzen JE, Nielsen OM. Aortobifemoral bypass with autogenous saphenous vein in treatment of paninfected aortic bifurcation graft. J Vasc Surg 1986; 3: 666-8 [PubMed] [Google Scholar]
- Yamashiro S, Arakaki R, Kise Y, et al. Potential role of omental wrapping to prevent infection after treatment for infectious thoracic aortic aneurysms. Eur J Cardiothorac Surg 2013; 43: 1177-82 [DOI] [PubMed] [Google Scholar]
- Gupta AK, Bandyk DF, Johnson BL. In situ repair of mycotic abdominal aortic aneurysms with rifampin-bonded gelatin-impregnated Dacron grafts: a preliminary case report. J Vasc Surg 1996; 24: 472-6 [DOI] [PubMed] [Google Scholar]
- Hayes PD, Nasim A, London NJ, et al. In situ replacement of infected aortic grafts with rifampicin-bonded prostheses: the Leicester experience (1992 to 1998). J Vasc Surg 1999; 30: 92-8 [DOI] [PubMed] [Google Scholar]
- Goëau-Brissonnière O, Leport C, Bacourt F, et al. Prevention of vascular graft infection by rifampin bonding to a gelatin-sealed Dacron graft. Ann Vasc Surg 1991; 5: 408-12 [DOI] [PubMed] [Google Scholar]
- Strachan CJ, Newsom SW, Ashton TR. The clinical use of an antibiotic-bonded graft. Eur J Vasc Surg 1991; 5: 627-32 [DOI] [PubMed] [Google Scholar]
- Lachapelle K, Graham AM, Symes JF. Antibacterial activity, antibiotic retention, and infection resistance of a rifampin-impregnated gelatin-sealed Dacron graft. J Vasc Surg 1994; 19: 675-82 [DOI] [PubMed] [Google Scholar]
- Uchida N, Katayama A, Tamura K, et al. In situ replacement for mycotic aneurysms on the thoracic and abdominal aorta using rifampicin-bonded grafting and omental pedicle grafting. Ann Thorac Surg 2012; 93: 438-42 [DOI] [PubMed] [Google Scholar]