By 2030, it is estimated that there will be 439 million people in the world with diabetes. Diabetes is a major risk factor for the development of atherosclerotic peripheral arterial disease (PAD), which is typically caused by progressive narrowing of the arteries in the lower extremities (1). Traditionally, the treatment of PAD has focused on smoking cessation, exercise to promote collateral blood flow, and pharmaceutical vasodilatation to optimize microvascular reserve. Often, aggressive revascularization such as angioplasty and bypass grafting is required to salvage limbs and avoid major amputation in patients with critical limb ischemia. However, restenosis rates after endovascular intervention are high, and while recent advances in drug-eluting balloons and stents have promise, their impact on limb salvage remains unproven (2). Recently, therapeutic angiogenesis has been proposed to induce new blood vessel growth for the treatment or prevention of critical limb ischemia by pharmacological and molecular targeting with vascular endothelial growth factor (VEGF), fibroblastic growth factor, granulocyte colony–stimulating factors, granulocyte-macrophage colony–stimulating factors, angiogenic gene therapy, and endothelial progenitor cells (3). Although preclinical and early-stage clinical results are promising, the strategy of augmenting expression of a single factor has failed to deliver significant clinical improvement. Thus, there remains a clear need for better interventions to induce therapeutic angiogenesis in diabetes-related PAD.
One therapeutic strategy is to increase nitric oxide (NO) in order to stimulate angiogenesis in conditions such as ischemia–reperfusion injury, cerebral ischemia, kidney injury, coronary artery disease, and PAD (4). NO induces endothelial cell (EC) migration, proliferation, angiogenesis, and VEGF expression, which, in turn, can further increase NO by enhancing endothelial NO synthase (eNOS) activity (Fig. 1). Multiple signaling pathways within ECs may be affected in response to NO generation, including cyclic guanosine monophosphate/protein kinase G, mitogen-activated protein kinases, hypoxia-inducible factor 1, and heme oxygenase 1 (5,6). Therapeutic strategies to increase NO are limited by the fact that NO is an unstable gaseous molecule and often metabolized before it reaches target cells. Pharmacological treatment with nitrite, an oxidation product of NO, may offer an alternative therapeutic approach since nitrite is considered to be highly stable, but nitrite has limited intrinsic biological activity at physiological ranges of pH and oxygen tension (7). Very important, conditions such as tissue chronic ischemia or ischemia reperfusion are optimal for the reduction of nitrite to NO by hypoxia, low pH, deoxyhemoglobin, deoxymyoglobin, xanthine oxidoreductase (XOR), as well as aldehyde oxidase (8–10). Thus, nitrite reduction to NO may serve as a critical mechanism to maintain NO reservoirs during pathophysiological states to minimize tissue ischemia, dysfunction, and injury in cardiovascular diseases (Fig. 1).
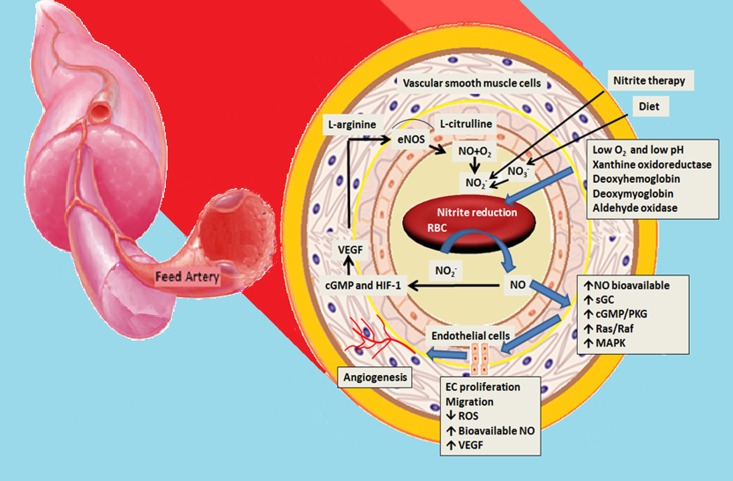
Figure 1.
Mechanisms of action for the NO2− in cardiovascular diseases. Under normal conditions, NO2− is fairly stable and available from conventional L-arginine/NOS pathway, NO2− therapy, and dietary consumption of NO3−/NO2− leading to salivary NO3− secretion and reduction to NO2− by commensal bacteria. However, during ischemia, low pH, and hypoxia, NO2− is reduced to NO via deoxyhemoglobin, deoxymyoglobin, xanthine oxidoreductase, myoglobin, and aldehyde oxidase. NO induces EC migration, proliferation, and angiogenesis by activating cGMP/PKG, Ras-Raf, and MAPK signaling pathways. NO activates HIF-1 and heme oxygenase 1 pathways to increase VEGF production, which can increase NO in turn by upregulating eNOS activity. NO2− therapy confers substantial benefit to cardiovascular disease. cGMP, cyclic guanosine monophosphate; HIF-1, hypoxia-inducible factor 1; MAPK, mitogen-activated protein kinases; NO3−, nitrate; NO2−, nitrite; PKG, protein kinase G; RBC, red blood cell; ROS, reactive oxygen species; sGC, solube guanylate cyclase.
In this issue, Bir et al. (11) investigated the therapeutic effect of sodium nitrite treatment on the ischemic revascularization by using permanent unilateral femoral artery ligation in a diabetic mice model. This study convincingly demonstrates that nitrite administered intraperitoneally, restored ischemic hind limb blood flow, decreased oxidative stress, and stimulated EC proliferation, migration, and angiogenesis with a NO/VEGF-dependent manner in aged diabetic mice. Administration of nitrite resulted in increased tissue nitrite bioavailability, as well as increased levels of S-nitrosothiol and S-nitrosoheme in the ischemic hind limb. Furthermore, the proangiogenic actions of sodium nitrite were abrogated when febuxostat, an XOR inhibitor, was administered and therefore provided evidence that these effects were reliant on XOR activity. This study further confirms the findings of these investigators in a previous study, which indicated that the nitrite anion acts as a novel prodrug, undergoing one electron reduction back to NO under tissue ischemia in normal mice (12) (Fig. 1).
Overall, the data are interesting and potentially translational, with some important caveats. First, nitrite is reduced to NO only under special conditions such as ischemia, hypoxia, and low pH. In this regard, Bir et al. did not compare the difference of NO, VEGF, EC, and angiogenesis in normal and ischemic hind limbs within the same diabetic mouse model. This approach would be necessary to address the concern as to whether nitrite is a highly selective therapy agent only in local ischemic revascularization without undesired consequences, such as hypotension, retinopathy, methemoglobinemia, and potential tumor angiogenesis. Second, nitrite and nitrate can be applied in different clinical situations although there were negative results with nitrate therapy in this study. Further, there are translational limitations related to the intraperitoneal route of administration of nitrite in the current study. An oral formulation of sodium nitrite would be optimal for translational therapy in patients. In this regard, bioactivation of dietary nitrate is carried out mainly by commensal bacteria in the gastrointestinal tract that express effective nitrate reductase enzymes. Indeed, recent research in animals and humans has confirmed the beneficial effects of dietary nitrate in metabolic syndrome, hypertension, coronary heart disease, kidney injury, and pulmonary diseases (13,14). Third, while this study found that XOR was an important player in the reduction of nitrite to NO and augmented ischemic limb blood flow, it did not explore the role of other factors such as heme-containing protein and aldehyde oxidase involved in conversion of nitrite to NO. Further, hyperuricemia is more common in obese, diabetic, hypertensive, and elderly patients (15) and the use of an XOR in these patients may alter the impact of therapy with sodium nitrite in diabetic patients with PAD.
Despite the noted limitations, Bir et al. (11) provide strong support for the notion that nitrite therapy effectively enhances beneficial ischemic tissue vascular remodeling in the setting of diabetes and aging. A well-controlled and well-designed clinical trial is needed to elucidate whether nitrite therapy could be as effective in patients with diabetes and PAD.
Article Information
Acknowledgments. The authors would like to thank Brenda Hunter for her editorial assistance.
Funding. J.R.S. has received funding from the National Institutes of Health (R01-HL-73101-01A and R01-HL-107910-01) and the Veterans Affairs Merit System (0018).
Duality of Interest. No potential conflicts of interest relevant to this article were report.
Footnotes
See accompanying original article, p. 270.
References
- 1.Albayati MA, Shearman CP. Peripheral arterial disease and bypass surgery in the diabetic lower limb. Med Clin North Am 2013;97:821–834 [DOI] [PubMed] [Google Scholar]
- 2.Conte MS. Diabetic revascularization: endovascular versus open bypass—do we have the answer? Semin Vasc Surg 2012;25:108–114 [DOI] [PubMed] [Google Scholar]
- 3.Raval Z, Losordo DW. Cell therapy of peripheral arterial disease: from experimental findings to clinical trials. Circ Res 2013;112:1288–1302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kevil CG, Kolluru GK, Pattillo CB, Giordano T. Inorganic nitrite therapy: historical perspective and future directions. Free Radic Biol Med 2011;51:576–593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kolluru GK, Shen X, Kevil CG. A tale of two gases: NO and H2S, foes or friends for life? Redox Biol 2013;1:313–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dulak J, Józkowicz A. Regulation of vascular endothelial growth factor synthesis by nitric oxide: facts and controversies. Antioxid Redox Signal 2003;5:123–132 [DOI] [PubMed] [Google Scholar]
- 7.Calvert JW, Lefer DJ. Myocardial protection by nitrite. Cardiovasc Res 2009;83:195–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shiva S, Rassaf T, Patel RP, Gladwin MT. The detection of the nitrite reductase and NO-generating properties of haemoglobin by mitochondrial inhibition. Cardiovasc Res 2011;89:566–573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cantu-Medellin N, Kelley EE. Xanthine oxidoreductase-catalyzed reduction of nitrite to nitric oxide: Insights regarding where, when and how. Nitric Oxide 2013;34:19–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pinder AG, Pittaway E, Morris K, James PE. Nitrite directly vasodilates hypoxic vasculature via nitric oxide-dependent and -independent pathways. Br J Pharmacol 2009;157:1523–1530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bir SC, Pattillo CB, Pardue S, et al. Nitrite anion therapy protects against chronic ischemic tissue injury in db/db diabetic mice in a NO/VEGF-dependent manner. Diabetes 2014;63:270–281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kumar D, Branch BG, Pattillo CB, et al. Chronic sodium nitrite therapy augments ischemia-induced angiogenesis and arteriogenesis. Proc Natl Acad Sci USA 2008;105:7540–7545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hendgen-Cotta UB, Luedike P, Totzeck M, et al. Dietary nitrate supplementation improves revascularization in chronic ischemia. Circulation 2012;126:1983–1992 [DOI] [PubMed] [Google Scholar]
- 14.Carlström M, Larsen FJ, Nyström T, et al. Dietary inorganic nitrate reverses features of metabolic syndrome in endothelial nitric oxide synthase-deficient mice. Proc Natl Acad Sci USA 2010;107:17716–17720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sowers JR. Diabetes mellitus and vascular disease. Hypertension 2013;61:943–947 [DOI] [PMC free article] [PubMed] [Google Scholar]