Abstract
OBJECTIVE
The study seeks to improve access for underserved patients via novel integration of Pedi-Flite (a critical care transport team) and to validate whether this safely enhances diabetes care and effectively expands the endocrine workforce.
RESEARCH DESIGN AND METHODS
The study retrospectively analyzed pager service use in a cohort of established diabetic patients (n = 979) after inception of Pedi-Flite support. Outcomes included incidence and severity of recurrent diabetic ketoacidosis (DKA) and cost savings generated from reduced referrals to the emergency department (ED) and on-call endocrinologist. We generated descriptive statistics to characterize the study population and ED visits for DKA and constructed logistic regression models to examine associations of pager use and likelihood of ED visitation and nonelective inpatient admission from an ED for DKA.
RESULTS
Pager users comprised 30% of the patient population. They were younger but had more established diabetes than nonusers. While pager users were 2.75 times more likely than nonusers to visit the ED for DKA (P < 0.0001), their visits were less likely to lead to inpatient admissions (odds ratio 0.58; P < 0.02). More than half (n = 587) of all calls to the pager were resolved without need for further referral. Estimates suggest that 439 ED visits and 115 admissions were avoided at a potential cost savings exceeding 760,000 USD.
CONCLUSIONS
Integration of a transport service provides a novel, cost-effective approach to reduce disparities in diabetes care. Advantages include scalability, applicability to other disease areas and settings, and low added costs. These findings enrich an emerging evidence base for telephonic care-management models supported by allied health personnel.
Introduction
No jurisdiction sustains an adequate pediatric endocrine workforce to meet the rising epidemics of pediatric diabetes, pediatric obesity, and attendant complications (1). In particular, the incidence of diabetic ketoacidosis (DKA) in the U.S. continues to increase more rapidly than the incidence of newly diagnosed diabetic patients (2). The relatively small population of pediatric subspecialists nationally is further challenged by uneven dispersion of these specialists relative to the populations to be served (1). Consequently, concern about the availability of comprehensive care for diabetic youth has driven development of novel health care delivery models for this growing population.
Generally accepted standards of diabetes care endorse health care professionals using detailed algorithms—under physician supervision—to assist patients with outpatient diabetes management (3). Several health information technology (HIT) tools have emerged to support such models. HIT applied to diabetes care has included online patient portals (4), telephone support/follow-up (5,6), and mobile phone support (7), as well as traditional telemedicine based in schools (8,9) or clinics (10). With the exception of one telephone follow-up study (5), use of HIT improved outcomes as determined by adherence (6), improved hemoglobin A1c (HbA1c) (4,10), reduced rates of DKA (7), and reduced visits to the hospital or emergency department (ED) (8,9).
We hypothesized that application of allied health personnel could significantly improve access to care in a cost-effective manner, promote continuity of care from prehospital to inpatient settings, and more effectively sustain the standard of care for pediatric diabetes self-management. The aim of this study was to determine whether use of a telephone-based, self-management support system could reduce 1) endocrinologist call burden, 2) ED visits, and 3) hospital admission rates for DKA in patients with established diabetes. The current report describes the novel synthesis of telephonic technology and allied health personnel to provide real-time, 24/7 support for pediatric diabetes self-management.
Research Design and Methods
Study Design and Setting
This retrospective study analyzed diabetes pager service use in a cohort of pediatric patients with their diabetes care established under the pediatric endocrine faculty practice for University of Tennessee Health Science Center at Memphis. To be included in the analysis, patients had to be continuously enrolled for at least 2 years during the period after implementation of a dedicated diabetes service pager (August 2009–December 2012). Continuous enrollment was defined by two or more visits (in 1 year or across consecutive years) to the clinic during the study period. Patients receiving care in other practices were excluded. The study was conducted at a tertiary care, freestanding children’s hospital. This study was approved by the joint institutional review board for University of Tennessee Health Science Center and Methodist/Le Bonheur Healthcare System (protocol no. 10-00947-XP).
Personnel and Protocols
Pedi-Flite is a pediatric critical care transport team that provides regional air and ground medical transport and coordinates emergency response services for the Mid-South through an onsite, 24-h transfer center. Staff members are certified emergency medical personnel, and all hold a minimum national certification at Emergency Medical Technician (EMT)-IV. During 2008, the pediatric endocrine and Pedi-Flite directors of University of Tennessee Health Science Center and Le Bonheur Children’s Hospital collaborated to devise a novel approach to manage after-hours calls to a public pager dedicated to the diabetes service. This approach has applied six protocols for transfer center staff to address common diabetes-management issues: sick patient, insulin pump management, wrong insulin dose, blood glucose level correction, prescription refill, or other issues. The approach was approved during August 2008, and a schematic of the decision tree matrix is provided online (Supplementary Fig. 1). Our pediatric diabetes program has long been recognized by the American Diabetes Association. An American Diabetes Association–certified diabetes educator trained all transfer center staff on pediatric diabetes management and protocol use, with periodic refresher training and new-hire training provided upon request.
Software supporting the Pedi-Flite Transfer Center has been using the Visual Studio .NET platform on an SQL server for data storage back end. The system has allowed clinical staff to listen to a caller, whose needs drive the protocol(s). Advice provided telephonically has been strictly managed according to the protocols, driven from the computer system and designed to ensure patient safety. For example, if a caretaker erroneously reports a total daily insulin dose of 1,000 units for a 3-kg diabetic patient, the computer would deem that dose out of range and recommend dosing based on weight (instead of the reported total daily dose). The system has been managing safety measures (including drug calculations and related math) and generating a script for the user to read back to the caller. The system resembles modern enhanced 911 (e-911) systems; however, the complexity of the patient issues and complexity of the instructions have often been more advanced.
Diabetes Service Pager Intervention
After initial beta testing by the service directors and Pedi-Flite staff and development of training materials for patients and their families, the diabetes pager was activated during August 2009. Upon pager activation, patients received information and instructions on pager use during all clinic and inpatient visits. The pager has routed inbound calls from patients or caregivers to the Transfer Center dispatcher, an EMT of Pedi-Flite. Information provided by the caller triggered the dispatcher to follow one of six decision trees. If the issue could not be resolved, the protocols have been directing the dispatcher to connect the caller to the endocrinologist on call, to refer the patient to the closest ED, or to advise follow-up in the endocrine clinic within 24 h. Each call lasted ~20 min. All calls have been digitally recorded for quality assurance. Transfer center staff have been monitoring the pager daily to ensure proper operation in order to screen for and quickly resolve potential equipment malfunctions. Finally, a parent or the patient’s legally authorized representative typically calls this pager. Pedi-Flite staff have been trained to request direct conversation with the parent or legally authorized representative whenever a minor calls, and the protocol includes a verification prompt for this action.
Outcomes of Interest
The primary outcome of interest was incidence of recurrent DKA for patients with established type 1 or type 2 diabetes. We used ICD-9 diagnostic codes to identify ED and inpatient visits with a DKA diagnosis (i.e., 250.1x). Visits associated with initial diabetes diagnosis were excluded, since those families had not yet been trained on use of the diabetes pager or established to our practice. We also excluded visits occurring during the honeymoon period, defined within 1 year of diagnosis per Greenbaum et al. (11). Secondary outcomes included cost savings related to potential avoidance of self-referred ED visits, reduced inpatient days, and reduced use of the endocrinologist on call.
Calls that did not lead to referrals for the ED, clinic, or endocrinologist on call were deemed to have been resolved. The number of resolved calls was multiplied by the average call time (20 min) and again by endocrinologist wage rate per minute (1.09 USD; sensitivity analysis: 0.99–1.21 USD) to estimate the cost savings for reduced on-call burden. Wage rate per minute was calculated by dividing the annual salary estimate by 124,800 min (equivalent to 2,080 work hours annually). Call records were extracted from the Transfer Center database. Estimate of a pediatric endocrinologist’s salary was sourced from the American Association of Medical Colleges (median 135,925 USD [range 123,500–151,218]).
We calculated the number of ED visits potentially avoided by pager use by multiplying the number of calls (less those referred to an ED) by 46%. This estimate, based on the method reported by Kempe et al. (12), reflects the proportion of parents who would have taken their child to the ED or urgent clinic in the absence of an after-hours call center service. The number of potentially avoided visits was then multiplied by the average cost for an ED visit for DKA (1,073 USD), derived from Javor et al. (13), to calculate cost savings from reduced visits. Finally, we multiplied our hospital’s average daily charge (4,695 USD) for ward admission of uncomplicated DKA by the average difference in inpatient length of stay for pager users and nonusers. Cost estimates are reported in 2013 USD.
Independent Variables of Interest
The primary independent variable of interest was pager use, defined as any call to the pager during the study period. We also calculated the total number of calls made to the pager as an alternate measure of exposure. Age, sex, race, ethnicity, disease duration, previous DKA episodes, patient-years in the clinic, and diabetes type covariates were included in analysis.
Data Analysis
We generated descriptive statistics to characterize the study population and ED visits for DKA. χ2 and t tests for discrete and continuous variables, respectively, were used to test for differences by pager use. After controlling for group differences and other confounders, we constructed multivariable logistic regression models to examine associations of pager use and likelihood of either ED visitation for DKA in the postimplementation period or nonelective inpatient admission from an ED. We summarized pager call use and outcomes using frequencies of call volume, protocol use, and patient disposition after the Transfer Center encounter. We calculated cost savings for potentially avoided self-referral to ED, reduced inpatient days, and reduced on-call burden using estimates from institutional and external sources.
Results
Cohort Characteristics
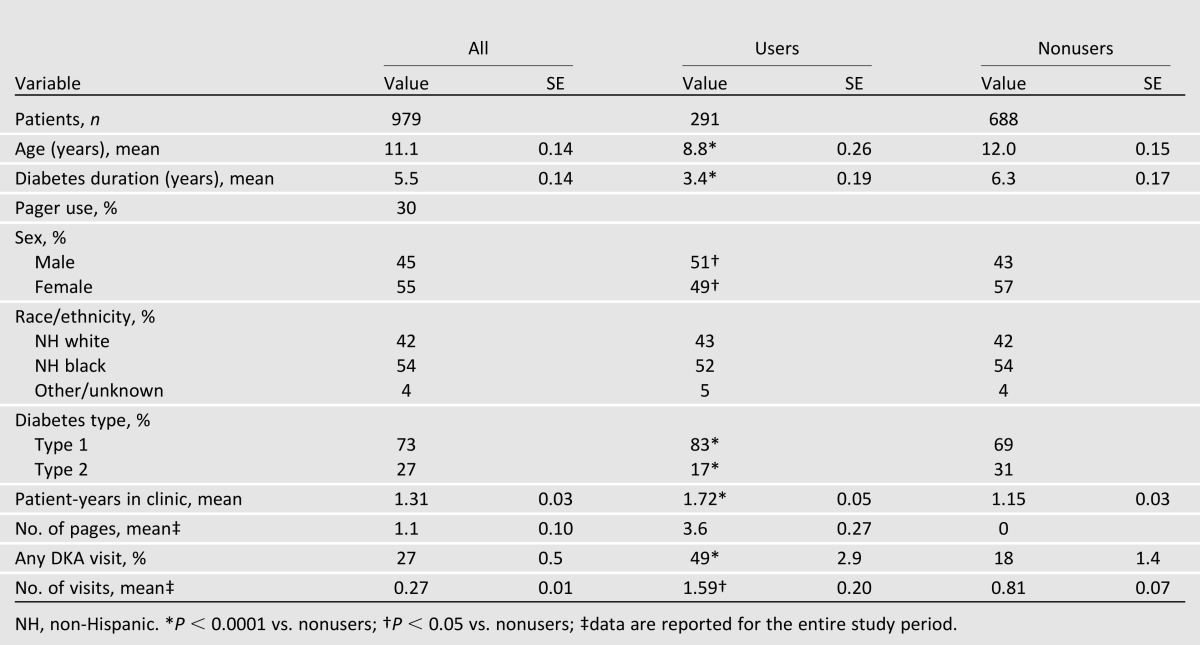
Table 1 provides a description of the study population and distinguishing characteristics of users and nonusers of the pager system. During the study period, the practice encountered 979 active diabetic patients. Of these, 30% were pager users. Pager users were younger, were more likely male, and had shorter disease duration but were more established in this practice. A larger proportion of pager users had type 1 diabetes, as expected, since all of those patients were using insulin. Both users and nonusers displayed similar racial/ethnic composition.
Table 1.
Pediatric endocrine clinic population characteristics, total and by pager use, 2009–2012
DKA Encounters and Inpatient Admissions
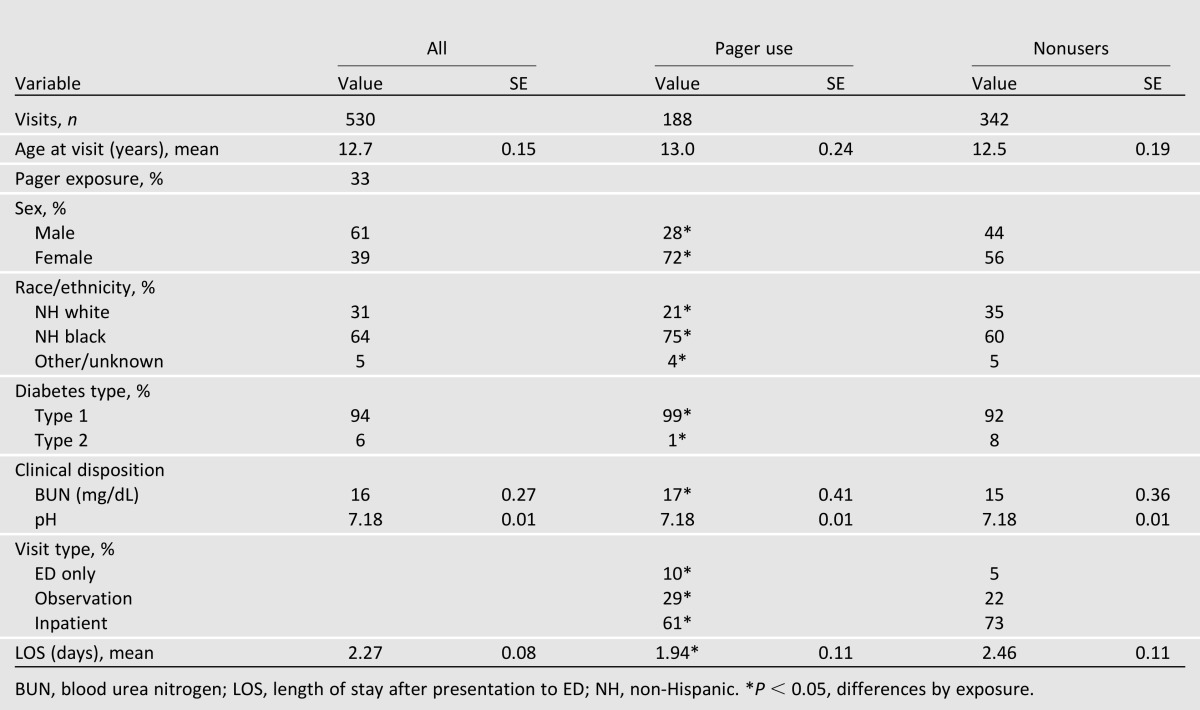
Table 2 describes ED visits for DKA by pager exposure during the study period. Clinic patients made 530 DKA-related ED visits over the study period; one-third of these were among pager users. ED visits associated with pager use had higher average blood urea nitrogen levels upon presentation to ED. Inpatient stays were, on average, 0.52 day shorter for pager users. After controlling for covariates by multivariable logistic regression, pager use was significantly associated with 2.75 times higher odds of ED visitation for DKA (P < 0.0001 vs. nonusers). Substitution of calls (as the alternate exposure variable) generated similar findings. However, ED visits for DKA among clinic patients with previous pager use were less likely to lead to inpatient admission than ED visits among nonusers (point estimate 0.58; P < 0.02 vs. nonusers). After controlling for covariates, the odds of inpatient admission for DKA from the ED were significantly lower by >40% among pager users (P < 0.02) and also significantly lower for older patients (P = 0.0002), those with shorter diabetes duration (P = 0.0005), or those with higher pH levels at presentation to ED (P < 0.0001).
Table 2.
Characteristics of DKA-related ED encounters at Le Bonheur Children’s Hospital, 2009–2012
Pager Use and Cost Outcomes
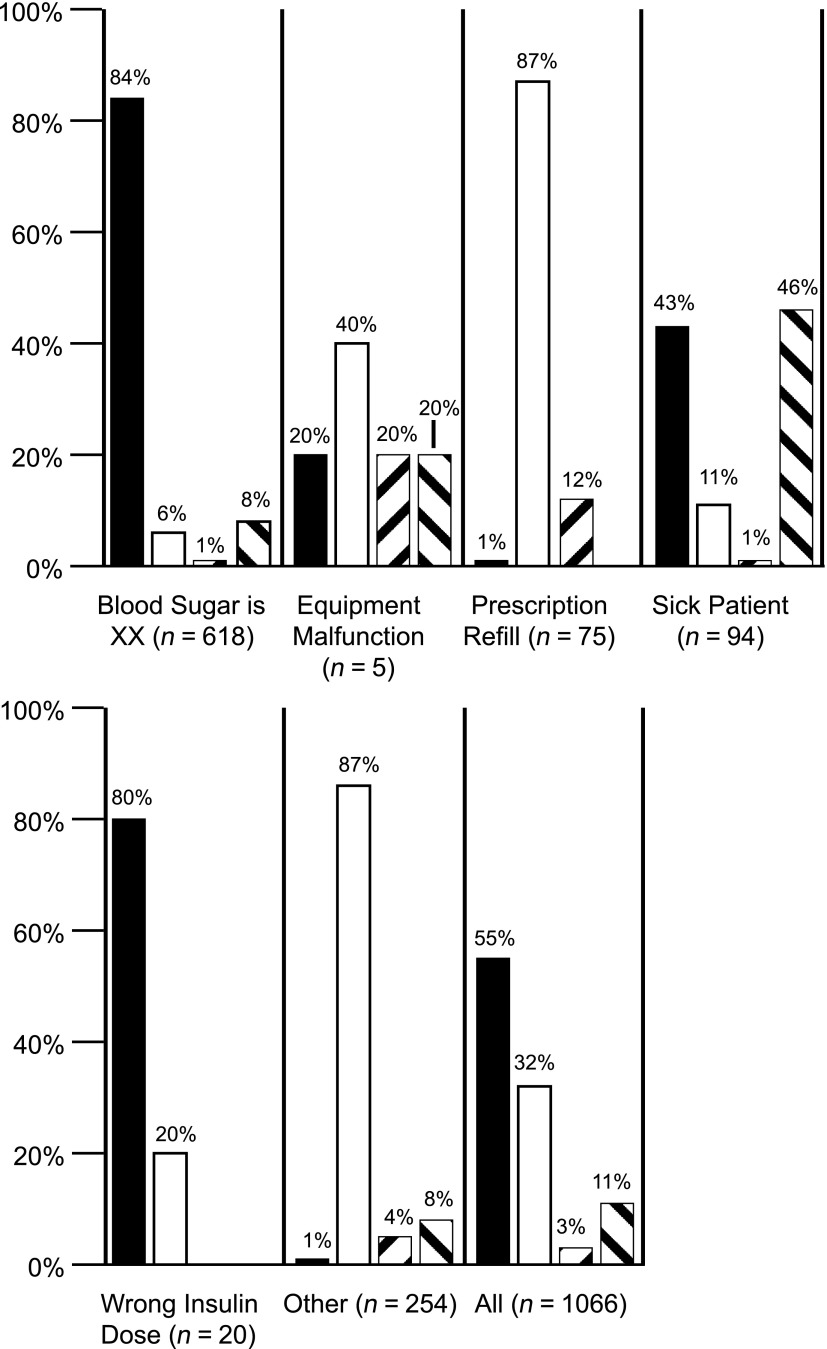
During the study period, Pedi-Flite personnel responded to 1,066 calls from 291 patients (or their parents). These calls were more frequent among more established (versus new‐onset) patients and particularly for those on insulin. Figure 1 summarizes the service use characteristics. More than half of all calls to the pager were resolved without further referral to the endocrinologist on call, clinic, or ED. Pedi-Flite staff were most effective at addressing routine blood glucose abnormalities and insulin-dosing issues. An estimated 439 ED visits were potentially avoided owing to issue resolution. Cost savings from potentially avoided ED self-referral and reduced on-call burden were, respectively, 471,047 and 12,840 USD (range 11,662–14,254). Further, ∼59 inpatient days (115 inpatient admissions × 0.52 days) were averted at a cost savings of 277,005 USD. Total cost savings exceeded 760,000 USD.
Figure 1.
Outcomes of pager call by protocol. Black bar, resolved; white bar, refer to endocrinologist; upward diagonal bar, refer to clinic; downward diagonal bar, refer to ED.
Conclusions
To our knowledge, this is the first report of the systematic application of allied health personnel using detailed algorithms to provide self-management support for diabetes. As evidenced in literature, the ability to make independent treatment decisions in real-time is a critical component of successful care-management models (14). Nurses and pharmacists have traditionally been used as alternative care providers (15). Here, Transfer Center personnel have effectively been resolving common diabetes-management issues that would otherwise have prompted ED, inpatient, or physician encounters. Further, there were no additional costs associated with use of existing transfer center staff, given the low daily call volume to the pager (∼1 call per day). Such feasibility has important implications for extending scope of practice to deliver appropriate and timely care to diabetic patients. This novel approach validates a cost-effective model to expand access to care, thereby reducing health care disparities.
The results confirmed the hypotheses that this model can significantly improve access to care in a cost-effective manner, promote continuity of care from prehospital to inpatient settings, and more effectively sustain the standard of care for pediatric diabetes self-management. Unlike some studies (7–9), our analysis did not exhibit reduced DKA admissions among pager users. However, this study revealed other important findings. Pager use was associated with lower clinical severity upon presentation to the ED and, therefore, reduced likelihood to result in inpatient admission. Also, patients at high risk for DKA (a potentially mortal complication) frequently used the pager service, an indication that it is reaching the patients for whom improved outcomes and access are most needed (16).
Our system carries distinct advantages of scalability, adaptation, and diffusion into other disease areas and care settings. The system provides easier, immediate access to self-care assistance for underserved populations by leveraging existing infrastructure, addressing multiple issues with the patient at home, and educating the patient on diabetes care. Simultaneously, this system improves glycemic control (through timely adjustment of insulin dose and correction of blood glucose level) as well as avoiding complications through improvement of metabolic control. The system is qualified as the work is carried out by certified personnel with a positive feedback mechanism that generates a script for the EMT to read back to the caller. We elected to implement a pager (rather than a hard line) owing to major moves of personnel and equipment associated with construction of our new children’s hospital during 2008–2010. So long as the number does not change, a hard line may be more reliable than a pager for such systems in the future.
A major strength of our study is that it involved a large pediatric diabetes population (n = 979), with a high proportion of minority and underserved patients. Similar studies used smaller cohorts. Also, support was provided in real-time by a dedicated, well-trained team. In comparison with other technologies (e.g., web portals or automated telephone systems), this approach has allowed for rapid interactive response.
Despite these strengths, limitations do exist. First, the quasi-experimental study design is subject to selection bias owing to nonrandom assignment to groups. Also, pager users account for a small proportion of the clinic population (291 of 979). We could not quantify patient use of other decision supports, such as the general on-call line during regular working hours and encounters at other EDs. The analysis would have been strengthened by knowledge of certain laboratory values (HbA1c and sodium bicarbonate upon presentation, which were not clinically indicated in all patients) and of caller feedback to enhance outcomes evaluation. This study could not estimate additional—and potentially large—cost savings for families related to reduced absenteeism (from work or school) and reduced commuting time between their homes and the closest ED.
Telephonic technology continues to be widely adapted for health care settings. Geographic barriers to pediatric diabetes care persist for minority populations. However, increased use of Internet and mobile technologies among African American and Hispanic populations make HIT applications more ideal than existing infrastructures to reduce disparities in care (17). Future studies are warranted to build the emerging evidence base for telephonic care management models supported by allied health personnel. New care delivery models emphasize greater use of allied care providers to enhance continuity of care for patients with chronic diseases.
Supplementary Material
Funding.
B.E.F. gratefully acknowledges research support from the University of Tennessee College of Pharmacy. R.J.F. gratefully acknowledges research support of Le Bonheur Foundation (Memphis, TN) and discloses unrelated research support from National Institutes of Health (NIH) R21 HD059292, NIH U01 DK085465, JDRF 1-2011-597, and Gabrielle’s Angel Foundation.
Duality of Interest. R.J.F. also discloses unrelated research support from MacroGenics, Eli Lilly & Co., Bristol-Myers Squibb, Novo Nordisk A/S, Ipsen, Diamyd Therapeutics AB, Pfizer, Tolerx, GlaxoSmithKline, and Takeda. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. B.E.F. researched data, contributed to discussion, and wrote the manuscript. S.C.C. authored software protocols, contributed to discussion, and reviewed and edited the manuscript. R.S. obtained institutional review board approval, contributed to discussion, and reviewed and edited the manuscript. M.M.A. inspired the hypothesis, contributed to discussion, and reviewed and edited the manuscript. D.T.M. researched data, contributed to discussion, and reviewed and edited the manuscript. R.J.F. conceived the hypothesis and study, authored treatment protocols, researched data, contributed to discussion, and wrote and edited the manuscript. R.J.F. is the guarantor of this work and, as such, had full access to all data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented in abstract form at the National Institutes of Health Network of Minority Research Investigators 11th Annual Workshop, Bethesda, Maryland, 18–19 April 2013, and at the 95th Annual Meeting and Expo of The Endocrine Society, San Francisco, California, 15–18 June 2013.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc13-1041/-/DC1.
A slide set summarizing this article is available online.
References
- 1.Lee JM, Davis MM, Menon RK, Freed GL. Geographic distribution of childhood diabetes and obesity relative to the supply of pediatric endocrinologists in the United States. J Pediatr 2008;152:331–336 [DOI] [PubMed] [Google Scholar]
- 2.Nyenwe E, Loganathan R, Blum S, et al. Admissions for diabetic ketoacidosis in ethnic minority groups in a city hospital. Metabolism 2007;56:172–178 [DOI] [PubMed] [Google Scholar]
- 3.American Diabetes Association Standards of medical care in diabetes—2012. Diabetes Care 2012;35(Suppl. 1):S11–S63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pinsker JE, Nguyen C, Young S, Fredericks GJ, Chan D. A pilot project for improving paediatric diabetes outcomes using a website: the Pediatric Diabetes Education Portal. J Telemed Telecare 2011;17:226–230 [DOI] [PubMed] [Google Scholar]
- 5.Nunn E, King B, Smart C, Anderson D. A randomized controlled trial of telephone calls to young patients with poorly controlled type 1 diabetes. Pediatr Diabetes 2006;7:254–259 [DOI] [PubMed] [Google Scholar]
- 6.Howe CJ, Jawad AF, Tuttle AK, et al. Education and telephone case management for children with type 1 diabetes: a randomized controlled trial. J Pediatr Nurs 2005;20:83–95 [DOI] [PubMed] [Google Scholar]
- 7.Farrell K, Holmes-Walker DJ. Mobile phone support is associated with reduced ketoacidosis in young adults. Diabet Med 2011;28:1001–1004 [DOI] [PubMed] [Google Scholar]
- 8.Izquierdo R, Morin PC, Bratt K, et al. School-centered telemedicine for children with type 1 diabetes mellitus. J Pediatr 2009;155:374–379 [DOI] [PubMed] [Google Scholar]
- 9.Malasanos TH, Burlingame JB, Youngblade L, Patel BD, Muir AB. Improved access to subspecialist diabetes care by telemedicine: cost savings and care measures in the first two years of the FITE diabetes project. J Telemed Telecare 2005;11(Suppl. 1):74–76 [DOI] [PubMed] [Google Scholar]
- 10.d’Annunzio G, Bellazzi R, Larizza C, et al. Telemedicine in the management of young patients with type 1 diabetes mellitus: a follow-up study. Acta Biomed 2003;74(Suppl. 1):49–55 [PubMed] [Google Scholar]
- 11.Greenbaum CJ, Beam CA, Boulware D, et al. Type 1 Diabetes TrialNet Study Group Fall in C-peptide during first 2 years from diagnosis: evidence of at least two distinct phases from composite Type 1 Diabetes TrialNet data. Diabetes 2012;61:2066–2073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kempe A, Luberti A, Belman S, et al. Outcomes associated with pediatric after-hours care by call centers: a multicenter study. Ambul Pediatr 2003;3:211–217 [DOI] [PubMed] [Google Scholar]
- 13.Javor KA, Kotsanos JG, McDonald RC, Baron AD, Kesterson JG, Tierney WM. Diabetic ketoacidosis charges relative to medical charges of adult patients with type 1 diabetes. Diabetes Care 1997;20:349–354 [DOI] [PubMed] [Google Scholar]
- 14.Davidson MB. How our current medical care system fails people with diabetes: lack of timely, appropriate clinical decisions. Diabetes Care 2009;32:370–372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davidson MB. The effectiveness of nurse- and pharmacist-directed care in diabetes disease management: a narrative review. Curr Diabetes Rev 2007;3:280–286 [DOI] [PubMed] [Google Scholar]
- 16.Rewers A. Current concepts and controversies in prevention and treatment of diabetic ketoacidosis in children. Curr Diab Rep 2012;12:524–532 [DOI] [PubMed] [Google Scholar]
- 17.NORC. Understanding the impact of health IT in underserved communities and those with health disparities [internet], 2013. Available from http://www.healthit.gov/sites/default/files/hit_disparities_report_050713.pdf Accessed 19 July 2013
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.