Abstract
BP variability (BPV) is an important predictor of outcomes in the general population, but its association with clinical outcomes in hemodialysis patients is not clear. We identified 11,291 patients starting dialysis in 2003–2008 and followed them through December 31, 2008 (median=22 months). Predialysis systolic BPV was assessed over monthly intervals. Outcomes included factors associated with BPV, mortality (all-cause and cardiovascular), and first cardiovascular event (cardiovascular death or hospitalization). Patients' mean age was 62 years, 55% of patients were men, and 58% of patients were white. Modifiable factors associated with higher BPV included obesity, higher calcium–phosphate product levels, and lower hemoglobin concentration; factors associated with lower BPV included greater fluid removal, achievement of prescribed dry weight during dialysis, higher hemoglobin concentration, and antihypertensive regimens without β-blockers or renin-angiotensin system blocking agents. In total, 3200 deaths occurred, including 1592 cardiovascular deaths. After adjustment for demographics, comorbidities, and clinical factors, higher predialysis BPV was associated with increased risk of all-cause mortality (hazard ratio [HR], 1.18; 95% confidence interval [95% CI] per 1 SD increase in BPV, 1.13 to 1.22), cardiovascular mortality (HR, 1.18; 95% CI, 1.12 to 1.24), and first cardiovascular event (HR, 1.11; 95% CI, 1.07 to 1.15). Results were similar when BPV was categorized in tertiles and patients were stratified by baseline systolic BP. In summary, predialysis systolic BPV is an important, potentially modifiable risk factor for death and cardiovascular outcomes in incident hemodialysis patients. Studies of BP management in dialysis patients should focus on both absolute BP and BPV.
Hypertension is highly prevalent in hemodialysis patients, occurring in over 90% of patients, but optimal strategies for management of hypertension in these patients remain unclear.1–4 A great majority of prior studies have focused on the association between patients’ mean predialysis BP levels and outcomes5–9; however, nearly all patients receiving dialysis also experience fluctuations in their BP (referred to here as BP variability [BPV]). BPV can be seen with different BP components, including systolic BP, diastolic BP, and pulse pressure, as well as predialysis, intradialytic, and postdialysis BPs. The factors associated with intradialytic BPV have recently been described,10 but the factors associated with predialysis BPV and its association with clinical outcomes are not well understood.
BPV reflects the disruption of BP homeostasis. It can result from both micro- and macrovascular disease, resulting in greater susceptibility to BP fluctuations in response to environmental stimuli.11,12 In hypertensive patients not on dialysis, CKD is associated with higher BPV, and BPV has been associated with higher risk of vascular events, such as stroke and myocardial infarction.13 Patients on hemodialysis are particularly prone to increased BPV because of a high prevalence of vascular disease combined with unique dialysis-related factors, such as stress, volume shifts, unusual antihypertensive medication schedules, and dialyzability of antihypertensive medications.2,10
Although recent studies have begun to show an association between BPV and mortality in patients on hemodialysis, many studies have not accounted for factors that can influence BPV, such as patients’ dialysis volume management or BP medication regimens.14 Thus, they have had limited ability to make causal links between BPV and patient outcomes. If BPV is indeed associated with greater mortality among hemodialysis patients (who already have extremely poor survival rates),15 studies better elucidating factors that decrease BPV could aid efforts to reduce excess mortality.
Predialysis systolic BP is generally used to make clinical decisions regarding management of hypertension in hemodialysis patients. Systolic BP is also the major contributor to pulse pressure. We therefore decided to assess the factors associated with predialysis systolic BPV and quantified the association of BPV with morbidity and mortality in a cohort of 11,291 incident hemodialysis patients.
Results
BPV Metric
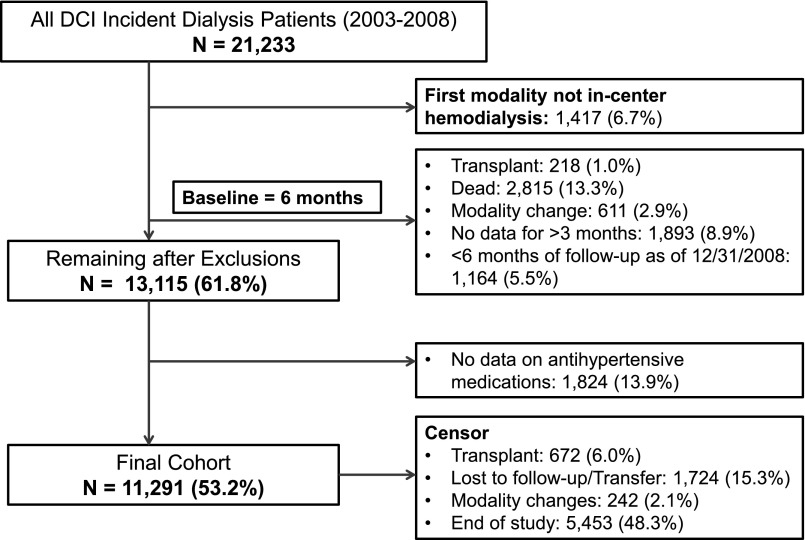
At baseline, the mean (SD) of the BPV metric was 0.115 (0.03). Figure 1 illustrates the clinical interpretation of the BPV metric. It shows that, for individuals with predialysis systolic BP of 100 mmHg (Figure 1A), individuals with a median (50th percentile) BPV value of 0.111 experienced systolic BP ranging from 80 to 125 mmHg, whereas for those individuals with a BPV metric at the 95th percentile (0.170), the range of experienced systolic BPs is from 71 to 140 mmHg. Similarly, for those individuals with systolic BP of 140 mmHg (Figure 1B), the range of experienced systolic BPs is 112–175 mmHg at a median value of BPV metric and 100–197 mmHg for BPV metric at the 95th percentile. The BPV metric was independent of the baseline systolic BP (Supplemental Figure 2).
Figure 1.
Graphical display of the mid 95% of systolic BP values for a hypothetical individual with a given predialysis systolic BP. (A) An individual with systolic BP of 100 mmHg. (B) An individual with systolic BP of 140 mmHg. (C) An individual with systolic BP of 180 mmHg. In each panel, the midpoint represents the average BP, and the bars represent the variability of systolic BP at a given percentile of the BPV metric (5th, 25th, 75th, and 95th percentiles).
Baseline Characteristics
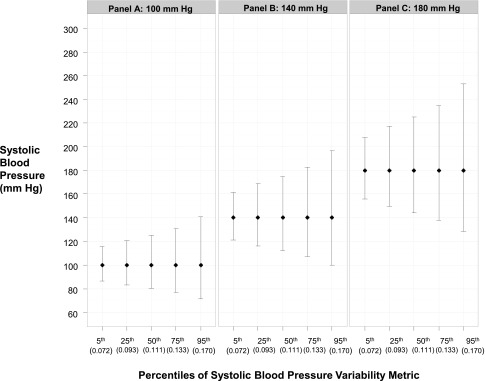
The final study cohort comprised 11,291 in-center hemodialysis patients that represented 53.2% of the initial cohort (Figure 2). Compared with all-incident dialysis patients, those patients included in the final cohort were more likely to be black (37% versus 28%) and have diabetes (58% versus 50%). During the study follow-up period, patients had 3,450,658 predialysis systolic BP measurements obtained (median measurements per patient=252, 25th to 75th percentiles=137–427). Table 1 presents the baseline characteristics of the study population overall and by tertile of BPV. The mean age of the study participants was 62 years, 55% of participants were men, and 58% of participants were white. At baseline, 65% of patients had diabetes, 56% of patients had cardiovascular (CV) disease (CVD), and 46% of patients had congestive heart failure (CHF). Average baseline predialysis systolic BP was 151±20 mmHg. Patients in the highest BPV tertile were more likely to be women, be black, and have diabetes, CVD, CHF, greater comorbidities, higher baseline systolic BP, lower serum albumin, and/or lower hemoglobin than those patients in the lower tertiles. Supplemental Table 2 presents the baseline characteristics of the study population by categories of systolic BP. Those patients with higher BP were more likely to be younger, be women, be black, and/or have diabetes, but they had a lower overall burden of comorbidities.
Figure 2.
Overview of cohort formation. Selection of the final cohort of 11,291 incident in-center hemodialysis patients from the initial cohort of all patients starting dialysis at Dialysis Clinic, Inc. (DCI) outpatient dialysis clinics from 2003 to 2008.
Table 1.
Baseline characteristics of 11,291 incident hemodialysis patients by tertiles of predialysis systolic BPV
| Characteristics | Overall | Tertiles of BPV | P Valuea | ||
|---|---|---|---|---|---|
| Lowest (<0.0990) | Middle (0.0990–0.1249) | Highest (>0.1249) | |||
| N (%) | 11,291 | 3728 (33.0) | 3841 (34.0) | 3722 (33.0) | |
| Demographics | |||||
| Age (yr) | 61.9±14.9 | 61.7±15.4 | 62.7±14.8 | 61.5±14.5 | 0.85 |
| Sex (% men) | 54.8 | 62.4 | 54.8 | 47.2 | <0.001 |
| Race (%) | |||||
| White | 58.4 | 65.4 | 59.5 | 50.3 | |
| Black | 37.3 | 30.4 | 36.4 | 45.2 | |
| Other | 4.2 | 4.2 | 4.1 | 4.5 | <0.001 |
| Ethnicity, Hispanic (%) | 5.7 | 6.2 | 5.6 | 5.3 | 0.27 |
| Race and ethnicity (%) | <0.001 | ||||
| Black Hispanic | 0.2 | 0.1 | 0.3 | 0.2 | |
| Black non-Hispanic | 37.1 | 30.3 | 36.1 | 44.9 | |
| Other | 4.2 | 4.2 | 4.1 | 4.5 | |
| White Hispanic | 5.1 | 5.8 | 4.9 | 4.6 | |
| White non-Hispanic | 53.3 | 59.6 | 54.6 | 45.7 | |
| Clinical | |||||
| Diabetes (%) | 64.9 | 59.8 | 64.4 | 70.5 | <0.001 |
| CVD (%) | 55.9 | 51.5 | 57 | 59.3 | <0.001 |
| CHF (%) | 46.2 | 42.9 | 46.8 | 48.7 | <0.001 |
| Comorbidity index (%) | |||||
| 0–3 | 41.4 | 46.2 | 40.7 | 37.2 | |
| 4–6 | 26.3 | 24.4 | 26.8 | 27.6 | |
| 7–9 | 19.5 | 17.9 | 19.4 | 21.2 | |
| ≥10 | 12.8 | 11.5 | 13 | 13.9 | <0.001 |
| BMI (kg/m2) | 27.8±7.0 | 27.1±6.0 | 27.9±7.0 | 28.2±7.8 | <0.001 |
| Baseline systolic BP (mmHg) | 150.0±20.0 | 148.4±19.6 | 149.7±19.9 | 151.9±20.4 | <0.001 |
| Baseline systolic BPV | |||||
| Mean (SD) | 0.115±0.030 | 0.084±0.011 | 0.111±0.007 | 0.149±0.022 | <0.001 |
| Median (25th, 75th percentiles) | 0.111 (0.093, 0.133) | 0.086 (0.077, 0.093) | 0.111 (0.105, 0.118) | 0.143 (0.133, 0.159) | |
| Heart rate (per min) | |||||
| Mean (SD) | 78.1 (11.9) | 78.3 (11.8) | 77.9 (11.9) | 78.2 (12.1) | 0.06 |
| Median (25th, 75th percentiles) | 77.2 (69.5, 85.9) | 77.5 (69.9, 86) | 77.1 (69.2, 85.8) | 77.1 (69.6, 86) | |
| ESRD related | |||||
| Cause of ESRD (%) | <0.001 | ||||
| Diabetes | 49.7 | 45.4 | 49 | 54.8 | |
| Hypertension | 28.1 | 26.6 | 29.1 | 28.7 | |
| GN | 9 | 11.3 | 9 | 6.8 | |
| Other | 13.1 | 16.7 | 13 | 9.7 | |
| Average Kt/V | 1.5±0.3 | 1.5±0.3 | 1.5±0.3 | 1.5±0.3 | 0.06 |
| Relative fluid removal per session (%) | 3.3±1.3 | 3.4±1.4 | 3.3±1.3 | 3.3±1.4 | 0.20 |
| Achieved target dry weight (%) | 51 | 54.3 | 51.8 | 46.9 | <0.001 |
| Laboratory parameters | |||||
| Serum albumin (g/dl) | 3.66±0.43 | 3.7±0.4 | 3.7±0.4 | 3.6±0.5 | <0.001 |
| Calcium phosphate product | 50.09±15.05 | 50.2±14.5 | 50.0±15.0 | 50.0±15.7 | 0.90 |
| Hemoglobin (g/dl) | 12.00±1.25 | 12.1±1.2 | 12.0±1.3 | 11.9±1.3 | <0.001 |
| Ferritin (ng/ml) | 448.8±335.3 | 443.2±339.0 | 443.6±330.8 | 459.9±336.1 | 0.04 |
| Antihypertensive medications (%) | <0.001 | ||||
| Any β-blocker regimen (without RAS) | 34.1 | 35.5 | 35.8 | 30.8 | |
| Any RAS regimen (without β-blocker) | 17 | 16.2 | 17.2 | 17.7 | |
| β-Blocker + RAS combination | 34.8 | 30.8 | 33.4 | 40.2 | |
| Other medications and combinations | 14.1 | 17.5 | 13.6 | 11.3 | |
| Number of antihypertensive medications (%) | <0.001 | ||||
| 0–2 | 51.9 | 57.5 | 52.3 | 46.1 | |
| 3–4 | 40.3 | 36.6 | 40.3 | 44.1 | |
| ≥5 | 7.7 | 6 | 7.4 | 9.8 | |
Data are presented as mean (SD) or column percent unless otherwise specified. Conversion factors: albumin in grams per deciliter to grams per liter, ×10; hemoglobin in grams per deciliter to grams per liter, ×10. No conversion is necessary for ferritin in nanograms per milliliter and micrograms per liter.
P values for continuous variables are P trend obtained from linear regression, and P values for categorical variables are obtained from chi-squared test.
Predictors of Baseline BPV
Table 2 describes the association of BPV with patient characteristics at baseline. After multivariate adjustment, patients who were women, were black, were obese (body mass index [BMI] above 40 kg/m2), had diabetes, had CVD, had a higher calcium-phosphate product, and/or had a lower hemoglobin (below 10 g/dl) tended to have higher BPV. Patients with lower BMI (below 18.5 kg/m2), greater fluid removal per dialysis session, higher albumin, and/or higher hemoglobin (above 10 g/dl) tended to have lower BPV. Compared with those patients receiving β-blocker–containing regimens, patients receiving regimens with renin-angiotensin system (RAS) drugs had higher BPV, whereas patients receiving regimens without β-blocker or RAS drugs had lower BPV.
Table 2.
Factors associated with predialysis systolic BPV in 11,291 incident hemodialysis patients
| Characteristics | Coefficient (95% CI)a | P Value |
|---|---|---|
| Demographics | ||
| Age (per SD) | −0.42 (−1.11 to 0.27) | 0.23 |
| Sex, women versus men | 5.87 (4.64 to 7.10) | <0.001 |
| Black versus white | 4.86 (3.43 to 6.30) | <0.001 |
| Hispanic versus non-Hispanic | −0.14 (−2.93 to 2.65) | 0.92 |
| Clinical | ||
| Diabetes | 2.59 (0.81 to 4.38) | 0.004 |
| CVD | 1.52 (0.09 to 2.95) | 0.04 |
| CHF | −0.95 (−2.75 to 0.86) | 0.31 |
| Comorbidity index | ||
| 0–3 | Reference | |
| 4–6 | 2.82 (0.90 to 4.73) | 0.004 |
| 7–9 | 2.06 (−0.49 to 4.61) | 0.11 |
| ≥10 | 2.48 (−0.55 to 5.51) | 0.11 |
| BMIb<18.5 kg/m2 (per SD) | −33.00 (−44.94 to −21.07) | <0.001 |
| BMIb>18.5 to ≤40 kg/m2 (per SD) | 0.73 (−0.08 to 1.54) | 0.08 |
| BMIb>40 kg/m2 (per SD) | 5.53 (3.01 to 7.95) | <0.001 |
| ESRD related | ||
| Cause of ESRD | ||
| Diabetes | Reference | |
| Hypertension | 2.98 (1.16 to 4.80) | 0.001 |
| GN | −5.26 (−7.69 to −2.82) | <0.001 |
| Other | −3.82 (−5.98 to −1.67) | <0.001 |
| Average Kt/V (per SD) | 0.23 (−0.42 to 0.88) | 0.49 |
| Relative fluid removal per session (per SD)c | −0.97 (−1.61 to −0.34) | 0.003 |
| Laboratory parameters | ||
| Serum albumin (per SD) | −3.31 (−3.91 to −2.71) | <0.001 |
| Calcium phosphate product (per SD) | 0.70 (0.11 to 1.30) | 0.02 |
| Hemoglobin (<10 g/dl, per SD) | 3.97 (0.35 to 7.60) | 0.03 |
| Hemoglobin (>10 g/dl, per SD) | −1.28 (−1.93 to −0.63) | <0.001 |
| Ferritin (per SD) | 0.26 (−0.33 to 0.85) | 0.38 |
| Antihypertensive medications | ||
| Any β-blocker regimen (without RAS) | Reference | |
| Any RAS regimen (without β-blocker) | 1.84 (0.15 to 3.52) | 0.03 |
| β-Blocker + RAS combination | 5.20 (3.83 to 6.56) | <0.001 |
| Other medications and combinations | −2.04 (−3.77 to −0.31) | 0.02 |
Coefficient for multivariable linear mixed effects models with a random intercept for the clinic to account for outcome clustering by providers. Value of coefficient represents change in BPV metric×10−3 per 1 unit change in the factors. Positive numbers indicate higher BPV per 1 unit change in factors, and negative numbers indicate lower BPV per 1 unit change in factors.
BMI is modeled as a linear spline with knots at 18.5 and 40 kg/m2.
Relative fluid removal per dialysis session=(predialysis weight−postdialysis weight)/postdialysis weight.
All-Cause Mortality
There were 3200 (28.3%) deaths over a median follow-up of 22 months (25th to 75th percentiles, 13–36 months). Higher BPV was associated with an increased risk of death in unadjusted and fully adjusted models (Table 3). In the fully adjusted model, each 1 SD increase in the BPV was associated with 18% higher risk of death (95% confidence interval [95% CI], 13% to 22%).
Table 3.
Association of predialysis systolic BPV and outcomes among 11,291 incident hemodialysis patients
| Outcomes | Events | Crudea | Minimally Adjustedb | Fully Adjustedc | |||
|---|---|---|---|---|---|---|---|
| HR (95% CI) | P Value | HR | P Value | HR | P Value | ||
| All-cause mortality | 3200 | 1.34 (1.30 to 1.39) | <0.001 | 1.41 (1.36 to 1.46) | <0.001 | 1.17 (1.13 to 1.21) | <0.001 |
| CV mortality | 1598 | 1.32 (1.26 to 1.38) | <0.001 | 1.38 (1.32 to 1.45) | <0.001 | 1.18 (1.12 to 1.23) | <0.001 |
| CV events | 4528 | 1.19 (1.15 to 1.23) | <0.001 | 1.21 (1.17 to 1.25) | <0.001 | 1.10 (1.07 to 1.14) | <0.001 |
Unadjusted model.
Adjusted for age, sex, race, and ethnicity.
Adjusted for demographic characteristics (age, sex, race, and ethnicity), clinical factors (history of diabetes, CVD, CHF, comorbidity index, and BMI), ESRD-related factors (cause of ESRD, Kt/V, and relative fluid removal), laboratory measurements (serum albumin, calcium–phosphate product, hemoglobin, and ferritin), and antihypertensive medications.
CV Mortality
We observed 1592 deaths from CV causes during the follow-up period (nonischemic heart disease, 56%; ischemic heart disease, 25%; cerebrovascular disease, 9%; ischemic bowel, 1%; other CV causes, 9%). Higher BPV was associated with an increased risk of CV death in unadjusted and fully adjusted models (Table 3). In the fully adjusted model, each 1 SD increase in the BPV was associated with 18% higher risk of CVD death (95% CI, 12% to 24%).
First CV Event
There were 4528 CV events during follow-up, of which 696 (15.4%) were CV deaths and 3832 (84.6%) were CV hospitalizations (ischemic heart disease, 23.5%; CHF, 25.4%; cerebrovascular disease, 14.5%; dysrhythmias, 11.4%; peripheral vascular disease, 22.5%; other, 2.8%). Table 3 presents the association of BPV with first CV event. Findings for BPV and first CV event were consistent with other outcomes, and higher BPV was again associated with a higher risk of first CV event.
Sensitivity Analyses
Analyses conducted without (complete case) and with imputation for missing variables carrying the last observation forward were similar to the primary analysis in both direction and magnitude (data not shown). BPV analyzed as tertiles had a similar association with outcomes as the primary analysis, and the risk of outcomes was higher for the middle and highest tertiles of BPV compared with the lowest tertile (Supplemental Table 3). After stratification by baseline systolic BP categories, the magnitude and direction of the association between BPV and outcomes were still similar to the primary analysis in each of the categories, suggesting that the association between BPV and outcomes was not dependent on baseline BP (Table 4).
Table 4.
Association of predialysis systolic BPV with outcomes after stratification by baseline predialysis systolic BP categories in 11,291 incident hemodialysis patients
| Outcomes | BP Range (mmHg) | Events | N | Crudea | Minimally Adjustedb | Fully Adjustedc | |||
|---|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | P Value | HR (95% CI) | P Value | HR (95% CI) | P Value | ||||
| All-cause mortality | |||||||||
| Q1.1 | <125 | 483 | 1168 | 1.28 (1.19 to 1.38) | <0.001 | 1.31 (1.22 to 1.42) | <0.001 | 1.22 (1.11 to 1.34) | <0.001 |
| Q1.2 | 125–133 | 328 | 1062 | 1.36 (1.23 to 1.51) | <0.001 | 1.42 (1.28 to 1.58) | <0.001 | 1.11 (0.99 to 1.26) | 0.08 |
| Q2 | 133–145 | 643 | 2402 | 1.39 (1.30 to 1.48) | <0.001 | 1.44 (1.35 to 1.53) | <0.001 | 1.16 (1.08 to 1.24) | <0.001 |
| Q3 | 145–155 | 555 | 2175 | 1.42 (1.32 to 1.53) | <0.001 | 1.50 (1.38 to 1.63) | <0.001 | 1.22 (1.13 to 1.32) | <0.001 |
| Q4 | 155–167 | 551 | 2171 | 1.39 (1.28 to 1.51) | <0.001 | 1.44 (1.32 to 1.56) | <0.001 | 1.16 (1.08 to 1.26) | <0.001 |
| Q5 | >167 | 640 | 2274 | 1.28 (1.21 to 1.37) | <0.001 | 1.34 (1.26 to 1.43) | <0.001 | 1.19 (1.11 to 1.27) | <0.001 |
| CV mortality | |||||||||
| Q1.1 | <125 | 241 | 1168 | 1.35 (1.20 to 1.51) | <0.001 | 1.37 (1.22 to 1.55) | <0.001 | 1.30 (1.14 to 1.48) | <0.001 |
| Q1.2 | 125–133 | 168 | 1062 | 1.38 (1.22 to 1.56) | <0.001 | 1.41 (1.25 to 1.60) | <0.001 | 1.16 (1.00 to 1.35) | 0.05 |
| Q2 | 133–145 | 314 | 2402 | 1.30 (1.17 to 1.43) | <0.001 | 1.35 (1.21 to 1.49) | <0.001 | 1.13 (1.01 to 1.26) | 0.03 |
| Q3 | 145–155 | 259 | 2175 | 1.39 (1.25 to 1.55) | <0.001 | 1.47 (1.31 to 1.65) | <0.001 | 1.20 (1.07 to 1.34) | 0.002 |
| Q4 | 155–167 | 276 | 2171 | 1.29 (1.16 to 1.44) | <0.001 | 1.33 (1.19 to 1.49) | <0.001 | 1.12 (1.01 to 1.25) | 0.04 |
| Q5 | >167 | 340 | 2274 | 1.29 (1.19 to 1.41) | <0.001 | 1.34 (1.23 to 1.47) | <0.001 | 1.20 (1.09 to 1.31) | <0.001 |
| CV events | |||||||||
| Q1.1 | <125 | 513 | 1168 | 1.16 (1.06 to 1.26) | <0.001 | 1.17 (1.07 to 1.28) | <0.001 | 1.11 (1.01 to 1.23) | 0.04 |
| Q1.2 | 125–133 | 435 | 1064 | 1.19 (1.10 to 1.30) | <0.001 | 1.21 (1.10 to 1.32) | <0.001 | 1.12 (1.02 to 1.22) | 0.01 |
| Q2 | 133–145 | 881 | 2407 | 1.22 (1.14 to 1.30) | <0.001 | 1.22 (1.13 to 1.32) | <0.001 | 1.09 (1.01 to 1.17) | 0.03 |
| Q3 | 145–155 | 823 | 2180 | 1.20 (1.12 to 1.29) | <0.001 | 1.23 (1.14 to 1.33) | <0.001 | 1.11 (1.03 to 1.20) | 0.01 |
| Q4 | 155–167 | 876 | 2174 | 1.18 (1.11 to 1.27) | <0.001 | 1.20 (1.12 to 1.29) | <0.001 | 1.10 (1.03 to 1.18) | 0.01 |
| Q5 | >167 | 1000 | 2279 | 1.15 (1.09 to 1.22) | <0.001 | 1.18 (1.11 to 1.25) | <0.001 | 1.11 (1.04 to 1.18) | <0.001 |
HR per 1 SD increase in the predialysis systolic BPV metric. Q1.1 to Q5 refers to categories of systolic BP at baseline (quintiles [fifths] of systolic BP, with the lowest quintile [Q1] further subdivided into two categories at the median [Q1.1 and Q1.2]).
Unadjusted model.
Adjusted for age, sex, race, and ethnicity.
Adjusted for demographic characteristics (age, sex, race, and ethnicity), clinical factors (history of diabetes, CVD, CHF, comorbidity index, and BMI), ESRD-related factors (cause of ESRD, Kt/V, and relative fluid removal), laboratory measurements (serum albumin, calcium–phosphate product, hemoglobin, and ferritin), and antihypertensive medications.
Additional Analyses
We did not find that the presence of a slow heart rate (<60/min) and antihypertensive medications use modified the associations noted in the primary analysis. P interaction for antihypertensive medications and heart rate was 0.45 for the model of predictors of BPV and 0.64, 0.80, and 0.03 for the models for BPV and all-cause mortality, CV mortality, and CV events, respectively. Number of antihypertensive medications prescribed was associated with BPV. BPV was higher in those patients receiving three or four medications (coefficient, 5.17; 95% CI, 3.88 to 6.46; P<0.001) and five or more medications (coefficient, 9.13; 95% CI, 6.87 to 11.38; P<0.001) compared with those patients receiving zero, one, or two medications. Adjustment for number of medications in the outcomes model did not change the association between BPV and outcomes. The adjusted hazard ratio (HR) per 1 SD increase in BPV for all-cause mortality was 1.18 (P<0.001), the adjusted HR per 1 SD increase in BPV for CV mortality was 1.18 (P<0.001), and the adjusted HR per 1 SD increase in BPV for CV events was 1.11 (P<0.001). Attainment of dry weight in ≥80% of the dialysis sessions was associated with lower BPV (coefficient, −4.69; 95% CI, −5.92 to −3.47; P<0.001) than attainment of dry weight in <80% of the dialysis sessions. However, adjustment for dry weight attainment in the outcomes model did not change the association between BPV and outcomes (data not shown).
Discussion
In this national cohort of 11,291 incident in-center hemodialysis patients, higher predialysis systolic BPV was independently associated with an increased risk of all-cause mortality, CV mortality, and first CV event (CV hospitalization or CV death). This association was present at all baseline systolic BP categories and after adjustment for a number of potential confounding factors, including antihypertensive medications and fluid removal during hemodialysis. At baseline, greater fluid removal during dialysis and the use of antihypertensive medication treatment regimens that did not contain β-blockers or RAS blocking drugs were both associated with lower BPV. Thus, predialysis systolic BPV seems to be a potentially modifiable risk factor for poor outcomes in hemodialysis patients.
BPV is emerging as a leading risk factor for adverse outcomes in nondialysis patients, and individuals with greater BPV are at higher risk for myocardial infarction and stroke.11,13,16,17 However, relatively few studies have attempted to analyze the association of BPV with outcomes in dialysis patients. In a report using data from 6961 incident dialysis patients treated at Fresenius-operated hemodialysis units in the United States, although greater BPV was associated with higher all-cause mortality, analyses did not account for the effect of fluid removal during dialysis and antihypertensive therapy.14 In an analysis of 397 prevalent hemodialysis patients participating in the Fosinopril in Dialysis trial, addition of BPV to the model along with traditional risk factors for mortality improved the model fit (R2) by 30%, and increased BPV was associated with a trend to increased CV events.12 In a recent retrospective analysis of the Hemodialysis study, predialysis systolic BPV was associated with higher risk of death, but the effect was only significant among those individuals with systolic BP<140 mmHg.18 The BPV metric used in this study was the coefficient of variation, which is highly dependent on the mean BP. Volume changes were not accounted for in this analysis. Our study both replicates and extends the findings of these prior studies. Our BPV metric was independent of mean BP (Supplemental Figure 2), avoiding some of the problems of previous studies, and we show a robust association between BPV and outcomes independent of both fluid removal and antihypertensive medication use.
Our study highlights the importance of fluid removal and attainment of dry weight in dialysis patients. Fluid overload is an important factor for uncontrolled hypertension in dialysis patients, and greater fluid removal in the Frequent Hemodialysis Network Trial was associated with lowering of predialysis BP and reduction in antihypertensive medications use.19 Our findings suggest that greater fluid removal is also associated with lower predialysis systolic BPV. Flythe et al.10 investigated the factors associated with systolic BPV during dialysis and noted that greater fluid removal during dialysis was associated with higher intradialytic systolic BPV but that antihypertensive medication class had no effect. Lower predialysis BPV in patients with higher fluid removal could be either because of improved control of BP with ultrafiltration and volume control or a reflection of achieving greater ultrafiltration in patients with stable BP.
In addition to volume removal, we found predialysis systolic BPV to be associated with several other modifiable and nonmodifiable factors. The nonmodifiable factors included women, black race, and history of diabetes or CVD (all associated with higher BPV). Perhaps more important, modifiable factors included BMI, type of antihypertensive medication regimen, calcium-phosphate product, and hemoglobin. We found that lower hemoglobin (below 10 g/dl) was also associated with higher BPV. This finding could be because of the possibility of greater comorbidities in those individuals with lower hemoglobin or possibly, greater use of erythropoietin-stimulating agents among such patients. We also noted that those individuals on a non–β-blocker and non-RAS antihypertensive regimen had lower BPV compared with individuals on β-blocker–containing regimens. This finding deserves special consideration given the widespread use of β-blockers in dialysis patients.15 It is possible that this effect could be because of the erratic dosing schedules for antihypertensive medications often used in clinical practice. For example, dialysis patients are often asked to hold medications before dialysis treatments, and patients on β-blockers could experience higher BPV caused by β-blocker withdrawal. Similar findings of increased BPV with β-blocker and RAS agents have also been reported in nondialysis patients.20 Although we carefully adjusted for comorbidities and CVD in our analysis, it is still possible that those individuals treated with β-blockers had CVD that was not captured with claims data (unmeasured confounders) and that higher BPV in the β-blocker group was caused by the greater burden of CVD. Importantly, we did not find that the effect of the antihypertensive regimen on BPV differed by the presence of bradycardia.
We focused on predialysis systolic BPV as a risk factor for outcomes in our study, but there are other aspects of systolic BP in hemodialysis patients that deserve mention. Home systolic BP measurements in dialysis patients are associated with left ventricular hypertrophy and mortality.21–23 Home BP results in more standardized measurements and multiple readings compared with dialysis unit measurements. As a result, measurement error in BP is likely to be lower and could yield a stronger association between home BP and outcomes compared with dialysis unit BP. Home BP measurements are, however, not routinely performed in the United States, and there are no guidelines for measurement, reporting, or target BP levels in dialysis patients. Recent work has also highlighted the importance of intradialytic hypertension as risk factor for mortality in dialysis patients.24,25 The relationships between home BP and BPV, predialysis systolic BPV, and intradialytic BP changes are not known and should be investigated in future studies. Endothelial cell dysfunction and sympathetic hyperactivity may contribute to higher home, predialysis, and intradialytic BPV, and they may potentially be therapeutic targets with therapies, such as carvedilol or renal denervation.26–28
Our findings have several implications for clinical practice and research. It is important for clinicians to recognize BPV in their dialysis patients as a risk factor for adverse CV events. Our findings are consistent with emerging evidence of adverse outcomes associated with BPV in nondialysis patients.16 As such, the optimal BP management strategy in dialysis patients should focus on both reduction in average BP levels as well as reduction or prevention of excessive fluctuations in BP. Similarly, guidelines for management of BP in dialysis patients, extrapolated from general population studies, have primarily focused on average BP levels before and after dialysis.2,29 These guidelines should recognize BPV as an emerging risk factor and consider clinical interventions aimed at reducing BPV or research recommendations for improving the understanding of its relationship with adverse outcomes. Finally, investigators conducting randomized trials of BP management in dialysis patients might consider BPV as both a predictor and an outcome of interest.
Several limitations of our study are worth noting. First, BP measurements were performed as part of routine clinical care and not standardized. As a result, it is possible that individuals with severe vascular disease may have had more variable readings, particularly if the BP measurement site was not constant. Nonetheless, clinicians managing BP in real world practices rely on clinical measures to adjust their treatment strategies, providing support for use of these measures in our analyses. Second, although we adjusted for fluid removal, we did not have assessment of overall volume status in these individuals. It is, therefore, possible that individuals with greater BPV were in a state of chronic volume overload. Third, although we had nurse-entered electronic medication lists for each patient, we did not have a direct assessment of medication adherence. It is possible that nonadherence to antihypertensive agents may be associated with higher BPV and adverse outcomes. Antihypertensive medication regimens may vary on dialysis and nondialysis days, and these variations could contribute to higher BPV. Fourth, we only analyzed the association between predialysis systolic BPV but not other components of BP, such as diastolic BP, pulse pressure, or postdialysis BP. Variability in each of these BP components may be a risk factor for adverse outcomes and deserves additional study. These limitations of our study are balanced by its strengths, including an incident dialysis cohort from a national not-for-profit organization, availability of detailed time-varying patient level data on key variables, including fluid removal and antihypertensive medications, detailed ascertainment of comorbidities using claims data, and ascertainment of cause of death using linkage with the National Death Index.
In conclusion, predialysis systolic BPV seems to be an important and potentially modifiable risk factor for all-cause mortality, CV mortality, and CV events. Future studies of BP management in dialysis patients should focus on optimal BP target as well as reducing BPV.
Concise Methods
Study Design and Population
As part of a larger project to study the comparative effectiveness of antihypertensive treatments in patients with ESRD,30 we constructed a cohort of incident hemodialysis patients to identify predictors of BPV and quantify the association of BPV with mortality and CV events. We used data from Dialysis Clinic, Inc. (DCI). DCI is a not-for-profit medium-sized dialysis provider in the United States with over 210 dialysis clinics in 27 states. The DCI population of patients is diverse, with characteristics similar to US dialysis patients (Supplemental Table 1). Our study cohort included adults over the age of 18 years who initiated in-center hemodialysis between January 1, 2003 and June 30, 2008 and were treated with antihypertensive medications and were alive and on in-center hemodialysis at 6 months (Figure 2). We used administrative billing claims data to ascertain patients’ accumulation of comorbidity during their first 180 days of hemodialysis. The rationale for choosing this 180-day period was twofold. First, a priori, we hypothesized that patients’ baseline comorbidity would contribute substantially to their BPV. Second, we felt that the first 90 days of dialysis, which are associated with high rates of morbidity,15 might not accurately reflect associations of BPV with outcomes among chronic stable hemodialysis patients. After assessment of comorbidities, we followed patients from day 181 on hemodialysis to December 31, 2008. We censored patients from the analysis if they underwent kidney transplantation, switched to a home dialysis modality (i.e., home hemodialysis or peritoneal dialysis), transferred to a non-DCI dialysis facility, withdrew from hemodialysis, or were lost to follow-up (Figure 2). We categorized patients’ follow-up time into 30-day discrete time intervals and summarized covariate values over each 30-day interval before the interval in which the outcome of interest occurred.
We obtained information on patients’ comorbidities, hospitalizations, dialysis treatments, laboratory tests, and medications from the DCI electronic medical records. We linked these data to the US Renal Data System registry to obtain additional information on comorbidities and health care use.30 We determined patients’ cause of death by linking data with the National Death Index, which is commonly used to ascertain the date and cause of death in population-based studies.30 The study was approved by the Johns Hopkins Medicine Institutional Review Board (Baltimore, MD).
Exposure
Predialysis systolic BPV was our primary exposure of interest. BP recordings were obtained in a sitting position before the start of each dialysis treatment using automated oscillometric devices as part of routine clinical care. We defined patients’ baseline systolic BP as the mean of all predialysis systolic BPs during month 6.
To quantify individual's BPV, we first fit linear mixed effects models to the natural log of a patient’s systolic BP values over time (details in Supplemental Material section on BPV metric). We then defined BPV as the SD of the residual deviations from the modeled average BP (Supplemental Figure 1). This methodology aimed to eliminate dependence of our BPV metric on mean systolic BP. To provide clinical relevance to the BPV metric, we constructed visual displays of the middle 95% range of BPs that a patient may experience at a given percentile of the BPV metric {exp[log(SBP)±2(BPV metric percentile)]}. We defined baseline BPV as the BPV from day 91 to day 180. During follow-up, we assessed BPV over rolling time-varying 90-day windows starting at day 181 after start of dialysis.
Outcome
Our primary outcome was all-cause mortality. Secondary outcomes were CV mortality and first CV event defined as the composite of first CV hospitalization (including ischemic heart disease, CHF, stroke, dysrhythmia, and peripheral vascular disease-related hospitalization) or CV death. CV deaths and hospitalizations were identified by International Classification of Diseases, version 10 codes based on extensive review of the literature as previously described.30
Covariates
Baseline covariates included age, sex, race (black, white, or other), ethnicity (Hispanic versus non-Hispanic), and cause of ESRD (hypertension, diabetes, GN, or other). Comorbidities were assessed based on Medicare claims and DCI clinical data. Baseline comorbidities were assessed over the first 180 days after dialysis initiation and then updated in each 30-day interval starting from day 181. Comorbidities assessed included CVD, diabetes, and CHF. To account for other comorbidities, a comorbidity index previously validated in dialysis patients was also calculated.31 Other time-varying covariates averaged over each 30-day period included BMI (weight in kilograms per height in meters2), relative volume removed per dialysis session [(predialysis weight−postdialysis weight)/postdialysis weight], serum albumin, hemoglobin, corrected calcium and phosphate product, and Kt/V. Serum ferritin values were averaged over 90-day periods, because they were obtained quarterly. Antihypertensive medications use was based on nurse-entered drug start and stop dates in DCI electronic medical records and summarized over 30-day intervals. Antihypertensive medications were classified as one of five mutually exclusive classes: β-blocker–containing regimen (without an RAS agent; BB), RAS-containing regimen without a β-blocker (RAS), regimen containing both a β-blocker and an RAS agent (BB + RAS), any other antihypertensive regimen without β-blocker or RAS agent (other), and any regimen of antihypertensive medication at baseline that was discontinued during follow-up. Covariates included in additional analysis included predialysis sitting heart rate (categorized as <60 or ≥60/min), number of antihypertensive medications prescribed in each 30-day interval (categorized as 0–2, 3–4, and ≥5) and dry weight attainment defined as achieving a postdialysis weight within 0.5 kg or below prescribed dry weight. Dry weight attainment was determined at each dialysis session and then categorized as <80% or ≥80% over each 30-day interval.
Statistical Analyses
We compared patients’ baseline characteristics across tertiles of BPV. We assessed factors independently associated with BPV at baseline using linear mixed effects models with a random intercept for the clinic to account for clustering of outcomes by providers. We incorporated other explanatory variables in models based on a priori reasoning, including demographic characteristics (age, sex, race, and ethnicity), clinical factors (history of diabetes, CVD, or CHF, comorbidity index, and BMI), ESRD cause, treatment factors (Kt/V and relative fluid removal), laboratory measurements (serum albumin, calcium-phosphate product, hemoglobin, and ferritin), and antihypertensive medications. We checked our model fit by examining plots of marginal residuals from the fitted model. Missing data rates for discrete time intervals were as follows: BMI (<1%), relative volume removed (<1%), Kt/V (<1%), antihypertensive medications (<1%), ferritin (3.2%), hemoglobin (3.8%), calcium–phosphate product (7.0%), and albumin (8.4%). Patients with greater than 1% missing data were more likely to be younger, black, and diabetic (P<0.05 for all). For variables with more than 1% missing data, we imputed data with 10 replicates. We analyzed the association of BPV with outcomes with discrete time proportional hazards models using binary regression with a complementary log–log link32 and fit with Generalized Estimating Equations33 to allow for clustering by clinic. We calculated HRs for each outcome per 1 SD increase in BPV after adjustment for the same a priori–defined confounders. We checked outcomes model fit by examining Pearson’s residual plots. In addition to the primary analyses listed above, we also conducted additional analyses to explore the effects of dry weight attainment, number of antihypertensive medications prescribed, and predialysis sitting heart rate. We conducted sensitivity analyses accounting for missing data, including complete case analyses and imputation using last observation carried forward for missing values. We also performed sensitivity analyses analyzing BPV by tertiles and quantifying the association of BPV with outcomes after stratification by categories of systolic BP at baseline (quintiles [fifths] of systolic BP with the lowest quintile further subdivided into two categories at the median). We defined statistical significance as P<0.05 using two-tailed tests. We performed all statistical analyses using SAS 9.2 (SAS Institute, Inc., Cary, NC).
Disclosures
None.
Supplementary Material
Acknowledgments
The authors thank the staff and patients of Dialysis Clinic, Inc.
The Developing Evidence to Inform Decisions about Effectiveness (DEcIDE) Network Patient Outcomes in ESRD Study was supported by the Agency for Healthcare Research and Quality (AHRQ) Contract HHSA290200500341I, Task Order #6. T.S. was supported by National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health Grant K23-DK-083514. D.C.C. was supported by the Amos Medical Faculty Development Program of the Robert Wood Johnson Foundation. W.M.M. was supported by Postdoctoral Full Fellowship Abroad Grant KFB 11.005 from the Dutch Kidney Foundation (Nierstichting).
Parts of this work were presented at the 2012 Annual Meeting of the American Society of Nephrology in San Diego, CA, on November 1–4, 2012.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. AHRQ: Identifiable information, on which this report, presentation, or other form of disclosure is based, is confidential and protected by federal law, Section 903(c) of the Public Health Service Act, 42 USC 299a-1(c). Any identifiable information that is knowingly disclosed is disclosed solely for the purpose for which it has been supplied. No identifiable information about any individual supplying the information or described in it will be knowingly disclosed except with the prior consent of that individual. The data reported here have been supplied by the US Renal Data System (USRDS). The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy or interpretation of the US Government. This research was conducted through a government contract with the AHRQ, an operating division of the US Department of Health and Human Services. Approval to assert copyright by the authors on the manuscript has been granted by the Government through the attached letter signed by the AHRQ Contracting Official. As stated in the letter, the Government retains rights to the use of the manuscript according to the contract and the Federal Acquisition Regulations (FAR). To meet the need for public accessibility to works funded by the Government, the authors request that the journal provide open access to the article if it is accepted for publication. Open access means that the final journal article is available electronically for free at the time of publication through the journal’s website. If this is not possible, the authors remain interested in having the manuscript be considered for journal publication. USRDS disclosure: The data reported here have been supplied by the USRDS. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy or interpretation of the US Government.
The DEcIDE Network Patient Outcomes in End-Stage Renal Disease Study Team consists of members from the Johns Hopkins University (L. Ebony Boulware, Karen Bandeen-Roche, Courtney Cook, Josef Coresh, Deidra Crews, Patti Ephraim, Bernard Jaar, Jeonyong Kim, Yang Liu, Jason Luly, Aidan McDermott, Wieneke Michels, Paul Scheel, Tariq Shafi, Stephen Sozio, Albert Wu, and Jing Zhou), University of California at San Francisco (Neil Powe), Chronic Disease Research Group (Allan Collins, Robert Foley, David Gilbertson, Haifeng Guo, Charles Herzog, Jiannong Liu, and Wendy St. Peter), Cleveland Clinic Foundation (Joseph Nally, Susana Arrigain, Stacey Jolly, Vicky Konig, Xiaobo Liu, Sankar Navaneethan, and Jesse Schold), University of New Mexico (Philip Zager), Tufts University (Dana Miskulin and Klemens Meyer), University of Miami (Julia Scialla), University of Manitoba (Navdeep Tangri), and Academic Medical Center, The Netherlands (Wieneke Michels).
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Blood Pressure Variability and Dialysis: Variability May Not Always Be the Spice of Life,” on pages 650–653.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2013060667/-/DCSupplemental.
References
- 1.Agarwal R, Nissenson AR, Batlle D, Coyne DW, Trout JR, Warnock DG: Prevalence, treatment, and control of hypertension in chronic hemodialysis patients in the United States. Am J Med 115: 291–297, 2003 [DOI] [PubMed] [Google Scholar]
- 2.Levin NW, Kotanko P, Eckardt KU, Kasiske BL, Chazot C, Cheung AK, Redon J, Wheeler DC, Zoccali C, London GM: Blood pressure in chronic kidney disease stage 5D-report from a Kidney Disease: Improving Global Outcomes controversies conference. Kidney Int 77: 273–284, 2010 [DOI] [PubMed] [Google Scholar]
- 3.Weir MR: Debate from the 2012 ASH Annual Scientific Sessions: Should blood pressure be reduced in hemodialysis patients? Con position. J Am Soc Hypertens 6: 443–447, 2012 [DOI] [PubMed] [Google Scholar]
- 4.Agarwal RL: Debate from the 2012 ASH Annual Scientific Sessions: Should blood pressure be reduced in hemodialysis patients? Pro position. J Am Soc Hypertens 6: 439–442, 2012 [DOI] [PubMed] [Google Scholar]
- 5.Kalantar-Zadeh K, Kilpatrick RD, McAllister CJ, Greenland S, Kopple JD: Reverse epidemiology of hypertension and cardiovascular death in the hemodialysis population: The 58th annual fall conference and scientific sessions. Hypertension 45: 811–817, 2005 [DOI] [PubMed] [Google Scholar]
- 6.Li Z, Lacson E, Jr., Lowrie EG, Ofsthun NJ, Kuhlmann MK, Lazarus JM, Levin NW: The epidemiology of systolic blood pressure and death risk in hemodialysis patients. Am J Kidney Dis 48: 606–615, 2006 [DOI] [PubMed] [Google Scholar]
- 7.Port FK, Hulbert-Shearon TE, Wolfe RA, Bloembergen WE, Golper TA, Agodoa LY, Young EW: Predialysis blood pressure and mortality risk in a national sample of maintenance hemodialysis patients. Am J Kidney Dis 33: 507–517, 1999 [DOI] [PubMed] [Google Scholar]
- 8.Robinson BM, Tong L, Zhang J, Wolfe RA, Goodkin DA, Greenwood RN, Kerr PG, Morgenstern H, Li Y, Pisoni RL, Saran R, Tentori F, Akizawa T, Fukuhara S, Port FK: Blood pressure levels and mortality risk among hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study. Kidney Int 82: 570–580, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zager PG, Nikolic J, Brown RH, Campbell MA, Hunt WC, Peterson D, Van Stone J, Levey A, Meyer KB, Klag MJ, Johnson HK, Clark E, Sadler JH, Teredesai P: “U” curve association of blood pressure and mortality in hemodialysis patients. Medical Directors of Dialysis Clinic, Inc. Kidney Int 54: 561–569, 1998 [DOI] [PubMed] [Google Scholar]
- 10.Flythe JE, Kunaparaju S, Dinesh K, Cape K, Feldman HI, Brunelli SM: Factors associated with intradialytic systolic blood pressure variability. Am J Kidney Dis 59: 409–418, 2012 [DOI] [PubMed] [Google Scholar]
- 11.Mancia G: Prognostic value of long-term blood pressure variability: The evidence is growing. Hypertension 57: 141–143, 2011 [DOI] [PubMed] [Google Scholar]
- 12.Rossignol P, Kessler M, Zannad F: Visit-to-visit blood pressure variability and risk for progression of cardiovascular and renal diseases. Curr Opin Nephrol Hypertens 22: 59–64, 2013 [DOI] [PubMed] [Google Scholar]
- 13.Rothwell PM, Howard SC, Dolan E, O’Brien E, Dobson JE, Dahlöf B, Sever PS, Poulter NR: Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet 375: 895–905, 2010 [DOI] [PubMed] [Google Scholar]
- 14.Brunelli SM, Thadhani RI, Lynch KE, Ankers ED, Joffe MM, Boston R, Chang Y, Feldman HI: Association between long-term blood pressure variability and mortality among incident hemodialysis patients. Am J Kidney Dis 52: 716–726, 2008 [DOI] [PubMed] [Google Scholar]
- 15.US Renal Data System : USRDS 2012 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2012 [Google Scholar]
- 16.Rothwell PM: Limitations of the usual blood-pressure hypothesis and importance of variability, instability, and episodic hypertension. Lancet 375: 938–948, 2010 [DOI] [PubMed] [Google Scholar]
- 17.Muntner P, Levitan EB, Reynolds K, Mann DM, Tonelli M, Oparil S, Shimbo D: Within-visit variability of blood pressure and all-cause and cardiovascular mortality among US adults. J Clin Hypertens (Greenwich) 14: 165–171, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chang TI, Flythe JE, Brunelli SM, Muntner P, Greene T, Cheung AK, Chertow GM: Visit-to-visit systolic blood pressure variability and outcomes in hemodialysis [published online ahead of print June 27, 2013]. J Hum Hypertens 10.1038/jhh.2013.49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chertow GM, Levin NW, Beck GJ, Depner TA, Eggers PW, Gassman JJ, Gorodetskaya I, Greene T, James S, Larive B, Lindsay RM, Mehta RL, Miller B, Ornt DB, Rajagopalan S, Rastogi A, Rocco MV, Schiller B, Sergeyeva O, Schulman G, Ting GO, Unruh ML, Star RA, Kliger AS, FHN Trial Group : In-center hemodialysis six times per week versus three times per week. N Engl J Med 363: 2287–2300, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Webb AJ, Fischer U, Mehta Z, Rothwell PM: Effects of antihypertensive-drug class on interindividual variation in blood pressure and risk of stroke: A systematic review and meta-analysis. Lancet 375: 906–915, 2010 [DOI] [PubMed] [Google Scholar]
- 21.Agarwal R: Managing hypertension using home blood pressure monitoring among haemodialysis patients—a call to action. Nephrol Dial Transplant 25: 1766–1771, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Agarwal R, Brim NJ, Mahenthiran J, Andersen MJ, Saha C: Out-of-hemodialysis-unit blood pressure is a superior determinant of left ventricular hypertrophy. Hypertension 47: 62–68, 2006 [DOI] [PubMed] [Google Scholar]
- 23.Moriya H, Oka M, Maesato K, Mano T, Ikee R, Ohtake T, Kobayashi S: Weekly averaged blood pressure is more important than a single-point blood pressure measurement in the risk stratification of dialysis patients. Clin J Am Soc Nephrol 3: 416–422, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Inrig JK, Oddone EZ, Hasselblad V, Gillespie B, Patel UD, Reddan D, Toto R, Himmelfarb J, Winchester JF, Stivelman J, Lindsay RM, Szczech LA: Association of intradialytic blood pressure changes with hospitalization and mortality rates in prevalent ESRD patients. Kidney Int 71: 454–461, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Van Buren PN, Kim C, Toto R, Inrig JK: Intradialytic hypertension and the association with interdialytic ambulatory blood pressure. Clin J Am Soc Nephrol 6: 1684–1691, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Converse RL, Jr., Jacobsen TN, Toto RD, Jost CM, Cosentino F, Fouad-Tarazi F, Victor RG: Sympathetic overactivity in patients with chronic renal failure. N Engl J Med 327: 1912–1918, 1992 [DOI] [PubMed] [Google Scholar]
- 27.Inrig JK, Van Buren P, Kim C, Vongpatanasin W, Povsic TJ, Toto R: Probing the mechanisms of intradialytic hypertension: A pilot study targeting endothelial cell dysfunction. Clin J Am Soc Nephrol 7: 1300–1309, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schlaich MP, Bart B, Hering D, Walton A, Marusic P, Mahfoud F, Böhm M, Lambert EA, Krum H, Sobotka PA, Schmieder RE, Ika-Sari C, Eikelis N, Straznicky N, Lambert GW, Esler MD: Feasibility of catheter-based renal nerve ablation and effects on sympathetic nerve activity and blood pressure in patients with end-stage renal disease. Int J Cardiol 168: 2214–2220, 2013 [DOI] [PubMed] [Google Scholar]
- 29.K/DOQI Workgroup : K/DOQI Clinical practice guidelines for cardiovascular disease in dialysis patients. Am J Kidney Dis 45[4 Suppl 3]: 16–153, 2005 [PubMed] [Google Scholar]
- 30.Boulware LE, Tangri N, Ephraim PL, Scialla JJ, Sozio SM, Crews DC, Shafi T, Miskulin DC, Liu J, St Peter W, Jaar BG, Wu AW, Powe NR, Navaneethan SD, Bandeen-Roche K, DEcIDE ESRD Patient Outcomes in Renal Disease Study Investigators : Comparative effectiveness studies to improve clinical outcomes in end stage renal disease: The DEcIDE patient outcomes in end stage renal disease study. BMC Nephrol 13: 167, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu J, Huang Z, Gilbertson DT, Foley RN, Collins AJ: An improved comorbidity index for outcome analyses among dialysis patients. Kidney Int 77: 141–151, 2010 [DOI] [PubMed] [Google Scholar]
- 32.Prentice RL, Kalbfleisch JD, Peterson AV, Jr., Flournoy N, Farewell VT, Breslow NE: The analysis of failure times in the presence of competing risks. Biometrics 34: 541–554, 1978 [PubMed] [Google Scholar]
- 33.Zeger SL, Liang K-Y: Longitudinal data analysis for discrete and continuous outcomes. Biometrics 42: 121–130, 1986 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.