Abstract
Objectives
The study determined if time perspective was associated with medication adherence among people with hypertension and diabetes.
Methods
Using the Health Beliefs Model, we used path analysis to test direct and indirect effects of time perspective and health beliefs on adherence among 178 people who participated in a community-based survey near Washington, D. C. We measured three time perspectives (future, present fatalistic, and present hedonistic) with the Zimbardo Time Perspective Inventory and medication adherence by self-report.
Results
The total model demonstrated a good fit (RMSEA = 0.17, 90% CI [0.10, 0.28], p = 0.003; comparative fit index = 0.91). Future time perspective and age showed direct effects on increased medication adherence; an increase by a single unit in future time perspective was associated with a 0.32 standard deviation increase in reported adherence. There were no significant indirect effects of time perspective with reported medication adherence through health beliefs.
Conclusion
The findings provide the first evidence that time perspective plays an under-recognized role as a psychological motivator in medication adherence.
Practice Implications
Patient counseling for medication adherence may be enhanced if clinicians incorporate consideration of the patient’s time perspective.
Keywords: medication adherence, time perspective, patient education
1. Introduction
The 100 million U.S. residents with hypertension or diabetes often struggle with medication adherence.1 On average, 65% of individuals report being non-adherent in some way.2 Their nonadherence contributes to many preventable consequences, including $100 billion in medical expenses,3 33% of hospital or nursing home admissions, and 124,000 deaths annually.4 Furthermore, the high prevalence of nonadherence among people with chronic diseases complicates attempts to ascertain the real benefits of medical care,5 and it increases risk of stroke and other adverse cardiovascular events.1 Interventions improving medication adherence would help mitigate medical risks and reduce costs of chronic disease management.
Converting discoveries about risk factors into knowledge about individual motivation remains a central issue in adherence research. For example, some studies associate better adherence with older age6 or having less education,7 where others report increased nonadherence among people using more medicines or more frequent dosing.4 Time since diagnosis can be another predictor of lower adherence.4,8-9 In one study, the percentage of individuals reporting nonadherence rose from 6 to 66% three years after diagnosis.9 In all, demographic and biomedical variables are largely external factors that individuals can neither determine nor modify.
1.1. Role of Psychological Factors in Understanding Medication Adherence
1.1.1 Health beliefs
Psychological frameworks may offer useful insights into factors that influence medication adherence beyond demographic and biomedical influences.7 They flexibly provide explanatory concepts or change theories to decipher how health habits develop over a lifetime, allowing clinicians to prescribe more holistic strategies for patient-centered chronic disease management.1,10-12 As Brown and Segal write, there is a broad understanding that “the decision to comply with medical regimens ultimately lies with the patient within the context of [his or her] beliefs and values” (p. 903).13-15 Individuals who have chronic diseases, like hypertension and diabetes, can make a series of trade-offs after receiving new medical information along six distinct dimensions: (1) perceived severity or interference with physical and mental functioning, (2) perceived potential threat from a medical condition, (3) perceived barriers to behavior change, (4) perceived benefits of behavior change, (5) behavioral cues, and (6) modifying factors.13
Early publications primarily reference the first four perceptions.13,16 The perceived severity dimension depicts feelings about a chronic condition’s seriousness and evaluations of consequences for changes in health status. The perceived susceptibility domain reflects how vulnerable a person believes he or she is to secondary complications. Perceived benefits describe the degree to which an individual believes specific treatments will be successful for curing or managing a condition. Finally, the perceived barriers domain represents the awareness of challenges that impede individuals from taking necessary actions to improve their health.13
Several studies largely attribute the motivation surrounding adherence to two health beliefs- an individual’s subjective perception of risk of complications related to chronic diseases (susceptibility) and the risk of interference with physical or mental functioning (disease severity).1,13-14 Investigators apply these concepts in studies involving prevention or asymptomatic conditions, including initial hypertension or cardiovascular disease screening, if the yex pectinternal motivators match or exceed overtsymptoms’ influence on medical outcomes.12,17 A recent meta-analysis of 27 investigations offers that people who believe diabetes is more dangerous are more compliant with drug regimens, but those who do not describe diabetes as severe are on average 22% less likely to be adherent.10 There is similar information on perceived susceptibility and medication-taking behaviors. Notably, findings show that individuals with higher adherence have elevated awareness of susceptibility to medical complications in the future.14 Inaccurate or biased perceptions of disease severity or of one’s susceptibility to health consequences of the disease may lead to unhealthy decisions.
1.1.2. Time perspective
There is potential that time perspective, working as a backdrop for health beliefs, influences the strength and direction of associations with several health behaviors and motivates medication adherence. Time perspective characterizes whether an individual has an orientation toward the present or future.18 This motivator represents a person's subconscious way of making sense of experiences from the past, prioritizing actions in the present, and setting goals for the future.18 Among supporting evidence, adults with elevated future time perspectives have reported better exercise habits,19-20 regular condom use for HIV prevention,20 less substance abuse,20 better psychological well-being, effective behavioral coping, and higher sense of control.21 On the other hand, individuals whose prominent time perspective emphasizes the present, and particularly those whose decision-making process can be motivated by immediate gratification or a strict belief in predetermined fate, more often endorse more substance abuse, risky sexual practices,20 problem gambling,22 less sense of control, more negative affect, and use of angry or maladaptive coping.21 In effect, a person with a dominant future outlook may invest energies toward anticipated long-term consequences and healthier outcomes, whereas those with predominantly present time perspectives may not prioritize behaviors according to similar uncertain or delayed outcomes.
Time perspective may further add context to how we understand motivations underlying medication-taking behaviors. For example, individuals with a dominant present-hedonistic outlook may be less adherent because they make immediate gratification and avoiding discomfort their priorities; nonadherence may minimize inconvenience, undesired lifestyle changes or side effects. Similarly, people with present-fatalistic outlooks, denoted by a strong belief in predetermined fate, may have little faith that efforts at better adherence will improve their current or future health. Lastly, those with more future-oriented time perspectives may invest their daily energies toward lifestyle changes that can improve health status over time.
1.2. Research Questions
In this study, we tested associations between measures of time perspective, health beliefs, and medication adherence. We hypothesized that health beliefs regarding disease severity and susceptibility would be proximate determinants of medication adherence, and that time perspective would in turn influence beliefs regarding disease severity and susceptibility. We sought to answer two questions with mediation analyses: Is time perspective directly associated with medication adherence among participants with hypertension or diabetes? Is time perspective indirectly associated with medication adherence through beliefs about disease severity and susceptibility to complications?
2. Methods
We conducted our study in three cities near Washington, D. C. - Silver Spring, Maryland; Hagerstown, Maryland; and Martinsburg, West Virginia. To recruit multicultural community samples, we surveyed patrons of beauty shops and barbershops in ethnically-diverse neighborhoods, including those that were working-class and more affluent. We chose to collect data in community settings rather than clinical settings to reduce the possible incentive to exaggerate reports of adherence in efforts to appease care providers. We met with patrons to explain the study, determine eligibility, and obtain verbal informed consent. The inclusion criteria were being 18-years-old or older, being literate in English, and being able to provide informed verbal consent. Study protocol and informed consent procedures were approved by our Office of Human Subjects Research.
Participants completed a 6-page written questionnaire on demographic characteristics and three subscales of the Zimbardo Time Perspective Inventory (ZTPI).18 We asked people who reported having either hypertension or diabetes to complete additional questions on health beliefs, use of medications, and the Morisky Medication Adherence Scale (MMAS).23 Of 791 participants, 268 reported that a physician had diagnosed them with hypertension or diabetes, of whom 178 individuals reported taking medications for either or both conditions at the time of the survey.
2.1. Measures
2.1.1. Medication adherence
The MMAS has four items to assess the degree of medication adherence. The questions ask, "Do you ever forget to take your medicine? Are you careless at times about taking your medicine? When you feel better do you sometimes stop taking your medicine? Sometimes if you feel worse when you take the medicine, do you stop taking it?" Participants respond either “yes” or “no” for items, providing a total score up to 4. Responses are then reverse coded to produce five categorical levels (0 = completely nonadherent, 1 = slightly adherent, 2 = adherent on average, 3 = mostly adherent, 4 = completely adherent). The four-item MMAS possesses admittedly marginal internal reliability with C ronbach’s alph a ratings of .60 among hypertension responses and .48 among diabetes responses. However, the scale has been a mainstay in clinical research, and has demonstrated construct and predictive validity for self-reported for hypertension status in hospital and community studies. 24-26
2.1.2. Health beliefs
The disease severity item asks, "Which of the following statements best describes your view of high blood pressure?" People selected one of four possible answers (1 = a serious problem, 2 = a minor problem, 3= a somewhat important problem, 4 = the least of my worries). The susceptibility item is "High blood pressure can increase a person’s risk of having stroke, heart trouble, or kidney failure in the future. Which of the following statements best describes how you think about your high blood pressure?" Individuals respond by endorsing one of four items (1 = hardly ever think about health and hypertension, 2 = sometimes think about health and hypertension but do not worry, 3 = often think about how hypertension affected health and sometimes worry, 4 = worry a lot about how high blood pressure might affect future health).
The study focused on disease severity and susceptibility based on the example of contemporary medication adherence studies.1, 10, 14 We reworded item stems to evaluate perception of severity and susceptibility related to diabetes in identical ways. Both sets of responses, including the reverse coded items, served as categorical variables. Both measures had face validity. Perceived susceptibility also had evidence of construct validity, as 25.6% of those who reported their health as fair or poor responded that they worried a lot about how their condition might affect their future health, compared to 18.2% of those who reported good health, and 10.7% of those who reported excellent or very good health (p = 0.06 by Jonckherre-Terpstra test).27
2.1.3. Time perspective
The three ZPTI subscales include 37 items that assess an individual’s orientation to present-hedonistic, present-fatalistic, and future time perspectives. The present-hedonistic subscale has 15 items that measure being spontaneous, taking risks, and seeking pleasure (i.e. "Taking risks keeps my life from becoming boring"). The present-fatalistic subscale has 9 items evaluating the sense that one does not control his or her fate (i.e. "Often luck pays off better than hard work"). Finally, the future subscale has 13 items that assess the importance of planning and considering consequences in a participant’s life (i.e. "I keep working at difficult uninteresting tasks if they will help me get ahead"). Responses used a 5-point Likert scale ranging from very untrue to very true. Answers are averaged and reverse coded when necessary so that higher scores (0 to 5) indicate more of the construct. Cronbach’s alpharatings show acceptable internal consistency reliability (present-hedonistic = .80, present-fatalistic = .80, future = .78). Additionally, the ZTPI demonstrates construct validity by its structural relationships with several risk behaviors- including marijuana use,28 hazardous driving,29 and problem gambling.30
2.2. Data Analysis
We first tested associations between time perspective, health beliefs, and participants’ adherence with Spearman correlations to investigate the strength and direction of associations between these variables. Next, we used path analysis to simultaneously test hypothesized associations between continuous predictor variables, categorical mediators, and categorical criterion variables. The mediation analysis included eight variables: medication adherence as the criterion variable; present-hedonistic time perspective score, present-fatalistic time perspective score, and future time perspective score as predictor variables; perception of disease severity and susceptibility to complications as mediators; and age and years of formal education as covariate independent variables. We examined total model fit, with and without time perspective variables, to determine their combined contribution to the model. Our meditational path analysis also tested the direction and magnitude of the direct effect of time perspective (TP) on medication adherence (MA) and indirect effects through health beliefs. Finally, our data munging corrected for missing data by altering "." to −999, as recommended by Muthén and Muthén for completing path analysis in Mplus.31
We employed SAS version 9.3 programs for all preliminary analyses.32 Initial regression and analysis of variance tests verified that medication adherence varied based on time perspective. We used Mplus software for all mediation analyses using p-values below 0.05 and model fit tests using conservative cutoffs for root mean square error of approximation (RMSEA) and comparative fit index (CFI) for rejecting null hypotheses.33
We pooled information from 178 participants with hypertension and diabetes for analysis, thereby treating adherence for antihypertensive and antidiabetic drugs as similar examples of health behaviors for chronic disease management. While each condition has unique treatment considerations, we followed other recent studies investigating hypertension and diabetes simultaneously for a few reasons.1,2,11 First, individuals with these diseases generally experience few symptoms, yet they must take drugs with delayed tangible health benefits. The advantages of adhering on a daily basis accrue over time. Additionally, contemporary literature indicates that managing a chronic diseases requires similar medication-taking behaviors.34-35 Lastly, patients typically administer drugs themselves for diabetes and hypertension, so researchers can generally attribute adherence to an individual’s own decision-making process.15
3. Results
3.1. Participant Characteristics
Of the 178 participants, 162 were assessed on adherence to antihypertensive medications, and 16 were assessed on adherence to diabetes medications. The majority of participants were older women with some college education (Table 1). Individuals on average reported moderately high future scores (mean = 3.67, SE = 0.04) and present-hedonistic scores (mean = 3.16, SE = 0.05), whereas they had slightly lower average scores on the present-fatalistic subscale (mean = 2.63, SE = 0.06). Participants were diverse in health beliefs and medication-taking behaviors. First, 61.4% perceived their disease as a serious problem. Large percentages of participants, 34.4% and 31.9%, respectively, also reported sometimes or often reflecting on future complications. A smaller group, 17.2% or 31 of 178 participants, reported the highest level of perception of susceptibility to complications. Finally, complete medication adherence was prevalent among participants- 59.9% of people reported being completely adherent.
Table 1.
Means, Standard Errors, and Prevalence Percentages for Participant Characteristics
| Variable | Mean ± SE/ Prevalence (%) |
|---|---|
| Age (years) | 62.93 ± 1.20 |
| Years of formal education | 13.99 ± 0.20 |
| Time perspective | |
| Present-hedonistic | 3.16 ± 0.05 |
| Present-fatalistic | 2.63 ± 0.06 |
| Future | 3.67 ± 0.04 |
| Gender | |
| Female | 61.2% |
| Male | 38.8% |
| Racial/ethnic background | |
| White (non-Hispanic origin) | 55.1% |
| Black | 30.3% |
| Asian or Pacific Islander | 2.8% |
| Hispanic | 4.5% |
| Other | 7.3% |
| Perception of disease severity | |
| Least of worries | 5.5% |
| A minor problem | 24.5% |
| A somewhat important problem | 8.6% |
| A serious problem | 61.4% |
| Perception of susceptibility to complications | |
| Hardly ever thought about | 16.4% |
| Sometimes thought about with no worry | 34.4% |
| Often thought about with worry | 31.9% |
| Worried about a lot | 17.2% |
| Medication adherence | |
| Completely nonadherent | 3.7% |
| Slightly adherent | 1.9% |
| Adherent on average | 9.8% |
| Mostly adherent | 24.7% |
| Completely adherent | 59.9% |
Correlation analyses revealed a number of relationships between participant characteristics and time perspective (Table 2). Individuals with higher future scores were more likely younger and had more formal education. People with higher present-fatalistic ratings were more likely older and less well-educated. People with higher present-hedonistic or present-fatalistic scores generally reported lower perceptions of disease severity and susceptibility to complications, in contrast to participants with higher future time perspectives.
Table 2.
Spearman Correlation Coefficients for Predictor Variables and Medication Adherence
| Variable | Age | Formal education |
Present- hedonistic |
Present- fatalistic |
Future | Perceived severity |
Perceived susceptibility |
|---|---|---|---|---|---|---|---|
| Age | |||||||
| Formal education | −0.03 | ||||||
| Present-hedonistic | 0.00 | 0.03 | |||||
| Present-fatalistic | 0.17 | −0.35** | 0.39** | ||||
| Future | −0.20* | 0.26** | −0.14 | −0.48** | |||
| Perceived severity | −0.13 | 0.03 | −0.01 | −0.22* | 0.18* | ||
| Perceived susceptibility | −0.29** | −0.13 | −0.13 | −0.14 | 0.24* | 0.45** | |
| Medication adherence | 0.18* | 0.08 | 0.02 | −0.08 | 0.12 | 0.10 | 0.15 |
p < .05
p < .001
When examining mean scores of responses by time perspective, there were several noteworthy associations (Table 3). There were no clear trends relating to perceived disease severity to time perspective. In contrast, participants’ perceived susceptibility to future complications increased with present-hedonistic or future outlook, where it decreased among individuals with elevated present-fatalistic outlook. Participants who reported high adherence also had higher future scores than those who were less adherent, whereas those who described themselves as only being adherent at times reported higher present-hedonistic scores. The individuals who said they were slightly adherent, as indicated by a 2 on the MMAS, typically endorsed higher present-fatalistic scores.
Table 3.
Mean ± SE for Health Beliefs and Medication Adherence for All Time Perspectives
| Variable | Present- hedonistic |
Present- fatalistic |
Future |
|---|---|---|---|
| Perception of disease severity | |||
| Least of worries | 3.21 ± 0.29 | 3.15 ± 0.29 | 3.57 ± 0.18 |
| A minor problem | 3.31 ± 0.14 | 2.83 ± 0.18 | 3.68 ± 0.14 |
| A somewhat important problem | 3.16 ± 0.09 | 2.78 ± 0.13 | 3.46 ± 0.10 |
| A serious problem | 3.18 ± 0.06 | 2.51 ± 0.08 | 3.75 ± 0.05 |
| Perceived susceptibility to complications | |||
| Hardly ever thought about | 3.28 ± 0.15 | 2.95 ± 0.16 | 3.42 ± 0.12 |
| Sometimes thought about with no worry | 3.21 ± 0.07 | 2.60 ± 0.11 | 3.59 ± 0.08 |
| Often thought about with worry | 3.18 ± 0.08 | 2.60 ± 0.10 | 3.77 ± 0.07 |
| Worried about a lot | 3.06 ± 0.11 | 2.49 ± 0.17 | 3.83 ± 0.09 |
| Medication adherence | |||
| Completely nonadherent | 3.36 ± 0.33 | 3.00 ± 0.45 | 3.03 ± 0.27 |
| Slightly adherent | 2.40 ± 0.65 | 2.19 ± 0.61 | 2.97 ± 0.45 |
| Adherent on average | 3.37 ± 0.15 | 2.95 ± 0.24 | 3.42 ± 0.20 |
| Mostly adherent | 3.12 ± 0.08 | 2.60 ± 0.13 | 3.80 ± 0.07 |
| Completely adherent | 3.20 ± 0.06 | 2.60 ± 0.08 | 3.70 ± 0.05 |
3.2. Total Model Fit
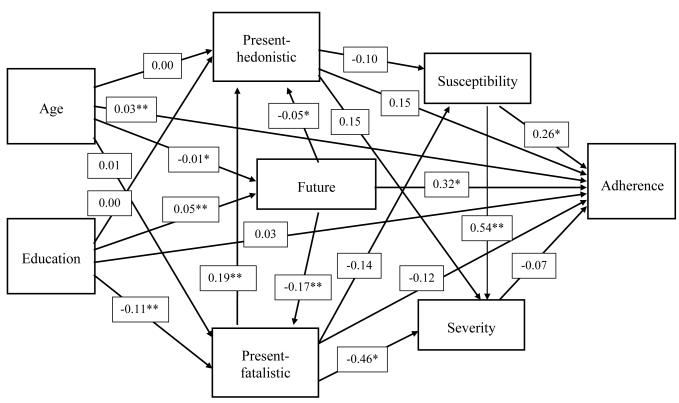
The results demonstrated a good fit (Figure 1. RMSEA = 0.17, 90% CI [0.10, 0.28], p = 0.003; CFI = 0.91), based on conservative considerations of RMSEA estimates below 0.08 and CFI above 0.95 indicate excellent fit.33 We evaluated the impact of including time perspective variables in the model by comparing the fit of weighted least squares models that included or excluded these variables. Time perspective had statistically significant associations and outperformed the null model (γ2 = 73.22, df =15, p-value < 0.0001), supporting that knowing responses on the time perspective variables influenced the probability of change in medication adherence. We translated the categorical data model to probabilities when reporting different adherence levels. Here, we also interpreted data in terms of standard deviations of the underlying latent variable, because probability change differed depending on how participant information compared to the overall distribution of reported medication adherence.
Figure 1.
Path Diagram of the Total Model. * p < .05. ** p < .001.
3.3. Direct effects
3.3.1. Independent variables
Direct effect tests for predictor variables yielded two statistically significant results. Age demonstrated a significant positive association with medication adherence (standardized parameter estimate = 0.03, SE = 0.01, p < 0.001; Figure 1). A one-year increase in age contributed to a 0.03 change in the likelihood of people being more adherent to medication; in effect, the participants’ estimated adherence would be on average 0.30 standard deviations higher than those who were a decade younger. The second notable result was the direct effect of future time perspective on medication adherence. An increase by a single unit in future time perspective (0 – 5 scale) was associated with a 0.32 standard deviation increase in the adherence to medication on average (Figure 2). This direct effect was the only significant association with medication adherence among the three time perspective scales. Future time perspective had the association of largest magnitude in predicting an increase in adherence among all predictor variables in the total model.
3.3.2. Mediator variables
The direct effect tests for mediators produced one statistically significant result. Perception of susceptibility to complications showed a significant positive association with medication adherence (standardized parameter estimate = 0.26, SE = 0.13, p < 0.05). An increase in this health belief by a single unit corresponded with a 0.26 SD increase in the average medication adherence. Alternatively, perception of disease severity was not associated with medication adherence in the model (standardized parameter estimate = −0.07, SE = 0.15, p = 0.64).
3.4. Indirect effects
3.4.1. Present-hedonistic time perspective
The present-hedonistic pathway did not demonstrate a total indirect effect (standardized parameter estimate = −0.04, SE = 0.04, p = 0.39).
3.4.2. Present-fatalistic time perspective
The present-fatalistic pathway did not yield a significant total indirect effect (standardized parameter estimate = −0.01, SE = 0.06, p = 0.93).
3.4.3. Future time perspective
The future pathway did not have a significant total indirect effect (standardized parameter estimate = 0.08, SE = 0.05, p = 0.16), despite its strong direct effect.
4. Discussion and Conclusion
4.1. Discussion
We have demonstrated that time perspective and age are associated with differences in people’s reported use of antihypertensive and antidiabetic drugs. Direct effect tests for these predictor variables revealed structural relationships with similar magnitude and direction. Future time perspective was directly associated with whether they are completely nonadherent versus adherent on average versus completely adherent. Lastly, the average adherence increases with age among people with the chronic diseases. Evidence suggests a downward parabolic association between age and future time perspective, where future outlook increases until middle-age and then decreases among older individuals as the potential length of the future shortens.7 In all, the age effect increases so that older patients’ use of prescribed drugs can be twice as high as that of their younger peers; individuals between 70- and 80-years-old have shown almost 92% success in taking antihypertensive medication.36 Prior work also found the association between age and present-fatalism to have a similar non-linear relationship.7 However, our analysis failed to identify associations between present-fatalistic time perspective andadherence.
4.4. Limitations
Our analysis depends on participants’ responses about health beliefs and medication adherence. We used single-item and 4-item scales with these variables, in order to shorten our questionnaire and to replicate prior investigations conducted outside medical settings.37-39 While brevity makes a self-report instrumental in a community setting, future studies must compare the results with objective outcomes like glycosylated hemoglobin or medical records, and they must employ measures with more optimal psychometric properties, perhaps by including all health belief subdomains and the 8-item MMAS.40 We pooled results from two diseases, treating both as examples of chronic diseases. Other adherence studies have recently provided several rationales for simultaneously investigating hypertension and diabetes management.1-2, 11 We did not ask about the complexity of medication regimens, which may have impacted the results. Studies of larger samples are needed to explore these questions.
One last limitation highlights strengths and weaknesses of results derived from community-based observational studies, that clinical trials have yet to corroborate the effectiveness of targeting time perspective to increase adherence through psychological interventions. More research is needed on whether behavior modi ficati on can increase patients’ future outlook, whether broadly or in chronic disease care specifically. Nonetheless, our findings contribute information amid a growing interest in recruiting more of the general patient population to gain insight into improving medication adherence.10, 41 Similar efforts to collect data in community settings may decrease the likelihood of reporting bias, and may provide more valid results than individual or small-group studies conducted with patients in settings where they receive care.12,24 The ongoing need for broader investigations requires one to interpret the results of categorical data modeling with some caution regarding theoretical implications. The nature of observational studies requires several additional steps, namely replication studies and clinical trials, to say conclusively medication adherence will improve based on tailoring treatment to patients’ psychological motivators.42
4.2. Conclusion
The findings provide the first evidence that time perspective plays a role as a psychological motivator in medication use. Future time perspective demonstrates the associations of largest magnitude in predicting an increase in adherence among all predictor variables. Additionally, the results reveal that a person's subjective perception of susceptibility to complications directly influences adherence, where his or her perception of disease severity was less influential.
4.3. Practice Implications
The findings offer several practical implications, even if surmising generalizable theory requires broader investigation, because the studied concepts add to a growing movement to tailor chronic disease management with psychological frameworks. Nonadherence only increases without intervention.4,8 The best solutions tailor care and scale the intensity of resources or technology, thereby demonstrating both conceptual framework and flexibility, to multiply the effectiveness of chronic disease management plans.43-50 Our study’s major practical implications center on answering two questions- How can ps yc hological const ructs i mpr ove a cli nician’s prescription for hypertension or diabetes? And how are they limited or able to generalize behavior change from one patient to others?
The current study suggests that time perspective serves a previously under-recognized role as a psychological motivator in medication adherence among people with hypertension or diabetes. In regard to improving a clinician’s prescription for hypert ensionordiabetes, this new knowledge can inform how healthcare professionals select and deliver treatment plans. It remains unclear whether or not individuals can permanently modify their orientation. Nevertheless, there is general consensus that many people can use perspectives in some cases and different perspectives in other situations, while others habitually gravitate to one time perspective.7,18-19 Given remaining need for further research, current emphasis must not be on confronting a person about his or her orientation concerning the present or future; but, clinicians can target beliefs about altering health status based on personal action to boost prescription drug use.12
Knowing a pati ent’s time perspective may allow counseling interventions to be better tailored to their needs. For example, brief psychoeducation or technology-based modifications will likely reduce minor challenges to adherence with goal-setting, behavior contracts, or self-monitoring, in those who come with a strong future-oreintation.12,43,51
Conversely, among those with more present orientation, motivational interviewing seems better suited to resolve ambivalence toward nonadherence without them feeling misjudged or rejected by health professionals.52-53 Here again, the emphasis would not be on confronting patients about their time perspective. Clinicians would promote change talk and a therapeutic alliance that build new intrinsic motivation. There are six major components- rolling with resistance, expressing empathy, avoiding arguments, developing discrepancy, promoting self-efficacy, supporting behavior change in the patient-provider relationship.53 Notably, developing discrepancy involves identifying conflict between values (e.g., significance of raising a family) and behavior (e.g. not taking medication that will prevent morbidity and mortality). Additionally, promoting self-efficacy requires celebrating minor successes as people approximate intended health goals.53 There is already some evidence that reinforcement fosters new confidence that encourages behavior change with chronic diseases.54-55 Lastly, the effective transition from contemplative change talk to better adherence relies on a supportive therapeutic climate. Motivational interviewing gives clinicians and patients opportunities to acknowledge and normalize intrinsic and perhaps practical barriers to taking prescribed medications. Health professionals work as collaborators in visits, instead of experts, in order to bolster faith in an individual’s ability; and, by default, they encourage his or her autonomy related to making healthier choices at home. Use of time perspective to tailor counseling interventions is testable in clinical trials.
ACKNOWLEDGEMENTS
The study was supported by the Intramural Research Program, National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health.
I confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Broadbent E, Donkin L, Stroh JC. Illness and treatment perceptions are associated with adherence to medications, diet, and exercise in diabetic patients. Diabetes Care. 2011;34:338–340. doi: 10.2337/dc10-1779. doi:10.2337/dc10-1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schimittdiel JA, Uratsu CS, Karter AJ, Heisler M, Subramanian U, Mangione CM, Selby JV. Why don’t diabetes patients achieve recommended risk factor targets? Poor adherence versus lack of treatment intensification. Journal of General Internal Medicine. 2008;23:588–594. doi: 10.1007/s11606-008-0554-8. doi:10.1007/s11606-008-0554-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dunbar-Jacob J, Mortimer-Stephens MK. Treatment adherence in chronic disease. Journal of Clinical Epidemiology. 2001;54:S57–S60. doi: 10.1016/s0895-4356(01)00457-7. doi.org/10.1016/S0895-4356(01)00457-7. [DOI] [PubMed] [Google Scholar]
- 4.Takiya LN, Peterson AM, Finley RS. Meta-analysis of interventions for medication adherence to antihypertensives. Annals of Pharmacotherapy. 2004;3:1617–1624. doi: 10.1345/aph.1D268. doi:10.1345/aph.1D268. [DOI] [PubMed] [Google Scholar]
- 5.Alhalaiqa F, Deane KHO, Nawafleh AH, Clark A, Gray R. Adherence therapy for medication non-compliant patients with hypertension: A randomised controlled trial. Journal of Human Hypertension. 2012;26:117–126. doi: 10.1038/jhh.2010.133. doi:10.1038/jhh.2010.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hashmi SK, Afridi MB, Abbas K, Sajwani RA, Saleheen D, Frossard PM, Ishaq M, Ambreen A, Ahmad U. Factors associated with adherence to anti-hypertensive treatment in Pakistan. PLoS ONE. 2007;2:e280. doi: 10.1371/journal.pone.0000280. doi:10.1371/journal.pone.0000280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guthrie LC, Butler SC, Ward MM. Time perspective and socioeconomic status: A link tosocioeconomic disparities in health? Social Science & Medicine. 2009;68:2145–2151. doi: 10.1016/j.socscimed.2009.04.004. doi: 10.1016/j.socscimed.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kothawala P, Badamgarav E, Ryu S, Miller RM, Halbert RJ. Systematic review and meta-analysis of real-world adherence to drug therapy for osteoporosis. Mayo Clinic Proceedings. 2007;82:1493–1501. doi: 10.1016/S0025-6196(11)61093-8. doi: 10.4065/82.12.1493. [DOI] [PubMed] [Google Scholar]
- 9.Levy RA. Improving compliance with prescription medications: An important strategy for containing health-care costs. Medical Interface. 1989:34–37. March Issue. [Google Scholar]
- 10.DiMatteo MR, Haskard KB, Williams SL. Health beliefs, disease severity, and patient adherence: A meta-analysis. Medical Care. 2007;45:521–528. doi: 10.1097/MLR.0b013e318032937e. doi:10.1097/MLR.0b013e318032937e. [DOI] [PubMed] [Google Scholar]
- 11.Mann DM, Ponieman D, Leventhal H, Halm EA. Predictors of adherence to diabetes medications: the role of disease and medication beliefs. Journal of Behavioral Medicine. 2009;32:278–284. doi: 10.1007/s10865-009-9202-y. doi: 10.1007/s10865-009-9202-y. [DOI] [PubMed] [Google Scholar]
- 12.Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annual Review of Public Health. 2010;31:399–418. doi: 10.1146/annurev.publhealth.012809.103604. doi: 10.1146/annurev.publhealth.012809.103604. [DOI] [PubMed] [Google Scholar]
- 13.Brown CM, Segal R. The effects of health and treatment perceptions on the use of prescribed medication and home remedies among African American and White American hypertensives. Social Science and Medicine. 1996;43:903–917. doi: 10.1016/0277-9536(95)00434-3. doi:10.1016/0277-9536(95)00434-3. [DOI] [PubMed] [Google Scholar]
- 14.Harvey JN, Lawson VL. The importance of health belief models in determining self-care behaviour in diabetes. Diabetic Medicine. 2009;26:5–13. doi: 10.1111/j.1464-5491.2008.02628.x. doi:10.1111/j.1464-5491.2008.02628.x. [DOI] [PubMed] [Google Scholar]
- 15.Löckenhoff CE, Carstensen LL. Socioeomotional selectivity theory, aging, and health: The increasingly delicate balance between regulating emotions and making tough choices. Journal of Personality. 2004;72:1395–1424. doi: 10.1111/j.1467-6494.2004.00301.x. doi:10.1111/j.1467-6494.2004.00301.x. [DOI] [PubMed] [Google Scholar]
- 16.Janz NK, Becker MH. The health belief model: A decade later. Health Education Behavior. 1984;11:1–47. doi: 10.1177/109019818401100101. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention National Breast and Cervical Cancer Early Detection Program Guidance Manual. 2007 [Google Scholar]
- 18.Zimbardo PG, Boyd JN. Putting time in perspective: A valid, reliable individual-differences metric. Journal of Personality and Social Psychology. 1999;77:1271–1288. doi:10.1037/0022-3514.77.6.1271. [Google Scholar]
- 19.Guthrie LC, Lessl K, Ochi O, Ward MM. Time perspective and smoking, obesity, and exercise in a community sample. American Journal of Health Behavior. 2013;37:171–180. doi: 10.5993/AJHB.37.2.4. doi:10.5993/AJHB.37.2.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Henson JM, Carey MP, Carey KB, Maisto SA. Associations among health behaviors and time perspective in young adults: Model testing with boot-strapping replication. Journal of Behavioral Medicine. 2006;29:127–137. doi: 10.1007/s10865-005-9027-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wills TA, Sandy JM, Yaeger AM. Time perspective and early–onset substance use: A model based on stress-coping theory. Psychology of Addictive Behaviors. 2001;15:118–125. doi: 10.1037//0893-164x.15.2.118. doi:10.1037//0893-164X.15.2.118. [DOI] [PubMed] [Google Scholar]
- 22.Hodgins DC, Engel A. Future time perspective in pathological gamblers. J Nervous Mental Dis. 2002;90:775–780. doi: 10.1097/00005053-200211000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Morisky DE, Green W, Levine DM, et al. Concurrent and predictive validity of a self-reported measure of medication adherence. Medical Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. doi:10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Patel RP, Taylor SD. Factors affecting medication adherence in hypertensive patients. Annals of Pharmacotherapy. 2002;86:40–45. doi: 10.1345/aph.1A046. doi: 10.1345/aph.1A046. [DOI] [PubMed] [Google Scholar]
- 25.Ross S, Walker A, MacLeod MJ. Patient compliance in hypertension: role of illness perceptions and treatment beliefs. Journal of Human Hypertension. 2004;18:607–613. doi: 10.1038/sj.jhh.1001721. doi:10.1038/sj.jhh.1001721. [DOI] [PubMed] [Google Scholar]
- 26.Shea S, Misra D, Francis CK. Predisposing factors for severe, uncontrolled hypertension in an inner-city minority population. New England Journal of Medicine. 1992;327:776–781. doi: 10.1056/NEJM199209103271107. doi:10.1056/NEJM199209103271107. [DOI] [PubMed] [Google Scholar]
- 27.Jonckheere AR. A distribution-free k-sample test again ordered alternatives. Biometrika. 1954;41:133–145. doi: 10.2307/2333011. [Google Scholar]
- 28.Apostolidis T, Fieulaine N, Soule F. Future time perspective as predictor of cannabis use: Exploring the role of substance perception among French adolescents. Addictive Behaviors. 2006;31:2339–2343. doi: 10.1016/j.addbeh.2006.03.008. doi: 10.1016/j.addbeh.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 29.Zimbardo PG, Keough KA, Boyd JN. Present time perspective as a predictor of risky driving. Personality and Individual Differences. 1997;23:1007–1023. doi:10.1016/S0191-8869(97)00113-X. [Google Scholar]
- 30.Hodgins DC, Engel A. Future time perspective in pathological gamblers. Journal of Nervous Mental Disorders. 2002;2002;190:775–780. doi: 10.1097/00005053-200211000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Muthén B, Jo B, Brown CH. Comment on the Barnard, Frangakis, Hill and Rubin article, Principal stratification approach to broken randomized experiments: A case study of school choice vouchers in New York City. Journal of the American Statistical Association. 2003;98:311–314. [Google Scholar]
- 32.Statistical Analysis System Institute Inc . What’s New in SAS® 9.3. SAS Institute Inc; Cary, NC: 2012. [Google Scholar]
- 33.Muthén LK, Muthén BO. Mplus User's Guide. 6th. Muthén & Muthén; Los Angeles, CA: Mplus User’s Guide. Sixth Edition. 1998-2010. [Google Scholar]
- 34.Lau DT, Nau DP. Oral antihyperglycemic medication nonadherence and subsequent hospitalization among individuals with type 2 diabetes. Diabetes Care. 2004;27:2149–2153. doi: 10.2337/diacare.27.9.2149. doi:10.2337/diacare.27.9.2149. [DOI] [PubMed] [Google Scholar]
- 35.Pladevall M, Williams L, Potts LA, Divine G, XH, Elston LJ. Clinical outcomes and adherence to medications measured by claims data in patients with diabetes. Diabetes Care. 2004;27:2800–2805. doi: 10.2337/diacare.27.12.2800. doi:10.2337/diacare.27.12.2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goldbacher EM, Matthews KA. Are psychological characteristics related to risk of the metabolic syndrome? A review of the literature. Annals of Behavioral Medicine. 2007;34:240–252. doi: 10.1007/BF02874549. doi: 10.1007/BF02874549. [DOI] [PubMed] [Google Scholar]
- 37.Atkins L, Fallowfield L. Intentional and non-intentional non-adherence to medication among breast cancer patients. European Journal of Cancer. 2006;42:2271–2276. doi: 10.1016/j.ejca.2006.03.004. doi:10.1016/j.ejca.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 38.Patel RP, Taylor SD. Factors affecting medication adherence in hypertensive patients. Annals of Pharmacotherapy. 2002;86:40–45. doi: 10.1345/aph.1A046. doi: 10.1345/aph.1A046. [DOI] [PubMed] [Google Scholar]
- 39.Wang PS, Bohn RL, Knight E, Glynn RJ, Mogun H, Avorn J. Noncompliance with antihypertensive medications: The impact of depressive symptoms and psychosocial factors. Journal of General Internal Medicine. 2002;17:504–511. doi: 10.1046/j.1525-1497.2002.00406.x. doi: 10.1046/j.1525- 1497.2002.00406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. The Journal of Clinical Hypertension. 2008;10:348–354. doi: 10.1111/j.1751-7176.2008.07572.x. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 41.Pinto BM, Frierson GM, Rabin C, Trunzo JJ, Marcus BH. Home-based physical activity intervention for breast cancer patients. Journal of Clinical Oncology. 2005;23:3577–3587. doi: 10.1200/JCO.2005.03.080. doi:10.1200/JCO.2005.03.080. [DOI] [PubMed] [Google Scholar]
- 42.Rothwell PM. External validity of randomized controlled trials: To whom do the results of this trial apply? Lancet. 2005;365:82–93. doi: 10.1016/S0140-6736(04)17670-8. [DOI] [PubMed] [Google Scholar]
- 43.Zullig LL, Peterson ED, Bosworth HD. Ingredients of successful interventions to improve medication adherence. Journal of the American Medical Association. 2013;310:E1–E2. doi: 10.1001/jama.2013.282818. doi: 10.1001/jama.2013.282818. [DOI] [PubMed] [Google Scholar]
- 44.Kripalani S, Yao X, Haynes B. Interventions to enhance medication adherence in chronic medical conditions: A systematic review. Archive of Internal Medicine. 2007;167:540–549. doi: 10.1001/archinte.167.6.540. doi:10.1001/archinte.167.6.540. [DOI] [PubMed] [Google Scholar]
- 45.Glanz K, Rimer BK, Lewis FM. Health Behavior and Health Education: Theory, Research, and Practice. 3rd Jossey-Bass; San Francisco: 2002. [Google Scholar]
- 46.Glanz K, Rimer BK, Viswanath K. Health Behavior and Health Education: Theory, Research, and Practice. 4th Jossey-Bass; San Francisco: 2008. [Google Scholar]
- 47.Roussos ST, Fawcett SB. A review of collaborative partnerships as a strategy for improving community health. Annual Review of Public Health. 2000;21:369–402. doi: 10.1146/annurev.publhealth.21.1.369. [DOI] [PubMed] [Google Scholar]
- 48.Vogt F, Hall S, Hankins M, Marteau TM. Evaluating three theory-based interventions to increase physicians’ recommendations of smoking cessation services. Health Psychology. 2009;28:174–82. doi: 10.1037/a0013783. [DOI] [PubMed] [Google Scholar]
- 49.Glanz K, Rimer BK, Viswanath K. Health Behavior and Health Education: Theory, Research, and Practice. 4th Jossey-Bass; San Francisco: 2008. [Google Scholar]
- 50.Noar SM, Chabot M, Zimmerman RS. Applying health behavior theory to multiple behavior change: considerations and approaches. Preventative Medicine. 2008;46:275–80. doi: 10.1016/j.ypmed.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 51.Duff AJA, Latchford GJ. Motivational interviewing for adherence problems in cystic fibrosis. Pediatric Pulmonology. 2010;45:211–220. doi: 10.1002/ppul.21103. doi:10.1002/ppul.21103. [DOI] [PubMed] [Google Scholar]
- 52.Borrelli B, Riekert KA, Weinstein A, Rathier L. Brief motivational interviewing as a clinical strategy to promote asthma medication adherence. The Journal of Allergy and Clinical Immunology. 2007;120:1023–1030. doi: 10.1016/j.jaci.2007.08.017. doi: 10.1016/j.jaci.2007.08.017. [DOI] [PubMed] [Google Scholar]
- 53.Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. Guilford Press; New York, NY: 2002. [Google Scholar]
- 54.Brodie D, Inoue A, Shaw DG. Motivational interviewing to change quality of life for people with chronic heart failure: A randomized controlled trial. International Journal of Nursing Studies. 2008;45:489–500. doi: 10.1016/j.ijnurstu.2006.11.009. doi:10.1016/j.ijnurstu.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 55.Schmaling KB, Blume AW, Afari N. A randomized controlled pilot study of motivational interviewing to change attitudes about adherence to medications for asthma. Journal of Clinical Psychology in Medical Settings. 2001;8:167–172. [Google Scholar]