Abstract
Background
Weight gain, insulin-like growth factor-I (IGF-I) levels, and excess exogenous steroid hormone use are putative cancer risk factors, yet their interconnected pathways have not been fully characterized. This cross-sectional study investigated the relationship between plasma IGF-I levels and weight gain according to body mass index (BMI), leptin levels, and exogenous estrogen use among postmenopausal women.
Methods
This study included 794 postmenopausal women who enrolled in an ancillary study of the Women's Health Initiative Observational Study between February 1995 and July 1998. The relationship between IGF-I levels and weight gain was analyzed using ordinal logistic regression. We used the molar ratio of IGF-I to IGF binding protein-3 (IGF-I/IGFBP-3) or circulating IGF-I levels adjusting for IGFBP-3 as a proxy of bioavailable IGF-I. The plasma concentrations were expressed as quartiles.
Results
Among the obese group, women in the third quartile (Q3) of IGF-I and highest quartile of IGF-I/IGFBP-3 were less likely to gain weight (>3% from baseline) than were women in the first quartiles (Q1). Among the normal weight group, women in Q2 and Q3 of IGF-I/IGFBP-3 were 70% less likely than those in Q1 to gain weight. Among current estrogen users, Q3 of IGF-I/IGFBP-3 had 0.5 times the odds of gaining weight than Q1.
Conclusions
Bioavailable IGF-I levels were inversely related to weight gain overall.
Impact
Although weight gain was not consistent with increases in IGF-I levels among postmenopausal women in this report, avoidance of weight gain as a strategy to reduce cancer risk may be recommend.
Keywords: postmenopausal women, insulin-like growth factor-I, exogenous estrogen, weight gain, obesity
Introduction
Nearly 70% of adults in the United States are currently overweight or obese.(1) Increasing obesity prevalence has prompted researchers to focus on the mechanisms linking obesity to cancer, and whether this risk can be reduced by weight loss. Current guidance indicates that a modest weight loss of 5% to 10% is likely to have significant health benefits.(2) Weight loss, regardless of type of intervention, is the main factor that can reduce cancer risk, and many plausible mechanisms are related to the effect of weight loss on cancer-relevant biomarkers.(3,4)
Insulin-like growth factor-I (IGF-I) is a key mitogen that promotes cell cycle progression and elevates risk for cellular transformation by rapid cell turnover.(3,5-7) IGF-I stimulates cellular proliferation and anti-apoptotic effects on certain cell lines that suggest an association with higher cancer risk.(2,4,5) About 80% of IGF-I proteins are bound to IGF binding protein-3 (IGFBP-3), and 19% of IGF-I is bound to other binding proteins, resulting in less than 1% of IGF-I being free, which speaks to the bioactivity of IGF-I.(7-11) The molar ratio of IGF-I to IGFBP-3 roughly represents free, bioavailable IGF-I.(10,12) The IGFs and IGF binding proteins (IGFBPs) are growth hormone (GH)-dependent. Although a decrease in GH in obesity reduces the generation of IGF-I, IGF-I levels can be elevated from excess amounts of adipose tissue.(13) Normal or higher IGF-I levels in obese people also can be attributable to factors other than GH, such as overnutrition and hyperinsulinemia,(10,11,14,15) but the precise mechanisms are unknown.
In obesity, a higher circulating concentration of IGF-I may play a role as an important mediator to stimulate cell proliferation and survival, and weight loss may reduce this risk.(2,4,5,7,16) Previous studies assessing changes in IGF-I levels before and after weight loss in obesity showed inconsistent results. Lower,(9-11) similar,(17-19) and higher(8,12,20-24) IGF-I levels have been observed in obese participants after weight loss. These discrepancies can be explained not only by the uncertainty of the biological mechanisms between adiposity and IGF-I proteins, but by specific analytic choices, including the use of different measures of IGF-I concentration such as total versus bioavailable IGF-I levels, as well as the use of different adiposity measures, such as body mass index (BMI) versus leptin levels.
The relationship between IGF-I and weight loss in postmenopausal women is complicated because adipose tissue promotes estrogen production, and the cancer-promoting role of body fat can be attributed to higher estrogen levels.(5,25) In addition to estrogen's role in regulating cellular differentiation, proliferation, and apoptosis induction,(4) estrogen can mediate the relationship between body fat and cancer by interacting with IGF-I; however, this relationship is not clear. Studies evaluating the association between IGF-I and estrogen following exogenous hormone use have not reported uniform results. IGF-I levels were lower,(26,27) similar,(16,28) and higher (29,30) in hormone-use groups than in nonuse groups. Few studies showed increased(31) or unchanged(7) IGF-I levels after weight loss in postmenopausal women, and these studies did not account for steroid hormone use.
This cross-sectional study investigated the relationship between plasma concentrations of bioavailable IGF-I and weight gain between study enrollment and the third annual visit (AV3), stratified by each of 2 different surrogate markers of adiposity (BMI and leptin) and exogenous estrogen use in postmenopausal women. Bioavailable IGF-I levels were measured using 2 statistical methods: molar ratio of IGF-I/IGFBP-3 and total IGF-I levels adjusting for IGFBP-3 levels. We hypothesized that IGF-I levels are proportionate to weight gain, and that the magnitude to which increased IGF-I levels are associated with weight gain would be more pronounced when BMI and leptin levels are higher and exogenous estrogen is used. To the best of our knowledge, this is the first study to analyze the relationship between IGF-I and weight gain among different weight groups (normal, overweight, and obese groups) according to estrogen use status (never, former, and current use).
Materials and methods
Study population
The study included 794 postmenopausal women enrolled in the ancillary study of the Women's Health Initiative Observation Study (WHI-OS) at the WHI clinical centers located at Baylor College of Medicine in Houston, TX and Wake Forest University School of Medicine in Winston-Salem, NC, and in Greensboro, NC, between February 1995 and July 1998. Participants were followed up to May 2001. Women were eligible for the study if they were 50 to 79 years of age, postmenopausal, planned to reside in the clinical center areas for at least 3 years, and able to provide written consent. The ancillary study included only European-American and African-American women. Of 834 participants, 9 women who did not complete a baseline screening questionnaire were excluded. Another 30 participants were excluded because their study outcomes (i.e., weight changes between baseline and AV3) or covariates at AV3 were not available. After excluding 1 data entry error, 794 participants (96% of 825 participants) were included in this study. Details on the rationale and design of the WHI have been described elsewhere.(32) The study was approved by the institutional review boards at the University of Texas MD Anderson Cancer Center, Baylor College of Medicine, and Wake Forest University School of Medicine.
Data collection
Self-administered questionnaires were used to assess demographic and behavioral factors and medical and reproductive history. Behavioral factors including smoking status, physical activity, and reproductive history such as estrogen use were evaluated at the time of study enrollment (baseline) and AV3. Anthropometric data including weight, height, and waist and hip circumferences were collected at each clinic visit by trained staff.(32) Data quality assurance procedures were established. Reporting or data entry errors were corrected or treated as missing. Discrepancies of answers between main-sub questions or among relevant variables were corrected according to quality assurance procedures.
Estrogen use status (both opposed and unopposed estrogen use) was classified as never, former, and current; former users were defined as those who stopped estrogen use upon enrollment, and current users included those who began to use estrogen both before and after enrollment and still took the drugs at AV3. Each physical activity was assigned a metabolic equivalent (MET) value according to its physical intensity,(33) and total MET·hours·week−1 was estimated by multiplying the MET level for the activity by the hours exercised per week and summing values for all types of activities.(33) MET changes were calculated between baseline and AV3 by subtracting MET values at AV3 from MET values at baseline. Total MET·hours·week−1 was classified into 3 MET groups as 0, 1-10, and >10 METs·hours·week−1, and MET changes were categorized as decreases, no change, and increases in the MET groups at AV3 compared with baseline.
Laboratory methods
Trained phlebotomists collected 3-mL fasting blood samples from each participant at AV3.(34) The samples were sent to clinics’ laboratories for processing, and plasma aliquots were stored at −70°C. The plasma analytes included total IGF-I, IGFBP-3, insulin, and leptin. IGF-I and IGFBP-3 were determined with an enzyme-linked immunosorbent assay kit (Diagnostic Systems Laboratories, Webster, TX), with inter-assay coefficients of variation of 4.16% and 6.01%, respectively. The assays for IGF-I and IGFBP-3 were sensitive to 0.03 ng/ml and 0.04 ng/ml, respectively. Plasma levels of leptin and insulin were measured using a multiplex, bead-based assay kit (Linco Diagnostic Services, St. Charles, MO). Detection limits of the assays for leptin and insulin were 42 pM and 18 pM, respectively.
Outcome variables
The outcome variables were 3 weight-change groups (weight loss, weight maintenance, and weight gain). Weight change was calculated by subtracting weight at AV3 from weight at baseline. Percentages of weight change were estimated by dividing weight changes by baseline body weights and categorized into 3 groups: weight loss, weight maintenance, and weight gain. The range of weight maintenance can be smaller than the amount of weight gain or loss at which risk for obesity-related health effects (e.g., cardiovascular disease and type 2 diabetes) begins to change. Weight maintenance indicated a weight change attributable to fluid fluctuation under normal conditions or measurement errors, and such changes were not clinically meaningful.(35) Weight maintenance was ultimately defined as a weight change of less than or equal to 3% of baseline body weight.(35)
Statistical analysis
Differences in characteristics of participants by weight change groups were evaluated using an omnibus F-test from an analysis of variance for continuous variables and chi-squared statistics for categorical variables. If continuous variables were skewed or had outliers, the Kruskal-Wallis test was implemented. Multicollinearity was assessed by using coefficient of multiple determination (R2), tolerance, and variance-inflation factor for each predictor variable using remaining covariates as its predictors, and no significant multicollinearity was observed.
Molar ratios of IGF-I/IGFBP-3 were created using conversion calculations.(36) As a proxy of bioavailable IGF-I, we used either IGF-I/IGFBP-3 with adjustment of IGF-I or total IGF-I by accounting for IGFBP-3. All plasma hormone levels were expressed as quartiles for the purpose of study. Proportional odds logistic regression was performed to produce ordinal odds ratios (ORs) and 95% confidence intervals (CIs) of IGF-I/IGFBP-3 or IGF-I for weight gain. Ordinal regression assumed that ORs of hormones for the weight-gain group compared to the weight-maintenance and weight-loss groups were the same as ORs for weight-gain and weight-maintenance groups compared to the weight-loss group. The parallel regression assumption was tested with a graphical method. A 2-tailed P value lower than 0.05 was considered significant. R (Version 2.15.1) was used.
Results
The median age was 61 years (range 50-79 years). The majority of participants was non-Hispanic white (81.2%) and had been pregnant at least once (92.2%). More than 50% of participants had more than a high school education (60.7%), no history of oral contraceptive (OC) use (67.0%), and no smoking history (never, 54.2%; former, 38.7%; and current, 7.2%). Most participants had a history of estrogen use (current, 60.7%; former, 14.1%), and 25.2% of participants were nonusers.
Among participants, 55.7% performed more than 1 MET·hours·week−1 at baseline (1-10 METs·hours·week−1, 33.4%; >10 METs·hours·week−1, 22.3%), and 55.3% of participants maintained their baseline MET group during 3-year follow-up. Decreased and increased changes in MET groups at AV3 from baseline occurred among 20.5% and 24.2% of participants, respectively. More than half of participants were obese (28.1%) or overweight (33.4%) at baseline and had lost (22.5%) or gained (36.5%) more than 3% of baseline weight at AV3.
Participant characteristics by weight-change group are summarized in Table 1. Participants who had gained weight at AV3 were more likely to be younger (P=0.0005) and had higher leptin levels at AV3 (P<0.0001). Higher levels of IGF-I/IGFBP-3 at AV3 (P=0.0172) were more likely to be found in the weight-loss group. No other significant differences in characteristics by weight-change groups were noted.
Table 1.
Characteristics of participants enrolled in the ancillary study of the Women's Health Initiative Observational Study at Baylor College of Medicine and Wake Forest University School of Medicine between February 1995 and July 1998
| Variable | Weight Change Groups (n= 794) |
|||||
|---|---|---|---|---|---|---|
| Weight loss (n= 179) |
Weight maintenance (n= 325) |
Weight gain (n= 290) |
||||
| n | (%) | n | (%) | n | (%) | |
| Age in years, median (range)* | 62.0 | (50.0 - 79.0) | 61.0 | (50.0 - 79.0) | 60.0 | (50.0 - 78.0) |
| Ethnicity | ||||||
| Black | 38 | (21.2) | 58 | (17.8) | 53 | (18.3) |
| White | 141 | (78.8) | 267 | (82.2) | 237 | (81.7) |
| Education | ||||||
| ≤ high school | 68 | (38.0) | 119 | (36.6) | 125 | (43.1) |
| > high school | 111 | (62.0) | 206 | (63.4) | 165 | (56.9) |
| Exogenous estrogen use | ||||||
| Never | 51 | (28.5) | 78 | (24.0) | 71 | (24.5) |
| Former | 24 | (13.4) | 46 | (14.2) | 42 | (14.5) |
| Current | 104 | (58.1) | 201 | (61.8) | 177 | (61.0) |
| Oral contraceptive use | ||||||
| No | 127 | (70.9) | 226 | (69.5) | 179 | (61.7) |
| Yes | 52 | (29.1) | 99 | (30.5) | 111 | (38.3) |
| Pregnancy history | ||||||
| No | 15 | (8.4) | 25 | (7.7) | 22 | (7.6) |
| Yes | 164 | (91.6) | 300 | (92.3) | 268 | (92.4) |
| METs at base (METs-hour-week−1), categorical | ||||||
| 0 | 86 | (48.0) | 135 | (41.5) | 131 | (45.2) |
| 1-10 | 61 | (34.1) | 110 | (33.8) | 94 | (32.4) |
| > 10 | 32 | (17.9) | 80 | (24.6) | 65 | (22.4) |
| MET-group change between baseline and AV3 | ||||||
| Decrease in MET group | 35 | (19.6) | 64 | (19.7) | 64 | (22.1) |
| No change in MET group | 99 | (55.3) | 184 | (56.6) | 156 | (53.8) |
| Increase in MET group | 45 | (25.1) | 77 | (23.7) | 70 | (24.1) |
| Smoking status | ||||||
| Never | 98 | (54.7) | 186 | (57.2) | 146 | (50.3) |
| Former | 73 | (40.8) | 118 | (36.3) | 116 | (40.0) |
| Current | 8 | (4.5) | 21 | (6.5) | 28 | (9.7) |
| BMI at baseline, kg/m2, median (range) | 27.8 | (15.4 - 59.5) | 26.6 | (16.1 - 51.6) | 27.5 | (16.2 - 48.4) |
| BMI, kg/m2, categorical | ||||||
| < 25.0 | 61 | (34.1) | 135 | (41.5) | 110 | (37.9) |
| 25.0-29.9 | 51 | (28.5) | 92 | (28.3) | 80 | (27.6) |
| ≥ 30.0 | 67 | (37.4) | 98 | (30.2) | 100 | (34.5) |
| Waist/hip at baseline, ratio, median (range) | 0.794 | (0.665 - 1.095) | 0.796 | (0.640 - 1.116) | 0.799 | (0.623 - 1.062) |
| Waist/hip at baseline, ratio¶, categorical | ||||||
| < 0.7960 | 92 | (51.4) | 164 | (50.5) | 141 | (48.6) |
| ≥ 0.7960 | 87 | (48.6) | 161 | (49.5) | 149 | (51.4) |
| Leptin, pM, median (range)* | 696.0 | (41.0 - 4501.0) | 1054.0 | (64.0 - 4501.0) | 1246.0 | (41.0 - 4501.0) |
| Leptin, pM¶, categorical* | ||||||
| < 1050.0 | 111 | (62.0) | 161 | (49.5) | 124 | (42.8) |
| ≥ 1050.0 | 68 | (38.0) | 164 | (50.5) | 166 | (57.2) |
| Insulin, pM, median (range) | 47.0 | (18.0 - 1014.0) | 47.0 | (20.0 - 1253.0) | 47.0 | (18.0 - 793.0) |
| IGF-I, ng/mL, median (range) | 136.6 | (34.4 - 409.3) | 137.6 | (36.4 - 306.6) | 128.0 | (25.1 - 406.7) |
| IGF-I, categorical | ||||||
| Quartile 1 | 42 | (23.5) | 78 | (24.0) | 79 | (27.2) |
| Quartile 2 | 45 | (25.1) | 73 | (22.5) | 80 | (27.6) |
| Quartile 3 | 44 | (24.6) | 93 | (28.6) | 61 | (21.0) |
| Quartile 4 | 48 | (26.8) | 81 | (24.9) | 70 | (24.1) |
| IGFBP-3, ng/mL, median (range) | 4893.0 | (2649.0 - 7861.0) | 4771.0 | (2212.0 - 7960.0) | 4930.0 | (1032.0 - 8143.0) |
| IGFBP-3, categorical | ||||||
| Quartile 1 | 46 | (25.7) | 82 | (25.2) | 71 | (24.5) |
| Quartile 2 | 42 | (23.5) | 92 | (28.3) | 64 | (22.1) |
| Quartile 3 | 43 | (24.0) | 73 | (22.5) | 82 | (28.3) |
| Quartile 4 | 48 | (26.8) | 78 | (24.0) | 73 | (25.2) |
| IGF-I/IGFBP-3, molar ratio†, median(range)* | 0.106 | (0.040 - 0.220) | 0.102 | (0.044 - 0.275) | 0.094 | (0.032 - 0.244) |
| IGF-I/IGFBP-3, categorical | ||||||
| Quartile 1 | 38 | (21.2) | 72 | (22.2) | 89 | (30.7) |
| Quartile 2 | 41 | (22.9) | 84 | (25.8) | 73 | (25.2) |
| Quartile 3 | 50 | (27.9) | 85 | (26.2) | 63 | (21.7) |
| Quartile 4 | 50 | (27.9) | 84 | (25.8) | 65 | (22.4) |
AV3, annual visit 3; BMI, body mass index; IGF-I, insulin-like growth factor-I; IGFBP-3, IGF-binding protein-3; MET, metabolic equivalent
P<0.05.
Median was used as a cut point to categorize into 2 groups.
Molar ratios of IGF-I to IGFBP-3 were estimated by conversion calculations.
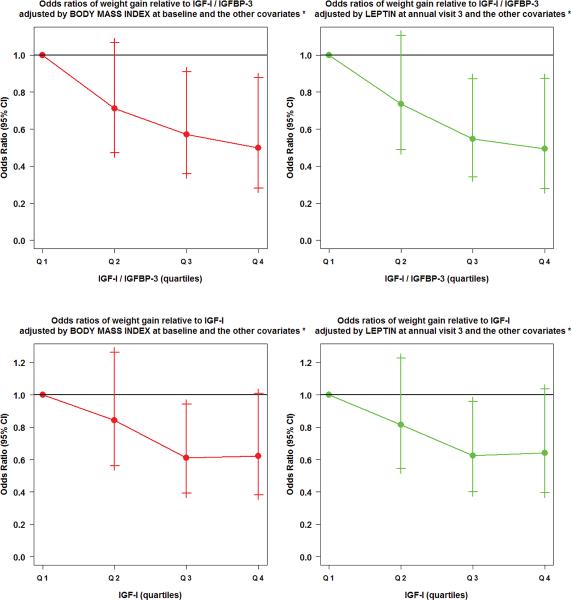
We first examined the relationships between weight gain and IGF-I/IGFBP-3 or IGF-I at AV3 by accounting for each of 2 surrogate adiposity-markers exclusively (BMI and leptin) (Figure 1). In general, those with higher bioavailable IGF-I levels at AV3, whether measured as IGF-I/IGFBP-3 or total IGF-I accounting for IGFBP-3, and whether adjusted for BMI or leptin levels, were less likely to report weight gain. Participants in the 2 highest quartiles (Q3 and Q4) of IGF-I/IGFBP-3 at AV3 were about 0.6 times as likely as the Q1 of IGF-I/IGFBP-3 to gain weight after accounting for either BMI or leptin and other covariates including age, ethnicity, education, estrogen use, OC use, pregnancy, smoking, baseline MET, MET change in group, baseline waist-to-hip ratio (WHR), insulin, and IGF-I.
Figure 1.
Distributions of multivariate ordinal regression odds ratios of weight gain relative to hormones (IGF-I/IGFBP-3 or IGF-I) in participants enrolled in the ancillary study of the Women's Health Initiative Observational Study at Baylor College of Medicine and Wake Forest University School of Medicine between February 1995 and July 1998. *Represents that the other covariates included age, ethnicity, education, exogenous estrogen use, oral contraceptive use, pregnancy history, smoking status, metabolic equivalents (METs) at baseline, MET-group change between baseline and annual visit 3, baseline waist to hip ratio, insulin, and IGF-I or IGFBP-3 when IGF-I/IGFBP-3 or IGF-I was an independent variable, respectively.
Similarly, those in Q3 of IGF-I at AV3 were 40% less likely to have gained weight than those in Q1 of IGF-I at AV3 after adjusting for BMI or leptin and the same covariates, except IGF-I was replaced with IGFBP-3. Findings among those in the highest quartile of IGF-I at AV3 showed similar results to those in Q3, reaching marginal significance. Because IGFs may interact with insulin, especially in patients with diabetes (n=77; 9.7% of 794 participants), we conducted a sensitivity test using data including diabetes history compared with data excluding diabetes history; no apparent differences were identified in univariate and multivariate analyses. In addition, compared with participants who do not have a history of cancer, cancer patients (n=151; 19%) may have different associations between IGF levels and weight gain. We implemented a sensitivity test with participants who reported a history of cancer; there were no significantly different relationships between IGF-I levels and weight gain.
Relationships between weight gain and IGF-I/IGFBP-3 or IGF-I, stratified by BMI or leptin level
We next examined the association of bioavailable IGF-I levels at AV3 with weight gain within different body-size groups as indicated by either BMI or leptin levels (Table 2). The results for bioavailable IGF-I levels in normal-weight and lower-leptin groups were generally similar to those in overweight, obese, and higher-leptin groups. Additionally, the associations of IGF-I/IGFBP-3 with weight gain across weight or leptin groups were largely comparable to those of IGF-I; however, some differences were noted. Participants in Q2 and Q3 of IGF-I/IGFBP-3 in the normal-weight and lower-leptin groups were 0.4 times as likely as those in Q1 of IGF-I/IGFBP-3 to gain weight, but those quartiles of IGF-I were not significant in the normal-weight and lower-leptin groups. In addition, those in the highest quartile of IGF-I/IGFBP-3 in the obese group was 64% less likely to have gained weight than Q1 IGF-I/IGFBP-3 participants (OR=0.36, 95% CI, 0.14-0.93); however, the Q4 of IGF-I in the obese group was not significant. Instead, participants in Q3 of IGF-I were 55% less likely to have gained weight than those in the Q1 of IGF-I in the obese group (OR=0.45, 95% CI, 0.21-0.99).
Table 2.
Multivariate ordinal regression odds ratios of hormones (IGF-I/IGFBP-3 or IGF-I) predicting weight gain by body mass index or leptin level in participants enrolled in the ancillary study of the Women's Health Initiative Observational Study at Baylor College of Medicine and Wake Forest University School of Medicine between February 1995 and July 1998
| Quartile 1 |
Quartile 2 |
Quartile 3 |
Quartile 4 |
||||
|---|---|---|---|---|---|---|---|
| Hormone | OR | OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value |
| IGF-I/IGFBP-3 | |||||||
| Quartile cut point, molar ratio† | ≤ 0.083 | 0.083< - 0.101 | 0.101< - 0.124 | > 0.124 | |||
| n (%) | 199(25) | 198(25) | 198(25) | 199(25) | |||
| BMI at baseline | |||||||
| Normal-weight group* | |||||||
| n (%) | 76(25) | 72(24) | 78(25) | 80(26) | |||
| OR¶ | 1.00‡ | 0.36 (0.17 - 0.75) | 0.01 | 0.38 (0.15 - 0.93) | 0.04 | 0.47 (0.15 - 1.45) | 0.19 |
| Overweight group | |||||||
| n (%) | 50(22) | 66(30) | 49(22) | 58(26) | |||
| OR¶ | 1.00‡ | 1.66 (0.76 - 3.67) | 0.21 | 0.70 (0.27 - 1.79) | 0.45 | 0.73 (0.25 - 2.09) | 0.55 |
| Obese group | |||||||
| n (%) | 73(28) | 60(23) | 71(27) | 61(23) | |||
| OR¶ | 1.00‡ | 0.59 (0.29 - 1.18) | 0.14 | 0.61 (0.29 - 1.25) | 0.18 | 0.36 (0.14 - 0.93) | 0.04 |
| Leptin** | |||||||
| Lower leptin group | |||||||
| n (%) | 107(27) | 106(27) | 91(23) | 92(23) | |||
| OR¶ | 1.00‡ | 0.41 (0.22 - 0.76) | 0.004 | 0.41 (0.19 - 0.87) | 0.02 | 0.43 (0.17 - 1.90) | 0.08 |
| Higher leptin group | |||||||
| n (%) | 92(23) | 92(23) | 107(27) | 107(27) | |||
| OR¶ | 1.00‡ | 1.32 (0.73 - 2.38) | 0.36 | 0.64 (0.34 - 1.18) | 0.15 | 0.50 (0.23 - 1.06) | 0.07 |
| IGF-I | |||||||
| Quartile cut point, ng/L | ≤ 102.1 | 102.1< - 134.6 | 134.6< - 175.5 | >175.5 | |||
| n (%) | 199(25) | 198(25) | 198(25) | 199(25) | |||
| BMI at baseline | |||||||
| Normal-weight group* | |||||||
| n (%) | 76(25) | 73(24) | 77(25) | 80(26) | |||
| OR¶ | 1.00‡ | 0.96 (0.48 - 1.91) | 0.90 | 0.88 (0.42 - 1.84) | 0.73 | 0.87 (0.38 - 1.98) | 0.74 |
| Overweight group | |||||||
| n (%) | 56(25) | 47(21) | 64(29) | 56(25) | |||
| OR¶ | 1.00‡ | 0.52 (0.22 - 1.21) | 0.13 | 0.55 (0.23 - 1.31) | 0.18 | 0.46 (0.17 - 1.22) | 0.12 |
| Obese group | |||||||
| n (%) | 67(25) | 78(29) | 57(22) | 63(24) | |||
| OR¶ | 1.00‡ | 0.98 (0.49 - 1.94) | 0.94 | 0.45 (0.21 - 0.99) | 0.05 | 0.58 (0.25 - 1.36) | 0.22 |
| Leptin** | |||||||
| Lower leptin group | |||||||
| n (%) | 103(26) | 97(24) | 102(26) | 94(24) | |||
| OR¶ | 1.00‡ | 0.65 (0.36 - 1.16) | 0.14 | 0.61 (0.33 - 1.13) | 0.12 | 0.63 (0.32 - 1.23) | 0.18 |
| Higher leptin group | |||||||
| n (%) | 96(24) | 101(25) | 96(24) | 105(26) | |||
| OR¶ | 1.00‡ | 0.97 (0.54 - 1.75) | 0.92 | 0.60 (0.32 - 1.13) | 0.11 | 0.61 (0.30 - 1.24) | 0.18 |
BMI, body mass index; CI, confidence interval; IGF-I, insulin-like growth factor-I; IGFBP-3, IGF-binding protein-3; OR, odds ratio
Molar ratios of IGF-I to IGFBP-3 were estimated by conversion calculations.
The normal-weight group included the lean-weight group (n= 20).
Odds ratios were adjusted for age, ethnicity, education, exogenous estrogen use, oral contraceptive use, pregnancy history, smoking status, metabolic equivalents (METs) at baseline, MET-group change between baseline and annual visit 3, baseline waist to hip ratio, insulin, and IGF-I or IGFBP-3 when IGF-I/IGFBP-3 or IGF-I was an independent variable, respectively.
Leptin was dichotomized using a median (= 1050.0 ng/L) for the purpose of analysis.
Quartile 1 group of IGF-1/IGFBP-3 or IGF-1 was used as referent.
Relationships between weight gain and IGF-I/IGFBP-3 or IGF-I, stratified by exogenous estrogen use
We also evaluated if the relationship between weight gain and IGF-I/IGFBP-3 or IGF-I differed by estrogen use (Table 3). Estrogen use significantly modified the association between IGF-I levels and weight gain (P=0.0498). Among current estrogen users, the Q3 of IGF-I/IGFBP-3, adjusted for either BMI or leptin, was 0.5 times the odds of gaining weight than was Q1 of IGF-I/IGFBP-3; former estrogen users demonstrated a similar relationship between lower IGF-I levels (measured by either IGF-I/IGFBP-3 or total IGF-I adjusted for IGFBP-3) and weight gain, but results of this relationship were opposite in nonusers. Among those who had never used estrogen, the weight-gain group was more likely to be found in Q2 and Q3 of IGF-I/IGFBP-3 and IGF-I, respectively, than in Q1, but small sample size prevented these findings from being significant. Furthermore, regardless of weight-change group (weight loss, weight maintenance, and weight gain), higher IGF-I/IGFBP-3 or IGF-I levels were associated with estrogen nonusers than users, indicating that IGF-I levels are inversely related to estrogen use (Supplemental Table S1).
Table 3.
Multivariate ordinal regression odds ratios of hormones (IGF-I/IGFBP-3 or IGF-I) predicting weight gain by exogenous estrogen use in participants enrolled in the ancillary study of the Women's Health Initiative Observational Study at Baylor College of Medicine and Wake Forest University School of Medicine between February 1995 and July 1998
| Quartile 1 |
Quartile 2 |
Quartile 3 |
Quartile 4 |
||||
|---|---|---|---|---|---|---|---|
| Hormone | OR | OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value |
| Never use | |||||||
| IGF-I/IGFBP-3 (molar ratio†) | |||||||
| n (%) | 23(12) | 36(18) | 57(28) | 84(42) | |||
| OR, adjusted* | 1.00‡ | 1.16 (0.39 - 3.38) | 0.79 | 1.04 (0.33 - 3.28) | 0.95 | 0.90 (0.25 - 3.16) | 0.86 |
| OR, adjusted** | 1.00‡ | 1.27 (0.43 - 3.74) | 0.67 | 1.09 (0.34 - 3.39) | 0.88 | 0.94 (0.26 - 3.33) | 0.93 |
| IGF-I (ng/L) | |||||||
| n (%) | 28(14) | 37(18) | 47(24) | 88(44) | |||
| OR, adjusted* | 1.00‡ | 1.21 (0.43 - 3.45) | 0.71 | 1.55 (0.54 - 4.46) | 0.41 | 1.16 (0.40 - 3.35) | 0.78 |
| OR, adjusted** | 1.00‡ | 0.76 (0.26 - 2.23) | 0.62 | 1.19 (0.41 - 3.45) | 0.75 | 0.82 (0.28 - 2.43) | 0.72 |
| Former use | |||||||
| IGF-I/IGFBP-3 (molar ratio†) | |||||||
| n (%) | 20(18) | 23(21) | 30(27) | 39(35) | |||
| OR, adjusted* | 1.00‡ | 0.69 (0.17 - 2.80) | 0.61 | 0.59 (0.12 - 2.74) | 0.50 | 0.26 (0.04 - 1.52) | 0.14 |
| OR, adjusted** | 1.00‡ | 0.59 (0.14 - 2.35) | 0.46 | 0.40 (0.08 - 1.92) | 0.26 | 0.19 (0.03 - 1.12) | 0.07 |
| IGF-I (ng/L) | |||||||
| n (%) | 22(20) | 22(20) | 33(29) | 35(31) | |||
| OR, adjusted* | 1.00‡ | 0.40 (0.10 - 1.47) | 0.17 | 0.37 (0.11 - 1.26) | 0.12 | 0.50 (0.13 - 1.84) | 0.30 |
| OR, adjusted** | 1.00‡ | 0.40 (0.10 - 1.49) | 0.18 | 0.41 (0.11 - 1.40) | 0.16 | 0.51 (0.13 - 1.91) | 0.32 |
| Current use | |||||||
| IGF-I/IGFBP-3 (molar ratio†) | |||||||
| n (%) | 156(32) | 139(29) | 111(23) | 76(16) | |||
| OR, adjusted* | 1.00‡ | 0.71 (0.44 - 1.15) | 0.16 | 0.53 (0.30 - 0.93) | 0.03 | 0.52 (0.25 - 1.10) | 0.09 |
| OR, adjusted** | 1.00‡ | 0.74 (0.46 - 1.19) | 0.21 | 0.52 (0.29 - 0.92) | 0.02 | 0.52 (0.25 - 1.10) | 0.09 |
| IGF-I (ng/L) | |||||||
| n (%) | 149(31) | 139(29) | 118(24) | 76(16) | |||
| OR, adjusted* | 1.00‡ | 0.93 (0.57 - 1.53) | 0.78 | 0.59 (0.34 - 1.04) | 0.07 | 0.62 (0.32 - 1.20) | 0.16 |
| OR, adjusted** | 1.00‡ | 0.95 (0.58 - 1.55) | 0.83 | 0.61 (0.35 - 1.07) | 0.08 | 0.66 (0.34 - 1.26) | 0.21 |
CI, confidence interval; IGF-I, insulin-like growth factor-I; IGFBP-3, IGF-binding protein-3; OR, odds ratio
Molar ratios of IGF-I to IGFBP-3 were estimated by conversion calculations.
Odds ratios were adjusted for body mass index at baseline and the other covariates (i.e., age, ethnicity, education, oral contraceptive use, pregnancy history, smoking status, metabolic equivalents (METs) at baseline, MET-group change between baseline and annual visit 3, baseline waist to hip ratio, insulin, and IGF-I or IGFBP-3 when IGF-I/IGFBP-3 or IGF-I was an independent variable, respectively).
Odds ratios were adjusted for leptin at annual visit 3 and the other covariates (i.e., age, ethnicity, education, oral contraceptive use, pregnancy history, smoking status, METs at baseline, MET-group change between baseline and annual visit 3, baseline waist to hip ratio, insulin, and IGF-I or IGFBP-3 when IGF-I/IGFBP-3 or IGF-I was an independent variable, respectively).
Quartile 1 group of IGF-I/IGFBP-3 or IGF-1 was used as referent.
Discussion
In this cross-sectional study with a large cohort of participants, we found that bioavailable IGF-I overall was inversely related to weight gain regardless of baseline body weight, leptin level, and estrogen use in postmenopausal women. Most published hormonal studies have found that IGF-I levels (which are lower in obese participants than in normal-weight participants) increase in obese participants after weight loss.(8,12,20-24) This is consistent with the present study results, which show that obese participants had lower IGF-I/IGFBP-3 or IGF-I levels than nonobese participants in the weight-gain and weight-maintenance groups; however, these relationships were reversed in the weight-loss group (i.e., higher IGF-I/IGFBP-3 or IGF-I levels were found in obese than in nonobese participants) (Supplemental Figure S1). We also demonstrated that higher IGF-I levels were associated with weight loss than weight gain across normal, overweight, and obese groups. Previous studies reported that low IGF-I and GH were found in obese populations and increased GH in proportion to IGF-I level after weight loss, indicating that IGF-I cannot be the main inhibitory mechanism accountable for decreases in GH; rather, reduced GH causes low IGF-I levels in obesity.(8,12)
Major regulators of IGF-I production in the liver include GH, diet, malnutrition, and altered glucose mechanism.(15,19) Several studies examining the inverse relationship of IGF-I and insulin resistance in obesity at baseline and after weight loss(20,37) concluded that improved insulin sensitivity following weight loss may up-regulate IGF-I.(14,20) We could not directly assess insulin sensitivity, but an inverse relationship was identified between insulin levels and weight loss (Supplemental Table S2), indicating that lower insulin levels (roughly representing improved insulin sensitivity) were associated with higher IGF-I levels.
Several studies demonstrated that IGF-I levels were higher in obese people and decreased after weight loss;(9-11) these findings are not consistent with our study. These discrepancies can be accounted for by different measures of IGF-I levels such as total and bioavailable IGF-I levels and molar ratios of IGF-I to IGFBP-3. The present study estimated bioavailable IGF-I levels in 2 analytic ways using IGF-I/IGFBP-3 and IGF-I by accounting for IGF-I or IGFBP-3 relatively, and both higher levels of IGF-I/IGFBP-3 and IGF-I were associated with weight loss.
One possible explanation for the varying IGF-I levels measured in obese people may involve different types of adiposity measures. Most studies use BMI, which serves well for dividing individuals' data into size-based groups, but BMI provides no information regarding variation in lean and fat mass. Differences in proportion of lean and fat mass within BMI categories may increase variation in IGF-I levels and contribute to conflicting findings, suggesting that use of an adiposity biomarker such as leptin may result in clearer findings from studies of hormones related to obesity. Some studies reported that IGF-I was inversely related to BMI,(6,8,23) but others did not find a correlation between BMI and IGF-I; rather, a significant relationship between leptin and IGF-I was found.(24,38) We examined whether study results that accounted for BMI differed from those that accounted for leptin, and no significant differences were shown.
Aging in women reduces the level of endocrine hormones including GH-IGFs and estrogen,(26,39) and in postmenopausal women, estrogen is generated by adipose tissues.(5,25) Higher estrogen levels may support the role of body fat in promoting carcinogenesis by interacting with IGF-I in postmenopausal women, but the clear mechanism is unknown. Recent studies have reported an inverse relationship between exogenous estrogen use and IGF-I among postmenopausal women(40-43) suggesting that estrogen suppresses hepatic IGF-I production.(44) Consistent with those of previous studies, our findings show that the IGF-I levels of estrogen nonusers were consistently higher than those of estrogen users in the weight-loss, weight-maintenance, and weight-gain groups (Supplemental Table S1). In addition, previous studies assessing the relationship between IGF-I levels and weight loss in postmenopausal women did not account for exogenous hormone use.(7,31,45) We examined the effect of interactions between exogenous estrogen and IGF-I on weight gain, showing that while there was an inverse relationship between IGF-I levels and weight gain in estrogen users, nonusers experienced somewhat increased IGF-I levels associated with weight gain, but these interactions lacked statistical power (Table 3). We performed subgroup analyses between unopposed (n= 274; 57% of 482 current users) and opposed (n= 208; 43% of 482 current users) estrogen use, and no apparent differences were observed (data not shown).
This study had limitations. We could not assess plasma hormone level changes between baseline and AV3 in this cross-sectional study. Our subanalysis including only extreme weight fluctuations (> 7% weight gain and < 7% weight loss) as outcomes and comparing IGF-I levels confirmed the present findings (higher IGF-I was related to extreme weight loss rather than extreme weight gain) (data not shown). We could not measure the interactions between nutritional data and IGF-I levels related to weight gain due to data unavailability. We acknowledge that with so many analyses, we might have a few false positive results, although the large sample size should reassure a bit against that issue. In any case, results should be interpreted with care, especially when p-values are close to the assumed level of significance.
Few studies(24) have examined the links between IGF-I and weight changes (not only weight loss, but also weight maintenance and weight gain); additionally, no study has normal-weight and overweight comparison groups (and not only obese groups) with which to examine relationships between IGF-I and weight loss across weight groups. Lien et al.(24) showed that obese participants have increased IGF-I levels with decreasing leptin levels and visceral fat mass during weight loss and even after weight regain, but they did not observe these relationships among different weight groups. As we included overweight and normal-weight groups as well as an obese group, our study findings extend those of Lien et al. in that we show consistent results among the other weight groups.
In conclusion, this study demonstrates that although estrogen users have lower overall levels of IGF-I than do nonusers, bioavailable IGF-I is inversely related to weight gain regardless of estrogen use in postmenopausal women, and weight gain is proportionate to insulin levels. Findings suggest potential hypotheses that weight loss may promote improvements in insulin sensitivity, which may up-regulate IGF-I, and that beyond estrogen users' association with lowering levels of IGF-I in general, these relationships are not modified by estrogen use. Cancer-promoting aspects of adipose tissue may be attributable to factors other than IGF-I, and a better understanding of the interconnected pathways of IGF-I, exogenous estrogen, and weight gain may expedite strategies to promote weight loss and maximize the benefits of weight loss, by reducing obesity-related cancer risk, morbidity, and mortality in postmenopausal women.
Supplementary Material
Acknowledgments
We thank Dr. Susan N. Perkins (Cancer Training Branch, Center for Cancer Training, National Cancer Institute, National Institutes of Health), for constructive comments on this manuscript; Heather Hill, a laboratory technician (Division of Cancer Prevention, National Cancer Institute, National Institutes of Health) for assistance with analyzing biological samples. We also thank Dr. Jennifer Hays Grudo (School of Community Medicine, University of Oklahoma at Tulsa) and Dr. Michael Pollak (Departments of Medicine and Oncology, McGill University) for initial collaboration and leadership in this research. The authors thank Dr. Marina Touillaud who assisted in data collection and the staff and leaders of the WHI study for their assistance.
Some of the data for this project were provided from the Women's Health Initiative Observation Study, which is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, and U.S. Department of Health and Human Services through contracts HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201100003C, HHSN268201100004C, and HHSN271201100004C.
Program Office: National Heart, Lung, and Blood Institute, Bethesda, MD: Jacques Rossouw, Shari Ludlam, Dale Burwen, Joan McGowan, Leslie Ford, and Nancy Geller.
Clinical Coordinating Center: Fred Hutchinson Cancer Research Center, Seattle, WA: Garnet Anderson, Ross Prentice, Andrea LaCroix, and Charles Kooperberg.
Investigators and Academic Centers: Brigham and Women's Hospital, Harvard Medical School, Boston, MA: JoAnn E. Manson; MedStar Health Research Institute/Howard University, Washington, DC: Barbara V. Howard; Stanford Prevention Research Center, Stanford, CA: Marcia L. Stefanick; The Ohio State University, Columbus, OH: Rebecca Jackson; University of Arizona, Tucson/Phoenix, AZ: Cynthia A. Thomson; University at Buffalo, Buffalo, NY: Jean Wactawski-Wende; University of Florida, Gainesville/Jacksonville, FL: Marian Limacher; University of Iowa, Iowa City/Davenport, IA: Robert Wallace; University of Pittsburgh, Pittsburgh, PA: Lewis Kuller; Wake Forest University School of Medicine, Winston-Salem, NC: Sally Shumaker.
Women's Health Initiative Memory Study: Wake Forest University School of Medicine, Winston-Salem, NC: Sally Shumaker.
This study was supported by NCI grant (R21 CA81641, PI: J Hays-Grudo)
Footnotes
There are no financial disclosures and conflicts of interest.
References
- 1.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA : the journal of the American Medical Association. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 2.Anderson AS, Caswell S. Obesity management--an opportunity for cancer prevention. The surgeon : journal of the Royal Colleges of Surgeons of Edinburgh and Ireland. 2009;7:282–285. doi: 10.1016/s1479-666x(09)80005-x. [DOI] [PubMed] [Google Scholar]
- 3.Boyd DB. Insulin and cancer. Integrative cancer therapies. 2003;2:315–329. doi: 10.1177/1534735403259152. [DOI] [PubMed] [Google Scholar]
- 4.Fair AM, Montgomery K. Energy balance, physical activity, and cancer risk. Methods Mol Biol. 2009;472:57–88. doi: 10.1007/978-1-60327-492-0_3. [DOI] [PubMed] [Google Scholar]
- 5.Sung MK, Yeon JY, Park SY, Park JH, Choi MS. Obesity-induced metabolic stresses in breast and colon cancer. Annals of the New York Academy of Sciences. 2011;1229:61–68. doi: 10.1111/j.1749-6632.2011.06094.x. [DOI] [PubMed] [Google Scholar]
- 6.Ong K, Kratzsch J, Kiess W, Dunger D. Circulating IGF-I levels in childhood are related to both current body composition and early postnatal growth rate. J Clin Endocrinol Metab. 2002;87:1041–1044. doi: 10.1210/jcem.87.3.8342. [DOI] [PubMed] [Google Scholar]
- 7.Kaaks R, Bellati C, Venturelli E, Rinaldi S, Secreto G, Biessy C, et al. Effects of dietary intervention on IGF-I and IGF-binding proteins, and related alterations in sex steroid metabolism: the Diet and Androgens (DIANA) Randomised Trial. European journal of clinical nutrition. 2003;57:1079–1088. doi: 10.1038/sj.ejcn.1601647. [DOI] [PubMed] [Google Scholar]
- 8.Rasmussen MH, Juul A, Hilsted J. Effect of weight loss on free insulin-like growth factor-I in obese women with hyposomatotropism. Obesity (Silver Spring) 2007;15:879–886. doi: 10.1038/oby.2007.607. [DOI] [PubMed] [Google Scholar]
- 9.Ben Ounis O, Elloumi M, Zouhal H, Makni E, Denguezli M, Amri M, et al. Effect of individualized exercise training combined with diet restriction on inflammatory markers and IGF-1/IGFBP-3 in obese children. Annals of nutrition & metabolism. 2010;56:260–266. doi: 10.1159/000275888. [DOI] [PubMed] [Google Scholar]
- 10.Wabitsch M, Blum WF, Muche R, Heinze E, Haug C, Mayer H, et al. Insulin-like growth factors and their binding proteins before and after weight loss and their associations with hormonal and metabolic parameters in obese adolescent girls. Int J Obes Relat Metab Disord. 1996;20:1073–1080. [PubMed] [Google Scholar]
- 11.De Pergola G, Zamboni M, Pannacciulli N, Turcato E, Giorgino F, Armellini F, et al. Divergent effects of short-term, very-low-calorie diet on insulin-like growth factor-I and insulin-like growth factor binding protein-3 serum concentrations in premenopausal women with obesity. Obesity research. 1998;6:408–415. doi: 10.1002/j.1550-8528.1998.tb00372.x. [DOI] [PubMed] [Google Scholar]
- 12.Rasmussen MH, Hvidberg A, Juul A, Main KM, Gotfredsen A, Skakkebaek NE, et al. Massive weight loss restores 24-hour growth hormone release profiles and serum insulin-like growth factor-I levels in obese subjects. J Clin Endocrinol Metab. 1995;80:1407–1415. doi: 10.1210/jcem.80.4.7536210. [DOI] [PubMed] [Google Scholar]
- 13.Nam SY, Marcus C. Growth hormone and adipocyte function in obesity. Horm Res. 2000;53(Suppl 1):87–97. doi: 10.1159/000053211. [DOI] [PubMed] [Google Scholar]
- 14.Franco C, Bengtsson BA, Johannsson G. The GH/IGF-1 Axis in Obesity: Physiological and Pathological Aspects. Metab Syndr Relat Disord. 2006;4:51–56. doi: 10.1089/met.2006.4.51. [DOI] [PubMed] [Google Scholar]
- 15.Rasmussen MH. Obesity, growth hormone and weight loss. Molecular and cellular endocrinology. 2010;316:147–153. doi: 10.1016/j.mce.2009.08.017. [DOI] [PubMed] [Google Scholar]
- 16.Jernstrom H, Barrett-Connor E. Obesity, weight change, fasting insulin, proinsulin, C-peptide, and insulin-like growth factor-1 levels in women with and without breast cancer: the Rancho Bernardo Study. Journal of women's health & gender-based medicine. 1999;8:1265–1272. doi: 10.1089/jwh.1.1999.8.1265. [DOI] [PubMed] [Google Scholar]
- 17.Rigamonti AE, Agosti F, De Col A, Marazzi N, Lafortuna CL, Cella SG, et al. Changes in plasma levels of ghrelin, leptin, and other hormonal and metabolic parameters following standardized breakfast, lunch, and physical exercise before and after a multidisciplinary weight-reduction intervention in obese adolescents. Journal of endocrinological investigation. 2010;33:633–639. doi: 10.1007/BF03346662. [DOI] [PubMed] [Google Scholar]
- 18.Reinehr T, Panteliadou A, de Sousa G, Andler W. Insulin-like growth factor-I, insulin-like growth factor binding protein-3 and growth in obese children before and after reduction of overweight. Journal of pediatric endocrinology & metabolism : JPEM. 2009;22:225–233. doi: 10.1515/jpem.2009.22.3.225. [DOI] [PubMed] [Google Scholar]
- 19.Butzow TL, Lehtovirta M, Siegberg R, Hovatta O, Koistinen R, Seppala M, et al. The decrease in luteinizing hormone secretion in response to weight reduction is inversely related to the severity of insulin resistance in overweight women. J Clin Endocrinol Metab. 2000;85:3271–3275. doi: 10.1210/jcem.85.9.6821. [DOI] [PubMed] [Google Scholar]
- 20.Belobrajdic DP, Frystyk J, Jeyaratnaganthan N, Espelund U, Flyvbjerg A, Clifton PM, et al. Moderate energy restriction-induced weight loss affects circulating IGF levels independent of dietary composition. Eur J Endocrinol. 2010;162:1075–1082. doi: 10.1530/EJE-10-0062. [DOI] [PubMed] [Google Scholar]
- 21.Rasmussen MH, Wildschiodtz G, Juul A, Hilsted J. Polysomnographic sleep, growth hormone insulin-like growth factor-I axis, leptin, and weight loss. Obesity (Silver Spring) 2008;16:1516–1521. doi: 10.1038/oby.2008.249. [DOI] [PubMed] [Google Scholar]
- 22.Pereira FA, de Castro JA, dos Santos JE, Foss MC, Paula FJ. Impact of marked weight loss induced by bariatric surgery on bone mineral density and remodeling. Brazilian journal of medical and biological research = Revista brasileira de pesquisas medicas e biologicas / Sociedade Brasileira de Biofisica ... [et al.] 2007;40:509–517. doi: 10.1590/s0100-879x2007000400009. [DOI] [PubMed] [Google Scholar]
- 23.Pardina E, Ferrer R, Baena-Fustegueras JA, Lecube A, Fort JM, Vargas V, et al. The relationships between IGF-1 and CRP, NO, leptin, and adiponectin during weight loss in the morbidly obese. Obesity surgery. 2010;20:623–632. doi: 10.1007/s11695-010-0103-5. [DOI] [PubMed] [Google Scholar]
- 24.Lien LF, Haqq AM, Arlotto M, Slentz CA, Muehlbauer MJ, McMahon RL, et al. The STEDMAN project: biophysical, biochemical and metabolic effects of a behavioral weight loss intervention during weight loss, maintenance, and regain. Omics : a journal of integrative biology. 2009;13:21–35. doi: 10.1089/omi.2008.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sedlacek SM, Playdon MC, Wolfe P, McGinley JN, Wisthoff MR, Daeninck EA, et al. Effect of a low fat versus a low carbohydrate weight loss dietary intervention on biomarkers of long term survival in breast cancer patients (‘CHOICE’): study protocol. BMC cancer. 2011;11:287. doi: 10.1186/1471-2407-11-287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bellantoni MF, Vittone J, Campfield AT, Bass KM, Harman SM, Blackman MR. Effects of oral versus transdermal estrogen on the growth hormone/insulin-like growth factor I axis in younger and older postmenopausal women: a clinical research center study. J Clin Endocrinol Metab. 1996;81:2848–2853. doi: 10.1210/jcem.81.8.8768841. [DOI] [PubMed] [Google Scholar]
- 27.Friend KE, Hartman ML, Pezzoli SS, Clasey JL, Thorner MO. Both oral and transdermal estrogen increase growth hormone release in postmenopausal women--a clinical research center study. J Clin Endocrinol Metab. 1996;81:2250–2256. doi: 10.1210/jcem.81.6.8964860. [DOI] [PubMed] [Google Scholar]
- 28.Bellantoni MF, Harman SM, Cho DE, Blackman MR. Effects of progestin-opposed transdermal estrogen administration on growth hormone and insulin-like growth factor-I in postmenopausal women of different ages. J Clin Endocrinol Metab. 1991;72:172–178. doi: 10.1210/jcem-72-1-172. [DOI] [PubMed] [Google Scholar]
- 29.Weissberger AJ, Ho KK, Lazarus L. Contrasting effects of oral and transdermal routes of estrogen replacement therapy on 24-hour growth hormone (GH) secretion, insulin-like growth factor I, and GH-binding protein in postmenopausal women. J Clin Endocrinol Metab. 1991;72:374–381. doi: 10.1210/jcem-72-2-374. [DOI] [PubMed] [Google Scholar]
- 30.Ho KK, Weissberger AJ. Impact of short-term estrogen administration on growth hormone secretion and action: distinct route-dependent effects on connective and bone tissue metabolism. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research. 1992;7:821–827. doi: 10.1002/jbmr.5650070711. [DOI] [PubMed] [Google Scholar]
- 31.Orsatti FL, Nahas EA, Maesta N, Nahas-Neto J, Burini RC. Plasma hormones, muscle mass and strength in resistance-trained postmenopausal women. Maturitas. 2008;59:394–404. doi: 10.1016/j.maturitas.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 32.The Women's Health Initiative Study Group Design of the Women's Health Initiative clinical trial and observational study. The Women's Health Initiative Study Group. Controlled clinical trials. 1998;19:61–109. doi: 10.1016/s0197-2456(97)00078-0. [DOI] [PubMed] [Google Scholar]
- 33.McTiernan A, Kooperberg C, White E, Wilcox S, Coates R, Adams-Campbell LL, et al. Recreational physical activity and the risk of breast cancer in postmenopausal women: the Women's Health Initiative Cohort Study. JAMA : the journal of the American Medical Association. 2003;290:1331–1336. doi: 10.1001/jama.290.10.1331. [DOI] [PubMed] [Google Scholar]
- 34.The Women's Health Initiative Study Group WHI Manuals: Volume 2-Procedures. Section 11-Blood and Urine Collection, Processing and Shipment. 1997 http://www.ncbi.nlm.nih.gov/projects/gap/cgibin/document.cgi?study_id=phs000200.v8.p2&phv=161362&phd=2022&pha=&pht=1515&phvf=&phdf=&phaf=&phtf=&dssp=1&consent=&temp=1.
- 35.Stevens J, Truesdale KP, McClain JE, Cai J. The definition of weight maintenance. Int J Obes (Lond) 2006;30:391–399. doi: 10.1038/sj.ijo.0803175. [DOI] [PubMed] [Google Scholar]
- 36.Ma J, Pollak MN, Giovannucci E, Chan JM, Tao Y, Hennekens CH, et al. Prospective study of colorectal cancer risk in men and plasma levels of insulin-like growth factor (IGF)-I and IGF-binding protein-3. Journal of the National Cancer Institute. 1999;91:620–625. doi: 10.1093/jnci/91.7.620. [DOI] [PubMed] [Google Scholar]
- 37.Succurro E, Andreozzi F, Marini MA, Lauro R, Hribal ML, Perticone F, et al. Low plasma insulin-like growth factor-1 levels are associated with reduced insulin sensitivity and increased insulin secretion in nondiabetic subjects. Nutrition, metabolism, and cardiovascular diseases : NMCD. 2009;19:713–719. doi: 10.1016/j.numecd.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 38.Bini V, Igli Baroncelli G, Papi F, Celi F, Saggese G, Falorni A. Relationships of serum leptin levels with biochemical markers of bone turnover and with growth factors in normal weight and overweight children. Horm Res. 2004;61:170–175. doi: 10.1159/000076134. [DOI] [PubMed] [Google Scholar]
- 39.Milewicz A, Tworowska U, Demissie M. Menopausal obesity--myth or fact? Climacteric : the journal of the International Menopause Society. 2001;4:273–283. [PubMed] [Google Scholar]
- 40.Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer. 2004;4:579–591. doi: 10.1038/nrc1408. [DOI] [PubMed] [Google Scholar]
- 41.McCormack VA, Dowsett M, Folkerd E, Johnson N, Palles C, Coupland B, et al. Sex steroids, growth factors and mammographic density: a cross-sectional study of UK postmenopausal Caucasian and Afro-Caribbean women. Breast Cancer Res. 2009;11:R38. doi: 10.1186/bcr2325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boyd NF, Stone J, Martin LJ, Jong R, Fishell E, Yaffe M, et al. The association of breast mitogens with mammographic densities. British journal of cancer. 2002;87:876–882. doi: 10.1038/sj.bjc.6600537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aiello EJ, Tworoger SS, Yasui Y, Stanczyk FZ, Potter J, Ulrich CM, et al. Associations among circulating sex hormones, insulin-like growth factor, lipids, and mammographic density in postmenopausal women. Cancer Epidemiol Biomarkers Prev. 2005;14:1411–1417. doi: 10.1158/1055-9965.EPI-04-0920. [DOI] [PubMed] [Google Scholar]
- 44.Jorgensen JO, Christensen JJ, Krag M, Fisker S, Ovesen P, Christiansen JS. Serum insulin-like growth factor I levels in growth hormone-deficient adults: influence of sex steroids. Horm Res. 2004;62(Suppl 1):73–76. doi: 10.1159/000080762. [DOI] [PubMed] [Google Scholar]
- 45.Thompson JL, Butterfield GE, Gylfadottir UK, Yesavage J, Marcus R, Hintz RL, et al. Effects of human growth hormone, insulin-like growth factor I, and diet and exercise on body composition of obese postmenopausal women. J Clin Endocrinol Metab. 1998;83:1477–1484. doi: 10.1210/jcem.83.5.4826. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.