Abstract
Background:
Voluntary counseling and testing (VCT) is a cost-effective tool to prevent and control human immunodeficiency virus (HIV)/acquired immodeficiency syndrome. Community conversation (CC) is a community-based strategy meant to enhance the community utilization of VCT. However, the role of CC in VCT service uptake has not yet been evaluated.
Aims:
This study was conducted to compare VCT service utilization between rural communities with well CC performance and rural communities with poor CC performance in Shebedino woreda.
Materials and Methods:
A cross-sectional comparative community-based study was conducted in 2010 among 462 selected adults in the age bracket of 15-59 years. VCT service uptake was compared between well CC performing communities and poor CC performing communities using two sample test of proportion. Predictors of VCT service uptake were determined using logistic regression model.
Results:
Uptake of VCT service and the related VCT knowledge were statistically higher in well CC performing communities than poor CC performing communities; [73.0% vs. 54.1%, P < 0.001) vs. 97.8% vs. 93.8%, P = 0.034]. CC, VCT knowledge, and knowledge on HIV transmission were independent predictors of VCT service utilization.
Conclusion:
Uptake of VCT service is higher in well CC performing communities. Emphasis should be given to strengthen CC performance.
Keywords: Community conversation, HIV/AIDS, Voluntary counseling and testing, Ethiopia
Introduction
Voluntary counseling and testing (VCT) is a cost-effective tool to prevent and control human immunodeficiency virus (HIV)/acquired immodeficiency syndrome (AIDS). It encourages people to know their HIV status, thus helping to break the chain of transmission of the infection. VCT is also a key entry point to care and support services for people living with HIV/AIDS.[1]
VCT service utilization is low in Ethiopia, only 20% of women and 21% of men have been tested for HIV and received the results in 2005 indicating that many people living with HIV/AIDS in Ethiopia do not know their HIV status.[2] However, to foster attitudes and behaviors that promote counseling and testing among community leaders and in communities, a community-based strategy called “community conversation”(CC) was introduced in Ethiopia in 2002.[1,3]
CC is a facilitated interactive process which brings people together and engages them to explore the underlying causes fuelling the HIV/AIDS epidemics in their environment.[3] It focuses on generating action plans. It has explicit problem solving agenda, aiming to incite critical thinking that enables people to formulate solutions to local issues.[4,5] CC is a process for dialogue and decision-making-for communities to investigate into the deep causes of the epidemic in their lives and generate their own solutions.[6] CC is one of the nation's strategies to increase VCT service utilization.[1] Its main purpose is empowerment of communities and individuals to identify and address issues that are important to them.[3,7]
The facilitators of CC in Ethiopia are Health Extension Workers (HEWs) who shared the ethnicity, home language, and had grown up in the same district of the CC participants. HEWs were trained on the facilitation skills and CC methodology frame work. They conduct CC every 2 weeks for a cross section of 36-40 people from the community-men and women, old and young, people living with HIV/AIDS and those who are not infected, religious, community and traditional leaders, and members of the community at large.[6] A CC participant graduates after completing 24 CC sessions.[8]
Aided by skilled facilitators from their own communities, people openly talk to each other and explore the implications of HIV/AIDS, identify their own cultural norms and values that are fuelling the epidemic and the social capital within the community to overcome them.[5,6]
During CC session, the facilitator poses questions related to HIV including but not limited to driving factors for HIV transmission in the community, health, social, economical, and psychological impacts of HIV/AIDS and role of VCT in HIV care and prevention.[6,8]
As problems and solutions are discussed, the facilitator guides the participants to develop concrete action plans. The facilitator convenes additional conversations on an on-going basis to discuss how implementing the action plans is going.
Though studies that related CC with HIV or VCT are scarce, the role of CC in increasing HIV-related competence has been demonstrated in one qualitative study conducted in Zimbabwe.[4] Also as a result of CC in Ethiopia, it is reported that CC participants have travelled long distance to the nearest health facility to get tested for HIV and convinced their partner to get tested. Moreover, CC is said to bring positive change with regard to receiving HIV test before marriage.[6] It also is a powerful tool to reduce risk behavior toward HIV and promotes HIV prevention and stigma reduction.[3,9]
However, the role of CC on VCT service uptake has not yet been evaluated using sound scientific methods in Ethiopia. This study was designed to compare VCT service utilization between rural communities with well CC performance and rural communities with poor CC performance in Shebedino woreda, South Ethiopia.
Materials and Methods
The study was conducted in Shebedino woreda, Sidamo zone, Southern Nations Nationalities and Peoples Region, Ethiopia in November 2010. Sidama zone is situated 274 km south of Addis Ababa. The woreda comprises of 35 kebeles (3 urban kebeles and 32 rural kebeles).
A cross-sectional comparative study was conducted among adult population who were in the age range; 15-59 years in the selected six kebeles (kebele is the smallest administrative unit) of the Woreda. The study protocol was approved by Research Ethical Committee of the School of Public Health, Addis Ababa University. Data were collected after securing informed consent.
Sample size and sampling
Sample size was calculated using Epi Info sample size calculator (Epi Info 3.3.2, CDC) for two population proportion by taking proportion of VCT service utilization of 20.1% among communities with well CC performance.[10] A 10% difference was assumed between well and poor CC kebeles so that the proportion of VCT service utilization among poor CC communities was set at 10.1%. Other assumptions considered were: 95% confidence level, 80% power, 5% level of significance, and the ratio of well to poor CC(r) = 1. The final sample size was 321 for each group. The source population was 15-59 years old population residing in rural kebeles implementing CC in Shebedino woreda.
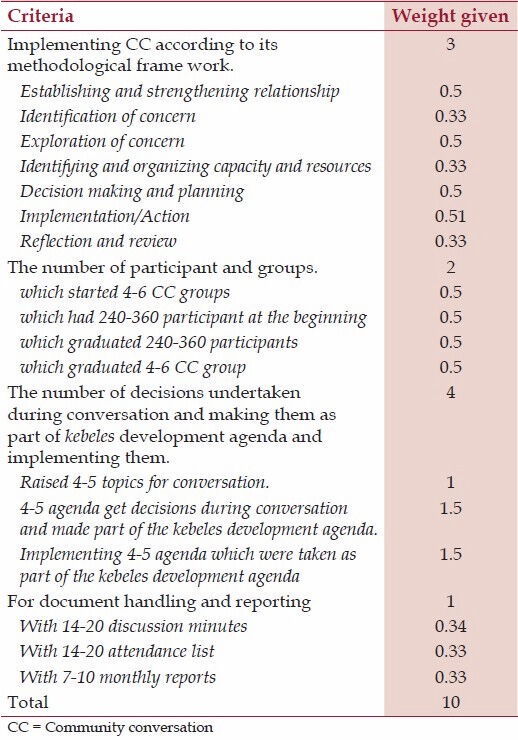
Rural kebeles were classified into well and poor CC groups based on their major activities on CC performance. Four major criteria (CC methodology frame work, number of participants, number of CC groups, number of decisions undertaken, document handling, and reporting) were considered to classify the study kebeles into well and poor CC groups. The CC performance of each kebele was evaluated by giving weights to each criterion. Accordingly, all kebeles were evaluated out of 10 (the sum of scores to each activity under the four criteria). A kebele was labeled as well performing CC group if its CC score was equal to or greater than the median value of 4.75; otherwise, it was labeled as a poor CC performing kebele. Detail descriptions on the criteria used to score CC is annexed [Table 1].
Table 1.
List of criteria and weight used to classify kebeles into poor and well CC groups
Out of 35 rural kebeles in the Woreda, 25 qualified to be sampled (seven kebeles had stopped CC). The 25 rural kebeles were stratified by their CC status into well (n = 13) and poor (n = 12). Then, kebeles under the two strata (well and poor) were further stratified into proximal (within 5 km), medium (5-10 km), and distal (more than 10 km) by their distance from the Woreda capital. One kebele was selected from each stratum by lottery method. From each selected kebele, proportional number individuals were included into the sample. Then households from the selected kebeles were selected using systematic random sampling technique through a door to door survey. From the selected households, data were collected from the selected adults in the age bracket of 15-59 years. When there were more than one eligible study participants, one was selected by lottery method. A structured questionnaire was used to collect the data. The tool was translated into local language (Sidamgna). Trained diploma nurses who are bilingual were recruited as data collectors. Same gender interviewers were used to decrease discomfort as some of the questions were about personal sexual lifestyle. Pretest was undertaken on 15% the sample before the actual data collection.
Data were entered into Epi Info 3.3.2 as part of data quality management and analyzed using SPSS version 16.0. Upon checking completeness and consistency of responses, 2.2% questionnaires were excluded from the analysis because they were partially filled.
Variables
The magnitude of VCT service uptake was determined by counting the number of study participants who underwent HIV test on voluntary basis. Risky sexual behavior was documented if the study participant had at least one of the following: Sex without condom, sex with multiple partners, inconsistent condom use, and sex after alcohol use. To measure knowledge, comprehensive set of knowledge questions was posed. Correct responses were given 1 and incorrect responses 0. The responses were summed for each study participant. Those who scored above the mean were considered as knowledgeable.
Statistical analysis
Percentages were used to determine the magnitude of knowledge and uptake of VCT service. A two sample proportion test was used to test the presence of statistical difference in the proportion of VCT service utilization between the two CC groups.
To determine the association between different predictors and VCT service utilization (dependent variable), a logistic regression model was employed. First, each predictor was entered into a separate binary logistic regression model to determine the crude effect of each variable on VCT uptake. Second, to account for the effect of confounders, a multiple logistic regression model was fitted with all predictors that have P ≤ 0.3 in the bivariate model. Eventually, only those variables that remained significant at P ≤ 0.05 in the final model were retained as independent predictors of VCT service uptake.
Results
Description of the study population
A total of 452 study participants completed the interview giving a response rate of 97.8%. The main reason for nonresponse was being busy in farming activities (60%). Nonresponse rate was not different by CC status.
Of the 452 who participated in the study, 226 (50.0%) were from well CC performing kebeles and 226 (50.0%) from poor CC performing kebeles. Female study participants constituted 53.5% in well and 50.0% in poor CC performing kebeles. Majority of the study participants; 119 (52.7%) in well and 109 (48.2%) in poor CC performing kebeles were in the age range of 15-24 years.
With respect to educational status, near to half of the study participants in well (44.7%) and in poor (46.9%) CC groups had no formal education. Regarding religion, about [183 (81.0%) vs. 180 (79.6%)] of the study participants were protestant in poor and well CC groups. Almost all of the study participants; 218 (96.5%) in well and 216 (95.6%) in poor CC groups were Sidama in ethnicity. Married study participants were [141 (62.4%) vs. 121 (53.5%)] followed by single [84 (37.4%) vs. 102 (45.1%)] in poor and well CC groups, respectively. Of the study participants; (37.6% vs. 30.5%) were students in occupation, followed by housewives (27.0% vs. 26.5%) and farmers (23.0% vs. 23.7%) in well and poor CC groups, respectively.
Majority of the study participants; [146 (64.6%) in well and 160 (70.6%)] in poor CC performing kebeles had started sexual intercourse by the time of data collection [Table 2].
Table 2.
The sociodemographic and sexual history of the study participants
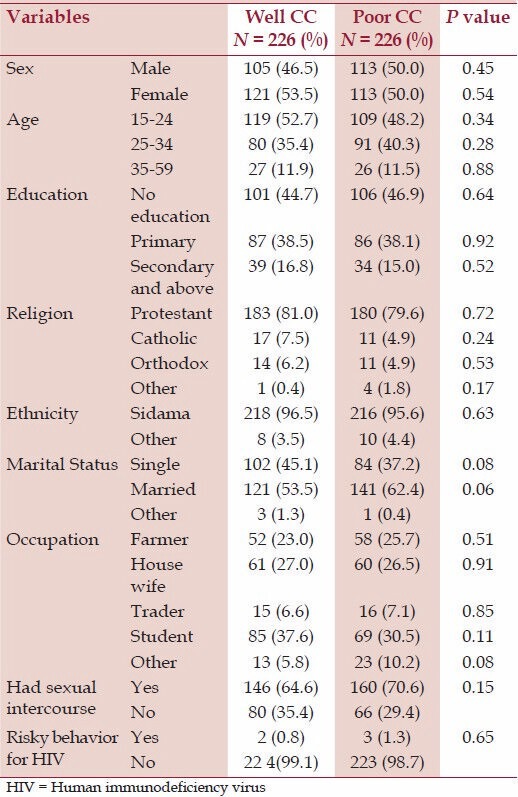
To determine the comparability of the study participants between well and poor CC performing kebeles, two sample test of proportion for major sociodemographic factors was computed. Accordingly, the study participants in well and poor CC performing kebeles were not statistically different (P > 0.05) by sex, age, religion, ethnicity, education, marital status, occupation, sexual practice, age at first sex, condom utilization, and risky behavior for HIV. Therefore, the study participants in well and poor CC performing kebeles were comparable [Table 2].
VCT Service utilization among the study participants
Significant number of study participants from well CC group compared with participants from poor CC group knew that VCT is important to break the chain of HIV spread (97.8% vs.93.8%, P = 0.034).
More study participants from well CC performing kebeles utilized HIV voluntary counseling and testing service than from poor CC performing kebeles (73.0% vs. 54.9%, P < 0.001). When the study was conducted, the operation period for CC was about 8 years. More than 97% of the study participants who utilized VCT did so with in 4 years before the survey which is 4 years well after the initiation of CC.
Predictors of VCT service uptake
The association of different predictors with VCT service uptake was assessed by fitting them into a logistic regression model. Accordingly, the odds of HIV test uptake for participants from well CC performing kebeles was found to be 2.5 times that for participants from poor CC performing kebeles [Adjusted Odds Ratio (AOR) (95% confidence interval (CI) = 2.51(1.63,3.86)]. And also those found in the age bracket of 15-24 years had the higher odds of HIV test uptake than those between 35 and 59 years [AOR (95% CI) = 3.14(1.37, 7.20)]. The odds of HIV test uptake was about three times higher in singles than in married [AOR (95% CI) = 2.55 (1.09, 5.99)]. Similarly, the odds of HIV test uptake was 3.36 times higher in traders than in farmers [AOR (95% CI) = 3.36 (1.03, 10.96)] [Table 3]. Also, the participants' knowledge about the benefits of VCT and the ways of HIV transmission were predictors of VCT service uptake with their corresponding estimates of [AOR (95% CI) = 3.51(1.15, 10.67)] and [AOR (95% CI) = 2.03(1.05, 3.91)], respectively [Table 3].
Table 3.
Factors associated with voluntary counseling and testing uptake (n = 452)
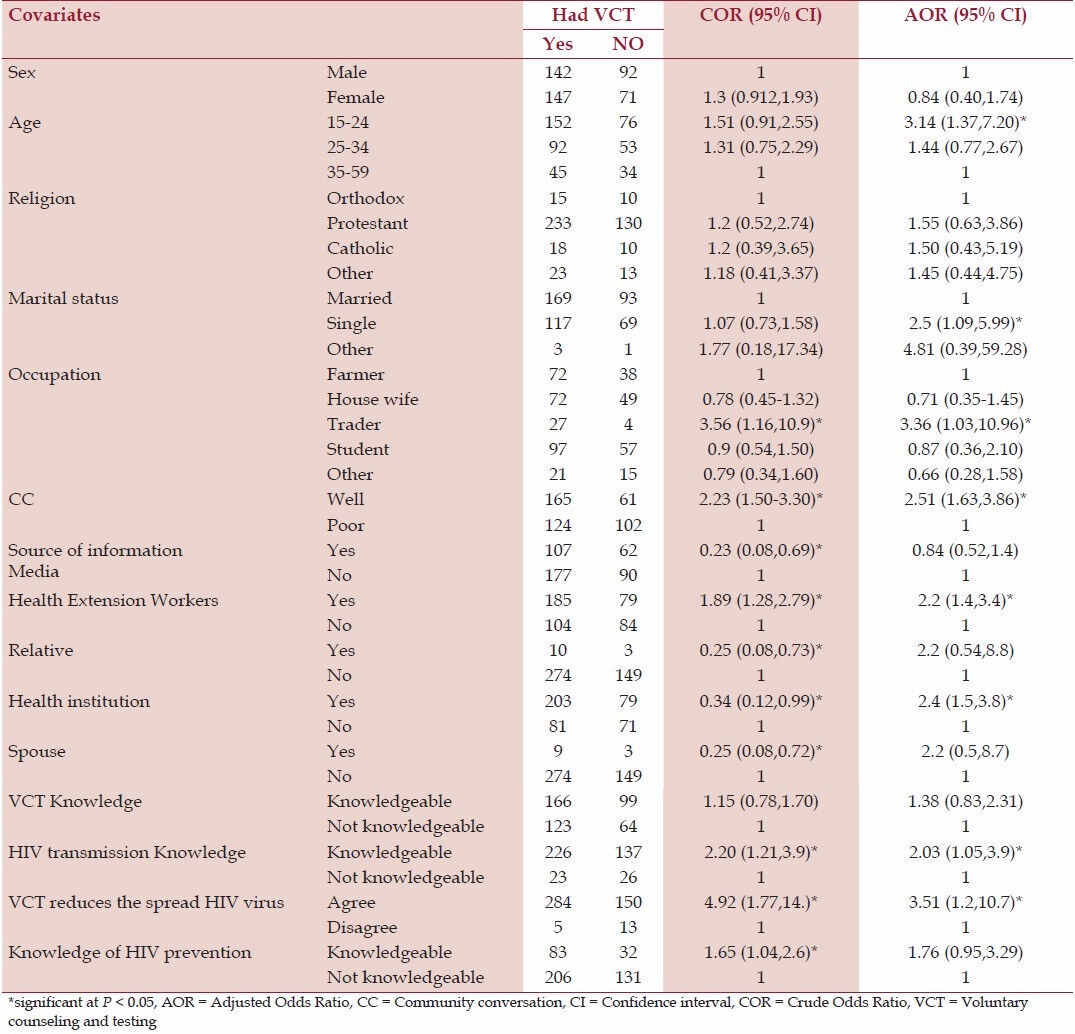
However sex, religion, occupational status other than trader, alcohol consumption, the preferred ways to get VCT result, attitude toward People Living with HIV/AIDS (PLWHAs) and knowledge about HIV prevention did not show statistically significant association with VCT uptake [Table 3].
Discussion
This study showed that significantly higher proportion of the study participants from well CC performing kebeles had utilized VCT compared with participants from poor CC performing kebeles (P < 0.001). This could be due to change in the community understanding of the pandemic as a result of CC sessions. Similarly, CC as a powerful tool in reducing risky sexual behavior embedded in the community and an early marriage has been documented in Ethiopia.[3] On the contrary, though could not reach statistical significance, representation of larger number of students in well CC group compared with poor CC group could have also positively affected the observed association.
VCT service uptake documented in the current study for well CC kebeles is higher than that reported in the recent Ethiopia Demographic and Health Survey (EDHS) report (73% vs. 67%).[11] Our finding that CC is an independent predictor of VCT service utilization is further supported by different reports from Ethiopia,[3,6,10] where after the CC program initiation, VCT service uptake showed increment. Moreover, being sexually active, having sex with a partner and having a colleague who utilized VCT were the reported predictors of VCT uptake among college youths in Ethiopia.[12]
The proportion of the study participants who knew that VCT service is important in reducing the spread of HIV infection was significantly higher in a well CC group (P = 0.034). The finding suggests that CC plays key role in improving knowledge of the community with regard to VCT.
Positive attitude toward VCT reported in this study (97.8% in well and 93.8% in poor CC groups) was consistent with a Harar and Jijiga[3,13] studies.
Consistent with a study done in North and South Gonder,[14] those who were in the age range of 15-24 years were found to significantly utilize VCT service compared to those aged between 35 and 59 years.
The finding that knowledge about HIV transmission is associated with HIV test uptake was also reported from Blantyre, Malawi.[15] As with the current study, lack of association between sex and religion has been reported by a study conducted in Ethiopia.[16]
This study is robust in that it has used a comparative cross-sectional design having a power of 80% to discriminate the difference. The study population were also homogenous on major sociodemographic characteristics, other than CC group, and hence were comparable. It has also used standard questionnaire from previous HIV behavioral surveillance surveys. Unlike the previous studies, this study determined the role of CC in VCT service utilization.
Apart from its strengths, this study has short comings also: It was difficult to establish temporal relationship between CC and utilization of VCT. Moreover, the criteria used to classify kebeles into well and poor CC groups were quite general and not specific to HIV/VCT topics. Though CC is advocated as a powerful tool, its benefits are offset by its dependence on the facilitators' skills. The criteria used to classify study kebeles into well or poor CC groups did not take facilitation skill into account. Thus misclassification bias cannot be ruled out. The bottom line assumption was if kebeles had generally well CC performance, they would address HIV/VCT well. However, as there are lots of community felt problems to be discussed in CC, the share of HIV/VCT might be low. Consequently, even in a well CC kebele, HIV/VCT topics might be addressed poorly. Though it is known that VCT uptake varies with VCT modality as a community-based or facility-based,[17] the study could not separate one modality from the other VCT modality. Another, noteworthy limitation is that the definition of risky sex in this study did not take into account the HIV status of the sex partner of the study participant.
Conclusion
This finding suggests that well CC performance is associated with increased VCT service uptake. Therefore, HIV interventions in the rural communities should support CC performance.
Acknowledgments
The study was supported by Addis Ababa University. The supporting source had no influence on study design; in the collection, analysis, and interpretation of the data; in the writing of the manuscript; and in the decision to submit the manuscript for publication. No one declared conflict of interests.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Guidelines for HIV Counselling and Testing in Ethiopia. Addis Ababa, Ethiopia: Federal HIV/AIDS Prevention and Control Office, Federal Ministry of Health; 2007. Jul, Federal Ministry of Health. [Google Scholar]
- 2.Central Statistical Agency. Ethiopia Demographic and Health Survey, CSA. Addis Ababa: Ethiopia Central Statistical Agency, Addis Ababa, Ethiopia, ORC Macro Calverton, Maryland, USA; 2006. [Google Scholar]
- 3.Getaneh H, Mekonen Y, Eshetu F, Pose B. Community conversation as a catalyst for stigma reduction and behavior change. Pilot study, Lessons learned from a CARE project in Ethiopia. 2008. [Accessed July 2013]. at http://www.popline.org/node/202118 .
- 4.Campbell C, Nhamo M, Scott K, Madanhire C, Nyamukapa C, Skovdal M, et al. The role of community conversations in facilitating local HIV competence: Case study from rural Zimbabwe. BMC Public Health. 2013;13:354. doi: 10.1186/1471-2458-13-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gueye M, Diouf D, Chaava T, Tiomkin D. Leadership for Results: UNDP's Response to HIV/AIDS. Community capacity enhancement handbook: HIV/AIDS Group. Bureau for development policy, UNDP. 2005. [Accessed June 2013]. at www.undp.org/content/dam/.../en/.../hiv-aids/...development.../20.pdf .
- 6.UNDP. Upscaling Community conversations in ethiopia: Unleashing capacities of communities for the HIV/AIDS response: UNDP. 2004. [Accessed June 2013]. at http://asksource.ids.ac.uk/cf/display/bibliodisplay.cfm?ID=33814 & db= keywords & display=full .
- 7.UNDP. Rapid appraisal of the community capacity empowerment programme and leadership development for results components of the enhancing an integrated response to HIV/AIDS and poverty programme. Pretoria, UNDP. 2004 [Google Scholar]
- 8.Strategic plan II for intensifying multisectoral HIV and AIDS response in Ethiopia, 2010/11–2014/15. Addis Ababa, Ethiopia: Federal HIV/AIDS Prevention and Control Office, Federal Ministry of Health; 2010. Feb, Federal Ministry of Health. [Google Scholar]
- 9.Global HIV/AIDS news and analysis Ethiopia ‘Community conversations' opening up the AIDS discussion’ Monday. 2010. Sep 13, [Accesssed June 2013]. at http://www.irinnews.org/report/73219/ethiopia-communityconversations-opening-up-the-aids-discussion .
- 10.Addissie A, Kebede Z. Baseline KABP survey on HIV /AIDS in hawassa zuria and boricha woredas of sidamo zone. Addis Ababa, Ethiopia: 2009. [unpublished] [Google Scholar]
- 11.Central Statistical Agency. Central Statistical Agency. Addis Ababa, Ethiopia: ORC Macro Calverton, Maryland, USA; 2012. Ethiopia Demographic and Health Survey. [Google Scholar]
- 12.Dirar A, Mengiste B, Kedir H, Godana W. Factors contributing to voluntary counselling and testing uptake among youth in colleges of Harar, Ethiopia. Sci J Public Health. 2013;1:91–6. [Google Scholar]
- 13.Zenebu Y, Berhane Y. Determinant of counseling and testing utilization among youth in Jijiga Town. Ethiopia; 2005. [unpublished] [Google Scholar]
- 14.Mengstu A, Yohannis F. Factors affecting acceptance of VCT among different proffessional and community groups in North and South gonder administrative zones, north west Ethiopia. Ethiop J Health Dev. 2006;20:24–31. [Google Scholar]
- 15.Baiden F, Akanlu G, Hodgson A, Akweongo P, Debpuur C, Binka F. Using lay counselors to promote community-based voluntary counseling and HIV testing in rural northern Ghana: A baseline survey on community acceptance and stigma. J Biosoc Sci. 2007;39:721–33. doi: 10.1017/S0021932006001829. [DOI] [PubMed] [Google Scholar]
- 16.Tsegay G, Edris M, Meseret S. Assessment of voluntary counseling and testing service utilization and associated factors among Debre Markos University Students, North West Ethiopia: A cross-sectional survey in 2011. BMC Public Health. 2013;13:243. doi: 10.1186/1471-2458-13-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mulogo EM, Abdulaziz AS, Guerra R, Baine SO. Facility and home based HIV Counseling and Testing: A comparative analysis of uptake of services by rural communities in southwestern Uganda. BMC Health Serv Res. 2011;11:54. doi: 10.1186/1472-6963-11-54. [DOI] [PMC free article] [PubMed] [Google Scholar]


