Abstract
Background:
Quality of life is an important aspect in diabetes because poor quality of life leads to diminished self-care, which in turn leads to worsened glycemic control, increased risks for complications, and exacerbation of diabetes overwhelming in both the short run and the long run.
Aims:
The aim of our study is to examine the health-related quality of life of diabetic patients in rural India.
Materials and Methods:
This case-control study was done among type 2 diabetes mellitus patients attending Medicine Outpatient department of a 780-bedded rural medical college located in central India. We used the World Health Organization Quality of Life Questionnaire — short version (WHOQOL-BREF) to assess quality of life.
Results:
The HRQOL among diabetics and non-diabetic controls is comparable to each other with bad physical health, bad psychological health, deteriorating social relationships, and bad environmental conditions affecting the HRQOL of both the groups equally. The overall HRQOL of the total study population (cases and controls) was poor.
Conclusion:
The finding of this study will help in health promotion in rural medical practice in India. It would beckon the much awaited avenue of holistic care of a diabetic patient with equal importance to the mental wellbeing and quality of life, as compared to physical well being.
Keywords: Diabetes mellitus, Health-related quality of life, HRQOL, WHO-BREF
Introduction
The prevalence of diabetes mellitus has increased significantly over the past two decades.[1] Recent estimates project around 285 million people with diabetes around the world presently, and this number is set to increase to 438 million by the year 2030.[2,3,4] According to the World Diabetes Atlas, India is projected to have around 51 million people with diabetes.[2] The public awareness of the disease is low, more so in the rural areas where there are increasing number of patients. Approximately 742 million people in India live in rural areas where the awareness of chronic disease in extremely low, and the ratio of unknown-to-known diabetes is 3:1, as compared to urban India wherein it is 1:1.[5,6] There are more than 37.76 million diabetics in India; 21.4 million in urban areas and 16.36 million in rural areas. Recently published data reveal that the age-standardized prevalence of total diabetes (previously diagnosed and previously undiagnosed diabetes) ranges from 8-18% in urban India and 2.4-8% in rural India.[7] Diabetes is estimated to be responsible for 109 thousand deaths, 1157 thousand years of life lost, and for 2263 thousand disability-adjusted life years (DALYs) during 2004.[8,9]
Quality of life is an important aspect in diabetes because poor quality of life leads to diminished self-care, which in turn leads to worsened glycemic control, increased risks for complications, and exacerbation of diabetes overwhelming in both the short run and the long run. Thus, it is apparent that quality of life issues are imperative and predict how well an individual would be able to handle his disease and maintain his long term health and well-being. It is also important for the assessment of patients' perceived burden of his chronic disease condition, to see the trends of health overtime and quantify the effect of treatment.[10,11] Diabetes significantly increases patient's risk of developing blindness, end-stage renal disease, lower limb amputations, as well as increases mortality due to coronary artery disease, cerebrovascular disease, or peripheral vascular disease. A considerable number of patients suffering from type 2 diabetes mellitus eventually risk developing acute and chronic micro and macrovascular complications including retinopathy, nephropathy, neuropathy, peripheral vascular disease, coronary heart disease, and stroke. The Chennai Urban Rural Epidemiological Study (CURES) found that 17.6% patients had diabetic retinopathy, 26.9% had microalbuminuria, and 26.1% had peripheral neuropathy.[12,13,14] In the Chennai Urban Population Study (CUPS), 21.4% of diabetes patients had coronary artery disease and 6.3% had peripheral vascular disease.[15,16] The United Kingdom Prospective Diabetes Study (UKPDS) has proven that a good glycemic control can decrease the diabetic complications significantly, thus paving way for benefits of early diagnosis and appropriate management.[17]
It is well recognized fact that diabetes mellitus is associated with increased morbidity and mortality. But, how this disease affects functional health status and sense of wellbeing is still not well established. The apparent difference between one's expectations and one's actual physical, emotional, and social functioning is HRQOL. As one might predict, people with diabetes rate their HRQOL significantly less favorably, on average, than people without diabetes. The concept of HRQOL and its determinants have evolved since the 1980s to encompass those aspects of overall quality of life that can be clearly shown to affect health-either physical or mental.[18,19,20] On the individual level, this includes physical and mental health perceptions and their correlates–including health risks and conditions, functional status, social support, and socio-economic status. On the community level, HRQOL includes resources, conditions, policies, and practices that influence a population's health perceptions and functional status.
Several studies have demonstrated that diabetes has a strong negative impact on HRQOL, especially in the presence of complications.[11,21,22,23,24,25,26] However, most of the studies on diabetes and HRQOL have been conducted in developed countries where there is access to better health care facilities. In developing countries, the morbidity associated with diabetes and its complications is certainly higher as compared to developed countries, which adversely affects the HRQOL of these patients. Moreover, studies of the HRQOL in diabetic patients in developing countries are rare.[11] Hence, we planned a study to examine the HRQOL of diabetic patients in rural India.
Materials and Methods
This study was done among type 2 diabetes mellitus patients attending Medicine Outpatient department of a 780-bedded rural medical college located in central India. The Medicine outpatient department (OPD) caters to an average of 75,000 patients annually. The study is a case-control study to assess the HRQOL of patients with type 2 diabetes mellitus (T2DM). The study was carried out between the periods of May 2012 and July 2012.
Cases were all consecutive patients of T2DM attending Medicine OPD in the period between May 2012 and July 2012. Diabetes mellitus was defined as according to ADA guidelines 2011. Patients with type 1 diabetes mellitus, pregnant females, or patients with co-morbidities other than that due to diabetes or its complications were excluded. At the time on inclusion in the study, the cases were not re-examined by the physician for complications. Information was collected on socio-demographic status (marital status, education, own housing versus rental, occupational status) and disease-related information (type of diabetes, duration of diabetes since the first diagnosis, medication for diabetes, complications of diabetes). The distinctions between co-morbidities and complications of diabetes were based on medical records of the patient and not re-evaluated at time of inclusion in the study.
We chose one age- and sex-matched control for each case. Controls were recruited from both the hospital and the community. The hospital controls were the relatives of the patients admitted for any illness. At the time of inclusion in study, we assessed the glycemic status of the subjects by doing their glycosylated hemoglobin (HbA1c), fasting blood sugar, and post-prandial blood sugar. We took ethics approval from institutional ethics committee for conducting this study. We also take informed consent from all study participants in the vernacular language. All the patients in the study were educated regarding their disease, its complications, and the importance of good glycemic control and its impact over their quality of life.
Study questionnaire
The study investigator explained the patients regarding the study and took their informed consent. The investigator then asked the patients to answer the HRQOL questionnaire. We used the World Health Organization Quality of Life Questionnaire – short version (WHOQOL-BREF) to assess quality of life.[27,28] This questionnaire was developed with 15 international field centers to obtain an assessment tool that is applicable cross-culturally. The four domains of the WHOQOL-BREF are physical health, psychological (e.g. self-esteem), social relationships (e.g. social support), and environment (e.g. freedom, physical safety). Subjects would rate all items on a 5-point Likert-type scale. The questionnaire was translated into vernacular language (Marathi) and then back-translated into English.
Statistical analysis
We entered all data initially on Microsoft excel and then transferred it electronically to STATA statistically software version 12.1 (Stata corporation, Texas, USA). We calculated means for all normally distributed variables and medians for others. We used the chi-square test for comparison of categorical variables and the t-test for the comparison of mean score values for the domains of WHOQOL-BREF between groups.
Results
A total of 70 patients with T2DM and 70 age- and sex-matched non-diabetic controls were enrolled in the study. Table 1 represents the distribution of demographic covariates among cases and controls.
Table 1.
Demographic characteristics of the study population
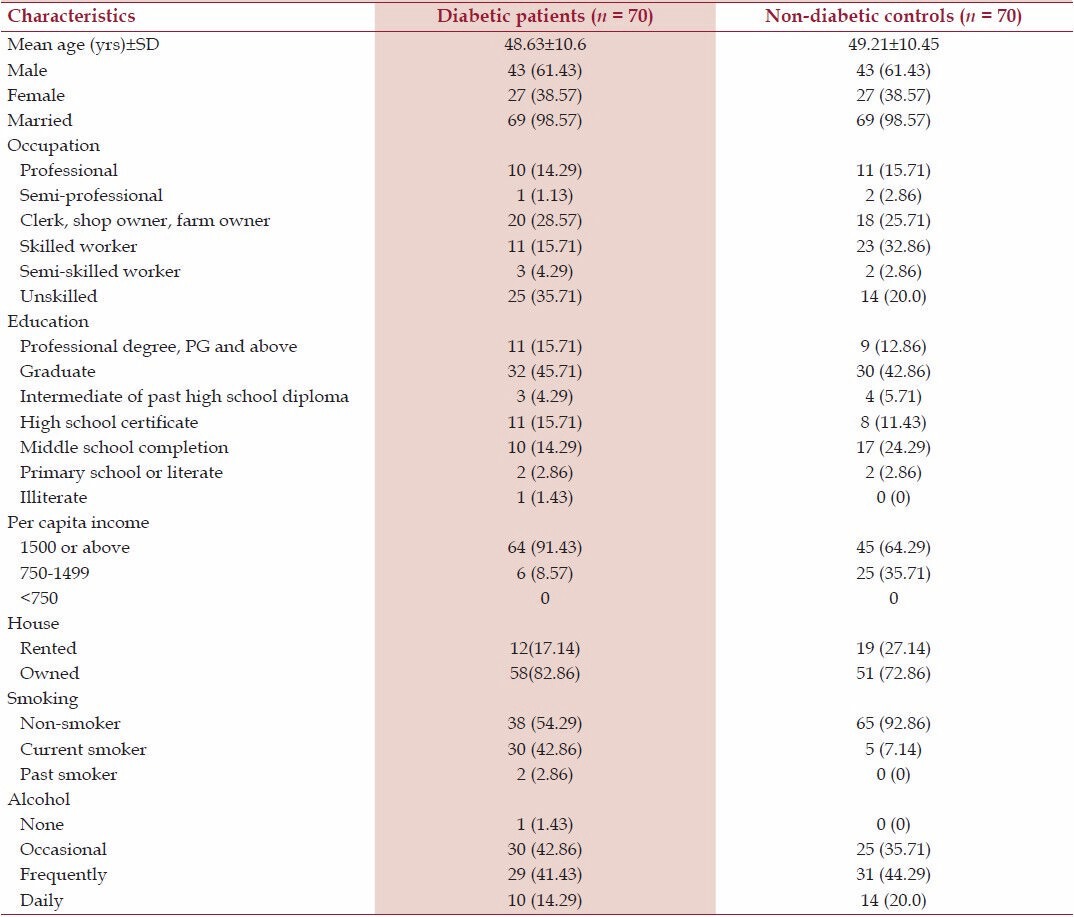
The mean age of participants was 48.63 ± 10.6 yrs for cases and 49.21 ± 10.45 yrs for controls. The control group had more skilled workers as compared to diabetic patient group, which had more number of unskilled workers. The control group had more number of subjects with education till at least middle school as compared to diabetes patient group. The per capita income of more than 90% diabetic patients was above 1500 rupees as compared to only 64% in control group (<0.001). More diabetic patients owned a house. About 43% of diabetic patients were current smokers as compared to 93% controls, which were non-smokers (P < 0.006).
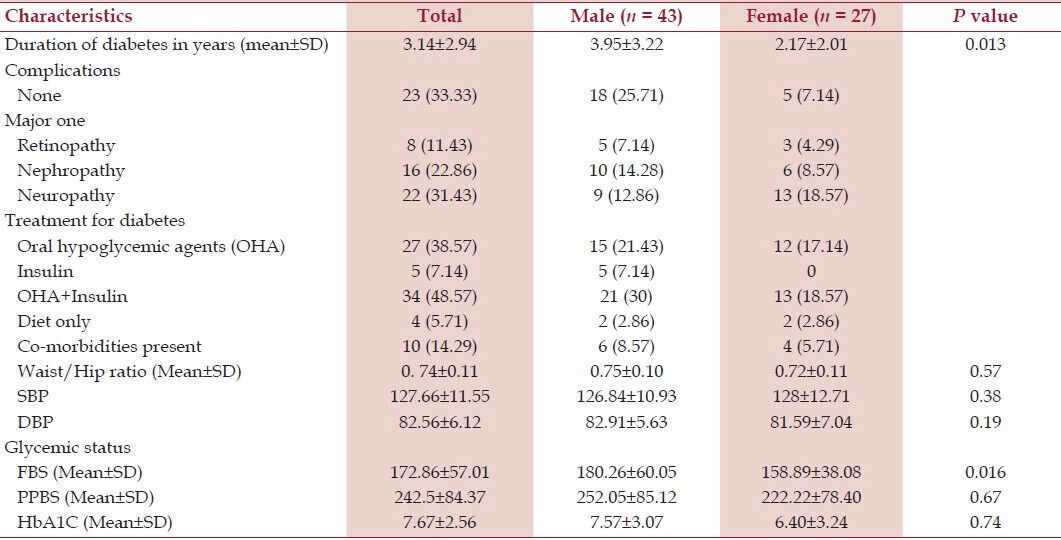
Table 2 represents the characteristics of diabetic patients (cases). The mean duration of diabetes among the cases was 3.14 ± 2.94 years. About 76% of the total diabetic subjects had at least one major complication of diabetes. Majority of diabetics were either on a combination of oral hypoglycemic agents and insulin or oral hypoglycemic agents alone for the control of their diabetes. In about 14% of the diabetic patients, co-morbidities like hypertension, dyslipidemia, coronary artery disease, and cerebrovascular disease were present. The mean fasting blood sugar (FBS), post-prandial blood sugar (PPBS), and glycosylated hemoglobin (HbA1C) were 172.86 ± 57.01, 242.5 ± 84.37, and 7.67 ± 2.56, respectively. The overall glycemic control was better in females as compared to males (FBS 158.89 ± 38.08 vs. 180.26 ± 60.05, P < 0.016).
Table 2.
Characteristics of diabetics in the study
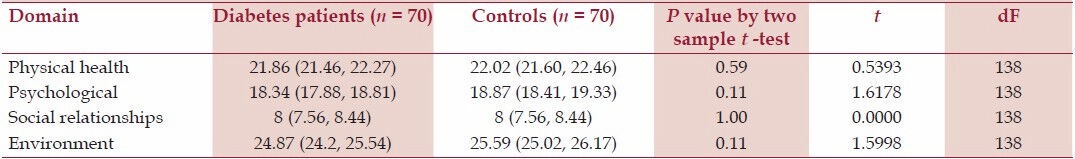
The crude domain scores among both the diabetics and controls were comparable [Table 3]. The scores for both the diabetic cases and controls were low in all the domains, like, physical health, psychological health, and environmental domains. But, the scores for both groups were extremely low in the domain of social relationships. This means that bad physical health, bad psychological health, deteriorating social relationships, and bad environmental conditions are affecting the HRQOL of both the groups equally.
Table 3.
Crude domain scores of WHOQOL-Bref for diabetic patients and controls (mean scores and 95% confidence intervals)
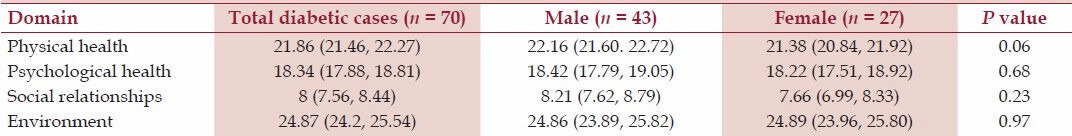
When we compared the male and female diabetics, there was no difference in crude domain scores in psychological health, social relationships, and environment between both the groups [Table 4]. But, there was a near significance in physical health suggesting that male diabetic's physical health was marginally better then female diabetics (P value = 0.06).
Table 4.
Crude domain scores of WHOQOL-Bref for male diabetic and female diabetic patients (mean scores and 95% confidence intervals)
Discussion
The HRQOL among diabetics and non-diabetic controls is comparable to each other with bad physical health, bad psychological health, deteriorating social relationships, and bad environmental conditions affecting the HRQOL of both the groups equally. The overall HRQOL of the total study population (cases and controls) was poor. As the HRQOL was comparable for both the groups, we did not do the multivariate analysis (as planned) for seeing which variables have effect over HRQOL.
Eljedi A et al.[21] analyzed the HRQOL in a sample of diabetic patients living in refugee camps in the Gaza strip in comparison to gender- and age-matched non-diabetic controls from the same camps. Diabetes and its complications affected negatively all of the domains of the WHOQOL-BREF; however, the effects were strongest for the physical health and psychological domains and weaker for the social relationships and environment domains. We found a strong effect of interactions between gender and disease status (diabetic patients vs. controls). Whereas this finding could be partly explained by the worse situation of female patients in respect to the disease in our sample, this is still an evidence for gender inequalities. Similar difference in HRQOL of both genders was observed in a study conducted in Iran.[29] Lower HRQOL in women with diabetes was also reported in other studies.[30,31] Age strongly affected the HRQOL of diabetic patients in physical health and psychological domains and had almost no effects on HRQOL among controls.
Strengths and limitations
This is one of the few studies, which have studied HRQOL of diabetic patients in the rural areas of Indian subcontinent. One of the strengths of our study is the inclusion of age-and sex-matched control group. There are, however, a few weakness of our study. One of the primary weaknesses of this study is a relatively small sample size due to constraint of finances and time. Diabetic patients recruited for this study are a random sub-sample of patients treated in our hospital and but may not represent all diabetic patients. Whereas this restriction does not threaten the internal validity of the analysis, findings may be not generalizable. Patients treated at our hospital may have a worse health condition than patients receiving care from other providers. In some cases, the medical records regarding complications of diabetes may have been incomplete. This information was not verified by an examination by the physician for the purpose of this study. This may have resulted in underreporting of complications, but this does not affect the comparison between diabetic patients and controls. This study has contributed to the literature by translating the WHOQOL-BREF into Marathi and by administering the assessment tool for the first time to a Marathi speaking sample.
Conclusions
Diabetic patients living in the rural areas have a HRQOL comparable to non-diabetic controls living under the same conditions. But overall, the HRQOL was quite considerably low. The prevalence of diabetes mellitus is increasing, and the disease places more and more demands on medical care and expenditure. In order to preserve a good HRQOL, it is obviously important to prevent diabetes complications and properly manage concomitant chronic diseases. The finding of this study will help in health promotion in rural medical practice in India. It would beckon the much awaited avenue of holistic care of a diabetic patient with equal importance to the mental wellbeing and quality of life, as compared to physical well being.
Footnotes
Source of Support: This study was done as a part of Indian council of medical research short term studentship programme (ICMR-STS) -2012.
Conflict of Interest: None declared.
References
- 1.Pearson TA. Education and income: Double-edged swords in the epidemiologic transition of cardiovascular disease. Ethn Dis. 2003;13(2 Suppl 2):S158–63. [PubMed] [Google Scholar]
- 2.Mensing C, Boucher J, Cypress M, Weinger K, Mulcahey K, Barta P, et al. National standards for diabetes self-management education. American Diabetes Association: Clinical practice recommendations 2001. Diabetes Care. 2001;24(Suppl 1):S1–133. [Google Scholar]
- 3.Niazi AK, Naizi SH. A novel strategy for the treatment of diabetes mellitus- sodium glucose co-transport inhibitors. N Am J Med Sci. 2010;2:556–60. doi: 10.4297/najms.2010.2556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: Prevalence, numerical estimates, and projections. Diabetes Care. 1998;21:1414–31. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 5.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 6.“Stop the global epidemic of chronic disease”-new report, preventing chronic diseases: A vital investment estimates hundreds of billions of dollars at stake. Indian J Med Sci. 2005;59:463–5. [PubMed] [Google Scholar]
- 7.Jali MV, Kambar S, Jali SM, Gowda S. Familial early onset of type-2 diabetes mellitus and its complications. N Am J Med Sci. 2009;1:377–80. doi: 10.4297/najms.2009.7377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anjana RM, Ali MK, Pradeepa R, Deepa M, Datta M, Unnikrishnan R, et al. The need for obtaining accurate nationwide estimates of diabetes prevalence in India - rationale for a national study on diabetes. Indian J Med Res. 2011;133:369–80. [PMC free article] [PubMed] [Google Scholar]
- 9.Venkataraman K, Kannan AT, Mohan V. Challenges in diabetes management with particular reference to India. Int J Diabetes Dev Ctries. 2009;29:103–9. doi: 10.4103/0973-3930.54286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vigneshwaran E, Padmanabhareddy Y, Devanna N, Alvarez-Uria G. Gender differences in health related quality of life of people living with HIV/AIDS in the era of highly active antiretroviral therapy. N Am J Med Sci. 2013;5:102–7. doi: 10.4103/1947-2714.107526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garratt AM, Schmidt L, Fitzpatrick R. Patient-assessed health outcome measures for diabetes: A structured review. Diabet Med. 2002;19:1–11. doi: 10.1046/j.1464-5491.2002.00650.x. [DOI] [PubMed] [Google Scholar]
- 12.Rema M, Premkumar S, Anitha B, Deepa R, Pradeepa R, Mohan V. Prevalence of diabetic retinopathy in urban India: The Chennai Urban Rural Epidemiology Study (CURES) eye study, I. Invest Ophthalmol Vis Sci. 2005;46:2328–33. doi: 10.1167/iovs.05-0019. [DOI] [PubMed] [Google Scholar]
- 13.Unnikrishnan RI, Rema M, Pradeepa R, Deepa M, Shanthirani CS, Deepa R, et al. Prevalence and risk factors of diabetic nephropathy in an urban South Indian population: The Chennai Urban Rural Epidemiology Study (CURES 45) Diabetes Care. 2007;30:2019–24. doi: 10.2337/dc06-2554. [DOI] [PubMed] [Google Scholar]
- 14.Pradeepa R, Rema M, Vignesh J, Deepa M, Deepa R, Mohan V. Prevalence and risk factors for diabetic neuropathy in an urban south Indian population: The Chennai Urban Rural Epidemiology Study (CURES-55) Diabet Med. 2008;25:407–12. doi: 10.1111/j.1464-5491.2008.02397.x. [DOI] [PubMed] [Google Scholar]
- 15.Mohan V, Deepa R, Rani SS. Chennai Urban Population Study (CUPS No.5). Prevalence of coronary artery disease and its relationship to lipids in a selected population in South India: The Chennai Urban Population Study (CUPS No. 5) J Am Coll Cardiol. 2001;38:682–7. doi: 10.1016/s0735-1097(01)01415-2. [DOI] [PubMed] [Google Scholar]
- 16.Premalatha G, Shanthirani S, Deepa R, Markovitz J, Mohan V. Prevalence and risk factors of peripheral vascular disease in a selected South Indian population: The Chennai Urban Population Study. Diabetes Care. 2000;23:1295–300. doi: 10.2337/diacare.23.9.1295. [DOI] [PubMed] [Google Scholar]
- 17.Davis TM, Cull CA, Holman RR. Relationship between ethnicity and glycemic control, lipid profiles, and blood pressure during the first 9 years of type 2 diabetes: U.K. Prospective Diabetes Study (UKPDS 55) Diabetes Care. 2001;24:1167–74. doi: 10.2337/diacare.24.7.1167. [DOI] [PubMed] [Google Scholar]
- 18.Gandek B, Sinclair SJ, Kosinski M, Ware JE., Jr Psychometric evaluation of the SF-36 health survey in Medicare managed care. Health Care Financ Rev. 2004;25:5–25. [PMC free article] [PubMed] [Google Scholar]
- 19.McHorney CA. Health status assessment methods for adults: Past accomplishments and future directions. Annu Rev Public Health. 1999;20:309–35. doi: 10.1146/annurev.publhealth.20.1.309. [DOI] [PubMed] [Google Scholar]
- 20.Selim AJ, Rogers W, Fleishman JA, Qian SX, Fincke BG, Rothendler JA, et al. Updated U.S. population standard for the Veterans RAND 12-item Health Survey (VR-12) Qual Life Res. 2009;18:43–52. doi: 10.1007/s11136-008-9418-2. [DOI] [PubMed] [Google Scholar]
- 21.Eljedi A, Mikolajczyk RT, Kraemer A, Laaser U. Health-related quality of life in diabetic patients and controls without diabetes in refugee camps in the Gaza strip: A cross-sectional study. BMC Public Health. 2006;6:268. doi: 10.1186/1471-2458-6-268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Speight J, Reaney MD, Barnard KD. Not all roads lead to Rome-a review of quality of life measurement in adults with diabetes. Diabet Med. 2009;26:315–27. doi: 10.1111/j.1464-5491.2009.02682.x. [DOI] [PubMed] [Google Scholar]
- 23.Hill-Briggs F, Gary TL, Hill MN, Bone LR, Brancatti FL. Health related quality of life in urban African-Americans with type 2 diabetes mellitus. J Gen Intern Med. 2002;17:412–9. doi: 10.1046/j.1525-1497.2002.11002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee WJ, Song KH, Noh JH, Choi YJ, Jo MW. Health-related quality of life using the EuroQol 5D questionnaire in Korean Patients with Type 2 Diabetes. J Korean Med Sci. 2012;27:255–60. doi: 10.3346/jkms.2012.27.3.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Graham JE, Stoebner-May DG, Ostir GV, Al Snih S, Peek MK, Markides K, et al. Health related quality of life in older Mexican Americans with diabetes: A cross-sectional study. Health Qual Life Outcomes. 2007;5:39. doi: 10.1186/1477-7525-5-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jiang L, Beals J, Whitesell NR, Roubideaux Y, Manson SM. AI-SUPERPFP Team. Health-related quality of life and help seeking among American Indians with diabetes and hypertension. Qual Life Res. 2009;18:709–18. doi: 10.1007/s11136-009-9495-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The WHOQOL Group. The World Health Organization Quality of Life Assessment (WHOQOL).Development and psychometric properties. Soc Sci Med. 1998;46:1569–85. doi: 10.1016/s0277-9536(98)00009-4. [DOI] [PubMed] [Google Scholar]
- 28.Development of the World Health Organization HOQOL-BREF quality of life assessment. The WHOQOL Group. Psychol Med. 1998;28:551–8. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 29.Aghamollaei T, Eftekhar H, Shojaeizadeh D, Mohammad K, Nakhjavani M, Ghofrani Pour F. Behavior, metabolic control and health-related quality of life in diabetic patients at Bandar Abbas Diabetic Clinic. Iran J Public Health. 2003;32:54–9. [Google Scholar]
- 30.Redekop WK, Koopmanschap MA, Stolk RP, Rutten GE, Wolffenbuttel BH, Niessen LW. Health-related quality of life and treatment satisfaction in Dutch patients with type 2 diabetes. Diabetes Care. 2002;25:458–463. doi: 10.2337/diacare.25.3.458. [DOI] [PubMed] [Google Scholar]
- 31.Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev. 1999;15:205–18. doi: 10.1002/(sici)1520-7560(199905/06)15:3<205::aid-dmrr29>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]


