Abstract
Background:
The use of suction catheter (SC) has been shown to improve success rate during ProSeal laryngeal mask airway (PLMA) insertion in expert users.
Aims:
The aim of this study was to compare insertion of PLMA performed by untrained physicians using a SC or the digital technique (DT) in anaesthetised non-paralysed patients.
Methods:
In this prospective randomised double-blind study, conducted in the operating setting, 254 patients (American Society of Anaesthesiologists I-II, aged 18-65 years), undergoing minor surgery were enrolled. Exclusion criteria were body mass index >35 kg/m2, laryngeal or oesophageal varices, risk of aspiration or difficult face mask ventilation either referred or suspected (Langeron's criteria ≥2) and modified Mallampati classification score >2. Participants were randomly allocated to one of the two groups in which PLMA was inserted using DT (DT-group) or SC (SC-group).
Statistical Analysis:
Chi-square test with Yates’ correction, Mann-Whitney U-test or Student's t-test were carried-out as appropriate.
Results:
The final insertion success rate was greater in SC-groupcompared with DT-group 90.1% (n = 109) versus 74.4% (n = 99) respectively (P = 0.002). Mean airway leak pressure was higher in SC-group compared to DT-group (23.7 ± 3.9 vs. 21.4 ± 3.2 respectively; (P = 0.001). There were no differences in insertion time, post-operative airway morbidity and complications.
Conclusion:
The findings of this study suggest that SC-technique improves the success rate of PLMA insertion by untrained physicians.
Keywords: Digital technique, ProSeal laryngeal mask airway, suction catheter technique, untrained physicians
INTRODUCTION
The ProSeal™ laryngeal mask airway (PLMA) has an orifice through which a nasogastric tube can be inserted; this drain tube was especially designed to prevent aspiration and gastric insufflations.[1,2] PLMA may be inserted by using digital manipulation or with an introducer tool; however, using both these techniques the insertion success rate is lower when compared to that obtained with the classic LMA.[3,4]
Many alternative techniques have been suggested to improve the success rate of insertion, with the bougie-guided one undergoing a considerable number of randomised control trials, which demonstrated the superiority of the bougie-guided PLMA insertion compared with the conventional digital technique (DT).[5,6] Furthermore, the use of a suction catheter (SC) has been shown to improve performance during insertion.[7,8] There are some advantages in using the SC over bougie for PLMA insertion which include less trauma, blind insertion without laryngoscope guidance and wide availability of this cheap device.
Moreover, as untrained physicians have not been involved yet in previous studies, it cannot be certainly stated the improvement of PLMA insertion by the SC technique compared with the DT in terms of usefulness and safety.
In this study, we tested the hypothesis that the insertion of PLMA performed by untrained physicians using a SC is more effective than the DT in anaesthetised non-paralysed adult patients. The primary outcome measure was the total success rate of insertion. Secondary outcomes were insertion time, airway morbidity and oropharyngeal leak pressure.
METHODS
After obtaining local Ethical Committee approval and patients’ written informed consent, 254 patients (American Society of Anaesthesiologists physical status I-II, aged 18-65 years), undergoing minor surgery (anorectal or open inguinal hernia repair) were enrolled. Patients excluded were those with body mass index >35 kg/m2, laryngeal or oesophageal varices, risk of aspiration or difficult face mask ventilation either referred or suspected (Langeron's criteria ≥2),[9] Mallampati score as modified by Samsoon and Young >2,[10] in order to exclude a confounding factor according to previous findings,[11] and those scheduled for surgical procedures with planned time duration of >1 h. In addition, during the pre-operative visit, the following difficult airway parameters were also collected: Mouth opening (cm) and the thyromental distance (cm).
Patients were randomly allocated into one of two groups, digital technique or suction catheter were used for PLMA insertion in DT and SC group, respectively. The randomisation was done based on the year in which the patients were born: Odd or even.[12] All patients were given aspiration prophylaxis with ranitidine 50 mg intravenous (iv) and metoclopramide 10 mg (iv) 1 h before surgery and were pre-medicated with midazolam 0.02 mg/kg iv 15 min before anaesthesia. Following the patients’ head positioning on a standard pillow (about 7 cm in height) and 3 min of pre-oxygenation, anaesthesia was induced with propofol infusion at a target concentration of 6 μg/ml (Alaris Medical System Diprifusor© incorporating TM target controlled infusion pump; CA, USA) and remifentanil infusion at 0.5 μg/kg/min iv. Face mask ventilation was performed until the following conditions were reached to enable insertion of PLMA© (North America Inc. San Diego CA, USA): Loss of corneal reflex, apnoea and no response to jaw thrust. The manufacturer's weight-based recommendations were used for size selection. Anaesthesia was maintained with propofol target concentration (3-5 μg/ml) and remifentanil at variable infusion rate (0.05-0.2 μg/kg/min) so as to maintain Bispectral Index (BIS) around 40 (BIS© Aspect Medical System, Inc. Natick, MA) and haemodynamic parameters by 20% of baseline. No other iv or inhalational anaesthetic were administered. Patients underwent volume controlled ventilation using a total gas (oxygen 50% and air) flow of 5 L/min, with a tidal volume set at 8 ml/kg and a respiratory rate adjusted to maintain an end-tidal CO2 (EtCO2) between 35 and 40 mmHg. The Datex-Ohmeda S/5 Avance© Anaesthesia System (GE Health-care Madison, Wisconsin, USA) was used.
The untrained physicians involved in this study were trainee anaesthesiologists (n = 30) who had performed less than 20 PLMA insertions in the setting of operating theatre after previous training on a manikin. Two attempts were allowed before PLMA insertion by the trainees was considered a failure and airway was managed by an expert anaesthesiologist who was present throughout the procedure. It was planned that the expert anaesthesiologist inserted the PLMA using SC technique, in case of failure by the trainees and classic LMA, in the event of further failure; he was also ready to change airway management strategy for orotracheal intubation, if necessary. The ease of PLMA insertion was classified as ‘easy’ if the first attempt was successful, ‘difficult’ in cases with success on the second attempt and ‘failure’ in cases where both attempts had failed.
Criteria for unsuccessful insertion included: (1) Failed passage into pharynx; (2) misplacement as detected by air leaks from oropharynx (listening over mouth)/stomach (auscultation over epigastrium)/drain tube (placing lubricant over proximal orifice of the drain tube) with a peak airway pressure below 20 cm H2O; (3) in effective ventilation (absence of square wave capnography or EtCO2 >45 mmHg during mechanical ventilation). The reasons for failed insertion were documented. Time between picking up the PLMA ready for insertion and successful placement with the establishment of an effective airway was recorded. DT-technique was performed according to the manufacturer's recommendations, using the index finger to press the PLMA mask into the mouth and advance it around the palatopharyngeal curve. The SC guided technique was carried out following previous indications[8] and involved the following steps: (1) A 16 Fr - 5.33 mm SC (Pennine Healthcare, UK) was lubrificated with water-based gel (K-Y Jelly, Johnson and Johnson, Pinewood, UK) and (2) was inserted into the orogastric tube channel of the PLMA with its tip protruding beyond the cuff of PLMA; finally, (3) after opening the mouth, the handle of PLMA was pushed while introducing the SC tip into the oropharynx blindly. Once the PLMA was inserted into the pharynx, the intra-cuff pressure was set at 60 cm H2O using a digital manometer (Mallinckrodt Medical, Athlone, Ireland). After removal of the SC, airway leak pressure (ALP) was measured by recording the circuit pressure at which gas was first heard to escape around the LMA leaving a fresh gas flow at 3 L/min with the circuit pop-off valve completely closed.
After surgery (18-24 h), patients were asked about airway morbidity (including sore throat, dysphagia and dysphonia). An un-blinded observer collected the intraoperative data and a blinded observer collected the post-operative data. Patients were unaware of insertion technique used.
Any episode of hypoxia as defined by a SpO2 <93% or other adverse events were registered.
The number of patients included in the study was based on a previous study[8] and on a priori power analysis assuming alpha of 0.05 and beta of 0.90. A minimum of 119 patients per each group was required to detect an increase of 15% in success rate of insertion for the SC group compared to control group. The investigators planned to recruit 254 patients, including the numbers of drop out.
Chi-square test with Yates’ correction, Mann-Whitney U-test or Student's t-test were carried-out, as appropriate. Data were presented as mean ± standard deviation or as numbers (percentage). A significance level of P < 0.05 was used. The statistical analyses were performed using Statistical for Windows 7.0 (Stat soft, Tulsa Ok, USA).
RESULTS
Demographic data and measured difficult airway parameters were similar in the two groups [Table 1]. Insertion success rates, insertion time, aetiology of failed insertion and oropharyngeal leak pressure are showed in Table 2.
Table 1.
Demographic data and airway parameters in the guided SC and DT groups
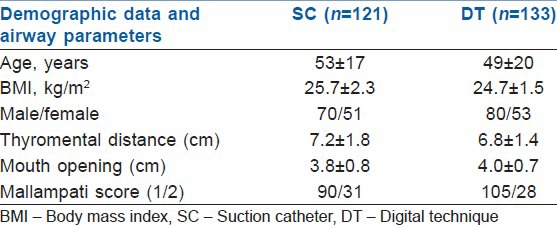
Table 2.
Final success rate, 1st attempt success rate, insertion time, ALP and airway morbidity in the SC and DT groups
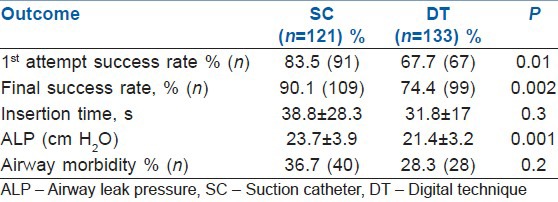
LMA insertion by the SC-guided technique was successful at the first attempt in 91 patients versus 67 patients from DT group (P = 0.01) [Table 2].
The final insertion success rate was greater in SC-group (n = 121) compared with DT-group (n = 133): 90.1% (n = 109) versus 74.4% (n = 99) respectively (P = 0.002).
Mean ALP was higher in SC group compared to DT group (23.7 ± 3.9 vs. 21.4 ± 3.2 respectively; P = 0.001). The insertion time was similar in the two groups (38.8 ± 28.3 vs. 31.8 ± 17.3 respectively); P = 0.3). There were no differences in post-operative airway morbidity occurrence between the two techniques (n = 28; 28.3% in DT group; n = 40; 36.7% in SC-group; P = 0.2) and in the frequency of visible blood or other complications of insertion [Table 3].
Table 3.
Aetiology of failure in the SC and DT groups and complications of insertions
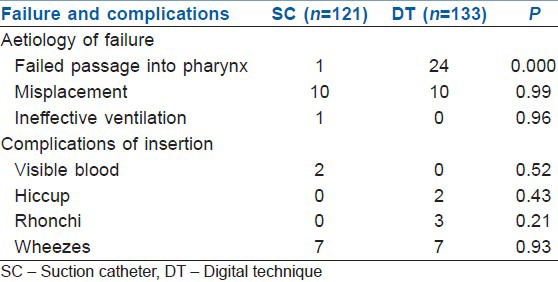
The main cause of failed insertion in DT group was a failed passage into pharynx (n = 24; 70.5%) while the main cause of failure with SC-technique was misplacement (n = 10; 83.3%) [Table 3].
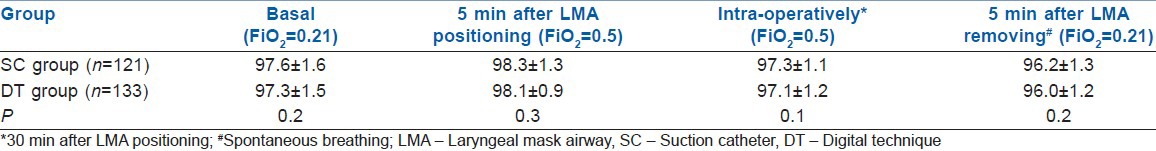
There were no differences in SpO2 trend between the two groups [Table 4].
Table 4.
SpO2 trend for SC and DT group
No adverse events were observed.
DISCUSSION
From this study, it emerges that the SC-technique may improve the success rate of insertion even by untrained users and may make this device more effective as shown by greater APL compared with that of DT-technique. These results mirror those of a previous study, which reported an enhanced success rate when SC-technique was used by expert physicians.[12]
As for our secondary outcomes, insertion time was similar for the two techniques indicating that both are likewise affected by lack of experience; furthermore, no difference was found with regard to airway morbidity between the two techniques confirming the safety of SC-technique even among untrained physicians.
Our results match those of the unique study that had been performed with the aim of comparing DT with SC-technique[8] among untrained physicians. Furthermore, Nagata et al. found that PLMA insertion by SC-technique was significantly more successful at the first attempt than the standard DT with a success rate of 100% versus 73%, respectively.[8] However, some differences arise from a comparison between the two studies. In their study, Nagata et al. involved physicians who had performed less than 100 insertions[8] while our inexperienced users had a lower level of training (<20 PLMA insertions). This may be the reason why the mean PLMA insertion times in Nagata's study were shorter for both SC-technique and DT-technique compared to those of our study (13 vs. 39 s and 25 vs. 32 s, respectively).
Brimacombe et al. advised on superiority of the gum elastic bougie-guided technique when compared to DT-technique and its rescue ability to replace the introducer tool technique in case of DT-technique failure.[6] The gum elastic bougie may improve the insertion success rate of PLMA as it is sufficiently rigid to eliminate the impaction at the back of the mouth with easier transition into the oesophagus. However, this technique requires laryngoscope guidance due to the stiffness of the device. This approach may be more traumatic for the oesophagus, especially in case of occult varices or mucosal lesions. In our opinion, the use of a SC seems a good compromise between the need to reinforce the cuff of PLMA and a safe use.[13,14] In this regard, we found that failed passage into pharynx was more frequent with the DT-technique revealing the previously described difficulties related to this approach. On the other hand, we found that the main cause of failure with SC-technique was the malposition. Since SC makes the distal cuff stiffer and less likely to fold over, it is reasonable that the SC-guided technique may be useful in directing the distal cuff around the oropharyngeal inlet and towards the oesophagus. However, the SC might not be sufficiently stiff to guide the distal cuff around the oropharynx in case of difficult airway.
Regarding as limitations, it has to be remembered that, in this study, the observer who collected intraoperative data was un-blinded leading to a potential source of bias.
CONCLUSION
In conclusion, our study is in line with the previous investigations about this issue and demonstrates that the SC-technique is more efficient than DT-technique when both were performed by inexperienced physicians. This technique is able to make the success rate of insertion by untrained personnel close to that of expert users with DT; thus, it could be recommended for training.
Since the majority of the studies, as ours, enrolled only patients with easy airways, further studies are needed to establish the usefulness of SC in difficult airways seeing that PLMA may be regarded as a rescue device.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sharma B, Sood J, Sahai C, Kumra VP. Troubleshooting ProSeal LMA. Indian J Anaesth. 2009;53:414–24. [PMC free article] [PubMed] [Google Scholar]
- 2.Goldmann K, Hechtfischer C, Malik A, Kussin A, Freisburger C. Use of ProSeal laryngeal mask airway in 2114 adult patients: A prospective study. Anesth Analg. 2008;107:1856–61. doi: 10.1213/ane.0b013e318189ac84. [DOI] [PubMed] [Google Scholar]
- 3.Brimacombe J, Keller C. The ProSeal laryngeal mask airway: A randomized, crossover study with the standard laryngeal mask airway in paralyzed, anesthetized patients. Anesthesiology. 2000;93:104–9. doi: 10.1097/00000542-200007000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Brimacombe J, Keller C, Fullekrug B, Agrò F, Rosenblatt W, Dierdorf SF, et al. A multicenter study comparing the ProSeal and Classic laryngeal mask airway in anesthetized, nonparalyzed patients. Anesthesiology. 2002;96:289–95. doi: 10.1097/00000542-200202000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Kuppusamy A, Azhar N. Comparison of bougie-guided insertion of Proseal laryngeal mask airway with digital technique in adults. Indian J Anaesth. 2010;54:35–9. doi: 10.4103/0019-5049.60494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brimacombe J, Keller C, Judd DV. Gum elastic bougie-guided insertion of the ProSeal laryngeal mask airway is superior to the digital and introducer tool techniques. Anesthesiology. 2004;100:25–9. doi: 10.1097/00000542-200401000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Taneja S, Agarwalt M, Dali JS, Agrawal G. Ease of Proseal Laryngeal Mask Airway insertion and its fibreoptic view after placement using Gum Elastic Bougie: A comparison with conventional techniques. Anaesth Intensive Care. 2009;37:435–40. doi: 10.1177/0310057X0903700306. [DOI] [PubMed] [Google Scholar]
- 8.Nagata T, Kishi Y, Tanigami H, Hiuge Y, Sonoda S, Ohashi Y, et al. Oral gastric tube-guided insertion of the ProSeal™ laryngeal mask is an easy and noninvasive method for less experienced users. J Anesth. 2012;26:531–5. doi: 10.1007/s00540-012-1361-2. [DOI] [PubMed] [Google Scholar]
- 9.Langeron O, Masso E, Huraux C, Guggiari M, Bianchi A, Coriat P, et al. Prediction of difficult mask ventilation. Anesthesiology. 2000;92:1229–36. doi: 10.1097/00000542-200005000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Lee A, Fan LT, Gin T, Karmakar MK, Ngan Kee WD. A systematic review (meta-analysis) of the accuracy of the Mallampati tests to predict the difficult airway. Anesth Analg. 2006;102:1867–78. doi: 10.1213/01.ane.0000217211.12232.55. [DOI] [PubMed] [Google Scholar]
- 11.McCrory CR, Moriarty DC. Laryngeal mask airway positioning is related to Mallampati grading in adults. Anesth Analg. 1995;81:1001–4. doi: 10.1097/00000539-199511000-00018. [DOI] [PubMed] [Google Scholar]
- 12.García-Aguado R, Viñoles J, Brimacombe J, Vivó M, López-Estudillo R, Ayala G. Suction catheter guided insertion of the ProSeal laryngeal mask airway is superior to the digital technique. Can J Anaesth. 2006;53:398–403. doi: 10.1007/BF03022507. [DOI] [PubMed] [Google Scholar]
- 13.Cook TM, Brooks TS, Van der Westhuizen J, Clarke M. The Proseal LMA is a useful rescue device during failed rapid sequence intubation: Two additional cases. Can J Anaesth. 2005;52:630–3. doi: 10.1007/BF03015775. [DOI] [PubMed] [Google Scholar]
- 14.García-Aguado R, Vivó M, Durá R, Tatay J, Cortés N. New method for inserting the Proseal laryngeal mask using an aspiration catheter in a case of difficult airway. Rev Esp Anestesiol Reanim. 2004;51:58–9. [PubMed] [Google Scholar]


