Abstract
Asthma represents a profound world-wide public health problem. The most effective anti-asthmatic drugs currently available include β2-agonists and glucocorticoids which can controls asthma in about 90-95% of patients. In Ayurveda, this miserable condition is comparable with Tamaka Shwasa type of Shwasa Roga. In the present study, 52 patients were treated with Sameera Pannaga Rasa at a dose of 30 mg twice a day for 4 weeks along with Nagavallidala (leaf of Piper betel Linn.) The results were assessed in terms of clinical recovery, symptomatic relief, pulmonary function improvement and on subjective and objective parameters. A significant improvement in subjective parameters, control on asthma, recurrence of asthma, increase in peak expiratory flow rate, considerable decrease in total and absolute, acute eosinophil count and erythrocyte sedimentation rate were observed. Overall marked improvement was found in 33.33%, moderate improvement in 44.44% and mild improvement in 20.00% was observed. The study reveals that Sameera Pannaga Rasa can be used as an effective drug in bronchial asthma.
Keywords: Bronchial asthma, pulmonary function, Sameera Pannaga Rasa, Shwasa
Introduction
Asthma represents a profound world-wide public health problem. The past decade has witnessed phenomenal increases in the incidences of asthma, asthma-related deaths and Glucocorticoids are the drugs frequently used (about 95%) in the treatment of bronchial asthma.[1] Currently glucocorticoid dependent asthma presents a great clinical burden and reducing the side-effects of glucocorticoids using novel steroid-sparing agents is needed.[2] However, the future therapies will need to focus on the 5-10% patients who do not respond well to these treatments and who account for approximately 50% of the health-care costs of asthma.[3] The surveys in adults show high prevalence of asthma symptoms and reduced lung functions particularly in lower socio-economic groups of the sufferers.[4,5] Asthma causes recurring episodes of wheezing, breathlessness, chest tightness and coughing, particularly at night or in the early morning. Common risk factors for asthma include exposure to allergens (such as those for house dust mites, animal with fur, cockroaches, pollens and mold),[6] occupational irritants,[7] tobacco smoke,[8] respiratory (viral) infections,[9] chemical irritants,[7] food allergies such as milk, peanuts and eggs[10] and psychological stress.[11] When airways are exposed to any of these risk factors; broncho-constriction will get manifested leading to inflammation. The airflow becomes limited and the patient suffers with the symptoms of asthma. The disease is comparable with Tamaka Shwasa type of Shwasa Roga in Ayurveda.[12] Ayurveda prefers a number of formulations to treat Tamaka Shwasa, which include few metallic preparation. Sameera Panaga Rasa (SPR) is an among such preperation, which is indicated in Tamaka Shwasa.[13]
SPR, an arsenal mercurial formulation is mentioned in Rasa Chandanshu in which Manahshila is not a component and later on it has been added by Ayurveda Aaushadhi Guna Dharma Shashtra. This later version has been accepted by Ayurvedic Formulary of India but, justification regarding the addition of Manahshila has not been provided. In addition to this; there is controversy regarding the final product, i.e., whether to collect Talastha or Ubhayastha (Galastha + Talastha). Considering this, it is planned to prepare SPR with and without Manahashila and collect Talastha and Ubhayastha one and compare their respective clinical efficacies in Tamaka Shwasa.
Materials and Methods
Selection of patients
For this study, 52 patients of bronchial asthma were registered from the out-patient department and inpatient department of Rasashastra and Bhaishajya Kalpana including Drug Research, IPGT and RA, Gujarat Ayurved University, Jamnagar. Of all, seven patients were dropped out and 45 completed the prescribed course of treatment. No direct or indirect drug related reason for discontinue of patient was noticed. All the patients registered in the study were informed about the nature of treatment. The study was started after obtaining approval from the Institutional Ethics Committee.
Criteria for inclusion
Age between 20 to 60 years
Difficulty in breathing
Paroxysmal attacks of dyspnea
Difficulty in expectoration
Wheezing sounds
Relief in upright position.
Criteria for exclusion
Age below 20 and above 60 years
Acute asthma requiring emergency medicines
History of Bronchiectasis, Tuberculosis, Pyothorax, Anemia, Malignancy, Diabetes Mellitus, Hypertention, Hepatic or Renal disease in the recent past
Dyspnea resulting from cardiac disease
Maha Shwasa, Urdhva Shwasa and Chhinna Shwasa (types of breathlessness explained in classics) which have been labeled as incurable in Ayurveda.
Posology
The trial drug (SPR) was prepared in the departmental laboratory by following standard manufacturing procedures (SMP). The formulation composition is shown in Table 1. SPR prepared without Manahshila was labeled as SPR and that prepared with Manahshila was labeled as SPRM. Groups for clinical trial were as follows:
Table 1.
Formulation composition of Sameera Pannaga Rasa
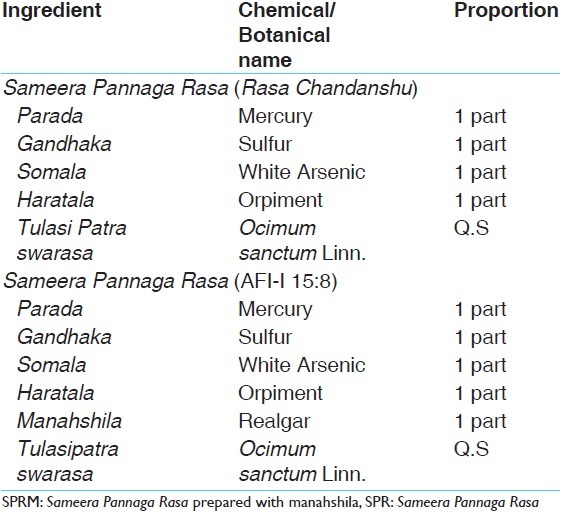
Group A: Treated with SPR prepared without Manahshila - Talastha (SPRT)
Group B: Treated with SPR prepared without Manahshila - Ubhayastha (Galastha + Talastha) (SPRU)
Group C: Treated with SPR prepared with Manahshila - Talastha (SPRMT)
Group D: Treated with SPR prepared with Manahshila - Ubhayastha (Galastha + Talastha) (SPRMU).
A capsule of 250 mg (containing 30 mg SPR + 220 mg starch powder) was administered twice a day for 28 days along with juice of Nagavallidala (leaf of Piper betel Linn.) as Sahapana (adjuvant). Follow-up was done after 2 weeks. Patients were advised not to get exposed to the susceptible triggering or aggravating factors narrated in Ayurveda as well as in modern texts.
Laboratory investigations
Routine hematological, biochemical investigations, and peak expiratory flow rate (PEFR) were done before and after the treatment. Sputum examination and chest X-ray were carried out to exclude pulmonary tuberculosis and other pulmonary diseases.
Assessment criteria
Registered patients were advised to visit the OPD at regular intervals of a week. Subjective and objective parameters were recorded in terms of improvement in pulmonary functions and other investigations. Overall assessment of the treatment was made on the basis of the results of the investigations as well as the symptomatic relief.
Results and interpretation
Overall effect of therapy on each scale was calculated with reference to percentage improvement in all symptoms, the relief was assessed on the below criteria:
<25% - Poor response/unchanged
26-50% - Mild improvement
51-75% - Moderate improvement
76-99% - Marked improvement
100% - Complete remission.
Statistical analysis
Wilcoxon signed rank test was applied to evaluate the overall effect of therapy. Paired t-test was applied to evaluate the effect on hematological, biochemical investigation and PEFR.
Observations and Results
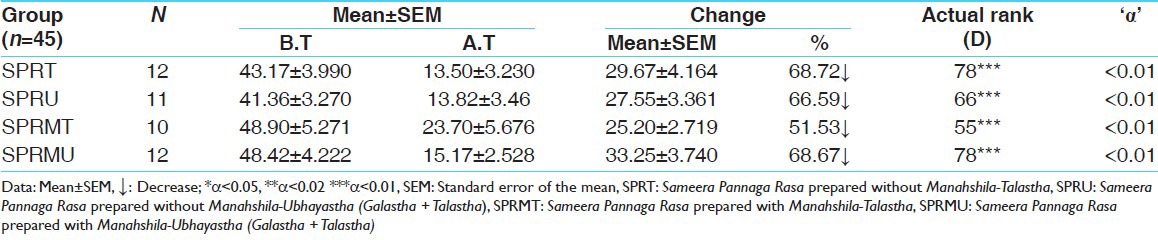
Four patients (33.33%) of SPRT group, four patients (36.36%) of SPRU group, two patients (20.00%) of SPRMT group and five patients of (41.67%) group SPRMU showed marked improvement. Five patients (41.67%) of SPRT group, five patients (45.45%) of SPRU group, three patients (30.00%) of SPRMT group and seven patients of (58.33%) group SPRMU showed moderate improvement and three patients (25.00%) of SPRT group, two patients (18.18%) of SPRU group and four patients (40.00%) of SPRMT group showed mild improvement. In SPRMT group, one patient (10.00%) did not respond to the treatment. Overall results have been tabulated in Table 2. All the groups have been found to be statistically highly significant providing in relief [Table 3].
Table 2.
Overall effect of the therapy (In percentage)
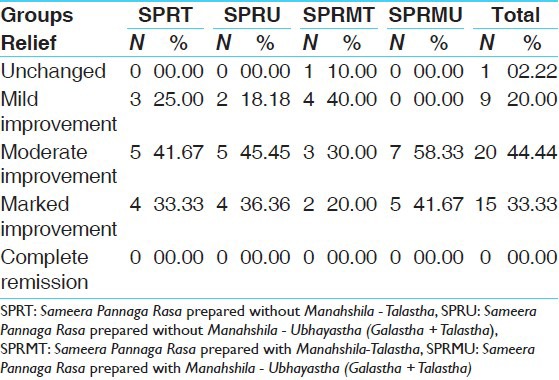
Table 3.
Effect of drugs on overall effect of therapy: (Applied Wilcoxon rank test)
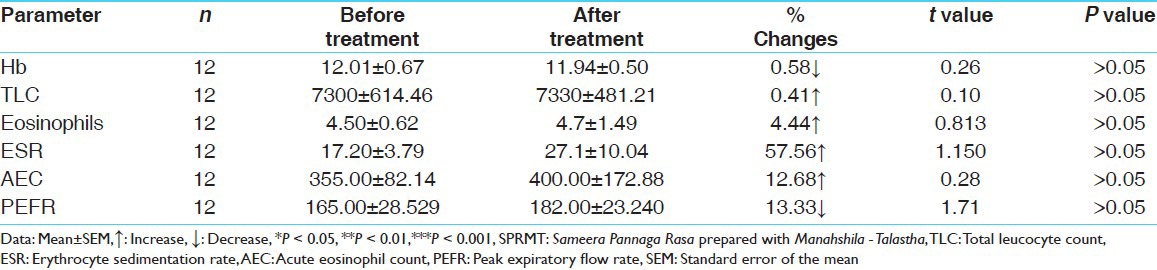
The reduction in eosinophils count, erythrocyte sedimentation rate (ESR) and total leucocyte count are found to be insignificant [Tables 4–7]. It was found in the study that, the duration, paroxysm, wheezing, chest tightness, nocturnal symptoms and dosage of allopathic emergency medicines were drastically reduced.
Table 4.
Hematological results of SPRT (applied paired t test)
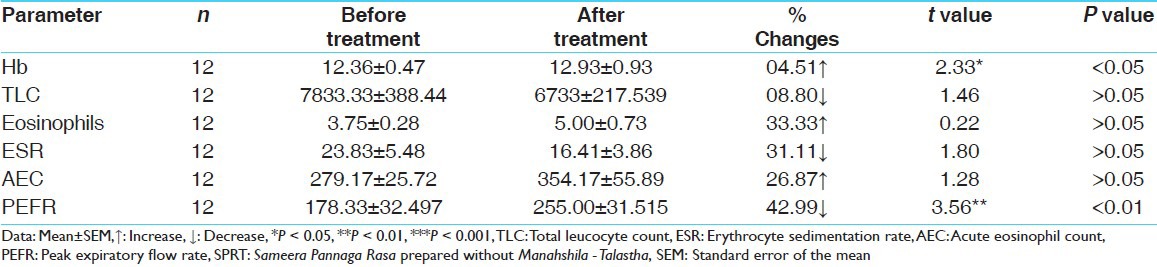
Table 7.
Hematological results of SPRMU (applied paired t test)
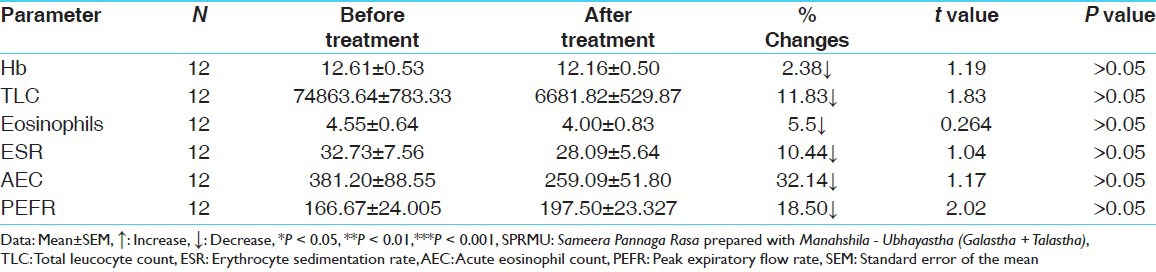
Table 5.
Hematological results of SPRT (applied paired t test)
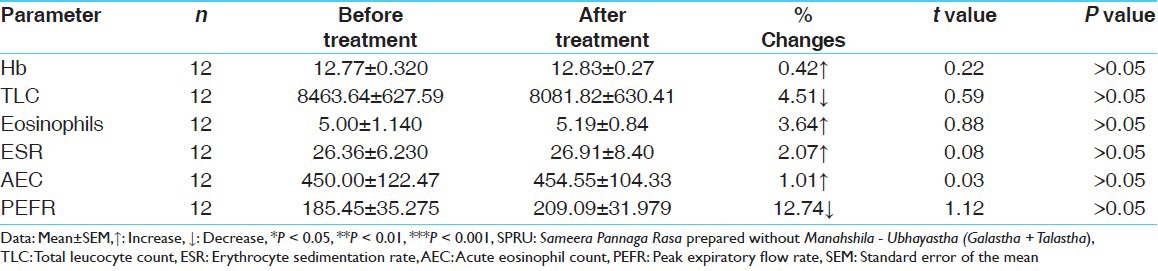
Table 6.
Hematological results of SPRMT (applied paired t test)
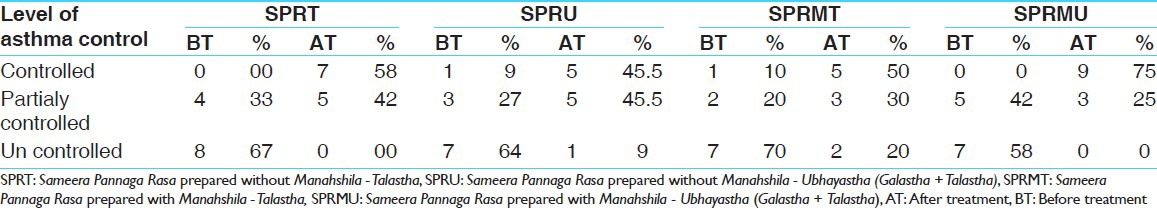
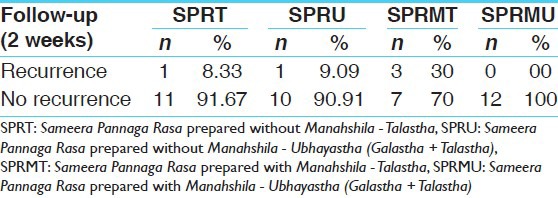
Interestingly, most of the patients in their follow-up period did not require the need of any emergency medication, particularly in SPRMU group followed by SPRT and SPRU group [Table 8]. Level of asthma control was higher in SPRMT group (50.00%) and in SPRU group (45.55%) [Table 9].
Table 8.
Effect of drugs on withdrawal of emergency drugs (applied Wilcoxon rank test)
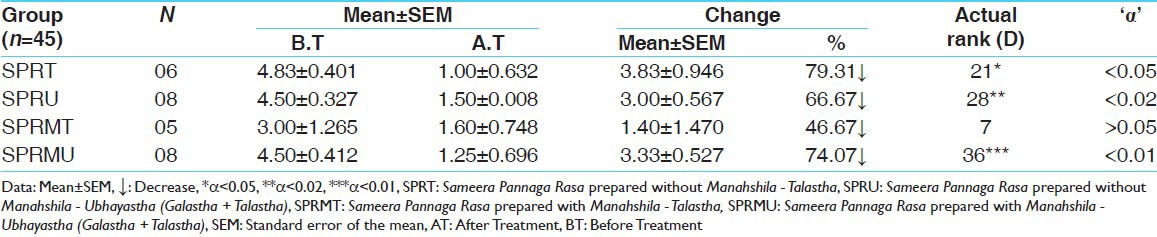
Table 9.
Level of asthma control before treatment and after treatment
As per ACT score, it was found that by SPRMU and SPRT groups provided statistically significant results in control of asthma [Table 10]. No recurrence of attacks was observed during follow-up period in SPRMU group [Table 11].
Table 10.
Effect of SPRT on asthma control† (applied χ2)
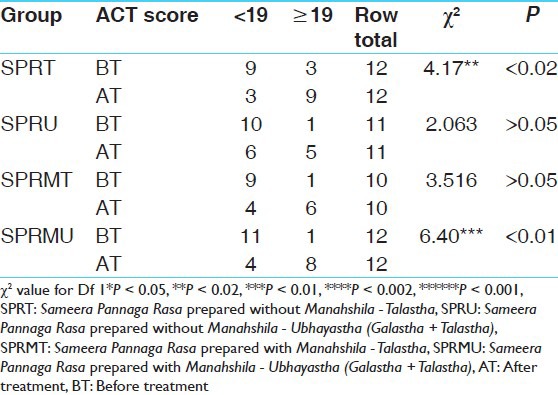
Table 11.
Recurrence asthma in follow-up period (in percentage)
Discussion
Survey of available literature points out that, vitiation of Vata, Kapha Dosha along with Prana, Udaka and Anna Vaha Srotas and Rasa Dhatu are the responsible factors in the manifestation of Tamaka Shwasa. The disease Shwasa has its root in the Pitta Sthana endorsed by Amashayodbhavaja Vikara.[14]
Considering the aggravated Vata and Kapha, Acharyas have advised the use of Vata kaphaghna, Ushna, Vatanulomaka drugs as first line of treatment in Shwasa. However, adoption of certain specification is always required for the breakdown of the three pathways of Samprapti. Furthermore, drugs exhibiting quick control over vitiated Vata and Kapha are required during Vegavastha, while exerting action on Agni or Pittasthana along with Vatakaphaghnata. Hence, logically, the drug administered in the treatment of Shwasa, should be able to overcome Vata and Kapha for immediate and symptomatic relief but should also pacify the Pitta for relief. Vagbhata emphasizes that, a drug acts by its Rasa, Vipaka, Virya, Guna and Prabhava. Normally, the effect of Rasa is less than that of Vipaka. Effect of Vipaka is lesser than that of Virya, which further is lesser than Prabhava, provided all are present in equal proportions. The overall pharmacodynamics of SPR is Katu Rasa, Ushna Guna, Ushna Virya, Katu Vipaka and Kapha Vataghna.[15] These dynamic actions are helpful in breaking the pathogenesis of Tamaka Shwasa. Asthma is now accepted as a T-helper type 2 lymphocyte-mediated chronic inflammatory disorder, characterized by airway eosinophilia and airway hyper responsiveness. Eosinophils appear to play a crucial role in the ongoing inflammation due to either an impaired clearance or a delayed apoptosis in the airways, where accumulation of a number of eosinophils cytotoxic proteins including major basic protein, cationic proteins and peroxidase could occur. As2o3 could alleviate the airway inflammation through promoting pulmonary eiosinophils (PE) apoptosis and lower PE infiltration. Low dose of As2o3 is proved to be effective with relative safety, it also has potential value in treating asthma.[16]
In modern point of view SPR is Mercury-Arsenical (Ubhayastha) or Arsenical preparation (Talastha).
In preparation of SPR, Tulsipatra Swarasa (leaf of Oscimum sanctum Linn.) as Bhavana Dravya is advocated. Studies have been proved that leaf extract of Ocimum sanctum is effective against arsenic induced toxicity. Ocimum sanctum has significant role in protecting animals from arsenic induced oxidative stress and in the depletion of arsenic concentration.[17] It has been proved that Ocimum extract can protect against mercury toxicity in mice. It significantly enhanced reduced glutathione, which is suggested that oral administration of Ocimum extract provides protection against mercury induced toxicity in Swiss albino mice.[18] Thus, Oscimum may help in nullifying possible ADRs of SPR.[19]
In the present study, Nagavallidala (P. betel) was taken as Sahapana for SPR. Studies have proved inhibitory effects of P. betel Linn. on production of allergic mediators by bone marrow derived mast cells and lung epithelial cells. PE significantly decreased histamine and granulocyte macrophage colony stimulating factors produced by an IgE mediated hypersensitive reaction and inhibited eotaxin and IL-8 secretion in a tumor necrosis factor-α and IL-4 induced allergic reaction.[20] Reduction of oxidative stress induced by free radicals by virtue of its anti-oxidant properties and chelation of heavy metals thereby minimizing its toxic potential and increasing safety margins were also found to be reported.[21] Considering all these, it is assumed that, Nagavallidala can reduce arsenic induced oxidative stress as well as the control of allergic diseases through inhibition of production of allergic mediators.
Conclusion
The results reveal that the SPR has a significant action in cases bronchial asthma and it could suppress total leukocyte count, eosinophil count, ESR and can improve PEFR along with providing symptomatic relief. Analysis of the data generated during the study shows that; all the groups of SPR have been highly significant in treating the condition. However, comparative evaluation shows that SPRMU group is better followed by SPRT and SPRU where SPRMT is less effective comparatively. None of the treated patients developed any adverse effects during the study period.
References
- 1.Agraval B, Mehta A. A clinical trial of Moringa olieophera Lam: Clinical study. Indian J Pharmacol. 2008;40:28–31. doi: 10.4103/0253-7613.40486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Caramori G, Groneberg D, Ito K, Casolari P, Adcock IM, Papi A. New drugs targeting Th2 lymphocytes in asthma. J Occup Med Toxicol. 2008;3(Suppl 1):S6. doi: 10.1186/1745-6673-3-S1-S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barnes PJ, Jonsson B, Klim JB. The costs of asthma. Eur Respir J. 1996;9:636–42. doi: 10.1183/09031936.96.09040636. [DOI] [PubMed] [Google Scholar]
- 4.Watson JP, Cowen P, Lewis RA. The relationship between asthma admission rates, routes of admission, and socioeconomic deprivation. Eur Respir J. 1996;9:2087–93. doi: 10.1183/09031936.96.09102087. [DOI] [PubMed] [Google Scholar]
- 5.Eachus J, Williams M, Chan P, Smith GD, Grainge M, Donovan J, et al. Deprivation and cause specific morbidity: Evidence from the Somerset and Avon survey of health. BMJ. 1996;312:287–92. doi: 10.1136/bmj.312.7026.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adkinson NF, Bochner BS, Busse WW, Holgate ST, Lemanske RF, Simons FE. Middleton's Allergy Principles and Practice. 7th Ed. St Louis, MO: Mosby Elsevier; 2008. Indoor allergens. [Google Scholar]
- 7.Nemery B, Hoet PH, Nowak D. Indoor swimming pools, water chlorination and respiratory health. Eur Respir J. 2002;19:790–3. doi: 10.1183/09031936.02.00308602. [DOI] [PubMed] [Google Scholar]
- 8.Jindal SK, Gupta D. The relationship between tobacco smoke and bronchial asthma. Indian J Med Res. 2004;120:443–53. [PubMed] [Google Scholar]
- 9.Zhao J, Takamura M, Yamaoka A, Odajima Y, Iikura Y. Altered eosinophil levels as a result of viral infection in asthma exacerbation in childhood. Pediatr Allergy Immunol. 2002;13:47–50. doi: 10.1034/j.1399-3038.2002.00051.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adkinson NF, Bochner BS, Busse WW, Holgate ST, Lemanske RF, Simons FE. Middleton's Allergy Principles and Practice. 7th ed. St Louis, MO: Mosby Elsevier; 2008. Adverse reactions to foods: Respiratory food hypersensitivity reactions. [Google Scholar]
- 11.Chen E, Miller GE. Stress and inflammation in exacerbations of asthma. Brain Behav Immun. 2007;21:993–9. doi: 10.1016/j.bbi.2007.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agivesha, Charaka, Dridhabala . Charaka Samhita Chikitsa Sthana, Hikkashwasa Chikitsa Adhyaya, 17/11. In: Vaidya Jadavaji Trikamji Acharya., editor. reprint edition. Varanasi: Chaukhambha Orientalia; 2011. p. 533. [Google Scholar]
- 13.Anonyms. 2nd revised ed. New Delhi: New Delhi, Department of Health and family welfare, Department of AYUSH, Govt. of India; 2009. Ayurvedic Formulary of India. Part 1. Section 15/8; p. 212. [Google Scholar]
- 14.Zhou LF, Yin KS. Effect of arsenic trioxide on apoptosis of pulmonary eosinophile in asthmatic guinea-pigs. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2002;22:292–4. [PubMed] [Google Scholar]
- 15.Agivesha, Charaka, Dridhabala . Charaka Samhita Chikitsa Sthana, Hikkashwasa Chikitsa Adhyaya, 17/147. In: Vaidya Jadavaji Trikamji Acharya., editor. reprint edition. Varanasi: Chaukhambha Orientalia; 2011. p. 539. [Google Scholar]
- 16.Maharaj SK. 17th ed. Almera: Published by Krishna Gopal Ayurveda Bhavan; 2006. Rasa Tantra Sara Va Siddha Praypga Sangraha Kupipakwa Prakarana/8; p. 278. [Google Scholar]
- 17.Sharmila Banu G, Kumar G, Murugesan AG. Effects of leaves extract of Ocimum sanctum L. on arsenic-induced toxicity in Wistar albino rats. Food Chem Toxicol. 2009;47:490–5. doi: 10.1016/j.fct.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 18.Sharma MK, Kumar M, Kumar A. Ocimum sanctum aqueous leaf extract provides protection against mercury induced toxicity in Swiss albino mice. Indian J Exp Biol. 2002;40:1079–82. [PubMed] [Google Scholar]
- 19.Bhavamishra . Revised. Varanasi: Chaukambha Bharati Academy; 2010. Bhava Prakash Nighantu-Purvardha, Pushpavarga/62-63. [Google Scholar]
- 20.Wirotesangthong M, Nagaki I, Tanaka Y, Thanakijcharoenpath W, Nagai H. Inhibitory effects of Piper betle on production of allergic mediators by bone marrow-derived mast cells and lung epithelial cells. Int Immunother. 2008;3:453–7. doi: 10.1016/j.intimp.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 21.Lean LP, Mohamed S. Antioxidative and antimycotic effects of turmeric, lemon-grass, betel leaves, clove, black pepper leaves and Garcinia atriviridis on butter cakes. J Sci Food Agric. 1999;79:1817–22. [Google Scholar]


