Abstract
Background:
The burden of diabetes and its foot complications is increasing in India. Prevention of these complications through foot care education should be explored. The objective of our study was to assess the risk factors of poor diabetic foot care and to find the effectiveness of health education in improving foot care practice among diabetes patients.
Materials and Methods:
A structured pre-tested questionnaire was administered to the outpatients of a rural health center with type 2 diabetes. Awareness regarding diabetes, care of diabetes and foot care practice ware assessed and scored. Individual and group health education focusing on foot care was performed. Foot care practice was reassessed after 2 weeks of education.
Results:
Only 54% were aware that diabetes could lead to reduced foot sensation and foot ulcers. Nearly 53% and 41% of the patients had good diabetes awareness and good diabetes care respectively. Only 22% of the patients had their feet examined by a health worker or doctor. The patients with poor, satisfactory and good practice scores were 44.7%, 35.9% and 19.4% respectively. Low education status, old age and low awareness regarding diabetes were the risk factors for poor practice of foot care. Average score for practice of foot care improved from 5.90 ± 1.82 to 8.0 ± 1.30 after 2 weeks of health education. Practice related to toe space examination, foot inspection and foot wear inspection improved maximally.
Conclusion:
Foot care education for diabetics in a primary care setting improves their foot care practice and is likely to be effective in reducing the burden of diabetic foot ulcer.
Keywords: Diabetes, diabetic foot ulcer, foot care, health education, India
INTRODUCTION
Currently, there are an estimated 366 million people affected with diabetes mellitus globally.[1] India is estimated to have 61.3 million diabetics, which is projected to cross 100 million by the year 2030.[1] Along with the rising prevalence of diabetes, an increase in its complications is expected. Diabetes along with its complications is expected to result in increasing morbidity, mortality and health expenditure due to the requirement of specialized care.[2] Furthermore, amputations due to diabetic foot ulcer are characterized by loss of productivity, which adds to the economic burden of diabetes.[3] The prevalence of diabetic foot ulcer among outpatient and inpatient diabetics in a rural Indian study was found to be 10.4%.[4]
Diabetic foot ulcer is a result of microvascular and neuropathic complications in diabetics. Studies such as the United Kingdom Prospective Diabetes Study have shown that proper control of blood glucose through diet, exercise and medications prevents the development of microvascular complications.[5] Furthermore, the practice of diabetic foot care including daily foot examination and use of appropriate footwear is considered important in its early detection and prevention of complications. People with poor knowledge and practice regarding diabetic foot care are known to have a higher incidence of diabetic foot ulcers.[6] On the other hand, simple health education measures can improve both the knowledge and practice regarding diabetic foot care.[7] Adoption of foot care practice after education has also been shown to reduce foot problems such as corns and callosities and promote healing of foot ulcers.[8] However, there is a dearth of studies in India, which assess the effect of health education on diabetic foot care practice of patients, especially in primary care setting. Thus, the objective of our study was to assess the risk factors for poor diabetic foot care and to determine the effectiveness of health education in improving diabetic foot care practice in a rural outpatient setting.
MATERIALS AND METHODS
Study design and setting
Our study design was cross-sectional with before and after comparison for diabetic foot care. We surveyed all the diabetic patients attending the weekly afternoon chronic disease clinic at our Institute Rural Health Center during March 2013. Patients visit the clinic every 2 weeks. A total of 103 diabetes patients were taking treatment at the health center at the time of the study. We administered a structured and pre-tested questionnaire to the patients. The diabetic foot care was reassessed after 2 weeks of health education.
Study instrument
The questionnaire consisted of four sections pertaining to awareness regarding diabetes, practice of diabetes care, practice of self-care of feet and feet examination details. The survey instrument on diabetic feet care was modified from a questionnaire prepared from the recommendation of the diabetes UK and used in previous studies.[9,10] It was administered by the investigator and MBBS interns who were adequately trained to ensure uniform data collection in the local language.
Finally, the patients were classified as having high-risk feet based on one of the five following criteria of the National Diabetes Education Program: Lack of protective sensation (sensory neuropathy), absent pedal pulses, foot deformity, current or past foot ulcer and history of foot amputation.[11] For testing sensory neuropathy, 10 g monofilament was applied on the plantar aspect of digits and the ball of great toe.
Health education
Following the questionnaire, each patient received face-to-face health education regarding self-care by the interns. This included advice for diet, exercise and regular medication and blood glucose checking. A ten-point education specific to diabetic foot care was also given. The total time allotted for the individual education session was 5-6 min. Group education by flipchart display and demonstration regarding foot cleaning, drying and foot examination was also done by nursing students for all patients. We assessed the foot care practice score after 2 weeks of initial data collection and health education.
Statistical analysis
The binary yes/no responses were converted into diabetes awareness and diabetes care scores, each ranging from 0 to 5 and diabetic foot care score ranging from 0 to 10. Diabetes awareness score and diabetes care score were divided into poor (0-3) and good (4-5) categories. Similarly, we divided the diabetic foot care score into poor (0-5), satisfactory (6-7) and good (8-10) categories.[10] Type of footwear use was also asked.
We explored the association of poor diabetic foot care practice with factors such as gender, low education status, old age, low income and low awareness and low diabetic care scores by calculating odds ratios. A P value of less than 0.05 was considered to be significant. Mann-Whitney U test was used to compare the baseline foot care scores across two categories. We used McNemar test to assess improvement in individual items of foot care practice following health education. We used Wilcoxon test to assess change in diabetic foot care practice score after health education. Mann-Whitney U test and Wilcoxon test were used, as the scores were not following a normal distribution.
RESULTS
Diabetes awareness
We covered 103 diabetics, consisting of 55 women and 48 men. Mean age of the patients was 54.8 ± 11.8 years. Only around half (54.4%) were aware that diabetes could cause reduced foot sensation leading to ulcers. Most of the patients were aware that diabetic feet could be prevented by diet, exercise and regular medication (91.1%) and that diabetic foot needed special care (85.7%). Around two-thirds (63%) of the patients were aware that diabetes could affect the various organs of the body. Only around one-third (33.0%) were especially aware that diabetes could lead to damage of the nerves. Considering these points, half of our patients (53.4%) were having good diabetes awareness score.
Diabetes care
The majority (58.3%) of patients followed diet-control and 45.6% patients did physical activity in addition to their routine work. Around three-fourth (75.7%) were having their blood glucose checked at least once in 3 months. A doctor or health worker had examined the feet of only 22.3% of the patients. Overall, 40.7% patients had a good diabetic care score comprising of regular blood glucose monitoring, foot examination at health center, compliance to diet and exercise and avoidance of smoking.
Foot care practice
Figure 1 shows that around half (47.6%) of the patients did not inspect their feet daily or their footwear regularly. The use of footwear outdoors was found among 97.1% of the patients, whereas indoor footwear use was found in 7.6% patients. Around 96.1% of patients reported that their footwear was fitting properly and 84.5% reported that they change their footwear whenever it gets damaged. Washing and drying of feet was present in 80.6% of the patients and healthy nail trimming using a curved nail clipper was found in 72.8% of the patients. However, only 22% of the patients used oil or moisturizers for their feet.
Figure 1.
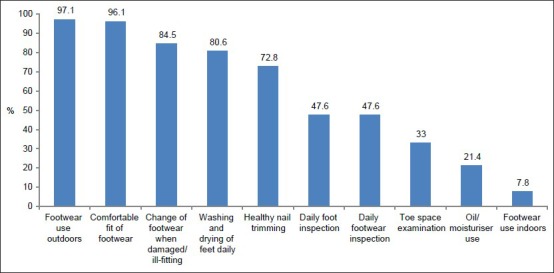
Diabetic foot care practice of 103 diabetic patients at baseline
After scoring, 44.7%, 35.9% and 19.4% of the patients had a poor, satisfactory and good diabetic foot care practice at the baseline. The use of slippers (chappals), sandal without strap, sandals with a strap or floaters was 78.7%, 15.5% and 3.0% respectively. Nobody was wearing shoes or footwear with therapeutic insole.
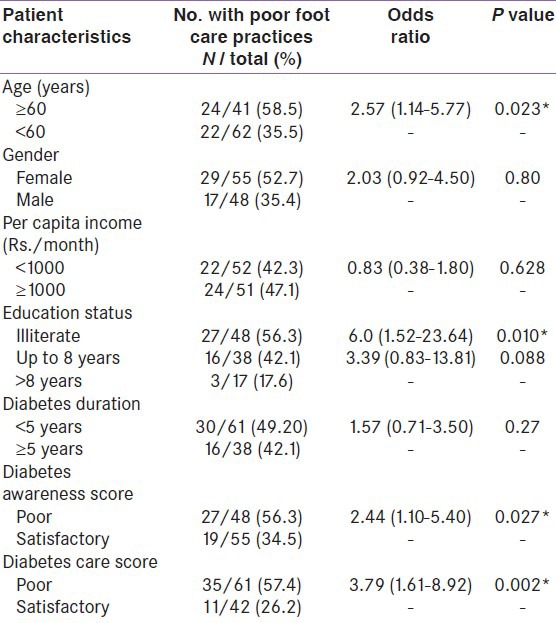
Risk factors for poor foot care practice
Low education status of patients was found to be associated with both poor diabetes awareness as well as poor diabetes care (P values 0.017 and 0.006, Chi-square test). Patients older than 60 years were at risk of having a poor diabetic foot care [Table 1]. However, there was no association with the duration of diabetes. Table 1 also shows that illiteracy, poor diabetic awareness score and poor diabetic care were associated with poor foot care practice.
Table 1.
Association of demographic variables as plausible risk factors for poor practice of diabetic foot care among 103 patients at baseline
High risk feet
Six patients were found to have high risk feet. Three patients had foot ulcers with peripheral neuropathy while another three had only neuropathy. Thus, the prevalence of diabetic foot ulcer was found to be 2.9% while that of sensory neuropathy was 5.8%. Diabetes awareness score was found significantly higher among high-risk patients compared with low-risk patients (4.83 vs. 3.09, P < 0.02, Mann-Whitney U test). Foot care practice was found better among patients with high risk feet compared with those with low risk feet; however, this was not found significant (7.0 vs. 5.84, P = 0.224, Mann-Whitney U test).
Effect of health education on foot care practice
Of the 103 patients who participated in baseline data collection and health education, only 60 could be contacted after 2 weeks. This was due to one of the next scheduled clinic visits falling on a holiday. Thus, dropout rate for reassessment of foot care practice was 42%. The percentage of females among those who dropped out and those who were reassessed was 51.2% and 55% and mean ages were 52.4 ± 10.3 and 56.5 ± 11.9 years, respectively. Diabetic foot care at baseline was similar in both the drop outs and returning patients as 46.5% and 43.3% had low foot care scores respectively. However, illiterates were higher among returning patients compared to those who dropped out (55.0% vs. 34.9%, P = 0.0437).
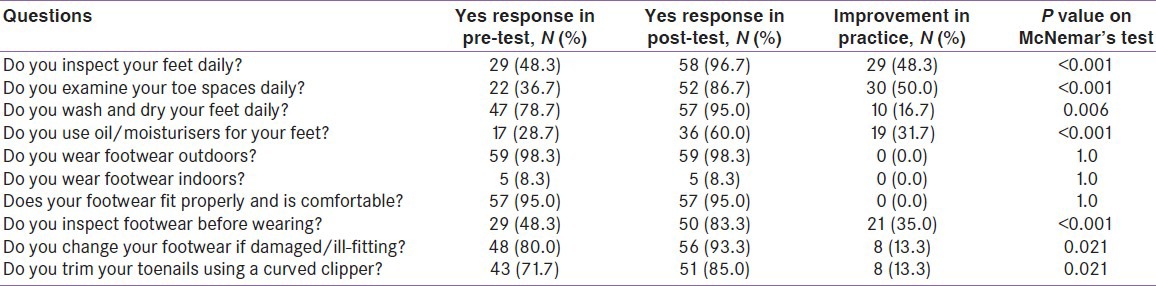
Out of these 60 returning patients, practice of 47 had improved, 12 had no improvement and one patient showed a reduction of score. The average foot care score at baseline was 5.90 ± 1.82 which improved to 8.0 ± 1.30 after 2 weeks of health education (P < 0.001, Wilcoxon test). Table 2 shows that foot care practices related to toe space examination, foot inspection and footwear inspection improved maximally (50.0%, 48.3% and 35% respectively). However, practice related to outdoor and indoor footwear use did not improve even after education.
Table 2.
Diabetic foot care practice before and after 2 weeks of health education for 60 patients
DISCUSSION
The awareness regarding diabetes leading to foot ulceration was similar to that of a Saudi study.[12] The fact that most of our patients knew that diabetic feet needs special care was a positive finding. However, around half the patients had a poor overall knowledge regarding diabetes, which was similar to the findings of earlier studies mostly in tertiary care settings.[9,10,12,13,14]
Out of all the factors assessed in diabetic care, foot examination was found to be the least satisfactory with only 22% having been examined. Regular blood glucose monitoring and compliance to diet and life-style advice were found to be comparatively better. This is in line with an earlier finding that foot care and health education were least suggested by doctors.[15] This shows a need to bring foot examination in diabetic care at primary care level by training the health workers and doctors.
The finding that patients with low educational status had poor awareness regarding diabetes has also been found in earlier studies done in Iran and Pakistan.[13,14] Also association between low educational status as well as low diabetes awareness level was found with poor practice of diabetic foot care, similar to another Pakistan study.[16] This suggests that education determines knowledge, awareness as well as practice of diabetic patients.
Practice of daily foot inspection found in our study was similar to that of earlier Nigerian and Saudi studies.[10,12] Barefoot walking was surprisingly found much lower (3%) in our study, compared with 62%, 38%, 18% and 10% in Iranian, Nigerian, Saudi and Indian multicentric studies respectively.[10,12,13,17] This might be explained by high awareness that diabetic foot need special care. However, footwear use was heavily skewed in favor of slippers (chappals) rather than sandals with strap, floaters or shoes which provide better support to the feet. No use of shoes was expected due to cultural reasons and a hot and humid climate. However, absence of use of therapeutic footwear points to a deficiency in care by the health-care providers. Regular footwear inspection being done in only half of our patients was similar to the findings of the Nigerian and Saudi studies.[10,12] Overall, the deficiency in foot care practice of patients was similar to that of the Nigerian and Pakistani studies where one-third to half of the patients were found to have poor foot care practice.[10,14]
The finding that patient education improved foot care practice was also shown in an Iranian study and a randomized controlled trial carried out in the UK.[7,18] However, there is insufficient evidence of the role of patient education in reducing outcomes such as ulcer and amputation incidence.[18,19] Furthermore in our study, the points of diabetic foot care did not improve equally even though education was given regarding all of them. Outdoor footwear use didn’t improve as it was already high, whereas indoor footwear use didn’t improve probably due to cultural reasons. Also there was no improvement in healthy nail trimming probably because a single education session was not sufficient to introduce this habit. Thus, diabetic foot care education should be regularly reinforced at outpatient clinic visits to be effective in the long run.
We had a limitation that turnout for post-test of foot care practice was not adequate. Furthermore, the improvement in clinical outcomes could not be studied due to the cross-sectional nature of the study.
CONCLUSION
We found that even 5-6 min of time devoted to individual patient education improved their foot care practice. When consistently reinforced, this education is likely to result in healthy habit formation, which may prevent disability and reduce medical expenditure in the long run. Furthermore, a training program of more than 3,000 primary care physicians in India showed that information on diabetic foot care was found highly educative by participants.[20] This shows a clear demand for learning foot care education and foot examination, among health providers. Thus integration of sustainable patient education at primary care level will be the most cost-effective way of reducing the burden of its complications.[21] Allocation of resources and training of health providers to ensure regular foot examination and foot education must be a priority of any strategy to control diabetes.
ACKNOWLEDGMENTS
We are thankful to Mr. Ramesh for his help in health education. We would like to acknowledge the help of doctors Aditya Gautam, Aishwarya PK, Deepak MJ, Krishin K, Surya Raj M, Tapan Gohain and Rajesh Raman for their help in data collection.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Unwin N, Whiting D, Guariguata L, Ghyoot G, Gan D, editors. 5th ed. Brussels, Belgium: International Diabetes Federation; 2011. Diabetes Atlas. [Google Scholar]
- 2.American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36:1033–46. doi: 10.2337/dc12-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schaper NC, Apelqvist J, Bakker K. Reducing lower leg amputations in diabetes: A challenge for patients, healthcare providers and the healthcare system. Diabetologia. 2012;55:1869–72. doi: 10.1007/s00125-012-2588-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehra BR, Thawait AP, Karandikar SS, Gupta DO, Narang RR. Evaluation of foot problems among diabetics in rural population. Indian J Surg. 2008;70:175–80. doi: 10.1007/s12262-008-0048-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) The Lancet. 1998;352:837–853. [PubMed] [Google Scholar]
- 6.Chellan G, Srikumar S, Varma AK, Mangalanandan TS, Sundaram KR, Jayakumar RV, et al. Foot care practice-the key to prevent diabetic foot ulcers in India. Foot (Edinb) 2012;22:298–302. doi: 10.1016/j.foot.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 7.Vatankhah N, Khamseh ME, Noudeh YJ, Aghili R, Baradaran HR, Haeri NS. The effectiveness of foot care education on people with type 2 diabetes in Tehran, Iran. Prim Care Diabetes. 2009;3:73–7. doi: 10.1016/j.pcd.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 8.Viswanathan V, Madhavan S, Rajasekar S, Chamukuttan S, Ambady R. Amputation prevention initiative in South India: Positive impact of foot care education. Diabetes Care. 2005;28:1019–21. doi: 10.2337/diacare.28.5.1019. [DOI] [PubMed] [Google Scholar]
- 9.Pollock RD, Unwin NC, Connolly V. Knowledge and practice of foot care in people with diabetes. Diabetes Res Clin Pract. 2004;64:117–22. doi: 10.1016/j.diabres.2003.10.014. [DOI] [PubMed] [Google Scholar]
- 10.Desalu OO, Salawu FK, Jimoh AK, Adekoya AO, Busari OA, Olokoba AB. Diabetic foot care: Self-reported knowledge and practice among patients attending three tertiary hospital in Nigeria. Ghana Med J. 2011;45:60–5. doi: 10.4314/gmj.v45i2.68930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bethesda (MD): National Institutes of Health, U.S. Department of Health and Human Services; 2000. National Diabetes Education Program. Feet Can Last a Lifetime: A Health Care Provider's Guide to Preventing Diabetes Foot Problems. [Google Scholar]
- 12.Al-Khaldi YM. Foot care among male diabetics in family practice center, Abha, Saudi Arabia. J Family Community Med. 2008;15:103–6. [PMC free article] [PubMed] [Google Scholar]
- 13.Khamseh ME, Vatankhah N, Baradaran HR. Knowledge and practice of foot care in Iranian people with type 2 diabetes. Int Wound J. 2007;4:298–302. doi: 10.1111/j.1742-481X.2007.00381.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hasnain S, Sheikh NH. Knowledge and practices regarding foot care in diabetic patients visiting diabetic clinic in Jinnah Hospital, Lahore. J Pak Med Assoc. 2009;59:687–90. [PubMed] [Google Scholar]
- 15.Shah VN, Kamdar PK, Shah N. Assessing the knowledge, attitudes and practice of type 2 diabetes among patients of Saurashtra region, Gujarat. Int J Diabetes Dev Ctries. 2009;29:118–22. doi: 10.4103/0973-3930.54288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saeed N, Zafar J, Atta A. Frequency of patients with diabetes taking proper foot care according to international guidelines and its impact on their foot health. J Pak Med Assoc. 2010;60:732–5. [PubMed] [Google Scholar]
- 17.Viswanathan V, Thomas N, Tandon N, Asirvatham A, Rajasekar S, Ramachandran A, et al. Profile of diabetic foot complications and its associated complications – A multicentric study from India. J Assoc Physicians India. 2005;53:933–6. [PubMed] [Google Scholar]
- 18.Lincoln NB, Radford KA, Game FL, Jeffcoate WJ. Education for secondary prevention of foot ulcers in people with diabetes: A randomised controlled trial. Diabetologia. 2008;51:1954–61. doi: 10.1007/s00125-008-1110-0. [DOI] [PubMed] [Google Scholar]
- 19.Dorresteijn JA, Kriegsman DM, Assendelft WJ, Valk GD. Patient education for preventing diabetic foot ulceration. Cochrane Database Syst Rev. 2012;10:CD001488. doi: 10.1002/14651858.CD001488.pub4. [DOI] [PubMed] [Google Scholar]
- 20.Murugesan N, Shobana R, Snehalatha C, Kapur A, Ramachandran A. Immediate impact of a diabetes training programme for primary care physicians – An endeavour for national capacity building for diabetes management in India. Diabetes Res Clin Pract. 2009;83:140–4. doi: 10.1016/j.diabres.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 21.Mohan V, Seedat YK, Pradeepa R. The rising burden of diabetes and hypertension in Southeast Asian and African regions: Need for effective strategies for prevention and control in primary health care settings. Int J Hypertens. 2013 doi: 10.1155/2013/409083. 409083. [DOI] [PMC free article] [PubMed] [Google Scholar]


