Abstract
Introduction:
Dyslipidemia is a primary, widely established as an independent major risk factor for coronary artery disease (CAD). Asians differs in prevalence of various lipid abnormalities than non-Asians. Hence, this study was conducted with objective to evaluate the lipid abnormalities and there correlation with traditional and non-traditional risk factors in known subjects with CAD.
Materials and Methods:
We studied the pattern and association of dyslipidemia with cardiovascular risk factors in 300 (Male: 216; Female: 84, age: 60.9 ± 12.4 years, range: 25-92 years) angiographically proved CAD patients. All patients were evaluated for anthropometry and cardiovascular risk factors and blood samples were collected for biochemical and inflammatory markers.
Results:
Hypercholesterolemia, hypertriglyceridemia and low high density lipoprotein (HDL) was present in 23.3%, 63.0% and 54.6% in the total study population respectively. A total of 41.3% had atherogenic dyslipidemia (raised triglycerides [TG] and low HDL). Percentage of patients with type-2 diabetes mellitus and hypertension were higher in subjects with atherogenic dyslipidemia. Insulin sensitivity was low; insulin and insulin resistance (IR) along with inflammatory markers were high in subjects with atherogenic dyslipidemia. Patients with atherogenic dyslipidemia had significantly lower serum vitamin B12 levels and higher homocysteine (Hcy) levels. Hypertriglyceridemia was positively correlated with insulin, homeostasis model assessment of IR, Hcy, interleukin-6, Tumor necrosis factor-alpha, highly sensitive C-reactive protein and negatively with vitamin B12 and quantitative insulin check index and an opposite correlation of all quoted parameters was observed with low HDL. The correlation of traditional and non-traditional risk factors was stronger with low HDL and high TG compared with hypercholesterolemia.
Conclusions:
Hypertriglyceridemia and low HDL cholesterol is common in patients with CAD compared with hypercholesterolemia. This suggests that different preventive strategy is required in Indian patients with CAD.
Keywords: Coronary artery disease, diabetes mellitus, dyslipidemia hypertension, inflammatory markers
INTRODUCTION
South Asians have a higher prevalence of cardiovascular risk factors, type-2 diabetes mellitus (T2DM) and earlier onset of cardiovascular disease (CVD) despite a normal body mass index (BMI) by international standards.[1,2] It is expected that individuals of Indian Asian ethnicity will account for 40-60% of global CVD burden within the next 10-15 years.[3] It has been hypothesized that higher risk observed in this ethnic group can be due to underlying genetic susceptibility[4] unmasked by environmental factors and excess accumulation of visceral body fat in adult life.[5] The metabolic abnormalities associated with increased visceral fat; raised triglycerides (TG) and low high density lipoprotein (HDL) cholesterol are more prevalent in individuals of South Asian origin.[1,6,7,8]
Dyslipidemia is a primary, widely established as an independent major risk factor for coronary artery disease (CAD) and may even be a prerequisite for CAD, occurring before other major risk factors come into play.[9] Studies have reported higher prevalence of lipid abnormalities among Asians compared with non-Asians.[10,11] Low HDL cholesterol and high TG concentrations have been implicated as possible independent predictors of CVD[11,12,13,14] and the combination of these two conditions are called as atherogenic dyslipidemia.[15] Asian Indian have a higher prevalence of low HDL cholesterol and lower prevalence of high cholesterol than non-Asian Indians,[16,17] which suggests impaired reverse cholesterol transport. These findings suggest the importance of high TG and low HDL cholesterol in Asian Indians compared with high cholesterol, which is more prevalent in western countries, which may have therapeutic implications.
The impact of dyslipidemia on the burden of CVD has been understudied in native South Asians, despite its large contribution to CVD in the other world populations.[16] Asian Indians have low prevalence of hypercholesterolemia and high prevalence of atherogenic dyslipidemia, which may have therapeutic implications. Hence, this study was conducted with objective to evaluate lipid abnormalities and there correlation with traditional and non-traditional risk factors in known subjects with CAD. We hypothesize that abnormalities of TG and HDL will be more prevalent and will reveal stronger association with CVD risk factors compared to total cholesterol in Indians patients with CAD.
MATERIALS AND METHODS
A total of 300 patients, who were admitted in Cardiology Department for evaluation of chest pain and found angiography positive, were selected in this study consecutively. Exclusion criteria were the presence of chronic kidney disease, hepatic dysfunction, known endocrinal (except diabetes mellitus) or rheumatologic diseases or chronic infections. All cases were interviewed using a questionnaire. Height, weight, waist, hip circumference were measured. BMI was calculated by dividing weight in Kg with the square of height in meters. Waist hip ratio (WHR) was calculated. Overweight/obesity was defined as BMI ≥25 kg/m2, central obesity by waist >90 cm in male and >80 in female, T2DM by history and criteria given by American Diabetes Association-2012, hypertension (HTN) by systolic and diastolic blood pressures ≥140 and 90 mmHg respectively. Atherogenic dyslipidemia was defined as TG level ≥150 mg/dl and HDL cholesterol level (<40 mg/dl) regardless of patient's gender.[18] In this study, relationship of individual lipid abnormalities was also studied and groups were made according to the presence or absence of lipid abnormality.
Fasting blood samples were collected after 14 h fasting. Lipids were measured by using cholesterol oxidase para aminoantipyrine, lipase/glycerol kinase (LIP/GK), enzymatic reaction respectively and low density lipoprotein (LDL) cholesterol and very low density lipoprotein cholesterol were calculated by Freidwald formula. Inter assay 3.84% and intra precision was 2% respectively for all biochemical parameters. HemoglobinA1c was measured by boronate affinity assay. Tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), highly sensitive C-reactive protein (hsCRP) and homocysteine (Hcy) were measured by ELISA (Enzyme linked immunosorbent assay) method with kits manufactured by Gen-probe Diaclone, France, Biochek, CA, USA and Axis-shield Diagnostic Ltd., UK respectively. Insulin, vitamin B12 and folic acid were done by micro-particle enzyme immunoassay (MEIA) and Ion Capture MEIA method respectively with commercial kits supplied by Abbott laboratory, USA. Intra assay and inter assay precision was <5% and <10% respectively for above parameters. Insulin resistance (IR) and sensitivity was calculated by using homeostatic model analysis (HOMA) model[19] (HOMA-IR = fasting insulin [μIU/ml) × fasting glucose (mmol/l]/22.5) and quantitative insulin check index (QUICKI) (QUICKI = 1/[log (fasting insulin μU/mL] + log[fasting glucose mg/dL])[20] respectively. The study was approved by Institutional ethics committee. Informed consent was obtained from all subjects. Vitamin B12 deficiency was defined by <200 pg/ml, folate deficiency by <3 ng/ml and hyperhomocysteinemia by >15 μmol/L.[21]
Statistical analysis was carried out using SPSS Version 20 (SPSS Inc. Chicago, USA). Data were presented as mean ± SD, median or number (%) unless specified. All non-parametric data such as HTN, dyslipidemia, smoking and number of vessel involved were analyzed by Chi-square test. All parametric data such as BMI, WHR, lipid parameters, HOMA-IR, vitamin B12, Hcy and inflammatory markers were analyzed by Student's t-test. If Bartlett's Chi-square test for equality of population variances was <0.05 then Kruskal-Wallis test was applied. Pearson correlation was used to evaluate the correlation between dependent variables like lipid parameters and independent variables like CVD risk factors. All non-parametric data were analyzed by Chi-square test. A P < 0.05 was considered as statistically significant.
RESULTS
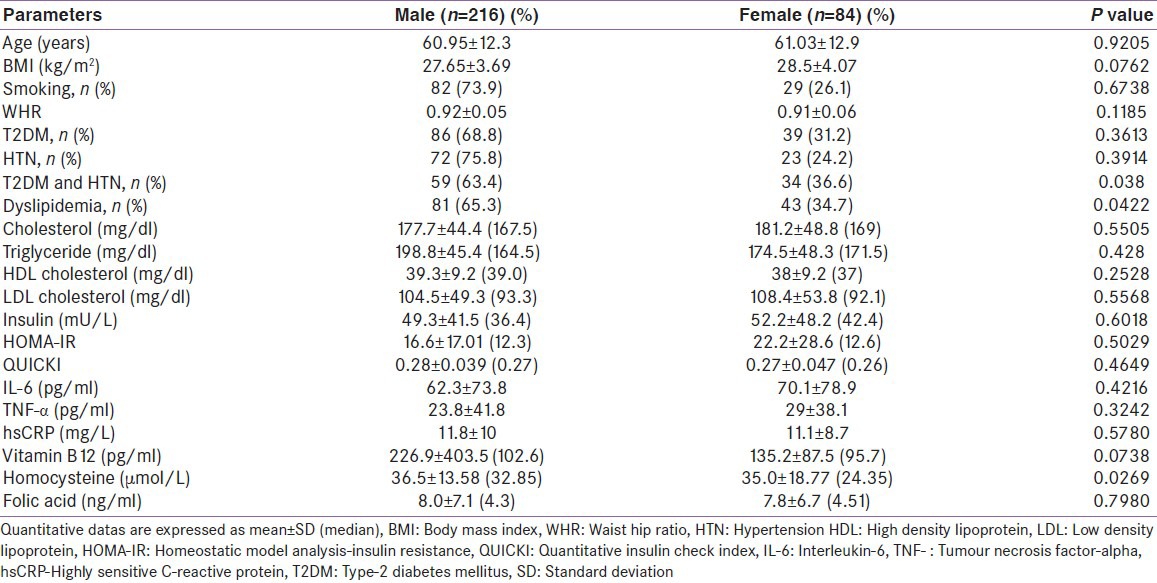
A total of patients with known CVD (Male: 216; Female: 84, age: 60.9 ± 12.4 years, range: 25-92 years) were studied. Table 1 shows baseline characteristics of the subjects studied. There was no age difference between males and females (Male: 60.95 ± 12.3; Female: 61.03 ± 12.9; P = 0.10). Males were more dyslipidemic when compared with females. Percentage of T2DM and/or HTN was higher in males compared with females.
Table 1.
Basic characteristics of the study population
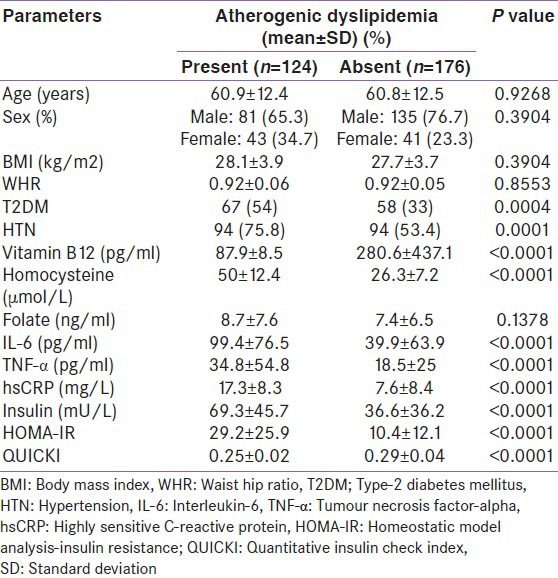
Among all patients with dyslipidemia, 54.6% had low HDL Cholesterol, 63.0% had hypertriglyceridemia and 23.3% had hypercholesterolemia. A total of 41.3% had atherogenic dyslipidemia in the present study. There was no association of atherogenic dyslipidemia with gender, age, BMI and WHR. T2DM and/or HTN were more common in patients with atherogenic dyslipidemia. Total cholesterol level (176.3 ± 42.6 vs. 180.4 ± 47.7, P = 0.44) and LDL cholesterol (102.6 ± 45.6 vs. 107.5 ± 53.7, P = 0.40) were comparable in patients with and without atherogenic dyslipidemia. There was no statistically significant difference in percentage of patients with hypercholesterolemia among patients with or without atherogenic dyslipidemia (22.6% vs. 23.9%; P = 0.90). Insulin sensitivity was low and insulin and IR along with inflammatory markers were high in subjects with atherogenic dyslipidemia [Table 2].
Table 2.
Status of traditional and non-traditional cardiovascular risk factors with atherogenic dyslipidemia
In the present study, percentage of patients withT2DM and HTN were higher in subjects with atherogenic dyslipidemia [Tables 3 and 4]. Percentage of patients with HTN was significantly higher in patients with hypercholesterolemia and there was no statistically significant difference in number patients with T2DM [Table 5].
Table 3.
Status of traditional and non-traditional cardiovascular risk factors with HDL levels
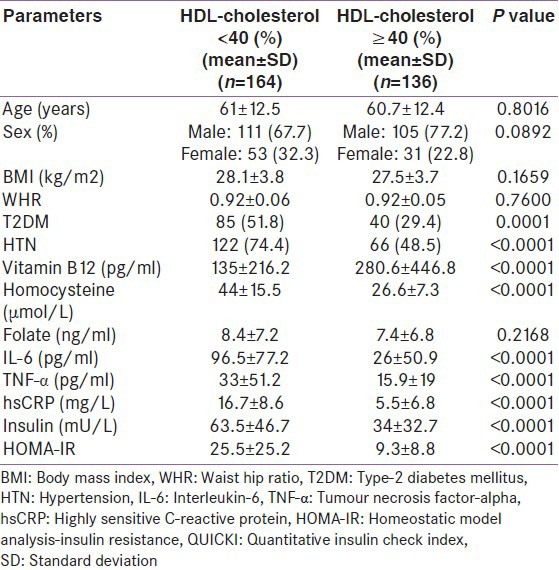
Table 4.
Status of traditional and non-traditional cardiovascular risk factors with triglyceride levels
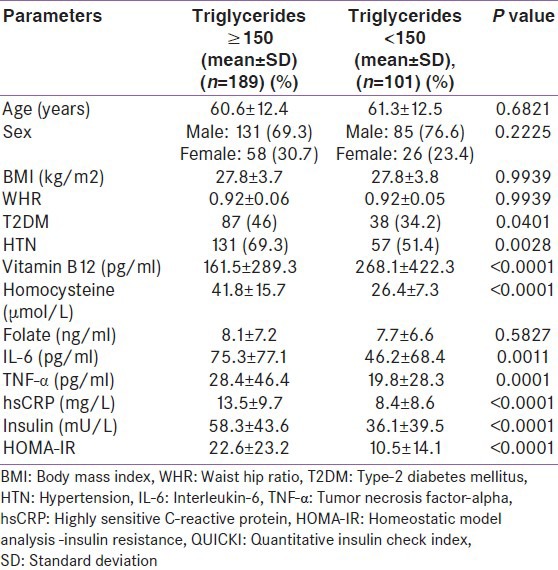
Table 5.
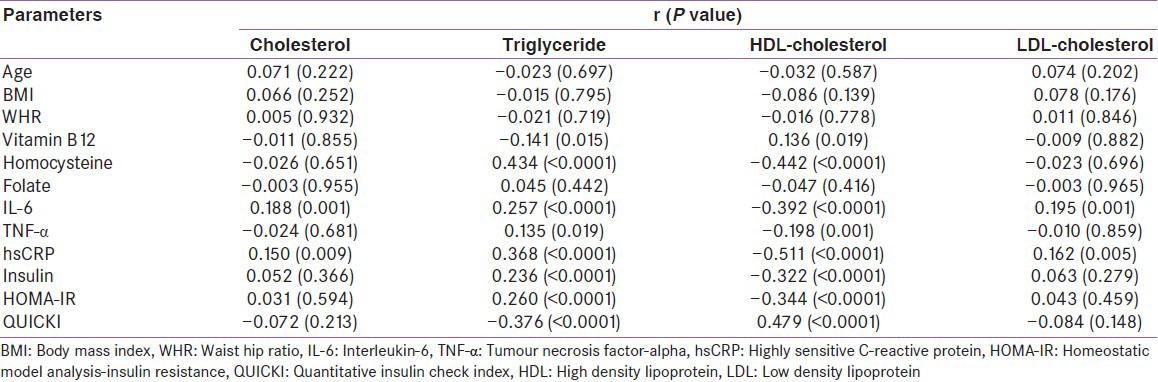
Correlation of traditional and non-traditional risk factors with lipid parameters
Patients with atherogenic dyslipidemia had significantly lower serum vitamin B12 levels and higher Hcy levels [Tables 3 and 4]. All subjects with atherogenic dyslipidemia were vitamin B12 deficient when compared with those without atherogenic dyslipidemia (100% vs. 77.3%; P < 0.0001) and had hyperhomocysteinemia (100% vs. 92%; P = 0.003). Similarly, IL-6, TNF-α, hsCRP, insulin and HOMA-IR levels were high and inpatients with atherogenic dyslipidemia. In patients with hypercholesterolemia, only levels of inflammatory markers were higher, but there was no statistical significant difference in serum vitamin B12, Hcy, insulin and HOMA-IR values.
Hypertriglyceridemia was positively correlated with insulin, HOMA-IR, Hcy, IL-6, TNF-α, hsCRP and negatively with vitamin B12 and QUICKI and an opposite correlation of all quoted parameters was observed with low HDL. Serum IL-6 and hsCRP were positively correlated with total cholesterol, but no significant correlation was observed with other non-traditional risk factors. The correlation of traditional and non-traditional risk factors was stronger with low HDL and high TG compared with hypercholesterolemia [Table 5 and Figure 1].
Figure 1.
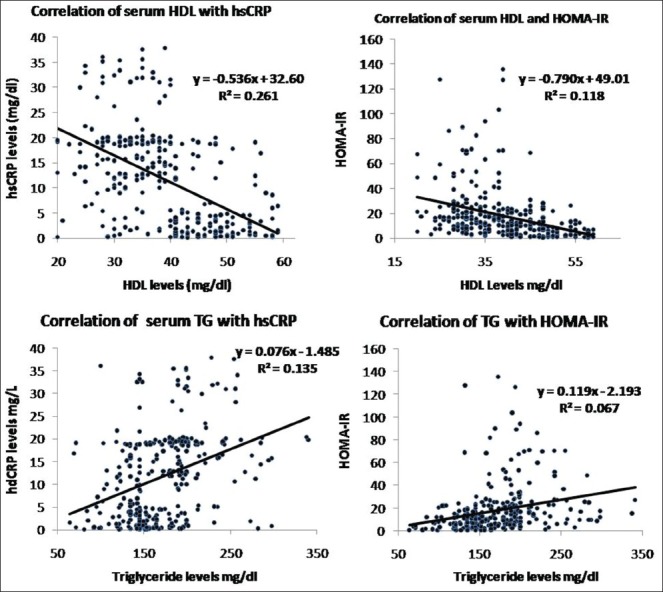
Correlation of serum triglycerides and high density lipoprotein cholesterol with inflammatory marker (highly sensitive C-reactive protein) and insulin resistance (homeostatic model analysis-insulin resistance)
DISCUSSION
Many population based prospective studies has been conducted to evaluate the impact of dyslipidemia on CVD.[2,7,11,17] Several studies have reported varying prevalence and type of dyslipidemia from different regions of India. The prevalence of high TG (28-72.2%), high LDL cholesterol (23.3-44.5%), low HDL (27-72.2%) and high total cholesterol (19-38.7%) were observed from north, west and southern part of India.[2,10,22,23,24,25] These variations can be explained by differences in the study population with respect to age and sex distribution, inclusion of patients with CVD and population or hospital-based study. There are limited studies, which have assessed differential relation of various dyslipidemia with CVD risk factors in patients with angiographically proven CAD.[24,25] In a study done in India (Delhi) in young (below 40 years) CAD patients, had high prevalence of raised TG (72.2%), low HDL (72.2%) and low prevalence of raised total cholesterol (29%), which is similar to our study.[25] In our study, atherogenic dyslipidemia was present in 41.3% of patients. In a study carried out in Italy, subjects with atherogenic dyslipidemia had comparable total cholesterol levels compared with those without atherogenic dyslipidemia, which is also similar to our study.[26] The Inter Heart investigators reported higher prevalence of dyslipidemia among study participants living in the five South Asian countries (45%) compared with participants from the other 47 countries represented in this study (35%).[10] Most western studies[27,28] and data from NHANES[29] emphasized the importance of elevated LDL and TC in the development of CAD compared to atherogenic dyslipidemia. This further highlights importance of low HDL and high TG in Indian population as cardiovascular risk factors compared with western population, which has also been highlighted by others.[10,13,16,17]
Atherogenic dyslipidemia is associated with age, gender, BMI and central obesity.[30] However, in the present study, there was no difference in age, gender, BMI and WHR in patients with or without dyslipidemia. Similar results were obtained in a study done in Italy, where no difference was observed in BMI in subjects with and without dyslipidemia with CAD.[26] All subjects in our study were of known CAD, which would have masked the relation of dyslipidemia with BMI and WHR. Most of our patients had mean WHR >0.9 and mean BMI >25, which were already higher than the normal population according to International and Indian Guideline,[31,32] which may explain no association observed in this study.
There were significantly higher numbers of subjects with T2DM and/or HTN in patients with than without atherogenic dyslipidemia. Contrary to this, in other study prevalence of HTN did not differ between patients with and without atherogenic dyslipidemia.[24] In univariate analysis, serum TG were correlated positively and HDL cholesterol was correlated negatively with the presence of T2DM and HTN. Similarly a weaker association was observed between blood pressure and atherogenic dyslipidemia in Genetic Epidemiology of Metabolic Syndrome Project, a family based study.[33] Atherogenic dyslipidemia also correlated with lower beta-cell function.[34] Patients with atherogenic dyslipidemia were more (HOMA-IR), had lower insulin sensitivity compared to those patients without dyslipidemia in the present study. In a similar study among CAD patients, subject with atherogenic dyslipidemia presented with comparable insulin levels, but higher IR.[24] IR is associated with atherogenic dyslipidemia and atherogenic dyslipidemia itself can aggravate IR.[35]
In the present study, total cholesterol, TG and LDL cholesterol showed significant positive and HDL cholesterol significant negative association with inflammatory markers (IL-6, TNF-α and hsCRP). Similar association has been reported by others.[36,37] A study from India in CAD patients[38] and a population based the Indian Atherosclerosis Research Study.[39] In T2DM patients a significant positive correlation between CRP and TG levels and a negative correlation with HDL levels was observed.[40]
In the present study, patients with atherogenic dyslipidemia had lower vitamin B12 and higher Hcy compared to those without it. In univariate analysis, TG were negatively correlated with vitamin B12 and positively with Hcy. As observed by us, other studies have noted a positive correlation between altered lipid profile and hyperhomocysteinemia.[41,42] However, other population based studies reported no correlation between Hcy and lipids.[43,44] Similar to our study higher plasma Hcy was associated with lower HDL level in a study done in Germany.[45] Hcy levels are positively correlated with serum TG and negatively with HDL cholesterol.[21] Vitamin B12 deficiency is common in Indians and Hcy is negatively correlated with vitamin B12 levels.[21]
Low HDL has been observed in Indian population since childhood and predicts CAD risk factors in large cohort followed up for more than 25 years.[46] Exact reason for this is unknown, but may be related to underlying genetic or environmental factors. The haplotype analysis in Chennai Urban Rural Epidemiology Study showed that the H+ Ser and H− -Ter were the “high-risk” and “low-risk” haplotypes for low HDL cholesterol and elevated TG levels, respectively. The H+ Ser haplotype of the lipoprotein lipase gene was associated with low HDL cholesterol levels and hypertriglyceridemia in Asian Indians.[47] Asians have higher IR compared with western population[5], which has been associated with atherogenic dyslipidemia.[16,23] Presence of nutritional deficiency since childhood may also contribute to high TG levels and low HDL levels. Vitamin B12 deficiency and hyperhomocysteinemia are common in Indians,[21] which has also been implicated in atherogenic dyslipidemia. The effect of Hcy on HDL cholesterol is probably related to inhibiting enzymes or molecules participating in HDL particle assembly. An animal study confirmed the negative correlation of HDL with Hcy in mice with targeted deletions of the genes for apolipoprotein E and cystathionine beta-synthase. It suggested suggest that Hcy-induced HDL-C and apoA-I inhibition represent a novel mechanism by which Hcy induces atherosclerotic CVD.[48] Low HDL may be related to underlying low grade inflammation. A study from India reported increased inflammatory markers compared to Caucasians, which is known to relate to low HDL.[49] It has been speculated that the reduced HDL seen in the inflammation result from increased serum concentration of serum amyloid A protein replacing apo-A1 as an apolipoprotein in HDL particles and that this leads to increased catabolism.[50]
CONCLUSION
The present study carried out in consecutive patients of CAD, provides and evidence for the importance of TG and HDL in CAD and also demonstrates its association with IR, inflammatory markers (hs-CRP, IL-6 and TNF-α) and hyperhomocysteinemia. Among Indian patients with CAD low HDL showed the strongest association with CVD risk factors followed by TG levels. Hypercholesterolemia shows weak association with CVD risk factors. Various trials in western population have shown the beneficial effect of lowering LDL cholesterol, but none or adverse effects of trials to increase HDL cholesterol on CAD.[18] Whether a similar effect will be observed in Indian population, which had different profile of dyslipidemia, remains unanswered. Hence, there is an urgent need for trials in Indian population with regards to treatment of dyslipidemia.
ACKNOWLEDGMENT
We thank Deenanath Mangeshkar Hospital and Research Center, Pune, for providing necessary facilities.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mohan V, Sandeep S, Deepa R, Shah B, Varghese C. Epidemiology of type 2 diabetes: Indian scenario. Indian J Med Res. 2007;125:217–30. [PubMed] [Google Scholar]
- 2.Joshi P, Islam S, Pais P, Reddy S, Dorairaj P, Kazmi K, et al. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297:286–94. doi: 10.1001/jama.297.3.286. [DOI] [PubMed] [Google Scholar]
- 3.Gaziano TA, Reddy KS, Paccaud F, Horton S, Chaturvedi V. Cardiovascular disease. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, et al., editors. Disease Control Priorities in Developing Countries. 2nd ed. New York: Oxford University Press; 2006. pp. 645–62. [Google Scholar]
- 4.Radha V, Mohan V. Genetic predisposition to type 2 diabetes among Asian Indians. Indian J Med Res. 2007;125:259–74. [PubMed] [Google Scholar]
- 5.Yajnik CS. Early life origins of insulin resistance and type 2 diabetes in India and other Asian countries. J Nutr. 2004;134:205–10. doi: 10.1093/jn/134.1.205. [DOI] [PubMed] [Google Scholar]
- 6.McKeigue PM, Ferrie JE, Pierpoint T, Marmot MG. Association of early-onset coronary heart disease in South Asian men with glucose intolerance and hyperinsulinemia. Circulation. 1993;87:152–61. doi: 10.1161/01.cir.87.1.152. [DOI] [PubMed] [Google Scholar]
- 7.Enas EA, Mehta J. Malignant coronary artery disease in young Asian Indians: Thoughts on pathogenesis, prevention, and therapy. Coronary Artery Disease in Asian Indians Study. Clin Cardiol. 1995;18:131–5. doi: 10.1002/clc.4960180305. [DOI] [PubMed] [Google Scholar]
- 8.Gupta M, Brister S. Is South Asian ethnicity an independent cardiovascular risk factor? Can J Cardiol. 2006;22:193–7. doi: 10.1016/s0828-282x(06)70895-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Genest JG., Jr Dyslipidemia and coronary artery disease. Can J Cardiol. 2000;16(Suppl A):3A–4. [PubMed] [Google Scholar]
- 10.Karthikeyan G, Teo KK, Islam S, McQueen MJ, Pais P, Wang X, et al. Lipid profile, plasma apolipoproteins, and risk of a first myocardial infarction among Asians: An analysis from the INTERHEART Study. J Am Coll Cardiol. 2009;53:244–53. doi: 10.1016/j.jacc.2008.09.041. [DOI] [PubMed] [Google Scholar]
- 11.Labreuche J, Touboul PJ, Amarenco P. Plasma triglyceride levels and risk of stroke and carotid atherosclerosis: A systematic review of the epidemiological studies. Atherosclerosis. 2009;203:331–45. doi: 10.1016/j.atherosclerosis.2008.08.040. [DOI] [PubMed] [Google Scholar]
- 12.Amarenco P, Labreuche J, Touboul PJ. High-density lipoprotein-cholesterol and risk of stroke and carotid atherosclerosis: A systematic review. Atherosclerosis. 2008;196:489–96. doi: 10.1016/j.atherosclerosis.2007.07.033. [DOI] [PubMed] [Google Scholar]
- 13.McBride PE. Triglycerides and risk for coronary heart disease. J Am Med Assoc. 2007;298:336–8. doi: 10.1001/jama.298.3.336. [DOI] [PubMed] [Google Scholar]
- 14.Rizos E, Mikhailidis DP. Are high density lipoprotein and triglyceride levels relevant in stroke prevention? Cardiovasc Res. 2001;52:199–207. doi: 10.1016/s0008-6363(01)00383-2. [DOI] [PubMed] [Google Scholar]
- 15.Fruchart JC, Sacks F, Hermans MP, Assmann G, Brown WV, Ceska R, et al. The residual risk reduction initiative: A call to action to reduce residual vascular risk in patients with dyslipidemia. Am J Cardiol. 2008;102:1K–34. doi: 10.1016/S0002-9149(08)01833-X. [DOI] [PubMed] [Google Scholar]
- 16.McKeigue PM, Miller GJ, Marmot MG. Coronary heart disease in south Asians overseas: A review. J Clin Epidemiol. 1989;42:597–609. doi: 10.1016/0895-4356(89)90002-4. [DOI] [PubMed] [Google Scholar]
- 17.Bhalodkar NC, Blum S, Rana T, Bhalodkar A, Kitchappa R, Kim KS, et al. Comparison of levels of large and small high-density lipoprotein cholesterol in Asian Indian men compared with Caucasian men in the Framingham offspring study. Am J Cardiol. 2004;94:1561–3. doi: 10.1016/j.amjcard.2004.08.040. [DOI] [PubMed] [Google Scholar]
- 18.Jellinger PS, Smith DA, Mehta AE, Ganda O, Handelsman Y, Rodbard HW, et al. American association of clinical endocrinologists’ guidelines for management of Dyslipidemia and prevention of atherosclerosis. Endocr Pract. 2012;18(Suppl 1):1–78. doi: 10.4158/ep.18.s1.1. [DOI] [PubMed] [Google Scholar]
- 19.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 20.Katz A, Nambi SS, Mather K, Baron AD, Follmann DA, Sullivan G, et al. Quantitative insulin sensitivity check index: A simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab. 2000;85:2402–10. doi: 10.1210/jcem.85.7.6661. [DOI] [PubMed] [Google Scholar]
- 21.Mahalle N, Kulkarni MV, Garg MK, Naik SS. Vitamin B12 deficiency and hyperhomocysteinemia as correlates of cardiovascular risk factors in Indian subjects with coronary artery disease. J Cardiol. 2013;61:289–94. doi: 10.1016/j.jjcc.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 22.Gupta R, Vasisht S, Bahl VK, Wasir HS. Correlation of lipoprotein (a) to angiographically defined coronary artery disease in Indians. Int J Cardiol. 1996;57:265–70. doi: 10.1016/s0167-5273(96)02800-8. [DOI] [PubMed] [Google Scholar]
- 23.Mohan V, Deepa R, Rani SS, Premalatha G Chennai Urban Population Study (CUPS No. 5) Prevalence of coronary artery disease and its relationship to lipids in a selected population in South India: The Chennai urban population study (CUPS No. 5) J Am Coll Cardiol. 2001;38:682–7. doi: 10.1016/s0735-1097(01)01415-2. [DOI] [PubMed] [Google Scholar]
- 24.Arca M, Montali A, Valiante S, Campagna F, Pigna G, Paoletti V, et al. Usefulness of atherogenic dyslipidemia for predicting cardiovascular risk in patients with angiographically defined coronary artery disease. Am J Cardiol. 2007;100:1511–6. doi: 10.1016/j.amjcard.2007.06.049. [DOI] [PubMed] [Google Scholar]
- 25.Sharma SB, Garg S, Veerwal A, Dwivedi S. hs-CRP and oxidative stress in young CAD patients: A pilot study. Indian J Clin Biochem. 2008;23:334–6. doi: 10.1007/s12291-008-0073-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sirimarco G, Deplanque D, Lavallée PC, Labreuche J, Meseguer E, Cabrejo L, et al. Atherogenic dyslipidemia in patients with transient ischemic attack. Stroke. 2011;42:2131–7. doi: 10.1161/STROKEAHA.110.609727. [DOI] [PubMed] [Google Scholar]
- 27.Neaton JD, Wentworth D. Serum cholesterol, blood pressure, cigarette smoking, and death from coronary heart disease. Overall findings and differences by age for 316,099 white men. Multiple risk factor intervention trial research group. Arch Intern Med. 1992;152:56–64. [PubMed] [Google Scholar]
- 28.Levy D, Kannel WB. Cardiovascular risks: New insights from Framingham. Am Heart J. 1988;116:266–72. doi: 10.1016/0002-8703(88)90099-3. [DOI] [PubMed] [Google Scholar]
- 29.Ninomiya JK, L’Italien G, Criqui MH, Whyte JL, Gamst A, Chen RS. Association of the metabolic syndrome with history of myocardial infarction and stroke in the Third National Health and Nutrition Examination Survey. Circulation. 2004;109:42–6. doi: 10.1161/01.CIR.0000108926.04022.0C. [DOI] [PubMed] [Google Scholar]
- 30.Micah FB, Nkum BC. Lipid disorders in hospital attendants in Kumasi, Ghana. Ghana Med J. 2012;46:14–21. [PMC free article] [PubMed] [Google Scholar]
- 31.Geneva: WHO; 2000. World Health Organization. Obesity: Preventing and managing the global epidemic. WHO Technical Report Series: No 894. [PubMed] [Google Scholar]
- 32.Misra A, Chowbey P, Makkar BM, Vikram NK, Wasir JS, Chadha D, et al. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India. 2009;57:163–70. [PubMed] [Google Scholar]
- 33.Wyszynski DF, Waterworth DM, Barter PJ, Cohen J, Kesäniemi YA, Mahley RW, et al. Relation between atherogenic dyslipidemia and the adult treatment Program-III definition of metabolic syndrome (Genetic Epidemiology of Metabolic Syndrome Project) Am J Cardiol. 2005;95:194–8. doi: 10.1016/j.amjcard.2004.08.091. [DOI] [PubMed] [Google Scholar]
- 34.Hermans MP, Ahn SA, Rousseau MF. The atherogenic dyslipidemia ratio [log(TG)/HDL-C] is associated with residual vascular risk, beta-cell function loss and microangiopathy in type 2 diabetes females. Lipids Health Dis. 2012;11:132. doi: 10.1186/1476-511X-11-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grundy SM. Atherogenic dyslipidemia associated with metabolic syndrome and insulin resistance. Clin Cornerstone. 2006;8(Suppl 1):S21–7. doi: 10.1016/s1098-3597(06)80005-0. [DOI] [PubMed] [Google Scholar]
- 36.Spranger J, Kroke A, Möhlig M, Hoffmann K, Bergmann MM, Ristow M, et al. Inflammatory cytokines and the risk to develop type 2 diabetes: Results of the prospective population-based European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam Study. Diabetes. 2003;52:812–7. doi: 10.2337/diabetes.52.3.812. [DOI] [PubMed] [Google Scholar]
- 37.Amanullah S, Jarari A, Govindan M, Basha MI, Khatheeja S. Association of HS-CRP with diabetic and non-diabetic individuals. Jordan J Biol Sci. 2010;3:7–12. [Google Scholar]
- 38.Bhagwat R, Gupte A, Yadav KS. Diagnostic utility of HS-CRP in coronary heart disease. Int J Mol Biol. 2012;3:36–9. [Google Scholar]
- 39.Rao VS, Kadarinarasimhiah NB, John S, Hebbagodi S, Shanker J, Kakkar VV. Usefulness of C-reactive protein as a marker for prediction of future coronary events in the asian Indian population: Indian atherosclerosis research study. Int J Vasc Med. 2010 doi: 10.1155/2010/389235. 389235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Akalin A, Alatas O, Colak O. Relation of plasma homocysteine levels to atherosclerotic vascular disease and inflammation markers in type 2 diabetic patients. Eur J Endocrinol. 2008;158:47–52. doi: 10.1530/EJE-07-0470. [DOI] [PubMed] [Google Scholar]
- 41.Gillum RF. Distribution of total serum homocysteine and its association with parental history and cardiovascular risk factors at ages 12-16 years: The Third National Health and Nutrition Examination Survey. Ann Epidemiol. 2004;14:229–33. doi: 10.1016/S1047-2797(03)00242-4. [DOI] [PubMed] [Google Scholar]
- 42.Huemer M, Vonblon K, Födinger M, Krumpholz R, Hubmann M, Ulmer H, et al. Total homocysteine, folate, and cobalamin, and their relation to genetic polymorphisms, lifestyle and body mass index in healthy children and adolescents. Pediatr Res. 2006;60:764–9. doi: 10.1203/01.pdr.0000246099.39469.18. [DOI] [PubMed] [Google Scholar]
- 43.Shai I, Stampfer MJ, Ma J, Manson JE, Hankinson SE, Cannuscio C, et al. Homocysteine as a risk factor for coronary heart diseases and its association with inflammatory biomarkers, lipids and dietary factors. Atherosclerosis. 2004;177:375–81. doi: 10.1016/j.atherosclerosis.2004.07.020. [DOI] [PubMed] [Google Scholar]
- 44.Yadav AS, Bhagwat VR, Rathod IM. Relationship of plasma homocysteine with lipid profile parameters in ischemic heart disease. Indian J Clin Biochem. 2006;21:106–10. doi: 10.1007/BF02913076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Obeid R, Herrmann W. Homocysteine and lipids: S-adenosyl methionine as a key intermediate. FEBS Lett. 2009;583:1215–25. doi: 10.1016/j.febslet.2009.03.038. [DOI] [PubMed] [Google Scholar]
- 46.Khalil A, Huffman MD, Prabhakaran D, Osmond C, Fall CH, Tandon N, et al. Predictors of carotid intima-media thickness and carotid plaque in young Indian adults: The New Delhi birth cohort. Int J Cardiol. 2013;167:1322–8. doi: 10.1016/j.ijcard.2012.03.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Radha V, Mohan V, Vidya R, Ashok AK, Deepa R, Mathias RA. Association of lipoprotein lipase Hind III and Ser 447 Ter polymorphisms with dyslipidemia in Asian Indians. Am J Cardiol. 2006;97:1337–42. doi: 10.1016/j.amjcard.2005.11.056. [DOI] [PubMed] [Google Scholar]
- 48.Liao D, Yang X, Wang H. Hyperhomocysteinemia and high-density lipoprotein metabolism in cardiovascular disease. Clin Chem Lab Med. 2007;45:1652–9. doi: 10.1515/CCLM.2007.358. [DOI] [PubMed] [Google Scholar]
- 49.Yajnik CS, Joglekar CV, Lubree HG, Rege SS, Naik SS, Bhat DS, et al. Adiposity, inflammation and hyperglycaemia in rural and urban Indian men: Coronary Risk of Insulin Sensitivity in Indian Subjects Study. Diabetologia. 2008;51:39–46. doi: 10.1007/s00125-007-0847-1. [DOI] [PubMed] [Google Scholar]
- 50.Han CY, Chiba T, Campbell JS, Fausto N, Chaisson M, Orasanu G, et al. Reciprocal and coordinate regulation of serum amyloid A versus apolipoprotein A-I and paraoxonase-1 by inflammation in murine hepatocytes. Arterioscler Thromb Vasc Biol. 2006;26:1806–13. doi: 10.1161/01.ATV.0000227472.70734.ad. [DOI] [PubMed] [Google Scholar]


