Abstract
Patellofemoral dislocations are frequently associated with chondral injury. Chondral and osteochondral lesions are often associated with traumatic (high energy) patellofemoral dislocations whereas atraumatic (low energy) patellofemoral dislocations in patients with significant patellofemoral risk factors have a much lower incidence of osteochondral damage. This article provides a historical overview and delineates the current state of radiographic and clinical outcomes of osteochondral lesions after patellofemoral dislocation. The importance of understanding risk factors of redislocation is emphasized and the current treatment options for these cartilage lesions associated with patellofemoral dislocation are briefly summarized.
Keywords: patella dislocation, osteochondral lesions, articular cartilage
Introduction
Articular cartilage lesions associated with patellar dislocations are common. However, it is important to recognize that the incidence and severity of these articular cartilage lesions is related to underlying anatomic factors. That is, the collateral damage associated with patellofemoral dislocations varies dependent upon the patient’s anatomy/pathoantatomy. It is intuitive that the amount of energy required for a dislocation to occur is inversely proportional to the amount of patellofemoral (PF) dysplasia. That is, very shallow morphology (highly dysplastic) with little bony restraint will allow a dislocation at lower energy levels than normal morphology would allow. This lower energy is associated with a lower magnitude of articular cartilage lesions in the acute setting when compared to a knee with normal morphology, which would require high-energy to dislocate such as in violent sporting accidents. Once the first dislocation has occurred, recurrent dislocations may lead to additional injury to the articular surfaces. These recurrent dislocations are another category. Surgeons would like to think that knees which undergo surgical “correction” to prevent further dislocations will experience less additional and/or less progression of chondral damage. However, careful attention is necessary to monitor these surgical outcomes. In the not too distant past, the Hauser procedure exhibited excellent results in terms of preventing instability yet at the expense of intermediate-term chondrosis progression.1,2 Additionally, Kuroda and Andrish demonstrated in the laboratory the potentially ill effects of over-medialization of the tuberosity, and Cosgarea demonstrated the potential overloading that could occur with non-anatomic positioning of an MPFL repair/reconstruction.3–5 It is, likewise, important to remember that "patellofemoral" dislocation includes the trochlea. This is not merely a semantic note, but meant to draw attention to the injuries that often occur at the femur. When considering the implications of chondral damage with PF dislocation, Nomura demonstrated with second- look arthroscopy after acute and recurrent patellar dislocations, some but not all articular cartilage lesions will progress in the near-term. Therefore, this article will not only describe the incidence and location of these lesions, but also help develop a thought process on when and how to treat these chondral lesions with the underlying goal of attempting to prevent chondrosis progression.
Incidence and location of articular cartilage lesions after patella dislocation
Historical Perspective
Osteochondral injury following acute patellar dislocation was described as early as 1905 when Kroner observed a large osteochondral fracture through the coronal plane of the patella following an acute lateral patellar dislocation.6 Reports of similar findings were echoed by Krida (1924) and Stewart (1925).7,8 In 1937 Meekison described a traumatic lateral patellar dislocation with injury to the inferomedial patella and suggested the mechanism was a resultant shearing force of the patella across the lateral femoral condyle.9 In 1945, Harmon presented an additional case of acute patellar dislocation and a cartilaginous defect of the medial patella. He suggested that these injuries can be present even if they are not visible on radiographs. He went on to describe the operative findings of the case, noting that the patella defect was replaced with fibrocartilage.10 Coleman (1948) added five additional cases in which he described two patients with acute patellar dislocation and osteochondral fracture of the patella and the lateral femoral condyle.11
Ahstrom (1965) was the first to suggest that there may be an underlying reason for a patella dislocation other than the acute trauma. He presented 18 cases of acute patellar dislocation with resultant osteochondral fracture in a series of patients with hypermobility, hypothesizing that the hypermobility predisposes the patella to dislocate and subsequently suffer an osteochondral fracture.12 In 1976, Rorabeck et al. studied a group of 18 patients with patella dislocations. He estimated the incidence of osteochondral fractures following patella dislocations to be around 5%.13 Cofield et al. (1977) evaluated a series of 50 patients with acute patellar dislocation between 1955 and 1969 and found 7 patients with radiographic evidence of osteochondral fracture with 6 at the medial patellar border and 1 at the lateral femoral condyle, giving an estimated incidence of 14%.14 Rorabeck also supported the notion that the reason for the osteochondral fracture was secondary to lateral shear forces acting on the patellofemoral joint during a lateral patellar dislocation. In their series, they reported this injury to predominantly affect the inferomedial pole of the patella, followed by lateral femoral condyle and combined fracture of both being less common.13
The Advent of Arthroscopy and MRI
After the adoption of arthroscopy and MRI, much higher rates of osteochondral fracture following dislocation have been reported. Hawkins et al. (1986) reported a 52% incidence by plain radiographs and arthroscopy.15 Kirsh et al. (1993) retrospectively used MRI to evaluate 26 patients with patellar dislocation and found a 58% incidence of patellar chondral or osteochondral fracture.16 Similarly, Virolainen et al. (1993) reported a rate of 76% osteochondral fracture.17
To evaluate the pediatric subgroup of osteochondral fracture following patellar dislocation, Nietosvaara et al. (1994) conducted a prospective two-year study to evaluate the true incidence of osteochondral fracture among children less than 16 years of age. Their findings showed a 39% incidence of osteochondral fracture.18 Stanitski (1996) supported the idea that patients with “hypermobility” of the patella may have a different incidence of articular fractures than patients with otherwise normal patellar stability. He found that overall 57% of patients suffered articular surface injury. He noted that patients with normal patellar stability who suffered traumatic first time dislocations were at a 2.5 times greater risk of articular surface damage compared to the “hypermobile” patients.19 Later in 1998, Stanitski revised his findings when he reported on 48 adolescent patients with acute patellar dislocation. He found 71% had articular damage by arthroscopic evaluation and reported that in 94% there was osteochondral injury, 6% there was chondral only damage, and 73% involved the medial facet of the patella. It is important to note that only 23% showed radiographic evidence of articular injury, which emphasizes that articular injuries following acute patellar dislocation are commonly missed radiographically. Furthermore, he emphasizes the importance of carefully considering the substantial diversity of patellar dislocations and argued for stratifying treatment by injury type (acute vs. recurrent dislocation), mechanism (contact vs. non-contact) and appreciating the age related differences.20 Sallay et al. (1996) evaluated 23 patients using MRI imaging and reported that 87% of patients had a bone contusion pattern at the periphery of the lateral femoral condyle near the level of the sulcus terminalis, 30% of patients sustained injury to the odd or medial patellar facet and 22% had loose body formation.21 In 2004, Beasley et al. reviewed the literature on the child and adolescent populations with patellar dislocation. The study identifying numerous predisposing risk factors to dislocation, including various anatomic derangements, such as patella alta, trochlear dysplasia, rotational malalignment, increased quadriceps angle and ligamentous laxity, as well as family history. As such, treatments strategies must be tailored to specific underlying causes for the greatest patient outcomes and high redislocation risk patients may require more aggressive surgical intervention.22
Progression of Cartilage damage/disease after high energy vs. low energy patellofemoral dislocation
In 2003, Nomura et al. added to the understanding of the pathology of articular damage with patellofemoral dislocation with a study of 39 knees after an acute lateral patella dislocation. He reported a 95% incidence of patellofemoral cartilage damage, 100% involvement of the patella and 31% of the lateral femoral condyle. Precise pathological evaluation of patellar lesions showed 7 (17%) had chondral or osteochondral fracturing and 9 (23%) had cracks (fissures) and 21 (54%) had lesions with both fracturing and cracks (fissures). Osteochondral defects were most commonly seen in the inferior medial facet of the patella and cracks were noted most frequently in the central dome consisting of 2 to 5 longitudinal striations. The authors suggested that caution should be taken as to avoid overlooking these discrete cartilage injuries as they believed these to be predictors of progressive chondral lesions.23 Following this original study, Nomura et al. (2004) went on to evaluate cartilage lesions longitudinally in patients with recurrent dislocation. In this study, 70 knees were evaluated after patella dislocation as well as after redislocation. He found that 96% had articular cartilage lesions of the patella with 76% showing fissuring, most commonly over the central dome and 77% with fissuring or erosions over the medial facet. The location of the more chronic appearing cartilage erosions was strongly correlated with the location of the cartilage lesion after the initial patella dislocation, suggesting that these more chronic cartilaginous changes were extensions of the original acute injury.24 In follow-up of this observation, Nomura et al. further evaluated 60 patients in 2005. He examined 30 patients with acute and 30 with recurrent patellar dislocation with second look arthroscopy. That study suggested that patients who had initial traumatic patella dislocations and no subsequent redislocations showed a progression to more severe cartilage damage than patients who suffered recurrent patella dislocations; supporting the notion that recurrent atraumatic (low energy) patella dislocations may indeed be less traumatic to the articular cartilage surface.25
This historical review suggests that acute patellofemoral dislocations result in predominantly lateral femoral condylar and medial patella facet lesions. The incidence is high and ranges from 70–93%. Bone bruises of the medial patella border and the lateral femoral condyle are present in 100% of all patients undergoing a first time traumatic patella dislocation, whereas in patients with recurrent or chronic patella dislocations the incidence of bone bruising is markedly lower. (It may be suggested for future investigations that this phenomenon is because the MPFL was injured with the first dislocation and thus less energy is required for subsequent dislocations to occur.)
As expected from the proposed mechanism of injury in the majority of cases the lateral femoral condyle lesions do not involve the weight-bearing articular surface (Figure 1). However, several case reports have been described in the literature suggesting that these injuries can be more extensive and affect the weight-bearing surface of the lateral femoral condyle26,27 when the injury (often delamination) extends from the lateral margin of the condyle to the central region of the condyle (Figure 2A-D). Mashoof et al. described this injury in a retrospective review of 7 cases over a six-year period of patellar dislocation from noncontact injury.26 Calleweir et al. later reported of a single case of a non-contact patellar dislocation in a 23 year-old patient that experienced resultant osteochondral fracture of the weight-bearing surface of the lateral femoral condyle.27 Sanders et al. (2006) published a review of acute patellar dislocation and associated MRI findings. In this retrospective radiological review of 25 cases, 20% (5/25) had an osteochondral injury to the mid-lateral weight-bearing portion of the lateral femoral condyle;28 evidence that these injuries are perhaps more common than previously reported.
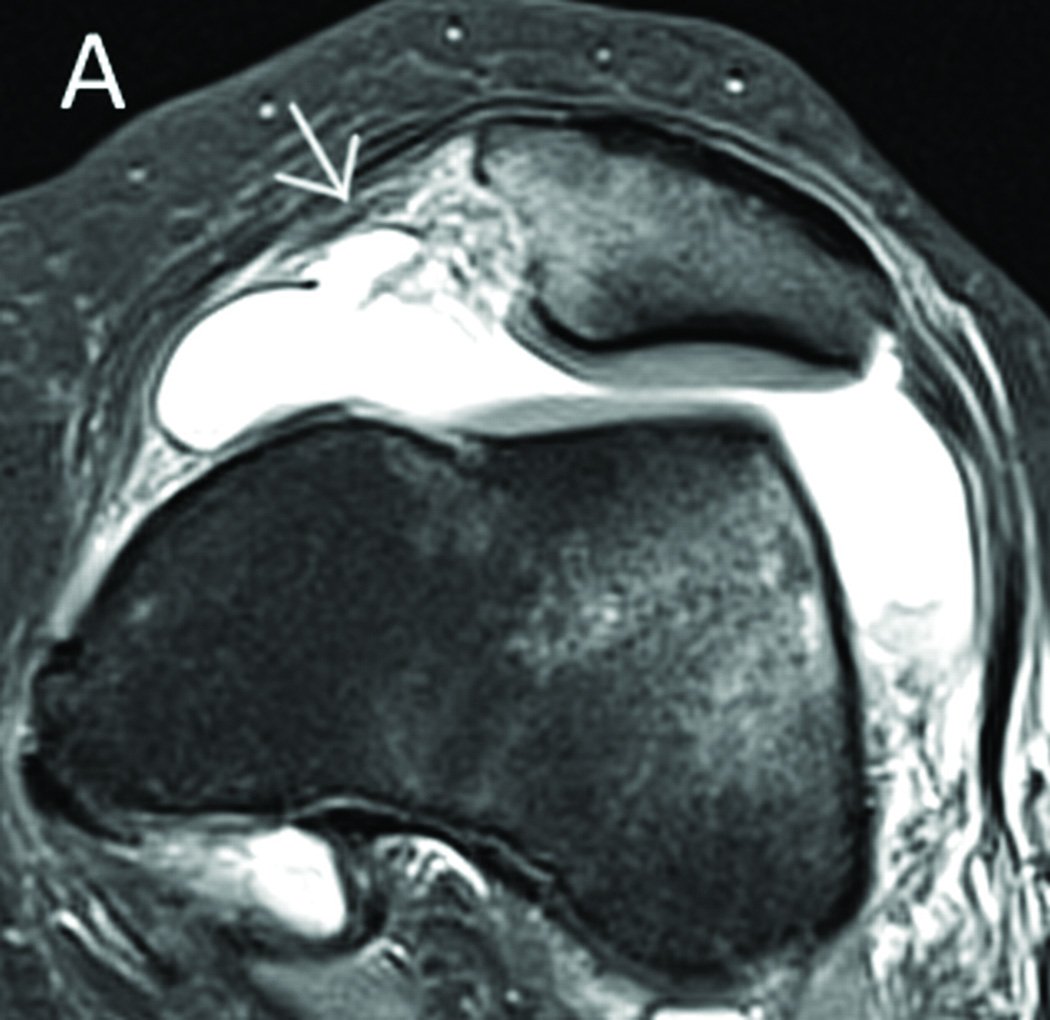
Figure 1.
MRI after an acute dislocation illustrates rupture of the MPFL (a) and a comminuted fracture of the medial facet of the patella with typical bone bruise pattern (b). Figure C shows a lesion to the non-weight bearing portion of the lateral femoral condyle.
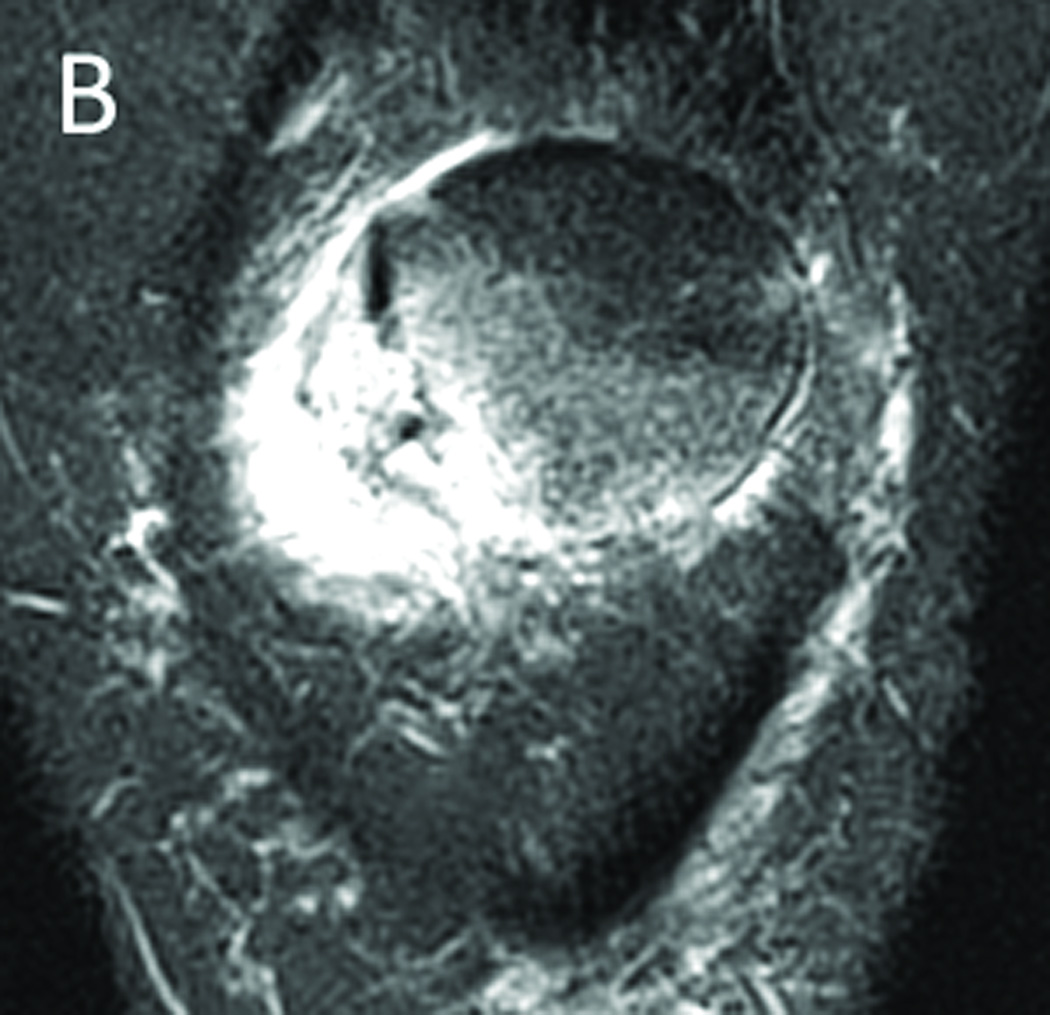
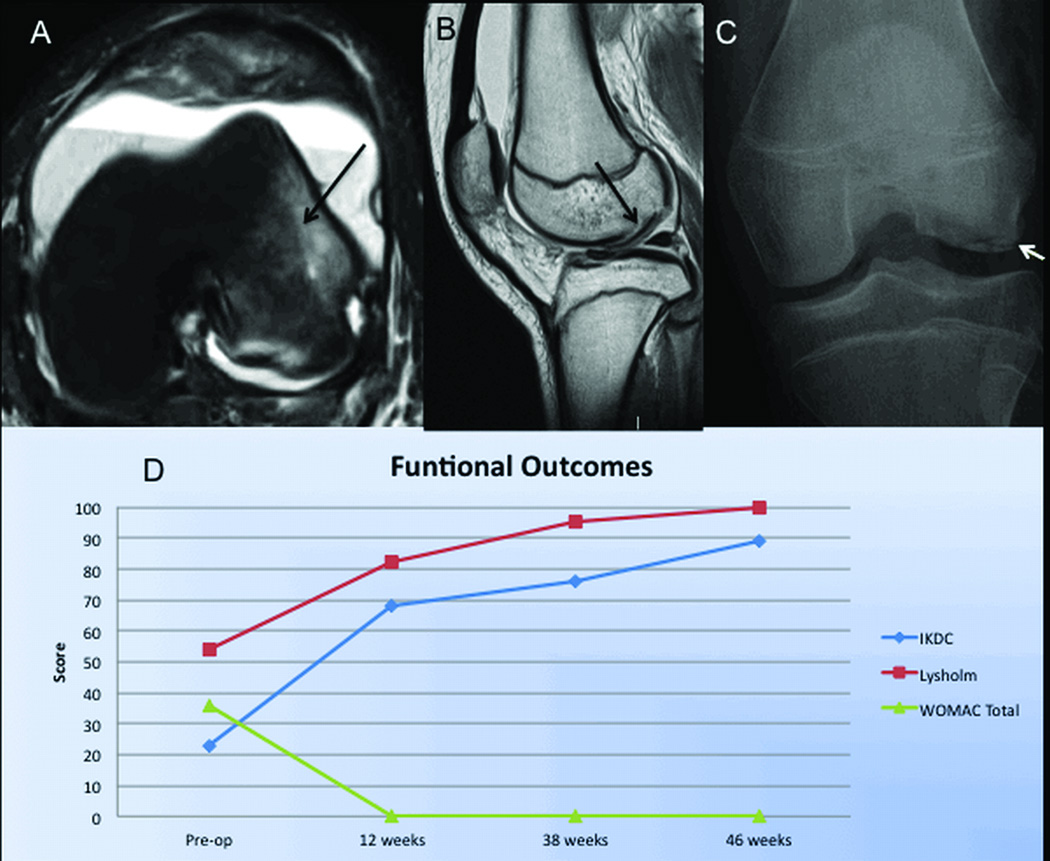
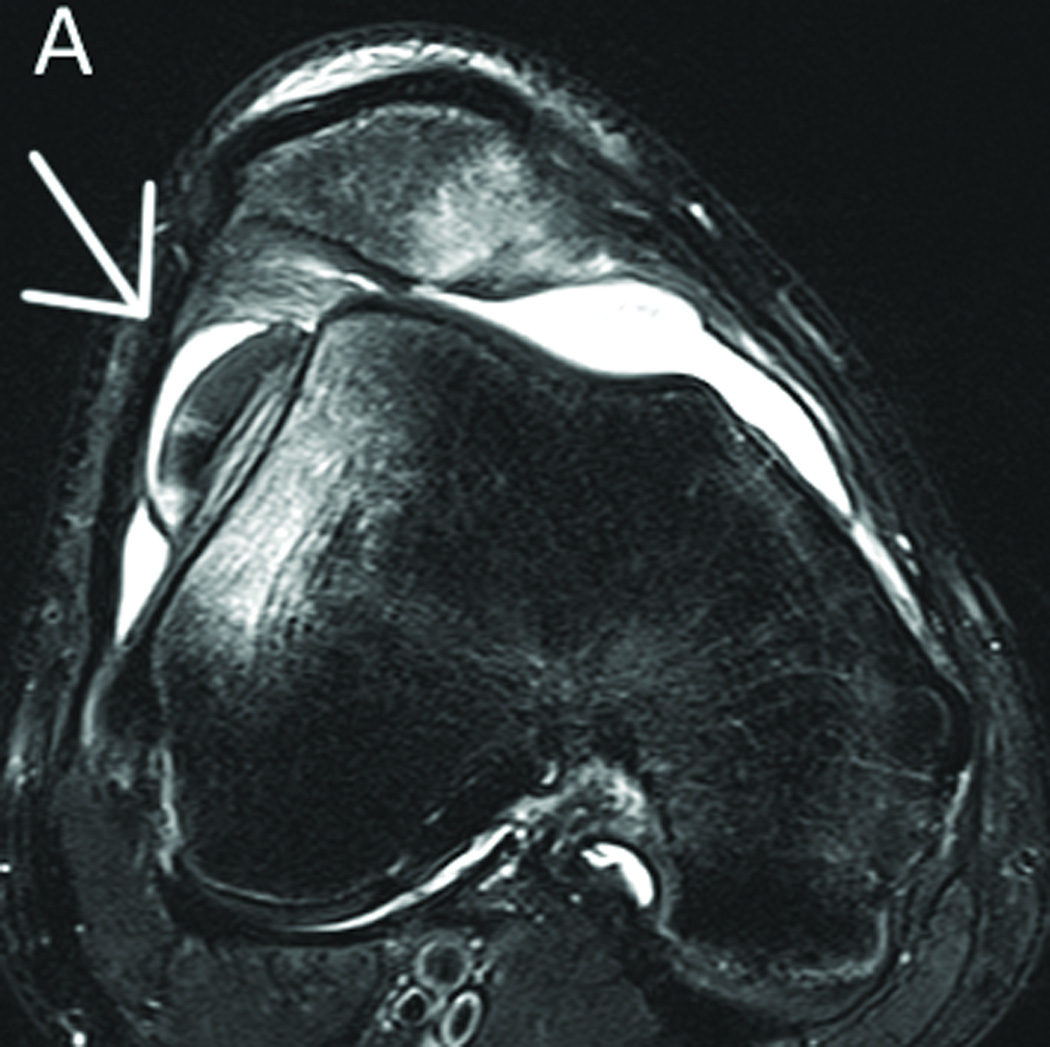
Figure 2.
Case example of a 13 year old female who suffered a traumatic patellofemoral dislocation with a large osteochondral fragment involving 2/3rds of the weight bearing surface of her lateral femoral condyle. Her initial x-rays and MRI show the typical lateral bone bruise (arrow A) and the clearly displaced fragment (black arrow B). After mini-open refixation of the fragment with double-pitched bioabsorbable screws (Arthrex, Naples, FL, USA) the fragment was well aligned (C white arrow). The patient-reported clinical outcomes measures (IKDC, WOMAC, Lysholm) showed a progression towards a normal knee function over 10 months post-operatively (D).
Clinical Outcomes in patella dislocations with articular cartilage lesions
In 1896 Hawkins et al. estimated that after a first time patellar dislocation, 30 to 50% of patients may suffer from residual symptoms of anterior knee pain and/or instability. Although the goal of the study was to define the role of operative treatment for osteochondral fracture, they were unable to make clear recommendations for surgical indications.15 Cash et al. (1998) compared operative versus non-operative treatment in patients suffering a traumatic patellar dislocation. In this study, 20 patients with loose bodies were treated with excision at the time of either arthroscopic or open surgical repair. Of these patients, only 1 patient reported poor result. In comparison, there were an additional 9 patients in the study who also had osteochondral fragments but underwent non-operative treatment for their loose bodies. 5 out of 9 of these (56%) reported poor results.29 These findings suggest that the presence of intra-articular osteochondral fractures clearly translate clinically into worse long-term patient outcomes and can be considered a relative indication for early surgical correction when identified. Nikku et al. in 2005 reported on 127 patients receiving operative versus non-operative treatment. The study concluded that the presence of loose body formation lowered both subjective and functional patient outcomes measures.30
In the evaluation of clinical outcomes, Sillanpaa et al. assessed subjective patient satisfaction following patella dislocation who underwent “non-anatomic” reconstruction of the medial patellofemoral ligament (MPFL) in a group of 37 patients at a minimum of 10 years follow-up. The study reported an incidence of 78% with osteoarthritis (OA) as determined by MR imaging and more than half of the patients reported unsatisfactory results. While only 22% reported recurrent instability of the patella, 78% of patients went on to develop OA thus highlighting that correction of instability alone does not prevent chondral breakdown and development of posttraumatic OA in the patellofemoral joint.31 This further illustrates the multifactorial nature of degenerative changes.
Acute versus chronic patellofemoral dislocation
It is important to evaluate not only the mechanism of the dislocation after an initial occurrence, but also to define the extent of chondral or osteochondral injury. With the low sensitivity of radiographs in detecting chondral and even osteochondral injury, it is prudent to obtain an MRI after the acute (first) patellar dislocation. Further knowledge about key anatomic parameters help to determine the extent of the potential damage suffered during the initial event. A patella dislocation in a patient with “normal” patellofemoral anatomy requires a significantly higher energy and thus is likely to lead to more severe chondral damage than a patella dislocation in a patient with patellofemoral dysplasia and/or patella alta. It is therefore important to analyze each parameter of the known risk factors for patellofemoral stability: patella alta, excessive lateral position of the tibial tuberosity (TT-TG), trochlear anatomy (dysplasia) and femoral/tibial axial rotation. This brings up the real world understanding that there is a broad continuum from normal anatomy to the extreme of pathoantatomy. The patient population anatomic range is quite variable in regards to trochlear dysplasia, patellar alta, femoral anteversion, tibial external torsion/lateral position of the tibial tuberosity and MPFL status. Just because a patient might be classified as having suffered a traumatic patella dislocation does not preclude a full evaluation of underlying risk factors for patellofemoral instability that may lead to chronic redislocations and unfavorable non-operative treatment. Not only are patients with these underlying risk factors for patellar instability at risk for redislocation, they are often at risk for PF dislocation of the contralateral knee.
Treatment of chondral and osteochondral lesions after patella dislocation
The treatment of focal lesions from chondral and osteochondral lesions varies extensively depending on defect size, damage to the osteochondral fragment and acuity of the injury. In a first time acute patella dislocation, the fragments can range in size from small comminuted pieces of debris to hemi-condylar avulsions. If there is a fragment that allows for technical fixation, then the fragment should be rescued and fixed in-situ. If fixation is performed, this should be performed according to best chondral practices using interfragmentary compression with absorbable or non-resorbable cannulated screws that may require hardware removal (Figure 3). Chronic lesions need to be addressed from a more restorative point of view. Partial thickness lesions less than 1cm2 may be potentially asymptomatic and may require only simple stabilization chondroplasty. In small full thickness lesions (1cm2), microfracture may be appropriate although in weightbearing areas of the patella as well as in small to medium size lesion (1–4cm2) results have been unfavorable for this technique32,33
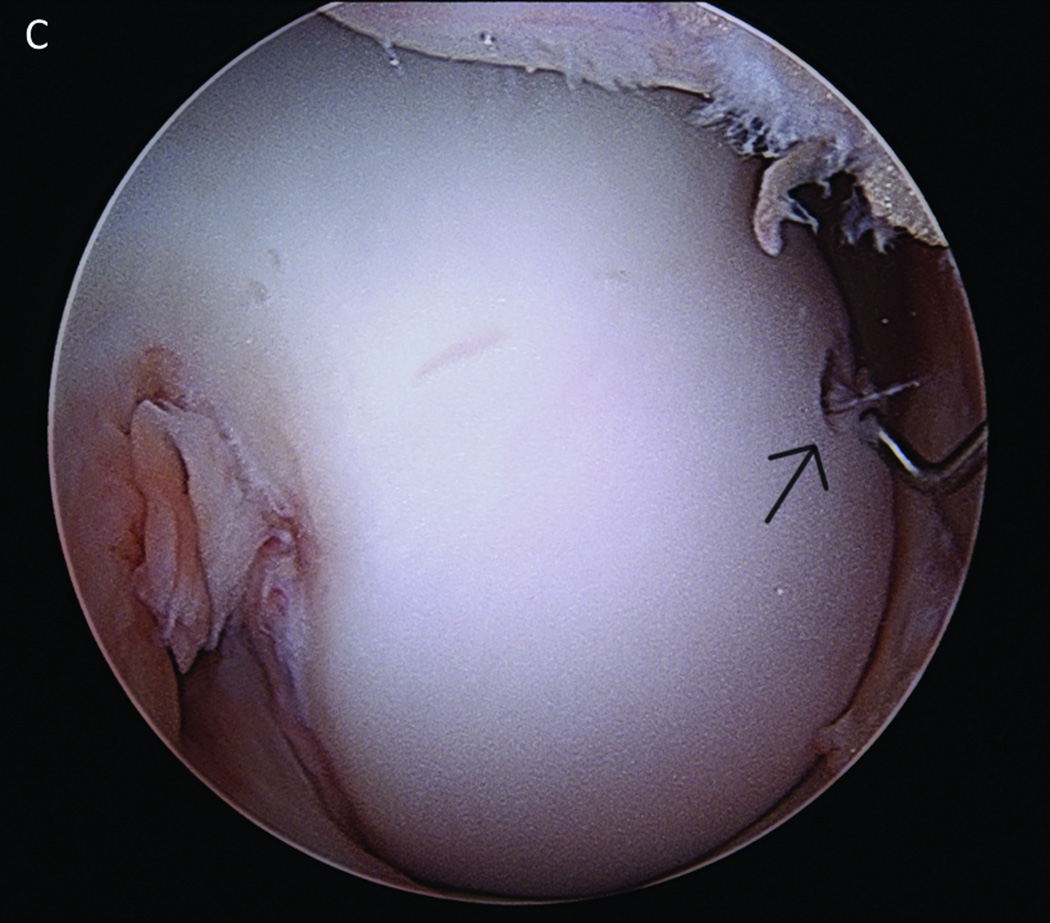
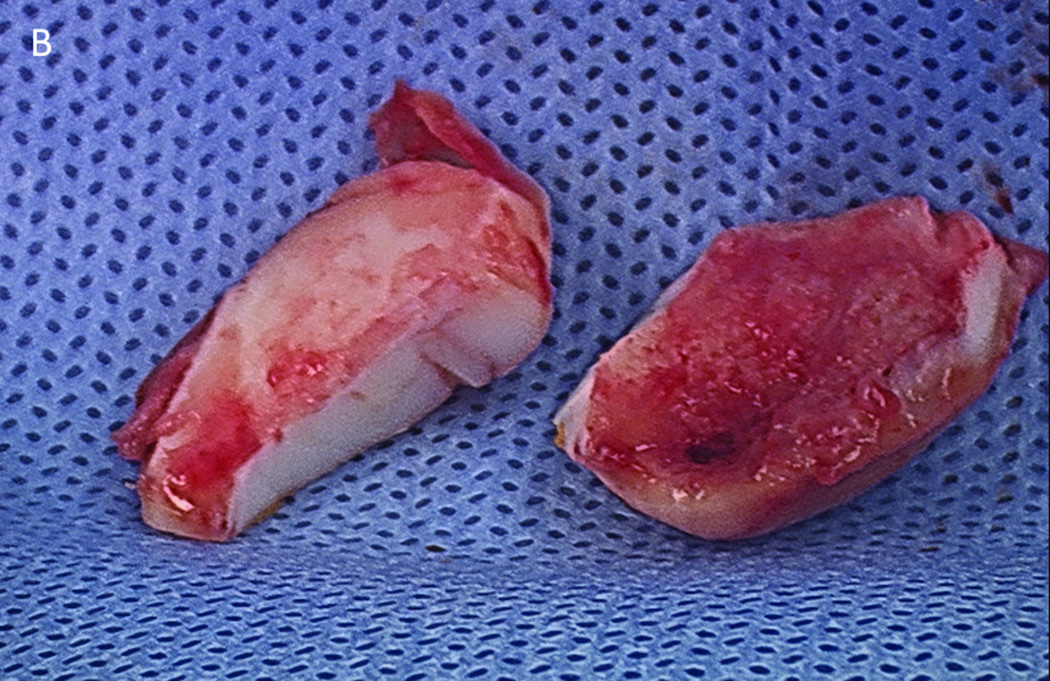
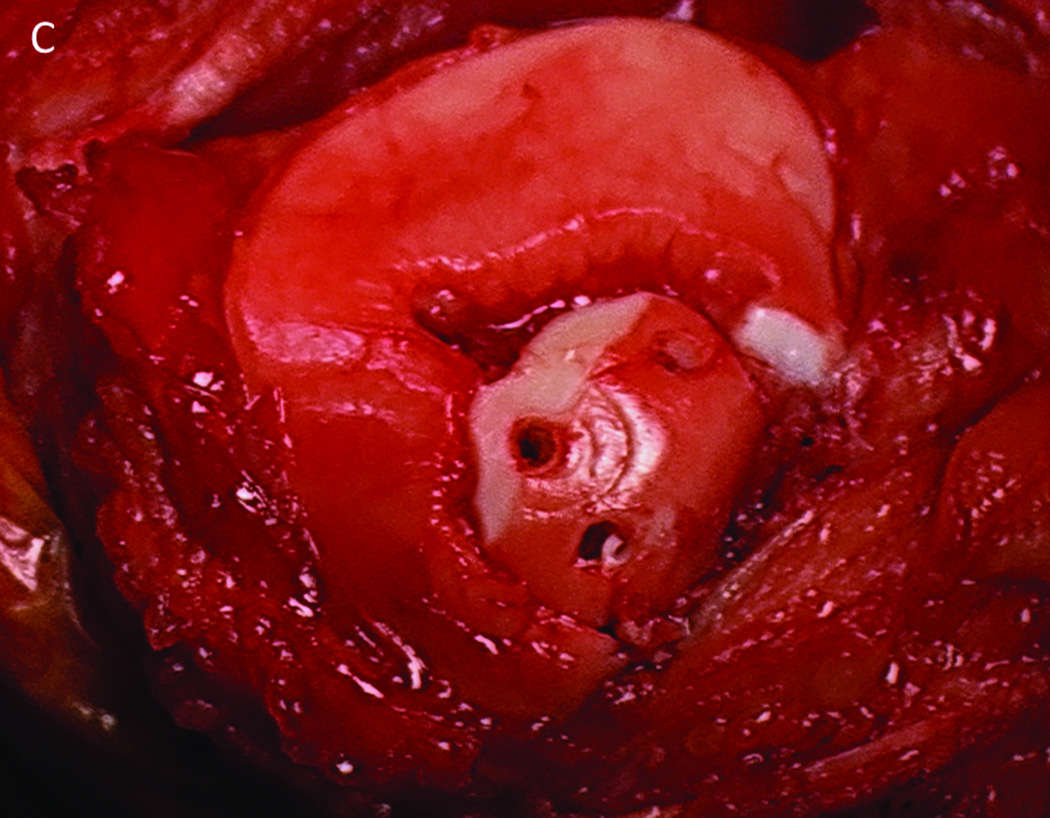
Figure 3.
MRI after an acute high-energy patellar dislocation. The arrow indicates a large osteochondral body from the medial facet of the patella (a). This fragment was excised and one portion (right side) was found to have bone attached while one section (left side) did not (b). This fragment was affixed to the medial side of the patella with biocompression screws (c).
Small to medium sized lesions 1–4 cm2 can be addressed with osteochondral autografts34,35 although Bentley’s results were less encouraging.36 For the treatment of larger lesions (2–10 cm2), autologous chondrocyte implantation is the most commonly reported technique.37–46 These patients, ideally, are younger, present with a focal defect, have a short onset of symptom duration and have had fewer than 2 previous treatments to the lesion.47 Alternatively, large deep lesions with significant subchondral bone erosion may require reconstruction of the osteochondral unit and may be candidates for an osteochondral allograft.48,49
Recommendations
Overall, patella dislocations are common in children and adults. The use of MRI examination in acute patella dislocations with effusions should be standard as the incidence of cartilaginous loose bodies is high and they cannot reliable be diagnosed using plain x-rays.
Patients need to be evaluated carefully for underlying risk factors (patella alta, lateralized patella tendon attachment, rotational deformity in femur and/or tibia and trochlear dysplasia) that may predispose them to recurrent patella dislocations. Chondral lesions after patella dislocation should be restored according to best practice in order to avoid rapid progression of chondral breakdown in the patellofemoral joint.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest and Source Funding
Authors acknowledge no conflicts of interest are present in the preparation of this manuscript.
References
- 1.Crosby EB, Insall J. Recurrent dislocation of the patella. Relation of treatment to osteoarthritis. J. Bone Joint Surg Am. 1976;58:9–13. [PubMed] [Google Scholar]
- 2.Barbari S, Raugstad TS, Lichtenberg N, et al. The Hauser operation for patellar dislocation. 3–32-year results in 63 knees. Acta Orthop Scand. 1990;61:32–35. doi: 10.3109/17453679008993061. [DOI] [PubMed] [Google Scholar]
- 3.Kuroda R, Kambic H, Valdevit A, et al. Articular cartilage contact pressure after tibial tuberosity transfer. A cadaveric study. Am J Sports Med. 2001;29:403–409. doi: 10.1177/03635465010290040301. [DOI] [PubMed] [Google Scholar]
- 4.Elias JJ, Cosgarea AJ. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: A computational analysis. Am J Sports Med. 2006;34:1478–1485. doi: 10.1177/0363546506287486. [DOI] [PubMed] [Google Scholar]
- 5.Bollier M, Fulkerson J, Cosgarea A, et al. Technical failure of medial patellofemoral ligament reconstruction. Arthroscopy. 2011;27:1153–1159. doi: 10.1016/j.arthro.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 6.Kroner M. Ein fall von flachenfraktur und luxation der patella. Deutache Med. Wochenschr. 1905;31:996–997. [Google Scholar]
- 7.Krida A. Osteochondral fractures of the knee joint. Gynec and Obstet. 1924;39:791–795. [Google Scholar]
- 8.Stewart SF. Frontal fractures of the patella. Ann. Surg. 1925;81:536–539. doi: 10.1097/00000658-192502010-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meekison D. A hitherto undescribed fracture of the patella. British J Surg. 1937;25:64–65. [Google Scholar]
- 10.Harmon P. Intra-articular osteochondral fracture as a cause of internal derangement of the knee in adolescents. J Bone and Joint Surg. 1945;27:703–705. [Google Scholar]
- 11.Coleman H. Recurrent osteochondral fracture of the patella. J Bone Joint Surg Br. 1948;30B:153–157. [PubMed] [Google Scholar]
- 12.Ahstrom JP., Jr Ostochondral fracture in the knee joint associated with hypermobility and dislocation of the patella. Report of eighteen cases. J Bone Joint Surg. 1965;47A:1491–1502. [PubMed] [Google Scholar]
- 13.Rorabeck C, Bobechko W. Acute dislocation of the patella with osteochondral fracture: a review of eight cases. J Bone Joint Surg Br. 1976;58:237–240. doi: 10.1302/0301-620X.58B2.932087. [DOI] [PubMed] [Google Scholar]
- 14.Cofield RH, Bryan RS. Acute dislocation of the patella: results of conservative treatment. J Trauma. 1977;17(7):526–531. doi: 10.1097/00005373-197707000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Hawkins R, Bell R, Anisette G. Acute patellar dislocations: The natural history. Am J Sports Med. 1986;14:117–120. doi: 10.1177/036354658601400204. [DOI] [PubMed] [Google Scholar]
- 16.Kirsch MD, Fitzgerald SW, Friedman H, et al. Transient lateral patellar dislocation: diagnosis with MR imaging. AJR Am J Roentgenol. 1993;161(1):109–113. doi: 10.2214/ajr.161.1.8517287. [DOI] [PubMed] [Google Scholar]
- 17.Virolainen H, Visuri T, Kuusela T. Acute dislocation of the patella: MR findings. Radiology. 1993;189:243–246. doi: 10.1148/radiology.189.1.8372201. [DOI] [PubMed] [Google Scholar]
- 18.Nieosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: Incidence and associated osteochondral fractures. J Pediatr Orthop. 1994;14:513–515. doi: 10.1097/01241398-199407000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Stanski CL. Articular hypermobility and chondral injury in patients with acute patellar dislocation. Am J Sports Med. 1996;24:52–60. doi: 10.1177/036354659502300203. [DOI] [PubMed] [Google Scholar]
- 20.Stanitski CL, Paletta GA., Jr Articular cartilage injury with acute patellar dislocation in adolescents: Arthroscopic and radiologic correlation. Am J Sports Med. 1998;26:52–55. doi: 10.1177/03635465980260012501. [DOI] [PubMed] [Google Scholar]
- 21.Sallay PI, Poggi J, Speer KP, et al. Acute dislocation of the patella: A correlative pathoanatomic study. Am J Sports Med. 1996;24:52–60. doi: 10.1177/036354659602400110. [DOI] [PubMed] [Google Scholar]
- 22.Beasley LS, Vidal AF. Traumatic patellar dislocation in children and adolescents: treatment update and literature review. Curr Opin Pediatr. 2004;16:29–36. doi: 10.1097/00008480-200402000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Nomura E, Inoue M, Kurimura M. Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy. 2003 Sep;19:717–721. doi: 10.1016/s0749-8063(03)00401-8. [DOI] [PubMed] [Google Scholar]
- 24.Nomura E, Inoue M. Cartilage lesions of the patella in recurrent patellar dislocation. Am J Sports Med. 2004;32:498–502. doi: 10.1177/0095399703258677. [DOI] [PubMed] [Google Scholar]
- 25.Nomura E, Inoue M. Second-look arthroscopy of cartilage changes of the patellofemoral joint, especially the patella, following acute and recurrent patellar dislocation. Osteoarthritis Cartilage. 2005;13:1029–1036. doi: 10.1016/j.joca.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 26.Mashoof AA, Scholl MD, Lahav A, et al. Osteochondral injury to the mid-lateral weight-bearing portion of the lateral femoral condyle associated with patella dislocation. Arthroscopy. 2005;21:228–232. doi: 10.1016/j.arthro.2004.09.029. [DOI] [PubMed] [Google Scholar]
- 27.Callewier A, Monsaert A, Lamraski G. Lateral femoral condyle osteochondral fracture combined to patellar dislocation: A case report. Orthop Traumatol Surg Res. 2009;95:85–88. doi: 10.1016/j.otsr.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 28.Sanders TG, Paruchuri NB, Zlatkin M. MRI of osteochondral defects of lateral femoral condyle: incidence and pattern of injury after transient lateral dislocation of the patella. Am J Roentgenol. 2006;187:1332–1337. doi: 10.2214/AJR.05.1471. [DOI] [PubMed] [Google Scholar]
- 29.Cash JD, Hughston JC. Treatment of acute patellar dislocation. Am J Sports Med. 1988;16:244–249. doi: 10.1177/036354658801600308. [DOI] [PubMed] [Google Scholar]
- 30.Nikku R, Nietosvaara Y, Aalto K, et al. Operative treatment of primary patellar dislocation does not improve medium-term outcome: a 7-year followup report and risk analysis of 127 randomized patients. Acta Orthop. 2005;76:699–704. doi: 10.1080/17453670510041790. [DOI] [PubMed] [Google Scholar]
- 31.Sillanpää PJ, Mattila VM, Visuri T, et al. Patellofemoral osteoarthritis in patients with operative treatment for patellar dislocation: a magnetic resonance-based analysis. Knee Surg Sports Traumatol Arthrosc. 2011;19:230–235. doi: 10.1007/s00167-010-1285-z. [DOI] [PubMed] [Google Scholar]
- 32.Fu FH, Zurakowski D, Browne JE, et al. Autologous chondrocyte implantation versus debridement for treatment of full-thickness chondral defects of the knee: An observational cohort study with 3-year follow-up. Am J Sports Med. 2005;33:1658–1666. doi: 10.1177/0363546505275148. [DOI] [PubMed] [Google Scholar]
- 33.Kreuz PC, Steinwachs MR, Erggelet C, et al. Results after microfracture of full-thickness chondral defects in different compartments in the knee. Osteoarthritis Cartilage. 2006;14:1119–1125. doi: 10.1016/j.joca.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 34.Bobic V. Arthroscopy osteochondral autogenous graft transplantation in anterior cruciate ligament reconstruction: A preliminary report. Knee Surg Sports Traumatol Arthros. 1996;3:262–264. doi: 10.1007/BF01466630. [DOI] [PubMed] [Google Scholar]
- 35.Hangody L, Kish G, Karpati Z, et al. Osteochondral plugs: Autogenous osteochondral mosaicplasty for the treatment of focal chondral osteochondral articular defects. Oper Tech Orthop. 1997;7:312–322. [Google Scholar]
- 36.Bentley G, Biant LC, Carrington RW, et al. A prospective, randomised comparison of autologous chondrocyte implantation versus mosaicplasty for osteochondral defects in the knee. J Bone Joint Surg Br. 2003 Mar;85(2):223–230. doi: 10.1302/0301-620x.85b2.13543. [DOI] [PubMed] [Google Scholar]
- 37.Cole BJ, Cohen B. Chondral injuries of the knee: A contemporary view of cartilage restoration. Orthopaedic Special Ed. 2000;6:71–79. [Google Scholar]
- 38.Minas T. Autologous chondrocyte implantation for focal chondral defects of the knee. Clin Orthop Relat Res. 2001 Oct;391(Suppl):S349–S361. doi: 10.1097/00003086-200110001-00032. [DOI] [PubMed] [Google Scholar]
- 39.Peterson L, Minas T, Brittberg M, et al. Treatment of osteochondritis dissecans of the knee with autologous chondrocyte transplantation: results at two to ten years. J Bone Joint Surg Am. 2003;85-A(Suppl 2):17–24. doi: 10.2106/00004623-200300002-00003. [DOI] [PubMed] [Google Scholar]
- 40.Knutsen G, Engebretsen L, Ludvigsen TC, et al. Autologous chondrocyte implantation compared with microfracture in the knee. A randomized trial. J Bone Joint Surg Am. 2004;86:455–464. doi: 10.2106/00004623-200403000-00001. [DOI] [PubMed] [Google Scholar]
- 41.Alford JW, Cole BJ, et al. Cartilage restoration, part 2: Techniques, outcomes, and future directions. Am J Sports Med. 2005;33:443–460. doi: 10.1177/0363546505274578. [DOI] [PubMed] [Google Scholar]
- 42.Browne JE, Anderson AF, Arciero R, et al. Clinical outcome of autologous chondrocyte implantation at 5 years in US subjects. Clin Orthop Relat Res. 2005;436:237–245. doi: 10.1097/00003086-200507000-00036. [DOI] [PubMed] [Google Scholar]
- 43.Fu FH, Zurakowski D, Browne JE, et al. Autologous chondrocyte implantation versus debridement for treatment of full-thickness chondral defects of the knee: An observational cohort study with 3-year follow-up. Am J Sports Med. 2005;33:1658–1666. doi: 10.1177/0363546505275148. [DOI] [PubMed] [Google Scholar]
- 44.Minas T, Bryant T. The role of autologous chondrocyte implantation in the patellofemoral joint. Clin Orthop Relat Res. 2005;(436):30–39. doi: 10.1097/01.blo.0000171916.40245.5d. [DOI] [PubMed] [Google Scholar]
- 45.Henderson IJ, Lavigne P. Periosteal autologous chondrocyte implantation for patellar chondral defect in patients with normal and abnormal patellar tracking. Knee. 2006;13(4):274–279. doi: 10.1016/j.knee.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 46.Farr J. Autologous chondrocyte implantation improves patellofemoral cartilage treatment outcomes. Clin Orthop Relat Res. 2007;463:187–194. [PubMed] [Google Scholar]
- 47.Krishnan SP, Skinner JA, Bartlett W, et al. Who is the ideal candidate for autologous chondrocyte implantation? J Bone Joint Surg Br. 2006;88:61–64. doi: 10.1302/0301-620X.88B1.16796. [DOI] [PubMed] [Google Scholar]
- 48.Bugbee WD, Convery RF. Osteochondral allograft transplantation. Clin Sports Med. 1999;18:67–75. doi: 10.1016/s0278-5919(05)70130-7. [DOI] [PubMed] [Google Scholar]
- 49.Torga Spak R, Teitge RA. Fresh osteochondral allografts for patellofemoral arthritis: long-term followup. Clin Orthop Relat Res. 2006;444:193–200. doi: 10.1097/01.blo.0000201152.98830.ed. [DOI] [PubMed] [Google Scholar]