Abstract
Preoperative management of advanced rectal cancer often includes chemoradiotherapy, but little is known about the late complications of radiotherapy. However, these are usually serious, making determination of the characteristics of late complications after radiation therapy critical. Accordingly, we investigated the complications occurring after adjuvant pelvic radiation therapy in patients with advanced rectal cancer. We enrolled 34 consecutive patients with TNM stage III rectal cancer who had undergone curative surgery with adjuvant pelvic radiation therapy. Data on the type of complication/organ involved, the number of complications, the phase of onset, and the treatments used were reviewed. Patients who experienced gut complications or edema were less likely to have their complications resolved than those with complications due to infection. Similarly, patients with multiple complications and late-onset complications were also less likely to have their complications resolved than those with single complications and those with early-onset complications, respectively. Adjuvant radiation therapy in patients with resected advanced rectal cancer was associated with various complications, characterized by late onset and impaired resolution. Therefore, patients indicated for radiation therapy should be selected with great caution.
Key words: Adjuvant radiation therapy, Advanced rectal cancer, Late complication
In the past, postoperative adjuvant pelvic radiation therapy was often performed for patients with advanced rectal cancer1–3; but in recent years, oxaliplatin, fluorouracil, and leucovorin (FOLFOX)4 and capecitabine plus oxaliplatin (XELOX)5 have been more commonly used without radiation. However, chemoradiotherapy is more often used for preoperative management of advanced rectal cancer than chemotherapy alone.6 Early complications of radiation therapy have been studied more extensively than late complications, which may be experienced up to 10 years postoperatively. Late complications are usually serious and difficult to resolve, and thus, determination of the characteristics of late complications after radiation therapy is critical. Accordingly, in this study we aimed to examine the spectrum of complications after adjuvant pelvic radiation therapy in patients with advanced rectal cancer. We evaluated parameters such as the type of complication/organ involved, the number of complications, the phase of onset, and appropriate treatments.
Materials and Methods
We enrolled 34 consecutive patients with TNM stage III rectal cancer who underwent curative surgery with adjuvant pelvic radiation therapy at Aichi Cancer Center Hospital in Nagoya, Japan, between January 1975 and December 2005. All subjects have given their informed consent and this manuscript is a retrospective study. In our hospital, in the event of a retrospective study, this procedure is equivalent to having obtained permission in our ethical committee on human research (Aichi Cancer Center Ethics Committee). Consequently, there is no approval code. Postoperative and intraoperative irradiation was performed in 31 and 3 cases, respectively. During this period, patients with positive dissected lateral lymph nodes received radiation therapy, although a positive lymph node status is currently a contraindication for irradiation. Complications developed after radiation therapy in 18 patients (24 events, 52.9%). All complications were of more than grade 2 severity according to the standard classification and severity grading scale (Common Terminology Criteria for Adverse Events, version 4.03; National Cancer Institute, Maryland, USA).7 During the same study period, 45 patients were contraindicated for treatment with postoperative adjuvant pelvic radiation therapy and received other types of therapy; their data were used for comparison.
Cases with the rectosigmoid colon as the primary cancer site were excluded. None of the patients had received chemotherapy or radiation therapy prior to surgery. Complete dissection of all the regional lymph nodes with mesorectal excision was performed in all cases. In Japan, lateral lymph node dissection is generally indicated if the lower margin of the primary cancer is located below the peritoneal reflection or anal canal, with invasion into the muscularis propria or beyond. The circumferential margin of resection was negative for all cases.
We reviewed the hospital records to obtain clinicopathological information about the patients, including sex and age (median, 56 years), lesion location, surgical procedure, dose of radiation, and adverse complications. Rectal cancer was defined as a tumor whose lowest border was located between the anal verge and the sacral promontory. Lesions were classified as upper or lower rectal cancers depending on their location with respect to the peritoneal reflection. The average total pelvic radiation dose was 4550 cGy (1440–6000 cGy). The radiation field was delineated by the aortic bifurcation at the cephalad end, Alcock's canal caudally, and the inguinal arteries laterally.
The mean follow-up period was 6.5 years (253–7330 days) for the determination of complication characteristics such as complication type/organ involved, number of complications, phase of onset, and treatment choice.
The Fisher exact probability text, univariate logistic regression, and multivariate stepwise logistic regression analysis were performed to identify factors that might influence complications. All data are expressed as the mean ± SD.
The log-rank test was used to evaluate the differences in the local recurrence-specific relapse-free survival rates between groups. Statistical significance was set at P < 0.05.
Results
Patients who received radiation therapy showed better local recurrence-specific relapse-free survival rates than those who did not receive radiation therapy, although this difference was not statistically significant (P = 0.817, Fig. 1).
Fig. 1.
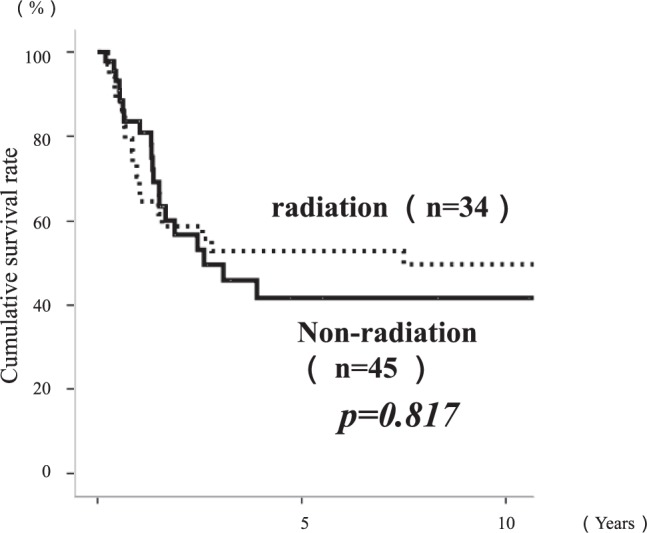
Comparison of patients treated with and without radiation therapy. The local recurrence-specific relapse-free survival rate was better with radiation therapy than without such treatment.
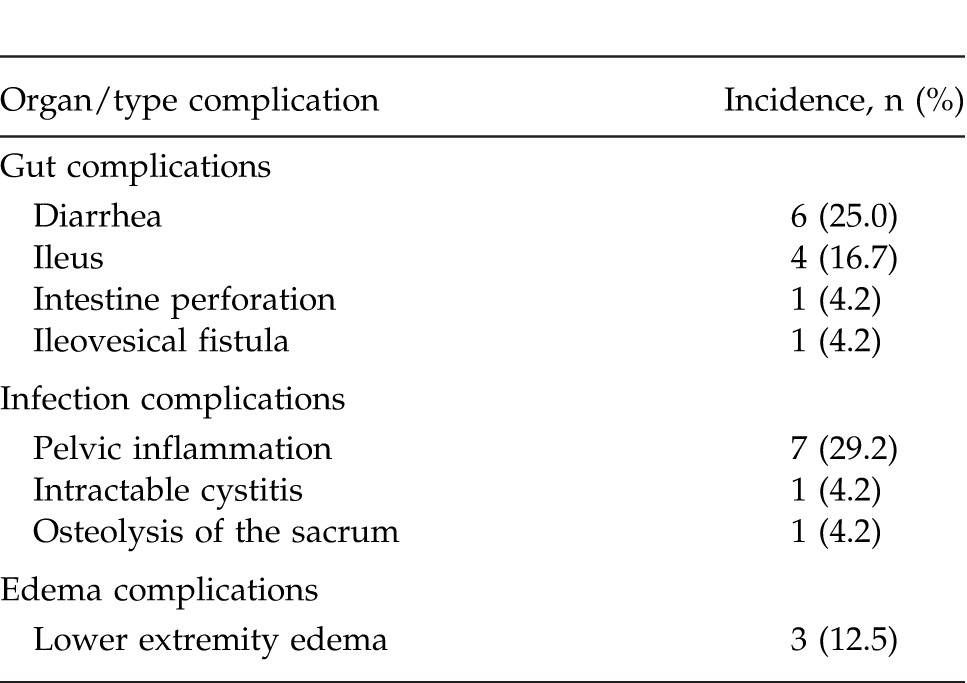
With regard to the complication type/organ involved, complications were classified as gut complications, infection complications, and edema complications. Gut complications were diarrhea (n = 6, 25%), ileus (n = 4, 16.7%), intestine perforation (n = 1, 4.2%), and ileovesical fistula (n = 1, 4.2%). Infection complications were pelvic inflammation (n = 7, 29.2%), intractable cystitis (n = 1, 4.2%), and osteolysis of the sacrum (n = 1, 4.2%). Lower extremity edema accounted for all edema complications (n = 3, 12.5%; Table 1).
Table 1.
Type/organ of complication after adjuvant radiation therapy
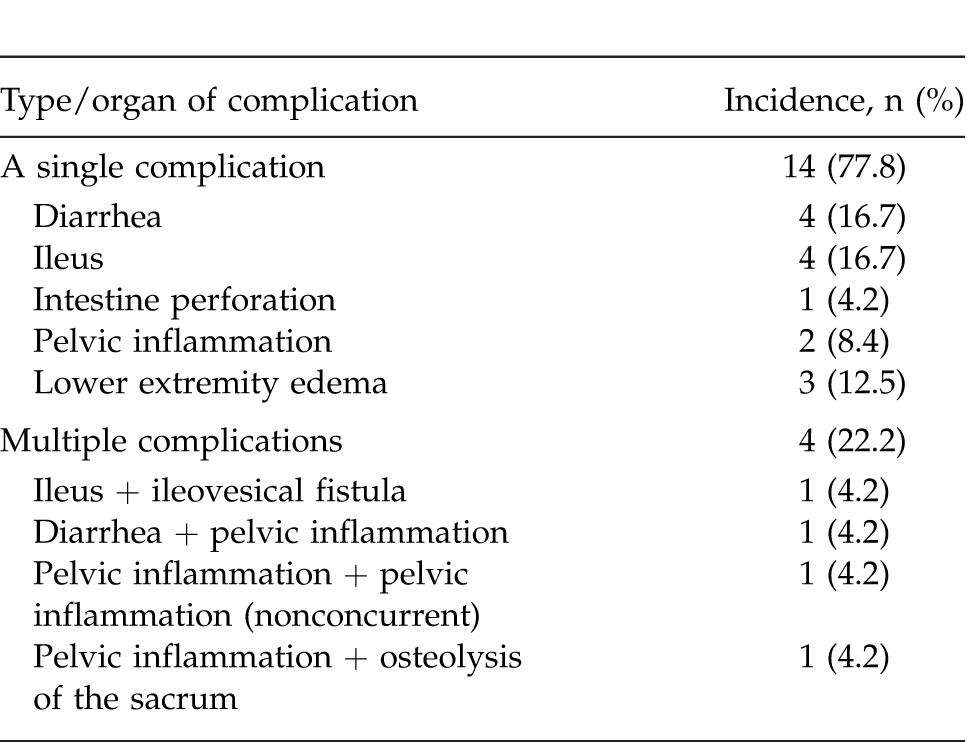
With regard to the number of complications, 14 patients (77.8%) had a single complication and 4 patients (22.2%) had multiple complications. Patients with a single complication had diarrhea (n = 4, 16.7%); ileus (n = 4, 16.7%); lower extremity edema (n = 3, 12.5%); pelvic inflammation (n = 2, 8.4%); or intestine perforation (n = 1, 4.2%). Those with multiple complications had ileus plus ileovesical fistula (n = 1, 4.2%); diarrhea plus pelvic inflammation (n = 1, 4.2%); pelvic inflammation plus pelvic inflammation (nonconcurrent; n = 1, 4.2%); or pelvic inflammation plus osteolysis of the sacrum (n = 1, 4.2%; Table 2).
Table 2.
Number of complications after adjuvant radiation therapy
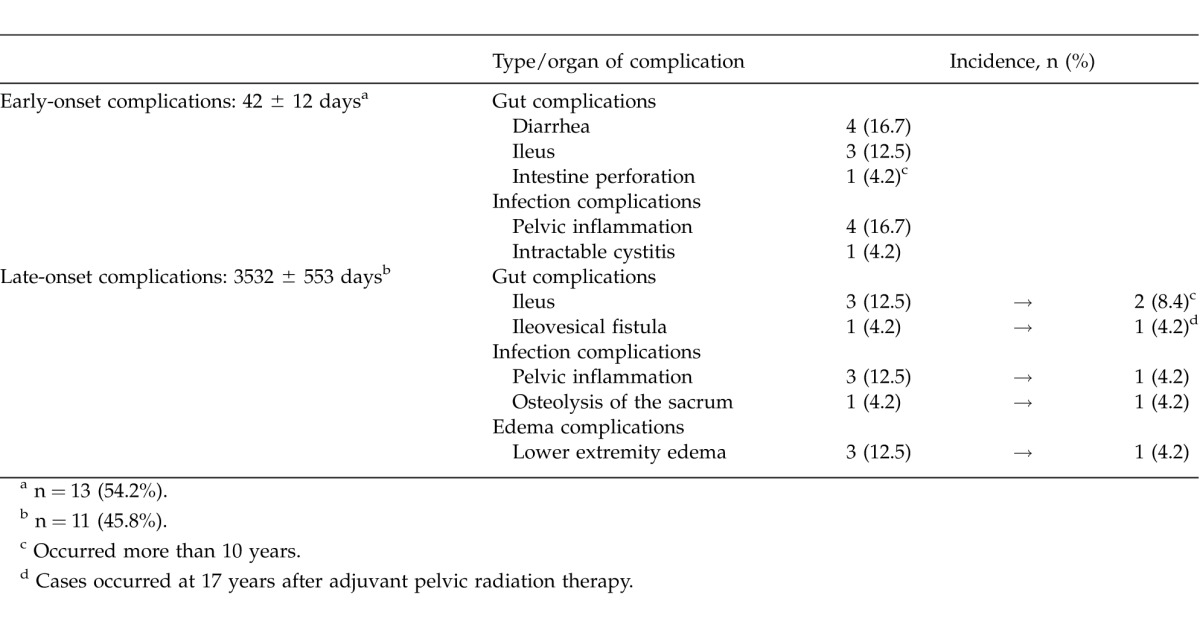
With regard to the phase of complication onset, 13 patients (54.2%) showed early onset and 11 patients (45.8%) showed late onset. Complications developed 42 ± 12 (mean ± SD) days after radiotherapy in patients with early-onset complications and 3532 ± 553 days after radiotherapy in patients with late-onset complications. Patients with early-onset complications had diarrhea (n = 4, 16.7%), ileus (n = 3, 12.5%), intestine perforation (n = 1, 4.2%), pelvic inflammation (n = 4, 16.7%), and intractable cystitis (n = 1, 4.2%). Those with late-onset complications had ileus (n = 3, 12.5%), ileovesical fistula (n = 3, 12.5%), pelvic inflammation (n = 3, 12.5%), osteolysis of the sacrum (n = 1, 4.2%), and lower extremity edema (n = 1, 4.2%). In 6 patients, complications occurred more than 10 years after radiation (ileus in 2 patients [8.4%] and ileovesical fistula, pelvic inflammation, osteolysis of the sacrum, and lower extremity edema in 1 patient each [4.2% each]). The longest interval between radiation therapy and complication development was 17 years (pelvic inflammation; Table 3).
Table 3.
Onset of complication after adjuvant radiation therapy
With regard to treatment for complications, 18 patients were treated conservatively (75.0%) and 6 patients underwent surgery (25.0%). Four patients underwent a single surgery (16.7%) and the remaining 2 required multiple surgeries (8.3%; Table 4).
Table 4.
Treatment complication after adjuvant radiation therapy

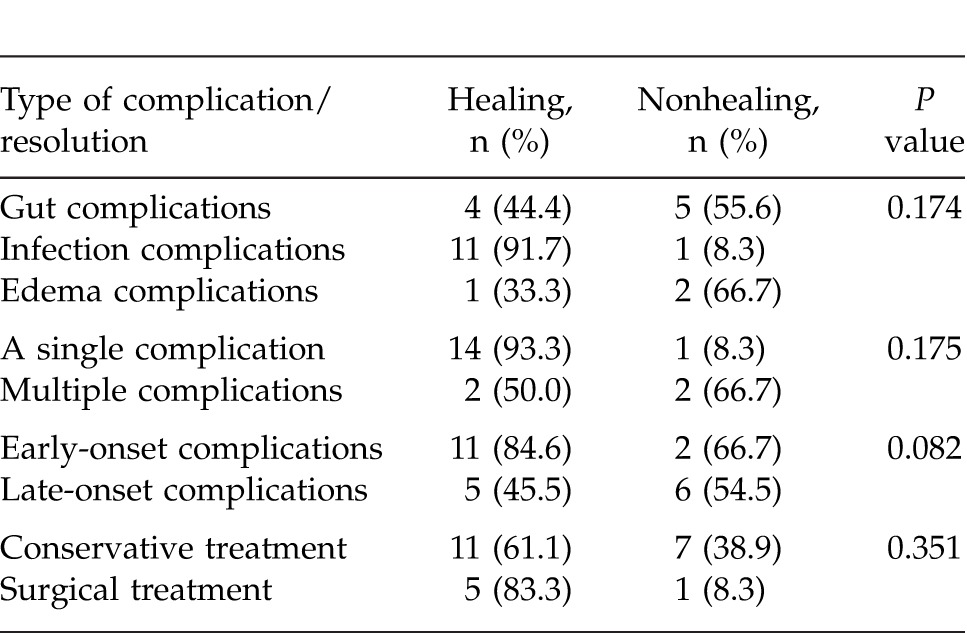
Complications were resolved in 16 patients (66.7%). Resolution of complications was not significantly associated with the type of complication (P = 0.174), number of complications (P = 0.175), phase of onset (P = 0.082), or treatment (P = 0.351). However, the rate of resolution of complications tended to be lower for gut and edema complications than for infection complications. Similarly, patients with multiple complications and late onset of complications tended to show lower rates of complication resolution than those with a single complication and early onset, respectively (Table 5).
Table 5.
Resolved cases
Discussion
Late complications after adjuvant radiotherapy have been previously reported for rectal and esophageal cancer.8–10 Those related to esophageal cancer include acute myocardial infarction, heart failure, pleural effusion, and radiation pneumonitis. For rectal cancer, previous studies only reported phenomenological events of complication and these were not analyzed in detail. To our knowledge, this is the first study to describe the characteristics of complications after adjuvant pelvic radiation therapy for rectal cancer in detail. The phase of complication onset is important because late-onset complications were frequent in this study, with 25% of complications occurring more than 10 years after treatment, indicating the necessity of an adequate follow-up period. In agreement with our findings, Henson et al. showed that late-onset bowel dysfunction can pose a significant problem after pelvic radiotherapy, emphasizing that clinical oncologists be aware of such possibilities.11 In our study, patients with late-onset complications demonstrated poorer complication resolution outcomes. In contrast, Zucali et al. reported that the side effects of radiotherapy were moderate and transient and that no late-onset small bowel complications were observed; however, the follow-up period in that study was <10 years.12
Ippolito et al. reported that after a median follow-up time of 45 months (range, 18–99 months), the 3-year incidence of late rectal complications of grade 2 severity or higher (as per the rectal European Organisation for Research and Treatment of Cancer/Radiation Therapy Oncology Group criteria)13 was 24%. All patients (24/24, 100%) experienced rectal bleeding and 1 patient also developed rectal urgency. Only 3 patients (2.9%) with grade 3 rectal bleeding required argon plasma coagulation. The authors made reference to the early (acute) onset of the complication, suggesting that rectal mucosal alterations were the strongest predictor of late rectal complications, indicative of the need for early proctoscopy.14 In the present study, the intestinal mucosa was not examined if patients did not complain of abdominal pain and colonoscopy was not performed; however, in light of the findings of Ippolito et al., routine colonoscopy may be necessary after radiation therapy.
Fuccio et al. reported on the pathogenic mechanisms of pelvic radiation disease and emphasized that clinicians should focus on using proven treatments correctly and avoiding misus.15 In our study, the local recurrence-specific relapse-free survival rates were approximately 10% better in patients receiving radiation therapy than in those managed without radiation. Compared with our data, adjuvant chemotherapy is associated with a good prognosis.
The use of radiation therapy after surgery is on the decline. However, it is often used as neoadjuvant treatment. The neoadjuvant radiotherapy field includes the delineated area of rectal cancer; therefore, the side effects were not unexpected. Syndikus et al. showed that dose-escalated radiation in patients with prostate cancer was associated with a statistically significant increased risk of various gastrointestinal adverse events.16 Similarly, Birgisson et al. showed that small bowel obstruction was more common in patients with rectal cancer treated with preoperative radiation therapy.17
Adjuvant radiation therapy was associated with various complications, characterized by impaired resolution and late onset. Of note, some complications had an exceedingly late onset, not occurring until 10 years after therapy. We conclude that careful decisions should be made when considering adjuvant radiotherapy for the treatment of these patients, especially in light of more favorable and recently available chemotherapy regimens.
Acknowledgments
References
- 1.Watanabe T. Chemoradiotherapy and adjuvant chemotherapy for rectal cancer. Int J Clin Oncol. 2008;13(6):488–497. doi: 10.1007/s10147-008-0849-0. [DOI] [PubMed] [Google Scholar]
- 2.Ishikura S, Ogino T, Ono M, et al. Preliminary results of pelvic autonomic nerve-preserving surgery combined with intraoperative and postoperative radiation therapy for patients with low rectal cancer. Jpn J Clin Oncol. 1999;29(9):429–433. doi: 10.1093/jjco/29.9.429. [DOI] [PubMed] [Google Scholar]
- 3.Masaki T, Takayama M, Matsuoka H, et al. Intraoperative radiotherapy for oncological and function-preserving surgery in patients with advanced lower rectal cancer. Langenbecks Arch Surg. 2008;393(2):173–180. doi: 10.1007/s00423-007-0260-8. [DOI] [PubMed] [Google Scholar]
- 4.Andre T, Boni C, Navarro M, et al. Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. Journal of clinical oncology. J Clin Oncol. 2009;27(19):3109–3116. doi: 10.1200/JCO.2008.20.6771. [DOI] [PubMed] [Google Scholar]
- 5.Doi T, Boku N, Kato K, et al. Phase I/II study of capecitabine plus oxaliplatin (XELOX) plus bevacizumab as first-line therapy in Japanese patients with metastatic colorectal cancer. Jpn J Clin Oncol. 2010;40(10):913–920. doi: 10.1093/jjco/hyq069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sadahiro S, Suzuki T, Maeda Y, et al. Effects of preoperative immunochemoradiotherapy and chemoradiotherapy on immune responses in patients with rectal adenocarcinoma. Anticancer Res. 2010;30(3):993–999. [PubMed] [Google Scholar]
- 7.Common Terminology Criteria for Adverse Events (CTCAE) Version 4.03. National Cancer Institute website. http://www.cancer.gov/. Accessed June 14, 2010. [Google Scholar]
- 8.Ishikura S, Nihei K, Ohtsu A, et al. Long-term toxicity after definitive chemoradiotherapy for squamous cell carcinoma of the thoracic esophagus. J Clin Oncol. 2003;21(14):2697–2702. doi: 10.1200/JCO.2003.03.055. [DOI] [PubMed] [Google Scholar]
- 9.Kumekawa Y, Kaneko K, Ito H, et al. Late toxicity in complete response cases after definitive chemoradiotherapy for esophageal squamous cell carcinoma. J Gastroenterol. 2006;41(5):425–432. doi: 10.1007/s00535-006-1771-8. [DOI] [PubMed] [Google Scholar]
- 10.Morota M, Gomi K, Kozuka T, et al. Late toxicity after definitive concurrent chemoradiotherapy for thoracic esophageal carcinoma. Int J Radiat Oncol Biol Phys. 2009;75(1):122–128. doi: 10.1016/j.ijrobp.2008.10.075. [DOI] [PubMed] [Google Scholar]
- 11.Henson CC, Andreyev HJ, Symonds RP, Peel D, Swindell R, Davidson SE. Late-onset bowel dysfunction after pelvic radiotherapy: a national survey of current practice and opinions of clinical oncologists. Clin Oncol (R Coll Radiol) 2011;23(8):552–557. doi: 10.1016/j.clon.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 12.Zucali R, Gardani G, Volterrani F. Adjuvant postoperative radiotherapy in locally advanced rectal and rectosigmoidal cancer. Tumori. 1980;66(5):595–600. doi: 10.1177/030089168006600506. [DOI] [PubMed] [Google Scholar]
- 13.Nose T, Peiffert D, Lapeyre M, Hoffstetter S, Koizumi M, Nishiyama K. Late effects of post-high-dose-rate brachytherapy for oropharyngeal carcinoma: are they severer than post-low-dose-rate? Strahlentherapie und Onkologie: Strahlenther Onkol. 2004;180(12):776–782. doi: 10.1007/s00066-004-1270-x. [DOI] [PubMed] [Google Scholar]
- 14.Ippolito E, Massaccesi M, Digesu C, et al. Early proctoscopy is a surrogate endpoint of late rectal toxicity in prostate cancer treated with radiotherapy. Int J Radiat Oncol Biol Phys. 2012;83(2):191–195. doi: 10.1016/j.ijrobp.2011.12.046. [DOI] [PubMed] [Google Scholar]
- 15.Fuccio L, Guido A, Laterza L, et al. Randomised clinical trial: preventive treatment with topical rectal beclomethasone dipropionate reduces post-radiation risk of bleeding in patients irradiated for prostate cancer. Aliment Pharmacol Ther. 2011;34(6):628–637. doi: 10.1111/j.1365-2036.2011.04780.x. [DOI] [PubMed] [Google Scholar]
- 16.Syndikus I, Morgan RC, Sydes MR, Graham JD, Dearnaley DP. MRC RT01 Collaborators. Late gastrointestinal toxicity after dose-escalated conformal radiotherapy for early prostate cancer: results from the UK Medical Research Council RT01 trial (ISRCTN47772397) Int J Radiat Oncol Biol Phys. 2010;77(3):773–783. doi: 10.1016/j.ijrobp.2009.05.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Birgisson H, Pahlman L, Gunnarsson U, Glimelius B. Late gastrointestinal disorders after rectal cancer surgery with and without preoperative radiation therapy. Br J Surg. 2008;95(2):206–213. doi: 10.1002/bjs.5918. [DOI] [PubMed] [Google Scholar]


