Abstract
Malignant tumors with mixed glandular and neuroendocrine characteristics with at least 30% of each component are classified as mixed adenoneuroendocrine carcinoma (MANEC) by the World Health Organization 2010 classification. We report here a case of very well-differentiated adenocarcinoma accompanied by carcinoid tumor, categorized as MANEC. A 41-year-old Japanese man was clinically diagnosed with ascending colon cancer and underwent right hemicolectomy. Using an immunohistologic technique, the pathologic diagnosis was very well-differentiated adenocarcinoma accompanied by carcinoid tumor and marked eosinophil infiltration, which was categorized as MANEC. By immunohistochemical analysis, tumor cells of the carcinoid component exhibited very low proliferation activity. Our case was thought to be MANEC without high malignant potential. MANEC as per the World Health Organization 2010 classification seems to include tumors with diverse grades of malignancy, and it might need to have subclassifications according to the malignancy potential of the tumor cells.
Key words: Colon cancer, Carcinoid, Mixed adenoneuroendocrine carcinoma
Neuroendocrine tumors (NETs) arise from the neuroendocrine cells of the diffuse neuroendocrine system. NETs of the esophagus, stomach, small intestine, pancreas, and colorectum are termed gastroenteropancreatic NETs.1 Originally, Oberndorfer2 reported 7 carcinoid tumor cases of the small intestine in 1907, and he considered them to be benign. However, in recent years it has become clear that the morphology and the biologic behavior of NETs are heterogeneous, and NETs are classified into low-grade and high-grade malignancies in the World Health Organization (WHO) classification.1,3,4 Of these, neuroendocrine carcinoma and mixed adenoneuroendocrine carcinoma (MANEC) are classified as high-grade malignant tumors of NETs in the WHO 2010 classification. In the category of MANEC, little attention is paid to the malignant potential of each tumor, although it is important to define the grade of malignancy of the MANEC for clinical treatment after surgery.
Here, we report a case of very well-differentiated adenocarcinoma with carcinoid tumor and marked eosinophil infiltration, which was categorized into MANEC but seemed to show low-grade malignancy.
Case Report
Severe anemia was found in a 41-year-old Japanese man by his family doctor. The patient visited our hospital without any complaints. Physical examination revealed a hard mass in the lower right abdomen. Laboratory data on admission showed a low hemoglobin level (8.6 g/dL), without abnormality of white blood cell count, differential count of leukocytes, or high serum levels of carcinoembryonic antigen and CA19-9 in blood tests. The patient had no specific individual or family medical history. He underwent lower endoscopic examination, which indicated a protruding tumor of 66 mm in diameter with an irregular surface in the ascending colon. The tumor biopsy specimen showed well-differentiated tubular adenocarcinoma. No abnormality was found in chest and abdominal X-rays. Computed tomography (CT) demonstrated a swollen ascending colon with strong enhancement. Furthermore, CT demonstrated intussusceptions of the oral side of the ascending colon into the anal side.
The patient was clinically diagnosed with ascending colon cancer with intussusceptions into the oral side and underwent right hemicolectomy. At surgery, no tumor invasion into the serosa of the ascending colon was found, and there was little adhesion of the ascending colon, including hard mass, to the surrounding tissue. A few enlarged lymph nodes close to the bowel were detected.
By pathologic examination, type 1 tumor with a dimple in the center was detected on the anal side of the Bauhin valve. Histologically, the tumor consisted of very well-differentiated tubular adenocarcinoma with differentiation to goblet cells and Paneth cells (Fig. 1), and it consisted of cells showing a sheetlike appearance or insular growth in some parts, which invaded the proper muscle layer. These 2 components were tightly mixed but clearly distinctive (Fig. 2). Characteristically, numerous eosinophils were assembled around the tumor (Fig. 3). Immunohistochemically, strong positivity for chromogranin A and CD56 was seen in the sheetlike or insular part of the tumor and a few tumor cells at the base of glandular structure, which indicated neuroendocrine differentiation of the tumor cells. The component of very well-differentiated tubular adenocarcinoma was negative for chromogranin A and CD56. The rates of MIB-1–positive proliferating cells of adenocarcinoma and neuroendocrine cell components were less than 5% and 2% each, respectively, which indicated the low proliferation activity of the tumor (Fig. 4). Both tubular adenocarcinoma and NET cells occupied more than 30% of the tumor. From these histologic and immunohistochemical findings, the pathologic diagnosis was very well-differentiated adenocarcinoma accompanied by carcinoid, which was categorized into MANEC by the 2010 WHO classification.
Fig. 1.
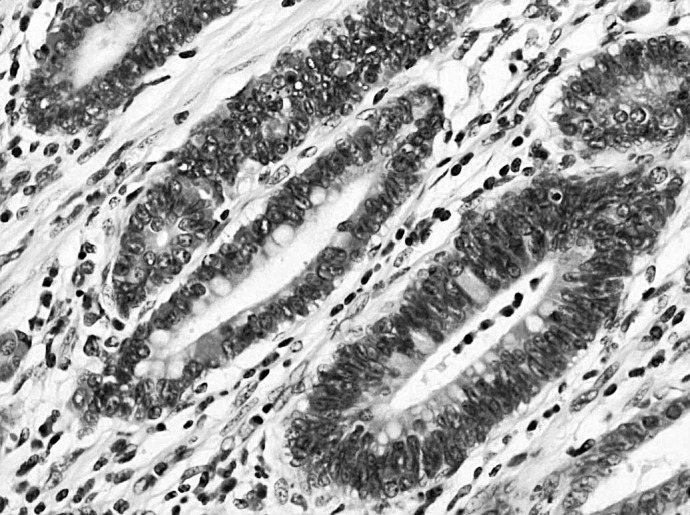
Very well-differentiated tubular adenocarcinoma with differentiation to goblet cells and Paneth cells in some parts.
Fig. 2.
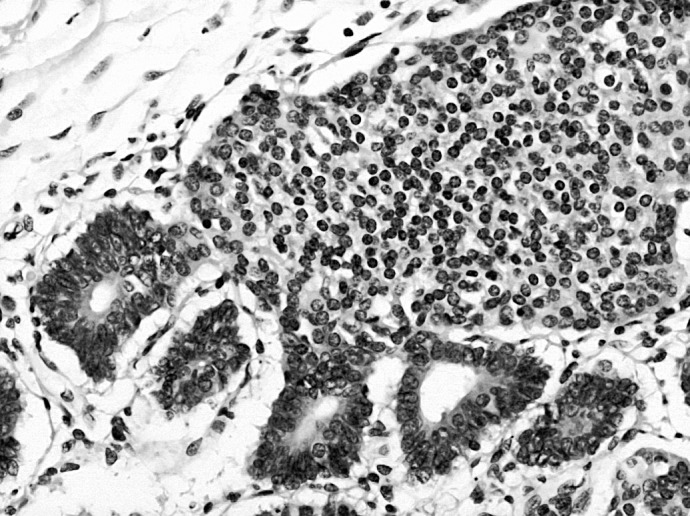
The proliferation of well-differentiated adenocarcinoma in a distinct region from the neuroendocrine component showing sheetlike appearance or insular growth.
Fig. 3.
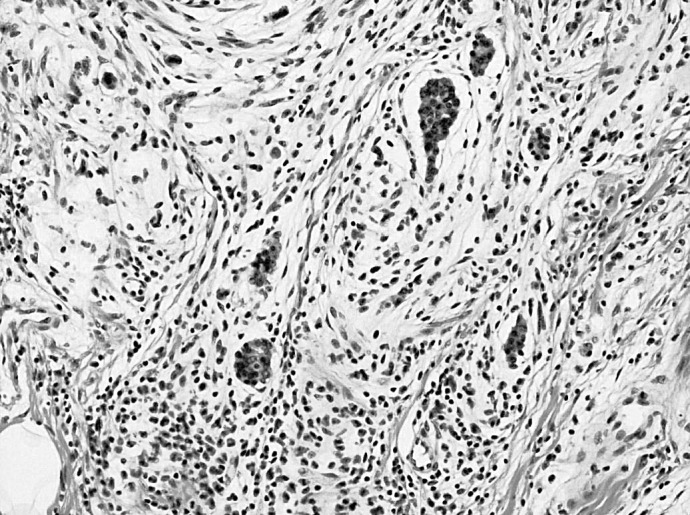
A number of eosinophils assembled around the tumor.
Fig. 4.
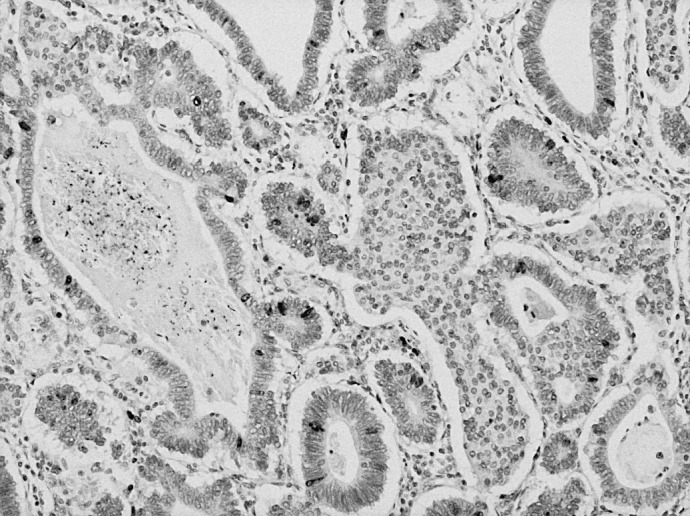
Immunostaining of proliferating cells of adenocarcinoma and neuroendocrine cell components for Ki-67 showed MIB-1 labeling indexes of less than 5% and 2%, respectively.
The postoperative course of the patient was uneventful, and he was discharged 8 days after surgery. The patient was followed up without adjuvant chemotherapy, since the tumor showed low proliferating activity and was thought to have low-grade malignant potential. The patient is still alive without metastatic findings 18 months after surgery.
Discussion
In the new 2010 WHO classification, NETs are classified into hyperplastic and preneoplastic lesions, NET G1, G2, neuroendocrine carcinoma G3, and MANEC.5 The histologic grading system from G1 to G3 represents the malignant nature of these tumors.3,4 The grading system of NETs is based on mitotic rate and Ki-67 labeling index, as proposed by the European Neuroendocrine Tumour Society.3,4 To date, the treatment of patients diagnosed with NETs is decided according to the histopathologic grading of the tumor.
On the other hand, MANECs do not have a subcategory according to their malignant grades because of the recognition that all MANECs have potentially high-grade malignancy.5 The tumor in our case consisted of very well-differentiated tubular adenocarcinoma, which showed differentiation to Paneth cells and goblet cells, accompanied by an invasive conventional carcinoid component; it was categorized as MANEC according to the 2010 WHO classification. However, in terms of low proliferation activity and very good differentiation of tumor cells, our case is quite different from tumors consisting of aggressive adenocarcinoma and aggressive neuroendocrine cell components, as reported by Bates and Belter.6 As to the treatment of NETs, Eggenberger7 reported that the resection of all visible primary disease was a reasonable treatment that offers the best prognosis for all midgut and hindgut NETs. However, there has been insufficient evidence of effective adjuvant chemotherapy after curative surgery for localized colon NETs.8,9 Besides complete resection of the tumor, MIB-1 labeling index was under 5% in both adenocarcinoma and NET components in our MANEC case, which indicated a low proliferation activity of the tumor cells. Thus, the patient in this case has not received any adjuvant chemotherapy and has been without recurrence 18 months after the operation.
Before the 2010 WHO classification, there were few reports of low-grade mixed glandular and neuroendocrine tumor. Three cases of colon tumor consisting of both adenoma and carcinoid components have been reported.10–12 Hock et al13 reported on mixed moderately differentiated adenocarcinoma and typical carcinoid tumor with distinct regions, which was similar to our case. On the other hand, in the cases reported by Klappenbach et al,14 Lew et al,15 and Jiao et al,16 the tumors consisted of poorly differentiated adenocarcinoma with an abundant endocrine cell component, and they were thought to involve high-grade malignancy. Although all of these tumors consisted of both glandular and endocrine cell components, the malignant grade of each tumor seemed to be quite different.
In general, once the metastasis of NETs occurs, we currently have no standardized chemotherapy protocols that improve the patient's prognosis.7 Therefore, the precise assessment of whether the primary tumor is low risk or high risk is needed clinically for appropriate adjuvant chemotherapy. However, as described previously, the 2010 WHO classification does not have subcategories of MANEC.
Recently, Rosa et al17 proposed the subcategorization of MANEC, in which mixed glandular and neuroendocrine tumor was subdivided into high-grade malignant MANEC; which consisted of adenoma/adenocarcinoma and neuroendocrine carcinoma, intermediate-grade malignant MANEC, which consisted of adenocarcinoma and G1/G2 NET or amphicrine carcinoma; and mixed adenoendocrine tumor, which consisted of adenoma NET. According to this classification, our case would be classified into intermediate-grade malignant MANEC. The clinical treatment of this category would be decided by the malignant grade of the adenocarcinoma component.
Recently, it has been indicated that progression of colorectal cancer seems to be suppressed by the adaptive immune system of the host.18,19 The correlation between the abundance of tumor-infiltrating T cells and improved clinical outcome has been reported.20 Besides the beneficial role of lymphocytes surrounding the tumor, tumor-associated eosinophilic infiltration has also been reported to associate with a better prognosis in colorectal cancer,21–23 although the correlation between tumor-associated eosinophilia and patient prognosis in other cancers seems to be unclear.24,25 In our case, marked eosinophil infiltration was observed around the tumor, which might indicate a better prognosis for the patient.
In conclusion, we reported a case of mixed very well-differentiated adenocarcinoma and carcinoid tumor with marked eosinophil infiltration, which was categorized as MANEC by the 2010 WHO classification. However, MANEC does not have subcategories according to the malignant grade of each tumor. Our case and those in previous reports indicate the need for subclassification of MANEC for appropriate clinical treatment after surgery. In this sense, our case might be classified into intermediate-grade malignant MANEC.
References
- 1.Kloppel G, Perren A, Heitz PU. The gastroenteropancreatic neuroendocrine cell system and its tumors: the WHO classification. Ann N Y Acad Sci. 2004;1014:13–27. doi: 10.1196/annals.1294.002. [DOI] [PubMed] [Google Scholar]
- 2.Oberndorfer S. Karzinoide Tumoren des dündarms. Frankf Z Pathol. 1907;1:426–432. [Google Scholar]
- 3.Rindi G, Kloppel G, Alhman H, Caplin M, Couvelard A, de Herder WW. TNM staging of foregut (neuro)endocrine tumors: a consensus proposal including a grading system. Virchows Arch. 2006;449(4):395–401. doi: 10.1007/s00428-006-0250-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rindi G, Kloppel G, Couvelard A, Komminoth P, Korner M, Lopes JM. TNM staging of midgut and hindgut (neuro) endocrine tumors: a consensus proposal including a grading system. Virchows Arch. 2007;451(4):757–762. doi: 10.1007/s00428-007-0452-1. [DOI] [PubMed] [Google Scholar]
- 5.Bosman FT, Carneiro F, Hruban RH, Theise N. WHO Classification of Tumors of the Digestive System. 2010 4th. International Agency for Research on Cancer (IARC) [Google Scholar]
- 6.Bates HR, Jr, Belter LF. Composite carcinoid tumor (argentaffinoma-adenocarcinoma) of the colon: report of 2 cases. Dis Colon Rectum. 1967;10(6):467–470. doi: 10.1007/BF02616821. [DOI] [PubMed] [Google Scholar]
- 7.Eggenberger JC. Carcinoid and other neuroendocrine tumors of the colon and rectum. Clin Colon Rectal Surg. 2011;24(3):129–134. doi: 10.1055/s-0031-1285996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boudreaux JP, Klimstra DS, Hassan MM, Woltering EA, Jensen RT, Goldsmith SJ. The NANETS consensus guideline for the diagnosis and management of neuroendocrine tumors: well-differentiated neuroendocrine tumors of the jejunum, ileum, appendix, and cecum. Pancreas. 2010;39(6):753–766. doi: 10.1097/MPA.0b013e3181ebb2a5. [DOI] [PubMed] [Google Scholar]
- 9.Anthony LB, Strosberg JR, Klimstra DS, Maples WJ, O'Dorisio TM, Warner RR. The NANETS consensus guidelines for the diagnosis and management of gastrointestinal neuroendocrine tumors (nets): well-differentiated nets of the distal colon and rectum. Pancreas. 2010;39(6):767–774. doi: 10.1097/MPA.0b013e3181ec1261. [DOI] [PubMed] [Google Scholar]
- 10.Varghese NM, Zaitoun AM, Thomas SM, Senapati A, Theodossi A. Composite glandular-carcinoid tumour of the terminal ileum. J Clin Pathol. 1994;47(5):427–429. doi: 10.1136/jcp.47.5.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lyda MH, Fenoglio-Preiser CM. Adenoma-carcinoid tumors of the colon. Arch Pathol Lab Med. 1998;122(3):262–265. [PubMed] [Google Scholar]
- 12.Moyana TN, Qizilbash AH, Murphy F. Composite glandular-carcinoid tumors of the colon and rectum: report of two cases. Am J Surg Pathol. 1988;12(8):607–611. doi: 10.1097/00000478-198808000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Hock YL, Scott KW, Grace RH. Mixed adenocarcinoma/carcinoid tumour of large bowel in a patient with Crohn's disease. J Clin Pathol. 1993;46(2):183–185. doi: 10.1136/jcp.46.2.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klappenbach RS, Kurman RJ, Sinclair CF, James LP. Composite carcinoma-carcinoid tumors of the gastrointestinal tract: a morphologic, histochemical, and immunocytochemical study. Am J Clin Pathol. 1985;84(2):137–143. doi: 10.1093/ajcp/84.2.137. [DOI] [PubMed] [Google Scholar]
- 15.Lew EA, Lewin KJ, Zarchy T, Pisegna JR. Adenocarcinoma of the colon with neuroendocrine features and secretory diarrhea. Am J Gastroenterol. 1999;94(6):1692–1694. doi: 10.1111/j.1572-0241.1999.01167.x. [DOI] [PubMed] [Google Scholar]
- 16.Jiao YF, Nakamura S, Arai T, Sugai T, Uesugi N, Habano W. Adenoma, adenocarcinoma and mixed carcinoid-adenocarcinoma arising in a small lesion of the colon. Pathol Int. 2003;53(7):457–462. doi: 10.1046/j.1440-1827.2003.01500.x. [DOI] [PubMed] [Google Scholar]
- 17.La Rosa S. MANECs of the gastrointestinal tract: an update. Cancers. 2012;4(1):11–30. doi: 10.3390/cancers4010011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salama P, Phillips M, Grieu F, Morris M, Zeps N, Joseph D. Tumor-infiltrating FOXP3+ T regulatory cells show strong prognostic significance in colorectal cancer. J Clin Oncol. 2009;27(2):186–192. doi: 10.1200/JCO.2008.18.7229. [DOI] [PubMed] [Google Scholar]
- 19.Schwitalle Y, Kloor M, Eiermann S, Linnebacher M, Kienle P, Knaebel HP. Immune response against frameshift-induced neopeptides in HNPCC patients and healthy HNPCC mutation carriers. Gastroenterology. 2008;134(4):988–997. doi: 10.1053/j.gastro.2008.01.015. [DOI] [PubMed] [Google Scholar]
- 20.Nosho K, Baba Y, Tanaka N, Shima K, Hayashi M, Meyerhardt JA. Tumour-infiltrating T-cell subsets, molecular changes in colorectal cancer, and prognosis: cohort study and literature review. J Pathol. 2010;222(4):350–366. doi: 10.1002/path.2774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pretlow TP, Keith EF, Cryar AK, Bartolucci AA, Pitts AM, Pretlow TG., 2nd Eosinophil infiltration of human colonic carcinomas as a prognostic indicator. Cancer Res. 1983;43(6):2997–3000. [PubMed] [Google Scholar]
- 22.Fisher ER, Paik SM, Rockette H, Jones J, Caplan R, Fisher B. Prognostic significance of eosinophils and mast cells in rectal cancer: findings from the National Surgical Adjuvant Breast and Bowel Project (protocol R-01) Hum Pathol. 1989;20(2):159–163. doi: 10.1016/0046-8177(89)90180-9. [DOI] [PubMed] [Google Scholar]
- 23.Fernandez-Acenero MJ, Galindo-Gallego M, Sanz J, Aljama A. Prognostic influence of tumor-associated eosinophilic infiltrate in colorectal carcinoma. Cancer. 2000;88(7):1544–1548. [PubMed] [Google Scholar]
- 24.Samoszuk M. Eosinophils and human cancer. Histol Histopathol. 1997;12(3):807–812. [PubMed] [Google Scholar]
- 25.Lowe D, Jorizzo J, Hutt MS. Tumour-associated eosinophilia: a review. J Clin Pathol. 1981;34(12):1343–1348. doi: 10.1136/jcp.34.12.1343. [DOI] [PMC free article] [PubMed] [Google Scholar]


