Abstract
Concomitant ingestion of alcohol and cephalosporin may cause a disulfiram-like reaction; however its fatal outcomes are not commonly known. We retrospectively reviewed 78 patients who had cephalosporin induced disulfiram-like reaction (CIDLR). The patients who had a negative skin test to cephalosporin prior to intravenous antibiotics were included, and those who were allergic to either alcohol or antibiotics were excluded. The average age of 78 patients was 37.8±12.2 (21–60) years. Of the 78 patients, 93.58% of the patients were males, 70.51% of the patients consumed alcohol after use of antibiotics, and 29.49% patients consumed alcohol initially, followed by intravenous antibiotics; however, no significant difference of morbidity was observed in these two groups. All patients were administered antibiotics intravenously. Five of 78 patients (6.41%) developed severe CIDLR too urgently to be rescued successfully. In conclusion, it is important for clinicians to educate patients that no alcohol should be used if one is taking cephalosporin. Also, clinicians should keep in mind that cephalosporin should not be prescribed for any alcoholics.
Key words: Alcohol, Cephalosporin, Disulfiram-like reaction
Consuming alcohol is so common a daily social activity that some people become addicted to it, which can lead to chronic alcoholism. For management of chronic alcoholism, disulfiram has been widely used since its approval by the US Food and Drug Administration in 1951.1 After consumption of alcohol, it is converted into acetaldehyde by alcohol dehydrogenate and subsequently metabolized into acetate by aldehyde dehydrogenase in the body.1,2 Disulfiram can irreversibly inhibit aldehyde dehydrogenase and prevent metabolism of acetaldehyde. The accumulated high serum level of acetaldehyde causes an unpleasant histamine-like reaction called disulfiram-like reactions.2 The manifestation of CIDLR (cephalosporin-induced disulfiram-like reaction) varies from mild reaction like facial flushing, nausea or vomiting, to a severe reaction including angioedema, hypotension, shock, or death.
In addition to disulfiram, some antibiotics can cause similar reaction as disulfiram-like reactions. A variety of antibiotics containing the fused β-lactam/dihydrothiazine ring system have been known as cephalosporin, and it was reported initially to adversely affect the metabolism of alcohol in 1980.3–6 Since then several medications with similar reaction have been reported. These medications include cefamandole, cefoperazone, moxalactam, longer-acting hypoglycemics (e.g., chlorpropamide, tolbutamide), and nitrates. As the widespread abuse of alcohol and or cephalosporin, CIDLR is not rare, it is still not well understood. A delayed diagnosis and management is not rare and can cause severe conditions or even death. We retrospectively studied CIDLR cases from January 2006 to December 2011 to characterize early diagnosis, management and prevention of CIDLR.
Methods and Patients
From January 2006 to December 2011, a total of 78 patients were diagnosed with cephalosporin-induced disulfiram-like reaction (CIDLR) and treated in the emergency department in our hospitals. Patients provided written consent for their information to be stored in the hospital database and used for research. This study has been approved by our hospital ethics committee.
Patients were diagnosed as CIDLR if they met the following criteria: consumption of alcohol and use of antibiotic cephalosporin intravenously, negative skin tests for cephalosporin prior to use of cephalosporin, no history of heart disease, and mild or severe symptoms from mild facial flushing to shock or even death. Electrocardiogram (ECG) showed no myocardial infarction. Patients were relieved after symptomatic treatment within 1–3 hours. Exclusion conditions in this study were patients who consume no alcohol or take oral antibiotics only, did not take a skin test or had a positive skin test to antibiotics and those did not meet the inclusion criteria mentioned above.
Once CIDLR was diagnosed, all patients were provided oxygen at 1–2 L/min, monitored with electrocardiogram, meanwhile symptomatic treatment and volume replacement were provided intravenously, including vitamin C, vitamin B6, 15% KCl in a bolus of 1 L of normal saline.
Results
The average age of 78 patients was 37.8±12.2 (21–60) years. Of 78 patients, 73 (93.58%) were males, 72 patients (92.31%) reported that their capability of consuming alcohol was halved at least after they had cephalosporin intravenously. All patients had no history of heart disease, and had a negative skin test to cephalosporin before receiving antibiotics, and there were no allergies to either alcohol or cephalosporin.
Patients received intravenous cephalosporin for infections such as respiratory tract infection, tonsillitis, pneumonia, urinary tract infection, etc (Table 1). The most common reason to use antibiotics is respiratory tract infection (47.44%), followed by cholecystitis (10.26%), pneumonia (8.97%), urinary tract infection (8.97%), acute appendicitis (7.69%), foot injury and infection (5.13%), tonsillitis (5.13%), skin abscess (3.85%), and toothache (2.56%). Table 2 shows that 70.51% of the patients consumed alcohol after use of antibiotics, 29.49% patients consumed alcohol initially and followed by antibiotics, however, no significant difference of the incidence of CIDLR was observed between these two groups (P < 0.05). All patients received the antibiotic intravenously, and developed CIDLR within 60 minutes after use of alcohol or antibiotics (Table 3). In terms of types and volume of alcohol the patients consumed, 53 of 78 (67.95%) patients consumed white wine ranging from 50 to 500 ml, the number of patients who consumed white wine in the range of 50 to 99 ml, 100 to 249 ml, above 250 ml was 48 (90.57%), 4 (5.13%) and 1 (1.28%), respectively. And 25 of 75 (32.05%) patients consumed the beer. Of 78 patients, 72 (92.31%) patients complained that the tolerable volume of alcohol used to consume was halved after intravenous antibiotics. In terms of awareness of risk of CIDLR, 19 (24.36%) patients reported knowing the risk of CIDLR, yet 69 (88.46%) patents did not know it at all.
Table 1.
Baseline patient characteristics

Table 2.
Types and sequence of consuming alcohol or antibiotics
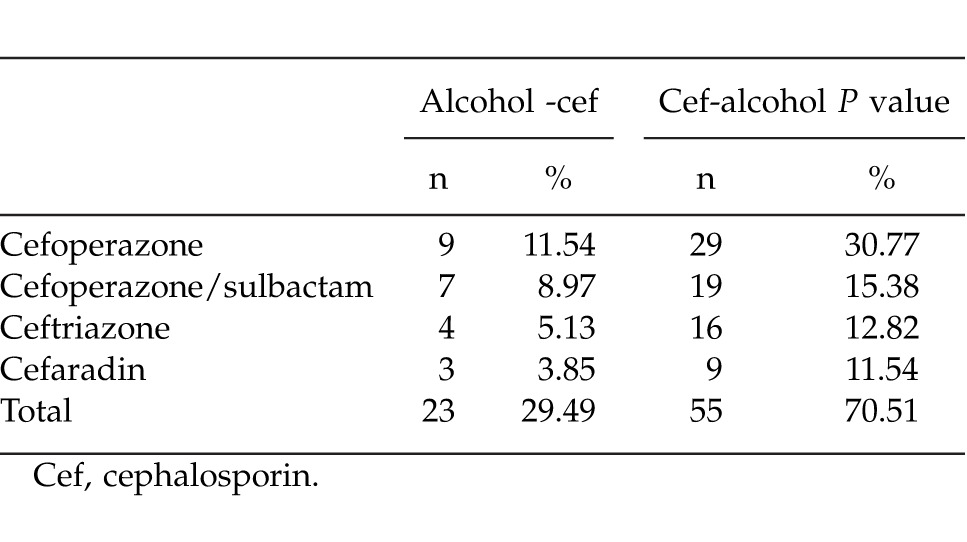
Table 3.
Timing periods CIDLR occurred
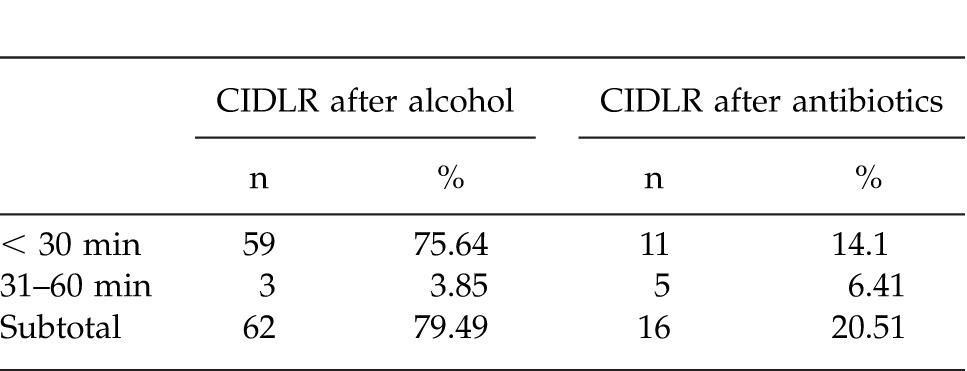
Table 4 illustrates the symptoms of patients with CIDLR. The clinical conditions were controlled symptomatically in 73 patients within 1–3 hours; the symptoms disappeared within 24 hours. Serum electrolytes and cell counts were in normal range. However, 5 patients (6.41%) died after symptomatic treatment. The first patient received intravenous cephalosporin for tonsillitis, and was warned to avoid to consume alcohol; however, he participated in his friend's wedding ceremony, and consumed 2 bottles of beer (1000 ml), 30 minutes later, he had facial flushing and short of breathing, walked unsteadily and could not speak fluently. He was sent to the emergency department, was found in shock status with systolic blood pressure at 40 mm Hg and died soon despite urgent rescue. The second patient was a 21-year-old young man, who consumed about 200 ml of alcohol, then went to a clinic for common cold and fever. Upon request by his doctor, he hid the fact that he was drinking alcohol. Subsequently, he was administered 1g cephalosporin intravenously. During infusion of antibiotics he felt chest pain and shortness of breath and was transferred to another hospital for urgent rescue. Unfortunately he died just after arrival to the emergency room. The third patient was a 24-year-old healthy man. He consumed approximately 500 ml of beer and 100 ml of white wine. Following intravenous cephalosporin he had palpitations and difficulty breathing and died upon arrival to the emergency department of the hospital. The fourth patient was a 46-year-old man who consumed 300 ml alcohol during the party and then went to a private clinic for bronchitis and was administered cephalosporin intravenously. During the course of treatment, he had difficulty breathing and was transferred to hospital for further treatment. Upon arrival to the emergency department, he was in shock status and died, despite resuscitation. The last patient was a 24-year-old male who had respiratory infection and was treated with cephalosporin intravenously 36 hours earlier. He consumed approximately 150 ml of white wine during his wedding ceremony, then he suddenly became faint and fell down. He was sent to the hospital without delay and died of shock after symptomatic treatment. His premarriage physical examination revealed healthy conditions with no heart or lung diseases. These 5 patients had been healthy. ECG examinations revealed no myocardial infarction or arrhythmia, and myocardial enzyme was normal.
Table 4.
Clinical manifestation of CIDLR

Discussion
Our retrospective study showed that five patients developed severe CIDLR too urgently to have time to be rescued successfully. The mortality was 6.4% (5/78) in this group. Most patients (70.51%) consuming alcohol after antibiotics developed CIDLR, while 29.49% using antibiotics after alcohol consumption had CIDLR. Yet no difference of morbidity was observed (P > 0.05) in these two groups. To our knowledge, this is the first report in English to detail mortality of patients who developed CIDLR. It is important for clinicians to counsel patients about safe use of alcohol and medications and for clinicians to refrain from administering cephalosporin to any suspected alcoholics.
Certain β-lactam cephalosporins such as cefamandole, cefoperazone, and moxalactam induce disulfiram-like reaction when alcohol is used.3,4 Cephem compounds carrying an N-methyltetrazolethiol substituent in the 3-position of the dihydrothiazine ring of the parent antibiotic, such as moxalactam, cefamandole, cefmetazole, cefonicid, cefmenoxime, cefoperazone, cefotiam, it is suggested that a direct interaction between N-methyltetrazolethiol and related heterocyclic thiols can induce CIDLR.5–7 Studies on Wistar rats demonstrated that concomitant administration of ethanol and cephalexin causes functional changes (inhibition of diuresis) and degenerative changes in capillary loops of some renal corpuscles apart from hyperemia,8 trophic changes in pancreas,9 atrophic changes in gastric glands, and strong reduction of mucous cells activity.10
Patients who are on antibiotics may have repeated mild or tolerable reaction of CIDLR as long as they consumed alcohol,7,11 they are not aware of the CIDLR and complain of the toxicities of alcohol. Most patients with mild reaction such as flush of face, nausea and vomiting may not seek medical care and can be self limited or can be managed by drinking plenty of water and resting, with no serious consequence. Severe cases may experience chest pain, nausea, vomiting with garlic smelling, arrhythmia, and death if the patients were misdiagnosed or delayed in seeking medical care. Most patients in our group developed CIDLR within 30 minutes after drinking alcohol; they had CIDLR so severe as to alarm them to seek medical care immediately. Presumably, many people who take cephalosporin orally then use alcohol have mild CIDLR and do not seek medical care. Therefore, only patients who were administered antibiotics intravenously were included in this retrospective study.
CIDLR is characterized by severe objective reaction (i.e., intoxication) after consuming a less than average amount of alcohol with less subjective signs on physical examination. Severe outcomes of CIDLR have been reported as refractive hypotension, loss of consciousness or even death,12–14 but reports of mortality due to CIDLR have not been found in English literature. Several cases of death due to CIDLR have been reported in Chinese literature.12–14 Three patients were reported to have died from CIDLR caused by cephalosporin in Chinese literature; two patients consumed alcohol after intravenous administration of cephalosporin,15,16 one patient died after consumption of alcohol followed by cefotaxime.15–17 The patients with CIDLR can be easily misdiagnosed as having myocardial infarction, alcohol or cephalosporin allergy. Therefore, CIDLR should be part of the differential diagnosis list. CIDLR should be differentiated with other conditions, such as cardiac diseases, alcohol allergy, and cephalosporin allergy.
The indication to use cephalosporin should be strictly followed. Before prescribing or using antibiotics, history of allergy to any drug or alcohol should be requested, and in suspected alcoholic patients, the speed of intravenous infusion should be slowed initially. In case any abnormal reaction occurs during infusion of cephalosporin, the intravenous infusion should be terminated immediately and the cause should be investigated seriously. Similarly, it is critical for patients to be aware of the potential risks of combined use of alcohol and some antibiotics to prevent the risk of CIDLR. Alcohol can stay in the body for approximately 12 hours, whereas it takes several days to metabolize the antibiotics completely in the body.18 Therefore, it is mandatory to strongly caution patients not to consume alcoholic beverages within a week after use of cephalosporin, or vice versa.
The CIDLR is caused by the interaction of metabolite of alcohol with the disulfiram-like agents such as cephalosporin; the severity of CIDLR is related to the concentration of alcohol and medication in the body. The incidence of CIDLR is associated with dosage of cephalosporin used, the speed and volume of alcohol being consumed, and the interval between the alcohol and cephalosporin used, which will impact the serum level of metabolite of alcohol and cephalosporin. No matter the route of administration of the cephalosporin, either intravenously or orally, as long as there is certain level of medications and alcohol in the body, the CIDLR could occur. However, the intravenous dosage is usually larger than the oral dosages, and thus the CIDLR is generally more severe in patients who were administered intravenously.
The limitation of this study is retrospective study and the volume of alcohol was recalled by patients or their relatives, and was not precise. However, for the precise diagnosis of our patients, we included patients who received cephalosporin intravenously only in our retrospective study. And our study illustrates the intensity of interaction of alcohol and cephalosporin. It is critical for both physician and patients to be aware of the fatal outcomes of combined use of alcohol and cephalosporin. The physician also should bear in mind the CIDLR in their differential diagnoses list.
Acknowledgments
Dr. Ren is the guarantor for this article. No conflicts exist among all authors.
References
- 1.Suh JJ, Pettinati HM, Kampman KM, O'Brien CP. The status of disulfiram: a half of a century later. J Clin Psychopharmacol. 2006;26(3):290–302. doi: 10.1097/01.jcp.0000222512.25649.08. [DOI] [PubMed] [Google Scholar]
- 2.Kamei C, Sugimoto Y, Tasaka K. The effects of cephem antibiotics and related compounds on the aldehyde dehydrogenase in rat liver mitochondria. Biochem Pharmacol. 1987;36(12):1933–1939. doi: 10.1016/0006-2952(87)90491-6. [DOI] [PubMed] [Google Scholar]
- 3.Buening MK, Wold JS. Ethanol-moxalactam interactions in vivo. Rev Infect Dis. 1982;4((6)Suppl):S555–563. doi: 10.1093/clinids/4.supplement_3.s555. [DOI] [PubMed] [Google Scholar]
- 4.Uri JV, Parks DB. Disulfiram-like reaction to certain cephalosporins. Ther Drug Monit. 1983;5(2):219–224. doi: 10.1097/00007691-198306000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Fromtling RA, Gadebusch HH. Ethanol-cephalosporin antibiotic interactions: an animal model for the detection of disulfiram (Antabuse)-like effects. Methods Find Exp Clin Pharmacol. 1983;5(9):595–600. [PubMed] [Google Scholar]
- 6.Matsubara T, Otsubo S, Ogawa A, Nakao H. Effects of beta-lactam antibiotics on the acetaldehyde-metabolizing system in germ-free rats. Jpn J Pharmacol. 1987;45(1):115–119. doi: 10.1254/jjp.45.115. [DOI] [PubMed] [Google Scholar]
- 7.Buening MK, Wold JS, Israel KS, Krammer RB. Disulfiram-like reaction to beta-lactams. JAMA. 1981;245(20):2027. [PubMed] [Google Scholar]
- 8.Lancut M, Zarebska A, Sekita-Krzak J, Czerny K. Histological changes of white rat kidney after experimental administration of ethanol and cephalexin. Ann Univ Mariae Curie Sklodowska Med. 2003;58(1):268–272. [PubMed] [Google Scholar]
- 9.Zarebska A, Bakiera K, Visconti J, Kwietniewska M, Czerny K. Histological changes in the pancreas of white rats after administering cephalexin and ethanol. Ann Univ Mariae Curie Sklodowska Med. 2002;57(1):167–173. [PubMed] [Google Scholar]
- 10.Zarebska A, Hernik D, Matusiewicz J, Czerny K. The influence of experimental administration of ethanol and cephalexin on stomach mucous barrier of rat. Ann Univ Mariae Curie Sklodowska Med. 2004;59(1):145–150. [PubMed] [Google Scholar]
- 11.Portier H, Chalopin JM, Freysz M, Tanter Y. Interaction between cephalosporins and alcohol. Lancet. 1980;2(8188):263. doi: 10.1016/s0140-6736(80)90151-8. [DOI] [PubMed] [Google Scholar]
- 12.Moreels S, Neyrinck A, Desmet W. Intractable hypotension and myocardial ischaemia induced by co-ingestion of ethanol and disulfiram. Acta Cardiol. 2012;67(4):491–493. doi: 10.1080/ac.67.4.2170696. [DOI] [PubMed] [Google Scholar]
- 13.Sande M, Thompson D, Monte AA. Fomepizole for severe disulfiram-ethanol reactions. Am J Emerg Med. 2011;30(1):262.e3–5. doi: 10.1016/j.ajem.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 14.Ho M, Yo C, Liu C, Chen C, Lee C. Refractive hypotension in a patient with disulfiram-ethanol reaction. Am J Med Sci. 2007;333(1):53–55. doi: 10.1097/00000441-200701000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Dang X. One patient died of disulfiram like reaction after combined intravenous cefoperazone and drinking alcohol. J Qianghai Med (Chinese) 2010;40(2):27. [Google Scholar]
- 16.Xian H, Yu Y. One patient died of disulfiram like reaction after consuming alcohol and subsequent intravenous cephalosporins. Journal of Clinical Rational Use of Medication (Chinese) 2011;4(1):71. [Google Scholar]
- 17.Yang R, Yang Y, Cheng L. One person died after consuming alcohol followed intravenous cefotaxime. Med Leg J (Chinese) 2010;3(4):221. [Google Scholar]
- 18.Yanagihara M, Okada K, Nozaki M, Tsurumi K, Fujimura H. [cephem antibiotics and alcohol metabolism] Jpn J Antibiot. 1985;38(3):634–642. [PubMed] [Google Scholar]


