Abstract
Totally implantable access ports (TIAPs) are generally used in oncology. Few studies have addressed complications associated with the insertion site. A total of 233 consecutive oncology patients were enrolled to receive TIAP inserts via internal jugular vein (IJV) or subclavian vein (SV). Data on clinicopathologic parameters and early/late complications were retrospectively collected. No differences were found early and late complication rates. Catheter injury was observed more frequently in the IJV group (2.9%) than in the SV group (1.0%) without statistical significance. Multivariate logistic regression analysis showed that age, switch to palliative use of TIAP, and the distribution of diseases (low risk in patients with colorectal cancer) were independent risk factors for determining complications. In conclusion, TIAP insertion site showed no impact on the early and late complication rates. Catheter injury appears to occur at the same frequency with both approaches. Therefore, medical doctors may choose their preferred puncture site when performing TIAP insertion.
Key words: TIAP, Internal jugular vein, Central venous port, Totally implantable venous access devices, TIVAD
Totally implantable access ports (TIAPs) have been widely used for the safe delivery of chemotherapy or parenteral nutrition in patients with malignant disease and other debilitating diseases.1−3 Early complications of TIAP placement have been reported to be pneumothorax, hemothorax, and arterial rupture. Late complications include infection and obstruction or fracture of the catheter.4,5 The pinch-off syndrome has been thought to reflect the occlusion or fracture of catheters inserted through the subclavian vein (SV).1 To avoid the occurrence of this syndrome, some researchers recommended that the TIAP catheter should be inserted through the right internal jugular vein (IJV)6−8 or infraclavicular axillary vein under ultrasound guidance.9 However, we have reported 2 rare cases of TIAP catheter fracture when introduced through the right IJV.10,11 Accordingly, we wished to evaluate whether TIAPs inserted via the IJV would present fewer catheter injury and complications than those inserted via the SV. To clarify this issue, we retrospectively compared early and late complications following TIAP insertion in our institute.
Methods
Patients
A total of 233 consecutive oncology patients were planned to receive TIAP inserts for systemic intravenous chemotherapy from January 2007 to July 2012 at the Department of Surgery, Shiga University of Medical Science in Shiga, Japan, and the associated hospital. The deadline for data acquisition was April 30, 2013. We retrospectively collected data on patient clinicopathologic parameters by reviewing medical records. We compared early and late complications between 2 different routes, the IJV and SV. We defined early complications as those observed peri-operatively and those related to the surgical procedure. We defined late complications as those reported at least 24 h after the surgical procedure, such as TIAP infection (including TIAP-related sepsis confirmed by microbiologic blood cultures), venous thrombosis, catheter injury, and catheter malfunctioning (allowing perfusion but not aspiration or total catheter obstruction), as previously reported in the other study.12 The early complications were compared between the planned IJV approach group and the planned SV approach group. Late complications were compared between the implanted via the IJV group and the implanted via the SV group. Patients received chest radiography or chest computed tomography for routine follow-up of malignant diseases care at least every 6 months or less. The catheter tip position and late complications such as port dislocation, catheter injury, and vein thrombosis were reviewed using these follow-up chest radiography or chest computed tomography compared to the initial tip position, catheter route, and port position.
Surgical procedure
The surgeons selected the first puncture position and placement site of the TIAPs. The TIAPs were implanted in the surgical room, using maximal barrier precautions under local anesthesia and electrocardiography, heart rate, blood pressure, and pulse oximetry monitoring. BARD X-port isp (Medicon Inc., Osaka, Japan) was used in all patients. We inserted the guide wire and catheter using the Seldinger technique under fluoroscopy to confirm placement in the superior vena cava. We checked the incidence of early complications using chest radiography after the surgical procedure. On puncturing the SV, the central vein was cannulated using the Seldinger technique according to an anatomical landmark. If the catheter could not be placed in the first planned SV, a different puncture site was selected. Ultrasound-guided puncture was employed to mark the position of the IJV. If venous puncture could not be completed, a different puncture site was selected.
Statistical analysis
Data for continuous variables are expressed as median values (range, minimum–maximum). Data for categorical variables are expressed as cases (percentages). We used JMP Version 9 (SAS Institute Inc., Cary, NC, USA) for statistical analysis. Wilcoxon and Kruskal-Wallis rank order tests were performed for ordinal variables. Comparison between 2 groups was performed using Fisher's exact test or the chi-square test. Reverse Kaplan-Meier plots were used to illustrate the risk of late complications after implantation of totally implantable access ports in the IJV and SV groups. To identify the prognostic risk factors for determining the late complications after the implantation of TIAPs, univariate and multivariate logistic regression analyses were performed. A P value of < 0.05 was considered to indicate statistical significance.
Results
Patients and backgrounds
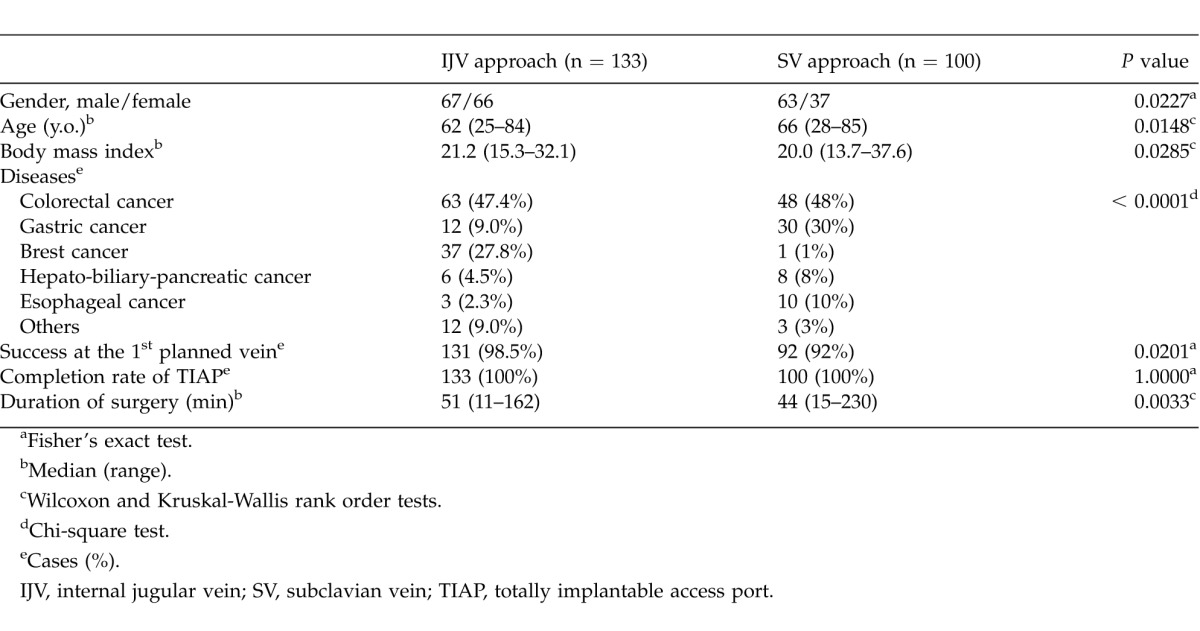
The first puncture site was the IJV in 133 patients (IJV approach group) and the SV in 100 patients (SV approach group). In the SV approach group, the insertion site was changed to the opposite side of the SV in 4 patients and to the IJV in 4 patients. In the IJV approach group, the puncture site was changed to the opposite side of the IJV in 1 patient and to the SV in 1 patient (Fig. 1). Gender distribution differed between the 2 groups: the number of female patients was higher in the IJV approach group than in the SV approach group. Patients in the SV approach group were older. Body mass index (BMI) was higher in the IJV approach group (P = 0.0285). The distribution of diseases was statistically different (P < 0.0001), particularly with regard to gastric cancer and breast cancer (Table 1). The completion rate of TIAP implantation was 100% in each group. The success rate for the first planned puncture site was significantly higher in the IJV approach group (98.5%) than in the SV approach group (92.0%; P = 0.0201). The duration of surgery was shorter in the SV approach group than in the IJV approach group (44 min vs. 51 min, P = 0.0033; Table 1).
Fig. 1.
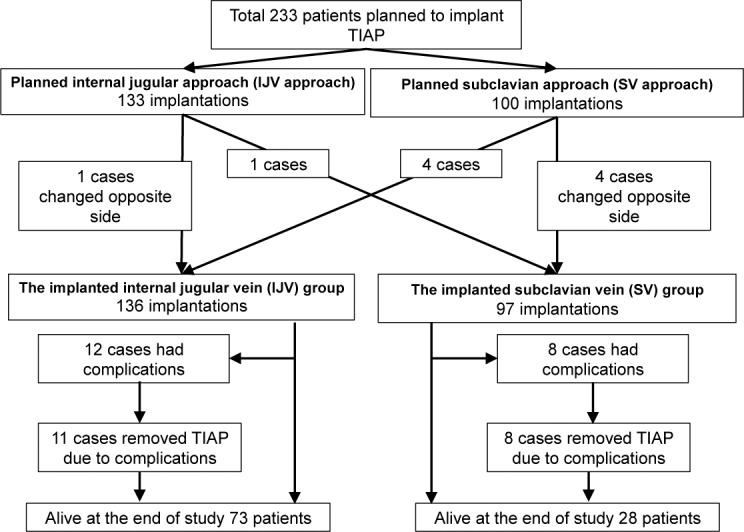
The study flow chart.
Table 1.
Patient characteristic among IJV and SV approach
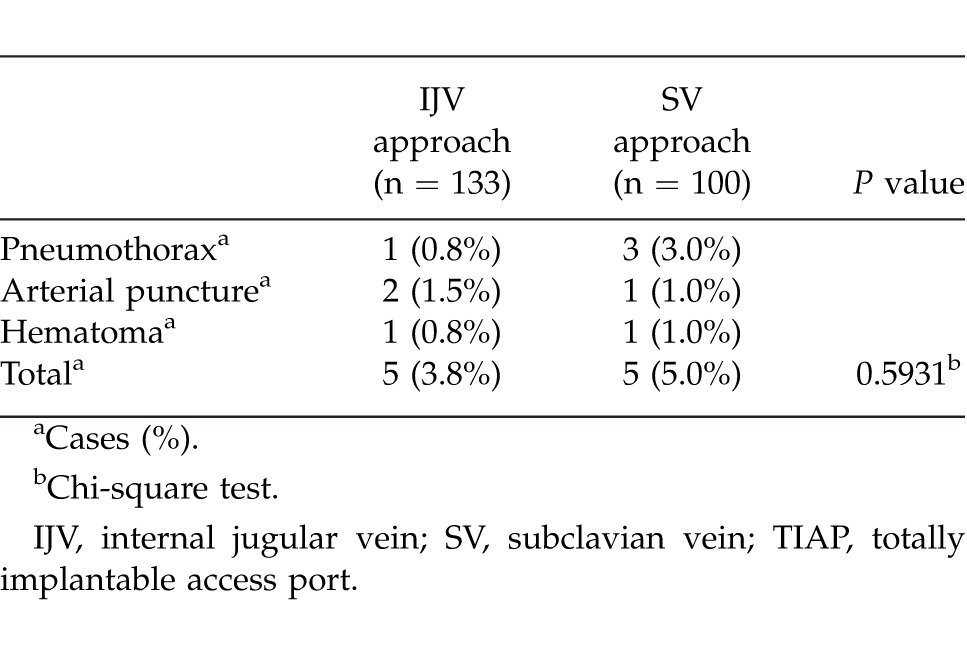
Early complications
Five patients in the IJV approach group (3.8%) and 5 patients in the SV approach group (5.0%) experienced early complications, and this difference was not statistically significant (P = 0.5931; Table 2).
Table 2.
Early complications following TIAP implantation via the IJV and SV
Late complications
The implanted via the IJV group included 136 cases, and the implanted via the SV group, 97 cases. The background characteristics of these 2 groups showed the same trends as those of the IJV approach group and the SV approach group (data not shown). The duration of the observation period differed significantly between the implanted via the IJV group (556 days) and the implanted via the SV group (402 days). More patients were alive at the end of the study in the implanted via the IJV group than in the implanted via the SV group. The frequency of switching to palliative use of TIAP was significantly higher in the implanted via the SV group than in the implanted via the IJV group (Table 3).
Table 3.
Patient outcomes after TIAP implantation via the IJV and SV
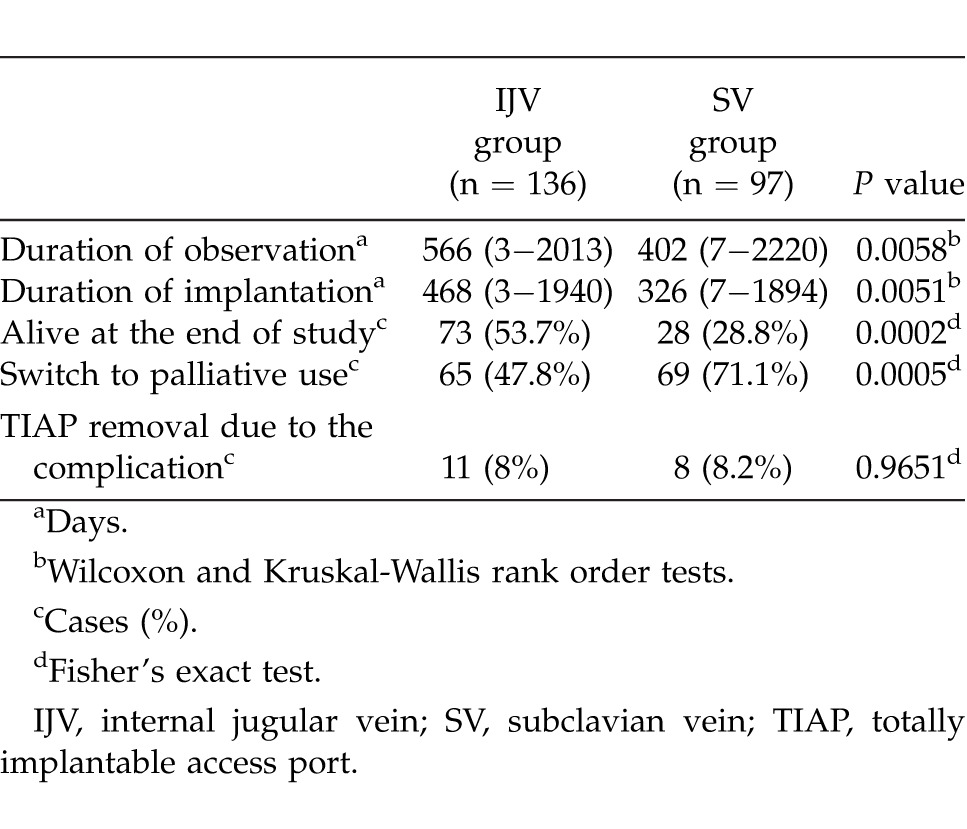
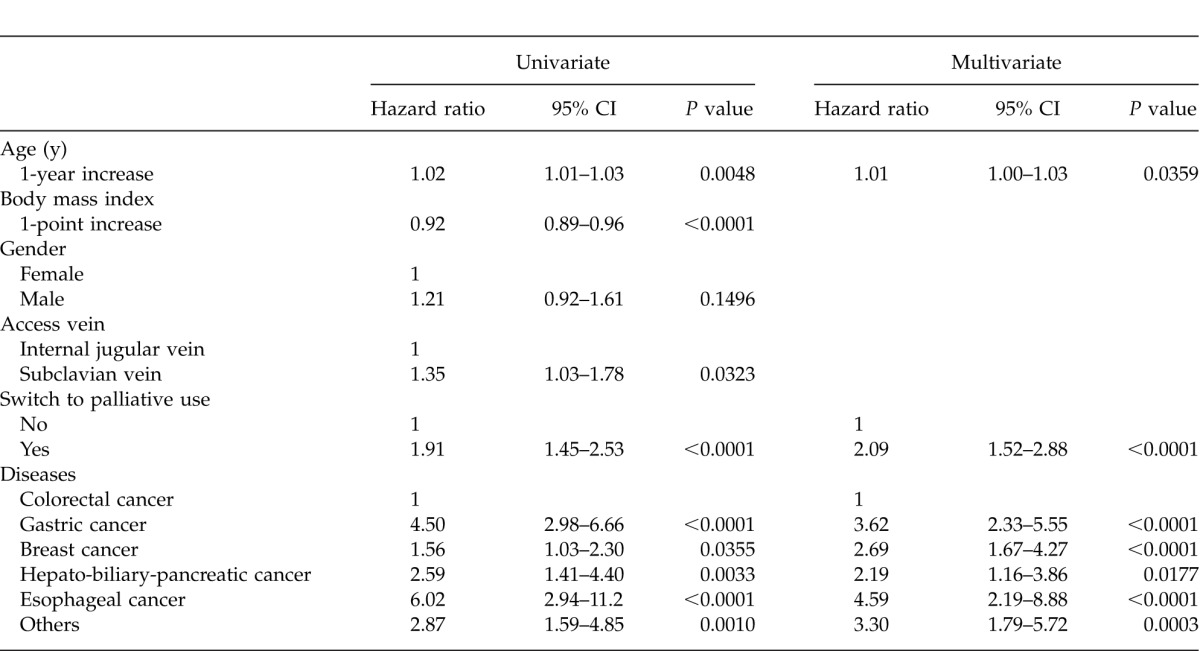
We observed late complications in 8 cases (8.2%) in the implanted via the SV group and in 12 cases (8.1%) in the implanted via the IJV group (P = 1.000). The characteristics of late complications associated with TIAPs did not differ significantly between TIAPs placed in the IJV and in the SV. The incidence of catheter injury (3 cases of catheter fracture and 1 case of pin hole leakage) was rather higher in the IJV group (2.9%) than that (1 case of catheter fracture) in the SV group (1.0%), but this difference was not statistically significant (Table 4). The cumulative risk of late complications after implantation of TIAPs did not differ significantly between the IJV group and the SV group (Fig. 2). Univariate analysis demonstrated statistical significance for age, BMI, access vein (IJV or SV), switch to palliative use, and the distribution of diseases. Multivariate logistic regression analysis showed that age, switch to palliative use, and the distribution of diseases were independent prognostic factors for determining late complications after implantation of TIAPs. In particular, patients with colorectal cancer presented the lowest risk for TIAP removal due to complications (Table 5).
Table 4.
Late complications of TIAP indwelling in the IJV and SV
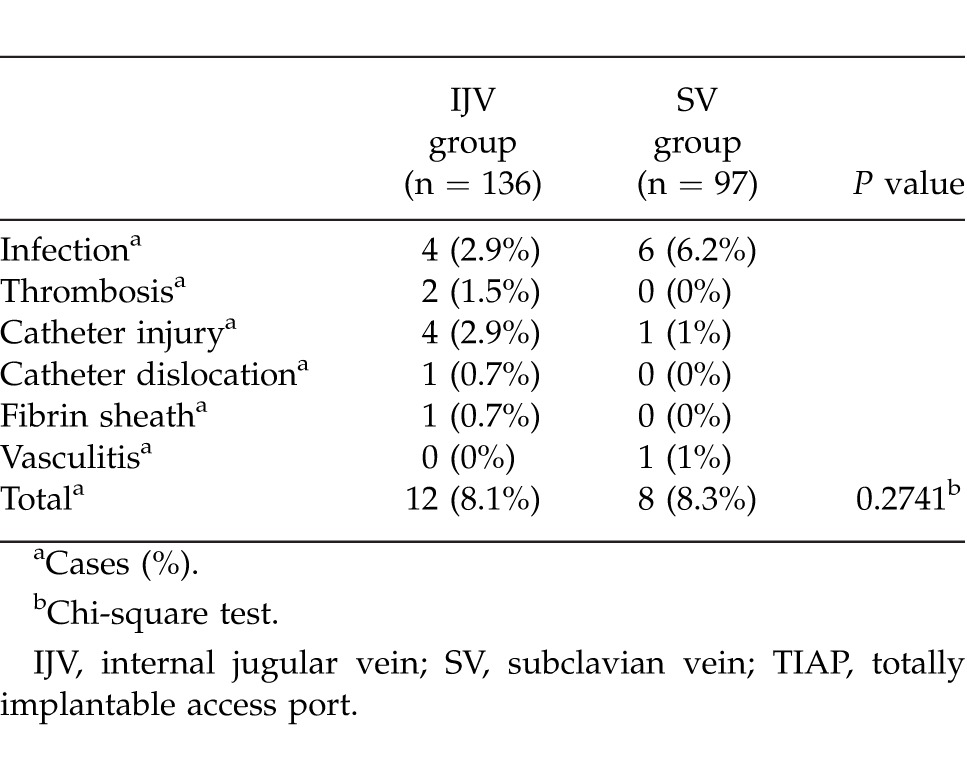
Fig. 2.
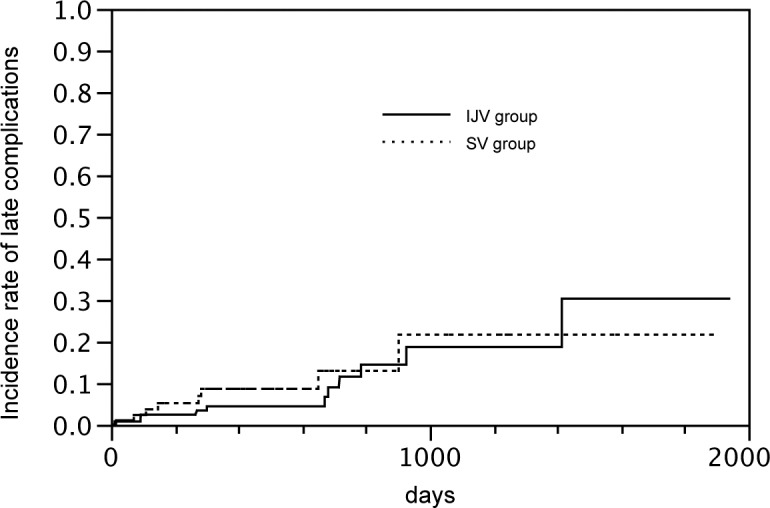
Reverse Kaplan-Meier plot showing the cumulative risk of late complications after implantation of TIAPs in the internal jugular vein (IJV) group and the subclavian vein (SV) group. There was no significant difference between the 2 groups. Log-rank test: P = 0.4935.
Table 5.
Univariate and multivariate logistic regression analyses of prognostic factors for determining the late complications of TIAP
Discussion
Some researchers have recommended that TIAPs be inserted through the IJV to avoid the pinch-off syndrome6,13, thrombosis, and stenosis14, but a few reports have compared SV and IJV. In the present study, we retrospectively compared early and late complications following the introduction of TIAPs via the IJV and SV in our institute. We hypothesized that TIAPs inserted via the IJV would present fewer catheter injuries and complications than those inserted via the SV. In particular, we expected a lower frequency of catheter injury in the IJV group than in the SV group; however, there was no difference in the incidence of early and late complications between TIAP insertion via the IJV and SV. A randomized control study also demonstrated that central venous insertion modality and sites (IJV, SV, and cephalic access) had no impact on either early or late complication rates.15 Charvat et al showed that late complications requiring removal of TIAPs were found in 6.2% of patients receiving an implant via the right IJV.6 Plumhans et al found no differences in late complications between indwelling in the IJV and SV.14 Our results were almost similar to those presented in these reports regarding early and late complications.
Our results showed that the incidence of catheter injury was 2.9% with IJV placement. The cause of catheter fracture in the SV group was pin-off syndrome. Catheter injury due to TIAPs inserted via the IJV is believed to be very rare. Growing evidence indicates that TIAPs inserted via the IJV cause catheter injury more frequently than expected.6,7,14,15 A recent large-scale retrospective study also showed that the incidence of catheter fracture in patients who had a TIAP catheter introduced via the right internal jugular vein was 1.69%.16 The incidence of catheter rupture because of the pinch-off syndrome is reported to range from 1.1% to 5.0%.1,17 It is possible that the risk of catheter injury on placing the catheter in the IJV is similar to that on placing the catheter in the SV. The causes of catheter fracture and pinhole leakage in the IJV group were suggested chronic stress against catheter. For example, we experienced the catheter fracture of the TIAP at the level of the clavicle. In this case, the strap of the patient's backpack appeared to come in contact with the catheter and compress it against the clavicle, resulting in catheter injury.10 The other case suggested the catheter fatigue and fracture were caused by chronic stress at the flexure of the catheter induced by the motion of the neck.11
Park et al showed that the right high jugular vein approach is a feasible alternative to the right low jugular vein approach.18 They reported that the right high jugular vein approach did not cause problems with catheter kinking, but could result in an acute angle between the subcutaneous portion and intravenous portion. We attempt to place TIAPs as low as possible in the IJV with ultrasound guidance in order to avoid catheter kinking and to shorten the subcutaneous tunnel. However, the catheter injury that we experienced during this observational period was suggested to be related to catheter kinking, in which we indicated right high jugular vein approach.11 Park et al did not experience any catheter fracture during their observational period; however, their study included only 21 cases in the high puncture group.18 Therefore, further studies are necessary to clarify whether the venous puncture position is related to catheter fatigue and fracture. Although the recommended venous puncture site in the IJV for TIAP remains unknown, we believe that lower puncture sites are safer when performing central venous insertion via the IJV for TIAP.
Moreover, multivariate logistic regression analysis to identify the prognostic factors for determining late complications of TIAPs showed that BMI (low risk in patients with a high BMI), switch to palliative use of TIAP, and the distribution of diseases (low risk in patients with colorectal cancer in particular) were selected as the independent risk factors. The patients' nutritional and immune status and disease progression appeared to be related to the occurrence of late complications, although we could not evaluate them in this study.19 For example, we observed five late complications in patients with palliative use of TIAP. Three of 5 patients (60%) had infectious complication of TIAP. Furthermore, it is difficult to find the reason why the late complications of TIAP are fewer in colorectal cancer patients. In the subgroup analysis of this study, the frequency in palliative use of TIAP was significantly different among disease distribution (gastric cancer, 81%; hepato-biliary-pancreatic cancer, 86%; esophageal cancer, 77%; colorectal cancer, 55%; breast cancer, 22%). The incidence of removal due to completion of chemotherapy was also significantly different among disease distribution (colorectal cancer, 5.4%; breast cancer, 21%; other diseases, 0%). These kinds of bias may influence the results of multivariate logistic regression analysis.
We acknowledge several limitations of the current study. At first, this study was a retrospective, nonrandomized, study. Second, although we verified that the late complication after the implantation of TIAPs might be similar between SV and IJV group, the patients' backgrounds were quite different between the two groups. Therefore, multivariate logistic regression analysis to identify the prognostic factors for determining late complications of TIAPs was performed. Furthermore, there have been reported complications of TIAPs that we have not experienced in our study period, such as catheter migration, leakage from the port membrane, drug extravasation, port-site and pocket infection, port rotation, catheter malposition and kinking of catheter.1 Additional prospective studies are needed to clarify the significant and proper risk factors for determining late complications of TIAPs.
In conclusion, TIAPs implanted through the IJV were associated with similar early and late complications to TIAPs implanted through the SV. The success rate for insertion via the IJV approach was higher than that via the SV approach. Age, switch to palliative use of TIAP, and distribution of diseases (low risk particularly in patients with colorectal cancer) were identified as independent prognostic factors for determining the late complications of TIAPs in this cohort. Therefore, medical doctors may choose their preferred puncture site when performing TIAP insertion.
Acknowledgments
Financial or material support was provided by the Department of Surgery, Shiga University of Medical Science, Shiga, Japan.
Footnotes
Yoshinobu Nagasawa and Tomoharu Shimizu contributed equally to this work.
References
- 1.Kurul S, Saip P, Aydin T. Totally implantable venous-access ports: local problems and extravasation injury. Lancet Oncol. 2002;3(11):684–692. doi: 10.1016/s1470-2045(02)00905-1. [DOI] [PubMed] [Google Scholar]
- 2.Sawayama H, Hayashi N, Watanabe M, Takamori H, Beppu T, Baba H. The central vein access port and catheter in outpatient chemotherapy for colorectal cancer: a retrospective study of 101 patients. Surg Today. 2012;42(1):29–34. doi: 10.1007/s00595-011-0016-5. [DOI] [PubMed] [Google Scholar]
- 3.Tsai YF, Ku YH, Chen SW, Huang WT, Lu CC, Tsao CJ. Right- and left-subclavian vein port-a-cath systems: comparison of complications. Eur Surg Res. 2012;49(2):66–72. doi: 10.1159/000339308. [DOI] [PubMed] [Google Scholar]
- 4.Surov A, Wienke A, Carter JM, Stoevesandt D, Behrmann C, Spielmann RP, et al. Intravascular embolization of venous catheter–causes, clinical signs, and management: a systematic review. JPEN J Parenter Enteral Nutr. 2009;33(6):677–685. doi: 10.1177/0148607109335121. [DOI] [PubMed] [Google Scholar]
- 5.Ishizuka M, Nagata H, Takagi K, Kubota K. Total parenteral nutrition is a major risk factor for central venous catheter-related bloodstream infection in colorectal cancer patients receiving postoperative chemotherapy. Eur Surg Res. 2008;41(4):341–345. doi: 10.1159/000160181. [DOI] [PubMed] [Google Scholar]
- 6.Charvat J, Linke Z, Horaekova M, Prausova J. Implantation of central venous ports with catheter insertion via the right internal jugular vein in oncology patients: single center experience. Support Care Cancer. 2006;14(11):1162–1165. doi: 10.1007/s00520-006-0073-2. [DOI] [PubMed] [Google Scholar]
- 7.Yip D, Funaki B. Subcutaneous chest ports via the internal jugular vein. A retrospective study of 117 oncology patients. Acta Radiol. 2002;43(4):371–375. doi: 10.1080/j.1600-0455.2002.430405.x. [DOI] [PubMed] [Google Scholar]
- 8.Teichgraber UK, Kausche S, Nagel SN, Gebauer B. Outcome analysis in 3,160 implantations of radiologically guided placements of totally implantable central venous port systems. Eur Radiol. 2011;21(6):1224–1232. doi: 10.1007/s00330-010-2045-7. [DOI] [PubMed] [Google Scholar]
- 9.Osawa H, Hasegawa J, Yamakawa K, Matsunami N, Mikata S, Shimizu J, et al. Ultrasound-guided infraclavicular axillary vein puncture is effective to avoid pinch-off syndrome: a long-term follow-up study. Surg Today. 2012;43(7):745–750. doi: 10.1007/s00595-012-0309-3. [DOI] [PubMed] [Google Scholar]
- 10.Shimizu T, Mekata E, Murata S, Yamamoto T, Tani T. A case of catheter fracture of a totally implantable access port introduced through the rght internal jugular vein. J Surg Oncol. 2011;103(5):460–461. doi: 10.1002/jso.21758. [DOI] [PubMed] [Google Scholar]
- 11.Nagasawa Y, Shimizu T, Sonoda H, Chou H, Mekata E, Tani T. Is catheter rupture rare after totally implantable access port implantation via the right internal jugular vein? Report of a case. Surg Today. 2013 doi: 10.1007/s00595-013-0631-4. Epub ahead of print. In press. [DOI] [PubMed] [Google Scholar]
- 12.Karanlik H, Kurul S. Modification of approach for totally implantable venous access device decreases rate of complications. J Surg Oncol. 2009;100(3):279–283. doi: 10.1002/jso.21341. [DOI] [PubMed] [Google Scholar]
- 13.Surov A, Jordan K, Buerke M, Arnold D, John E, Spielmann RP, et al. Port catheter insufficiency: incidence and clinical-radiological correlations. Onkologie. 2008;31((8–9)):455–461. doi: 10.1159/000140454. [DOI] [PubMed] [Google Scholar]
- 14.Plumhans C, Mahnken AH, Ocklenburg C, Keil S, Behrendt FF, Gunther RW, et al. Jugular versus subclavian totally implantable access ports: catheter position, complications and intrainterventional pain perception. Eur J Radiol. 2011;79(3):338–342. doi: 10.1016/j.ejrad.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 15.Biffi R, Orsi F, Pozzi S, Pace U, Bonomo G, Monfardini L, et al. Best choice of central venous insertion site for the prevention of catheter-related complications in adult patients who need cancer therapy: a randomized trial. Ann Oncol. 2009;20(5):935–940. doi: 10.1093/annonc/mdn701. [DOI] [PubMed] [Google Scholar]
- 16.Wu CY, Fu JY, Feng PH, Kao TC, Yu SY, Li HJ, et al. Catheter fracture of intravenous ports and its management. World J Surg. 2011;35(11):2403–2410. doi: 10.1007/s00268-011-1200-x. [DOI] [PubMed] [Google Scholar]
- 17.di Carlo I, Fisichella P, Russello D, Puleo S, Latteri F. Catheter fracture and cardiac migration: a rare complication of totally implantable venous devices. J Surg Oncol. 2000;73(3):172–173. doi: 10.1002/(sici)1096-9098(200003)73:3<172::aid-jso11>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 18.Park HS, Kim YI, Lee SH, Kim JI, Seo H, Lee SM, et al. Central venous infusion port inserted via high versus low jugular venous approaches: retrospective comparison of outcome and complications. Eur J Radiol. 2009;72(3):494–498. doi: 10.1016/j.ejrad.2008.09.015. [DOI] [PubMed] [Google Scholar]
- 19.Chang YF, Lo AC, Tsai CH, Lee PY, Sun S, Chang TH, et al. Higher complication risk of totally implantable venous access port systems in patients with advanced cancer - a single institution retrospective analysis. Palliat Med. 2013 Feb;27(2):185–191. doi: 10.1177/0269216311428777. [DOI] [PubMed] [Google Scholar]


