Abstract
Objectives.
Across many research domains, evidence for complicated grief as a distinct psychopathology continues to grow. Previous research from neuropsychology has shown an increased attentional bias to emotionally relevant stimuli in those suffering from complicated grief. This study furthers our understanding of the characteristics that distinguish complicated grief. We expand on previous research by (a) testing older adults, (b) excluding those with comorbid major depressive disorder, (c) using participant-chosen grief-related stimuli, and (d) using a married, nonbereaved control group.
Methods.
We recruited 76 older adults in 3 groups: spousally bereaved with complicated grief, spousally bereaved with noncomplicated grief, and nonbereaved controls. Performance on the Wisconsin Card Sorting Task, Digit Span Backwards, and the emotional counting Stroop was examined.
Results.
Results indicate longer reaction time across 3 blocks of grief-related words in the complicated grief group but no difference across 3 blocks of the neutral words. The 3 groups performed comparably on the other neurocognitive tasks, indicating no cognitive differences in working memory or set shifting between groups. Furthermore, these effects of complicated grief generalize to older adults and appear independent of major depression.
Discussion.
Complicated grief has cognitive interference as a neuropsychological component highlighting it as distinct from noncomplicated grief.
Key Words: Aging, Attention, Bereavement, Complicated grief, Stroop, Widow.
More than 900,000 older adults are widowed each year in the United States, and over half of all American women aged more than 64 have suffered conjugal bereavement (Elliott & Simmons, 2011; Moss, Moss, & Hansson, 2001). Although many are quite resilient, others have a more complicated course (Bonnano et al., 2002). Recently, researchers have used empirical data to categorize complicated versus noncomplicated grief and to demonstrate their distinct determinants, discriminant validity (e.g., complicated grief vs. depression), concomitant physiology, and predictive validity for postbereavement physical and mental health (Prigerson et al., 1997). This research has spurred the consideration of including complicated grief (also called traumatic grief, prolonged grief, and persistent complex bereavement disorder) in the Diagnostic and Statistical Manual of Mental Disorders—Fifth edition (DSM-V). Specific symptoms of grief, persisting for more than 6 months, comprise the consensus criteria for distinguishing normal grief and complicated grief (Prigerson & Jacobs, 2001). These symptom clusters include (a) separation distress (intense yearning and searching for the deceased, intrusive preoccupying thoughts about the deceased, and excessive loneliness) and (b) cognitive, emotional, and behavior symptoms (futility about the future, numbness or detachment, disbelief about the death, feeling that life is meaningless or part of oneself has died, a lost sense of security or trust, assuming physical symptoms of the deceased, or excessive anger related to the death). Several studies show discrimination between complicated grief and major depression and between complicated grief and posttraumatic stress disorder (Neria et al., 2007; Simon et al., 2007).
Intrusive thoughts and the avoidance of those thoughts are prevalent during bereavement (Clayton, 1990; Horowitz, Wilner, & Alvarez, 1979). Strong, unbidden thoughts and images of the deceased loved one and the death event occur and compel one’s attention. In most bereaved individuals, intrusive thoughts and avoidance decrease over time, but they may persist for years (Zisook, Devaul, & Click, 1982). The criteria for complicated grief include unusually high levels of intrusive thoughts and yearning for the deceased loved one. Those individuals with complicated grief are more likely to be “triggered” by bereavement-related cues or to have an attentional bias for these cues.
Cognitive changes that occur during bereavement include poor memory, intrusive thoughts, and concentration difficulty and are significantly more pronounced than those reported by nonbereaved controls (Clayton, Halikes, & Maurice, 1971). In individuals aged 65–80, widow(er)hood is an independent predictor of cognitive decline, even when controlling for physical functioning and depressive symptoms (Aartsen, Van Tilburg, Smits, Comijs, & Knipscheer, 2005). Neuropsychological functioning in bereaved individuals aged 80–95, compared with a matched nonbereaved sample (Xavier, Ferraz, Trentini, Freitas, & Moriguchi, 2002), showed that bereavement was longitudinally associated with worsened cognitive performance, specifically involving attention and memory. This decreased performance could not be explained by greater symptoms of depression.
Executive functioning, and specifically response interference, can be measured through neuropsychological tests such as the Stroop task (Stroop, 1935). In its original form, the Stroop task was composed of a series of color names printed in various colors. Reaction time to names of colors printed in contrasting ink is reliably slower than reaction times to words printed in the same color as the color name (e.g., the word “blue” printed in blue). Response interference occurs when one must respond to the word’s meaning rather than to the word’s color.
To assess the interference component of emotional dysregulation, a modified Stroop task has been developed using emotional words (i.e., the emotional Stroop [e-Stroop]). The words chosen are either neutral or specific to an emotional disorder such as generalized anxiety or, in this study, complicated grief. Because of the greater attention to these emotion-specific cues, the e-Stroop effect manifests as longer reaction time to grief words than neutral words. The e-Stroop can assess the extent to which there is an attentional bias to emotional stimuli, or in other words, to which attentional resources have been redirected toward the stimuli (Williams, Mathews, & MacLeod, 1996). The e-Stroop has been shown to differentiate healthy individuals from those with generalized anxiety disorder (Mathews & MacLeod, 1985), obsessive–compulsive disorder (Foa, Ilai, McCarthy, & Shoyer, 1993), and posttraumatic stress disorder (Foa, Feske, Murdock, Kozak, & McCarthy, 1991), with longer reaction times of these groups to disorder-relevant emotional words.
This study builds on recent work examining the nature of attentional bias in complicated grief using the e-Stroop paradigm. Maccallum and Bryant (2010) found that younger adults suffering from complicated grief showed slower response times to death-related stimuli compared with neutral stimuli. Their findings indicate information-processing biases for emotionally salient stimuli. This did not hold for the noncomplicated grief group, which showed comparatively faster response times. Similarly, Mancini and Bonanno (2012) evidenced that younger adults in the complicated grief group were unaffected by a priming stimulus that consistently decreased response time in a noncomplicated grief group. This study differed from these prior two studies in the following four ways: (a) we used an older population (62–82 years); (b) we excluded from all groups (including complicated grief) those persons diagnosed with major depressive disorder; (c) we included a nonbereaved control group, in addition to complicated and noncomplicated grief groups; and (d) we used emotional words chosen by the participants as reflective of their own grief experience (i.e., personalized stimuli).
Although previous work in the neurocognitive arena support a maladaptive response to grief stimuli in complicated grief, these previous studies fail to adequately distinguish complicated grief as a separate pathology from depression. This study recruited a group of older adults who had complicated grief but did not have comorbid major depressive disorder, because although the disorders can be comorbid (Sung et al., 2011), complicated grief is distinct from depression in 50%–60% of clinical samples (Neria et al., 2007; Simon et al., 2007). Statistical methods such as stepwise multiple regression have been used previously in an effort to account for depressive symptomatology (Maccallum & Bryant, 2010). However, manipulations of this kind can inherently distort the construct being studied. More specifically, complicated grief and major depression have some symptoms in common (e.g., low mood); controlling for depression may remove variance due to symptoms of depression that overlap with those seen in complicated grief. Removing this variance would then give an incomplete picture of the effect of complicated grief (Miller & Chapman, 2001).
One way this issue of overlap can be addressed is by screening and excluding complicated grievers currently suffering from major depression, a methodological distinction of this study. As measured by the Beck Depression Inventory-II (BDI-II), major depression is generally seen in those scoring at or above 30 points (Beck et al., 1961). Indeed, the aforementioned study by Maccallum and Bryant (2010) utilized a Complicated Grief sample with a mean (M) score of 30.30, qualifying them as having the disorder. Our sample, however, involved a Complicated Grief subsample with a mean BDI score of 18.07, indicating only mild symptoms of depression (Beck et al., 1961).
Given prior findings with the Stroop and e-Stroop, we hypothesized that those older adults with complicated grief should evidence longer reaction times to personal reminders of their loved one’s absence due to difficulties from interference compared with those with noncomplicated grief and nonbereaved controls.
Methods
Participants
Seventy-seven older adults were recruited from the Los Angeles region by direct mailing lists and advertisements at area senior centers. Participants were between 62 and 82 years of age (M = 71.85), were predominantly female (72%), and were predominantly Caucasian (75%). Of this sample, 17 met criteria for complicated grief, 28 had noncomplicated grief, and 32 were nonbereaved, married control participants.
Exclusion criteria used for this study included (a) presence of current major psychiatric disorder (e.g., major depressive disorder, alcohol, or substance dependence) as assessed with the Structured Clinical Interview for DSM-IV (SCID-I) (Spitzer, Williams, Gibbons, & First, 1994), (b) use of psychotropic medications initiated since the death event, (c) immunosuppressive medication, (d) current major medical illnesses (e.g., cancer), and (e) Mini-Mental State Examination (MMSE) score of less than or equal to 18. For the nonbereaved, married controls, exclusion criteria included the death of a first-degree family member or a close friend in the past 3 years.
The UCLA Institutional Review Board approved the study and all participants gave written informed consent after a complete description of the study.
Procedures
In order to define groups, bereaved participants were given the 19-item Inventory of Complicated Grief (ICG; Prigerson et al., 1995). An ICG score of 30 or higher was used to diagnose complicated grief (Shear, Frank, Houck, & Reynolds, 2005). The BDI-II (Beck, Steer, Ball, & Ranieri, 1996) was used to further assess the presence of any depressive symptoms.
An emotional counting Stroop (ec-Stroop) was developed in order to prevent the need for verbal responding, which is particularly important in neuroimaging of Stroop tasks, due to motion artifact from jaw movement (Bernal & Altman, 2009; Gianaros, May, Siegle, & Jennings, 2005). This study used the ec-Stroop because a subsample performed the task in the scanner (data not reported here). In the ec-Stroop, the target word is printed between one and four times in a column, and instead of ink color being reported by the participant, the number of words is reported with a button press.
A list of 73 grief-related words was developed from interviews with bereaved participants in prior research studies by the principal investigator (Gundel, O’Connor, Littrell, Fort, & Lane, 2003; O’Connor et al., 2008). Each grief-related word in the list was matched with a neutral word that had the same number of letters, the same number of syllables, the same part of speech, and the same frequency in the language. Bereaved participants (i.e., both complicated and noncomplicated grief groups) were presented with the list and asked to indicate which ones were relevant to their own grief experience, creating an idiographic list (within a limited range) for each bereaved participant (Williams et al., 1996). Each nonbereaved participant was matched to a bereaved participant and was given the bereaved participant’s grief-related words, so that study participants saw the same words across the whole sample.
The ec-Stroop was administered in six blocks preceded by a 10-s fixation stimulus. Three blocks contained grief-related words and three contained matched neutral words. Each block contained 20 stimuli presented for a duration of 1.45 s. The run began with a 0.05 s orienting stimulus (a “+” centered on the screen). All participants were given a10-trial practice run with neutral stimuli to demonstrate adequate understanding of the task. Participants were allowed to repeat the practice run one additional time if necessary. The presentation order of grief and neutral trials was randomized across participants.
In addition to the ec-Stroop, three other assessments of cognitive ability were administered to all participants. First, the MMSE was administered to provide a brief assessment of global cognitive functioning (Folstein, Folstein, & McHugh, 1975). Second, the Wechsler Memory Scale (WMS) Digit Span Backwards, a subtest of the WMS-III(Wechsler, 1945/1997), was used to assess elements of working memory, transformation of information, and mental manipulation (Groth-Marnat & Baker, 2003). As per standard administration of this test, individuals were presented with a series of number strings and were instructed to recall and say aloud the numbers in reverse order. There were seven levels, where level one consisted of a two-digit string length and increased to an eight-digit string.
Third, the Wisconsin Card Sorting Task (WCST; Heaton, 1981) is a measure of flexible thinking and reasoning and was used to assess an aspect of executive functioning (i.e., the ability to form and shift cognitive sets). The WCST computerized version 2 (WCST-64: CV2; Heaton, 2003) was administered and stimulus cards were chosen using either mouse or keyboard input. All default settings were used. Feedback was given visually and was displayed for 3 s. When the card was selected, the participant had a 2.5 s window to change his or her answer prior to getting a feedback about their choice. Responses were not timed and 64 trials were administered.
Statistical Analyses
IBM SPSS Statistics v. 19.0 (SPSS, Chicago, IL) was used for all statistical analyses. Analysis of variance (ANOVA) and chi-square tests were used to compare groups on demographic variables. An analysis of covariance (ANCOVA) was conducted to compare complicated grief, noncomplicated grief, and nonbereaved control groups on measures of cognitive function (e.g., MMSE, WCST, Digit Span Backwards). A repeated measures ANOVA was used to compare the three groups on the ec-Stroop. Additionally, covariates were added to assess the effect of age on the ec-Stroop because of the established association between age and reaction time. The alpha level for all effects tests was set at p < .05.
Results
Depressive Symptoms
Demographic and depressive symptoms are listed in Table 1. Low mean scores for the nonbereaved and bereaved groups (M = 2.46 and M = 5.44, respectively) indicate minimal or no depression with no significant difference between groups. Although higher than the other two groups (M = 18.07), the complicated grief group also indicated only mild-to-moderate symptoms (and did not have major depressive disorder according to DSM criteria; see Methods section). Missing BDI-II data included nonbereaved (n = 6), noncomplicated grief (n = 2), and complicated grief (n = 2).
Table 1.
Demographic Description of the Study Sample
| Nonbereaved (n = 32) | Noncomplicated grief (n = 28) | Complicated grief (n = 17) | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean/N | SD/% | Mean | SD/% | Mean/N | SD/% | F value/χ2 | p Value | |
| Age | 72.06 | 4.76 | 73.07 | 5.33 | 70.41 | 6.44 | 1.30 | .28 |
| Gender (female) | 22 | 69% | 21 | 75% | 12 | 71% | 0.29 | .86 |
| Ethnicity (non-Caucasian) | 6 | 19% | 6 | 21% | 7 | 41% | 17.10 | .25 |
| Employment (retired) | 19 | 59% | 22 | 79% | 14 | 82% | 6.98 | .32 |
| Education (postgraduate) | 13 | 41% | 9 | 32% | 3 | 18% | 8.97 | .35 |
| Years married/partnered | 38.25 | 14.73 | 36.46 | 15.81 | 42 | 12.52 | 0.75 | .48 |
| Body mass index | 27.29 | 4.22 | 26.58 | 5.9 | 28.2 | 4.32 | 0.56 | .57 |
| Smoke (smokes) | 0 | 0% | 0 | 0% | 1 | 5.9% | 3.58 | .17 |
| Alcohol (drinks per week) | 2.70 | 4.95 | 2.13 | 4.44 | 2.31 | 4.51 | 0.11 | .89 |
| BDI-II | 2.46 | 3.24 | 5.44 | 5.37 | 18.07 | 11.03 | 28.83 | <.01 |
| ICG | — | — | 15.26 | 7.13 | 36.88 | 9.47 | 74.25 | <.01 |
| MMSE | 28.48 | 1.75 | 27.96 | 2.03 | 26.47 | 3.52 | 4.25 | .02 |
| Digit Span Backwards | 7.53 | 2.92 | 7.11 | 2.87 | 6.73 | 3.17 | 0.38 | .69 |
| WCST standard perseverative errors | 120.89 | 20.3 | 124.71 | 17.54 | 112.54 | 41.27 | 0.37 | .69 |
| WCST categories achieved | 3.33 | 0.92 | 3.57 | 1.17 | 3.38 | 1.26 | 0.30 | .74 |
Notes: ANOVA = analysis of variance; BDI-II = Beck Depression Inventory-II; ICG = Inventory of Complicated Grief; MMSE = Mini-Mental State Examination; WCST = Wisconsin Card Sorting Task.
Continuous variables: mean (± SD), F value (ANOVA); categorical variables: n (%), χ2 value (Chi-square test). Due to incomplete testing: MMSE (N = 76), Digit Span (N = 72), and WCST (N = 61).
Cognitive Measures
An effect of group (nonbereaved control, noncomplicated grief, complicated grief, N = 76) was seen specifically on performance in the MMSE, F(2,72) = 4.25, p = .02. There was no significant effect of age as a covariate on MMSE performance, F(1,72) = 0.38, p = .54; F = 3.35, p = .07). Post hoc testing demonstrated that the complicated grief group differed significantly from both nonbereaved and noncomplicated groups (p = .005 and p = .035, respectively). Nonbereaved and noncomplicated groups did not differ significantly on MMSE performance.
No effect of group (N = 72) was seen in performance on the Digit Span Backwards test, F(2,68) = 0.38, p = .69. The standard measures of the WCST include raw correct total, standard perseverative responses, standard perseverative errors, nonperseverative errors, categories, trials to complete, and failure to maintain set. No effect of group (N = 59) was seen on any of the standard outcome measures of the WCST, F(2,57) = 0.19–0.93, p = 0.39–0.83. There were no sex differences on any of the cognitive tests.
Emotional Counting Stroop
Because the amount of interference created by emotional stimuli increases across stimuli presentations (Williams et al., 1996), we used a repeated measures ANOVA, controlling for age, to compare groups on three blocks of grief stimuli and neutral stimuli in separate analyses. Age was included as a covariate because it is correlated with reaction time performance. We found a significant group by block interaction, F(4,73) = 3.24, p = .014, in blocks with grief words (when BDI was added to the model, group was still near significance, although reduced, F(3, 62) = 2.26, p = .067, and BDI was not significant in between-groups analysis; Figure 1A). A post hoc pairwise comparison revealed that the complicated grief group differed significantly from the noncomplicated grief group (p = .04) and from the nonbereaved group (p = .03), such that complicated grief showed a longer reaction time to the emotionally significant words. The latter two groups did not differ significantly from each other. There was no main effect for block, but a trend toward an effect for group in the between-groups analysis (F = 2.86, p = .06).
Figure 1.
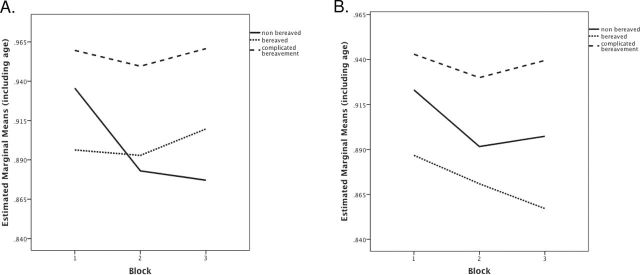
Reaction time to emotional counting Stroop (ec-Stroop) task across three trials of (A) personalized grief-related words and (B) matched neutral words.
The same analysis with neutral stimuli blocks indicated no significant main effect of block (p = .20) and no interaction of group × block (p = .73; Figure 1B). Again, there was a trend toward a group effect in the between-groups analysis (F = 2.9, p = .06). Post hoc analysis showed that this was driven by a significant difference between complicated grief and noncomplicated grief groups (p = .02), such that complicated grief showed a longer reaction time.
Next, a “Stroop effect” variable was computed, which is the difference in reaction time between the grief-related and neutral words across all blocks. Because this is a difference score, the average reaction times for grief-related and neutral blocks were transformed into z scores in order to create reaction time distributions that meet interval scale assumptions. The grief-related z score was then subtracted from the neutral z score for each individual. In order to investigate a Stroop effect across all blocks, a composite score subtracting neutral reaction time from grief reaction time was derived. An ANOVA indicated a significant effect of group (group was still near significance when BDI was added to the model, though it was reduced, F(3, 62) = 2.44, p = .095. However, BDI was not a significant predictor, F(3, 62) = 1.08, p = .30) on the Stroop effect, F(2,76) = 3.08, p = .05. Post hoc analyses revealed that there was a significant difference between nonbereaved and noncomplicated grief groups (p = .03), and a trend for a difference between the nonbereaved and complicated grief groups (p = .07), such that both grief groups had a greater Stroop effect or, in other words, had a longer reaction time to grief words than neutral words across all blocks.
Discussion
This study demonstrated that older spousally bereaved adults had slower reaction times across three blocks of the ec-Stroop to idiographic grief-related words and did not differ from noncomplicated grief and nonbereaved controls across three blocks of matched neutral words. However, these group differences were not found in the Digit Span Backwards, or in the WCST, suggesting that the neuropsychological difference between the groups is not in working memory or set shifting. The between-groups difference in the ec-Stroop performance demonstrates that those with complicated grief are responding to all words more slowly. However, the group × block interaction, only in the grief condition, demonstrates that the emotional impact of the grief-related words increases the interference over repeated presentations only in the complicated grief group.
The complicated grief group did have lower MMSE scores than both the noncomplicated grief and control group. The MMSE is a global measure of cognitive functioning, and therefore, it is difficult to pinpoint the neuropsychological function that distinguished these groups from their performance. Given the cross-sectional nature of this study, we are unable to determine the causal direction between complicated grief and cognitive functioning. Having complicated grief may increase cognitive impairment in older adults or having cognitive impairment may increase the likelihood of developing complicated grief after the death of a spouse.
The slower reaction time to the ec-Stroop in our older population with complicated grief replicates prior work with the same results in younger populations (Maccallum & Bryant, 2010; Mancini & Bonanno, 2012). Several key features of this study extend our understanding of interference in complicated grief. First, our population was older than in prior studies, and therefore, complicated grief continues to show reduced attentional control during emotion-specific words even in older age when reaction time in general is reduced. Second, none of our study participants had clinically defined major depressive disorder. This included the complicated grief group. Although prior work has statistically controlled for depressive symptoms, this is the first study to show the e-Stroop effect in complicated grief without depression. Because depression has a known effect on the reaction time, the present results cannot be a result of overall slowing due to depressive symptomatology.
Third, this study utilized words that were chosen by the participants as personally relevant to their grief experience. Words that are personalized to the person’s relevant clinical disorder has been shown to discriminate other psychopathologies, such as generalized anxiety disorder (Mathews & MacLeod, 1985), obsessive–compulsive disorder (Foa et al., 1993), and posttraumatic stress disorder (Foa et al., 1991). Finally, this study used a nonbereaved control group. Because grief-related words are salient for all persons (not just for those who have recently experienced bereavement), this study establishes the differences between the slower reaction times of those with complicated grief from the response times of those who have not recently been exposed to bereavement.
How can an individual receive a moderate BDI-II score but not be diagnosed with major depressive disorder? A very clear distinction between depressive and complicated grief symptomatology is that, whereas depressive cognitions and experiences are global, in complicated grief, symptoms are very specific to the loss of the loved one. For example, guilt in major depression must be pervasive, but in complicated grief, guilt is specific only to the circumstances of the death event (Shear et al., 2011). Thus, a person may respond in a self-report format that they experience guilt but not be diagnosed with this criterion symptom in a clinician interview. The complicated grief group also does not appear to have “vascular depression,” based on two pieces of data. First, the executive functioning (as measured by the WCST and Digit Span Backwards) does not differ between the complicated grief and nonbereaved, nondepressed groups, and second, the rates of cardiovascular medication (i.e., antihypertensives, statins, aspirin) do not differ between groups (data not shown). Similarly, subsyndromal or minor depression may exist in some of the Complicated Grief however, although major depression and minor depression share many characteristics, cognitive impairment is not characteristic of older persons with minor depression (Koenig, 1997). Although it may not be possible to determine the exact contribution of mild depressive symptoms, the observation of cognitive difficulties in Complicated Grief persons is of interest in its own right.
This study requires replication, preferably in a larger sample. Additional neuropsychological testing, if done longitudinally, may show when these cognitive differences appear between groups and when (if ever) they resolve. Functional MRI data may shed light on how these words are being processed differently in the brain, and therefore, what neurocognitive features of complicated grief are distinct. However, this study adds to a growing body of literature showing cognitive, clinical, and physiological differences between complicated and noncomplicated grief and should be used to underscore the relevance of complicated grief as a unique category in the DSM-V.
Funding
This research was supported by the National Institute of Aging (NIA; K01-AG028404), Los Angeles Community Academic Partnership for Research in Aging (L.A. CAPRA) center, the Arizona Alzheimer’s Disease Core (National Institutes of Health [NIH]/NIA grant P30-AG019610-12), and the UCLA Cousins Center for Psychoneuroimmunology.
Acknowledgment
Thanks to Alfred W. Kaszniak for his comments on an earlier draft of this manuscript.
References
- Aartsen M. J., Van Tilburg T., Smits C. H., Comijs H. C., Knipscheer K. C. (2005). Does widowhood affect memory performance of older persons? Psychological Medicine, 35, 217–226. 10.1017/S0033291704002831 [DOI] [PubMed] [Google Scholar]
- Beck A. T., Ward C. H., Mendelson M., Mock J., Erbaugh J. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4, 561–571. 10.1001/archpsyc.1961.01710120031004 [DOI] [PubMed] [Google Scholar]
- Beck A. T., Steer R. A., Ball R., Ranieri W. (1996). Comparison of Beck Depression Inventories-IA and -II in psychiatric outpatients. Journal of Personal Assessment, 67, 588–597. 10.1207/s15327752jpa6703_13 [DOI] [PubMed] [Google Scholar]
- Bernal B., Altman N. (2009). Neural networks of motor and cognitive inhibition are dissociated between brain hemispheres: An fMRI study. International Journal of Neuroscience, 119, 1848–1880. 10.1080/00207450802333029 [DOI] [PubMed] [Google Scholar]
- Bonnano G. A., Wortman C. B., Lehman D. R., Tweed R. G., Haring M., Sonnega J. … Nesse R. M. (2002). Resilience to loss and chronic grief: A prospective study from preloss to 18-months postloss. Journal of Personality & Social Psychology, 83, 1150–1164. 10.1037/0022-3514.83.5.1150 [DOI] [PubMed] [Google Scholar]
- Clayton P. J. (1990). Bereavement and depression. Journal of Clinical Psychiatry, 51, 34–40 Clayton 1990 ISSN: 01606689; PMID: 2195011. [PubMed] [Google Scholar]
- Clayton P. J., Halikes J. A., Maurice W. L. (1971). The bereavement of the widowed. Diseases of the Nervous System, 32, 597–604 Clayton 1971 ISSN: 0012-3714. [PubMed] [Google Scholar]
- Elliott D. B., Simmons T. (2011). Marital Events of Americans: 2009, (American Community Survey Reports, ACS-13). Washington, DC: U.S. Census Bureau; [Google Scholar]
- First M B., Spitzer R. L, Gibbon M., Williams J. B. W. (2002). Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition. (SCID-I/NP) New York: Biometrics Research, New York State Psychiatric Institute.
- Foa E. B., Feske U., Murdock T. B., Kozak M. J., McCarthy P. R. (1991). Processing of threat-related information in rape victims. Journal of Abnormal Psychology, 100, 156–162. 10.1037/ 0021-843X.100.2.156 [DOI] [PubMed] [Google Scholar]
- Foa E. B., Ilai D., McCarthy P. R., Shoyer B. (1993). Information processing in obsessive-compulsive disorder. Cognitive Therapy & Research, 17, 173–189. 10.1007/BF01172964 [Google Scholar]
- Folstein M. F., Folstein S. E., McHugh P. R. (1975). “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189–198. 10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- Gianaros P. J., May J. C., Siegle G. J., Jennings J. R. (2005). Is there a functional neural correlate of individual differences in cardiovascular reactivity? Psychosomatic Medicine, 67, 31–39. 10.1097/01.psy.0000151487.05506.dc [DOI] [PubMed] [Google Scholar]
- Groth-Marnat G., Baker S. (2003). Digit Span as a measure of everyday attention: A study of ecological validity. Perceptual and Motor Skills, 97, 1209–1218. 10.2466/pms.2003.97.3f.1209 [DOI] [PubMed] [Google Scholar]
- Gundel H., O’Connor M.-F., Littrell L., Fort C., Lane R. D. (2003). Functional neuroanatomy of grief: An fMRI Study. American Journal of Psychiatry, 160, 1946–1953. 10.1176/appi.ajp.160.11.1946 [DOI] [PubMed] [Google Scholar]
- Heaton R. K. (1981). Wisconsin Card Sorting Test manual, Odessa, FL: Psychological Assessment Resources; [Google Scholar]
- Heaton R K. (2003). WCST-64: Computerised Version 2 Research Edition. Florida: Psychological Assessment Resources [Google Scholar]
- Horowitz M., Wilner N., Alvarez W. (1979). Impact of Event Scale: A measure of subjective stress. Psychosomatic Medicine, 41, 209–218 [DOI] [PubMed] [Google Scholar]
- Koenig H. G. (1997). Differences in psychosocial and health correlates of major and minor depression in medically ill older adults. Journal of the American Geriatrics Society, 45, 1487–1495 ISSN 00028614 PMID 9400559. [DOI] [PubMed] [Google Scholar]
- Maccallum F., Bryant R. A. (2010). Attentional bias in complicated grief. Journal of Affective Disorders, 125, 316–322. 10.1016/j.jad.2010.01.070 [DOI] [PubMed] [Google Scholar]
- Mancini A. D., Bonanno G. A. (2012). The persistence of attachment: Complicated grief, threat, and reaction times to the deceased’s name. Journal of Affective Disorders, 139, 256–263. 10.1016/j.jad.2012.01.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathews A., MacLeod C. (1985). Selective processing of threat cues in anxiety states. Behaviour Research and Therapy, 23, 563. 10.1016/0005-7967(85)90104-4 [DOI] [PubMed] [Google Scholar]
- Miller G. A., Chapman J. P. (2001). Misunderstanding analysis of covariance. Journal of Abnormal Psychology, 110, 40–48. 10.1037//0021-843X.110.1.40 [DOI] [PubMed] [Google Scholar]
- Moss M. S., Moss S. Z., Hansson R. O. (2001). Bereavement and old age. In Stroebe M. S., Hansson R. O. (Eds.), Handbook of bereavement research: Consequences, coping, and care, (pp. 241–260). Washington, DC: American Psychological Association; 10.1037/10436-010 [Google Scholar]
- Neria Y., Gross R., Litz B., Maguen S., Insel B., Seirmarco G. … Marshall R. D. (2007). Prevalence and psychological correlates of complicated grief among bereaved adults 2.5–3.5 years after September 11th attacks. Journal of Traumatic Stress, 20, 251–262. 10.1002/jts.20223 [DOI] [PubMed] [Google Scholar]
- O’Connor M.-F., Wellisch D. K., Stanton A. L., Eisenberger N. I., Irwin M. R., Lieberman M. D. (2008). Craving love? Enduring grief activates brain’s reward center. Neuroimage, 42, 969–972. 10.1016/j.neuroimage.2008.04.256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prigerson H. G., Bierhals A. J., Kasl S. V., Reynolds C. F., 3rd, Shear M. K., Day N.… Jacobs S. (1997). Traumatic grief as a risk factor for mental and physical morbidity. American Journal of Psychiatry, 154, 616–623 Prigerson 1997 ISSN: 1535-7338. [DOI] [PubMed] [Google Scholar]
- Prigerson H. G., Jacobs S. C. (2001). Traumatic grief as a distinct disorder: A rationale, consensus criteria, and preliminary empirical test. In Stroebe M. S., Hansson R. O., Stroebe W., Schut H. (Eds.), Handbook of bereavement research: Consequences, coping and care, (pp. 613–645). Washington, DC: American Psychological Association; [Google Scholar]
- Prigerson H. G., Maciejewski P. K., Reynolds C. F., 3rd, Bierhals A. J., Newsom J. T., Fasiczka A. … Miller M. (1995). Inventory of Complicated Grief: A scale to measure maladaptive symptoms of loss. Psychiatry Research, 59, 65–79. 10.1037/10436-026 [DOI] [PubMed] [Google Scholar]
- Shear K., Frank E., Houck P. R., Reynolds C. F., 3 rd (2005). Treatment of complicated grief: A randomized controlled trial. Journal of the American Medical Association, 293, 2601–2608. 10.1001/jama.293.21.2601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shear M. K., Simon N., Wall M., Zisook S., Neimeyer R., Duan N. … Keshaviah A. (2011). Complicated grief and related bereavement issues for DSM-5. Depression and Anxiety, 28, 103–117. 10.1002/da.20780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon N. M., Shear K. M., Thompson E. H., Zalta A. K., Perlman C., Reynolds C. F. … Silowash R. (2007). The prevalence and correlates of psychiatric comorbidity in individuals with complicated grief. Comprehensive Psychiatry, 48, 395–399. 10.1016/j.comppsych.2007.05.002 [DOI] [PubMed] [Google Scholar]
- Stroop J. R. (1935). Studies of interference in serial verbal reactions. Journal of Experimental Psychology, 18, 643–662. 10.1037/h0054651 [Google Scholar]
- Sung S. C., Dryman M. T., Marks E., Shear M. K., Ghesquiere A., Fava M., Simon N. M. (2011). Complicated grief among individuals with major depression: Prevalence, comorbidity, and associated features. Journal of Affective Disorders, 134, 453–458. 10.1016/j.jad.2011.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. (1945/1997). Wechsler Memory Scale®—Third edition (WMS-III), San Antonio, TX: Harcourt Assessment; [Google Scholar]
- Williams J. M., Mathews A., MacLeod C. (1996). The emotional Stroop task and psychopathology. Psychological Bulletin, 120, 3–24. 10.1037/0033-2909.120.1.3 [DOI] [PubMed] [Google Scholar]
- Xavier F. M. F., Ferraz M. P. T., Trentini C. M., Freitas N. K., Moriguchi E. H. (2002). Bereavement-related cognitive impairment in an oldest-old community-dwelling Brazilian sample. Journal of Clinical & Experimental Neuropsychology, 24, 294–301. 10.1076/jcen.24.3.294.983 [DOI] [PubMed] [Google Scholar]
- Zisook S., Devaul R. A., Click M. A. (1982). Measuring symptoms of grief and bereavement. American Journal of Psychiatry, 139, 1590–1593 Zisook 1982 ISSN: 1535-7228. [DOI] [PubMed] [Google Scholar]


