Abstract
Objectives.
We draw on cognitive discrepancy theory to hypothesize and test a pathway from poor health to loneliness in later life. We hypothesize that poor health will have a negative influence on social participation and social resources, and these factors will mediate between health and loneliness. We hypothesize that rural environments will amplify any difficulties associated with social participation or accessing social resources and that depression will moderate how intensely people react to levels of social contact and support.
Methods.
We conceptualize a mediation model and a moderated-mediation model. Nationally representative data on older people living in the Republic of Ireland are used to validate the hypothesized pathways.
Results.
In the mediation model, health has a significant indirect effect on loneliness through the mediating variables social resources and social participation. In the moderated-mediation model, rurality moderates the pathway between health and social resources but not social participation. Depressive symptoms moderate the effect of social resources on loneliness but not social participation.
Discussion.
The results provide further credence to cognitive discrepancy theory, suggesting that depressive symptoms influence cognitive processes, interfering with judgments about the adequacy of social interaction. The theory is extended by demonstrating the impact of the environment on loneliness.
Key Words: Analysis–moderated-mediation modeling, Environment, Health, Social participation, Social resources.
Competing theories have attempted to explain loneliness in later life (Victor, Scambler, Bond, & Bowling, 2000), with evolutionary (Cacioppo, Hughes, Waite, Hawkley, & Thisted, 2006), psychodynamic (Leiderman, 1969), and interactionist (Essex & Nam, 1987) perspectives being brought to bear on the subject. This article draws on cognitive discrepancy theory to hypothesize a pathway from poor health to loneliness in later life. Reflecting the complex relationship between poor health and loneliness, the article takes into account the mediating and moderating effects of environmental, social, and psychological factors.
Cognitive discrepancy theory suggests that loneliness is a subjective, unpleasant, and distressing phenomenon stemming from a discrepancy between individuals’ desired and achieved levels of social relations (Perlman & Peplau, 1981). Loneliness arises from a mismatch between actual and expected quality and frequency of social interaction, with potential sources of mismatch being associated with specific circumstances and life events, including the onset of one or more chronic conditions, migration, and widowhood. Avoiding loneliness entails addressing the mismatch, by adjusting either expectations regarding the quality and frequency of social interaction or achieved quality and frequency of social interaction to balance both elements.
Much of the research on loneliness in older populations reports on prevalence (e.g., Theeke, 2009; Victor, Scambler, Bowling, & Bond, 2005; Yang & Victor, 2008) or predictors of loneliness. Studies consistently report that certain life events have impact on loneliness, including poor health (Creecy, Berg, & Wright, 1985), retirement migration (Wenger, Davies, Shahtahmasebi, & Scott, 1996), and widowhood (de Jong Gierveld, van Tilburg, & Dykstra, 2006). These life events precipitate changes in achieved social relations (Perlman & Peplau, 1981). For example, poor health affects individuals’ ability to maintain their usual lifestyles, including customary levels of social interaction (Slivinske, Fitch, & Morawski, 1996), whereas spousal bereavement results in termination of a key relationship that usually provides an “exclusive, close, and intimate tie” (Dykstra & Fokkema, 2007, p. 9). Retirement migration may precipitate physical separation from family and friends, possibly resulting in decreased contact. However, decreased social interaction does not necessarily result in a permanent state of loneliness. For example, the loneliness experienced after widowhood declines over time (Wenger et al., 1996), suggesting that older people adjust either their levels of social interaction or personal expectations about types of relationship that are feasible or likely (Peplau & Caldwell, 1978).
In addition to life events and social resources, other factors associated with loneliness include age, gender, childlessness, poverty, education, income, environment, cognitive function, anxiety, and depression (Victor et al., 2005). Although a comprehensive review of literature on the predictors of loneliness is beyond the scope of this paper (see Luanaigh & Lawlor, 2008; Pitkala & Routasalo, 2003), evidence relating to sociodemographic, environmental, and psychological factors that are pertinent to our hypotheses is summarized below.
Research has been inconclusive regarding the role of age in predicting loneliness among older adults (Perlman, 1991, 2004). Although some studies show increasing loneliness with age (van Tilburg, Havens, & de Jong Gierveld, 2004; Wenger & Burholt, 2004), others show no effect (Creecy et al., 1985; de Jong-Gierveld, 1987; Jylhä, 2004). Research on the effect of gender on loneliness is equally inconclusive. Although most studies suggest that women express greater levels of loneliness than men (Borys & Perlman, 1985; de Jong Gierveld et al., 2006), others report the opposite (Dykstra & Fokkema, 2007). It has been noted that gender effects on loneliness are confounded by the use of measures that refer to the word “lonely,” with men appearing more reluctant than women to label themselves as lonely (Borys & Perlman, 1985). Despite contrary findings for both gender and age, poor material circumstances (such as income, education, socioeconomic status) are consistently related to greater levels of loneliness (de Jong Gierveld & Tesch-Romer, 2012; Savikko, Routasalo, Tilvis, & Strandberg, 2005). Thus, there is sufficient evidence to suggest that age, gender, and material circumstances should be controlled for in any model attempting to explain loneliness.
Although numerous studies explore the associations between sociodemographic variables and loneliness, relatively few address environmental correlates, or consider the physical environments to which individuals are exposed. De Jong Gierveld and colleagues (2006) note that “a relatively new area of research concerns (a) the societal patterning of standards for evaluating one’s social network of relationships and (b) the societal patterning of social and economic resources contributing to social integration” (p. 491). Consequently, few studies explore the impact of impoverished neighborhoods and social exclusion on loneliness (Scharf & de Jong Gierveld, 2008; Scharf, Phillipson, & Smith, 2004), or compare levels of loneliness experienced by older people in rural and urban areas (Burholt & Dobbs, 2012). Studies comparing loneliness in rural and urban areas reveal contrary findings, suggesting that expectations for social interaction and subsequently the experience of loneliness are culturally bound and influenced by local norms and values (Drennan et al., 2008; Paúl, Fonseca, Martín, & Amado, 2003). However, one U.K. study established a relationship between loneliness and population density in rural areas. The authors suggested that sparsity (in rural areas), coupled with a decrease in the functional ability of an older person, affects on the capacity to maintain social relationships with people who may be scattered residentially over a large rural area (Burholt, 2011). This suggests that the influence of health on loneliness may be amplified in rural areas.
Although few studies explore associations between loneliness and environmental factors, a proliferation of research has examined the relationship between loneliness and depression. Loneliness and depression are strongly correlated (e.g., Osborn et al., 2003), yet empirically and theoretically distinct (Hawkley et al., 2008). Regardless of the distinction between them, the terms are often used synonymously (Perlman, Gerson, & Spinner, 1978). For example, older people frequently describe depressive symptoms in terms of loneliness (Barg et al., 2006). However, neither all lonely people are depressed nor all depressed people are lonely (Koropeckyj-Cox, 1998). Although loneliness arises from the mismatch between perceived and actual social interaction, depression may have a greater range of origins (Perlman & Peplau, 1984).
Methodological Considerations
Although many individual (psychological and health), social, and environmental factors affect the experience of loneliness in later life, knowledge of how these factors influence loneliness remains limited. Not only do cross-sectional data make inferences about causality problematic, equally challenging is the lack of theoretical reasoning underpinning data analysis. Consequently, data-driven investigations of loneliness outweigh studies testing theoretical assumptions.
Several studies have attempted to assess the direction of association (causality) between loneliness and depression. Although participants in Barg and colleagues’ (2006) qualitative study viewed loneliness as a precursor to depression, the authors noted that despite the language used by participants, loneliness may be a manifestation of depression. Using cross-sectional data in a series of regression models, Alpass and Neville (2003) concluded that health and loneliness predicted depression. However, they noted that the cross-sectional nature of the data meant that the reverse could also be true. Indeed, Koropeckyj-Cox (1998) interpreted the results of her cross-sectional research in this manner, suggesting that depression interferes with social interaction, subsequently affecting loneliness (see also Cohen, 1990). Longitudinal studies of loneliness and depression have found that changes in loneliness (between baseline and follow-up) coincided with increased depression (Cacioppo et al., 2006; Heikkinen & Kauppinen, 2004). However, Cacioppo and colleagues’ (2006) study of middle-aged and older adults indicated that depression also predicted changes in loneliness, concluding that influences between loneliness and depressive symptoms are reciprocal.
In addition to the two longitudinal studies noted above, one other notable study has attempted to use more sophisticated analytical techniques to model loneliness in older adults. Fees, Martin, and Poon (1999) built on a body of work that had used demographic characteristics and health as predictors of loneliness, with social network and social activity as mediating variables (Creecy et al., 1985; de Jong-Gierveld, 1987). Fees and colleagues (1999) extended these analyses to include personality (anxiety) and mental health (cognition) as predictors alongside age and social contact (visiting behavior, telephone contact; see also Poon et al., 1992). Two structural models estimated the mediating effect of health between the independent variables and loneliness, and the mediating effect of loneliness between the same independent variables and health. Although poor subjective health predicted greater feelings of loneliness, health status did not mediate the other constructs. Conversely, loneliness predicted poor health and mediated between age, anxiety, and health. Although Fees and colleagues (1999) offered an a posteriori explanation of the models’ structure, this article develops an a priori conceptual model to test theoretical assumptions about how variables might interact and affect one another.
Since publication of Fees and colleagues’ (1999) paper, there have been substantial advances in statistical methods: the effect of multiple mediators and moderators can be estimated in the same model while controlling for other important characteristics. Furthermore, computationally intensive methods, such as bootstrapping for inference about indirect effects, can now be employed. Here, we build on the existing evidence regarding associations between individual, social, and environmental factors to conceptualize a mediation model and a moderated-mediation model (Hayes, 2012a; Muller, Judd, & Yzerbyt, 2005). The conceptual model is followed by empirical validation of the hypothesized pathways using a nationally representative data set of older people living in the Republic of Ireland to test cognitive discrepancy theory.
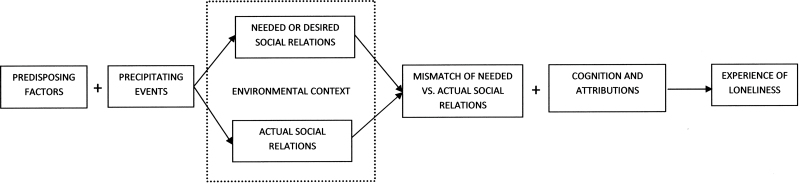
Perlman and Peplau (1998) developed a discrepancy model of loneliness, which is outlined in Figure 1. Our analytical mediation and moderated-mediation models are presented in Figures 2 and 3. In Figure 1, predisposing variables are those factors that put people at risk of loneliness but do not necessarily cause it (Perlman & Peplau, 1981). In this respect, in Figures 2 and 3, the predisposing variables are sociodemographic characteristics that are significantly associated with loneliness and are entered in our model as controls. In Figure 1, precipitating events are those which lead to a decrease in achieved levels of social interaction. In Figures 2 and 3, health is the independent variable and primary precipitating event. We hypothesize that poor health will be associated with greater levels of loneliness.
Figure 1.
A discrepancy model of loneliness adapted from Perlman and Peplau (1998).
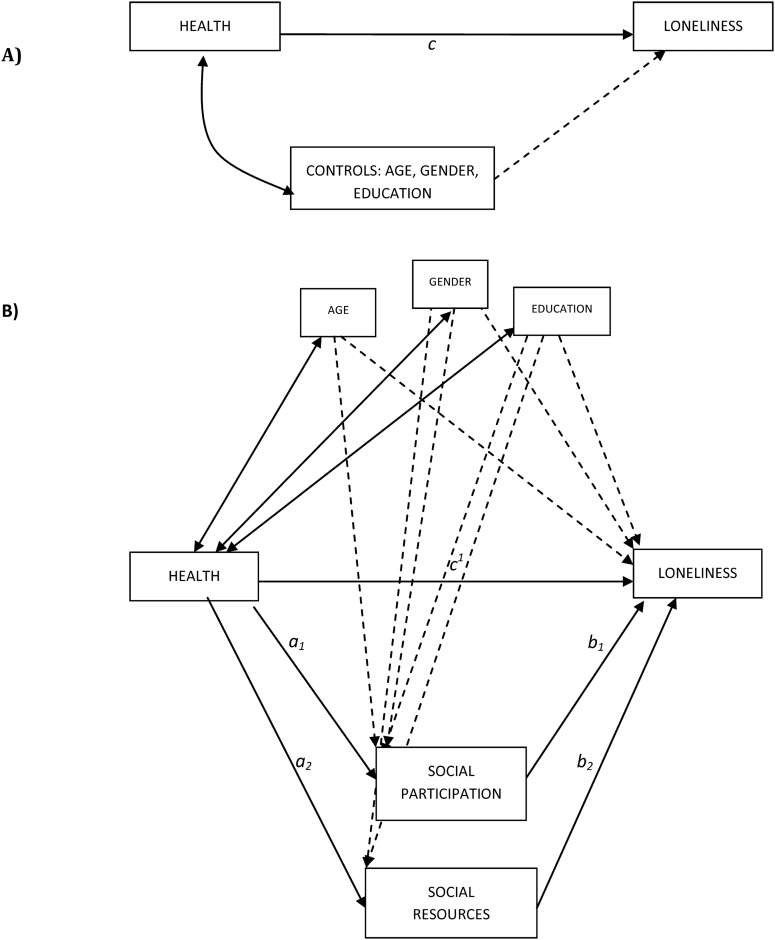
Figure 2.
Analytic diagram of the multiple-mediation model proposed.
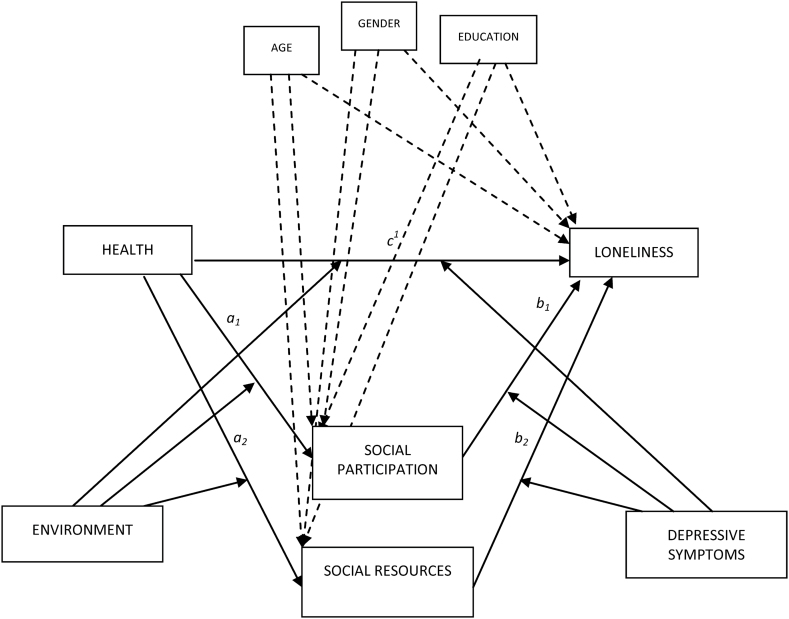
Figure 3.
Analytic diagram of the moderated-mediation model proposed.
Mediation is undertaken when one is interested in explaining the mechanism by which an independent variable causally influences a dependent variable (Hayes, 2012a). In the analytical model (Figure 2), we hypothesize that poor health will have a negative influence on social participation and social resources, and thus negatively influence the achieved level of social interaction: social participation and social resources will mediate between health and loneliness.
Moderation is used when one is interested in testing whether the magnitude of a variable’s effect on a dependent variable is dependent on a third set of variables (Hayes, 2012a). In this respect, we hypothesize that the environment will have an impact on achieved levels of social interaction, specifically that rural environments will amplify any difficulties associated with social participation or accessing social resources. We expect environment to moderate the model’s a and c paths (Figure 3). The model thereby moves beyond the original components of cognitive discrepancy theory to incorporate the contextual characteristics of an individual’s environment (de Jong Gierveld et al., 2006).
Finally, we take into account the desired level of social interaction and an older person’s ability to modify this to match their level of social interaction and avoid feelings of loneliness. Elsewhere, Dykstra and Fokkema (2007) explored the discrepancy model in relation to “emotional” loneliness using proxies (relational conflict and partnered centeredness) to approximate the mismatch between actual and desired quality of the relationship with a significant other. Although the authors operationalize the motivational reasons that could indicate discrepancy, they neither measure directly the expectation for social contact nor explore the cognitive processes that modulate the loneliness experience. Perlman and Peplau (1981) explain that any discrepancy between desired and achieved social relations may be labeled by an individual as loneliness, but that this self-labeling does not lead directly (or inevitably) to loneliness and may be modified by the person’s reaction to the situation. In this article, we neither measure expectations for social interaction directly nor include a proxy measure for discrepancy. Instead, we draw on Beck (1972) to propose that depression is a “cognitive process” that moderates how intensely people react to levels of social contact and support (see Figure 1).
Older people with depression are more likely than those without depressive symptoms to hold dysfunctional beliefs and negatively process personal information. For example, in the event of a failure to meet one’s own standards of social relations, older people with depression may attribute this to personal characteristics construing themselves as worthless, unlovable, and deficient. Furthermore, it has been suggested that people with depression have a negative view of their environment and the future, and do not believe that any action(s) will change their lives (Beck, 1972; Gonca & Savasir, 2001). Consequently, older people with depression will be less likely than those without depressive symptoms to alter their benchmark for “desired” social relations. Thus, we hypothesize that depression will have a moderating influence on the model’s b and c paths and that greater levels of depressive symptoms will amplify the influence of health on loneliness through the mediating variables social participation and social resources. This element of the cognitive discrepancy theory has been omitted from previous analysis (Figure 3).
Methods
Data and Sample
We address our research questions by drawing on cross-sectional (Wave 1) data from the Irish Longitudinal Study on Ageing (TILDA), a nationally representative study of community-dwelling people aged 50 and older in Ireland (Barrett, Savva, Timonen, & Kenny, 2011). Ireland represents an ideal national context for the analysis, given that 38% of the general population, and 42% of those aged 65 and older, were residing in rural areas at the 2011 national Census (Connolly, Finn, & O’Shea, 2012). Using a cluster approach to sample selection, all postal addresses in Ireland were assigned to one of 3,155 geographic clusters. Six hundred and forty clusters were selected for the sample stratified by socioeconomic group and geography to ensure representativeness. Forty households were selected from each cluster, and these were visited by an interviewer who ascertained the eligibility of all household members for inclusion in the sample (i.e., whether they were aged 50 years or older). All eligible individuals and their partners (regardless of age) were invited to participate in the study.
Interviewing commenced in October 2009 and was completed in February 2011 (Savva, 2011). Participants had face-to-face (computer-assisted personal interviewing) interviews in their own homes. In cases where two participants were married or living as married in the same home, only one provided the detailed response on family and financial circumstances. In total, 8,178 interviews were conducted with participants aged 50 and older and 329 with younger partners of eligible individuals (primarily to provide information regarding family and financial circumstances). The response rate for eligible households was 62% (Savva, 2011). Each participant was left a self-completion questionnaire to return to the research team by post. A total of 7,191 forms were returned, representing a response rate of 88%. This article is based on a sample of 6,613 participants with no missing data on the variables used in the analysis.
Cohort analysis has indicated that individuals with lower educational achievement are underrepresented in TILDA. Furthermore, there are minor differences in response rate among particular age and gender groups (Kearney et al., 2011). We have not applied weights to account for these differences in our analyses, using instead 5,000 bootstrap samples to derive robust estimates of confidence intervals for the coefficients in the models tested below.
Independent Variable
Health (representing a precipitating event) was measured using the number of self-reported general-practitioner-diagnosed chronic diseases from a list of seven: hypertension, diabetes (or high blood sugar), cancer, lung disease (including asthma), heart disease (including any of: angina, heart attack, congestive heart failure, heart murmur, abnormal heart rhythm, other heart trouble), stroke (including ministroke), and arthritis (Crimmins, Kim, & Solé-Auró, 2010).
Dependent Variable
Loneliness was measured using a three-item scale (Hughes, Waite, Hawkley, & Cacioppo, 2004), based on the widely used 20-item revised UCLA loneliness scale (Russell, 1996). The three items were “How often do you feel you lack companionship?,” “How often do you feel isolated from others?,” and “How often do you feel left out?” The score is the sum of all items, where higher scores represent greater levels of loneliness. The three-item scale has a reported alpha coefficient of reliability of 0.72, and in the present study, it was 0.81. Previously, external validity was demonstrated in strong significant correlations between the scale and the revised UCLA scale. Convergent and discriminant validity was demonstrated through associations, with measures of mood, emotion, and subjective and objective social isolation that other research has indicated are related to loneliness (Hughes et al., 2004).
Mediating Variables
Social resources were measured using the Berkman–Syme Social Networks Index (SNI). This is a composite measure of four types of social connection based on marital status (married vs. not), sociability (number and frequency of contact with children, close relatives, and close friends), religious group membership, and membership in other community groups. The index measures social resources at four levels: low social network resources (i.e., characterized by individuals with low intimate contacts [not married, fewer than six friends or relatives], and no membership in either church or community groups); medium social network resources; medium-high social network resources; and high resources. The operationalization of the SNI is described elsewhere (Berkman, 1977; Loucks et al., 2006).
Social participation was measured by counting the number of social activities in which participants were engaged at least monthly. The social activities were attending films, plays, concerts; attending classes, lectures; traveling for pleasure; playing cards, bingo, games; going to the pub; eating out; undertaking a sport, or other forms of exercise; and performing charity work.
Moderating Variables
Environment was captured using a dichotomous variable. The location of participating households was categorized as “Dublin city or county,” “another town or city,” or a “rural area.” In this analysis, we combine the first two categories and contrast with “rural areas.”
The Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977) was selected to assess depression in TILDA. It is designed to measure depressive symptoms in the general population (i.e., nonpsychiatric persons older than 18 years). The 20-item scale measures the major components of depressive symptomatology experienced in the previous week. In this article, in order to evaluate the role of depressive symptoms, we eliminated an item referring to feeling lonely from the remaining CES-D items before calculating the total score. The resulting scale ranges from 0 (low depressive symptoms) to 56 (high depressive symptoms; Hawkley, Masi, Berry, & Cacioppo, 2006).
Covariates
Demographic covariates used in the analysis were gender (male/female), age (4-year age bands), and education. The variable representing education was dichotomized: having some primary education (not complete) was coded 1 and contrasted with greater levels of education (comprising: primary or equivalent; intermediate/junior/group certificate or equivalent; leaving certificate or equivalent; diploma/certificate; primary degree; postgraduate/higher degree) coded 0.
Analysis
First, we adopt an analytical technique for mediation analysis, which can simultaneously test the effects of multiple variables (multiple mediation) and can determine the relative magnitude of the mediators’ specific indirect effects in relation to each other (Preacher & Hayes, 2008). Using multiple mediation, we test whether social resources and social participation (in parallel) mediate the effects of health on loneliness (Figure 2). We seek to determine the individual mediating effects of each variable after controlling for age, gender, and education, and for the remaining mediators. Thus, the direct, indirect, and total effects of X on Y are calculated partialing out the controls’ effect. We bootstrap the indirect effects of health on loneliness using the SPSS version of Preacher and Hayes’ (2008) macro for multiple mediation. The bootstrap estimates reported are based on 5,000 bootstrap samples. We use 95% bias corrected and accelerated (BCa) confidence intervals (CI) to determine significant mediation effects: mediators are only considered to have a significant effect when the 95% BCa CI for the point estimate does not include zero.
Second, we perform moderated-mediation analysis through construction and estimation of a conditional process model (Hayes, 2012a). Building on the mediation model, we explore the moderating effects of environment on the model’s a and c paths, and depressive symptoms on the model’s b and c paths (Figure 3). In a moderated-mediation model, the indirect effect of X on Y is dependent on the value of one or more moderators (Muller et al., 2005). Thus, in this moderated-mediation model, we estimated the extent to which an indirect effect of health on loneliness through the mediators “social resources” and “social participation” depends on the moderators “environment” and “depressive symptoms.” For this analysis, we use PROCESS, a computation procedure for SPSS developed by Hayes (2012a) that implements a moderated-mediation analysis and tests the analytical model specified in Figure 3 (Model 29: Hayes, 2012b).
Results
Respondents’ Characteristics
The sample comprised 94.7% Irish, 3.9% British, and 1.4% other nationalities. Most participants were married or living with a partner (71.5%). There were slightly fewer men (45.8%) than women (54.2%). A slightly greater proportion of older people lived in urban (52.3%) than in rural areas (47.7%) (Table 1 presents a full analysis of sample characteristics by location).
Table 1.
Sample Characteristics by Geographic Location
| Location | Urban, N = 3,458 | Rural, N = 3,155 | Total, N = 6,613 |
|---|---|---|---|
| % | % | % | |
| Agea | |||
| 50–54 | 19.8 | 20.6 | 20.2 |
| 55–59 | 20.3 | 20.7 | 20.5 |
| 60–64 | 17.3 | 17.6 | 17.4 |
| 65–69 | 15.4 | 14.7 | 15.1 |
| 70–74 | 12.2 | 11.2 | 11.7 |
| 75–79 | 8.2 | 8.7 | 8.4 |
| 80–84 | 4.7 | 4.2 | 4.4 |
| 85–89 | 1.8 | 1.8 | 1.8 |
| 90+ | 0.5 | 0.6 | 0.5 |
| Gendera | |||
| Male | 45.7 | 46.0 | 45.8 |
| Female | 54.3 | 54.0 | 54.2 |
| Educationa | |||
| Some primary education | 2.7 | 2.7 | 2.7 |
| Primary or equivalent | 21.7 | 27.4 | 24.4 |
| Intermediate | 21.7 | 25.8 | 23.7 |
| Leaving certificate or equivalent | 18.5 | 16.4 | 17.5 |
| Diploma/certificate | 16.9 | 15.6 | 16.3 |
| Primary degree | 10.8 | 7.7 | 9.3 |
| Postgraduate/higher degree | 7.5 | 4.3 | 6.0 |
| None | 0.1 | 0.1 | 0.1 |
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Number of chronic conditionsb | 1.42 (1.29) | 1.36 (1.3) | 1.39 (1.3) |
| Social resourcesb | 2.79 (0.89) | 2.95 (0.84) | 2.87 (0.87) |
| Social participationb | 2.68 (1.61) | 2.43 (1.59) | 2.56 (1.6) |
| Depressive symptomsb | 5.67 (6.93) | 5.05 (6.18) | 5.37 (6.59) |
| Lonelinessb | 4.11 (1.48) | 4.11 (1.48) | 4.11 (1.48) |
Notes. aPearson chi-square: age (χ 2 = 4.50, degrees of freedom [df] = 8, n.s.); gender (χ 2 = 0.04, df = 1, n.s.); education (χ 2 = 84.87, df = 7, p < .00).
bAnalysis of variance: number of chronic condition (F = 3.94, p < .05) range 0–6; social resources (F = 54.91, p < .00) range 0–4; social participation (F = 40.54, p < .00) range 0–8; depressive symptoms (F = 14.64, p < .00) range 0–50; loneliness (F = 0.04, n.s.) range 3–9.
Bivariate correlations of study variables are presented in Table 2. The control variable age was significantly associated with the independent variable and both mediators, with greater age associated with a greater number of chronic diseases (worse health status), greater levels of social resources but lower levels of social participation. Gender was associated with the dependent variable and one mediator (social participation): women were significantly lonelier and had lower levels of social participation than men. Education was associated with the independent variable, the dependent variable, and both mediators. Incomplete primary education was associated with poor outcomes: greater number of chronic conditions, greater levels of loneliness, and lower levels of social resources and social participation. Location was associated with the independent variable and both mediators. Participants living in rural areas were in worse health and had lower levels of social participation than those living elsewhere; however, they also had greater levels of social resources.
Table 2.
Bivariate Correlations Among the Study Variables
| 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|
| 1 Chronic conditions | 0.08*** | 0.32** | 0.02 | 0.06** | 0.12** | −0.03* | −0.05** | −0.11** |
| 2 Loneliness | 0.00 | 0.03* | 0.05** | 0.35** | 0.01 | −0.21** | −0.12** | |
| 3 Age | −0.02 | 0.10** | −0.02 | −0.01 | 0.04** | −0.13** | ||
| 4 Gender | −0.04** | 0.11** | −0.00 | −0.02 | −0.03* | |||
| 5 Education | 0.07** | −0.00 | −0.07** | −0.07** | ||||
| 6 Depressive symptoms | −0.04** | −0.16** | −0.12** | |||||
| 7 Location | 0.09** | −0.08** | ||||||
| 8 Social relations | 0.22** | |||||||
| 9 Social participation |
Notes. *Correlation is significant at the 0.05 level (two-tailed).
**Correlation is significant at the 0.01 level (two-tailed).
Unmoderated Mediation Model
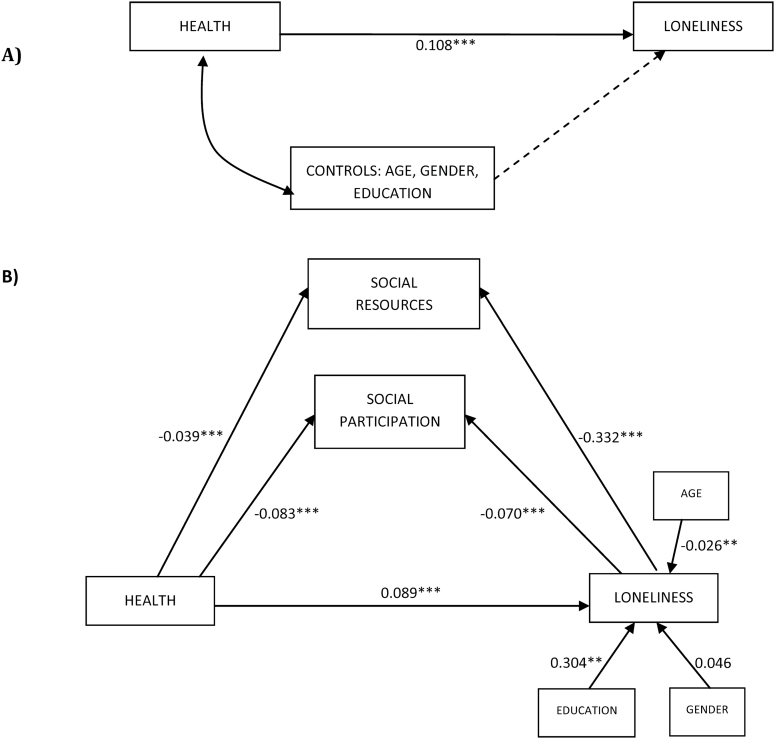
Diagram A in Figure 4 shows estimated coefficients for the total effect of health on loneliness (corrected for the effect of controls age, gender, and education) and indicates that a greater number of chronic conditions leads to higher levels of loneliness. Diagram B in Figure 4 shows estimated coefficients for the effect of health on the mediators (a paths) and the mediators’ effect on loneliness (b paths) partialing out the effect of health (and correcting for control variables). The total effect of health on loneliness is significant (c path), as is the direct effect (c 1) although the strength of the association is weaker, suggesting that health is partially mediated, and has an indirect effect on loneliness through the mediating variables.
Figure 4.
Statistical mediation model for health, mediators, controls, and loneliness. **p < .01, ***p < .001.
By examining the 95% BCa CIs, health has a significant indirect effect on loneliness through the mediating variables social resources and social participation (Table 3). Although a greater number of chronic conditions has a negative effect on the mediators (poor health decreases social participation and social resources), greater levels of social participation and social resources decrease levels of loneliness. Thus, each of the mediating variables decreases the effect of health on loneliness, weakening (rather than attenuating) the direct relationship between health and loneliness.
Table 3.
Mediation of the Effect of Health on Loneliness Through Social Resources and Social Participation
| Bootstrapping | ||||
|---|---|---|---|---|
| Estimate | Standard error | BCa 95% CI | ||
| Lower | Upper | |||
| Social resources | 0.013 | 0.004 | 0.007 | 0.019 |
| Social participation | 0.006 | 0.001 | 0.003 | 0.009 |
| Total | 0.019 | 0.004 | 0.012 | 0.026 |
| Social resources versus social participation | 0.007 | 0.003 | 0.001 | 0.014 |
Note. BCa, bias corrected and accelerated, 5,000 bootstrap samples.
Moderated-Mediation Model
Turning to the moderators’ impact on the mediation model, the path between health (chronic conditions) and social participation and between health and social resources is significant (Figure 5). As in the mediation model, poor health predicted lower participation in social activities and lower levels of social resources.
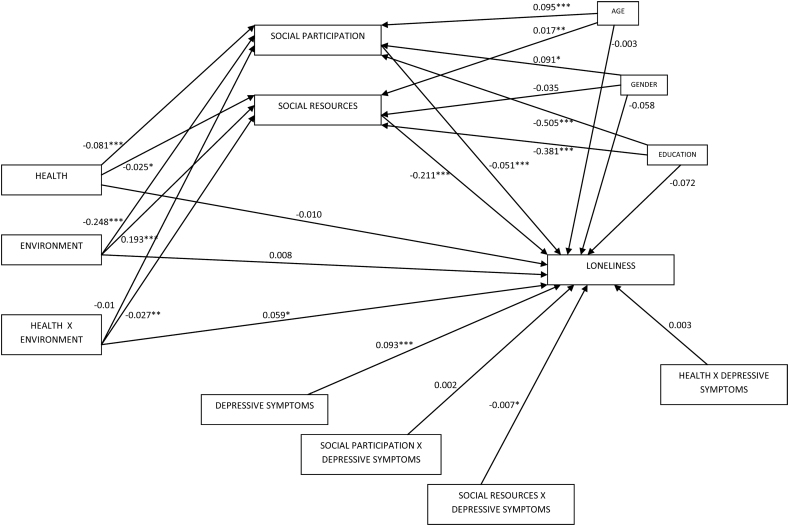
Figure 5.
Statistical moderated-mediation model for health, moderators, mediators, controls, and loneliness. *p < .05, **p < .01, ***p < .001.
Environment has significant relationships with both mediators: in rural areas, while social participation is lower, social resources are greater. This reflects reduced access to mainstream leisure facilities (such as theaters, adult education, restaurants, and sport centers), which are more usually located in urban areas. Furthermore, the association between environment and social resources points to stronger kinships and friendship ties in rural than urban areas. Although location is significantly associated with social participation, the interaction between health and location is not, suggesting that rurality does not exacerbate the link between poor health and social participation. However, the interaction between health and location does have a significant negative effect on social resources. This suggests that location amplifies the association between poor health and social resources: poor health has a greater negative impact on levels of social resources in rural areas compared with urban areas. A significant effect on loneliness was also observed with regard to the interaction between health and location via the direct or c path.
Considering the model’s b paths, as demonstrated in the mediation model, social participation and social resources have a significant impact on loneliness with greater levels of participation and social resources decreasing loneliness. Depressive symptoms also have a significant impact on loneliness, whereby greater levels of depressive symptoms increase levels of loneliness. With regard to the moderating effect of depressive symptoms, although depressive symptoms do not moderate the pathway between social participation and loneliness, they do moderate the effect of social resources on loneliness. In this respect, a greater number of depressive symptoms weakens the association between social resources and loneliness. The independent variable, health, is also moderated by depressive symptoms.
Finally, the pathway between health and loneliness (c 1) is not significant. This suggests that the effect of health on loneliness is accounted for entirely through the moderated-mediation pathways.
Conclusions
The findings suggest that our hypotheses are partially supported, lending further credence to the relevance of cognitive processes in discrepancy theory (Perlman & Peplau, 1998). Starting from a theoretical understanding of loneliness that has its roots in psychology, we have applied a human ecology lens and have demonstrated empirically that there are distinct pathways from poor health to loneliness in rural areas. The statistical models increase our understanding of the processes that lead to the experience of loneliness and suggest that it is insufficient to consider loneliness as an outcome of interactions between individual-level characteristics. This article extends discrepancy theory by incorporating contextual characteristics of an individual’s environment (de Jong Gierveld et al., 2006) and showing how loneliness is the product of complex interactions and is dynamically shaped by several interacting systems. Our mediation analysis has demonstrated that loneliness is influenced by (but not entirely dependent on) the microsystem through an individual’s health status, the mesosystem through social resources, the exosystem, and the availability of leisure facilities for older people to participate socially in rural areas (expressed through levels of social participation). The moderated-mediation analysis demonstrates that loneliness is also a product of the interaction between the exosystem (characteristics of rural environments) and microsystem (individual levels of depression).
Returning to the discrepancy model, we have shown, first, that increasing numbers of chronic conditions (comorbidity) can be considered as a precipitating event, which leads to a decrease in achieved levels of social interaction. In our model, comorbidity decreases social resources and social participation. Second, the environment also affects achieved levels of social relations; specifically, rural environments amplify difficulties associated with chronic conditions in accessing social resources. However, the environment does not moderate the relationship between poor health and social participation: it is difficult for older people in poor health to participate in social activities (regardless of location) and difficult for older people in rural areas to participate (regardless of health). Third, depressive symptoms had a moderating influence on two paths in the model: depressive symptoms amplified the direct effect of health on loneliness and also the indirect impact of health on loneliness through the social resource mediator. The influences of rural areas and depressive symptoms on the experience of loneliness are discussed in turn.
Approximately 42% of the population aged 65 years or older in Ireland lives in rural areas (Connolly et al., 2012). Thus, the spatial distribution of Ireland’s older population has more similarities with economically less-developed countries in Asia and Africa than with other economically developed countries in Europe or North America. Despite a greater proportion of people living in rural areas, the characteristics of Ireland’s rural areas bear similarities with those elsewhere. For example, some rural areas are characterized by in-migration of older people and out-migration of younger people, and these population changes result in the demographic ageing of rural populations.
Authors have hypothesized that loneliness of older people in rural areas (of Finland and Turkey) may be linked to out-migration of younger people (Hazer & Boylu, 2010; Savikko et al., 2005). However, this supposition has only been backed up with empirical evidence from rural areas of Albania and China (Du, Ding, Li, & Gui, 2004; Vullnetari & King, 2008), where expectations for familial contact may be culturally specific. Elsewhere, in the United Kingdom, Germany, and New Zealand, research has highlighted the resilience of many rural families who retain emotional intimacy at distance (e.g., Keeling, 2001; Scharf, 2001; Wenger & Burholt, 2001). This suggests that in countries where nuclear households are the norm, the accessibility and availability of friends or confidants may be more important constituents of social resources than proximate family members in protecting against loneliness.
Although some rural areas are characterized by migration, others are typified by residential stability. A recent U.K. study has shown that social resources mediate the relationship between length of residence and social attachment to place in rural areas (the strength of belonging that a person feels to their community based on social interaction, engagement, and community participation; Burholt, Curry, Keating, & Eales, 2014). Thus, the residential history of an older rural dweller—their migration or residential stability—may in turn influence their levels of social resources and social attachment to place and subsequently affect later life loneliness.
Overall, we cannot assume that the moderating influence of rurality outlined in the discrepancy model of loneliness is due to migration or residential stability: both are apparent in rural areas but may have converse effects on social resources. However, there are other less mutable rural influences that we can draw on that may explain this effect. In this respect, we highlight the primacy of transportation to access facilities for social participation and to connect older people to their social networks in rural areas. In Ireland (McDonagh, 2006), United States (Kerschner, 2006), Australasia (Davey, 2007), and Europe (Tacken & van Lemoen, 2005), poor rural public transport renders older people dependent on private means of transport. Responding to poor health, older people often quit driving and subsequently rely on others to provide transport. In these instances, discretionary trips (for pleasure such as social engagements) are often sacrificed and requests for help limited to essential trips in order to reduce imposition on others (Davey, 2007). Transport policy, advances in intelligent transport systems, and universal design have the potential to reduce the experience of loneliness in rural areas. For example, changes in the design of public transport and improved timetabling may facilitate social engagement for older people in ill health or with disabilities. Moreover, advanced technological changes to private transport may facilitate safer driving later in life than has hitherto been possible (Metz, 2003).
Although the environmental context influences social resources, further along the pathway to the experience of loneliness as proposed in cognitive discrepancy theory, we have examined depressive symptoms in relation to their influence on cognitive processes. Rather than describing depression as an outcome of loneliness (Cacioppo et al., 2006), the cognitive discrepancy theory contends that loneliness is not a direct response to external circumstances, such as the level of social contact, but represents the subjective assessment of the social situation. In this respect, our statistical model suggests that depressive symptoms interfere with judgments about the adequacy of social interaction and have an indirect moderating effect on loneliness. The findings suggest that depression is a “cognitive process” that moderates how intensely people react to their personal levels of social contact and support, and their functional ability to participate fully in society. Adjusting one’s expectations regarding quantity and quality of social contact—desired social relations—in light of one’s physical ability to maintain social ties is more difficult to achieve for those with depression.
The cognitive discrepancy model presented here suggests that increasing social interaction with others may not combat feelings of loneliness for older people in poor physical and mental health. Instead, older people with depressive symptoms may need to make psychological adjustments concerning desired level of social relations by changing patterns of thinking and patterns of behavior. For example, cognitive behavioral therapy can help the older person to examine other real-life experiences—the social relationships of other older people in poor health—to identify with situations similar to their own (e.g., Blazer, 2003). In the light of a more realistic perspective, loneliness may decrease as actual and desired levels of social relations converge.
Increasing social contact is often considered the “cure” for loneliness (Rokach, Orzeck, & Neto, 2004). Although interventions that increase social contact may be valuable for people with few friends or family or those who have experienced social network shrinkage, this approach does not consider other elements that contribute to an older person’s experience of loneliness. Considering that age, gender, education, health, environment, and depressive symptoms all play a significant part in the pathway to loneliness, the challenge is to tackle these predisposing factors, precipitating events, environmental factors, and cognitive processes. Responding to these issues may facilitate an increase in social relations by removing barriers to participation or by changing ways of thinking about participation and social relations, and ultimately the impact on feelings of loneliness for older people.
There are several limitations to the research reported here. As the research has been conducted in Ireland, the model should be tested with data from other countries to ascertain its applicability in other cultural contexts. Moreover, our analysis is limited by its focus on a simple distinction between rural and urban environments. Future analyses might test the model within rural and urban settings to provide a more differentiated understanding of environmental influences. The mediation and moderated-mediation models provide only two examples of pathways to loneliness, and other models may fit the data better. For example, our model is a partial representation of cognitive discrepancy theory as it focuses on the influence of the environment and cognitive processes on loneliness and does not include a measure of expectations for social interaction. Furthermore, we could have chosen to explore depression as an outcome variable and loneliness as a mediator. Although the nature of the bidirectional relationship between loneliness and depression is important, in order to develop effective interventions, the theorizing behind the relationship needs to be explicit. Understanding the link between the individual, their environment, social behavior, and cognitive processes offers the advantage of a “generalizable framework” and may inform the delivery and development of intervention strategies (Improved Clinical Effectiveness through Behavioural Research Group & Frances, 2006). In order to understand the dynamic interplay between the role of environment and cognitive process in discrepancy theory, we have examined empirical data from Ireland. Our model is limited because of the (currently) cross-sectional nature of TILDA data. We therefore cannot be sure of the direction of causality. However, the model is supported by other research that suggests loneliness may be the consequence of poor mental health (Bowling, Edelmann, Leaver, & Hoekel, 1989; Tiikkainen & Heikkinen, 2005). Furthermore, although loneliness is related to the perceived adequacy of social relationships, alternative pathways to depression exist (e.g., Reynolds, Alexopoulos, & Katz, 2002). Finally, TILDA is a longitudinal study, and future waves of data will provide opportunities to test these causal pathways with greater conviction.
Acknowledgment
This paper has drawn on data from The Irish Longitudinal Study of Ageing (TILDA), which was conducted with the financial support from Irish Life, the Atlantic Philanthropies, and the Department of Health and Children, Republic of Ireland. The authors wish to acknowledge the work of the TILDA research team including the Project Director, Professor Alan Barrett, lead Principal Investigator Professor Rose Anne Kenny, and the collaborators from higher educational establishments in Ireland, in particular the lead institution Trinity College Dublin. The authors also extend thanks to the research participants. The lead author is grateful to colleagues at the Irish Centre for Social Gerontology, National University of Ireland Galway, for hosting a visiting fellowship in 2011/2012 during which time this paper was drafted. V. Burholt performed all statistical analyses and wrote the first draft of the paper. T. Scharf contributed to the conceptualization of the model and revised and contributed to the development of the full paper.
References
- Alpass F. M., Neville S. (2003). Loneliness, health and depression in older males. Aging & Mental Health, 7, 212–216. 10.1080/1360786031000101193 [DOI] [PubMed] [Google Scholar]
- Barg F. K., Huss-Ashmore R., Wittink M. N., Murray G. F., Bogner H. R., Gallo J. J. (2006). A mixed-methods approach to understanding loneliness and depression in older adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 61, S329–S339. 10.1093/geronb/61.6.S329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett A., Savva G., Timonen V., Kenny R. A. (Eds.) (2011). Fifty plus in Ireland 2011: First results from the Irish Longitudinal Study on Ageing (TILDA). Dublin: Trinity College Dublin [Google Scholar]
- Beck A. T. (1972). Depression: Causes and treatment. Philadelphia: University of Pennsylvania Press [Google Scholar]
- Berkman L. F. (1977). Social networks, host resistance, and mortality: A follow-up study of Alameda County residents (Doctoral dissertation). University of California, Berkeley [Google Scholar]
- Blazer D. G. (2003). Depression in late life: Review and commentary. Journals of Gerontology: Medical Sciences, 58A, M249–M265. 10.1093/Gerona/58.3.M249 [DOI] [PubMed] [Google Scholar]
- Borys S., Perlman D. (1985). Gender differences in loneliness. Personality and Social Psychology Bulletin, 11, 63–76. 10.1177/0146167285111006 [Google Scholar]
- Bowling A., Edelmann R., Leaver J., Hoekel T. (1989). Loneliness, mobility, well-being and social support in a sample of over 85 years’ olds. Journal of Personality and Individual Differences, 10, 1189–1192. 10.1177/0146167285111006 [Google Scholar]
- Burholt V. (2011). Loneliness of older men and women in rural areas of the UK. In Safeguarding the convoy (pp. 35–29). Oxford: Age UK Oxfordshire [Google Scholar]
- Burholt V., Curry N., Keating N., Eales J. (2014). Connecting with community: The nature of belonging among rural elders. In Hennessey C. H., Means R., Burholt V. (Eds), Countryside connections: Older people, community and place in rural Britain. Bristol, UK: Policy Press [Google Scholar]
- Burholt V., Dobbs C. (2012). Research on rural ageing: Where have we got to and where are we going? Journal of Rural Studies, 28, 432–446. 10.1016/j.jrurstud.2012.01.009 [Google Scholar]
- Cacioppo J. T., Hughes M. E., Waite L. J., Hawkley L. C., Thisted R. A. (2006). Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychology and Aging, 21, 140–151. 10.1037/0882-7974.21.1.140 [DOI] [PubMed] [Google Scholar]
- Cohen G. (1990). Psychopathology and mental health in the mature and elderly adult. In Birren J. E., Schaie K. W. (Eds.), Handbook of the psychology of aging (3rd ed., pp. 359–371). San Diego: Academic Press [Google Scholar]
- Connolly S., Finn C., O’Shea E. (2012). Rural ageing in Ireland: Key trends and issues. Galway: Irish Centre for Social Gerontology [Google Scholar]
- Creecy R., Berg W., Wright R. (1985). Loneliness among the elderly: A causal approach. Journal of Gerontology, 40, 487–493. 10.1093/geronj/40.4.487 [DOI] [PubMed] [Google Scholar]
- Crimmins E. M., Kim J. K., Solé-Auró A. (2010). Gender differences in health: Results from SHARE, ELSA and HRS. European Journal of Public Health, 21, 81–91. 10.1093/eurpub/ckq022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davey J. A. (2007). Older people and transport: Coping without a car. Ageing and Society, 27, 49–65. 10.1017/S0144686X06005332 [Google Scholar]
- de Jong-Gierveld J. (1987). Developing and testing a model of loneliness. Journal of Personality and Social Psychology, 53, 119–128. 10.1037//0022-3514.53.1.119 [DOI] [PubMed] [Google Scholar]
- de Jong Gierveld J., Tesch-Romer C. (2012). Loneliness in old age in Eastern and Western European societies: Theoretical perspectives. European Journal of Ageing, 9, 285–295. 10.1007/s10433-012-0248-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jong Gierveld J., van Tilburg T., Dykstra P. A. (2006). Loneliness and social isolation. In Vangelisti A., Perlman D. (Eds.), Cambridge handbook of personal relationships (pp. 485–500). Cambridge: Cambridge University Press [Google Scholar]
- Drennan J., Treacy M., Butler M., Byrne A., Fealy G., Frazer K., Irving K. (2008). The experience of social and emotional loneliness among older people in Ireland. Ageing and Society, 28, 1113–1132. 10.1017/S0144686X08007526 [Google Scholar]
- Du P., Ding Z., Li Q., Gui J. (2004). The impact of out labor migration on the elderly stayers in rural areas. Population Research, 28, 44–52 [Google Scholar]
- Dykstra P. A., Fokkema T. (2007). Social and emotional loneliness among divorced and married men and women: Comparing the deficit and cognitive perspectives. Basic and Applied Social Psychology, 29, 1–12. 10.1080/01973530701330843 [Google Scholar]
- Essex M. J., Nam S. (1987). Marital status and loneliness among older women: The differential importance of close family and friends. Journal of Marriage and Family, 49, 93–106. 10.2307/352674 [Google Scholar]
- Fees B. S., Martin P., Poon L. W. (1999). A model of loneliness in older adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 54, 231–239. 10.1093/geronb/54B.4.P231 [DOI] [PubMed] [Google Scholar]
- Gonca S., Savasir I. (2001). The relationship between interpersonal schemas and depressive symptomatology. Journal of Counseling Psychology, 48, 359–364. 10.1037/0022-0167.48.3.359 [Google Scholar]
- Hawkley L. C., Hughes M. E., Waite L. J., Masi C. M., Thisted R. A., Cacioppo J. T. (2008). From social structural factors to perceptions of relationship quality and loneliness: The Chicago Health, Aging, and Social Relations Study. Journal of Gerontology: Social Sciences, 63B, S375–S384. 10.1093/geronb/63.6.S375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley L. C., Masi C. M., Berry J. D., Cacioppo J. T. (2006). Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychology and Aging, 21, 152–164. 10.1037/0882-7974.21.1.152 [DOI] [PubMed] [Google Scholar]
- Hayes A. F. (2012a). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling (White paper). Retrieved from http://www.afhayes.com/public/process2012.pdf
- Hayes A. F, (2012b). PROCESS [SPSS syntax]. Retrieved from http://www.afhayes.com/public/process.pdf
- Hazer O., Boylu A. A. (2010). The examination of the factors affecting the feeling of loneliness of the elderly. Procedia Social and Behavioral Sciences, 9, 2083–2089. 10.1016/j.sbspro.2010.12.450 [Google Scholar]
- Heikkinen R-L., Kauppinen M. (2004). Depressive symptoms in late life: A 10-year follow-up. Archives of Gerontology & Geriatrics, 38, 239–250. 10.1016/j.archger.2003.10.004 [DOI] [PubMed] [Google Scholar]
- Hughes M. E., Waite L. J., Hawkley L. C., Cacioppo J. T. (2004). A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging, 26, 655–672. 10.1177/0164027504268574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Improved Clinical Effectiveness through Behavioural Research Group, & Frances J. (2006). Designing theoretically-informed implementation interventions. Implementation Science, 1, 4. 10.1186/1748-5908-1-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jylhä M. (2004). Old age and loneliness: Cross-sectional and longitudinal analyses in the Tampere Longitudinal Study on Aging. Canadian Journal on Aging, 23, 157–168. 10.1353/cja.2004.0023 [DOI] [PubMed] [Google Scholar]
- Kearney P. M., Cronin H., O’Regan C., Kamiya Y., Savva G. M., Whelan B., Kenny R. (2011). Cohort profile: The Irish Longitudinal Study on Ageing. International Journal of Epidemiology, 40, 877–884. 10.1093/ije/dyr116 [DOI] [PubMed] [Google Scholar]
- Keeling S. (2001). Relative distance: Ageing in rural New Zealand. Ageing and Society, 21, 605–619. 10.1017/S0144686X01008443 [Google Scholar]
- Kerschner H. (2006). Transportation and aging: Challenges in rural America. In Goins R. T., Krout J. (Eds.), Service delivery to rural older adults: Research, policy, and practice (pp. 183–197). New York: Springer Publishing Company [Google Scholar]
- Koropeckyj-Cox T. (1998). Loneliness and depression in middle and old age: Are the childless more vulnerable? Journal of Gerontology: Social Sciences, 53B, S303–S312. 10.1093/geronb/53B.6.S303 [DOI] [PubMed] [Google Scholar]
- Leiderman P. H. (1969). Loneliness: A psychodynamic interpretation. International Psychiatry Clinics, 6, 155–174 [PubMed] [Google Scholar]
- Loucks E., Sullivan L., D’Agostino R., Larson M., Berkman L., Benjamin E. (2006). Social networks and inflammatory markers in the Framingham Heart Study. Journal of Biosocial Science, 38, 835–842. 10.1017/S0021932005001203 [DOI] [PubMed] [Google Scholar]
- Luanaigh C. O., Lawlor B. A. (2008). Loneliness and the health of older people. International Journal of Geriatric Psychiatry, 23, 1213–1221. 10.1002/gps.2695 [DOI] [PubMed] [Google Scholar]
- McDonagh J. (2006). Transport policy instruments and transport-related social exclusion in rural Republic of Ireland. Journal of Transport Geography, 14, 355–366. 10.1016/j.jtrangeo.2005.06.005 [Google Scholar]
- Metz D. (2003). Transport policy for an ageing population. Transport Reviews, 23, 375–386. 10.1080/0144164032000048573 [Google Scholar]
- Muller D., Judd C. M., Yzerbyt V. Y. (2005). When moderation is mediated and mediation is moderated. Journal of Personality and Social Psychology, 89, 852–863. 10.1037/0022-3514.89.6.852 [DOI] [PubMed] [Google Scholar]
- Osborn D. P., Fletcher A. E., Smeeth L., Stirling S., Bulpitt C. J., Breeze E. … Tulloch A. (2003). Factors associated with depression in a representative sample of 14,217 people aged 75 and over in the United Kingdom: Results from the MRC trial of assessment and management of older people in the community. International Journal of Geriatric Psychiatry, 18, 623–630. 10.1002/gps.896 [DOI] [PubMed] [Google Scholar]
- Paúl C., Fonseca A. M., Martín I., Amado J. (2003). Psychosocial profile of rural and urban elders in Portugal. European Psychologist, 8, 160–167. 10.1027//1016-9040.8.3.160 [Google Scholar]
- Peplau L. A., Caldwell M. (1978). Loneliness: A cognitive analysis. Essence, 2, 207–220 [Google Scholar]
- Perlman D. (1991). Age differences in loneliness: A metaanalysis. Vancouver, BC: University of British Columbia [Google Scholar]
- Perlman D. (2004). European and Canadian studies of loneliness among seniors. Canadian Journal on Aging, 23, 181–188. 10.1353/cja.2004.0025 [DOI] [PubMed] [Google Scholar]
- Perlman D., Gerson A. C., Spinner B. (1978). Loneliness among senior citizens: An empirical report. Essence, 2, 239–248 [Google Scholar]
- Perlman D., Peplau L. A. (1981). Toward a social psychology of loneliness. In Duck S. W., Gilmour R. (Eds.), Personal relationships in disorder (pp. 31–56). London: Academic Press [Google Scholar]
- Perlman D., Peplau L. A. (1984). Loneliness research: A survey of empirical findings. In Peplau L. A., Goldston S. (Eds.), Preventing the harmful consequences of severe and persistent loneliness (pp. 13–46). Washington, DC: U.S. Government Printing Office [Google Scholar]
- Perlman D., Peplau L. A. (1998). Loneliness. In Friedman H. (Ed.), Encyclopedia of mental health (Vol. 2, pp. 571–581). San Diego, CA: Academic Press [Google Scholar]
- Pitkala K. H., Routasalo P. (2003). Loneliness among older people. Reviews in Clinical Gerontology, 13, 303–311. 10.1017/S095925980400111X [Google Scholar]
- Poon L. W., Clayton G. M., Martin P., Johnson M. A., Courtenay B. C., Sweaney A. L. … Thielman S. B. (1992). The Georgia Centenarian Study. International Journal of Aging & Human Development, 34, 1–17. 10.2190/8M7H-CJL7-6K5T-UMFV [DOI] [PubMed] [Google Scholar]
- Preacher K. J., Hayes A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. 10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- Radloff L. S. (1977). The CES–D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. 10.1177/014662167700100306 [Google Scholar]
- Reynolds C. F., Alexopoulos G. S., Katz I. R. (2002). Geriatric depression: Diagnosis and treatment. Generations, 26, 28–31 [Google Scholar]
- Rokach A., Orzeck T., Neto F. (2004). Coping with loneliness in old age: A cross-cultural comparison. Current Psychology, Developmental, Learning, Personality, Social, 23, 124–137. 10.1007/BF02903073 [Google Scholar]
- Russell D. W. (1996). UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of Personality Assessment, 66, 20–40. 10.1207/s15327752jpa6601_2 [DOI] [PubMed] [Google Scholar]
- Savikko N., Routasalo P., Tilvis R. S., Strandberg T. E. (2005). Predictors and subjective causes of loneliness in an aged population. Archives of Gerontology and Geriatrics, 41, 223–233. 10.1016/j.archger.2005.03.002 [DOI] [PubMed] [Google Scholar]
- Savva G. (2011). Methodology. In Barrett A., Savva G., Timonen V., Kenny R. A. (Eds.), Fifty plus in Ireland 2011: First results from the Irish Longitudinal Study on Ageing (TILDA) (pp. 293–303). Dublin: Trinity College Dublin [Google Scholar]
- Scharf T. (2001). Ageing and intergenerational relationships in rural Germany. Ageing and Society, 21, 547–566. 10.1017/S0144686X01008388 [Google Scholar]
- Scharf T., de Jong Gierveld J. (2008). Loneliness in urban neighbourhoods: An Anglo-Dutch comparison. European Journal of Ageing, 5, 103–115. 10.1007/s10433-008-0080-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scharf T., Phillipson C., Smith A. E. (2004). Poverty and social exclusion—Growing older in deprived urban neighbourhoods. In Walker A., Hagan Hennessy C. (Eds.), Growing older—Quality of life in old age (pp. 81–106). Maidenhead: Open University Press [Google Scholar]
- Slivinske L. R., Fitch V. L., Morawski D. P. (1996). The wellness index: Developing an instrument to assess elders’ well-being. Journal of Gerontological Social Work, 25, 185–204. 10.1300/J083V25N03_12 [Google Scholar]
- Tacken M., van Lemoen E. (2005). Transport behaviour and realised journeys and trips. In Mollenkopf H., Marcellini F., Ruopilla I., Széman Z., Tacken M. (Eds.), Enhancing mobility in later life: Personal coping, environmental resources and technical support, the out-of-home mobility of older adults in urban and rural regions of five European countries. Amsterdam: IOS Press [Google Scholar]
- Theeke L. (2009). Predictors of loneliness in U.S. adults over age sixty-five. Archives of Psychiatric Nursing, 23, 387–396. 10.1016/j.apnu.2008.11.002 [DOI] [PubMed] [Google Scholar]
- Tiikkainen P., Heikkinen R. L. (2005). Associations between loneliness, depressive symptoms and perceived togetherness in older people. Aging & Mental Health, 9, 526–534. 10.1080/13607860500193138 [DOI] [PubMed] [Google Scholar]
- van Tilburg T., Havens B., de Jong Gierveld J. (2004). Loneliness among older adults in The Netherlands, Italy, and Canada: A multifaceted comparison. Canadian Journal on Aging, 23, 169–180. 10.1353/cja.2004.0026 [DOI] [PubMed] [Google Scholar]
- Victor C. R., Scambler S., Bowling A., Bond J. (2005). The prevalence of, and risk factors for, loneliness in later life: A survey of older people in Great Britain. Ageing and Society, 25, 357–375. 10.1017/S0144686X04003332 [Google Scholar]
- Victor C. R., Scambler S. J., Bond J., Bowling A. (2000). Being alone in later life: Loneliness, isolation and living alone in later life. Reviews in Clinical Gerontology, 10, 407–417. 10.1017/S0959259800104101 [Google Scholar]
- Vullnetari J., King R. (2008). ‘Does your granny eat grass?’ On mass migration, care drain and the fate of older people in rural Albania. Global Networks, 8, 139–171. 10.1111/j.1471-0374.2008.00189.x [Google Scholar]
- Wenger G. C., Burholt V. (2001). Differences over time in older people’s relationships with children, grandchildren, nieces and nephews in rural North Wales. Ageing & Society, 21, 567–590. 10.1017/S0144686X01008406 [Google Scholar]
- Wenger G. C., Burholt V. (2004). Changes in levels of social isolation and loneliness among older people in rural Wales - A 20-year longitudinal study. Canadian Journal on Aging, 23, 477–493. 10.1353/cja.2004.0028 [DOI] [PubMed] [Google Scholar]
- Wenger G. C., Davies R., Shahtahmasebi S., Scott A. (1996). Social isolation and loneliness in old age: Review and model refinement. Ageing and Society, 16, 333–358. 10.1017/S0144686X00003457 [Google Scholar]
- Yang K., Victor C. R. (2008). The prevalence of and risk factors for loneliness among older people in China. Ageing and Society, 28, 305–327. 10.1017/S0144686X07006848 [Google Scholar]