Abstract
BACKGROUND
Among patients in the United States with chronic kidney disease, black patients are at increased risk for end-stage renal disease, as compared with white patients.
METHODS
In two studies, we examined the effects of variants in the gene encoding apolipoprotein L1 (APOL1) on the progression of chronic kidney disease. In the African American Study of Kidney Disease and Hypertension (AASK), we evaluated 693 black patients with chronic kidney disease attributed to hypertension. In the Chronic Renal Insufficiency Cohort (CRIC) study, we evaluated 2955 white patients and black patients with chronic kidney disease (46% of whom had diabetes) according to whether they had 2 copies of high-risk APOL1 variants (APOL1 high-risk group) or 0 or 1 copy (APOL1 low-risk group). In the AASK study, the primary outcome was a composite of end-stage renal disease or a doubling of the serum creatinine level. In the CRIC study, the primary outcomes were the slope in the estimated glomerular filtration rate (eGFR) and the composite of end-stage renal disease or a reduction of 50% in the eGFR from baseline.
RESULTS
In the AASK study, the primary outcome occurred in 58.1% of the patients in the APOL1 high-risk group and in 36.6% of those in the APOL1 low-risk group (hazard ratio in the high-risk group, 1.88; P<0.001). There was no interaction between APOL1 status and trial interventions or the presence of baseline proteinuria. In the CRIC study, black patients in the APOL1 high-risk group had a more rapid decline in the eGFR and a higher risk of the composite renal outcome than did white patients, among those with diabetes and those without diabetes (P<0.001 for all comparisons).
CONCLUSIONS
Renal risk variants in APOL1 were associated with the higher rates of end-stage renal disease and progression of chronic kidney disease that were observed in black patients as compared with white patients, regardless of diabetes status. (Funded by the National Institute of Diabetes and Digestive and Kidney Diseases and others.)
In the United States, black patients have approximately twice the risk of end-stage renal disease observed among white patients, after accounting for differences in socioeconomic and clinical risk factors.1–4 This increased risk occurs despite a similar prevalence in earlier stages of chronic kidney disease5–8 in the two racial groups, which suggests that kidney function declines more rapidly after the onset of chronic kidney disease in black patients. However, there is little direct evidence in support of this hypothesis.9–13 The identification of factors that mediate differences in the progression of chronic kidney disease between black patients and white patients, as well as among black patients, is necessary to reduce the excess burden of end-stage renal disease and its complications in black patients.
In previous studies, a region on chromosome 22 containing the genes encoding nonmuscle myosin heavy chain 9 (MYH9) and apolipoprotein L1 (APOL1) has been implicated in the increased risk among black patients of human immunodeficiency virus nephropathy,14,15 focal segmental glomerulosclerosis,14,15 chronic kidney disease attributed to hypertension,16 and end-stage renal disease not related to diabetes.14,15,17 Recent data suggest that this risk is strongly associated with two common variants (G1 and G2) in the last exon of APOL116–18 that confer resistance to lethal Trypanosoma brucei infections. The G1 and G2 variants are common in populations of recent African descent but are very rare or absent in most other populations. These variants are believed to account for much of the disparity in rates of end-stage renal disease between black patients and white patients.19,20 However, evidence linking APOL1 to end-stage renal disease associated with diabetes is equivocal.21,22
We examined the effects of APOL1 risk variants on the progression of chronic kidney disease separately in the African American Study of Kidney Disease and Hypertension (AASK) and the Chronic Renal Insufficiency Cohort (CRIC) study. In AASK, which enrolled black patients with chronic kidney disease attributed to hypertension who did not have diabetes, we studied the effects of APOL1 risk variants on progression and the interactive effects of these variants with baseline proteinuria and the blood-pressure goal and anti-hypertensive-drug interventions in the trial. In the CRIC study, which enrolled both black patients and white patients with chronic kidney disease, approximately half of whom had diabetes, we compared disease progression in white patients with that in black patients (both those with and those without APOL1 high-risk variants), stratified on the basis of diabetes status.
METHODS
STUDY DESIGN AND OVERSIGHT
In each study, the institutional review board at each study center approved the study protocol. All patients provided written informed consent. The design and methods of both studies have been described previously.23–28 The Supplementary Appendix, available with the full text of this article at NEJM.org, provides additional details.
AASK
Study Population
Patients in AASK were self-identified as black and had chronic kidney disease attributed to hypertension. The inclusion and exclusion criteria are listed in the Supplementary Appendix.
Design and Data Collection
The study had a trial phase that extended from 1995 through 2001; this phase was followed by a cohort phase from 2002 through 2007. Initially, 1094 patients were randomly assigned to receive either intensive blood-pressure control (goal of mean arterial pressure, ≤92 mm Hg) or standard control (goal of mean arterial pressure, 102 to 107 mm Hg). Patients were also randomly assigned to receive one of three initial therapies: ramipril, an angiotensin-converting–enzyme (ACE) inhibitor; metoprolol, a sustained-release beta-blocker; or amlodipine, a dihydropyridine calcium-channel blocker. In April 2002, patients who had not received a diagnosis of end-stage renal disease were invited to enroll in the cohort study, in which they received protocol-driven blood-pressure treatment. During the trial phase, 836 patients provided written informed consent for collection of DNA; 693 had adequate genotyping data and were included in this study (Table S1 in the Supplementary Appendix).
Genotyping
Seven single-nucleotide polymorphisms (SNPs) in APOL1 and MYH9 (rs73885319, rs60910145, rs71785313, rs4821480, rs2032487, rs4821481, and rs3752462) and 140 ancestry-informative markers were typed (see the Supplementary Appendix).
Outcomes
The primary outcome was a composite renal outcome, which was defined as a doubling of the serum creatinine level (roughly equivalent to a reduction of 50% in the glomerular filtration rate [GFR]) from baseline or incident end-stage renal disease. The serum creatinine level was measured twice at baseline and every 6 months thereafter. In analyses of the interaction between APOL1 variants and trial interventions, the composite outcome was a reduction of 50% in the GFR (as measured by iothalamate clearance) or incident end-stage renal disease.
Statistical Analysis
The primary exposure variable was APOL1 risk status. The G1 risk allele was defined by the presence of rs73885319 (S342G) and rs60910145 (I384M), which are nearly perfectly correlated, and the G2 risk allele by the presence of rs71785313. APOL1 risk was defined according to the number of copies of the risk alleles (0, 1, or 2 copies). We assessed the association between APOL1 and outcome using Cox proportional-hazards models, adjusted for age, sex, percentage of European ancestry, and baseline GFR. We present both a co-dominant genetic model and a recessive genetic model for APOL1. After verifying that the risk in patients with 1 copy of the risk variants was similar to the risk in the reference group with 0 copies (a finding consistent with that in previous studies17,19), we used a recessive genetic model and compared patients with 2 copies of the risk variants (called the APOL1 high-risk group) with all other patients (APOL1 low-risk group). The evaluation of interactions between genetic factors and trial interventions were limited to the trial phase.
CRIC STUDY
Study Population
From June 2003 through August 2008, a total of 3288 black patients and white patients with an estimated GFR (eGFR) of 20 to 70 ml per minute per 1.73 m2 of body-surface area were enrolled in the CRIC study. Patients were recruited from primary care and nephrology practices (see the Supplementary Appendix for inclusion and exclusion criteria). Analyses were restricted to 2955 black patients and white patients with adequate DNA samples and genotyping.
Design and Data Collection
Demographic characteristics, self-reported medical history, anthropometric measures, and medication use were ascertained at baseline.25 The serum creatinine level was measured at baseline and annually. The GFR was estimated by means of an equation developed with the use of the iothalamate GFR in a subgroup of 1433 CRIC study participants.29 Total proteinuria was measured from 24-hour urine collections. Patients were considered to have diabetes if they had a fasting glucose level of 126 mg per deciliter (7.0 mmol per liter) or higher or a nonfasting glucose level of 200 mg per deciliter (11.1 mmol per liter) or higher or if they used insulin or an oral hypoglycemic agent.
Genotyping
Ancestry-informative markers were genotyped in all patients, and APOL1 G1 and G2 and MYH9 haplotype-tagging SNPs18,30,31 were genotyped only in black patients. For details of the genotyping, see the Supplementary Appendix.
Outcomes
The primary outcomes were the rate of decline in kidney function (slope of the eGFR over time) and the composite of end-stage renal disease or a decline in the eGFR of at least 50% from baseline. We imputed the time until a reduction of 50% in the eGFR, assuming a linear decline in kidney function between in-person annual follow-up visits and the onset of end-stage renal disease.
Statistical Analysis
The primary exposure variables were genotype-derived African or European racial ancestry (black or white) and APOL1 risk status among the black patients. We used mixed-effects models and Cox proportional-hazards models to adjust for covariates and to estimate the associations between exposure variables and outcomes. We performed four separate analyses: a comparison between all white patients and all black patients, a comparison between all white patients and all black patients with APOL1 high-risk variants, a comparison between all white patients and black patients with APOL1 low-risk variants, and a comparison between black patients with APOL1 high-risk variants and black patients with APOL1 low-risk variants. In the time-to-event analysis, data were censored at the time of death, withdrawal from the study, or the last study visit or as of March 31, 2011 (administrative censoring).
For each outcome, we constructed a set of hierarchical models retaining all covariates from each previous model. Model 1 is the base model with adjustment for age, sex, clinical site, and baseline eGFR. Model 2 added socioeconomic variables (education level, treatment by a nephrologist, and use of either an ACE inhibitor or angiotensin-receptor blocker [as a proxy for treatment access]). Model 3 added clinical risk factors (systolic blood pressure, body-mass index, glycated hemoglobin level, and smoking status). Model 4 added total 24-hour urinary protein excretion. Model 3 was chosen as the primary model because proteinuria may mediate the association between APOL1 and the progression of chronic kidney disease. Thus, the inclusion of proteinuria in model 4 might be an overadjustment.
RESULTS
AASK
Study Population
Table 1 summarizes the baseline characteristics of the 693 patients who were included in the current analysis. A total of 160 (23.1%) had 2 copies of the APOL1 risk variants; at baseline, these patients, as compared with the patients in the other groups, had the lowest mean GFR (44.0 ml per minute per 1.73 m2, P = 0.01) and the highest prevalence of proteinuria (48.1%, P<0.001).
Table 1.
Baseline Characteristics of the 693 Patients in AASK, According to the Number of APOL1 Variants.*
| Characteristic | All Patients (N = 693) | No Copies of APOL1 Risk Variants (N = 234) | 1 Copy of APOL1 Risk Variants (N = 299) | 2 Copies of APOL1 Risk Variants (N = 160) | P Value for Trend† |
|---|---|---|---|---|---|
| Age — yr | 54.1±10.6 | 55.0±10.0 | 54.6±10.2 | 51.7±11.8 | 0.005 |
| Male sex — % | 59.7 | 65.4 | 56.9 | 56.9 | 0.07 |
| Body-mass index‡ | 31.1±6.7 | 30.1±6.0 | 31.5±6.8 | 31.7±7.2 | 0.02 |
| Glomerular filtration rate — ml/min/1.73 m2 | 47.3±13.5 | 48.0±13.9 | 48.6±12.9 | 44.0±13.6 | 0.01 |
| Serum creatinine — mg/dl | 2.0±0.7 | 2.0±0.7 | 1.9±0.6 | 2.1±0.7 | 0.03 |
| Median urinary protein-to-creatinine ratio (IQR)§ | 74.2 (27.4–307.4) | 67.9 (27.1–223.5) | 56.5 (25.1–220.1) | 203.0 (43.2–723.4) | 0.01 |
| Patients with proteinuria — %¶ | 30.4 | 25.2 | 25.1 | 48.1 | <0.001 |
| Patients with history of heart disease — % | 50.5 | 51.7 | 53.5 | 43.1 | 0.14 |
| Mean arterial pressure — mm Hg | 114.1±16.4 | 113.3±16.6 | 116.2±16.8 | 111.2±15.0 | 0.41 |
| Blood pressure — mm Hg | |||||
| Systolic | 150.4±24.3 | 149.4±25.1 | 153.5±24.4 | 146.2±22.0 | 0.37 |
| Diastolic | 95.9±14.6 | 95.2±14.3 | 97.6±15.2 | 93.7±13.7 | 0.53 |
| European ancestry — % of genetic makeup | 16.7±13.3 | 17.9±14.1 | 16.3±13.5 | 15.6±11.6 | 0.08 |
Plus–minus values are means ±SD. To convert the values for creatinine to micromoles per liter, multiply by 88.4. AASK denotes African American Study of Kidney Disease and Hypertension, and IQR interquartile range.
P values for trend were calculated by means of logistic regression, with the number of APOL1 risk-variant copies as the independent variable.
The body-mass index is the weight in kilograms divided by the square of the height in meters.
Urinary protein was measured in milligrams, and creatinine in grams.
Proteinuria was defined as a ratio of urinary protein to creatinine of at least 220, with urinary protein was measured in milligrams and creatinine in grams, or 0.22, with both levels measured in grams.
Renal Outcomes
Over a median follow-up of 9 years, 77 patients (11.1%) died before reaching the composite renal outcome, 204 (29.4%) received a diagnosis of end-stage renal disease, and 288 (41.6%) reached the composite renal outcome (Table 2). APOL1 status was not significantly associated with death before a diagnosis of end-stage renal disease.
Table 2.
Distribution of Incident Outcomes and Adjusted Hazard Ratios, According to Genetic Model and APOL1 Risk Status, among Patients in AASK.*
| APOL1 Risk Status | All Patients | End-Stage Renal Disease | End-Stage Renal Disease or Doubling of Serum Creatinine Level | Death before End-Stage Renal Disease | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Hazard Ratio (95% CI) | P Value | Hazard Ratio (95% CI) | P Value | Hazard Ratio (95% CI) | P Value | |||||
| no. (%) | no. (%) | no. (%) | ||||||||
| All patients | 693 | 204 (29.4) | 288 (41.6) | 77 (11.1) | ||||||
|
| ||||||||||
| Codominant genetic model | ||||||||||
|
| ||||||||||
| Patients with 0 copies of APOL1 risk variants | 234 | 56 (23.9) | 1.00 | 83 (35.5) | 1.00 | 28 (12.0) | 1.00 | |||
|
| ||||||||||
| Patients with 1 copy of APOL1 risk variants | 299 | 69 (23.1) | 1.04 (0.72–1.48) | 0.83 | 112 (37.5) | 1.15 (0.86–1.53) | 0.34 | 33 (11.0) | 0.98 (0.59–1.62) | 0.93 |
|
| ||||||||||
| Patients with 2 copies of APOL1 risk variants | 160 | 79 (49.4) | 2.21 (1.56–3.14) | <0.001 | 93 (58.1) | 2.03 (1.50–2.74) | <0.001 | 16 (10.0) | 1.24 (0.67–2.30) | 0.50 |
|
| ||||||||||
| Recessive genetic model | ||||||||||
|
| ||||||||||
| Patients with 0 or 1 copy of APOL1 risk variants | 533 | 125 (23.5) | 1.00 | 195 (36.6) | 1.00 | 61 (11.4) | 1.00 | |||
|
| ||||||||||
| Patients with 2 copies of APOL1 risk variants | 160 | 79 (49.4) | 2.16 (1.62–2.89) | <0.001 | 93 (58.1) | 1.88 (1.46–2.41) | <0.001 | 16 (10.0) | 1.25 (0.72–2.18) | 0.43 |
Patients with 2 copies of APOL1 risk variants were considered to be at high risk, whereas those with 0 or 1 copy were considered to be at low risk. Hazard ratios have been adjusted for age, sex, percentage of European ancestry, and baseline glomerular filtration rate. P values are for the comparison with the reference value used in that model. CI denotes confidence interval.
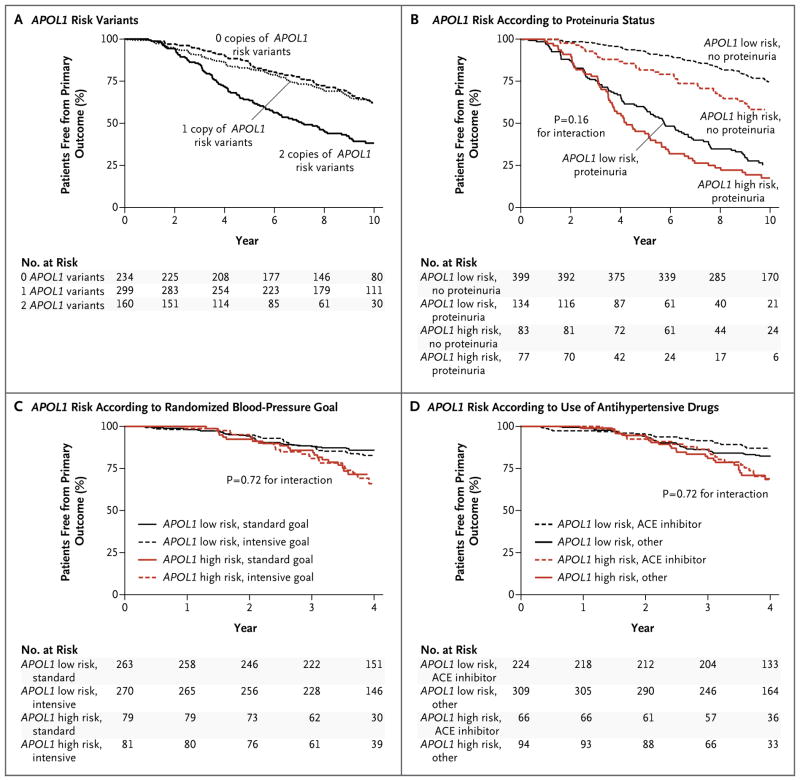
Of the 160 patients with 2 copies of the APOL1 risk variants, 93 (58.1%) reached the composite renal outcome during follow-up. On the basis of the codominant genetic model, patients with 2 copies of the APOL1 risk variants were about twice as likely to progress to the composite renal outcome as was the reference group (hazard ratio, 2.03; P<0.001), whereas the risk of the composite renal outcome in those with 1 copy of the risk variants was similar to the risk in the reference group (hazard ratio, 1.15; P = 0.34) (Table 2 and Fig. 1A). Similar associations were observed with only end-stage renal disease as the outcome. On the basis of the recessive genetic model, the hazard ratio for the composite renal outcome in the APOL1 high-risk group, as compared with the low-risk group, was 1.88 (P<0.001).
Figure 1. Proportion of Patients Free from Progression of Chronic Kidney Disease in AASK.
In the African American Study of Kidney Disease and Hypertension (AASK), the primary outcome was defined as a doubling of the serum creatinine level or incident end-stage renal disease (the analyses shown in Panels A and B). In analyses of the interaction between APOL1 variants and trial interventions, the composite outcome was a reduction of 50% in the glomerular filtration rate (as measured by iothalamate clearance) or incident end-stage renal disease (the analyses shown in Panels C and D). Panel A shows the proportion of patients, among all 693 patients who were included in the study, who were free from progression of chronic kidney disease, according to the number of copies of the high-risk APOL1 variants (0, 1, or 2 copies). In Panels B, C, and D, patients who had 2 copies of high-risk APOL1 variants were classified as being in the APOL1 high-risk group; those with 0 or 1 copy were categorized as being in the APOL1 low-risk group. Panel B shows the results with stratification of the patients according to the proteinuria status at baseline and APOL1 risk status. Proteinuria was defined as a ratio of urinary protein to creatinine of at least 220 (with urinary protein measured in milligrams and creatinine in grams) or 0.22 (with both measured in grams). Panel C shows the results with stratification of the patients according to the randomized level of blood-pressure control (intensive vs. standard) and APOL1 risk status. Panel D shows the results with stratification of the patients according to whether they were assigned to receive an angiotensin-converting–enzyme (ACE) inhibitor or other antihypertensive medication and APOL1 risk status.
Blood-Pressure Control
The effect of APOL1 on the progression of chronic kidney disease was not confounded by levels of blood pressure. At baseline, the mean blood pressure was 146/94 mm Hg in the APOL1 high-risk group and 152/97 mm Hg in the APOL1 low-risk group. Throughout the trial phase, the mean blood pressure was the same in the two risk groups (135/82 mm Hg). During the cohort phase, the mean blood pressures were again similar (134/78 mm Hg and 133/78 mm Hg, respectively). During the trial, 42.1% of patients in the APOL1 high-risk group and 43.8% in the APOL1 low-risk group were receiving an ACE inhibitor or angiotensin-receptor blocker. The corresponding percentages during the cohort phase were 86.2% and 84.7%.
Proteinuria and Randomized Therapies
Although baseline proteinuria was a major predictor of disease progression, it did not significantly modify the effect of APOL1 on progression (P = 0.16 for interaction) (Fig. 1B). In addition, there was no significant interaction between APOL1 status and the randomized blood-pressure goal with respect to the progression of chronic kidney disease (P = 0.72 for interaction) (Fig. 1C), nor was there a significant interaction between APOL1 status and the randomized antihypertensive medication with respect to progression (P = 0.72 for interaction) (Fig. 1D, and Tables S2 and S3 in the Supplementary Appendix).
MYH9 Analyses
A total of 34 patients had two copies of the high-risk MYH9 haplotype but no copies of the high-risk APOL1 haplotype. Of these 34 patients, 10 reached the composite outcome, resulting in a relative hazard of 0.73 as compared with the reference group of no risk alleles at both MYH9 and APOL1 (P = 0.35) (Table S4 in the Supplementary Appendix).
CRIC STUDY
Study Population
Among the 2955 patients for whom adequate genotyping data were available, 48% were black, and 45.5% had diabetes (Table 3). There were significant differences between black patients and white patients with respect to many of the baseline characteristics, including higher mean blood pressure and more severe proteinuria in black patients. There were few significant differences in baseline characteristics between black patients in the APOL1 high-risk group and those in the APOL1 low-risk group (Table 3, and Table S5 in the Supplementary Appendix). The most notable difference was a higher mean rate of 24-hour urinary protein excretion in the APOL1 high-risk group than in the APOL1 low-risk group among patients without diabetes. (See Table S6 in the Supplementary Appendix for the distribution of APOL1 risk variants among black patients according to diabetes status.)
Table 3.
Baseline Characteristics and Events during the CRIC Study, Stratified According to Diabetes Status, Race, and APOL1 Status.*
| Variable | With Diabetes
|
Without Diabetes
|
||||||
|---|---|---|---|---|---|---|---|---|
| All White Patients (N = 624) | All Black Patients (N = 722) | Black Patients with APOL1 Low Risk (N = 610) | Black Patients with APOL1 High Risk (N = 112) | All White Patients (N = 920) | All Black Patients (N = 689) | Black Patients with APOL1 Low Risk (N = 531) | Black Patients with APOL1 High Risk (N = 158) | |
| Baseline characteristic | ||||||||
|
| ||||||||
| Age — yr | 59.5±9.8 | 60.0±9.4 | 60.0±9.2 | 59.6±10.2 | 58.7±11.5 | 56.1±11.6† | 57.8±10.6 | 50.5±13.0‡ |
|
| ||||||||
| Male sex — no. (%) | 411 (65.9) | 345 (47.8)† | 296 (48.5) | 49 (43.8) | 509 (55.3) | 348 (50.5) | 265 (49.9) | 83 (52.5) |
|
| ||||||||
| Hypertension — no. (%)§ | 550 (88.1) | 688 (95.3)† | 582 (95.4) | 106 (94.6) | 669 (72.7) | 625 (90.7)† | 476 (89.6) | 149 (94.3) |
|
| ||||||||
| Blood pressure — mm Hg | ||||||||
|
| ||||||||
| Systolic | 125.6±19.1 | 136.6±23.6† | 136.2±24.2 | 138.7±20.0 | 119.3±17.7 | 128.9±21.7† | 129.9±21.7 | 125.6±21.4¶ |
|
| ||||||||
| Diastolic | 66.9±11.3 | 71.6±13.5† | 71.0±13.5 | 74.5±13.3¶ | 70.4±11.0 | 76.4±13.8† | 76.1±13.4 | 77.2±15.0 |
|
| ||||||||
| Estimated glomerular filtration rate — ml/min/1.73 m2 | 43.4±14.7 | 41.3±14.8|| | 41.4±14.8 | 40.8±15.1 | 50.8±17.9 | 46.6±17.4† | 46.2±17.0 | 48.0±18.5 |
|
| ||||||||
| Proteinuria — g/24 hr | ||||||||
|
| ||||||||
| Mean | 1.1±2.6 | 1.5±2.8|| | 1.5±2.7 | 1.9±3.4 | 0.4±1.1 | 0.6±1.3|| | 0.5±1.1 | 0.9±1.6‡ |
|
| ||||||||
| Median | 0.2 | 0.4 | 0.4 | 0.6 | 0.1 | 0.1 | 0.1 | 0.4 |
|
| ||||||||
| Event during study | ||||||||
|
| ||||||||
| Duration of follow-up — yr | 4.2±2.2 | 3.8±2.2† | 3.8±2.2 | 3.5±2.2 | 4.9±2.0 | 4.4±2.2† | 4.5±2.2 | 4.2±2.2 |
|
| ||||||||
| Estimated glomerular filtration rate slope — ml/min/1.73 m2/yr | −1.5±4.3 | −2.9±4.9† | −2.7±4.7 | −4.3±5.6¶ | −0.7±3.1 | −1.4±4.2† | −1.0±4.0 | −2.9±4.5‡ |
|
| ||||||||
| Patients with renal event — no. (%)** | 152 (24.4) | 274 (38.0)† | 220 (36.1) | 54 (48.2)¶ | 95 (10.3) | 155 (22.5)† | 106 (20.0) | 49 (31.0)†† |
|
| ||||||||
| Renal event rate — no. per 100-person yr | 5.8 | 10.1† | 9.5 | 13.7¶ | 2.1 | 5.1† | 4.4 | 7.5‡ |
|
| ||||||||
| Incident end-stage renal disease — no. (rate per 100 person-yr) | 100 (3.2) | 219 (6.5)† | 177 (6.2) | 42 (8.1) | 67 (1.3) | 122 (3.4)† | 82 (2.9) | 40 (5.0)†† |
|
| ||||||||
| Deaths — no. (rate per 100 person-yr) | 82 (3.3) | 95 (4.1) | 82 (4.0) | 13 (4.3) | 69 (1.5) | 58 (1.9) | 47 (2.0) | 11 (1.7) |
|
| ||||||||
| Withdrawal from study before renal event — no./total no. (%) | 28/472 (5.9) | 29/448 (6.5) | 24/390 (6.2) | 5/58 (8.6) | 44/825 (5.3) | 30/534 (5.6) | 27/425 (6.4) | 3/109 (2.8) |
Plus–minus values are means ± SD. The APOL1 risk genotype was based on the recessive genetic model. The only significant between-group differences at baseline are indicated. CRIC denotes Chronic Renal Insufficiency Cohort.
P<0.001 for the comparison between all white patients and all black patients.
P<0.001 for the comparison between the APOL1 high-risk group and the APOL1 low-risk group.
Patients were considered to have hypertension if they had a blood pressure of 140/90 mm Hg or more or were receiving an antihypertensive medication.
P<0.05 for the comparison between the APOL1 high-risk group and the APOL1 low-risk group.
P<0.01 for the comparison between all white patients and all black patients.
A renal event was defined as the diagnosis of end-stage renal disease or a reduction of 50% in the eGFR from baseline.
P<0.01 for the comparison between the APOL1 high-risk group and the APOL1 low-risk group.
Change in eGFR and Renal Outcome
Over a mean follow-up of 4.4 years, 676 composite renal events occurred. Overall, among both patients with diabetes and those without diabetes, black patients had a steeper decline in the eGFR and a higher rate of the composite renal outcome than did white patients (Table 3). Among the patients with diabetes, the eGFR slope (as measured in milliliters per minute per 1.73 m2 per year) was −1.5 among white patients, −2.7 among black patients in the APOL1 low-risk group, and −4.3 among black patients in the APOL1 high-risk group. Among the patients without diabetes, the corresponding eGFR slopes were −0.7, −1.0, and −2.9.
Similar patterns were observed with respect to the composite renal outcome. Among patients with diabetes, white patients had the lowest event rate, followed by black patients in the APOL1 low-risk group and then by black patients in the APOL1 high-risk group (5.8, 9.5, and 13.7 per 100 person-years, respectively); among those without diabetes, the event rates were 2.1, 4.4, and 7.5 per 100 person-years, respectively. Within each stratum (diabetes or no diabetes), death rates for black patients were similar to those for white patients.
Multivariate Analyses of eGFR Slopes
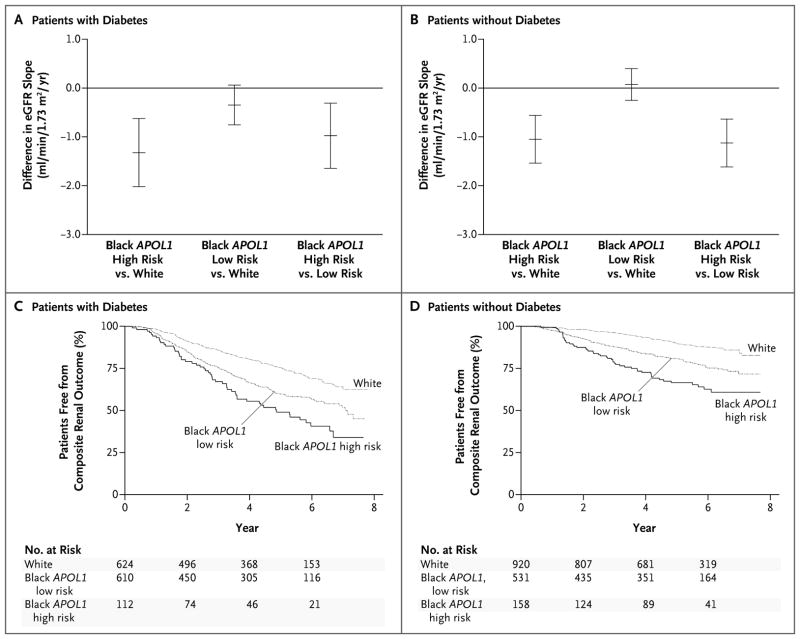
In the subgroup of patients with diabetes, there was a more rapid decline in kidney function, after adjustment for demographic, socioeconomic, and clinical risk factors (model 3), among black patients in the APOL1 high-risk group than among white patients (mean adjusted difference in eGFR slope, −1.32 ml per minute per 1.73 m2 per year; P<0.001) (Table 4 and Fig. 2A) and than among black patients in the APOL1 low-risk group (mean adjusted difference in eGFR slope, −1.07 ml per minute per 1.73 m2 per year; P = 0.005) (Fig. 2A, and Table S7 in the Supplementary Appendix).
Table 4.
Multivariable Analyses of Differences in the eGFR Slope and Risk of the Composite Renal Outcome in the CRIC Study.*
| Multivariate Model and Comparison Group | Difference in eGFR Slope | Risk of Composite Renal Outcome | ||||||
|---|---|---|---|---|---|---|---|---|
| With Diabetes | Without Diabetes | With Diabetes | Without Diabetes | |||||
| ml/min/1.73 m2/yr (95% CI) | P value | ml/min/1.73 m2/yr (95% CI) | P value | hazard ratio (95% CI) | P value | hazard ratio (95% CI) | P value | |
| Model 1 | ||||||||
|
| ||||||||
| All black patients vs. all white patients | −1.08 (−1.48 to −0.69) | <0.001 | −0.28 (−0.57 to 0.01) | 0.06 | 1.77 (1.42 to 2.20) | <0.001 | 2.20 (1.65 to 2.94) | <0.001 |
|
| ||||||||
| Black patients with APOL1 high risk vs. all white patients | −2.00 (−2.72 to −1.28) | <0.001 | −1.12 (−1.6 to −0.63) | <0.001 | 2.48 (1.79 to 3.43) | <0.001 | 3.05 (2.07 to 4.48) | <0.001 |
|
| ||||||||
| Black patients with APOL1 low risk vs. all white patients | −0.92 (−1.33 to −0.52) | <0.001 | −0.05 (−0.36 to 0.25) | 0.72 | 1.65 (1.32 to 2.07) | <0.001 | 1.96 (1.44 to 2.67) | <0.001 |
|
| ||||||||
| Model 2 | ||||||||
|
| ||||||||
| All black patients vs. all white patients | −0.96 (−1.37 to −0.55) | <0.001 | −0.28 (−0.59 to 0.03) | 0.07 | 1.79 (1.43 to 2.24) | <0.001 | 2.15 (1.58 to 2.91) | <0.001 |
|
| ||||||||
| Black patients with APOL1 high risk vs. all white patients | −1.95 (−2.68 to −1.22) | <0.001 | −1.16 (−1.66 to −0.66) | <0.001 | 2.48 (1.78 to 3.45) | <0.001 | 3.05 (2.05 to 4.53) | <0.001 |
|
| ||||||||
| Black patients with APOL1 low risk vs. all white patients | −0.78 (−1.20 to −0.36) | <0.001 | −0.04 (−0.36 to 0.29) | 0.82 | 1.67 (1.32 to 2.11) | <0.001 | 1.88 (1.36 to 2.61) | <0.001 |
|
| ||||||||
| Model 3 | ||||||||
|
| ||||||||
| All black patients vs. all white patients | −0.48 (−0.88 to −0.09) | 0.02 | −0.17 (−0.48 to 0.13) | 0.27 | 1.49 (1.18 to 1.88) | <0.001 | 1.80 (1.31 to 2.49) | <0.001 |
|
| ||||||||
| Black patients with APOL1 high risk vs. all white patients | −1.32 (−2.02 to −0.63) | <0.001 | −1.05 (−1.54 to −0.56) | <0.001 | 1.95 (1.39 to 2.73) | <0.001 | 2.68 (1.78 to 4.05) | <0.001 |
|
| ||||||||
| Black patients with APOL1 low risk vs. all white patients | −0.35 (−0.75 to 0.06) | 0.09 | 0.08 (−0.25 to −0.40) | 0.65 | 1.40 (1.10 to 1.78) | 0.006 | 1.57 (1.11 to 2.21) | 0.01 |
|
| ||||||||
| Model 4 | ||||||||
|
| ||||||||
| All black patients vs. all white patients | −0.21 (−0.55 to 0.14) | 0.25 | −0.21 (−0.50 to 0.08) | 0.16 | 1.34 (1.06 to 1.70) | 0.02 | 1.98 (1.44 to 2.72) | <0.001 |
|
| ||||||||
| Black patients with APOL1 high risk vs. all white patients | −0.79 (−1.41 to −0.17) | 0.01 | −0.81 (−1.26 to −0.35) | <0.001 | 1.58 (1.12 to 2.24) | 0.009 | 2.84 (1.84 to 4.38) | <0.001 |
|
| ||||||||
| Black patients with APOL1 low risk vs. all white patients | −0.11 (−0.47 to 0.25) | 0.55 | −0.03 (−0.34 to 0.27) | 0.84 | 1.29 (1.01 to 1.65) | 0.04 | 1.78 (1.28 to 2.49) | <0.001 |
The composite outcome was incident end-stage renal disease or a reduction of 50% in the eGFR from baseline. The APOL1 risk was based on the recessive genetic model. Model 1 is the multivariable-adjusted base model with adjustment for age, sex, clinical site, and baseline eGFR. Model 2 includes all the variables in model 1 plus education level, treatment by a nephrologist, and the use of either an angiotensin-converting–enzyme inhibitor or an angiotensin-receptor blocker. Model 3 includes all the variables in model 2 plus systolic blood pressure, body-mass index, glycated hemoglobin level, and smoking status. Model 4 includes all the variables in model 3 plus the total 24-hour urinary protein excretion.
Figure 2. Between-Group Comparisons of the Estimated Glomerular Filtration Rate (eGFR) Slope and Proportion of Patients Free from a Primary Outcome Event in the CRIC Study.
In the Chronic Renal Insufficiency Cohort (CRIC) study, the primary outcomes were the eGFR slope and a composite of end-stage renal disease or a reduction of 50% in the eGFR from baseline. Shown are mean differences in the eGFR slope for black patients in the APOL1 high-risk group versus white patients, black patients in the APOL1 low-risk group versus white patients, and black patients in the APOL1 high-risk group versus black patients in the APOL1 low-risk group, among patients with diabetes (Panel A) and among those without diabetes (Panel B). In Panels A and B, the I bars indicate 95% confidence intervals. I bars that cross above the horizontal black line indicate that the difference in eGFR is not significant. Also shown are the proportions of white patients and black patients in the APOL1 high-risk and low-risk groups who were free from the primary outcome of end-stage renal disease or a reduction of 50% in the eGFR from baseline, among patients with diabetes (Panel C) and among those without diabetes (Panel D).
These differences were also observed in the subgroup of patients without diabetes in model 3, with a more rapid decline in eGFR among black patients in the APOL1 high-risk group than among white patients (mean adjusted difference in eGFR slope, −1.05 ml per minute per 1.73 m2 per year; P<0.001) (Table 4 and Fig. 2B) and than among black patients in the APOL1 low-risk group (mean adjusted difference in estimated GFR, −1.21 ml per minute per 1.73 m2 per year; P<0.001) (Fig. 2B, and Table S7 in the Supplementary Appendix). In model 3, there was no significant difference in the eGFR slope between black patients in the APOL1 low-risk group and white patients, regardless of diabetes status (Table 4).
Multivariate Analyses of the Composite Renal Outcomes
As compared with white patients, black patients in both the APOL1 high-risk group and the APOL1 low-risk group had a higher risk of the composite renal outcome regardless of diabetes status (model 3 in Table 4 and Fig. 2C and 2D). Among patients with diabetes, the adjusted hazard ratios for black patients in the APOL1 high-risk group and those in the APOL1 low-risk group, as compared with white patients, were 1.95 (P<0.001) and 1.40 (P = 0.006), respectively. Black patients in the APOL1 high-risk group also had a significantly higher risk of the composite renal outcome than did those in the APOL1 low-risk group (hazard ratio, 1.46; P = 0.02) (Table S7 in the Supplementary Appendix).
Similar associations were observed among patients without diabetes, among whom the adjusted hazard ratios in the comparison with white patients were 2.68 for black patients in the APOL1 high-risk group (P<0.001) and 1.57 for those in the APOL1 low-risk group (P = 0.01). Black patients in the APOL1 high-risk group also had a significantly higher risk of the composite renal outcome than did those in the APOL1 low-risk group (hazard ratio, 1.61; P = 0.01) (Table S7 in the Supplementary Appendix).
Sensitivity and Supplemental Analyses
The results of sensitivity analyses with the outcomes of end-stage renal disease alone and measured iothalamate GFR slope were similar to those of the primary analyses (Tables S8 and S9 in the Supplementary Appendix). As in AASK, the presence of a single APOL1 risk variant was not significantly associated with renal events or the eGFR slope. The presence of the MYH9 risk genotype was not associated with either eGFR slope or the risk of composite renal events (Table S10 in the Supplementary Appendix).
DISCUSSION
In two prospective, multicenter studies involving patients with chronic kidney disease, we found a consistent, strong relationship between the presence of APOL1 risk variants and disease progression. This relationship, in part, explains the disparities in rates of end-stage renal disease between black patients and white patients. In AASK, which enrolled black patients with chronic kidney disease attributed to hypertension, about 60% of patients in the APOL1 high-risk group had progression to the composite renal outcome. The APOL1 status of the patients did not modify the effects of proteinuria and the treatment regimens tested in AASK.
The results from the CRIC study extended the findings in AASK by the inclusion of data from patients with diabetes and a comparison group of white patients. Independent of diabetes status, black patients overall and the subgroups of black patients with and without the APOL1 high-risk variants had a significantly higher risk of the composite renal outcome (a reduction of 50% in the eGFR or incident end-stage renal disease) than did white patients. In parallel analyses, the decline in the eGFR was more rapid among black patients who had APOL1 high-risk variants than among white patients and black patients with APOL1 low-risk variants. In contrast to the results of the time-to-event analyses, the eGFR decline did not differ significantly between white patients and black patients in the APOL1 low-risk group, regardless of whether patients had diabetes. Despite the strong associations between the presence of APOL1 high-risk variants and disease progression, our results do not fully explain the well-documented racial disparities in rates of end-stage renal disease.
APOL1 encodes apolipoprotein L1, a circulating protein that can lyse T. brucei and various other trypanosomes.32,33 Relatively little is known about the role of apolipoprotein L1 in the kidney, other than that this protein is expressed in the glomerulus.34 Therefore, it remains possible that the consistently strong association that has been observed between the APOL1 G1 and G2 variants and renal outcomes in human studies is due to their linkage with other causal variants or genes.
Although previous studies have provided indirect evidence that APOL1 is associated with increased progression of chronic kidney disease, the case–control design of those studies could not distinguish between increased rates of disease progression and increased incidence of chronic kidney disease. We previously found an association between an increased rate of decline in the eGFR and the presence of APOL1 high-risk variants over the relatively short time frame of the AASK trial,16 but recent analyses have shown that the eGFR trajectory over a 10-year period in AASK is highly variable.35 In this study, we now provide direct evidence from AASK and the CRIC study that the APOL1 high-risk variants are associated with increased disease progression over the long term.
In AASK, there was no significant interaction between APOL1 and the trial interventions. Currently, therapeutic options to retard disease progression are limited. The use of ACE inhibitors slowed progression in AASK,28 but even while patients were receiving the recommended therapy, a majority had disease progression during a 10-year period.36 The lack of significant interaction between APOL1 and treatment with an ACE inhibitor suggests that patients in the APOL1 high-risk group still benefit from this class of drugs. Although some traditional risk factors for progression, such as proteinuria, still apply to patients in the APOL1 high-risk group, there are clearly other risk factors that affect this group, since approximately 40% of patients in the APOL1 high-risk group did not have progression to the composite renal outcome.
An important finding from the CRIC study is the strong association between APOL1 high-risk variants and the progression of chronic kidney disease among patients with diabetes. Although genetic variants in the region of chromosome 22 have been associated with various kidney diseases14–19,37 in black patients, studies involving patients with both diabetes and kidney disease have been inconsistent.21,22 Initial studies focused on MHY9 rather than APOL1 variants, and none were longitudinal.14,38–40 One study did not show an association between APOL1 and chronic kidney disease among patients with diabetes; however, the statistical power for that study was low.22 A recent study41 showed an association between APOL1 high-risk variants and both incident chronic kidney disease and end-stage renal disease in unstratified analyses that included patients with and those without diabetes and provided suggestive evidence of a similar association among patients with diabetes. The rate of decline in eGFR has not, to our knowledge, been reported previously among patients with diabetes.
Our studies have limitations. The precise cause of chronic kidney disease was not ascertained in either study. In AASK, the sample size was relatively small for interaction analyses. In addition, not all AASK patients provided DNA samples or were successfully genotyped, raising the potential for bias. However, APOL1 variants were not associated with mortality in either study, and the risk relationship between APOL1 variants and disease progression was similar in AASK and the CRIC study. Strengths of both studies include their long duration of follow-up, low rates of missing outcome data, and adjustment for a large number of potential confounders. Specific strengths of the CRIC study include substantial representation of both black patients and white patients, both those with and those without diabetes, and estimation of the GFR with the use of a study-derived estimating equation. Specific strengths of AASK include its trial phase, which allowed exploration of the interactive effects of APOL1 with antihypertensive therapies. In addition, throughout AASK, including the trial and cohort phases, blood pressure was well controlled.36 Our finding that patients in the APOL1 high-risk group and those in the low-risk group had similar levels of blood pressure makes it unlikely that the effects of APOL1 on disease progression are mediated through blood pressure.
In conclusion, renal high-risk variants in APOL1 were associated with an increased risk of progression of chronic kidney disease among black patients, even among those with well-controlled blood pressure. These variants may explain, in part, the markedly increased risk of end-stage renal disease among black patients, as compared with white patients, regardless of diabetes status. These results also highlight the need to identify other risk factors that can account for residual disparities in end-stage renal disease between black patients and white patients. In the context of previous studies, our results suggest that APOL1 high-risk variants increase the risk of progression of chronic kidney disease among black patients, regardless of the cause.
Supplementary Material
Acknowledgments
AASK was supported by grants to each clinical center and the coordinating center from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), the Office of Research in Minority Health (now the National Center on Minority Health and Health Disparities), and institutional grants from the National Institutes of Health (NIH) (M01 RR-00080, M01 RR-00071, M0100032, P20-RR11145, M01 RR00827, M01 RR00052, 2P20 RR11104, RR029887, and DK 2818-02); King Pharmaceuticals provided monetary support and antihypertensive medications to each clinical center; Pfizer, AstraZeneca Pharmaceuticals, GlaxoSmithKline, Forest Laboratories, Pharmacia, and Upjohn also donated antihypertensive medications. The CRIC study was supported by cooperative agreements with the NIDDK (U01DK060990, U01DK060984, U01DK061022, U01DK061021, U01DK061028, U01DK060980, U01DK060963, and U01DK060902); Clinical and Translational Science Awards to the University of Pennsylvania (UL1 RR-024134), Johns Hopkins University (UL1 RR-025005), Clinical and Translational Science Collaborative of Cleveland (UL1 RR-024989), Michigan Institute for Clinical and Health Research (UL1 RR-024986), University of Illinois at Chicago (UL1 RR-029879), and Kaiser Permanente Northern California (UL1 RR-024131); University of Maryland General Clinical Research Center (M01 RR-16500) and the Multi-disciplinary Research Career Development Program (K12 RR023250); Tulane University Translational Research in Hypertension and Renal Biology (P30 GM103337); the National Cancer Institute, under contract HHSN26120080001E; the Intramural Research Programs of the NIDDK and the Center for Cancer Research of the National Cancer Institute; and the National Center for Advancing Translational Sciences component of the NIH and the NIH Roadmap for Medical Research (UL1 TR-000439).
We thank the patients and staff members who participated in the AASK and CRIC studies for their sustained commitment to the studies, and Jennifer Miskimon for assistance in the preparation of the manuscript.
APPENDIX
The authors’ affiliations are as follows: University of Maryland School of Medicine (A.P., J.C.F.), Johns Hopkins Bloomberg School of Public Health (W.H.L.K., M.L., L.J.A.), Johns Hopkins University School of Medicine (M.J.C., L.J.A.), and Johns Hopkins University, Welch Center for Prevention, Epidemiology, and Clinical Research (W.H.L.K., L.J.A.) — all in Baltimore; University of Pennsylvania Perelman School of Medicine and the Center for Clinical Epidemiology and Biostatistics, University of Pennsylvania — both in Philadelphia (D.X., H.I.F., A.H.A., K.T.); University of Wisconsin School of Medicine and Public Health, Madison (B.C.A.); University of California at San Francisco, San Francisco (C.-Y.H.); University of Toronto, Hospital for Sick Children and University Health Network, Toronto (R.S.P.); National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda (J.W.K., J.B.K.), and the Center for Cancer Research, SAIC-Frederick, National Cancer Institute, Frederick (C.A.W.) — both in Maryland; University of Utah School of Medicine, Salt Lake City (T.H.G.); Case Western Reserve University School of Medicine, Cleveland (J.T.W.); University of Illinois College of Medicine, Chicago (J.P.L.); Wake Forest School of Medicine, Winston-Salem, NC (B.I.F.); University of Michigan School of Medicine, Ann Arbor (A.O.); George Washington University School of Medicine (D.S.R.) and Georgetown University School of Medicine (M.S.L.) — both in Washington, DC; Tulane University School of Public Health and Tropical Medicine, New Orleans (J.H.); and Kaiser Permanente of Northern California, Oakland (C.-Y.H., N.G.J.).
Footnotes
A complete list of investigators and staff in the African American Study of Kidney Disease and Hypertension (AASK) and the Chronic Renal Insufficiency Cohort (CRIC) study is provided in the Supplementary Appendix, available at NEJM.org.
The authors’ affiliations are listed in the Appendix.
The views expressed in this article do not necessarily reflect those of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. government.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.McClellan W, Tuttle E, Issa A. Racial differences in the incidence of hypertensive end-stage renal disease (ESRD) are not entirely explained by differences in the prevalence of hypertension. Am J Kidney Dis. 1988;12:285–90. doi: 10.1016/s0272-6386(88)80221-x. [DOI] [PubMed] [Google Scholar]
- 2.Cowie CC, Port FK, Wolfe RA, Savage PJ, Moll PP, Hawthorne VM. Disparities in incidence of diabetic end-stage renal disease according to race and type of diabetes. N Engl J Med. 1989;321:1074–9. doi: 10.1056/NEJM198910193211603. [DOI] [PubMed] [Google Scholar]
- 3.Hall YN, Hsu CY, Iribarren C, Darbinian J, McCulloch CE, Go AS. The conundrum of increased burden of end-stage renal disease in Asians. Kidney Int. 2005;68:2310–6. doi: 10.1111/j.1523-1755.2005.00691.x. [DOI] [PubMed] [Google Scholar]
- 4.Lipworth L, Mumma MT, Cavanaugh KL, et al. Incidence and predictors of end stage renal disease among low-income blacks and whites. PLoS One. 2012;7(10):e48407. doi: 10.1371/journal.pone.0048407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hsu CY, Lin F, Vittinghoff E, Shlipak MG. Racial differences in the progression from chronic renal insufficiency to end-stage renal disease in the United States. J Am Soc Nephrol. 2003;14:2902–7. doi: 10.1097/01.asn.0000091586.46532.b4. [DOI] [PubMed] [Google Scholar]
- 6.Choi AI, Rodriguez RA, Bacchetti P, Bertenthal D, Hernandez GT, O’Hare AM. White/black racial differences in risk of end-stage renal disease and death. Am J Med. 2009;122:672–8. doi: 10.1016/j.amjmed.2008.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McClellan W, Warnock DG, McClure L, et al. Racial differences in the prevalence of chronic kidney disease among participants in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Cohort Study. J Am Soc Nephrol. 2006;17:1710–5. doi: 10.1681/ASN.2005111200. [DOI] [PubMed] [Google Scholar]
- 8.Grams ME, Chow EK, Segev DL, Coresh J. Lifetime incidence of CKD stages 3–5 in the United States. Am J Kidney Dis. 2013;62:245–52. doi: 10.1053/j.ajkd.2013.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hunsicker LG, Adler S, Caggiula A, et al. Predictors of the progression of renal disease in the Modification of Diet in Renal Disease Study. Kidney Int. 1997;51:1908–19. doi: 10.1038/ki.1997.260. [DOI] [PubMed] [Google Scholar]
- 10.Walker WG, Neaton JD, Cutler JA, Neuwirth R, Cohen JD. Renal function change in hypertensive members of the Multiple Risk Factor Intervention Trial: racial and treatment effects. JAMA. 1992;268:3085–91. [PubMed] [Google Scholar]
- 11.Derose SF, Rutkowski MP, Crooks PW, et al. Racial differences in estimated GFR decline, ESRD, and mortality in an integrated health system. Am J Kidney Dis. 2013;62:236–44. doi: 10.1053/j.ajkd.2013.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peralta CA, Vittinghoff E, Bansal N, et al. Trajectories of kidney function decline in young black and white adults with preserved GFR: results from the Coronary Artery Risk Development in Young Adults (CARDIA) study. Am J Kidney Dis. 2013;62:261–6. doi: 10.1053/j.ajkd.2013.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barbour SJ, Schachter M, Er L, Djurdjev O, Levin A. A systematic review of ethnic differences in the rate of renal progression in CKD patients. Nephrol Dial Transplant. 2010;25:2422–30. doi: 10.1093/ndt/gfq283. [DOI] [PubMed] [Google Scholar]
- 14.Kao WH, Klag MJ, Meoni LA, et al. MYH9 is associated with nondiabetic end-stage renal disease in African Americans. Nat Genet. 2008;40:1185–92. doi: 10.1038/ng.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kopp JB, Smith MW, Nelson GW, et al. MYH9 is a major-effect risk gene for focal segmental glomerulosclerosis. Nat Genet. 2008;40:1175–84. doi: 10.1038/ng.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lipkowitz MS, Freedman BI, Langefeld CD, et al. Apolipoprotein L1 gene variants associate with hypertension-attributed nephropathy and the rate of kidney function decline in African Americans. Kidney Int. 2013;83:114–20. doi: 10.1038/ki.2012.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Genovese G, Friedman DJ, Ross MD, et al. Association of trypanolytic ApoL1 variants with kidney disease in African Americans. Science. 2010;329:841–5. doi: 10.1126/science.1193032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tzur S, Rosset S, Shemer R, et al. Missense mutations in the APOL1 gene are highly associated with end stage kidney disease risk previously attributed to the MYH9 gene. Hum Genet. 2010;128:345–50. doi: 10.1007/s00439-010-0861-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kopp JB, Nelson GW, Sampath K, et al. APOL1 genetic variants in focal segmental glomerulosclerosis and HIV-associated nephropathy. J Am Soc Nephrol. 2011;22:2129–37. doi: 10.1681/ASN.2011040388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The 1000 Genomes Project Consortium. An integrated map of genetic variation from 1,092 human genomes. Nature. 2012;491:56–65. doi: 10.1038/nature11632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pollak MR, Genovese G, Friedman DJ. APOL1 and kidney disease. Curr Opin Nephrol Hypertens. 2012;21:179–82. doi: 10.1097/MNH.0b013e32835012ab. [DOI] [PubMed] [Google Scholar]
- 22.Friedman DJ, Kozlitina J, Genovese G, Jog P, Pollak MR. Population-based risk assessment of APOL1 on renal disease. J Am Soc Nephrol. 2011;22:2098–105. doi: 10.1681/ASN.2011050519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Appel LJ, Middleton J, Miller ER, III, et al. The rationale and design of the AASK Cohort Study. J Am Soc Nephrol. 2003;14(Suppl 2):S166–S172. doi: 10.1097/01.asn.0000070081.15137.c0. [DOI] [PubMed] [Google Scholar]
- 24.Sika M, Lewis J, Douglas J, et al. Baseline characteristics of participants in the African American Study of Kidney Disease and Hypertension (AASK) Clinical Trial and Cohort Study. Am J Kidney Dis. 2007;50:78–89. doi: 10.1053/j.ajkd.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 25.Lash JP, Go AS, Appel LJ, et al. Chronic Renal Insufficiency Cohort (CRIC) Study: baseline characteristics and associations with kidney function. Clin J Am Soc Nephrol. 2009;4:1302–11. doi: 10.2215/CJN.00070109. [Erratum, Clin J Am Soc Nephrol 2011;6: 2548–63.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Feldman HI, Appel LJ, Chertow GM, et al. The Chronic Renal Insufficiency Cohort (CRIC) Study: design and methods. J Am Soc Nephrol. 2003;14(Suppl 2):S148–S153. doi: 10.1097/01.asn.0000070149.78399.ce. [DOI] [PubMed] [Google Scholar]
- 27.Fischer MJ, Go AS, Lora CM, et al. CKD in Hispanics: baseline characteristics from the CRIC (Chronic Renal Insufficiency Cohort) and Hispanic-CRIC Studies. Am J Kidney Dis. 2011;58:214–27. doi: 10.1053/j.ajkd.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wright JT, Jr, Bakris G, Greene T, et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA. 2002;288:2421–31. doi: 10.1001/jama.288.19.2421. [Erratum, JAMA 2006;295:2726.] [DOI] [PubMed] [Google Scholar]
- 29.Anderson AH, Yang W, Hsu CY, et al. Estimating GFR among participants in the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis. 2012;60:250–61. doi: 10.1053/j.ajkd.2012.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Freedman BI, Kopp JB, Langefeld CD, et al. The apolipoprotein L1 (APOL1) gene and nondiabetic nephropathy in African Americans. J Am Soc Nephrol. 2010;21:1422–6. doi: 10.1681/ASN.2010070730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Genovese G, Friedman DJ, Pollak MR. APOL1 variants and kidney disease in people of recent African ancestry. Nat Rev Nephrol. 2013;9:240–4. doi: 10.1038/nrneph.2013.34. [DOI] [PubMed] [Google Scholar]
- 32.Pays E, Vanhollebeke B. Human innate immunity against African trypanosomes. Curr Opin Immunol. 2009;21:493–8. doi: 10.1016/j.coi.2009.05.024. [DOI] [PubMed] [Google Scholar]
- 33.Vanhamme L, Paturiaux-Hanocq F, Poelvoorde P, et al. Apolipoprotein L-I is the trypanosome lytic factor of human serum. Nature. 2003;422:83–7. doi: 10.1038/nature01461. [DOI] [PubMed] [Google Scholar]
- 34.Madhavan SM, O’Toole JF, Konieczkowski M, Ganesan S, Bruggeman LA, Sedor JR. APOL1 localization in normal kidney and nondiabetic kidney disease. J Am Soc Nephrol. 2011;22:2119–28. doi: 10.1681/ASN.2011010069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li L, Astor BC, Lewis J, et al. Longitudinal progression trajectory of GFR among patients with CKD. Am J Kidney Dis. 2012;59:504–12. doi: 10.1053/j.ajkd.2011.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Appel LJ, Wright JT, Jr, Greene T, et al. Intensive blood-pressure control in hypertensive chronic kidney disease. N Engl J Med. 2010;363:918–29. doi: 10.1056/NEJMoa0910975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Reeves-Daniel AM, DePalma JA, Bleyer AJ, et al. The APOL1 gene and allograft survival after kidney transplantation. Am J Transplant. 2011;11:1025–30. doi: 10.1111/j.1600-6143.2011.03513.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Freedman BI, Hicks PJ, Bostrom MA, et al. Non-muscle myosin heavy chain 9 gene MYH9 associations in African Americans with clinically diagnosed type 2 diabetes mellitus-associated ESRD. Nephrol Dial Transplant. 2009;24:3366–71. doi: 10.1093/ndt/gfp316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Behar DM, Rosset S, Tzur S, et al. African ancestry allelic variation at the MYH9 gene contributes to increased susceptibility to non-diabetic end-stage kidney disease in Hispanic Americans. Hum Mol Genet. 2010;19:1816–27. doi: 10.1093/hmg/ddq040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Matsha TE, Masconi K, Yako YY, et al. Polymorphisms in the non-muscle myosin heavy chain gene (MYH9) are associated with lower glomerular filtration rate in mixed ancestry diabetic subjects from South Africa. PLoS One. 2012;7(12):e52529. doi: 10.1371/journal.pone.0052529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Foster MC, Coresh J, Fornage M, et al. APOL1 variants associate with increased risk of CKD among African Americans. J Am Soc Nephrol. 2013;24:1484–91. doi: 10.1681/ASN.2013010113. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.