Abstract
Objectives. We compared homeless patients’ experiences of care in health care organizations that differed in their degree of primary care design service tailoring.
Methods. We surveyed homeless-experienced patients (either recently or currently homeless) at 3 Veterans Affairs (VA) mainstream primary care settings in Pennsylvania and Alabama, a homeless-tailored VA clinic in California, and a highly tailored non-VA Health Care for the Homeless Program in Massachusetts (January 2011-March 2012). We developed a survey, the “Primary Care Quality-Homeless Survey," to reflect the concerns and aspirations of homeless patients.
Results. Mean scores at the tailored non-VA site were superior to those from the 3 mainstream VA sites (P < .001). Adjusting for patient characteristics, these differences remained significant for subscales assessing the patient–clinician relationship (P < .001) and perceptions of cooperation among providers (P = .004). There were 1.5- to 3-fold increased odds of an unfavorable experience in the domains of the patient–clinician relationship, cooperation, and access or coordination for the mainstream VA sites compared with the tailored non-VA site; the tailored VA site attained intermediate results.
Conclusions. Tailored primary care service design was associated with a superior service experience for patients who experienced homelessness.
In the United States, homelessness affects more than 1.5 million persons per year and more than 630 000 individuals nightly.1,2 A lack of stable domiciles makes medical care much more challenging, and is associated with increased prevalence of medical and psychiatric conditions3 and mortality.4 Accompanying these challenges is a pattern of excess hospital and emergency department utilization,5 lack of a usual source of care,6 uninsured status,7 and inadequate access to care when needed.8
Health care programs to remediate homeless persons’ challenges in accessing health care began in 1985, when the Robert Wood Johnson Foundation and the Pew Memorial Trust initiated funding for specialized Health Care for the Homeless Programs. In 1987, this funding was assumed by the federal government.9 Since that time, experts have advocated tailoring service design and delivery to assure that high quality care is provided to homeless patients.10–12 However, it is helpful to view tailored service design on a continuum because modifications are diverse and may include a combination of elements, such as outreach workers to develop relationships outside of traditional settings, primary care services in shelters or on the streets, team-based care, co-location of homeless-dedicated primary and mental health providers, special education for providers, capacity to assist with sustenance needs such as food or hygiene items, and a robust consumer role in organizational governance.12–14 Some modified programs have reported improved appointment attendance,15 reductions in hospital admissions, and improvements in disease outcomes.16 However, such modifications are not required of publicly funded homeless primary care providers, and they are not the norm. For example, among 208 federally funded Health Care for the Homeless Programs in 2010, only 15 had designated outreach providers (National Health Care for the Homeless Council, analysis of health resources and services administration uniform data set, unpublished data, 2012). One policy analysis reported that primary care for the homeless remains inadequate, even when insurance is available.17 The Patient Protection and Affordable Care Act (PPACA), coupled with efforts to encourage the Patient-Centered Medical Home model in public and private settings18 lends impetus to efforts to assure that vulnerable populations obtain care that is truly patient-centered.7,19,20
To date, there has been no evaluation of whether efforts to tailor service delivery for homeless clients yield a superior patient experience. Homeless patients’ experiences in primary care are important for several reasons. Patient ratings of their care correlate with whether care relationships are sustained,21 recommendations are adhered to,22 and in some reports, whether behavioral conditions improve.23,24 Also, as emphasized by developers of other primary care rating tools,25,26 patients are the optimum reporters of whether primary care delivery fulfills the desired attributes described by the Institute of Medicine and others,27,28 including accessibility, comprehensiveness, continuity, ease of communication, and sensitivity to context.29
Our study compares patients' assessments of their own care across 5 primary care settings that varied in the degree of homeless-tailored service design, from none (i.e., “mainstream primary care”) to intensive tailoring. Given the lack of a population-specific survey, we developed a new patient-reported instrument specifically for homeless persons. We hypothesized that ratings would be superior for care obtained in settings that tailored services for homeless clientele. Because homeless patients have reported significant negative experiences in care,30,31 our secondary hypothesis was that unfavorable experiences would be more common in mainstream primary care compared with tailored settings.
METHODS
This study entailed a survey-based comparison of patient experiences of primary care at 5 federally funded sites (4 within the US Department of Veterans Affairs [VA] and 1 funded through the Department of Health and Human Services) that differed in the degree to which primary care service delivery was tailored for the homeless. The assessment of patient-perceived primary care was administered as part of a 40 to 60 minute survey battery conducted face-to-face by research associates at each site from January 2011 through March 2012. Participants received a single payment of $20 for their time.
Sites
To test the primary hypothesis, we selected 5 sites with (1) variation in service tailoring characteristics (based both on investigator direct knowledge supplemented by interviews with staff), (2) adequately sized panels of currently or recently homeless patients, and (3) the presence of a local investigative team capable of conducting a random sampling and survey methodology. The sites differed in service design and delivery in ways that the literature and clinical experience suggested could be important to homeless care (Figure 1 and Table 1).10,12 Notably, 3 were traditional primary care operations (in Pennsylvania and Alabama) within VA settings where most primary care occurred in standard clinics serving homeless and housed patients alike without unique staff or other resources (mainstream VA A, mainstream VA B, and mainstream VA C). Among these, mainstream VA A was a multisite health system that included, for some patients, primary care provided in shelters and a VA domiciliary. Because of the minimal provision of primary care services outside standard clinics and the absence of additional tailoring modifications, we classified this site as mainstream. The remaining 2 sites offered tailored services; one was a VA site (CA), and the other was a non-VA site (MA). The tailored non-VA site was a 26-year old Health Care for the Homeless (HCH) Program32 that provided care in streets, shelters, and hospital-based clinics, with a specialized electronic record system, homeless-focused medical and nursing staff, as well as representation of homeless and formerly homeless persons in governing and advisory bodies. The tailored VA site, which began operations in 2002, was designed and funded specifically for homeless patients, including co-located mental health and primary care, with an emphasis on access without scheduling delay.33a
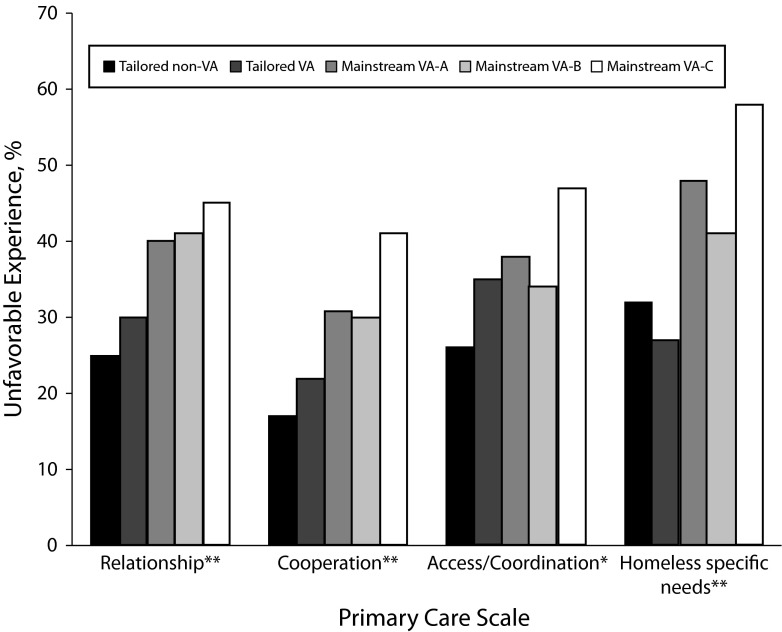
FIGURE 1—
Unfavorable experiences in primary care, among persons receiving primary care in 5 different primary care programs, January 2011–March 2012.
Note. VA = US Department of Veterans Affairs. Unfavorable experience was defined based on the number of “frankly unfavorable” responses falling into the highest tertile observed for that particular scale (i.e., agree or strongly agree with a negatively worded item, or disagree or strongly disagree with a positively worded item). The highest tertile for unfavorable responses was found to be 2 or more frankly unfavorable responses for the relationship, cooperation and access/coordination scales, and 1 or more frankly unfavorable responses for the homeless-specific needs scale. Tailored non-VA refers to a 26-year old Health Care for the Homeless Program. Mainstream VA sites are non-tailored primary care sites in Pennsylvania (A), and Alabama (B and C). Tailored VA is a VA homeless-tailored primary care program (California).
*P < .05; **P < .01.
TABLE 1—
Variation in Degree of Primary Care Service Tailoring in Tailored vs Nontailored Care Programs: 5 Study Sites, January 2011–March 2012
| Primary Care Service Design Characteristics | Mainstream VA B Mainstream VA C (Alabama) | Mainstream VA A (Pennsylvania) | Tailored VA (California) | Tailored Non-VA (Massachusetts) |
| Explicit homeless mission | X | X | ||
| Primary care in shelters and streets | X | X | ||
| Team design assures continuity from streets/shelters to clinic | X | |||
| Formal relationships to community shelters | X | X | ||
| Homeless-focused staff training | X | X | ||
| PC and mental health in same clinical space | X | X | X | |
| PC clinic equipped to directly meet tangible needsa | ||||
| Linkage to national homeless organizations | X | |||
| Formerly homeless persons in organizational governance | X | |||
| > 10 y explicit homeless mission focus | X |
Note. PC = primary care; VA = Veterans Affairs. Tailored non-VA refers to a 26-year old Health Care for the Homeless Program. Mainstream VA sites are non-tailored primary care sites in Pennsylvania (A), and Alabama (B and C). Tailored VA is a VA homeless-tailored primary care program (California). Characteristics pertain to the design of the primary care service utilized by study participants. Survey questions defined primary care as the person or team seen for a check-up or for a general medical problem when it is not an emergency. By design, recruitment was initiated only with persons who had recorded evidence of 2 or more primary care visits. An X indicates the characteristic pertains to the primary care service utilized. Thus “clinic equipped to directly meet tangible needs” is designated only when the primary care site utilized by patients was specifically equipped to directly meet such needs, and not designated if such a service was available elsewhere in the same hospital-based system of care.
Such as clothing and food.
Recruitment
Recruitment was designed to obtain a random sample of homeless-experienced, English-speaking persons who received primary care from each site of care. An automated query of records was used to identify persons with (1) presumptive past or current homelessness and (2) receipt of primary care at the site of care 2 or more times in the past 2 years. In the 4 VA sites, presumptive past or current homelessness was based on an International Classification of Diseases-9-CM code of V60.0 (i.e., homeless) diagnosis.33b In the tailored non-VA site, past or current homelessness was based on utilization of the site for care. A random subset at each site was targeted for recruitment, with the number targeted based on consideration of (1) number of homeless served at the site and (2) numbers necessary to identify differences in satisfaction with sufficient power. Entry was further restricted based on the respondent verbally affirming receipt of primary care at the site of interest. Across all 5 sites, 6371 persons met the criteria from July 1, 2008, to June 30, 2010. After random selection, 2584 (41%) were subject to recruiting, 870 (14%) were successfully contacted and screened, 634 (10%) entered the study, and 601 (9.4%) were included in analysis. Of the 33 entrants excluded from analysis, 19 did not receive care at the site, 1 had a mistaken identity, 1 had prohibitive behavioral issues, 1 refused to sign a Health Insurance Portability and Accountability Act consent, and 11 had survey administration that was compromised (e.g., stopped because of competing appointment; data available as a supplement to the online version of this article at http://www.ajph.org).
The Primary Care Quality-Homeless Survey
Although patient-reported primary care assessments exist,34,35 there is no standard survey instrument to assess primary care for homeless populations. Because research has shown that the concerns, priorities, and aspirations of homeless patients can differ from those in mainstream populations,36,37 we developed a new instrument, the Primary Care Quality-Homeless (PCQ-H) Survey.
A 2-year qualitative research process began with review of 2 Institute of Medicine reports27,38 to define major constructs relevant to primary care quality. These constructs were explored in semistructured interviews with 36 homeless-experienced patients and 22 experts in homeless health care. Based on interview coding, we developed a preliminary set of 78 items. After administration to all study participants, items were submitted to factor analysis to identify groups of items measuring distinct domains, and then within domains, item response theory (2 parameter graded response analysis39) was applied to identify a subset of these items that was optimally discriminating for and adequately covered the range of responses for each domain. Items that were psychometrically equivalent and did not address conceptually unique aspects of the measured domains were dropped. The resulting 33-item PCQ-H Survey consisted of 4 scales: (1) patient–clinician relationship (15 items), (2) cooperation among clinicians (3 items), (3) accessibility or coordination (11 items), and (4) homeless-specific needs (4 items; data available as a supplement to the online version of this article at http://www.ajph.org).
Each item on the survey is a simple statement regarding the primary care provider or the site or program where the client obtained primary care (e.g., “My primary care provider makes sure health care decisions fit with the other challenges in my life”), scored on a 4-point Likert scale with reverse-coding for negatively worded items. Averaging the responses generated a subscale score from 1 (least favorable) to 4 (most favorable).
Covariates
To more accurately compare ratings of primary care across sites, our analysis controlled for a range of patient characteristics. These characteristics were selected on the basis of existing empirical literature regarding patient-level predictors of satisfaction40–42 and characteristics identified by the Behavioral Model for Vulnerable populations43 (which predicts service use among the homeless8,44,45).
Items related to residential status were drawn from previous work focused on residence in the past 2 weeks,46–48 homelessness in the past 6 months,49 and questions to assess whether the person had been “chronically homeless” in the past 3 years (≥ 4 episodes in 3 years or a period longer than 1 year).50,51 Health status was measured by the single-item general self-reported health question, which was shown to strongly predict both mortality and health care utilization.52,53 Psychiatric symptoms were assessed with the 14-item Colorado Symptom Index.54 In some models, a binary indicator of “severe psychiatric symptoms” was based on affirming any 1 of the following experiences several times per week or more: being told one acted suspicious or paranoid; hearing voices others could not hear, feeling suspicious or paranoid, or feeling like hurting or killing oneself or another (a safety algorithm included clinical response to persons affirming this item). Substance use measures came from the World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) 3.0.55
Analysis
Analysis proceeded in 3 phases. First, respondents participating at the 5 recruitment sites were compared with respect to a range of demographic, health, and health service utilization measures using analysis of variance for continuous variables and the χ2 test for categorical variables. Second, continuous PCQ-H scores were compared across sites, first without covariate adjustment and then controlling for case mix, including all covariates in a multiple linear regression model. Because the recruitment strategy risked enriching the sample with “more stable” or “less vulnerable” homeless-experienced persons, analyses included a priori plans to assess for differences within stratified groups: persons with a history of chronic homelessness; persons with fair or poor general health status; and persons with current severe psychiatric symptoms. Last, in light of the interest in reducing negative experiences in homeless persons’ health care, we developed a categorical “unfavorable experience” indicator based on the number of unfavorable responses in the top tertile (33%) for each subscale, analogous to bottom-box scoring. An unfavorable response would be agree or strongly agree with a negative item (e.g., “It is often difficult to get health care at this place”) or disagree or strongly disagree with a positive item (e.g. “My primary care provider takes my health concerns seriously”). We used the χ2 test to compare the prevalence of unfavorable experiences, adjusting for case mix with multiple logistic regression. All site comparison analyses were conducted using SAS versions 9.2 and 9.3 (SAS Institute, Cary, NC), whereas factor analyses were completed with MPlus version 6.12,56 and item response theory analyses utilized the R module ltm.57
RESULTS
Participants were mostly men (85%), with a mean age of 53 years (±8.3 years). Sixty-eight percent reported it was hard to pay for basic necessities like food and shelter (Table 2). Overall, 70% had met temporal criteria for chronic homelessness in the previous 3 years (an episode > 1 year, or ≥ 4 times in 3 years). As might be expected given the recruitment approach (mail and telephone contact), literal homelessness in the 6 months before study participation (e.g., any nights on the streets or in shelters) was less common (24% overall).
TABLE 2—
Characteristics of Participants by Site in a Comparison of Homeless Persons’ Care in Tailored vs Nontailored Care Programs: 5 Study Sites, January 2011–March 2012
| Characteristics | Tailored Non-VA (Massachusetts, n = 195), No. (%) or Mean ±SD | Tailored VA (California, n= 94), No. (%) or Mean ±SD | Mainstream VA A (Pennsylvania, n = 124), No. (%) or Mean ±SD | Mainstream VA B (Alabama, n = 150), No. (%) or Mean ±SD | Mainstream VA C (Alabama, n = 38), No. (%) or Mean ±SD | Pa | |
| Demographics | |||||||
| Age, y | 51.1 ±10.5 | 55.9 ±6.8 | 53.6 ±6.9 | 53.7 ±7.1 | 50.9 ±9.6 | < .001 | |
| Gender | |||||||
| Male | 133 (68.2) | 94 (100) | 112 (90.3) | 139 (92.7) | 34 (89.5) | < .001 | |
| Female | 59 (30.3) | 0 | 11 (8.9) | 11 (7.3) | 4 (10.5) | ||
| Other/transgender | 3 (1.5) | 0 | 1 (0.8) | 0 | 0 | ||
| Race | |||||||
| Hispanic, Latino, or Spanish origin | 20 (10.5) | 6 (06.5) | 2 (1.6) | 1 (0.7) | 0 (0.0) | < .001 | |
| White | 77 (39.5) | 13 (13.8) | 49 (39.5) | 33 (22.0) | 12 (31.6) | < .001 | |
| Black, African American | 75 (38.5) | 73 (77.7) | 66 (53.2) | 111 (74.0) | 21 (55.3) | ||
| American Indian/Alaska Native | 2 (01.0) | 1 (01.1) | 5 (4.0) | 1 (0.7) | 2 (5.3) | ||
| Asian/Pacific Islander | 2 (01.0) | 1 (01.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Other | 39 (20.0) | 5 (06.4) | 4 (3.2) | 5 (3.3) | 3 (7.9) | ||
| Race non-White | 119 (61.0) | 81 (86.2) | 75 (60.5) | 117 (78.0) | 26 (68.4) | < .001 | |
| Ever served in military | 27 (14.4) | 94 (100) | 124 (100) | 150 (100) | 38 (100) | < .001 | |
| Difficulty paying for basic necessities | 63 (67.7) | 123 (67.7) | 84 (68.9) | 97 (66.9) | 27 (77.1) | .823 | |
| Residential history | |||||||
| Chronically homeless in past 3 y | 164 (84.1) | 68 (72.3) | 67 (54.0) | 85 (56.7) | 21 (55.3) | < .001 | |
| Spent ≥ 1 nights in street, in car or abandoned building or in emergency shelters, last 2 wk | 37 (18.7) | 7 (7.5) | 10 (8.1) | 14 (9.3) | 1 (2.6) | .002 | |
| Self-designates as currently homeless | 61 (31.3) | 27 (29.0) | 33 (26.6) | 50 (33.3) | 14 (36.8) | .685 | |
| Currently domiciled, last 2 wkb | 117 (60.0) | 57 (60.6) | 92 (74.2) | 88 (58.7) | 23 (60.5) | .064 | |
| Health services | |||||||
| Health insurancec | 181 (92.8) | 83 (88.3) | 106 (85.5) | 141 (94.0) | 33 (86.8) | .078 | |
| “How many times have you seen this provider in last 6 months?” | 4.7 ±5.1 | 2.3 ±1.8 | 1.6 ±1.2 | 3.3 ±6.8 | 2.2 ±2.3 | < .001 | |
| Health status | |||||||
| General health status fair or poor | 89 (46.6) | 35 (38.0) | 48 (39.0) | 66 (44.3) | 18 (47.4) | .539 | |
| Psychiatric symptom intensity in last 6 mo, Colorado (range = 0–56)d | 16.6 ±11.1 | 15.8 ±10.6 | 15.2 ±10.6 | 17.6 ±12.4 | 25.3 ±11.6 | < .001 | |
| Severe psychiatric symptoms several times per wkd | 40 (20.9) | 21 (22.3) | 18 (14.6) | 50 (34.0) | 16 (42.1) | < .001 | |
| Drug Global Continuum Score (ASSIST)e | 27.6 ±27.2 | 23.8 ±18.8 | 25.0 ±23.9 | 18.6 ±15.4 | 19.8 ±18.2 | .005 | |
| Alcohol Specific Substance Involvement Score (ASSIST),e | 9.8 ±9.9 | 5.8 ±6.5 | 7.5 ±8.3 | 18.6 ±15.4 | 8.5 ±8.3 | < .004 | |
Note. VA = Veterans Affairs. Tailored non-VA refers to a 26-year old Health Care for the Homeless Program. Mainstream VA sites are non-tailored primary care sites in Pennsylvania (A), and Alabama (B and C). Tailored VA is a VA homeless-tailored primary care program (California).
P values are based on comparison among the 5 sites using the χ2 test (categorical) or analysis of variance (continuous).
“Currently domiciled” was designated for persons reporting at least 1 night during the past 2 weeks in their “own apartment/house” or in “permanent supportive housing provided by an organization or the government.”
Insured status included affirmation of having “a source of insurance that can pay for your medical expenses,” including private insurance, Medicare, Medicaid, or VA benefits.
Psychiatric symptoms probed using previously validated Colorado Symptom Index.48 “Severe” symptoms were being told one acted suspicious or paranoid, hearing voices others could not hear, feeling suspicious or paranoid, feeling like hurting or killing oneself or another person.
Scores related to drug and alcohol use were devised from the World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST).49
Nearly half the participants characterized their general health as fair or poor (43.1%) compared with 9.6% of Americans in the general population.58 Severe psychiatric symptoms several times per week were common (24.5%), especially among participants at mainstream site VA C (42.1%).
For each of the 4 subscales assessed, PCQ-H mean scores (rang = 1–4) were as low (unfavorable) as 2.43 and as high (favorable) as 3.32, with standard deviations ranging from 0.35 (relationship) to 0.6 (cooperation).
Comparison of Primary Care Quality-Homeless Continuous Scores
Comparisons of unadjusted mean PCQ-H scores across the 5 sites showed that scores differed on all 4 subscales (patient–clinician relationship and cooperation, P < .001; accessibility or coordination, P = .024; and homeless-specific needs, P = .033). Specifically, scores at the tailored non-VA site were higher (reflecting more positive experience with care) than those at the 3 mainstream VA sites. The tailored VA site generally had scores that were either similar to those of the 3 mainstream VA sites or somewhat higher, depending on the subscale of interest. The mainstream VA 3 had consistently lower scores, often close to a full SD below the tailored VA site, which was a large effect size.
Adjusting for patient characteristics, differences remained significant for the relationship (P < .001) and cooperation (P = .005) subscales, whereas they fell short of statistical significance in the case of access or coordination (P = .055) and homeless-specific needs (P = .21).
As shown in Table 3, the magnitude of difference favoring the tailored non-VA site over mainstream VA B site was 0.25 to 0.50 SD for relationship and cooperation, which was a small to moderate effect size. The magnitude of difference was more modest in comparison with the mainstream VA A site (because it performed better) and more pronounced in comparison with the mainstream VA C site (which performed worse).
TABLE 3—
Comparison of Primary Care Quality-Homeless Scores by Site of Care in Tailored vs Nontailored Care Programs: January 2011–March 2012
| Tailored, Mean ±SD, Mean (SE), or OR (95% CI) |
Mainstream, Mean ±SD, Mean (SE), or OR (95% CI) |
||||||
| Scores | No. | Tailored Non-VA | Tailored VA | Mainstream VA A | Mainstream VA B | Mainstream VA C | Pa |
| Subscale scores, unadjusted | |||||||
| Relationship | 600 | 3.32 ±0.41 | 3.28 ±0.46 | 3.28 ±0.55 | 3.13 ±0.49 | 2.95 ±0.49 | < .001b |
| Cooperation | 566 | 2.97 ±0.52 | 2.85 ±0.82 | 2.81 ±0.82 | 2.75 ±0.70 | 2.43 ±0.62 | < .001b |
| Access/coordination | 600 | 3.17 ±0.40 | 3.10 ±0.48 | 3.15 ±0.53 | 3.12 ±0.44 | 2.90 ±0.39 | .024c |
| Homeless-specific needs | 596 | 3.17 ±0.46 | 3.17 ±0.49 | 3.05 ±0.60 | 3.05 ±0.51 | 2.96 ±0.50 | .033 |
| Subscale scores, adjustedd | |||||||
| Relationship | 551 | 3.45 (0.09) | 3.38 (0.10) | 3.37 (0.09) | 3.26 (0.09) | 3.07 (0.12) | < .001 |
| Cooperation | 522 | 3.15 (0.13) | 2.96 (0.15) | 2.93 (0.14) | 2.89 (0.14) | 2.71 (0.18) | .005 |
| Access/coordination | 551 | 3.29 (0.08) | 3.19 (0.10) | 3.24 (0.09) | 3.24 (0.09) | 3.03 (0.11) | .055 |
| Homeless-specific needs | 547 | 3.38 (0.09) | 3.38 (0.11) | 3.25 (0.10) | 3.31 (0.10) | 3.26 (0.13) | .209 |
| Unfavorable experiencede | |||||||
| Relationship | 551 | Ref | 1.84 (0.96, 3.54) | 2.60 (1.49, 4.56) | 2.57 (1.48, 4.47) | 2.38 (1.03, 5.48) | .005 |
| Cooperation | 522 | Ref | 1.87 (0.88, 4.00) | 2.73 (1.46, 5.09) | 2.73 (1.45, 5.14) | 2.70 (1.06, 6.84) | .01 |
| Access/coordination | 551 | Ref | 2.36 (1.22, 4.57) | 2.50 (1.42, 4.41) | 1.96 (1.11, 3.46) | 2.38 (1.02, 5.56) | .018 |
| Homeless-specific needs | 547 | Ref | 0.96 (0.51, 1.81) | 2.15 (1.27, 3.63) | 1.45 (0.87, 2.44) | 1.90 (0.85, 4.28) | .021 |
Note. CI = confidence interval; OR = odds ratio; VA = Veterans Affairs. Tailored non-VA refers to a 26-year old Health Care for the Homeless Program. Mainstream VA sites are non-tailored primary care sites in Pennsylvania (A), and Alabama (B and C). Tailored VA is a VA homeless-tailored primary care program (California).
In unadjusted comparisons, the P value is from an overall test for significant differences among the 5 included sites. In the 2 adjusted analysis, the P value reflects a test of whether the site (5 categories, degrees of freedom = 4) was significant after controlling for variables detailed under footnote b.
Post hoc tests revealed significant pairwise differences between tailored non-VA and mainstream VA B; tailored non-VA and mainstream VA C; tailored VA and mainstream VA C; and mainstream VA A and mainstream VA C.
Post hoc tests revealed significant pairwise differences between tailored non-VA and mainstream VA C; and mainstream VA A and mainstream VA C.
Adjusted analyses control for age, gender, Black race, having had one’s own domicile (apartment or house) in past 2 weeks, psychiatric symptoms (Colorado score), drug and alcohol risk scores on the World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST), general self-reported health, and low income status.
Unfavorable experience was defined based on the number of “frankly unfavorable” responses falling into the highest tertile observed for that particular scale (i.e., agree or strongly agree with a negatively worded item, or disagree or strongly disagree with a positively worded item). The highest tertile for unfavorable responses was found to be 2 or more unfavorable responses for the relationship, cooperation and access/coordination scales, and 1 or more unfavorable responses for the homeless-specific needs scale.
Adjusted differences among the sites were of similar magnitude and statistically significant after restriction to subgroups defined by history of chronic homelessness or fair or poor general health status (data available as a supplement to the online version of this article at http://www.ajph.org). The tailored VA site typically attained an intermediate position in these comparisons.
Comparison of Categorical “Unfavorable Experience” Indicator
Finally, an unfavorable experience was 1.5 to 2 times more common at the mainstream VA sites compared with the tailored non-VA site (all P < .01 in unadjusted χ2 comparisons), and these contrasts remained statistically significant after adjusting for patient characteristics for the relationship, cooperation, and access or coordination scales. Analyses comparing the tailored VA site with the tailored non-VA site obtained an intermediate result. Specifically, patients at the tailored VA site were more likely than patients at the tailored non-VA site to have an unfavorable experience on the access or coordination subscale, but not with the other 3 subscales.
DISCUSSION
We tested the hypothesis that homeless-experienced patients would rate their primary care experience more highly when care was obtained in settings that explicitly tailored services for this population through variations in service design (Table 1). This hypothesis was supported by our results, both in comparison of mean scores from the PCQ-H subscales, and in the likelihood of a categorical outcome indicating an unfavorable experience in primary care.
Patient experiences are typically influenced by patient, provider, and environmental characteristics.29 Despite the range of characteristics that could dilute detection of an effect from tailored service design, survey scores for patient–clinician relationship and perceptions of cooperation among providers were highest where homeless-tailoring was most pronounced. The comparison of “unfavorable experiences” produced a more striking contrast. For 3 subscales (relationship, cooperation, and access or coordination), such unfavorable experiences were 1.5 to 2 times more frequent in the 3 mainstream settings. The tailored VA site obtained results that were, on whole, intermediate, which often lined up with the 2 better performing mainstream VA sites (in analyses of mean scores), and were sometimes more like the tailored non-VA site (e.g., for unfavorable experience on items related to relationship, cooperation, and homeless-specific needs).
A review of study sites (Table 1) underscored that service tailoring was not all-or-none, but rather could be viewed on a continuum. The tailored VA site had fewer elements of tailoring than the tailored non-VA site, and attained ratings that were, on the whole, intermediate between the mainstream VA sites and the tailored non-VA site. The mainstream VA A site offered some shelter-based and domiciliary-based primary care for a subset of patients, which was also a potential element of tailored service design.
Tradeoffs characterize the question of whether to prioritize mean score comparisons versus a categorical unfavorable experience. We believe both are useful. As noted for the widely used Consumer Assessment of Health Plans,59 mean scores are more precise in capturing performance relative to average, but experience the downside that scores are compressed in a small part of the available range and could be hard for consumers to interpret. Conversely, categorical results better illustrated important outcomes to consumers, although they sacrificed precision.59 In this study, both sets of results aligned with the expectation that high levels of tailoring were associated with a better experience. Importantly, however, we could make no claim to a correlation between improved patient experiences with any medical outcome, such as decreased morbidity or mortality. Health improvements might only be demonstrable through study of persons whose poor experiences led to disengagement from primary care, a group we were not positioned to study.
Limitations and Strengths
This study had limitations. First, individuals were not randomly assigned to clinics. Thus, it was possible that some characteristics of the patients or the 5 clinical settings, other than service tailoring, could account for the results. It could be speculated that VA facilities delivered a less patient-friendly experience than non-VA organizations. However, the higher quality reported from the VA in comparison with the private sector settings,60 coupled with VA satisfaction ratings similar to those from commercial insurance,61 made this less plausible. Similarly, although homeless veterans differed from homeless nonveterans in some samples, the differences were not systematic and consistent across studies.62 Ultimately, more robust efforts to disentangle potential VA-specific influences await research from a wider range of VA and non-VA care settings.
We measured and adjusted for several patient characteristics, but it can be assumed that other environmental factors influenced results. For example, the 38 participants at the mainstream VA C site offered considerably lower ratings. Because that facility included a regional psychiatric and rehabilitative facility, it was conceivable that aspects of its referral pattern differed in ways not captured by our measures or by the homeless-tailoring concept.
Second, by studying 4 VA sites and a health center in Massachusetts, few in the sample lacked financial coverage for care, and questions concerning financial access might have been less informative. Because financial barriers arise elsewhere,63 we believed these items might prove helpful in other settings.
Lastly, recruitment utilized a random record query, with initial contact often via telephone or mail. Although reducing a bias toward “happy customers” obtained with waiting room samples, our sample was dominated by persons who were homeless-experienced rather than homeless at the time of the survey. Because results favoring tailored care were more pronounced among vulnerable subgroups (i.e., persons who met the federal chronic homeless definition, or persons in fair or poor health), we believed this was not a severe limitation.
Alongside limitations, our study had strengths in the breadth of characteristics assessed and statistically adjusted, and in randomly sampling a population that could be challenging to recruit. Finally, our might be the first to utilize homeless patients in every aspect of questionnaire design. The resulting 33-item instrument might be useful with homeless and potentially other vulnerable populations facing challenges to obtaining high-quality primary care.30,36,64
Implications for Primary Care Settings
Understanding how specific organizational characteristics affect patients’ primary care experiences will require further research. However, some speculation could be offered regarding the relationship and cooperation subscales, in which differences were most pronounced. Patient perceptions of cooperation among caregivers might be influenced by actual co-location of services (e.g., primary medical, mental, social work) as well as demonstration that team members actually communicated with each other in ways that went beyond the medical record. Communication might become evident to patients when they see providers speaking with each other, when providers mention each other by name, or when they describe conversations with other team members. Such events might occur more readily and be most apparent to patients when care is delivered in distinct mission-driven teams, as in the 2 tailored settings. Items that scaled together as the “relationship” subscale encompassed aspects of communication and trust. In mainstream settings, homeless patients might feel either mistrusted or unwelcome.30 Tailored clinics might remediate these challenges in part by recruiting providers who wish to work with the homeless population. Mutual support and mentorship might be more readily fostered among like-minded professionals, so that challenges to the clinical relationship (e.g., a lost prescription, a missed appointment) are handled constructively.
Implications for Health Care Policy
A recent policy analysis found that the dominant mainstream model for delivering primary care to homeless individuals is not adequate, but little empirical evidence exists to guide selection of a superior approach.17 Both the US Department of Veterans Affairs and the US Department of Health and Human Services support some tailored programs focused on the primary care of homeless individuals, and they have the wherewithal to encourage tailored approaches to care, to the degree that evidence in their favor is persuasive. Patient reports of their own experiences offer important evidence in favor of expanding these tailored approaches.
More broadly, these findings have implications for how health care system changes may affect homeless patients, many of whom will become eligible for Medicaid under the PPACA. The Act funds payment and delivery arrangements across insurers, and implements demonstration projects that seek to improve quality and accountability. However, identifying the optimum mechanism to assure good care experiences for vulnerable patient populations remains a key challenge. Federally Qualified Health Centers, which PPACA expands, have in recent years been encouraged to seek recognition as Patient-Centered Medical Homes according to national criteria.65 A number of criteria embody principles of practice adopted by homeless-tailored programs, including an emphasis on coordination, accessibility, and individualizing care to patient needs and circumstances.12–14,66 In this regard, the experience of successful homeless primary care programs could inform policymakers dedicated to vulnerable patient populations. The present study suggests that tailored service delivery matters to patients in ways that are readily measurable. Future work will be needed to learn which aspects of service tailoring matter most, and whether they are easily translated across service environments for both homeless and nonhomeless patient populations.
Acknowledgments
Research was funded by the Department of Veterans Affairs, Health Services Research & Development Branch (Grant IAA-07-069-2). E. Stringfellow received additional support from the National Institute on Drug Abuse (T32DA01035).
Although we had no commercial conflicts of interest, we want to acknowledge that most of the authors, except for J. F. Jones, C. L. Holt, and D. E. Pollio, have been employed or are currently employed by institutions studied in this articles (4 VA hospitals, and 1 independent nonprofit Health Care for the Homeless Program).
Preliminary versions of the findings in this article were previously presented at the Annual Meetings of the Society of General Internal Medicine (2012, 2013), the VA Health Services Research and Development Conference (2012), the Annual Conference of the American Public Health Association (2012), and Academy Health (2012).
We would like to thank Carol Ashton, Joshua Richman, Alison Borden, John D. Harding, Lori Henault, Jane Liebschutz, Sonia Schwartz, Dawn Glover, John Andrew Young, and Calvin Elam for their assistance in the design or execution of this study.
Note. The opinions expressed are those of the authors and do not represent the positions of the Department of Veterans Affairs or any other entity of the United States federal government.
Human Participant Protection
Research was conducted under the approval of 5 separate institutional review boards at the 5 included study sites. We affirm that the research was conducted in keeping with the Principles of the Ethical Practice of Public Health.
References
- 1.Burt MR, Aron LY, Lee E, Valente J. Helping America’s Homeless: Emergency Shelter or Affordable Housing? Washington, DC: The Urban Institute Press; 2001. [Google Scholar]
- 2. United States Department of Housing and Urban Development. 2012 Point-in-Time Estimates of Homelessness: Volume 1 of the 2012 Annual Homeless Assessment Report. 2012. Available at: http://www.onecpd.info/resource/2753/2012-pit-estimates-of-homelessness-volume-1-2012-ahar. Accessed December 26, 2012.
- 3.Kleinman LC, Freeman H, Perlman J, Gelberg L. Homing in on the homeless: assessing the physical health of homeless adults in Los Angeles County using an original method to obtain physical examination data in a survey. Health Serv Res. 1996;31(5):533–549. [PMC free article] [PubMed] [Google Scholar]
- 4.O’Connell JJ. Premature Mortality in Homeless Populations: A Review of the Literature. Nashville: National Health Care for the Homeless Council; 2005. [Google Scholar]
- 5.Salit SA, Kuhn EM, Hartz AJ, Vu JM, Mosso AL. Hospitalization costs associated with homelessness in New York City. N Engl J Med. 1998;338(24):1734–1740. doi: 10.1056/NEJM199806113382406. [DOI] [PubMed] [Google Scholar]
- 6.Gallagher TC, Andersen RM, Koegel P, Gelberg L. Determinants of regular source of care among homeless adults in Los Angeles. Med Care. 1997;35(8):814–830. doi: 10.1097/00005650-199708000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Washington, DC: The Henry J. Kaiser Family Foundation; 2012. Kaiser Commission on Medicaid and the Uninsured. Medicaid Coverage and Care for the Homeless Population: Key Lessons to Consider for the 2014 Medicaid Expansion. [Google Scholar]
- 8.Baggett TP, O’Connell JJ, Singer DE, Rigotti NA. The unmet health care needs of homeless adults: a national study. Am J Public Health. 2010;100(7):1326–1333. doi: 10.2105/AJPH.2009.180109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Health Care for the Homeless Council. Frequently Asked Questions About Health Care for the Homeless. Nashville, TN: NHCHC; 2011. [Google Scholar]
- 10.Brickner PW, Scanlan BC, Conanan B et al. Homeless persons and health care. Ann Intern Med. 1986;104(3):405–409. doi: 10.7326/0003-4819-104-3-405. [DOI] [PubMed] [Google Scholar]
- 11.Brickner PW, Scharer LK, Conanan BA, Savarese M, Scanlan BC. Under the Safety Net: The Health and Social Welfare of the Homeless in the United States. New York, NY: W.W. Norton & Co.; 1990. [Google Scholar]
- 12.McMurray-Avila M, Gelberg L, Breakey WR. Balancing act: clinical practices that respond to the needs of homeless people. In: Fosburg LB, Dennis DL, eds. The 1998 National Symposium on Homelessness Research, 1998. Arlington, VA: US Department of Health and Human Services and Department of Housing and Urban Development; 1999:8-1–8-49. [Google Scholar]
- 13.O’Connell JJ. Dying in the shadows: the challenge of providing health care for homeless people. CMAJ. 2004;170(8):1251–1252. doi: 10.1503/cmaj.1040008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brickner PW. Health Care of Homeless People. New York, NY: Springer Publishing Co.; 1985. [Google Scholar]
- 15.Henry R. Los Angeles, CA: University of California Los Angeles School of Public Health; 2006. Determinants of appointment keeping by veterans with hypertension [dissertation] [Google Scholar]
- 16.O’Toole TP, Buckel L, Bourgault C et al. Applying the chronic care model to homeless veterans: can a population approach to primary care impact utilization and clinical outcomes? Am J Public Health. 2010;100(12):2493–2499. doi: 10.2105/AJPH.2009.179416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shortt SE, Hwang S, Stuart H, Bedore M, Zurba N, Darling M. Delivering primary care to homeless persons: a policy analysis approach to evaluating the options. Healthc Policy. 2008;4(1):108–122. [PMC free article] [PubMed] [Google Scholar]
- 18.Ku L, Shin P, Jones E, Bruen B. Transforming Community Health Centers into Patient-Centered Medical Homes: The Role of Payment Reform. New York, NY: The Commonwealth Fund; 2011. [Google Scholar]
- 19.Washington, DC: Health Resources and Services Administration; 2011. Health Resources and Services Administration. Program Assistance Letter: HRSA Patient-Centered Medical/Health Home Initiative. [Google Scholar]
- 20.Piette J, Holtz B, Beard A et al. Improving chronic illness care for veterans within the framework of the Patient-Centered Medical Home: experiences from the Ann Arbor Patient-Aligned Care Team Laboratory. Behav Med Pract Policy Res. 2011;1(4):615–623. doi: 10.1007/s13142-011-0065-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Safran DG, Montgomery JE, Chang H, Murphy J, Rogers WH. Switching doctors: predictors of voluntary disenrollment from a primary physician’s practice. J Fam Pract. 2001;50(2):130–136. [PubMed] [Google Scholar]
- 22.Roumie CL, Greevy R, Wallston KA et al. Patient centered primary care is associated with patient hypertension medication adherence. J Behav Med. 2011;34(4):244–253. doi: 10.1007/s10865-010-9304-6. [DOI] [PubMed] [Google Scholar]
- 23.Kim TW, Samet JH, Cheng DM, Winter MR, Safran DG, Saitz R. Primary care quality and addiction severity: a prospective cohort study. Health Serv Res. 2007;42(2):755–772. doi: 10.1111/j.1475-6773.2006.00630.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levy BD, O’Connell JJ. Health care for homeless persons. N Engl J Med. 2004;350(23):2329–2332. doi: 10.1056/NEJMp038222. [DOI] [PubMed] [Google Scholar]
- 25.Safran DG. Defining the future of primary care: what can we learn from patients? Ann Intern Med. 2003;138(3):248–255. doi: 10.7326/0003-4819-138-3-200302040-00033. [DOI] [PubMed] [Google Scholar]
- 26.Starfield B, Cassady C, Nanda J, Forrest CB, Berk R. Consumer experiences and provider perceptions of the quality of primary care: implications for managed care. J Fam Pract. 1998;46(3):216–226. [PubMed] [Google Scholar]
- 27.Committee on the Future of Primary Care for the Institute of Medicine. Primary Care: America’s Health in a New Era. Washington, DC: National Academy Press; 1996. [Google Scholar]
- 28.Starfield B. Primary Care: Balancing Health Needs, Services, and Technology. New York, NY: Oxford University Press; 1998. [Google Scholar]
- 29.Sofaer S, Firminger K. Patient perceptions of the quality of health services. Annu Rev Public Health. 2005;26:513–559. doi: 10.1146/annurev.publhealth.25.050503.153958. [DOI] [PubMed] [Google Scholar]
- 30.Wen CK, Hudak PL, Hwang SW. Homeless people’s perceptions of welcomeness and unwelcomeness in healthcare encounters. J Gen Intern Med. 2007;22(7):1011–1017. doi: 10.1007/s11606-007-0183-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Martins DC. Experiences of homeless people in the health care delivery system: a descriptive phenomenological study. Public Health Nurs. 2008;25(5):420–430. doi: 10.1111/j.1525-1446.2008.00726.x. [DOI] [PubMed] [Google Scholar]
- 32.O’Connell JJ, Oppenheimer SC, Judge CM et al. The Boston Health Care for the Homeless Program: a public health framework. Am J Public Health. 2010;100(8):1400–1408. doi: 10.2105/AJPH.2009.173609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33a.Blue-Howells J, McGuire J, Nakashima J. Co-location of health care services for homeless veterans: a case study of innovation in program implementation. Soc Work Health Care. 2008;47(3):219–231. doi: 10.1080/00981380801985341. [DOI] [PubMed] [Google Scholar]
- 33b. International Classification of Diseases, Ninth Revision, Clinical Modification. Hyattsville, MD: National Center for Health Statistics; 1980. DHHS publication PHS 80-1260.
- 34.Hays RD, Shaul JA, Williams VS et al. Psychometric properties of the CAHPS 1.0 survey measures. Consumer Assessment of Health Plans Study. Med Care. 1999;37(3 suppl):MS22–MS31. doi: 10.1097/00005650-199903001-00003. [DOI] [PubMed] [Google Scholar]
- 35.Safran DG, Kosinski M, Tarlov AR et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36(5):728–739. doi: 10.1097/00005650-199805000-00012. [DOI] [PubMed] [Google Scholar]
- 36.Nickasch B, Marnocha SK. Healthcare experiences of the homeless. J Am Acad Nurse Pract. 2009;21(1):39–46. doi: 10.1111/j.1745-7599.2008.00371.x. [DOI] [PubMed] [Google Scholar]
- 37.Davis E, Tamayo A, Fernandez A. “Because Somebody Cared about Me. That's How It Changed Things”: homeless, chronically ill patients’ perspectives on case management. PLoS ONE. 2012;7:e45980. doi: 10.1371/journal.pone.0045980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Committee on Quality of Health Care in America IoM. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 39.Samejima F. Graded response model. In: Van der Linden W, Hambleton RK, editors. Handbook of Item Response Theory. New York: Springer-Verlag; 2010. pp. 85–100. [Google Scholar]
- 40.Kontopantelis E, Roland M, Reeves D. Patient experience of access to primary care: identification of predictors in a national patient survey. BMC Fam Pract. 2010;11:61. doi: 10.1186/1471-2296-11-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Salisbury C, Wallace M, Montgomery AA. Patients’ experience and satisfaction in primary care: secondary analysis using multilevel modelling. BMJ. 2010;341:c5004. doi: 10.1136/bmj.c5004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Paddison C, Elliott M, Parker R et al. Should measures of patient experience in primary care be adjusted for case mix? Evidence from the English General Practice Patient Survey. BMJ Qual Saf. 2012;21(8):634–640. doi: 10.1136/bmjqs-2011-000737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 44.Kim TW, Kertesz SG, Horton NJ, Tibbetts N, Samet JH. Episodic homelessness and health care utilization in a prospective cohort of HIV-infected persons with alcohol problems. BMC Health Serv Res. 2006;6:19. doi: 10.1186/1472-6963-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kertesz SG, Larson MJ, Cheng DM et al. Need and non-need factors associated with addiction treatment utilization in a cohort of homeless and housed urban poor. Med Care. 2006;44(3):225–233. doi: 10.1097/01.mlr.0000199649.19464.8f. [DOI] [PubMed] [Google Scholar]
- 46.LaGory M, Ritchey FJ, Fitzpatrick K, Irwin J. A Needs Assessment of the Homeless of Birmingham and Jefferson County. Birmingham, AL: University of Alabama at Birmingham; 2005. [Google Scholar]
- 47.Irwin J, LaGory M, Ritchey F, Fitzpatrick K. Social assets and mental distress among the homeless: exploring the roles of social support and other forms of social capital on depression. Soc Sci Med. 2008;67(12):1935–1943. doi: 10.1016/j.socscimed.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 48.Mitchell CU, LaGory M. Social capital and mental distress in an impoverished community. City Community. 2002;1(2):199–216. [Google Scholar]
- 49.Kertesz SG, Horton NJ, Friedmann PD, Saitz R, Samet JH. Slowing the revolving door: stabilization programs reduce homeless persons’ substance use after detoxification. J Subst Abuse Treat. 2003;24(3):197–207. doi: 10.1016/s0740-5472(03)00026-6. [DOI] [PubMed] [Google Scholar]
- 50. Homeless Emergency Assistance and Rapid Transition. Housing (HEARTH) Act of 2009. 42 USC 11301. United States of America; 2009.
- 51. Notice of Funding Availability (NOFA) for the Collaborative Initiative to Help End Chronic Homelessness. 2003. Available at: http://archives.hud.gov/funding/2003/other/hmless.htm. Accessed August 2, 2013.
- 52.Idler EL, Kasl SV. Self-ratings of health: do they also predict change in functional ability? J Gerontol B Psychol Sci Soc Sci. 1995;50(6):S344–S353. doi: 10.1093/geronb/50b.6.s344. [DOI] [PubMed] [Google Scholar]
- 53.DeSalvo KB, Fan VS, McDonell MB, Fihn SD. Predicting mortality and healthcare utilization with a single question. Health Serv Res. 2005;40(4):1234–1246. doi: 10.1111/j.1475-6773.2005.00404.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Conrad KJ, Yagelka JR, Matters MD, Rich AR, Williams V, Buchanan M. Reliability and validity of a modified Colorado Symptom Index in a national homeless sample. Ment Health Serv Res. 2001;3(3):141–153. doi: 10.1023/a:1011571531303. [DOI] [PubMed] [Google Scholar]
- 55.Humeniuk R, Ali R. WHO ASSIST Phase II Study Group. Technical Report: Validation of the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) and Pilot Brief Intervention: A WHO Technical Report of Phase II findings. Geneva, Switzerland: World Health Organization Department of Mental Health and Substance Dependence; 2005. [Google Scholar]
- 56.Muthen LK, Muthen BO. Mplus: Statistical Analysis With Latent Variables User’s Guide. Los Angeles, CA: Muthen & Muthen; 2007. [Google Scholar]
- 57.Rizopoulos D. ltm: An R Package for Latent Variable Modeling and Item Response Analysis. J Stat Softw. 2006;17(5):1–25. [Google Scholar]
- 58.National Center for Health Statistics. Health, United States, 2011: With Special Feature on Socioeconomic Status and Health. Hyattsville, MD: Centers for Disease Control; 2012. [PubMed] [Google Scholar]
- 59.American Institutes for Research. How to Report Results of the CAHPS Clinician & Group Survey. Princeton, NJ: Robert Wood Johnson Foundation; 2010. [Google Scholar]
- 60.Trivedi AN, Matula S, Miake-Lye I, Glassman PA, Shekelle P, Asch S. Systematic review: comparison of the quality of medical care in Veterans Affairs and non-Veterans Affairs settings. Med Care. 2011;49(1):76–88. doi: 10.1097/MLR.0b013e3181f53575. [DOI] [PubMed] [Google Scholar]
- 61.Office of Quality SaV. VHA Facility Quality and Safety Report. Washington, DC: Department of Veterans Affairs; 2012. [Google Scholar]
- 62.Tessler R, Rosenheck R, Gamache G. Homeless veterans of the mil-volunteer force: a social selection perspective. Armed Forces Soc. 2003;29(4):509–524. [Google Scholar]
- 63.Hoffman C, Sered SS. Threadbare: Holes in America’s Health Care Safety Net. Menlo Park, CA: The Henry A. Kaiser Family Foundation; 2005. [Google Scholar]
- 64.Song J, Bartels DM, Ratner ER, Alderton L, Hudson B, Ahluwalia JS. Dying on the streets: homeless persons’ concerns and desires about end of life care. J Gen Intern Med. 2007;22(4):435–441. doi: 10.1007/s11606-006-0046-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.National Committee for Quality Assurance. NCQA’s PCMH 2011 and CMS Stage 1 Meaningful Use Requirements Appendix 2. Washington, DC: NCQA; 2011. [Google Scholar]
- 66.Buck DS, Rochon D, Davidson H, McCurdy S. Involving homeless persons in the leadership of a health care organization. Qual Health Res. 2004;14(4):513–525. doi: 10.1177/1049732303262642. [DOI] [PubMed] [Google Scholar]