Abstract
The benefits of Pathways Housing First in addressing chronic homelessness for persons with severe mental illness have been well established. However, the implementation and effectiveness of such programs in rural areas has yet to be examined. We described the model’s adaptations in Vermont, including the use of hybrid assertive community treatment–intensive case management teams, which consisted of service coordinators with geographically based caseloads (staff/client ratio of 1:20) and regional multidisciplinary specialists. The program’s innovative and widespread inclusion of technology into operations facilitated efficiency and responsiveness, and a pilot telehealth initiative supplemented in-person client visits. The program achieved a housing retention rate of 85% over approximately 3 years, and consumers reported decreased time spent homeless, demonstrating that program adaptations and technological enhancements were successful.
KEY FINDINGS
▪ Scatter-site Housing First can be implemented within a rural setting but may require adapting teams to use a hybrid ACT–ICM model and to incorporate technology to improve efficiency and mobility.
▪ Telehealth can be incorporated into the Housing First model, supporting team accessibility and increased consumer contact. Consumers are very receptive to in-home computers.
▪ Housing retention was 85%, suggesting that housing outcomes for rural Housing First are consistent with previous research.
THE UNITED STATES’ comprehensive Federal Strategic Plan to Prevent and End Homelessness has recognized supportive housing using the Housing First model as the “clear solution” to chronic homelessness.1 The Housing First model developed by Pathways to Housing offers immediate access to private-market, scatter-site housing without prerequisites for sobriety, “psychiatric stability,” or completion of previous treatment.2,3 Community-based and consumer-driven support teams targeting individuals with high needs have generally used assertive community treatment (ACT), whereas those targeting individuals with more moderate needs have used intensive case management (ICM). These teams provide or broker access to comprehensive services, including education and employment, family and social support, finances, psychiatric treatment, and substance use treatment.
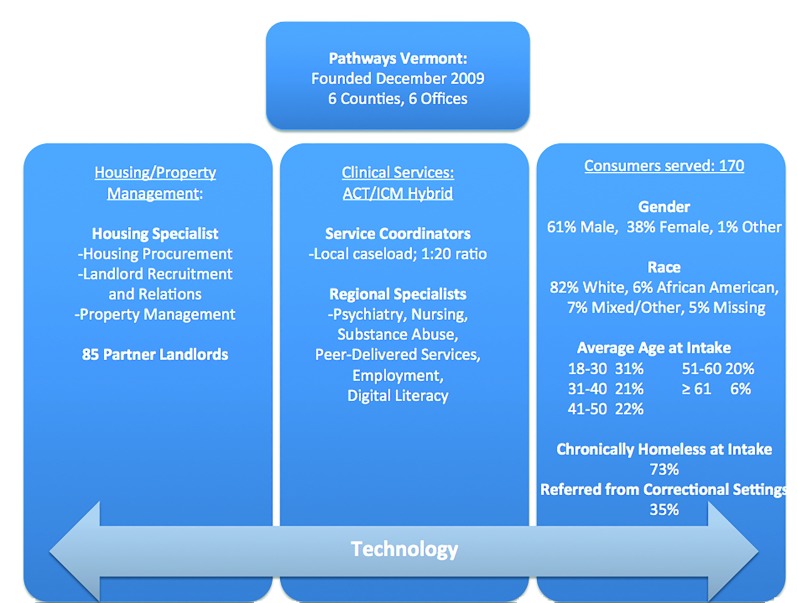
Scatter-site Housing First implementation and research has largely occurred in urban areas. Challenges to implementation in rural areas include low population density, large geographic distances, limited public transportation, workforce shortages, and limited housing stock, which often result in less intensive services, fewer multidisciplinary staff, and less care coordination.4–7 This report describes how Housing First-ACT was adapted and enhanced for a rural setting (Figure 1) and examines the program’s housing-related outcomes. Evaluation data included administrative data, program observation, interviews with clients, and interviews with staff during a fidelity assessment site visit near the end of year 1, as well as ongoing follow-up phone interviews with project managers.
FIGURE 1.
Pathways to Housing Vermont, 2009.
Note. ACT = assertive community treatment; ICM = intensive case management
PATHWAYS VERMONT: PROGRAM DESCRIPTION
In December 2009, a Pathways Housing First program began in Burlington, Vermont, and soon expanded to more rural areas. A fidelity evaluation found that the program was particularly strong on aspects related to housing choice and structure (e.g., providing affordable, integrated, private apartments of the consumer’s choosing), as well as issues related to separation of housing and services (e.g., no housing readiness requirements, standard leases or tenant agreements) and aspects of service philosophy (e.g., consumer choice–driven services, supporting consumer self-determination). The biggest barrier to rapid housing was two challenges commonly faced nationwide: a shortage of housing subsidies and low vacancy rates. Nevertheless, housing specialists recruited more than 85 landlords, procured housing units, assisted with property management issues, and served as liaisons with landlords. Staff with urban and rural Housing First expertise reported fairly similar experiences with housing across settings, with the exception that large landlord or property management companies were less common in rural areas, creating a more personal dynamic when managing those partnerships. Additionally, given the “small town” nature, a landlord’s negative experience with a tenant was somewhat more likely to delay re-housing.
Initial challenges to service delivery were consistent with other large-scale Housing First demonstration projects8 and included providing access to specialized services (e.g., psychiatry, supported employment) and implementing aspects of service philosophy (e.g., need for greater training in motivational interviewing, assertive engagement). Although services were initially structured to provide moderate-to-high fidelity ACT (e.g., multidisciplinary staff, shared caseloads, and 1:10 staff/consumer ratios), expansions in geographic boundaries of service and consumer populations with mixed levels of need resulted in both program adaptation and innovation. To address these challenges the program implemented a hybrid ACT–ICM model (adaptation) and incorporated technology for both staff and consumers (innovation).
Adaptation: Team Structure
Teams consisted of service coordinators with geographically based caseloads and staff-to-client ratios of 1:20, and regional specialists such as psychiatrists and employment specialists who provided care as needed. Service coordinators provided, at minimum, weekly in-person visits to consumers on their caseload and offered support with housing issues, entitlements, accessing community resources, social integration, as well as assistance with other activities of case management. Unlike service coordinators who saw their assigned caseload of consumers on a regular basis, specialists saw consumers based on the individual’s needs or interests, and might have worked full time or part-time. Nursing staff, for example, visited individuals who needed assistance with medical after-care, or an employment specialist visited someone who had expressed interest in finding work. Within this design, the availability of local service coordinators enabled consistent and responsive case management services, whereas accessibility of regional specialists ensured that consumers still had direct access to a wide spectrum of multidisciplinary services. There was continued emphasis on preserving overall team functioning (e.g., maintaining familiarity across caseloads, providing coverage, and conducting regular meetings). The hybrid model contributed to the success of the program by minimizing travel time with geographically-based caseloads, thus allowing for frequent and responsive services, and by capitalizing on the advantages of working within a team model (e.g., multidisciplinary expertise, continuity of care, mutual staff support).
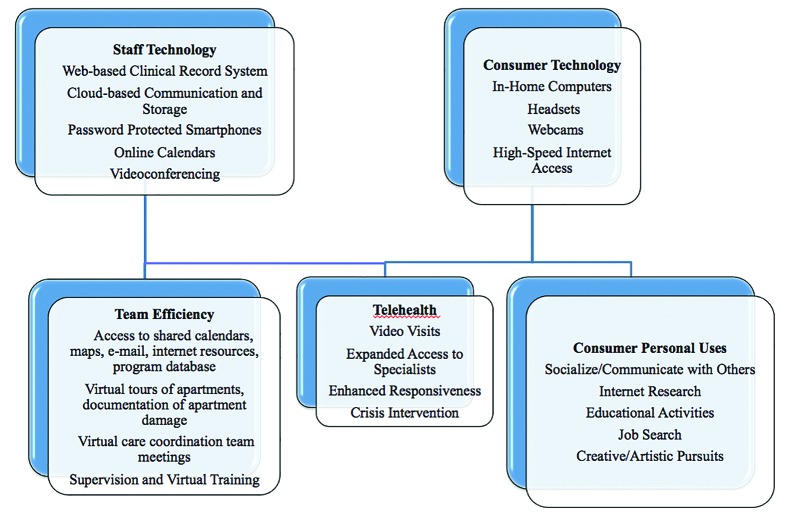
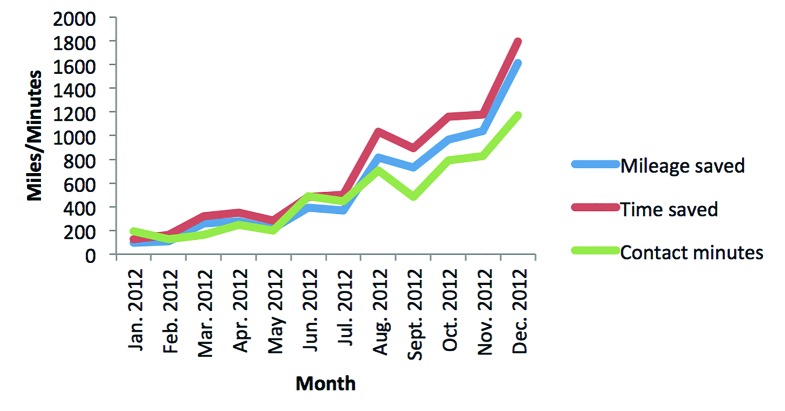
Innovation: Technology and Telehealth
To further address geographic and transportation challenges, the program adopted technology for both staff and consumers (Figure 2; Technology Sidebar). This made team processes and fieldwork more efficient, allowed for staff video visits with consumers through a Telehealth9 pilot project (Figure 3), and provided consumers with a resource to bridge the “digital divide.” Technological enhancements for staff permitted the team to respond to consumers more swiftly and efficiently. For consumers, the program provided in-home computers (that were either purchased affordably or donated) and Internet access (at bulk subscriber negotiated reduced rates), which allowed for “video visits” with staff and provided a resource to bridge the digital divide. The team’s digital literacy specialists oriented consumers to technology and provided on-going support. Consumers expressed interest and enthusiasm to receiving computers, highlighted specific and multiple ways in which they could use them, and equipment retention was quite high, with only 2 incidents of consumers reselling their computers.
FIGURE 2.
Pathways Vermont Technology.
FIGURE 3.
Pathways Vermont Telehealth Implementation.
HOUSING OUTCOMES
The program served 170 individuals: 122 individuals in northern counties of Vermont and 48 individuals in southern counties. The consumer population in Vermont differed from most other Pathways Housing First research: consumers were predominantly White and disproportionately more individuals (35%) entered the program from jail because of supplemental program funding from the Department of Corrections. After nearly 3 years, overall housing retention was 85% (calculated as: 170 consumers − 15 pending first unit = 155 consumers housed − 8 deaths = 147 − 22 not currently housed or discharged from program = 125; 125/147 = 85%.), similar to previous Housing First studies.10,11 Longitudinal data on time spent homeless were also available for a subset of participants (n = 88) who completed an interviewer-administered assessment at intake and 6-month intervals for the more established team in northern Vermont. Mixed-effect zero-inflated Poisson regression analysis indicated that the number of days participants spent homeless during the last 30 days decreased significantly from baseline (mean [SD] = 11.02 [13.55]) to 12-month follow-up (1.96 [7.01]; b = −4.17; SE = 1.55; P < .001).
INNOVATION: TECHNOLOGY
| Staff technological enhancements |
| The widespread use of technology allows for effective team communication, efficient processes, and maximizes time spent with consumers, resulting in an intensity of service delivery that is comparable to other non-rural Housing First teams run by the same agency.a Care coordination meetings are conducted virtually, thus preserving team functioning while allowing for more time spent with consumers versus traveling. Voice-to-text e-mail notification of consumers’ calls “off-hours” allows supervisors to better monitor crisis responding, and teams can attend virtual trainings. Smartphones or tablets enable full functionality for staff in the field. |
| Telehealth pilot project |
| Community visits are supplemented with “video visits,” that increase staff availability by minimizing travel time. This facilitates the work of specialists in particular, who can cover larger geographic areas to reach a broader base of consumers across the caseload: for example, a consumer who is working can receive follow-up support from an employment specialist or a consumer with a medication question can discuss concerns with the psychiatrist. |
| Consumer personal use |
| Qualitative interviews, completed with 133 clients, gauged their interest in receiving a computer. An overwhelming majority expressed excitement, with participants stating that, among other uses, it would greatly facilitate socialization and communication: “I’ll be able to talk to people with similar mental illnesses and learn more about mine, communicate with Pathways more, and talk to my daughter.” Several also noted how it could help alleviate issues with mental health; for example, by allowing individuals who have trouble with crowds to shop online. Some participants also expressed interest, but felt slightly apprehensive about their computer skills and ability to address technical problems, reinforcing the critical need for the role of the digital literacy specialist. |
aRural Housing First Assertive Community Treatment–Intensive Case Management (ACT–ICM) Hybrid Team: 5 face-to-face (FTF) contacts per client per month, on average (no regulatory minimum); Urban Housing First-ACT Team: 7 FTF contacts (minimum 6); and Suburban Housing First-ICM team 3 (minimum 2).
EVALUATION
This report demonstrated that Housing First could be successfully implemented in rural settings and achieves housing outcomes similar to urban programs. Although homelessness outcomes relied on retrospective self-report by consumers whose recall might be somewhat inaccurate, the interview used a shorter reference period (past 30 days) to maximize the likelihood of accurate recall. Shorter time periods might skew results by representing only brief snapshots of participants’ residential histories, but the high housing retention rate calculated over time using administrative data bolstered confidence in the positive housing outcomes. By blending 2 housing first service models into 1 program (ACT, ICM) and adding the technology enhancement, the program was also able to expand its ability to provide reliable and responsive supports as well as comprehensive, multidisciplinary services that were consistent with core Housing First philosophical and operational concepts (e.g., no housing readiness, consumer choice, and harm reduction).
The use of technology and telehealth in supportive housing is novel and may also be applied in urban settings with highly dispersed housing and transportation challenges, potentially facilitating transitions to lower levels of care by bridging initial gaps in intensity and serving as a resource for broader social integration and meaningful activity. Further research to investigate this possibility, as well as the long-term impact on client outcomes and any potential cost savings, is warranted.
Acknowledgments
This study was supported by funding from the Substance Abuse and Mental Health Services Administration (SAMHSA) Services in Supportive Housing Grant SM059197 and SAMHSA’s Cooperative Agreements to Benefit Homeless Individuals Grant TI023514.
We thank Lei Duan, Eric Lindberg, and Jessie Ulsoy, and express deep appreciation and gratitude to Lindsay Casale, Patrick Gallagher, Laura-Nicole Sisson, Brian Smith, Stasia Savasuk, and all the participants of Pathways Vermont.
Note. A. Stefancic, H. Melton, R. Lawrence-Gomez, and S. Tsemberis are employed by Pathways to Housing, Inc.
Human Participant Protection
This study was approved by the institutional review board of Pathways to Housing, and all study participants provided informed consent.
References
- 1.U.S. Interagency Council on Homelessness. Opening Doors: Federal Strategic Plan to Prevent and End Homelessness. Washington, DC: US Interagency Council on Homelessness; 2010. [Google Scholar]
- 2.Tsemberis S. Housing First: The Pathways Model to End Homelessness for People with Mental Illness and Addiction. Center City, MN: Hazelden; 2010. [Google Scholar]
- 3.Tsemberis S, Gulcur L, Nakae M. Housing First, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am J Public Health. 2004;94(4):651–656. doi: 10.2105/ajph.94.4.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meyer PS, Morrissey JP. A comparison of assertive community treatment and intensive case management for patients in rural areas. Psychiatr Serv. 2007;58(1):121–127. doi: 10.1176/ps.2007.58.1.121. [DOI] [PubMed] [Google Scholar]
- 5.Fekete DM, Bond GR, McDonel EC, Saiyers M, Chen A, Miller L. Rural assertive community treatment: a field experiment. Psychiatr Rehabil J. 1998;21(4):371–379. [Google Scholar]
- 6.Beer A, Delfabbro P, Natalier K, Oakley S, Verity F. Developing Models of Good Practice in Meeting the Needs of Homeless Young People in Rural Areas. AHURI Positioning Paper No. 62. Melbourne, Australia: Australian Housing and Urban Research Institute; 2003. [Google Scholar]
- 7.Forchuk C, Montgomery P, Berman H, et al. Gaining ground, losing ground: the paradoxes of rural homelessness. Can J Nurs Res. 2010;42(2):138–152. [PubMed] [Google Scholar]
- 8.Nelson G, et al. A mixed methods implementation evaluation of a multi-site Housing First intervention for homeless people with mental illness. Evaluation and Program Planning. doi: 10.1016/j.evalprogplan.2013.10.004. In press. [DOI] [PubMed] [Google Scholar]
- 9.McLaren P. Telemedicine and telecare: what can it offer mental health services? Adv Psychiatr Treat. 2003;9(1):54–61. [Google Scholar]
- 10.Tsemberis S, Kent D, Respress C. Housing stability and recovery among chronically homeless persons with co-occurring disorders in Washington, DC. Am J Public Health. 2012;102(1):13–16. doi: 10.2105/AJPH.2011.300320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stefancic A, Tsemberis S. Housing First for long-term shelter dwellers with psychiatric disabilities in a suburban county: a four-year study of housing access and retention. J Prim Prev. 2007;28(3-4):265–279. doi: 10.1007/s10935-007-0093-9. [DOI] [PubMed] [Google Scholar]