Abstract
Objectives. We identified risk and need profiles of homeless veterans and examined the relation between profiles and referrals and admissions to Department of Veterans Affairs (VA) homeless service programs.
Methods. We examined data from the VA’s new Homeless Operations Management and Evaluation System on 120 852 veterans from 142 sites nationally in 2011 and 2012 using latent class analyses based on 9 homeless risk factors. The final 4-class solution compared both referral and admission to VA homeless services.
Results. We identified 4 latent classes: relatively few problems, dual diagnosis, poverty–substance abuse–incarceration, and disabling medical problems. Homeless veterans in the first group were more likely to be admitted to the VA’s permanent supportive housing program, whereas those in the second group were more likely to be admitted to more restrictive VA residential treatment. Homeless veterans in the third group were more likely to be admitted to the VA’s prisoner re-entry program, and those in the fourth group were more likely to be directed to VA medical services.
Conclusions. The heterogeneous risk and need profiles of homeless veterans supported the diversity of VA homeless services and encouraged the development of specialized services to meet their diverse needs.
Although homelessness has been an important national problem in the United States for more than 3 decades,1,2 and various homeless services have been developed,3 there is little understanding of the matching of the diverse needs of this heterogeneous population to different types of services. Studies have shown that there are different patterns of needs among homeless adults; developing a taxonomy of individuals based on modifiable homeless risk factors may enhance the fit and quality of services provided to this population.4
One commonly cited study used cluster analysis to examine 73 000 homeless public shelter users in New York City and developed a 3-group typology: transitionally homeless, episodically homeless, and chronically homeless.5 Another cluster analytic study of homeless shelter users in the Midwest found 4 groups, each with different problems: criminality, psychiatric history, transiency, or criminal victimization.6 A handful of other studies using small homeless samples in other settings found other groups, such as those who are economically disadvantaged, those with mental health or substance abuse problems, and those with relatively few problems.7,8 A few studies included sociodemographic characteristics in their cluster analyses that contributed to the literature, but did not identify groups with modifiable characteristics or specific needs that could be directly addressed with services.9,10
However, there has not been a comprehensive attempt to classify homeless individuals based on their risk profiles; that is, basing the classification on well-known modifiable risk factors for homelessness. Modifiable risk factors do, in essence, reflect needs that can be addressed with services.11 Thus, developing such a classification may allow better matching of needs and services to serve this diverse population and to guide the continued development of new services that can address their needs.
A body of literature has identified numerous modifiable risk factors for homelessness, including alcohol or drug use disorders, incarceration histories, poverty, poor physical health, history of adverse childhood events, inadequate health insurance, and schizophrenia or bipolar disorder.12–20 Schizophrenia and bipolar disorder may have the most impact on the risk for homelessness at the individual level (i.e., highest relative risk), whereas substance abuse may have the most impact on risk at the population level (i.e., highest attributable risk).19
Military veterans are an important and overrepresented segment of the homeless adult population.21,22 Ending homelessness among veterans has become a national concern and a top priority of the Department of Veterans Affairs (VA). In 2009, the VA declared a goal of ending homelessness among veterans and has dramatically ramped up funding for a variety of programs and services for homeless veterans.23 Thus, it is an opportune time to further examine the risks and needs of homeless veterans and the VA-funded services created to address them.
Identified modifiable risk factors for homelessness among veterans are similar to those found among homeless adults in the general population. Among veterans, risk factors include unemployment, disability, poor physical health, psychiatric disorders (especially schizophrenia or bipolar disorder), substance use disorders, and negative childhood experiences, whereas having a college education, being married, and having a total income of $600 a month or higher are protective factors.24–28
One study that conducted cluster analysis on psychosocial characteristics of a national sample of 565 homeless veterans found 4 groups: alcoholic, psychiatrically impaired, multiproblem, and best-functioning groups.4 However, that study was based on data collected more than 2 decades ago from a specialized program for homeless veterans with chronic mental illness. A pair of studies that used diagnostic data on a sample of homeless veterans in the northeast and conducted separate cluster analyses for medical and psychiatric diagnoses found 3 psychiatric clusters consisting of addiction, psychosis, and personality disorders,29 and 4 medical clusters consisting of generalized illness, hepatic disease, lung disease, and neurologic disorders.30 However, these studies treated medical and psychiatric problems separately and did not include assessments of psychosocial problems beyond diagnoses.
We used the VA’s recently implemented national database system and drew on all its specialized homeless programs to (1) describe and classify over 120 000 homeless veterans on known modifiable risk factors utilizing latent class analysis (LCA), and (2) examine the relation between homeless veteran characteristics and program referral and admission patterns in a real-world context. There has been no previous study of this kind—identifying latent classes among such a large heterogeneous sample of homeless veterans in relation to such a broad array of available homeless services. Our results might be informative for public health efforts to address homelessness among US veterans.
METHODS
The VA Homeless Operations Management and Evaluation System (HOMES) is a recently implemented online VA data collection system. HOMES is one of several data streams to a comprehensive homeless registry that offers a near–real-time resource for service providers, policymakers, administrators, and researchers. HOMES reflects the primary data collection of specialized homeless programs and may provide numerous benefits, including the ability to track the care of homeless veterans, evaluate the effectiveness of interventions, target resources that can be used to prevent homelessness, and identify best practices. The homeless registry is designed to provide a facility-, regional-, and national-level snapshot of progress toward the VA’s plan to end homelessness among veterans. We used client-level data from April 2011 to November 2012. The original data set included 148 465 records. Some clients had more than 1 record; in those cases, a random record was sampled. The total sample used in this study included 120 852 homeless veterans across 142 national sites.
Program Descriptions and Measures
Five main VA programs that fall under the umbrella of VA homeless services are briefly described.1 The Housing and Urban Development-Veterans Affairs (HUD-VA) Supportive Housing program offers homeless veterans HUD Housing Choice vouchers to subsidize their rent and supportive case management from VA staff to help them acquire and retain permanent housing.2 The Grant and Per Diem program funds community agencies to provide structured transitional housing for homeless veterans where they can stay for up to 2 years with the goal of helping them achieve residential stability, receive treatment for mental and addictive disorders, increase their skill levels and incomes, and obtain greater capacity for community reintegration.3 The Healthcare for Re-Entry Veterans program assists incarcerated veterans soon to be re-entering the community by connecting them to needed VA health services to prevent recidivism and homelessness through outreach, pre-release assessments, and post-release referrals and linkages to medical, psychiatric, and social services.4 The Veterans Justice Outreach program, in contrast, serves veterans recently involved in the criminal justice system to avoid the unnecessary criminalization of mental illness and extended incarceration by providing direct outreach, assessment, diversion, and case management services, along with acting as a liaison with local courts, jails, and local justice system partners.5 The Domiciliary Care for Homeless Veterans program provides time-limited residential rehabilitation and treatment services on VA grounds, including medical, psychiatric, substance abuse treatment, and vocational rehabilitation. Additional details about these programs can be found in other sources.31–33
VA homeless staff conduct assessment interviews with all homeless veterans who are prospective clients of VA homeless programs using the measures described in the following.
For recent housing history, clients were asked where they spent each of the past 30 days from a list of 20 living arrangements. For this analysis, we collapsed these living arrangements into 5 categories: own place (own or rented apartment or house), someone else’s place (family or friend’s house or apartment), residential treatment or transitional housing (VA or non-VA residential treatment, domiciliary, transitional housing, or hotel), an institution (hospital, prison, or jail), or homeless (shelter, outdoors, or automobile). For a history of chronic homelessness, clients were asked how long their most recent episode of homelessness was for and how many episodes of homelessness they experienced in the past 3 years. Consistent with the federal definition, chronic homelessness was defined as being continuously homeless for 1 year or more or having 4 or more episodes of homelessness in the past 3 years.34
Incarceration history was assessed by asking clients how much total time they spent in jail or prison during their lifetime. Then, responses were coded dichotomously as having an incarceration history or not.
Employment history and current income were assessed by asking clients to describe their employment pattern in the last 3 years and what their total income was in the past month. Employment history was coded as either employed full-time, part-time, or not employed. Clients were asked about various sources of income, including income from employment, VA disability compensation, non-VA disability insurance programs (e.g., Social Security Disability), child support, and other support, which were summed for total income. Total income was then coded as either equal to or greater than $600 a month or less than $600 a month, based on a recent study that determined $600 was an important cutoff point for homeless veterans among the population of VA service users in 2010.28
Medical history was assessed by asking clients whether a doctor or nurse had ever told them they had the following medical conditions: HIV/AIDS, HCV, tuberculosis, chronic obstructive pulmonary disease, heart disease, stroke, diabetes, seizures, chronic pain, or other medical conditions. Clients were also asked to rate their physical health in the past month on a 5-point scale from poor to excellent, which was categorized as excellent or very good, good or fair, and poor.
Psychiatric history was assessed by clinicians in their assessment interview and through review of existing medical records. Psychiatric diagnoses were categorized as affective disorders (including depression), military-related posttraumatic stress disorder (PTSD), other anxiety disorders, substance use disorders (alcohol use or drug use disorder), and psychotic disorders (schizophrenia, bipolar disorder, or other psychotic disorder). Clients were further asked whether they had ever been hospitalized for a psychiatric problem.
Data Analysis
LCA is a statistical modeling technique used to find groups, subtypes, or latent classes of cases in multivariable categorical data. Unlike cluster analysis, which assigns individuals to orthogonal groups using ad hoc distance measures for classification and assumes observed variables have direct relationships, LCA is based on a probabilistic model that assigns probabilities of membership to individuals and considers observed variables as related to latent variables.35 LCA not only allows for greater flexibility in modeling but formalizes classification, arguably provides a more realistic view of nature, and is considered superior to traditional clustering methods.36,37
LCAs were conducted on 9 dichotomous, modifiable risk factors for homelessness to characterize risk and need profiles of homeless veterans in the following domains (specific risk factors in parentheses): homeless history (chronically homeless or not), incarceration history (any incarceration or none), unemployment history (no work, or full-time or part-time work in past 3 years), income (received less than $600 in the past month or $600 or more), medical history (any chronic medical condition), and psychiatric history (any military-related PTSD, any substance use disorder, any psychotic disorder, and any psychiatric hospitalizations).
As recommended in LCA for large sample sizes,38–40 fit statistics, parsimony, theory and interpretability, and percentage of participants in each class were examined to guide model selection. More specifically, the number of classes in the final model solution was determined by
relatively low Akaike information criterion (AIC) and Bayesian information criterion (BIC) values, high entropy values, and significant Lo-Mendell-Rubin (LMR) and bootstrapped likelihood ratio (BLR) tests;
graphing different class solutions to visually examine meaningful divisions of classes;
guidance from previous classificatory work in this area5–8,41;
requiring a 10% minimum in the smallest class; and
using the smallest (most parsimonious) number of classes necessary.
After a latent class solution was identified, different classes were compared on sociodemographic characteristics, clinical diagnoses, and the programs to which they were referred or admitted to using analysis of variance and the χ2 test. Post hoc analyses were conducted with the Tukey honestly significant different test and the pairwise χ2 test. To adjust for multiple comparisons and inflated type I error, the significance for all analyses was conducted at the .01 level.
RESULTS
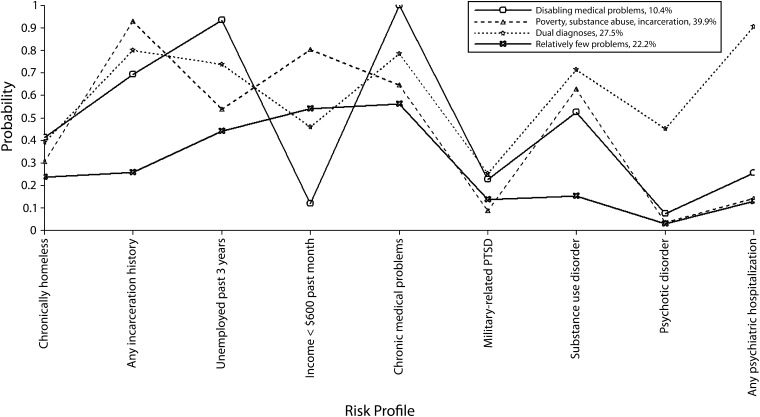
Fit indexes of the LCA showed an increasing number of classes provided better fit (lower log-likelihood, AIC, BIC, and adjusted BIC values, and significant LMR and BLR tests) with the entropy values plateauing at 4 classes (fit indexes and graphs of alternative latent class solutions are available upon request from the author). Based on theory, parsimony, and clinical significance, the 4-class model was determined to provide the most meaningful differentiation and was selected as the final solution (Figure 1). Of the total sample, 26 888 veterans (22.25%) were classified as having “relatively few problems,” 33 245 (27.51%) as “dual diagnosis,” 48 183 (39.87%) as “poverty–substance abuse–incarceration,” and 12 536 (10.37%) as “disabling medical problems.”
FIGURE 1—
Four latent classes of homeless veterans, risk profiles, and relation to program referral and admissions: Homeless Operations Management and Evaluation System, Department of Veterans Affairs, United States, 2011–2012.
Note. PTSD = posttraumatic stress disorder.
Table 1 shows the individual characteristics of the total sample by each latent class. In terms of sociodemographic characteristics, the relatively few problems group was significantly younger, more likely to be female, more likely to be married, and had more years of education than other groups. The disabling medical problems group was the oldest group, whereas the dual diagnosis group was most likely to be White (all test statistics are available upon request from the author).
TABLE 1—
Characteristics of 4 Latent Classes of Homeless Veterans, Risk Profiles, and Relation to Program Referral and Admissions: Homeless Operations Management and Evaluation System, Department of Veterans Affairs, United States, 2011–2012
| Individual characteristics | Total Sample (n = 120 852), No. (%) or Mean ±SD | Relatively Few Problems (n = 26 888), No. (%) or Mean ±SD | Dual Diagnosis (n = 33 245), No. (%) or Mean ±SD | Poverty–Substance Abuse–Incarceration (n = 48 183), No. (%) or Mean ±SD | Disabling Medical Problems (n = 12 536), No. (%) or Mean ±SD | Group Comparisona P < .001 |
| Age, y | 49.92 ±11.54 | 47.82 ±13.35 | 50.04 ±10.94 | 49.33 ±10.49 | 56.38 ±10.39 | 4 > 2 > 3 > 1 |
| Gender | ||||||
| Male | 103 109 (92.23) | 19 554 (82.46) | 28 336 (92.32) | 43 853 (96.68) | 11 366 (94.50) | 3 > 4 > 2 > 1 |
| Female | 8684 (7.77) | 4158 (17.54) | 2357 (7.68) | 1508 (3.32) | 661 (5.50) | |
| Race | ||||||
| White | 63 529 (55.15) | 13 011 (55.12) | 18 701 (57.74) | 25 408 (54.11) | 6409 (52.39) | 2 > 1 > 4; 2 > 3 |
| Black | 47 612 (41.33) | 9708 (41.13) | 12 593 (38.88) | 19 902 (42.38) | 5409 (44.22) | |
| Other | 4045 (3.51) | 886 (3.75) | 1095 (3.38) | 1649 (3.51) | 415 (3.39) | |
| Married | 12 758 (10.92) | 3680 (15.31) | 3008 (9.17) | 4705 (9.89) | 1365 (11.01) | 1 > 4 > 2,3 |
| Years of education | 12.95 ±1.85 | 13.30 ±1.97 | 12.90 ±1.87 | 12.82 ±1.70 | 12.89 ±2.01 | 1 > 2,3,4 |
| Days living in past mo | ||||||
| Own place | 4.20 ±9.84 | 6.54 ±11.85 | 3.87 ±9.38 | 2.76 ±8.18 | 6.03 ±11.36 | 1 > 4 > 2 > 3 |
| Someone else’s place | 7.77 ±12.11 | 10.69 ±13.43 | 7.03 ±11.50 | 6.68 ±11.48 | 8.31 ±12.44 | 1 > 4 > 2 > 3 |
| Residential/transitional | 6.20 ±11.27 | 4.99 ±10.34 | 7.70 ±12.07 | 5.68 ±10.94 | 6.58 ±11.57 | 2 > 4 > 3 > 1 |
| Institution | 5.42 ±10.80 | 0.74 ±4.05 | 5.34 ±10.16 | 8.71 ±13.05 | 1.95 ±6.45 | 3 > 2 > 4 > 1 |
| Homeless | 6.94 ±11.57 | 6.94 ±11.57 | 6.05 ±10.80 | 6.16 ±11.12 | 7.11 ±11.65 | 1,4 > 2,3 |
| Chronically homeless | 37 623 (32.38) | 5577 (23.49) | 12 707 (38.90) | 14 506 (30.62) | 4833 (38.96) | 4,2 > 1,3 |
| Any incarceration history | 81 361 (71.59) | 1242 (5.33) | 25 788 (80.84) | 45 216 (97.27) | 9115 (76.24) | 1 > 4 > 2 > 3 |
| Employment history, past 3 y | ||||||
| Not employed | 71 628 (61.23) | 13 875 (58.17) | 7322 (22.21) | 24 165 (50.69) | 0 (0.00) | 1 > 3 > 2 > 4 |
| Full-time/part-time | 45 362 (38.77) | 9979 (41.83) | 25 646 (77.79) | 23 510 (49.31) | 12 493 (100.0) | |
| Income | ||||||
| < $600/mo | 66 509 (57.71) | 11 936 (50.86) | 13 995 (43.23) | 40 531 (86.36) | 47 (0.38) | 3 > 1 > 2 > 4 |
| ≥ $600/mo | 48 734 (42.29) | 11 533 (49.14) | 18 380 (56.77) | 6401 (13.64) | 12 420 (99.62) | |
| Income sources, $ | ||||||
| Employment | 125.67 ±635.70 | 224.65 ±947.77 | 84.56 ±413.31 | 115.41 ±595.91 | 61.78 ±348.44 | 1 > 3 > 2 > 4 |
| Disability | 350.61 ±906.76 | 240.80 ±655.68 | 623.35 ±1249.25 | 75.46 ±405.05 | 920.39 ±1181.74 | 4 > 2 > 1 > 3 |
| Rating of physical health | ||||||
| Excellent/very good | 19 855 (17.22) | 4609 (19.65) | 3959 (12.20) | 10 269 (21.82) | 1018 (8.25) | 3 > 1 > 2 > 4 |
| Good/fair | 76 498 (66.33) | 15 538 (66.23) | 21 951 (67.62) | 30 916 (65.70) | 8093 (65.57) | |
| Poor | 18 968 (16.45) | 3312 (14.12) | 6552 (20.18) | 5873 (12.48) | 3231 (26.18) | |
| Psychiatric diagnoses | ||||||
| Affective disorder | 42 202 (34.92) | 7446 (27.70) | 15 955 (47.99) | 14 077 (29.22) | 4724 (37.68) | 2 > 4 > 3 > 1 |
| Military-related PTSD | 18 738 (15.51) | 3865 (14.38) | 8711 (26.20) | 3779 (7.84) | 2383 (19.01) | |
| Other anxiety disorder | 20 445 (16.92) | 3866 (14.38) | 7996 (24.05) | 6429 (13.34) | 2154 (17.18) | |
| Substance use disorder | 63 435 (52.49) | 3180 (11.83) | 23 949 (72.04) | 29 499 (61.22) | 6807 (54.30) | |
| Psychotic disorder | 17 077 (14.13) | 485 (1.80) | 14 135 (42.52) | 1686 (3.50) | 771 (6.15) | |
| Any psychiatric hospitalizations | 40 064 (34.73) | 2496 (10.67) | 31 873 (97.19) | 4637 (9.86) | 1058 (8.71) | 2 > 1,3 > 4 |
Note. PTSD = posttraumatic stress disorder. Percentages may not sum to 100% because of rounding.
Analysis of variance was conducted on continuous variables and χ2 test on categorical variables. Post hoc comparisons were conducted with Tukey’s honestly significant difference test and pairwise χ2 test.
Veterans in the relatively few problems group were characterized as having the lowest probability for all 9 homeless risk factors, except for low income and military-related PTSD, for which they also had relatively low prevalences. Veterans in the dual diagnosis group were characterized as having the highest rates of substance use disorders, psychotic disorders, and psychiatric hospitalizations. Veterans in the poverty–substance abuse–incarceration group were characterized as being most likely to receive less than $600 in the past month, as having a relatively high rate of substance use disorders, and being most likely to have a lifetime history of incarceration. Lastly, veterans in the disabling medical problems group were characterized as being most likely to have a chronic medical condition and being most likely to be unemployed in the past 3 years (likely the result of disability because this group also received the largest amount of disability income).
Table 2 shows the initial point of contact at which veterans connected with the VA homeless service teams. Among the total sample, the most common initial point of contact was through self-referrals and street or community outreach. Compared with other groups, the relatively few problems group was most likely to have been contacted through street or community outreach or referred from the VA homeless hotline, whereas the poverty–substance abuse–incarceration group was most likely to be contacted through justice system outreach or referred from the criminal justice system. The dual diagnosis group was more likely to be referred from a residential or transitional program or from a mental health or medical service provider than other groups. The disabling medical problems group was more likely to be referred from the emergency department or through self-referral than other groups.
TABLE 2—
Initial Point of Contact Among 4 Latent Classes of Homeless and At-Risk Veterans’ Risk Profiles and Relation to Program Referral and Admissions: Homeless Operations Management and Evaluation System, Department of Veterans Affairs (VA), United States, 2011–2012
| Initial Contact | Total Sample (n = 117 630), No (%) | Relatively Few Problems (n = 24 336), No (%) | Dual Diagnosis (n = 32 995), No (%) | Poverty–Substance Abuse–Incarceration (n = 47 860), No. (%) | Disabling Medical Problems (n = 12 439), No (%) |
| Street/community outreach | 20 748 (17.64) | 5062 (20.80) | 5515 (16.71) | 7767 (16.23) | 2404 (19.33) |
| Justice system outreach | 13 896 (11.81) | 340 (1.40) | 2798 (8.48) | 10 281 (21.48) | 477 (3.83) |
| Referral from residential/transitional program | 14 325 (12.18) | 2364 (9.71) | 4898 (14.84) | 5675 (11.86) | 1388 (11.16) |
| Referral from mental health services | 8469 (7.20) | 1616 (6.64) | 3221 (9.76) | 2585 (5.40) | 1047 (8.42) |
| Referral from medical services | 8602 (7.31) | 1848 (7.59) | 3544 (10.74) | 2221 (4.64) | 989 (7.95) |
| Referral from emergency department | 683 (0.58) | 155 (0.64) | 237 (0.72) | 198 (0.41) | 93 (0.75) |
| Referral from VA homeless hotline | 2661 (2.26) | 1290 (5.30) | 367 (1.11) | 734 (1.53) | 270 (2.17) |
| Referral from criminal justice system | 6419 (5.46) | 423 (1.74) | 1800 (5.46) | 3622 (7.57) | 574 (4.61) |
| Referral from others | 14 692 (12.49) | 4434 (18.22) | 3347 (10.14) | 5206 (10.88) | 1705 (13.71) |
| Self-referred | 27 135 (23.07) | 6804 (27.96) | 7268 (22.03) | 9571 (20.00) | 3492 (28.07) |
Note. Percentages may not sum to 100% because of rounding.
Table 3 describes the various VA programs to which the 4 latent classes of homeless veterans were referred, and Table 4 describes the programs to which they were actually admitted to after referral. Among the 4 latent classes, the relatively few problems group was most likely to be referred to the HUD-VA Supportive Housing program, whereas the dual diagnosis group and the poverty–substance abuse–incarceration group were most likely to be referred to the Grant and Per Diem program. The poverty–substance abuse–incarceration group was more likely to be referred to the Healthcare for Re-Entry Veterans program and VA vocational services than other groups, whereas the disabling medical problems group was more likely to be referred to VA medical services. The dual diagnosis group was more likely to be referred a variety of services compared with other groups, including VA mental health services, the Veterans Justice Outreach program, the Domiciliary Care for Homeless Veterans program, VA disability compensation, and the VA emergency department.
TABLE 3—
Referral Patterns Among 4 Latent Classes of Homeless Veterans, Risk Profiles, and Relation to Program Referral and Admissions: Homeless Operations Management and Evaluation System, Department of Veterans Affairs, United States, 2011–2012
| Referral | Total Sample (n = 95 757), No. (%) | Relatively Few Problems (n = 20 082), No. (%) | Dual Diagnosis (n = 26 999), No. (%) | Poverty– Substance Abuse–Incarceration (n = 39 298), No. (%) | Disabling Medical Problems (n = 9378), No. (%) | Group Comparisona |
| HUD-VA supportive housing | 33 883 (35.38) | 10 434 (51.96) | 9089 (33.66) | 9763 (24.84) | 4597 (49.02) | 1 > 4 > 2 > 3 |
| Grant & Per Diem | 29 034 (30.32) | 5862 (29.19) | 8486 (31.43) | 12 325 (31.36) | 2361 (25.18) | 2,3 > 1 > 4 |
| VA medical service | 22 905 (23.92) | 4091 (20.37) | 6908 (25.59) | 9519 (24.22) | 2387 (25.45) | 2,4 > 1; 3 > 1 |
| VA mental health service | 22 779 (23.79) | 3240 (16.13) | 8479 (31.40) | 8793 (22.38) | 2267 (24.17) | 2 > 4 > 3 > 1 |
| Healthcare for Re-Entry Veterans | 11 226 (11.72) | 123 (0.61) | 1963 (7.27) | 9012 (22.93) | 128 (1.36) | 3 > 2 > 4 > 1 |
| Veterans Justice Outreach | 10 223 (10.68) | 833 (4.15) | 3520 (13.04) | 4853 (12.35) | 1017 (10.84) | 2,3 > 4 > 1 |
| Domiciliary Care for Homeless Veterans | 7048 (7.36) | 802 (3.99) | 2855 (10.57) | 2906 (7.39) | 485 (5.17) | 2 > 3 > 4 > 1 |
| VA vocational service | 6354 (6.64) | 1070 (5.33) | 1883 (6.97) | 3020 (7.68) | 381 (4.06) | 2,3 > 1 > 4 |
| VA disability compensation | 5467 (5.72) | 1133 (5.64) | 1761 (6.52) | 2138 (5.44) | 444 (4.73) | 2 > 1,3,4 |
| VA emergency department | 1310 (1.37) | 169 (0.84) | 486 (1.80) | 536 (1.36) | 119 (1.27) | 2 > 3 > 1 |
Note. HUD = Housing and Urban Development; VA = Veteran's Affairs. Rows arranged by order of total program referrals. Percentages may not sum to 100% because of rounding.
Omnibus χ2 test was conducted before post hoc pairwise χ2 test.
TABLE 4—
Program Admissions Among 4 Latent Classes of Homeless Veterans, Risk Profiles and Relation to Program Referral and Admissions: Homeless Operations Management and Evaluation System, Department of Veterans Affairs (VA), United States, 2011–2012
| Program Admissions | Total Sample (n = 90 889), No. (%) | Relatively Few Problems (n = 18 668), No (%) | Dual Diagnosis (n = 25 694), No. (%) | Poverty–Substance Abuse–Incarceration (n = 37 702), No. (%) | Disabling Medical Problems (n = 8825), No. (%) | Group Comparison P < .001 |
| HUD-VA Supportive Housing | 30 992 (34.10) | 9719 (52.06) | 8215 (31.97) | 8883 (23.56) | 4175 (47.31) | 1 > 4 > 2 > 3 |
| Grant & Per Diem | 27 530 (30.29) | 5565 (29.81) | 7996 (31.12) | 11 756 (31.18) | 2213 (25.08) | 1,2,3 > 4 |
| Healthcare for Re-Entry Veterans | 9342 (10.28) | 107 (0.57) | 1675 (6.52) | 7449 (19.76) | 111 (1.26) | 3 > 2 > 4 > 1 |
| Veterans Justice Outreach | 8932 (9.83) | 725 (3.88) | 3172 (12.35) | 4123 (10.94) | 912 (10.33) | 2 > 3,4 > 1 |
| Domiciliary Care for Homeless Veterans | 7031 (7.74) | 796 (4.26) | 2861 (11.13) | 2902 (7.70) | 472 (5.35) | 2 > 3 > 4 > 1 |
Note. HUD = Housing and Urban Development. Rows arranged by order of program admissions. Percentages may not sum to 100% because of rounding.
Table 4 shows the actual admission patterns among the 4 latent classes of homeless veterans after referral. Similar to their referral patterns, the relatively few problems group was more likely to be admitted to the HUD-VA Supportive Housing program than other groups, the disabling medical problems group was least likely to be admitted to the Grant and Per Diem program, the poverty–substance abuse–incarceration group was most likely to be admitted to the Healthcare for Re-Entry Veterans program, and the dual diagnosis group was most likely to be admitted to the Veterans Justice Outreach program and the Domiciliary Care for Homeless Veterans program.
DISCUSSION
We found that a national sample of over 120 000 homeless veterans could be classified into 4 groups: (1) a group with relatively low probabilities for 9 homeless risk factors; (2) a dual diagnosis group with high probabilities for severe mental illness and comorbid substance use disorder; (3) a group with high probabilities for multiple risk factors, particularly poverty, substance abuse, and history of incarceration; and (4) a group with high probabilities for disabling medical problems. Identification of these groups not only illustrated the heterogeneity of the homeless veteran population but also extended previous studies on smaller samples that found distinct homeless groups characterized by alcohol or drug abuse problems, psychiatric impairments, problems in multiple domains, and a group with few of these problems.4,6–8
The 2 largest groups of homeless veterans found in this study both had high probabilities for substance use disorders (dual diagnosis group and the poverty–substance abuse–incarceration group), consistent with numerous studies documenting substance abuse as one of the strongest risk factors for homelessness.13,19,28 The smallest group, which had chronic medical problems that were likely to have been disabling as reflected by high monthly disability payments they received, was not previously identified in the literature, possibly because previous classificatory studies typically did not include assessments of both psychosocial and medical problems, with a few exceptions.8 Nonetheless, homeless veterans with chronic medical conditions might require special medical attention, especially with conditions such as HIV and tuberculosis, which are concerns among homeless populations.42 The fourth group, representing nearly one fifth of homeless veterans, had relatively few problems. This was a group that might be important to identify for newly developed housing interventions, such as rapid re-housing and other secondary prevention efforts.11
These 4 latent classes might be important in understanding how homeless veterans differed from each other and what services might be most appropriate for each group. Examination of point of initial contact, program referral, and program admission patterns revealed noteworthy distinctions that provided some degree of validation for the 4 latent classes and supported the need for a diversity of homeless services to meet diverse client needs. For example, the relatively few problems group was more likely to be initially contacted through community outreach than other groups, suggesting community outreach was most effective for those who wanted to be found, but those with relatively more problems might not be as easily contacted through this type of outreach. Other forms of outreach, such as through the criminal justice system for those in the poverty–substance abuse–incarceration group, might be needed.
In program referral and admission patterns, the dual diagnosis group was more likely to be referred and admitted to the Veterans Justice Outreach program (jail diversion program) than other groups, likely because of their higher probability for substance use–related crimes. The poverty–substance abuse–incarceration group was more likely to be referred and admitted to the Healthcare for Re-Entry Veterans program (prisoner re-entry program) than other groups because of their current incarceration status, and the disabling medical problems group was more likely to be referred to VA medical services and less likely to be referred to the Grant and Per Diem program (transitional housing) than other groups because of their medical conditions and low level of problems with substance use.
Interestingly, compared with other groups, the relatively few problems group was most likely to be referred and admitted to the HUD-VA Supportive Housing program, whereas the 2 groups with substance abuse problems were most likely to be referred to the more restrictive and structured programs: the Grant and Per Diem program or the Domiciliary Care for Homeless Veterans program (both transitional or residential treatment programs). These findings suggested permanent supportive housing was seen by service providers as most suitable for homeless veterans who were “housing ready.” By contrast, those with substance use problems tended to be referred to more structured services, presumably to foster sobriety and prepare them for life in permanent housing. This approach was discussed recently as an alternative to harm reduction-oriented Housing First models.43 However, this referral pattern might change because the Housing First model,44,45 which seeks to provide immediate housing to homeless individuals with no requirements for sobriety or treatment, is being promoted in the HUD-VA Supportive Housing program.41
Limitations
There were several limitations to this study worth noting. Administrative data from HOMES were used, including clinical diagnoses, which relied on the accurate and diligent documentation of VA clinicians. Risk factors for homelessness were dichotomized, although some variables should arguably be treated as continuous variables. Longitudinal data on client outcomes were not available, which would have been useful to examine how groups differed over time. The group labeled with relatively few problems was only based on the risk factors examined in the study, and there might be other risk factors and needs of this group that were not discovered. It was also notable that this group was younger, more highly educated, and more likely to be female than other groups, which might be related to its higher functioning status, although further research is needed to determine this. Future studies using more complex mixture modeling techniques that incorporate categorical and continuous variables and longitudinal data might provide more refined groupings and additional meaningful information about long-term outcomes. The limitations of the study were counterbalanced by its strengths, which included a large national sample, use of a statistical technique more advanced than commonly used cluster analytic procedures, and examination of program processes in real-world conditions.
Conclusions
Four subgroups of homeless veterans were identified based on known, modifiable risk factors for homelessness, which were related to different program referral and admission patterns. The heterogeneous risk and need profiles of homeless veterans supported the diversity of VA homeless services available and encouraged the continued development of specialized services to meet their diverse needs consistent with the “matching hypothesis” in the substance abuse field.46 The results also illustrated the utility of a national homeless registry, such as HOMES, in monitoring program development and operation.
Acknowledgments
This work was supported by a career development award-2 through the Department of Veterans Affairs, Health Services Research, and Development service, and approved by the National Center on Homelessness Among Veterans.
Note. The views presented here are those of the authors alone, and do not represent the position of any federal agency or of the United States Government.
Human Participant Protection
This study was approved by the institutional review boards of the VA Connecticut Healthcare System and Yale University.
References
- 1.Borus JF. De-institutionalization of the chronically mentally ill. N Engl J Med. 1981;305(6):339–342. doi: 10.1056/NEJM198108063050609. [DOI] [PubMed] [Google Scholar]
- 2.Feldman S. Out of the hospital, onto the streets: the overselling of benevolence. Hastings Cent Rep. 1983;13(3):5–7. [PubMed] [Google Scholar]
- 3.Leff HS, Chow CM, Pepin R, Conley J, Allen IE, Seaman CA. Does one size fit all? What we can and can’t learn from a meta-analysis of housing models for persons with mental illness. Psychiatr Serv. 2009;60(4):473–482. doi: 10.1176/ps.2009.60.4.473. [DOI] [PubMed] [Google Scholar]
- 4.Humphreys K. Sequential validation of cluster analytic subtypes of homeless veterans. Am J Community Psychol. 1995;23(1):75–98. [Google Scholar]
- 5.Kuhn R, Culhane D. Applying cluster analysis to test a typology of homelessness by pattern of shelter utilization: results from the analysis of administrative data. Am J Community Psychol. 1998;26(2):207–232. doi: 10.1023/a:1022176402357. [DOI] [PubMed] [Google Scholar]
- 6.Solarz A, Bogat GA. When social support fails: the homeless. J Community Psychol. 1990;18(1):79–96. [Google Scholar]
- 7.Mowbray CT, Bybee D, Cohen E. Describing the homeless mentally ill: cluster analysis results. Am J Community Psychol. 1993;21(1):67–93. doi: 10.1007/BF00938208. [DOI] [PubMed] [Google Scholar]
- 8.Aubry T, Klodawsky F, Coulombe D. Comparing the housing trajectories of different classes within a diverse homeless population. Am J Community Psychol. 2012;49(1-2):142–155. doi: 10.1007/s10464-011-9444-z. [DOI] [PubMed] [Google Scholar]
- 9.Shelton KH, Mackie P, Bree M, Taylor PJ, Evans S. Opening doors for all American youth? Evidence for federal homelessness policy. Housing Policy Debate. 2012;22(3):483–504. [Google Scholar]
- 10.Bonin JP, Fournier L, Blais R. A typology of mentally disordered users of resources for homeless people: towards better planning of mental health services. Adm Policy Ment Health. 2009;36(4):223–235. doi: 10.1007/s10488-009-0206-2. [DOI] [PubMed] [Google Scholar]
- 11.Culhane DP, Metraux S, Byrne T. A prevention-centered approach to homelessness assistance: a paradigm shift? Housing Policy Debate. 2011;21(2):295–315. [Google Scholar]
- 12.Caton CL, Shrout PE, Dominguez B, Eagle PF, Opler LA, Cournos F. Risk factors for homelessness among women with schizophrenia. Am J Public Health. 1995;85(8 Pt 1):1153–1156. doi: 10.2105/ajph.85.8_pt_1.1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Folsom DP, Hawthorne W, Lindamer LA et al. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am J Psychiatry. 2005;162:370–376. doi: 10.1176/appi.ajp.162.2.370. [DOI] [PubMed] [Google Scholar]
- 14.Fischer PJ, Breakey WR. The epidemiology of alcohol, drug, and mental disorders among homeless persons. Am Psychol. 1991;46(11):1115–1128. doi: 10.1037//0003-066x.46.11.1115. [DOI] [PubMed] [Google Scholar]
- 15.Greenberg GA, Rosenheck RA. Correlates of past homelessness in the National Epidemiological Survey on Alcohol and Related Conditions. Adm Policy Ment Health. 2010;37(4):357–366. doi: 10.1007/s10488-009-0243-x. [DOI] [PubMed] [Google Scholar]
- 16.Cortes A, Leopold J, Buron L, Khadduri J, Culhane DP. The 2010 Annual Homeless Assessment Report to Congress. Washington, DC: U.S. Department of Housing and Urban Development; 2011. [Google Scholar]
- 17.Koegel P, Melamid E, Burnam A. Childhood risk factors for homelessness among homeless adults. Am J Public Health. 1995;85(12):1642–1649. doi: 10.2105/ajph.85.12.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tsai J, Edens EL, Rosenheck RA. A typology of childhood problems among chronically homeless adults and its association with housing and clinical outcomes. J Health Care Poor Underserved. 2011;22(3):853–870. doi: 10.1353/hpu.2011.0081. [DOI] [PubMed] [Google Scholar]
- 19.Susser E, Moore R, Link B. Risk factors for homelessness. Epidemiol Rev. 1993;15(2):546–556. doi: 10.1093/oxfordjournals.epirev.a036133. [DOI] [PubMed] [Google Scholar]
- 20.Caton CL, Dominguez B, Schanzer B et al. Risk factors for long-term homelessness: findings from a longitudinal study of first-time homeless single adults. Am J Public Health. 2005;95(10):1753–1759. doi: 10.2105/AJPH.2005.063321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.US Department of Housing and Urban Development, US Department of Veterans Affairs. Veteran Homelessness: A Supplemental Report to the 2010 Annual Homeless Assessment Report to Congress. Washington, DC: US Department of Housing and Urban Development, Office of Community Planning and Development; US Department of Veterans Affairs, National Center on Homelessness Among Veterans; 2011. [Google Scholar]
- 22.Fargo J, Metraux S, Byrne T . Washington, DC: National Center on Homelessness Among Veterans; 2011. Prevalence and risk of homelessness among U.S. veterans: a multisite investigation. White Paper. [Google Scholar]
- 23.US Department of Veterans Affairs. Secretary Shinseki details plans to end homelessness for veterans. Available at: http://www.va.gov/opa/pressrel/pressrelease.cfm?id=1807. Accessed January 5, 2012.
- 24.Washington DL, Yano EM, McGuire J, Hines V, Lee M, Gelberg L. Risk factors for homelessness among women veterans. J Health Care Poor Underserved. 2010;21(1):82–91. doi: 10.1353/hpu.0.0237. [DOI] [PubMed] [Google Scholar]
- 25.Rosenheck R, Fontana A. A model of homelessness among male veterans of the Vietnam War generation. Am J Psychiatry. 1994;151(3):421–427. doi: 10.1176/ajp.151.3.421. [DOI] [PubMed] [Google Scholar]
- 26.Tsai J, Rosenheck RA. Conduct disorder behaviors, childhood family instability, and childhood abuse as predictors of severity of adult homelessness among American veterans. Soc Psychiatry Psychiatr Epidemiol. 2013;48(3):477–486. doi: 10.1007/s00127-012-0551-4. [DOI] [PubMed] [Google Scholar]
- 27.O’Connell MJ, Kasprow W, Rosenheck RA. Rates and risk factors for homelessness after successful housing in a sample of formerly homeless veterans. Psychiatr Serv. 2008;59(3):268–275. doi: 10.1176/ps.2008.59.3.268. [DOI] [PubMed] [Google Scholar]
- 28.Edens EL, Kasprow W, Tsai J, Rosenheck RA. Association of substance use and VA service-connected disability benefits with risk of homelessness among veterans. Am J Addict. 2011;20(5):412–419. doi: 10.1111/j.1521-0391.2011.00166.x. [DOI] [PubMed] [Google Scholar]
- 29.Goldstein G, Luther JF, Jacoby AM, Haas GL, Gordon AJ. A preliminary classification system for homeless veterans with mental illness. Psychol Serv. 2008;5(1):36–48. [Google Scholar]
- 30.Goldstein G, Luther JF, Jacoby AM, Haas GL. A taxonomy of medical comorbidity for veterans who are homeless. J Health Care Poor Underserved. 2008;19(3):991–1005. doi: 10.1353/hpu.0.0040. [DOI] [PubMed] [Google Scholar]
- 31.Seibyl CL, Medak S, Baldino L, Desai RA. The Twenty-Second Progress Report on the Department of Veterans Affairs (VA) Domiciliary Care for Homeless Veterans Program: Fiscal Year (FY) 2010. West Haven, CT: Northeast Program Evaluation Center; 2011. [Google Scholar]
- 32.US Department of Veterans Affairs. Health Care for Homeless Veterans Programs: Twenty-Fourth Annual Report. West Haven, CT: Northeast Program Evaluation Center; 2011. [Google Scholar]
- 33.US Department of Veterans Affairs. Department of Housing and Urban Development-Department of Veterans Affairs Supported Housing program (HUD-VASH) West Haven, CT: Northeast Program Evaluation Center; 2010. [Google Scholar]
- 34.US Department of Housing and Urban Development. Defining Chronic Homelessness: A Technical Guide for HUD Programs. Washington, DC: US Department of Housing and Urban Development; 2007. [Google Scholar]
- 35.McLachlan GJ, Basford KE. Mixture Models: Inference and Applications to clustering. New York: Marcel Dekker; 1988. [Google Scholar]
- 36.McLachlan G, Peel D. Finite Mixture Models. New York: Wiley-Interscience; 2000. [Google Scholar]
- 37.Magidson J, Vermunt JK. Latent class models for clustering: a comparison with K-means. Can J Market Res. 2002;20:37–44. [Google Scholar]
- 38.Muthen B. Latent variable analysis: growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. Handbook of Quantitative Methodology for the Social Sciences. Thousand Oaks, CA: Sage Publications; 2004. pp. 345–368. [Google Scholar]
- 39.Muthén B. Statistical and substantive checking in growth mixture modeling: comment on Bauer and Curran (2003) Psychol Methods. 2003;8(3):369–377. doi: 10.1037/1082-989X.8.3.369. [DOI] [PubMed] [Google Scholar]
- 40.Nylund KL, Asparouhov T, Muthen B. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Modeling. 2007;14(4):535–569. [Google Scholar]
- 41.US Interagency Council on Homelessness. Targeting Veterans Experiencing Chronic Homelessness and Using Housing First. Washington, DC: US Interagency Council on Homelessness; 2011. [Google Scholar]
- 42.Zolopa AR, Hahn JA, Gorter R et al. HIV and tuberculosis infection in San Francisco’s homeless adults: prevalence and risk factors in a representative sample. JAMA. 1994;272(6):455–461. [PubMed] [Google Scholar]
- 43.Kertesz SG, Crouch K, Milby JB, Cusimano RE, Schumacher JE. Housing First for homeless persons with active addiction: are we overreaching? Milbank Q. 2009;87(2):495–534. doi: 10.1111/j.1468-0009.2009.00565.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tsemberis S. From streets to homes: an innovative approach to supported housing for homeless adults with psychiatric disabilities. J Community Psychol. 1999;27(2):225–241. [Google Scholar]
- 45.Tsemberis S, Gulcur L, Nakae M. Housing first, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am J Public Health. 2004;94(4):651–656. doi: 10.2105/ajph.94.4.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Finney JW, Moos RH. Matching patients with treatment: conceptual and methodological issues. J Stud Alcohol. 1986;47(2):122–134. doi: 10.15288/jsa.1986.47.122. [DOI] [PubMed] [Google Scholar]