Abstract
Objectives. We comprehensively assessed health care utilization in a population-based sample of homeless adults and matched controls under a universal health insurance system.
Methods. We assessed health care utilization by 1165 homeless single men and women and adults in families and their age- and gender-matched low-income controls in Toronto, Ontario, from 2005 to 2009, using repeated-measures general linear models to calculate risk ratios and 95% confidence intervals (CIs).
Results. Homeless participants had mean rates of 9.1 ambulatory care encounters (maximum = 141.1), 2.0 emergency department (ED) encounters (maximum = 104.9), 0.2 medical–surgical hospitalizations (maximum = 14.9), and 0.1 psychiatric hospitalizations per person-year (maximum = 4.8). Rate ratios for homeless participants compared with matched controls were 1.76 (95% CI = 1.58, 1.96) for ambulatory care encounters, 8.48 (95% CI = 6.72, 10.70) for ED encounters, 4.22 (95% CI = 2.99, 5.94) for medical–surgical hospitalizations, and 9.27 (95% CI = 4.42, 19.43) for psychiatric hospitalizations.
Conclusions. In a universal health insurance system, homeless people had substantially higher rates of ED and hospital use than general population controls; these rates were largely driven by a subset of homeless persons with extremely high-intensity usage of health services.
Homelessness is a serious problem in North America. High rates of unemployment and mortgage foreclosures resulting from the recent global economic downturn have further perpetuated this crisis.1 Approximately 650 000 people will experience homelessness each night in the United States, of whom more than one third are people in families.2 More than 1.6 million Americans spend at least 1 night in an emergency shelter or transitional housing each year.2 In Toronto, Ontario, more than 4000 individuals experience homelessness on any given night, and approximately 27 000 people use emergency shelters each year.3,4
Compared with the general population, homeless people have higher rates of chronic and acute health conditions and are at increased risk for all-cause mortality.5–8 Despite their increased need for health services, homeless people are a marginalized population who frequently encounter barriers to accessing primary or preventive health care.6,9–17 In addition, they often face competing priorities for basic subsistence needs,18 factors that may result in delays in health care seeking, deterioration in health status, unmet needs for care, increased mortality, and use of more expensive forms of health care delivery.6,11,19–21
Evidence has suggested that homeless people can be more intensive users of health services than the general population,12,22–26 yet no comprehensive assessment of health care utilization among homeless persons is available. Such data are difficult to obtain in the United States using administrative databases because more than 50% of homeless adults lack any health insurance.12 Many previous studies have relied solely on self-reports,11,12,27–29 assessed only 1 type of health service (e.g., emergency department [ED] visits),22,26,30 lacked a comparison group in the general population,11,19 or exclusively assessed utilization for homeless individuals who had contact with the health care system.22,25,26,30
In this study, we examined health care utilization by a population-based cohort of homeless single men, single women, and adults in families using administrative data in a setting in which all residents, regardless of their housing, employment, or income status, are covered under a publicly funded universal health insurance system. We compared health care utilization rates of homeless individuals and age- and gender-matched low-income controls from the general population and examined patterns of health care utilization, with a focus on those considered to be frequent users of health services.
METHODS
We enrolled a representative cohort of 1189 homeless adults who have universal health insurance in Toronto. Participants were recruited over 12 consecutive months from December 2004 to December 2005 from homeless shelters and meal programs. Details of our recruitment strategy have previously been described.20,31,32 We stratified enrollment to obtain a 2:1:1 ratio of single men (i.e., men without dependent children), single women (i.e., women without dependent children), and adults with families (i.e., adults accompanied by a partner, dependent children, or both) to approximate the demographic profile of the homeless population and to ensure an adequate sample size for comparisons. In a pilot study, we determined that about 90% of homeless people in Toronto slept at shelters and 10% did not use shelters but used meal programs.33 We therefore recruited 90% of our sample at shelters and the remaining 10% at meal programs.
We defined homelessness as living during the past 7 days at a shelter, public place, vehicle, abandoned building, or someone else’s home and not having a home of one’s own. We excluded participants if they did not meet our definition of homelessness, were unable to communicate in English, or were unable to provide informed consent. Because the goal of recruiting participants at meal programs was to enroll homeless persons who did not use shelters, only meal program users who had not used a shelter in the past 7 days were eligible to participate. We also excluded individuals if they had never been issued a provincial health insurance number because this information was required for linkage to administrative data. Individuals were selected at random from bed lists or meal lines and assessed for their eligibility and willingness to participate. All participants provided written informed consent.
For the purposes of recruitment, we considered families as units. In instances in which 2 adults of the same family unit were present, we randomly selected 1 adult for inclusion in the analysis. Of the 2516 single adults and family units who were screened, 882 (35.1%) were ineligible to participate: 229 (9.1%) were not currently homeless, 104 (4.1%) were unable to communicate in English, 54 (2.1%) were persons recruited from meal programs who had used a shelter in the past 7 days, 53 (2.1%) were unable to provide informed consent, and 442 (17.6%) did not have a valid provincial health card number. An additional 443 (17.6%) individuals declined to participate and 2 were identified as duplicate or invalid records. In total, 1189 unique adults were included in the study, corresponding to a response rate of 73%. We obtained demographic and health status data for homeless participants using structured, in-person interviews. Components of the survey instrument have previously been described.20,31,32
Linkage to Administrative Data
We accessed health care utilization data through the Institute for Clinical Evaluative Sciences, an independent, nonprofit organization funded by the Ontario Ministry of Health and Long-Term Care. We linked to administrative data using each participant’s provincial health insurance number, a unique 10-digit number assigned to every eligible resident under the Ontario Health Insurance Plan.
We achieved an exact match between the participants’ provided provincial health number and the Institute for Clinical Evaluative Sciences registry of valid health numbers for 94% of participants. For the remaining participants for whom an exact match was not possible, either because the participant’s health number could not be obtained (3%) or the health number provided was not valid (3%), we made an effort to link the participant to the registry on the basis of first name, last name, gender, and date of birth. This procedure resulted in a match for an additional 4% of participants. Thus, we obtained health care utilization data for 1165 (98%) homeless persons.
Matched Controls
We identified age- and gender-matched low-income control individuals in Toronto using the Registered Persons Database, an administrative registry of all persons registered with the provincial health insurance plan in a given year. We converted 3-digit forward sortation areas into census tracts using the Postal Code Conversion File from Statistics Canada. Individuals were eligible to be a control if they resided in the City of Toronto, were alive and registered in the Registered Persons Database during the study recruitment period, and lived in a census tract belonging to the lowest income quintile of Toronto on the basis of data from the 2006 census.34 These census tracts make up one fifth of the city of Toronto’s population or just more than 500 000 people, of whom 40.9% live below the low-income cutoff rate (vs 24.4% for the entire city of Toronto).35 The average annual after-tax household income for individuals living in Toronto’s lowest income quintile is CAN $43 480 (range = $25 084–$78 279), and the unemployment rate is 10.4%.35 We matched eligible controls 1:1 to homeless participants by gender and birth year using an algorithm that randomly assigned 1 eligible individual to each homeless participant. We achieved matching for 1165 (100%) of the homeless participants who provided consent for data linkage and who possessed a valid personal health number.
Health Care Utilization Data
We obtained ambulatory care data from the Ontario Health Insurance Plan database of physician claims paid for under a fee-for-service remuneration system. Records were restricted to office-based physician claims; laboratory records and claims for nonmedical practitioners were excluded. We considered claims by the same physician for the same patient on the same day to be a single health care encounter.
We obtained data on ED visits from the National Ambulatory Care Reporting System. Planned or scheduled visits to the ED were excluded, as were duplicate records. We obtained hospitalization data from the Canadian Institute for Health Information Discharge Abstract Database and the Ontario Mental Health Reporting Systems database. Psychiatric admissions to inpatient mental health beds were considered separately from medical and surgical admissions. We excluded pregnancy-related encounters from all analyses to eliminate the effect of these encounters on gender-specific differences in rates, especially with respect to hospitalizations.
We estimated health care costs using episode-level data from the 2006 Medical Expenditure Panel Survey, sponsored by the Agency for Healthcare Research and Quality, for the US civilian noninstitutionalized population for hospital inpatient services, ED services, and office-based physician services.36 We multiplied the mean weighted expense per episode by the total number of encounters for each type of health care.
Analysis
We compared demographic and health status characteristics for homeless participants across demographic groups using analysis of variance for normally distributed continuous variables and the χ2 test for categorical variables. We assessed health care utilization for a follow-up period from the participant’s enrollment date into the study (in 2004–2005) to March 31, 2009. Health care utilization rates were calculated by dividing the total number of encounters for each source of health care by the total amount of time under observation during the study period (person-time at risk). We obtained date of death for homeless participants and matched control individuals from the Registered Persons Database and used it to adjust (if necessary) the person-time at risk. Using repeated-measures general linear models, we calculated risk ratios and 95% confidence intervals comparing annualized rates between homeless participants and matched control individuals.
Preliminary examination of the data indicated that a small number of homeless participants were disproportionately represented in the health care encounters data. To further investigate these frequent users, we performed additional analyses on the subset of homeless participants (n = 117) whose health care utilization rates were in the top decile of users within each type of health care. We defined cutoff values as follows: 23.0 encounters per person-year for ambulatory care, 4.7 encounters per person-year for EDs, 0.3 hospitalizations per person-year for medical–surgical hospitalizations, and 0.2 hospitalizations per person-year for psychiatric hospitalizations. Risk ratios were calculated for frequent users and their matched controls, as described in the preceding paragraph.
We performed analyses using SAS statistical analysis software, version 9.2 (SAS Institute, Cary, NC). A P value of .05 was considered statistically significant.
RESULTS
In total, we obtained health care utilization data for 1165 homeless participants, including 587 single men, 296 single women, and 282 adults with families who possessed a valid provincial health number (Table 1). The mean duration of follow-up was 3.9 years for homeless participants (SD = 0.3 years; range = 1.1–4.3 years) and 3.8 years for matched control individuals (SD = 0.5 years; range = 0.1–4.3 years).
TABLE 1—
Characteristics of Homeless Participants: Toronto, Ontario, 2005–2009
| Demographic Group, No. (%) or Mean ±SD |
|||||
| Characteristic | Total, No. (%) or Mean ±SD (n = 1165) | Single Men (n = 587) | Single Women (n = 296) | Adults with Families (n = 282) | P |
| Age, y | 36.1 ±12.4 | 38.5 ±12.7 | 35.2 ±13.1 | 32.3 ±9.5 | < .001 |
| Gender | … | ||||
| Male | 625 (53.6) | 587 (100.0) | 0 (0.0) | 38 (13.5) | |
| Female | 540 (46.4) | 0 (0.0) | 296 (100.0) | 244 (86.5) | |
| Lifetime duration of homelessness | < .001 | ||||
| < 2 y | 584 (50.1) | 220 (37.5) | 144 (48.7) | 220 (78.0) | |
| ≥ 2 y | 581 (49.9) | 367 (62.5) | 152 (51.4) | 62 (22.0) | |
| Race/ethnicity | < .001 | ||||
| White | 650 (55.8) | 383 (65.3) | 155 (52.4) | 112 (39.7) | |
| Black | 260 (22.3) | 84 (14.3) | 77 (26.0) | 99 (35.1) | |
| Aboriginal | 96 (8.2) | 54 (9.2) | 31 (10.5) | 11 (3.9) | |
| Other visible minorities | 159 (13.7) | 66 (11.2) | 33 (11.2) | 60 (21.3) | |
| Place of birth | < .001 | ||||
| Canada | 796 (68.3) | 445 (75.8) | 205 (69.3) | 146 (51.8) | |
| Outside Canada | 369 (31.7) | 142 (24.2) | 91 (30.7) | 136 (48.2) | |
| Highest level of education | < .001 | ||||
| Some high school or less | 587 (50.5) | 337 (57.6) | 132 (44.6) | 118 (42.0) | |
| High school diploma or equivalent | 248 (21.3) | 109 (18.6) | 71 (24.0) | 68 (24.2) | |
| College, vocational training, or higher | 327 (28.1) | 139 (23.8) | 93 (31.4) | 95 (33.8) | |
| Monthly income, CAN $ | < .001 | ||||
| < 500 | 562 (49.5) | 296 (51.9) | 161 (55.3) | 105 (38.3) | |
| 500–999 | 313 (27.6) | 147 (25.8) | 89 (30.6) | 77 (28.1) | |
| ≥ 1000 | 260 (22.9) | 127 (22.3) | 41 (14.1) | 92 (33.6) | |
| Chronic health conditionsa | .012 | ||||
| None | 470 (40.4) | 214 (36.5) | 121 (40.9) | 135 (47.9) | |
| 1 | 324 (27.8) | 187 (31.9) | 70 (23.7) | 67 (23.8) | |
| 2 | 202 (17.4) | 101 (17.2) | 54 (18.2) | 47 (16.7) | |
| ≥ 3 | 168 (14.4) | 84 (14.3) | 51 (17.2) | 33 (11.7) | |
| Alcohol problem in past 30 db | 339 (29.1) | 248 (42.3) | 64 (21.6) | 27 (9.6) | < .001 |
| Drug problem in past 30 db | 458 (39.1) | 307 (52.3) | 118 (39.9) | 33 (11.7) | < .001 |
| Mental health problem in past 30 db | 438 (37.6) | 201 (34.2) | 136 (46.0) | 101 (35.8) | .003 |
Chronic health conditions include diabetes; anemia; hypertension; heart disease and stroke; liver problems (including chronic viral hepatitis); arthritis, rheumatism, or joint problems; cancer; physical handicaps; or HIV/AIDS.
Alcohol, drug, and mental health problems in the past 30 days were assessed using the Addiction Severity Index.37–39
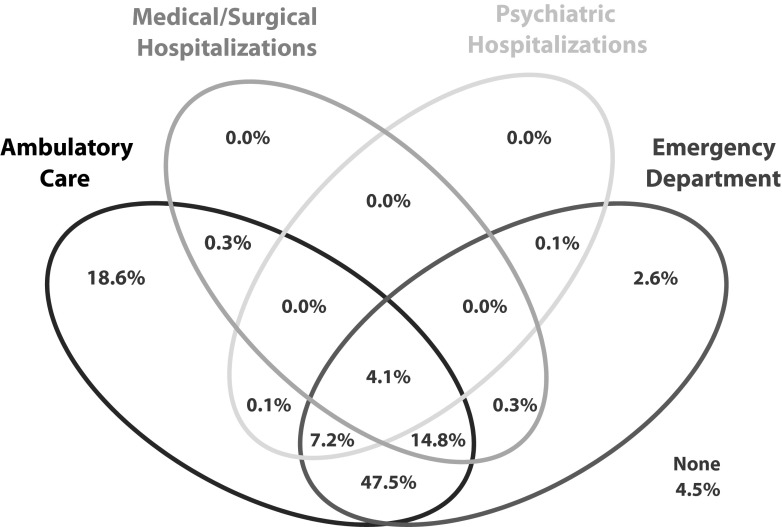
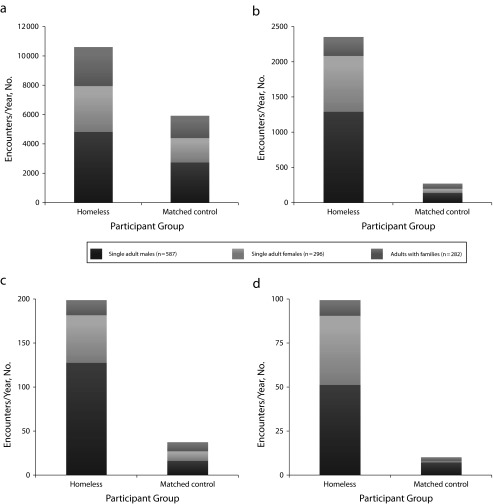
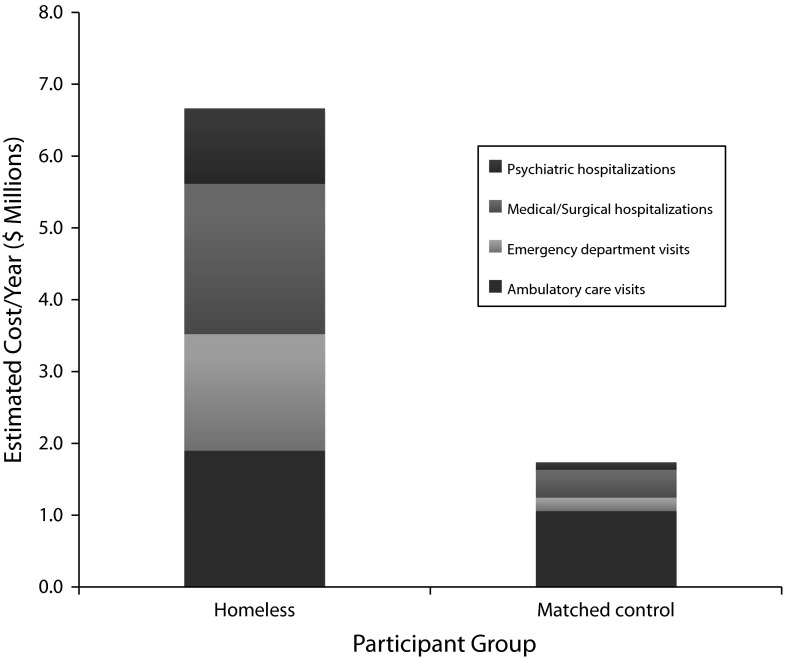
During the observation period, 95.5% of homeless participants had at least 1 encounter with health services: 92.5% visited a physician’s office, 76.6% visited an ED, 19.5% were hospitalized in a medical–surgical bed, and 11.5% were hospitalized in a psychiatric bed (Figure 1). By comparison, 84.2% of matched controls had at least 1 encounter with health services: 83.8% visited a physician’s office, 35.6% visited an ED, 7.1% were hospitalized in a medical–surgical bed, and 1.6% were hospitalized in a psychiatric bed. Homeless participants had an average of 13 240 encounters with health services annually (10 594 ambulatory care encounters, 2348 ED encounters, 199 medical–surgical hospitalizations, and 99 psychiatric hospitalizations), whereas their matched controls had an average of 6220 encounters annually (5903 ambulatory care encounters, 270 ED encounters, 37 medical–surgical hospitalizations, and 10 psychiatric hospitalizations; Figure 2). On the basis of mean weighted costs from the Medical Expenditure Panel Survey, these encounters represented an estimated US $6.67 million annually (or US $5725 per person per year) in health care expenditures for homeless participants compared with US $1.75 million (or US $1500 per person per year) for matched controls (Figure 3).
FIGURE 1—
Venn diagram showing patterns of health care use among homeless participants over a mean follow-up duration of 3.9 years: Toronto, Ontario, 2005–2009.
FIGURE 2—
Annual number of health care encounters among homeless participants and age- and gender-matched low-income control individuals by demographic group for (a) ambulatory care, (b) emergency department care, (c) medical-surgical hospitalization, and (d) psychiatric hospitalization: Toronto, Ontario, 2005–2009.
FIGURE 3—
Estimated health care expenditures per year among 1165 homeless participants and 1165 age- and gender-matched low-income control individuals, by type of health care: Toronto, Ontario, 2005–2009.
Note. Expenditures are based on mean weighted cost episode-level estimates from the Medical Expenditure Panel Survey for hospital inpatient services, emergency room services, and office-based physician services36; estimated costs are in US dollars.
Homeless participants had a mean rate of 9.1 encounters per person-year with ambulatory care, 2.0 encounters per person-year with EDs, 0.2 medical–surgical hospitalizations per person-year, and 0.1 psychiatric hospitalizations per person-year (Table 2). The highest rates occurred among homeless single men and single women (Table 2). The rate ratios comparing homeless participants with matched controls were 1.76 for ambulatory care encounters (95% CI = 1.58, 1.96; P < .001), 8.48 for ED encounters (95% CI = 6.72, 10.70; P < .001), 4.22 for medical–surgical hospitalizations (95% CI = 2.99, 5.94; P < .001), and 9.27 (95% CI = 4.42, 19.43; P < .001) for psychiatric hospitalizations.
TABLE 2—
Rates of Health Care Utilization and Risk Ratios Between Homeless Participants and Age- and Gender-Matched Low-Income Control Individuals by Type of Health Care and Demographic Group: Toronto, Ontario, 2005–2009
| Type of Health Care | Homeless Participants, Mean (SD) per Person-Year | Matched Controls, Mean (SD) per Person-Year | RR (95% CI) |
| Ambulatory care | |||
| Single men | 8.18 (12.40) | 4.64 (6.98) | 1.72 (1.45, 2.04) |
| Single women | 10.54 (13.18) | 5.66 (6.39) | 1.85 (1.53, 2.22) |
| Adults with families | 9.47 (11.76) | 5.34 (5.12) | 1.74 (1.45, 2.09) |
| Total | 9.09 (12.48) | 5.07 (6.44) | 1.76 (1.58, 1.96) |
| Emergency department | |||
| Single men | 2.20 (4.50) | 0.23 (0.73) | 9.19 (6.62, 12.75) |
| Single women | 2.67 (7.35) | 0.20 (0.42) | 13.31 (8.94, 19.81) |
| Adults with families | 0.95 (2.86) | 0.27 (0.82) | 3.46 (2.13, 5.60) |
| Total | 2.02 (5.12) | 0.23 (0.69) | 8.48 (6.72, 10.70) |
| Medical–surgical hospitalizationsa | |||
| Single men | 0.22 (0.96) | 0.03 (0.14) | 5.39 (3.33, 8.75) |
| Single women | 0.18 (0.75) | 0.04 (0.18) | 4.80 (2.43, 9.49) |
| Adults with families | 0.06 (0.23) | 0.04 (0.16) | 1.77 (0.91, 3.43) |
| Total | 0.17 (0.79) | 0.03 (0.16) | 4.22 (2.99, 5.94) |
| Psychiatric hospitalizations | |||
| Single men | 0.09 (0.41) | 0.01 (0.14) | 6.51 (2.42, 17.50) |
| Single women | 0.13 (0.44) | 0.00 (0.02) | 76.72 (18.11, 324.92) |
| Adults with families | 0.03 (0.22) | 0.01 (0.05) | 3.58 (1.21, 10.61) |
| Total | 0.09 (0.38) | 0.1 (1.0) | 9.27 (4.42, 19.43) |
Note. CI = confidence interval; RR = rate ratio.
Refers to hospitalization admissions to nonpsychiatric acute-care beds.
The frequent users of each type of health care service represented, by design, 10% of the homeless population, but they accounted for 43.0% of the total annual ambulatory care encounters, 60.3% of ED encounters, 79.9% of medical–surgical hospitalizations, and 85.9% of psychiatric hospitalizations. Among the frequent ED users, 49.1% were also frequent users of medical–surgical hospitalizations and 40.2% were also frequent users of psychiatric hospitalizations. Twenty-five participants (2.2%) were frequent users of both medical–surgical hospitalizations and psychiatric hospitalizations, and 11 participants (0.9%) were frequent users of all 4 types of health care. Frequent users had a mean rate of 39.0 encounters per person-year with ambulatory care (maximum = 141.1 per person-year), 12.1 encounters per person-year with EDs (maximum = 104.9 per person-year), 1.5 medical–surgical hospitalizations per person-year (maximum = 14.9 per person-year), and 0.8 psychiatric hospitalizations per person-year (maximum = 4.8 per person-year). Compared with their matched controls, frequent users were 6.59 times (95% CI = 5.32, 8.17; P < .001) more likely to use ambulatory care services, 55.65 times (95% CI = 36.54, 84.73; P < .001) more likely to visit an ED, and 55.84 times (95% CI = 29.02, 107.44; P < .001) more likely to be hospitalized in a medical–surgical bed.
DISCUSSION
Our findings show that, within a system of universal health insurance, people who are homeless have substantially higher rates of health care utilization than age- and gender-matched low-income control individuals from the general population, particularly for ED and inpatient hospital use. We observed notable differences when comparisons were stratified by demographic group; single men and women had the largest differences in rates compared with their matched control counterparts. Rates among homeless adults in families, although significantly higher than those of their matched controls, were not as extreme as the differences observed among single adults for all types of health care. Examination of health care utilization patterns suggests that the vast majority of ED use occurred among participants who had at least 1 ambulatory care encounter during the study period, contrary to the hypothesis that homeless individuals present to the ED because they lack adequate access to primary care.11,19,40
Our data also show that the homeless population includes a subset of individuals who are extremely frequent users of health services. This very high-intensity service use by a relatively small number of homeless people can have a substantial impact on the health care system, including higher health care costs and ED overcrowding.11,19,26,41 Total health care expenditures for homeless persons in our sample were estimated at US $6.7 million per year. This estimate is likely conservative given that homeless persons generally have longer inpatient stays, and consequently higher total hospital costs, than housed patients.42
Our findings, by accurately quantifying health care utilization across multiple sources of care, support prior research in this area.12,22–26 In previous studies, homelessness has been associated with more frequent visits to the ED and longer inpatient stays.22,24–26 Studies based on self-report have shown that ED use among homeless persons is 3 times higher than US norms,11 and hospitalization rates are 4 times higher.12 In a national probability sample of ED encounters, homeless persons contributed 0.5% of total ED encounters but represented only 0.25% of the general population.30
Several factors explain why homelessness is associated with intensive health care utilization. Homeless people have an inherently greater need for health services, because of their high burden of disease from acute and chronic health conditions and the effects of socioeconomic deprivation.5,43,44 Indeed, our data show that more than one half of homeless participants in our sample reported having at least 1 chronic health condition, and self-reported mental health and substance use problems were highly prevalent. In addition to increased need factors, nonfinancial barriers such as lack of knowledge regarding where to obtain care, lack of transportation, lack of child care, perceived discrimination in health care settings, and cognitive impairment may contribute to delayed presentation for care and high rates of ED use.10–17
Our findings have important policy implications for the effective organization and delivery of health services, especially given recent legislative changes to the US health care system that expand Medicaid coverage to low-income Americans. Traditionally, a lack of health insurance has been identified as a primary barrier to obtaining ambulatory care in the United States, potentially resulting in inappropriate ED use and avoidable hospitalizations.12 However, as our findings demonstrate, homeless individuals within a system of universal health insurance continue to have much higher rates of ED and inpatient hospital use than population-based controls. The provision of universal health insurance, although vital, will not fully address the barriers to appropriate health care for this vulnerable population. Efforts to reduce the frequency of ED encounters and hospitalizations will also require reducing nonfinancial barriers to obtaining appropriate ambulatory care, improving the long-term management of physical and mental illnesses, and addressing structural factors such as a lack of stable housing.10–17,20,43,45
Limitations
This study has certain limitations that should be acknowledged. Homelessness was assessed at 1 point in time and cannot be assumed for the entire duration of follow-up.46,47 Our sampling strategy excluded individuals who did not use either shelters or meal programs; however, prior research has suggested that the unsheltered homeless population in Toronto is very small.4 Homeless participants were required to have a valid provincial health card number to be eligible, which may have biased our sample toward participants who have better access to the health care system. Furthermore, 18% of homeless individuals who were screened declined to participate in our study, which may have decreased the representativeness of our homeless sample. We included only ambulatory encounters paid for under a fee-for-service remuneration system; these data miss approximately 18% of total physician expenditures in Ontario paid for under alternative payment plans.48 As a result, our data may underestimate health services utilization among homeless participants who access health care at low-barrier sites such as community health centers. We identified age- and gender-matched population controls using administrative registries; as such, limited demographic information was available for matching. Low-income status for each control was determined at a neighborhood level on the basis of census tract and does not necessarily correspond to income status at the individual level. We were unable to adjust our analyses for health care need because survey data were not available for matched controls.
Conclusions
Our results comprehensively delineate at a population level the very high rates of health care utilization among homeless adults in a system in which all residents, regardless of housing, employment, or income status, have access to universal health insurance coverage. Our findings show that in this setting, homelessness is associated with substantially greater use of health services in comparison with low-income, population-based controls, independent of the effects of age and gender. These differences are driven to a substantial extent by a small subset of homeless individuals who are extremely high-intensity users of EDs and hospitals. Interventions that focus on providing more effective care for this group of high users have the potential to have a substantial impact on both individual- and system-level outcomes.
Acknowledgments
This project was supported by operating grants from the Agency for Healthcare Research and Quality (1 R01 HS014129-01) and the Canadian Institutes of Health Research (MOP-62736) and by an Interdisciplinary Capacity Enhancement grant on Homelessness, Housing, and Health from the Canadian Institutes of Health Research (HOA-80066). This study was supported by the Institute for Clinical Evaluative Sciences (ICES) and the Centre for Research on Inner City Health, which is funded by annual grants from the Ontario Ministry of Health and Long-Term Care.
Note. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the article. The opinions, results, and conclusions reported in this article are the views of the authors and do not necessarily reflect the views of any of the above-named organizations. No endorsement by ICES or the Ontario Ministry of Health and Long-Term Care should be intended or inferred.
Human Participant Protection
This study was approved by the Research Ethics Board at St. Michael’s Hospital in Toronto, Canada. All participants provided written informed consent.
References
- 1.National Coalition for the Homeless. Foreclosure to Homelessness 2009: The Forgotten Victims of the Subprime Crisis. Washington, DC: National Coalition for the Homeless; 2009. [Google Scholar]
- 2.US Department of Housing and Urban Development. The 2010 Annual Homeless Assessment Report to Congress. Washington, DC: US Department of Housing and Urban Development, Office of Community Planning and Development; 2010.
- 3. City of Toronto. 2010 per diem rates for the purchase of service shelter system and results of the review of the per diem funding model: Appendix D: total number of unique individuals using the shelter system—2000–2008. Available at: http://www.toronto.ca/housing/research-reports-appendices.htm. Accessed July 27, 2013.
- 4.City of Toronto. Street Needs Assessment Results. Toronto, ON, Canada: Shelter, Support, and Housing Administration, City of Toronto; 2009. [Google Scholar]
- 5.Goering P, Tolomiczenko G, Sheldon T, Boydell K, Wasylenki D. Characteristics of persons who are homeless for the first time. Psychiatr Serv. 2002;53(11):1472–1474. doi: 10.1176/appi.ps.53.11.1472. [DOI] [PubMed] [Google Scholar]
- 6.Hwang SW, Dunn JR. Homeless people. In: Galea S, Vlahov D, editors. Handbook of Urban Health: Populations, Methods, and Practice. New York, NY: Springer; 2005. pp. 21–41. [Google Scholar]
- 7.Hwang SW, Wilkins R, Tjepkema M, O’Campo PJ, Dunn JR. Mortality among residents of shelters, rooming houses, and hotels in Canada: 11 year follow-up study. BMJ. 2009;339 doi: 10.1136/bmj.b4036. b4036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khandor E, Mason K. The Street Health Report 2007. Toronto, ON, Canada: Street Health; 2007. [Google Scholar]
- 9.Hwang SW. Homelessness and health. CMAJ. 2001;164(2):229–233. [PMC free article] [PubMed] [Google Scholar]
- 10.Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21(1):71–77. doi: 10.1111/j.1525-1497.2005.00278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kushel MB, Perry S, Bangsberg D, Clark R, Moss AR. Emergency department use among the homeless and marginally housed: results from a community-based study. Am J Public Health. 2002;92(5):778–784. doi: 10.2105/ajph.92.5.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200–206. doi: 10.1001/jama.285.2.200. [DOI] [PubMed] [Google Scholar]
- 13.Lewis JH, Andersen RM, Gelberg L. Health care for homeless women. J Gen Intern Med. 2003;18(11):921–928. doi: 10.1046/j.1525-1497.2003.20909.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lim YW, Andersen R, Leake B, Cunningham W, Gelberg L. How accessible is medical care for homeless women? Med Care. 2002;40(6):510–520. doi: 10.1097/00005650-200206000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Rosenheck R, Lam JA. Client and site characteristics as barriers to service use by homeless persons with serious mental illness. Psychiatr Serv. 1997;48(3):387–390. doi: 10.1176/ps.48.3.387. [DOI] [PubMed] [Google Scholar]
- 16.Weinreb L, Goldberg R, Perloff J. Health characteristics and medical service use patterns of sheltered homeless and low-income housed mothers. J Gen Intern Med. 1998;13(6):389–397. doi: 10.1046/j.1525-1497.1998.00119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weinreb L, Perloff J, Goldberg R, Lessard D, Hosmer DW. Factors associated with health service utilization patterns in low-income women. J Health Care Poor Underserved. 2006;17(1):180–199. doi: 10.1353/hpu.2006.0036. [DOI] [PubMed] [Google Scholar]
- 18.Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997;87(2):217–220. doi: 10.2105/ajph.87.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Han B, Wells BL. Inappropriate emergency department visits and use of the Health Care for the Homeless Program services by homeless adults in the northeastern United States. J Public Health Manag Pract. 2003;9(6):530–537. doi: 10.1097/00124784-200311000-00014. [DOI] [PubMed] [Google Scholar]
- 20.Hwang SW, Ueng JJ, Chiu S et al. Universal health insurance and health care access for homeless persons. Am J Public Health. 2010;100(8):1454–1461. doi: 10.2105/AJPH.2009.182022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hwang SW, O’Connell JJ, Lebow JM, Bierer MF, Orav EJ, Brennan TA. Health care utilization among homeless adults prior to death. J Health Care Poor Underserved. 2001;12(1):50–58. doi: 10.1353/hpu.2010.0595. [DOI] [PubMed] [Google Scholar]
- 22.D’Amore J, Hung O, Chiang W, Goldfrank L. The epidemiology of the homeless population and its impact on an urban emergency department. Acad Emerg Med. 2001;8(11):1051–1055. doi: 10.1111/j.1553-2712.2001.tb01114.x. [DOI] [PubMed] [Google Scholar]
- 23.Kessell ER, Bhatia R, Bamberger JD, Kushel MB. Public health care utilization in a cohort of homeless adult applicants to a supportive housing program. J Urban Health. 2006;83(5):860–873. doi: 10.1007/s11524-006-9083-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mandelberg JH, Kuhn RE, Kohn MA. Epidemiologic analysis of an urban, public emergency department’s frequent users. Acad Emerg Med. 2000;7(6):637–646. doi: 10.1111/j.1553-2712.2000.tb02037.x. [DOI] [PubMed] [Google Scholar]
- 25.Pearson DA, Bruggman AR, Haukoos JS. Out-of-hospital and emergency department utilization by adult homeless patients. Ann Emerg Med. 2007;50(6):646–652. doi: 10.1016/j.annemergmed.2007.07.015. [DOI] [PubMed] [Google Scholar]
- 26.Salit SA, Kuhn EM, Hartz AJ, Vu JM, Mosso AL. Hospitalization costs associated with homelessness in New York City. N Engl J Med. 1998;338(24):1734–1740. doi: 10.1056/NEJM199806113382406. [DOI] [PubMed] [Google Scholar]
- 27.Nyamathi AM, Leake B, Gelberg L. Sheltered versus nonsheltered homeless women. J Gen Intern Med. 2000;15(8):565–572. doi: 10.1046/j.1525-1497.2000.07007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O’Toole TP, Gibbon JL, Hanusa BH, Fine MJ. Utilization of health care services among subgroups of urban homeless and housed poor. J Health Polit Policy Law. 1999;24(1):91–114. doi: 10.1215/03616878-24-1-91. [DOI] [PubMed] [Google Scholar]
- 29.Padgett DK, Struening EL, Andrews H, Pittman J. Predictors of emergency room use by homeless adults in New York City: the influence of predisposing, enabling and need factors. Soc Sci Med. 1995;41(4):547–556. doi: 10.1016/0277-9536(94)00364-y. [DOI] [PubMed] [Google Scholar]
- 30.Ku BS, Scott KC, Kertesz SG, Pitts SR. Factors associated with use of urban emergency departments by the US homeless population. Public Health Rep. 2010;125(3):398–405. doi: 10.1177/003335491012500308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chiu S, Redelmeier DA, Tolomiczenko G, Kiss A, Hwang SW. The health of homeless immigrants. J Epidemiol Community Health. 2009;63(11):943–948. doi: 10.1136/jech.2009.088468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hwang SW, Colantonio A, Chiu S et al. The effect of traumatic brain injury on the health of homeless people. CMAJ. 2008;179(8):779–784. doi: 10.1503/cmaj.080341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hwang SW, Chiu S, Kiss A et al. Use of meal programs and shelters by homeless people in Toronto [abstract] J Urban Health. 2005;82(suppl 2) ii46. [Google Scholar]
- 34.Statistics Canada. 2006 Census. Available at: http://www12.statcan.gc.ca/census-recensement/2006/index-eng.cfm. Accessed May 8, 2012. [Google Scholar]
- 35.McKeown D, MacCon K, Day N, Fleiszer P, Scott F, Wolfe SA. The Unequal City: Income and Health Inequalities in Toronto. Toronto, ON, Canada: Toronto Public Health, City of Toronto; 2008. [Google Scholar]
- 36.Agency for Healthcare Research and Quality. Medical expenditure panel survey. Available at: http://meps.ahrq.gov/mepsweb. Accessed September 28, 2012. [DOI] [PubMed]
- 37.McGahan PL, Griffith JA, Parente R, McLellan AT. Addiction Severity Index: Composite Scores Manual. Philadelphia: University of Pennsylvania/Veterans Administration Center for Studies of Addiction; 1986. [Google Scholar]
- 38.McLellan AT, Kushner H, Metzger D et al. The fifth edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- 39.Burt MR, Aron LY, Douglas T. Homelessness: Programs and the People They Serve. Findings of the National Survey of Homeless Assistance Providers and Clients. Washington, DC: Interagency Council on the Homeless; 1999. Rep. No. 6-2-6-3. [Google Scholar]
- 40.Newton MF, Keirns CC, Cunningham R, Hayward RA, Stanley R. Uninsured adults presenting to US emergency departments: Assumptions vs data. JAMA. 2008;300(16):1914–1924. doi: 10.1001/jama.300.16.1914. [DOI] [PubMed] [Google Scholar]
- 41.Derlet R, Richards JR, Kravitz RL. Frequent overcrowding in US emergency departments. Acad Emerg Med. 2001;8(2):151–155. doi: 10.1111/j.1553-2712.2001.tb01280.x. [DOI] [PubMed] [Google Scholar]
- 42.Hwang SW, Weaver J, Aubry T, Hoch JS. Hospital costs and length of stay among homeless patients admitted to medical, surgical, and psychiatric services. Med Care. 2011;49(4):350–354. doi: 10.1097/MLR.0b013e318206c50d. [DOI] [PubMed] [Google Scholar]
- 43.Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 44.Rodriguez RM, Fortman J, Chee C, Ng V, Poon D. Food, shelter and safety needs motivating homeless persons’ visits to an urban emergency department. Ann Emerg Med. 2009;53(5):598–602. doi: 10.1016/j.annemergmed.2008.07.046. [DOI] [PubMed] [Google Scholar]
- 45.Khandor E, Mason K, Chambers C, Rossiter K, Cowan L, Hwang SW.Access to primary health care among homeless adults in Toronto, Canada: results from the Street Health survey Open Med 20115(2e94 [PMC free article] [PubMed] [Google Scholar]
- 46.Aubry T, Klodawsky F, Nemiroff R, Birnie S, Bonetta C. Panel Study on Persons who are Homeless in Ottawa: Phase Two Results. Ottawa, ON, Canada: Centre for Research on Community Services, University of Ottawa; 2007. [Google Scholar]
- 47.Culhane D, Dejowski EF, Ibanez J, Needham E, Macchina I. Public shelter admission rates in Philadelphia and New York City: the implications of turnover for sheltered population counts. Housing Policy Debate. 1994;5(2):107–140. [Google Scholar]
- 48.Canadian Institute for Health Information. Physicians in Canada: The Status of Alternative Payment Programs 2005-2006. Ottawa, ON: Canadian Institute for Health Information; 2008. [Google Scholar]