Abstract
Objectives. We identified predictors of emergency department (ED) use among a population-based prospective cohort of homeless adults in Toronto, Ontario.
Methods. We assessed ED visit rates using administrative data from the Institute for Clinical Evaluative Sciences (2005–2009). We then used logistic regression to identify predictors of ED use. Frequent users were defined as participants with rates in the top decile (≥ 4.7 visits per person-year).
Results. Among 1165 homeless adults, 892 (77%) had at least 1 ED visit during the study. The average rate of ED visits was 2.0 visits per person-year, whereas frequent users averaged 12.1 visits per person-year. Frequent users accounted for 10% of the sample but contributed more than 60% of visits. Predictors of frequent use in adjusted analyses included birth in Canada, higher monthly income, lower health status, perceived unmet mental health needs, and perceived external health locus of control from powerful others; being accompanied by a partner or dependent children had a protective effect on frequent use.
Conclusions. Among homeless adults with universal health insurance, a small subgroup accounted for the majority of visits to emergency services. Frequent use was driven by multiple predisposing, enabling, and need factors.
Frequent emergency department (ED) use among homeless persons has been the subject of research studies1–5 and high-profile media attention.6–8 These articles highlight the significant burden placed on the health care system from frequent emergency health care use in terms of economic costs, poor patient outcomes, treatment delays, and lower quality of care.9,10 For example, in a nationwide US study, homeless adults were 3 times more likely to have repeat ED visits and were more than twice as likely to return to the ED after hospitalization compared with nonhomeless people.1 Homeless adults contributed an estimated 0.5% of total ED visits across the United States but represent only 0.25% of the general population.1
Frequent health care utilization among homeless persons may be the result of an increased need for emergency health services.2,11–14 Homeless people experience disproportionately high rates of chronic and acute health conditions and traumatic injuries and assaults.15,16 Substance use and mental illness are also highly prevalent.1–4,17 However, the increased use of emergency services may also be an indicator of lack of access to primary health care in ambulatory settings,17–21 often in the presence of competing priorities for basic subsistence needs.22 These factors may increase the need for emergency services because of potentially preventable deteriorations in health status.2,23 According to the Behavioral Model of Health Services Utilization for Vulnerable Populations,24 determinants of health care use can be grouped into predisposing factors (i.e., demographic characteristics and social structural attributes that affect the propensity to use services), enabling factors (i.e., personal, family, and community resources that facilitate the use of services), and need factors (i.e., symptoms or health conditions that precipitate health service use).
We undertook this prospective cohort study to identify predictors of frequent ED use among a population-based sample of homeless adults in Toronto, Ontario. We examined these predictors within a framework of the Behavioral Model of Health Services Utilization for Vulnerable Populations.24 This phenomenon was difficult to study using administrative data in the United States, where more than one-half of homeless people lack any form of health insurance.17 Most US studies rely on self-reported data2,17,25,26 or restrict their analysis to a single health care institution.1,3 This study had the unique advantage of being able to accurately quantify health care use among homeless adults using a population-based approach in a setting where all individuals have access to universal health insurance and all ED visits for the province are recorded in a single administrative database. Using these administrative databases, this study was also able to compare rates of ED use among homeless participants to age- and gender-matched, low-income population controls.
METHODS
Recruitment and sampling methods for this study were previously described.27–29 Briefly, a random sample of homeless participants was selected from shelters and meal programs in Toronto over 12 consecutive months in 2004 and 2005. Recruitment was stratified to obtain a 2:1:1 ratio of single adult men (i.e., men without dependent children), single adult women (i.e., women without dependent children), and family adults (i.e., men or women accompanied by a partner or dependent children) to ensure adequate sample size for comparison and to approximate the demographic characteristic profile of Toronto’s homeless population.16 Based on a pilot study, we determined that about 90% of homeless people in Toronto slept at shelters, whereas 10% did not use shelters but used meal programs.30 We therefore recruited 90% of our sample at shelters and the remaining 10% at meal programs. Meal program users were eligible if they were homeless but had not used a shelter in the past 7 days.
Homelessness was defined as living within the last 7 days at a shelter, public place, vehicle, abandoned building, or someone else’s home, and not having a home of one’s own.31 Participants were excluded if they did not meet our definition of homelessness, were unable to communicate in English, or were unable to provide informed consent. Participants were also excluded if they did not have a valid provincial health insurance number, because this information was required for linkage to administrative data. All participants provided written informed consent and received CAN $15 for their participation.
For the purposes of recruitment, we considered families as units. In instances in which 2 adults of the same family unit were present, we randomly selected 1 adult for inclusion in our analysis. Of the 2516 single adults and family units who were screened, 882 (35.1%) were ineligible to participate, and an additional 443 (17.6%) individuals declined to participate. In total, 1189 adults were included in the study, corresponding to a response rate of 73%.
Survey Instrument
We assessed predisposing, enabling, and need factors using structured, in-person interviews at baseline. The presence of alcohol, drug, and mental health problems was assessed using the Addiction Severity Index.32,33 Addiction Severity Index scores were dichotomized using cutoff scores for each subscale (≥ 0.17 for alcohol problems, ≥ 0.10 for drug problems, and ≥ 0.25 for mental health problems), based on criteria used in a survey of homeless persons across the United States.31 Propensity to underseek care was assessed by asking participants the importance of seeking health care, on a 4-point scale, if they experienced (1) weight loss of more than 10 pounds in a month when not dieting; (2) shortness of breath with light exercise or light work; (3) chest pain when exercising; (4) loss of consciousness, fainting, or passing out; or (5) bleeding other than nosebleeds and not caused by accident or injury.34 Total scores ranged from 0 to 5, with 1 point assigned for each symptom rated as “a little important” or “not at all important.” Higher scores represented more underseeking of care. Visible minority status was defined as “persons, other than Aboriginal peoples, who are non-Caucasian in race or non-white in colour.”35
Competing priorities were based on frequency of difficulty in meeting shelter, food, clothing, washing, and bathroom needs over the past 30 days using a 4-point scale.22 Participants were classified as having competing priorities if they responded “usually” to any of the 5 items. Health locus of control, a measure of a person’s belief that their health is determined by their own behavior, was assessed using Form A of the Multidimensional Health Locus of Control (MHLC) instrument, which consists of three 6-item subscales: internal control, external control from powerful others, and external control caused by chance.36 Perceived access to financial, instrumental, and emotional social support from informal social networks (i.e., family, friends and neighbors) was based on items adapted from Lam and Rosenheck.37 These items were dichotomized to indicate the presence or absence of social support.38 To assess unmet needs for care, participants were asked “Have you needed to see a doctor/nurse in the past 12 months but were not able?” To assess unmet needs for mental health care, participants were asked “Have you needed mental health care in the past 12 months but were not able to get help?” To assess whether participants had a primary care provider, they were asked “Is there one particular person or place that you usually go to when you are sick or need advice about health?”
Perceived health status was measured using the validated 12-item Short Form (SF-12) Health Survey.39,40 SF-12 physical component summary (PCS) and mental component summary (MCS) scores were calculated according to the publishers’ specifications.40 Scores range continuously from 13 to 69 for physical health and from 10 to 70 for mental health, and are standardized to the general population in the United States (mean = 50; SD = 10), with higher scores representing better overall health status.40 Chronic health conditions were based on items from the National Survey of Homeless Assistance Providers and Clients and included diabetes, anemia, high blood pressure, heart disease or stroke, liver problems including viral hepatitis, arthritis, rheumatism or joint problems, cancer, problems walking, lost limb or other handicap, and HIV infection or AIDS.31
Administrative Data Linkage
Administrative data were accessed through the Institute for Clinical Evaluative Sciences, an independent, nonprofit organization funded by the Ontario Ministry of Health and Long-Term Care. Homeless participants were linked to administrative data using a unique 10-digit provincial health number assigned to eligible individuals under the Ontario Health Insurance Plan (OHIP). In instances where either the participants’ health care number could not be obtained (3% of the sample) or the health care number provided was not valid (an additional 3%), efforts were made to perform the linkage based on the participant’s first and last name, gender, and date of birth. Overall, linkage was achieved for 1165 (98%) of study participants.
Age- and gender-matched low-income population control individuals were identified using the Registered Persons Database (RPDB), which provides vital statistics for all persons registered with OHIP in a given year. Individuals were eligible to be a control if they resided in Toronto and were registered during the study recruitment period. Census tracts were restricted to those belonging to the lowest income quintile for Toronto according to the 2006 Census of Canada to determine low-income status. Homeless participants (n = 1165) were randomly matched 1:1 to control individuals according to gender and birth year. This comparison sample was used to examine rates of ED use among the low-income general population of Toronto. Matched control individuals were not included in our analysis of predictors of ED use because survey data were only available for homeless participants.
Administrative data for ED use were obtained from the National Ambulatory Care Reporting System (NACRS) database.41 This database has been used extensively in previous research studies and is considered a valid approach for defining ED use in Ontario.42–45 Data were obtained for all ED visits in the province during the study, defined as the participant’s enrollment date to the end of March 2009. Scheduled visits to the ED and duplicate or overlapping records were excluded. ED visits related to pregnancy or childbirth were also excluded to eliminate the effect of these encounters on gender-specific differences in rates.
Analysis
Rates were calculated by dividing the total number of ED visits by the total period under observation. Dates of death were obtained from the RPDB and were used to adjust person-time of observation. Repeated measures general linear models were used to calculate risk ratios, and 95% confidence intervals (CIs) comparing annualized rates between homeless participants and matched controls.
Logistic regression was used to calculate odds ratios (ORs) and 95% CIs to compare (1) homeless participants with any ED use with those without any ED use, and (2) homeless participants considered to be frequent ED users with those not considered to be frequent users. Frequent ED use was defined as those participants with rates in the top 10% of all participants, which equaled a rate of 4.7 or more visits per person-year. Backward stepwise selection was used to identify significant predictors, using P = .1 as the significance level for entry into the model and P = .05 as the significance level for removal. The demographic group variable was forced into all multivariate regression models regardless of its significance. Interaction terms between demographic group and all significant variables were examined to test for effect modification; none of the tested interaction terms were significant. Independent variables were assessed for multicollinearity, and no problems were detected. Social support variables were added to the survey partway through the study enrollment period; consequently, social support data were missing for approximately 20% of participants. Social support variables were included in univariate analyses, but not multivariate analyses, to maximize our analytical sample size.
Analyses were performed using SAS 9.2 statistical analysis software (SAS Institute, Cary, NC).
RESULTS
A total of 1165 homeless participants were included in our analysis, of whom 587 (50.4%) were single adult men, 296 (25.4%) were single adult women, and 282 (24.2%) were adults in families (Table 1). Of the 282 adults in families, 201 (71.3%) were single mothers accompanied by their dependent children. The mean duration of follow-up was 3.9 years (SD = 0.3 years; range = 1.1–4.3 years).
TABLE 1—
Characteristics of Homeless Participants With Any Emergency Department (ED) Use and Frequent Use: Toronto, Ontario, 2005–2009
| Characteristic | Overall (n = 1165), No. (%) or Mean ±SD | Any ED use (n = 892), No. (%) or Mean ±SD | Frequent ED use (n = 117), No. (%) or Mean ±SD |
| Predisposing factors | |||
| Demographic group | |||
| Single adult male | 587 (50.4) | 449 (50.3) | 73 (62.4) |
| Single adult female | 296 (25.4) | 253 (28.4) | 39 (33.3) |
| Family adult | 282 (24.2) | 190 (21.3) | 5 (4.3) |
| Age, y | 36.1 ±12.4 | 35.9 ±12.4 | 38.7 ±12.0 |
| Lifetime duration of homelessness, y | |||
| < 2 | 584 (50.1) | 426 (47.8) | 44 (37.6) |
| ≥ 2 | 581 (49.9) | 466 (52.2) | 73 (62.4) |
| Race/ethnicity | |||
| White | 650 (55.8) | 522 (58.5) | 78 (66.7) |
| Black | 260 (22.3) | 178 (20.0) | 15 (12.8) |
| Aboriginal | 96 (8.2) | 87 (9.8) | 16 (13.7) |
| Other visible minorities | 159 (13.7) | 105 (11.8) | 8 (6.8) |
| Place of birth | |||
| Canada | 796 (68.3) | 657 (73.7) | 97 (82.9) |
| Outside Canada | 369 (31.7) | 235 (26.4) | 20 (17.1) |
| Highest level of education | |||
| < high school diploma | 587 (50.5) | 469 (52.7) | 71 (60.7) |
| High school diploma or equivalent | 248 (21.3) | 190 (21.4) | 19 (16.2) |
| ≥ college/vocational training | 327 (28.1) | 231 (26.0) | 27 (23.1) |
| History of traumatic brain injury | 553 (47.6) | 452 (50.8) | 72 (61.5) |
| Physical assault in past 12 mo | 330 (28.6) | 267 (30.2) | 42 (35.9) |
| Sexual assault in past 12 mo | 63 (5.5) | 54 (6.1) | 12 (10.4) |
| Current smoker | 826 (71.0) | 667 (74.9) | 100 (85.5) |
| ASI alcohol problem in past 30 d | 339 (29.1) | 271 (30.4) | 51 (43.6) |
| ASI drug problem in past 30 d | 458 (39.1) | 382 (42.8) | 60 (51.3) |
| ASI mental health problem in past 30 d | 438 (37.6) | 360 (40.4) | 61 (52.1) |
| Propensity to underseek care score | |||
| 0 | 670 (57.5) | 512 (57.4) | 62 (53.0) |
| 1 | 228 (19.6) | 167 (18.7) | 28 (23.9) |
| ≥ 2 | 267 (22.9) | 213 (23.9) | 27 (23.1) |
| Enabling factors | |||
| Monthly income, CAN $ | |||
| < 500 | 562 (49.5) | 421 (48.5) | 41 (36.0) |
| 500–999 | 313 (27.6) | 246 (28.3) | 39 (34.2) |
| ≥ 1000 | 260 (22.9) | 201 (23.2) | 34 (29.8) |
| Has a primary care provider | 865 (74.4) | 670 (75.3) | 96 (82.1) |
| Unmet need for health care | 192 (16.5) | 152 (17.1) | 30 (25.6) |
| Unmet need for mental health care | 121 (10.5) | 108 (12.2) | 21 (18.0) |
| Competing priorities | 62 (5.3) | 53 (6.0) | 12 (10.3) |
| MHLC internal subscale score | 27.6 ±5.5 | 27.6 ±5.5 | 27.5 ±5.8 |
| MHLC chance subscale score | 19.6 ±6.4 | 19.6 ±6.4 | 20.4 ±6.6 |
| MHLC powerful others subscale score | 21.0 ±6.9 | 21.0 ±6.8 | 22.7 ±7.0 |
| Social support—short-term loan | 647 (68.0) | 480 (66.2) | 51 (53.1) |
| Social support—ride to appointment | 551 (58.0) | 408 (56.4) | 44 (45.8) |
| Social support—suicide | 655 (69.5) | 492 (68.5) | 59 (62.1) |
| Need factors | |||
| PCS-12 score | 46.0 ±11.2 | 44.9 ±11.3 | 38.9 ±12.9 |
| MCS-12 score | 40.7 ±13.2 | 40.0 ±13.1 | 39.4 ±13.0 |
| No. of chronic health conditions | |||
| None | 470 (40.4) | 321 (36.0) | 32 (27.4) |
| 1 | 324 (27.8) | 249 (28.0) | 21 (18.0) |
| 2 | 202 (17.4) | 173 (19.4) | 22 (18.8) |
| ≥ 3 | 168 (14.4) | 148 (16.6) | 42 (35.9) |
Note. ASI = Addiction Severity Index; MCS-12 = SF-12 mental component summary; MHLC =multidimensional health locus of control; PCS-12 = SF-12 physical component summary.
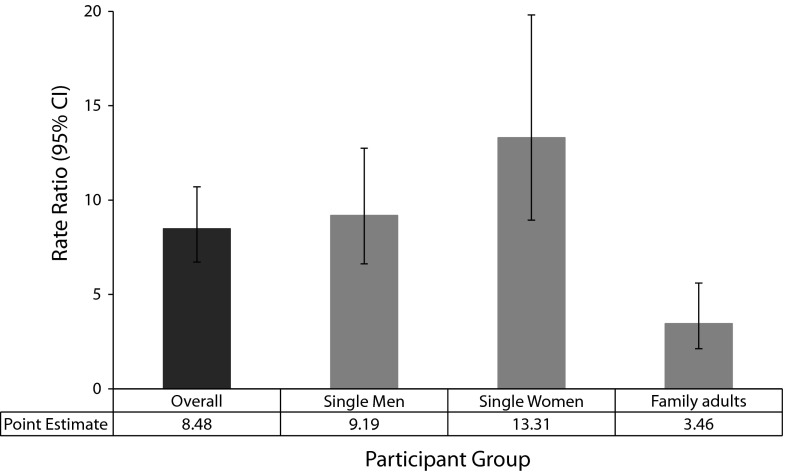
During the study, 892 (76.6%) homeless participants visited an ED. These participants contributed a total of 8566 ED visits during the study, or on average, 2348 ED visits per year. The rate of ED visits was 2.0 visits per person-year (SD = 5.1; range = 0.0–104.9 visits per person-year). Rates of ED visits were significantly higher among homeless participants than age- and gender-matched control individuals across all demographic groups (Figure 1). The rate ratio comparing homeless participants to matched controls was 8.48 (95% CI = 6.72, 10.70) for the overall sample. By definition, 117 (10.0%) homeless participants were considered frequent users. These frequent users accounted for 60.3% of total ED encounters during the study. The rate of ED visits among frequent users was 12.1 visits per person-year (SD = 11.8; range = 4.7–104.9 visits per person-year).
FIGURE 1—
Rate ratios for emergency department (ED) use among homeless participants compared with age- and gender-matched low-income population controls: Toronto, Ontario, 2005–2009.
Note. Error bars represent 95% confidence interval (CIs) for the rate ratio. All 95% CIs exclude 1, indicating that rates of ED use are significantly higher among homeless participants compared with matched control individuals.
Homeless single adult women, compared with single adult men, were more likely to have at least 1 ED visit during the study, whereas adults with families were less likely to have an ED visit (Table 2). Predisposing factors significantly associated with any ED use were being homeless 2 years or more, Aboriginal race/ethnicity, birth in Canada, lower education, history of traumatic brain injury, physical assault in the past 12 months, being a current smoker, and having a drug or mental health problem in the past 30 days. Enabling factors significantly associated with any ED use were self-reported unmet needs for mental health care and social support for a short-term loan. In terms of need factors, lower PCS-12 and MCS-12 scores, indicating worse health status, and a higher number of chronic health conditions were associated with higher odds of having any ED visits during the study.
TABLE 2—
Predictors of Any Emergency Department (ED) Use Among Homeless Participants: Toronto, Ontario, 2005–2009
| Univariate Models |
Multivariate Model |
|||
| Characteristic | OR (95% CI) | P | AOR (95% CI) | P |
| Predisposing factors | ||||
| Demographic group | ||||
| Single adult male (Ref) | 1.00 | 1.00 | ||
| Single adult female | 1.81 (1.24, 2.63) | .002 | 2.27 (1.50, 3.42) | < .001 |
| Family adult | 0.64 (0.46, 0.87) | .005 | 1.10 (0.76, 1.59) | .62 |
| Age, y | 0.99 (0.98, 1.01) | .277 | ||
| Lifetime duration of homelessness, y | ||||
| < 2 (Ref) | 1.00 | |||
| ≥ 2 | 1.50 (1.14, 1.98) | .004 | ||
| Race/ethnicity | ||||
| White (Ref) | 1.00 | |||
| Black | 0.53 (0.38, 0.74) | < .001 | ||
| Aboriginal | 2.37 (1.16, 4.83) | .018 | ||
| Other visible minorities | 0.48 (0.33, 0.70) | < .001 | ||
| Place of birth | ||||
| Outside Canada (Ref) | 1.00 | 1.00 | ||
| Canada | 2.70 (2.04, 3.57) | < .001 | 2.26 (1.65, 3.10) | < .001 |
| Highest level of education | ||||
| < high school diploma (Ref) | 1.00 | |||
| High school diploma or equivalent | 0.82 (0.58, 1.18) | .288 | ||
| ≥ college/vocational training | 0.61 (0.44, 0.83) | .002 | ||
| History of traumatic brain injury | 1.76 (1.33, 2.33) | < .001 | ||
| Physical assault in past 12 mo | 1.42 (1.04, 1.95) | .029 | ||
| Sexual assault in past 12 mo | 1.89 (0.92, 3.88) | .083 | ||
| Current smoker | 2.14 (1.61, 2.84) | < .001 | 1.49 (1.06, 2.09) | .023 |
| ASI alcohol problem in past 30 d | 1.32 (0.97, 1.79) | .082 | ||
| ASI drug problem in past 30 d | 1.94 (1.44, 2.61) | < .001 | 1.50 (1.05, 2.14) | .025 |
| ASI mental health problem in past 30 d | 1.69 (1.26, 2.27) | < .001 | ||
| Propensity to underseek care score | ||||
| 0 (Ref) | 1.00 | |||
| 1 | 0.85 (0.60, 1.19) | .336 | ||
| ≥ 2 | 1.22 (0.86, 1.72) | .268 | ||
| Enabling factors | ||||
| Monthly income, CAN $ | ||||
| < 500 (Ref) | 1.00 | |||
| 500–999 | 1.23 (0.88, 1.71) | .22 | ||
| ≥ 1000 | 1.14 (0.81, 1.62) | .457 | ||
| Has a primary care provider | 1.22 (0.90, 1.65) | .203 | ||
| Unmet need for health care | 1.20 (0.82, 1.75) | .342 | ||
| Unmet need for mental health care | 2.77 (1.53, 5.01) | < .001 | 2.29 (1.22, 4.30) | .01 |
| Competing priorities | 1.86 (0.90, 3.81) | .093 | ||
| MHLC internal subscale score | 0.99 (0.97, 1.02) | .469 | ||
| MHLC chance subscale score | 1.00 (0.97, 1.02) | .621 | ||
| MHLC powerful others subscale score | 1.00 (0.98, 1.02) | .785 | ||
| Social support—short-term loan | 0.69 (0.50, 0.97) | .031 | ||
| Social support—ride to appointment | 0.75 (0.55, 1.02) | .066 | ||
| Social support—suicide | 0.83 (0.59, 1.15) | .266 | ||
| Need factors | ||||
| PCS-12 score | 0.96 (0.95, 0.98) | < .001 | 0.96 (0.95, 0.98) | < .001 |
| MCS-12 score | 0.98 (0.97, 0.99) | .001 | ||
| No. of chronic health conditions | ||||
| None (Ref) | 1.00 | |||
| 1 | 1.54 (1.12, 2.13) | .009 | ||
| 2 | 2.77 (1.79, 4.29) | < .001 | ||
| ≥ 3 | 3.44 (2.07, 5.70) | < .001 | ||
Note. AOR = adjusted odds ratio; ASI = Addiction Severity Index; CI = confidence interval; MCS-12 = SF-12 mental component summary; MHLC = multidimensional health locus of control; OR = odds ratio; PCS-12 = SF-12 physical component summary.
In adjusted analyses, single adult women were more likely to have any ED encounters during the study compared with single adult men (Table 2). Other factors that remained significant in the final adjusted model included birth in Canada, current smoking status, having a drug problem in the past 30 days, perceived unmet needs for mental health care, and lower PCS-12 scores.
Homeless adults in families were less likely to be frequent users compared with single adult men (Table 3). Predisposing factors significantly associated with frequent ED use were older age, being homeless 2 years or more, birth in Canada, White race/ethnicity, history of traumatic brain injury, sexual assault in past 12 months, being a current smoker, and having an alcohol, drug, or mental health problem in the past 30 days. Enabling factors significantly associated with frequent ED use were higher monthly incomes, having a primary care provider, self-reported unmet needs for health care or mental health care, having competing priorities, higher MHLC powerful others subscale scores, and social support for a short-term loan or ride to an appointment. In terms of need factors, lower PCS-12 scores and having 3 or more chronic health conditions were significantly associated with frequent ED use during the study.
TABLE 3—
Predictors of Frequent Emergency Department (ED) Use Among Homeless Participants: Toronto, Ontario, 2005–2009
| Univariate Models |
Multivariate Model |
|||
| Characteristic | OR (95% CI) | P | AOR (95% CI) | P |
| Predisposing factors | ||||
| Demographic group | ||||
| Single adult male (Ref) | 1.00 | 1.00 | ||
| Single adult female | 1.07 (0.70, 1.62) | .755 | 0.96 (0.60, 1.53) | .861 |
| Family adult | 0.13 (0.05, 0.32) | < .001 | 0.13 (0.05, 0.34) | < .001 |
| Age, y | 1.02 (1.00, 1.03) | .016 | ||
| Lifetime duration of homelessness, y | ||||
| < 2 (Ref) | 1.00 | |||
| ≥ 2 | 1.76 (1.19, 2.61) | .005 | ||
| Race/ethnicity | ||||
| White (Ref) | 1.00 | |||
| Black | 0.45 (0.25, 0.80) | .006 | ||
| Aboriginal | 1.45 (0.82, 2.64) | .201 | ||
| Other visible minorities | 0.39 (0.18, 0.82) | .013 | ||
| Place of birth | ||||
| Outside Canada (Ref) | 1.00 | 1.00 | ||
| Canada | 2.42 (1.47, 3.99) | < .001 | 2.13 (1.22, 3.73) | .008 |
| Highest level of education | ||||
| < high school diploma (Ref) | 1.00 | |||
| High school diploma or equivalent | 0.60 (0.36, 1.02) | .061 | ||
| ≥ College/vocational training or higher | 0.65 (0.41, 1.04) | .074 | ||
| History of traumatic brain injury | 1.88 (1.27, 2.78) | .002 | ||
| Physical assault in past 12 mo | 1.46 (0.98, 2.18) | .066 | ||
| Sexual assault in past 12 mo | 2.26 (1.17, 4.38) | .015 | ||
| Current smoker | 2.60 (1.53, 4.42) | < .001 | ||
| ASI alcohol problem in past 30 d | 2.04 (1.38, 3.01) | < .001 | ||
| ASI drug problem in past 30 d | 1.72 (1.17, 2.52) | .006 | ||
| ASI mental health problem in past 30 d | 1.94 (1.32, 2.85) | < .001 | ||
| Propensity to underseek care score | ||||
| 0 (Ref) | 1.00 | |||
| 1 | 1.37 (0.86, 2.21) | .19 | ||
| ≥ 2 | 1.10 (0.69, 1.78) | .686 | ||
| Enabling factors | ||||
| Monthly income, CAN $ | ||||
| < 500 (Ref) | 1.00 | 1.00 | ||
| 500–999 | 1.81 (1.14, 2.87) | .003 | 1.73 (1.05, 2.86) | .031 |
| ≥ 1000 | 1.91 (1.18, 3.09) | .01 | 2.46 (1.45, 4.16) | < .001 |
| Has a primary care provider | 1.65 (1.01, 2.69) | .047 | ||
| Unmet need for health care | 1.88 (1.20, 2.94) | .006 | ||
| Unmet need for mental health care | 2.05 (1.23, 3.44) | .006 | 1.96 (1.10, 3.50) | .022 |
| Competing priorities | 2.28 (1.18, 4.42) | .015 | ||
| MHLC internal subscale score | 1.00 (0.96, 1.03) | .785 | ||
| MHLC chance subscale score | 1.02 (0.99, 1.05) | .173 | ||
| MHLC powerful others subscale score | 1.04 (1.01, 1.07) | .005 | 1.04 (1.01, 1.08) | .009 |
| Social support—short-term loan | 0.49 (0.32, 0.76) | .001 | ||
| Social support—ride to appointment | 0.58 (0.38, 0.89) | .012 | ||
| Social support—suicide | 0.69 (0.45, 1.08) | .102 | ||
| Need factors | ||||
| PCS-12 score | 0.94 (0.93, 0.96) | < .001 | 0.96 (0.94, 0.98) | < .001 |
| MCS-12 score | 0.99 (0.98, 1.01) | .236 | ||
| No. of chronic health conditions | ||||
| None (Ref) | 1.00 | 1.00 | ||
| 1 | 0.95 (0.54, 1.68) | .856 | 0.66 (0.35, 1.22) | .186 |
| 2 | 1.67 (0.95, 2.96) | .077 | 1.00 (0.52, 1.90) | .995 |
| ≥ 3 | 4.56 (2.77, 7.53) | < .001 | 1.71 (0.89, 3.30) | .108 |
Note. AOR = adjusted odds ratio; ASI = Addiction Severity Index; MCS-12 = SF-12 mental component summary; MHLC = multidimensional health locus of control; PCS-12 = SF-12 physical component summary.
In adjusted analyses, family adult status was associated with a greatly decreased likelihood of frequent ED use (Table 3). Other factors that remained significant in the final adjusted model included birth in Canada, having higher monthly incomes, perceived unmet needs for mental health care, higher MHLC powerful others subscale scores, and lower PCS-12 scores.
DISCUSSION
Over the course of an approximately 4-year follow-up, almost 900 homeless adults in our sample had more than 8500 ED visits. On average, this represents 2 ED visits per person annually. Frequent ED users, defined as those in the top decile of users, represented only 10% of the sample but contributed to more than 60% of total ED visits during the study. Among frequent users, the average rate of ED use was 12 visits per person annually. Compared with the low-income population of Toronto, homeless participants in our sample visited an ED more than 8 times as often, independent of the effects of age and gender.
Our results showed that homeless single adult women were more likely to have an ED encounter during the study, whereas adults with families—mostly women with dependent children—were far less likely to be frequent users compared with single adult men. Women are known to be disproportionately frequent users of emergency services among nonhomeless populations11; however, homeless women with dependent children in our study were less likely to be frequent users compared with single men. Single homeless women generally had a higher prevalence of mental illness, whereas single homeless men had a higher prevalence of substance abuse.31,46–48 Homeless mothers had relatively lower rates of both these conditions, which might partially explain why family adults in our sample had lower rates of ED use. Mental health and substance use problems in the past 30 days were identified as important predictors of frequent use in univariate analyses; however, these variables did not remain significant in the final adjusted model.
Groups perceived to be minorities were less likely to use ED services; however, only the association between immigrant status and ED use remained significant in the final adjusted analysis. The fact that homeless recent immigrants tended to be healthier than homeless persons who were born in Canada, and consequently had less need for emergency services, might explain this finding.28 Conversely, factors related to language, awareness of services, socioeconomic barriers, and perceived discrimination or stigma might have deterred these individuals from seeking care in the ED.49,50 Surprisingly, higher monthly income amounts were associated with a greater likelihood of frequent ED use. We speculated that individuals might be engaging in more frequent risk behaviors, such as binge alcohol or drug use, following receipt of welfare or other social support payments,51,52 which might explain this finding.
The increased need for health services, as measured by poor physical health status, was a strong predictor of both ED use and frequent use in our analysis. The high burden of serious and complex health conditions—conditions that often cannot be adequately treated or prevented in ambulatory settings—likely accounted for much of the frequent ED use among homeless participants.11,12 Studies in general population samples also confirmed the strong association between poor health status and use of emergency services.13,14,53,54 Although not directly comparable because of differences in research methodology, definitions of frequent use, and structure of the health care system, previous research in homeless populations on frequent ED use also suggested a predominance of need and predisposing factors.2,21
Enabling factors related to health care access, such as having a primary care provider, did not remain significant in our final models, likely because poor health status confounded the relationship between having a primary care provider and frequent ED use. Self-reported unmet needs for mental health care was, however, a predictor in both final models, suggesting homeless people used emergency services because of, in part, a lack of perceived access to health care, particularly in relation to mental health services. Although poor mental health status was significantly associated with any ED use and frequent ED use, it did not remain significant in final adjusted models. Problematic substance use was significantly and independently associated with ED use, but not frequent use, during the study. Participants with higher MHLC powerful others subscores were also more likely to be frequent ED users, suggesting that these participants’ belief that their health was under external control by powerful others (e.g., physicians) affected their tendency to seek health care in an ED setting.36
Limitations
Although this study had numerous strengths, including using a population-based approach to examine health care utilization among a prospective cohort of homeless persons within a system of universal health insurance, certain limitations should be acknowledged. Health care utilization was assessed using administrative data that were provincial in scope; as such, ED encounters that occurred outside of Ontario were missed. Predictors of ED use were assessed at 1 point in time using a cross-sectional survey and could not be assumed to be constant for the entire duration of follow-up. Age- and gender-matched low-income population controls were identified using administrative registry databases; as such, predictors of ED use derived from survey data were not available for matched controls. Controls were not able to be matched to homeless participants on characteristics other than age and gender. The 10% cutoff value for defining frequent users was arbitrary and was selected to ensure an adequate sample size for analysis. However, our cutoff rate of 4.7 visits per person-year was consistent with other studies of “frequent ED use,” a term for which there is no consensus definition.11 Stratified analyses by demographic group were not performed because of sample size limitations; however, tests for interaction showed no evidence of effect modification. Homeless participants were required to have a valid provincial health number to be eligible for this study, which might have biased our sample toward individuals with better health care access. Our sampling strategy excluded individuals who did not use either shelters or meal programs; however, previous research suggested that this unsheltered homeless population in Toronto is very small.55
Conclusions
Although homeless people represented a very small proportion of all ED users, our findings showed that a subgroup of homeless individuals were extremely high utilizers of emergency services and had multiple, complex health care needs. Predictors of frequent ED use in our study were similar to those predicting any ED use, most notably poor health status, perceived unmet needs for mental health care, and nonimmigrant status. Other studies showed that interventions such as Intensive Case Management or Housing First models have the potential to reduce ED visits, lower costs, and improve social and clinical outcomes among these extremely frequent, high-cost users of the health care system.56–59 However, additional research is needed to determine the impact of these interventions on health care use when expanded more broadly to the homeless population, rather than only those individuals who are frequent ED users.60 Most notably, reducing frequent emergency health care use among homeless persons will require sustained efforts to reduce unmet needs for health care, particularly for mental health services, and improvement in the coordination of care across health and social services.61
Acknowledgments
This project was supported by operating grants from the Agency for Healthcare Research and Quality (1 R01 HS014129-01) and the Canadian Institutes of Health Research (MOP-62736), and by an Interdisciplinary Capacity Enhancement grant on Homelessness, Housing, and Health from the Canadian Institutes of Health Research (HOA-80066). This study was supported by the Institute for Clinical Evaluative Sciences (ICES) and the Centre for Research on Inner City Health, which are funded by annual grants from the Ontario Ministry of Health and Long-Term Care.
Note. The funders had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the article. The opinions, results, and conclusions reported in this article are the views of the authors and do not necessarily reflect the views of any of the previously named organizations. No endorsement by ICES or the Ontario Ministry of Health and Long-Term Care should be intended or inferred.
Human Participant Protection
This study was approved by the Research Ethics Board at St. Michael’s Hospital in Toronto, Ontario, Canada. All participants provided written informed consent.
References
- 1.Ku BS, Scott KC, Kertesz SG, Pitts SR. Factors associated with use of urban emergency departments by the U.S. homeless population. Public Health Rep. 2010;125(3):398–405. doi: 10.1177/003335491012500308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kushel MB, Perry S, Bangsberg D, Clark R, Moss AR. Emergency department use among the homeless and marginally housed: results from a community-based study. Am J Public Health. 2002;92(5):778–784. doi: 10.2105/ajph.92.5.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.D’Amore J, Hung O, Chiang W, Goldfrank L. The epidemiology of the homeless population and its impact on an urban emergency department. Acad Emerg Med. 2001;8(11):1051–1055. doi: 10.1111/j.1553-2712.2001.tb01114.x. [DOI] [PubMed] [Google Scholar]
- 4.Pearson DA, Bruggman AR, Haukoos JS. Out-of-hospital and emergency department utilization by adult homeless patients. Ann Emerg Med. 2007;50(6):646–652. doi: 10.1016/j.annemergmed.2007.07.015. [DOI] [PubMed] [Google Scholar]
- 5.Mandelberg JH, Kuhn RE, Kohn MA. Epidemiologic analysis of an urban, public emergency department’s frequent users. Acad Emerg Med. 2000;7(6):637–646. doi: 10.1111/j.1553-2712.2000.tb02037.x. [DOI] [PubMed] [Google Scholar]
- 6.Gladwell M. Million-dollar Murray. New Yorker. February 13, 2006 96-107. [Google Scholar]
- 7.Picard A. We need to treat ‘million-dollar’ patients better. The Globe and Mail. February 27, 2012 [Google Scholar]
- 8.Gawande A. The Hot Spotters: can we lower medical costs by giving the neediest patients better care? New Yorker. January 24, 2011:40–51. [PubMed] [Google Scholar]
- 9.Guttmann A, Schull MJ, Vermeulen MJ, Stukel TA. Association between waiting times and short term mortality and hospital admission after departure from emergency department: population based cohort study from Ontario, Canada. BMJ. 2011;342 doi: 10.1136/bmj.d2983. d2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trzeciak S, Rivers EP. Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J. 2003;20(5):402–405. doi: 10.1136/emj.20.5.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.LaCalle E, Rabin E. Frequent users of emergency departments: the myths, the data, and the policy implications. Ann Emerg Med. 2010;56(1):42–48. doi: 10.1016/j.annemergmed.2010.01.032. [DOI] [PubMed] [Google Scholar]
- 12.Ruger JP, Richter CJ, Spitznagel EL, Lewis LM. Analysis of costs, length of stay, and utilization of emergency department services by frequent users: implications for health policy. Acad Emerg Med. 2004;11(12):1311–1317. doi: 10.1197/j.aem.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 13.Hunt KA, Weber EJ, Showstack JA, Colby DC, Callaham ML. Characteristics of frequent users of emergency departments. Ann Emerg Med. 2006;48(1):1–8. doi: 10.1016/j.annemergmed.2005.12.030. [DOI] [PubMed] [Google Scholar]
- 14.Khan Y, Glazier RH, Moineddin R, Schull MJ. A population-based study of the association between socioeconomic status and emergency department utilization in Ontario, Canada. Acad Emerg Med. 2011;18(8):836–843. doi: 10.1111/j.1553-2712.2011.01127.x. [DOI] [PubMed] [Google Scholar]
- 15.Hwang SW, Dunn JR. Homeless people. In: Galea S, Vlahov D, editors. Handbook of Urban Health: Populations, Methods, and Practice. New York, NY: Springer; 2005. pp. 21–41. [Google Scholar]
- 16.Khandor E, Mason K. The Street Health Report 2007. Toronto, Ontario, Canada: Street Health; 2007. [Google Scholar]
- 17.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200–206. doi: 10.1001/jama.285.2.200. [DOI] [PubMed] [Google Scholar]
- 18.Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21(1):71–77. doi: 10.1111/j.1525-1497.2005.00278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lim YW, Andersen R, Leake B, Cunningham W, Gelberg L. How accessible is medical care for homeless women? Med Care. 2002;40(6):510–520. doi: 10.1097/00005650-200206000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Lewis JH, Andersen RM, Gelberg L. Health care for homeless women. J Gen Intern Med. 2003;18(11):921–928. doi: 10.1046/j.1525-1497.2003.20909.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weinreb L, Perloff J, Goldberg R, Lessard D, Hosmer DW. Factors associated with health service utilization patterns in low-income women. J Health Care Poor Underserved. 2006;17(1):180–199. doi: 10.1353/hpu.2006.0036. [DOI] [PubMed] [Google Scholar]
- 22.Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997;87(2):217–220. doi: 10.2105/ajph.87.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Han B, Wells BL. Inappropriate emergency department visits and use of the Health Care for the Homeless Program services by homeless adults in the northeastern United States. J Public Health Manag Pract. 2003;9(6):530–537. doi: 10.1097/00124784-200311000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 25.O’Toole TP, Gibbon JL, Hanusa BH, Fine MJ. Utilization of health care services among subgroups of urban homeless and housed poor. J Health Polit Policy Law. 1999;24(1):91–114. doi: 10.1215/03616878-24-1-91. [DOI] [PubMed] [Google Scholar]
- 26.Padgett DK, Struening EL, Andrews H, Pittman J. Predictors of emergency room use by homeless adults in New York City: the influence of predisposing, enabling and need factors. Soc Sci Med. 1995;41(4):547–556. doi: 10.1016/0277-9536(94)00364-y. [DOI] [PubMed] [Google Scholar]
- 27.Hwang SW, Colantonio A, Chiu S et al. The effect of traumatic brain injury on the health of homeless people. CMAJ. 2008;179(8):779–784. doi: 10.1503/cmaj.080341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chiu S, Redelmeier DA, Tolomiczenko G, Kiss A, Hwang SW. The health of homeless immigrants. J Epidemiol Community Health. 2009;63(11):943–948. doi: 10.1136/jech.2009.088468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hwang SW, Ueng JJ, Chiu S et al. Universal health insurance and health care access for homeless persons. Am J Public Health. 2010;100(8):1454–1461. doi: 10.2105/AJPH.2009.182022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hwang SW, Chiu S, Kiss A et al. Use of meal programs and shelters by homeless people in Toronto. [abstract] J Urban Health. 2005;82(suppl 2) ii46. [Google Scholar]
- 31.Burt MR, Aron LY, Douglas T . Homelessness: Programs and the People they Serve. Findings of the National Survey of Homeless Assistance Providers and Clients. Washington, DC: Interagency Council on the Homeless; 1999. (Rep. No. 6-2-6-3) [Google Scholar]
- 32.McGahan PL, Griffith JA, Parente R, McLellan AT. Addiction Severity Index: Composite Scores Manual. Philadelphia, PA: The University of Pennsylvania/Veterans Administration Centre for Studies of Addiction; 1986. [Google Scholar]
- 33.McLellan AT, Kushner H, Metzger D et al. The Fifth Edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- 34.Bindman AB, Grumbach K, Osmond D et al. Preventable hospitalizations and access to health care. JAMA. 1995;274(4):305–311. [PubMed] [Google Scholar]
- 35.Statistics Canada. Visible minority of person. Available at: http://www.statcan.gc.ca/concepts/definitions/minority-minorite1-eng.htm. Accessed March 22, 2013.
- 36.Wallston KA, Wallston BS, DeVellis R. Development of the Multidimensional Health Locus of Control (MHLC) Scales. Health Educ Monogr. 1978;6(1):160–170. doi: 10.1177/109019817800600107. [DOI] [PubMed] [Google Scholar]
- 37.Lam JA, Rosenheck R. Social support and service use among homeless persons with serious mental illness. Int J Soc Psychiatry. 1999;45(1):13–28. doi: 10.1177/002076409904500103. [DOI] [PubMed] [Google Scholar]
- 38.Hwang SW, Kirst MJ, Chiu S et al. Multidimensional social support and the health of homeless individuals. J Urban Health. 2009;86(5):791–803. doi: 10.1007/s11524-009-9388-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Larson CO. Use of the SF-12 instrument for measuring the health of homeless persons. Health Serv Res. 2002;37(3):733–750. doi: 10.1111/1475-6773.00046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ware JE, Kosinski M, Keller D. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. Vol 2. Boston, MA: The Health Institute, New England Medical Center; 1995. [Google Scholar]
- 41.Canadian Institute for Health Information. National Ambulatory Care Reporting System. Available at: http://www.cihi.ca/CIHI-ext-portal/internet/en/document/types+of+care/hospital+care/emergency+care/NACRS_METADATA. Accessed June 18, 2013.
- 42.Canadian Institute for Health Information. Data Quality Study of Emergency Department Visits for 2004-2005. Vol. 2: Main Study Findings. Ottawa, Ontario, Canada: CIHI; 2008. [Google Scholar]
- 43.Vermeulen MJ, Ray JG, Bell C, Cayen B, Stukel TA, Schull MJ. Disequilibrium between admitted and discharged hospitalized patients affects emergency department length of stay. Ann Emerg Med. 2009;54(6):794–804. doi: 10.1016/j.annemergmed.2009.04.017. [DOI] [PubMed] [Google Scholar]
- 44.Schull MJ, Hatcher CM, Guttmann A . Toronto, Ontario, Canada: Institute for Clinical Evaluative Sciences; 2010. Development of a Consensus on Evidence-based Quality of Care Indicators for Canadian Emergency Departments. [Google Scholar]
- 45.Li G, Lau JT, McCarthy ML, Schull MJ, Vermeulen M, Kelen GD. Emergency department utilization in the United States and Ontario, Canada. Acad Emerg Med. 2007;14(6):582–584. doi: 10.1197/j.aem.2007.02.030. [DOI] [PubMed] [Google Scholar]
- 46.Bassuk EL, Weinreb LF, Buckner JC, Browne A, Salomon A, Bassuk SS. The characteristics and needs of sheltered homeless and low-income housed mothers. JAMA. 1996;276(8):640–646. [PubMed] [Google Scholar]
- 47.Gelberg L, Linn LS. Demographic differences in health status of homeless adults. J Gen Intern Med. 1992;7(6):601–608. doi: 10.1007/BF02599198. [DOI] [PubMed] [Google Scholar]
- 48.North CS, Smith EM. A comparison of homeless men and women: different populations, different needs. Community Ment Health J. 1993;29(5):423–431. doi: 10.1007/BF00754410. [DOI] [PubMed] [Google Scholar]
- 49.Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O. Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003;118(4):293–302. doi: 10.1016/S0033-3549(04)50253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Institute of Medicine. Washington, DC: National Academy Press; 2002. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. [PMC free article] [PubMed] [Google Scholar]
- 51.Verheul G, Singer SM, Christenson JM. Mortality and morbidity associated with the distribution of monthly welfare payments. Acad Emerg Med. 1997;4(2):118–123. doi: 10.1111/j.1553-2712.1997.tb03717.x. [DOI] [PubMed] [Google Scholar]
- 52.Phillips DP, Christenfeld N, Ryan NM. An increase in the number of deaths in the United States in the first week of the month – an association with substance abuse and other causes of death. N Engl J Med. 1999;341(2):93–98. doi: 10.1056/NEJM199907083410206. [DOI] [PubMed] [Google Scholar]
- 53.Weber EJ, Showstack JA, Hunt KA, Colby DC, Callaham ML. Does lack of a usual source of care or health insurance increase the likelihood of an emergency department visit? Results of a national population-based study. Ann Emerg Med. 2005;45(1):4–12. doi: 10.1016/j.annemergmed.2004.06.023. [DOI] [PubMed] [Google Scholar]
- 54.Zuckerman S, Shen YC. Characteristics of occasional and frequent emergency department users: do insurance coverage and access to care matter? Med Care. 2004;42(2):176–182. doi: 10.1097/01.mlr.0000108747.51198.41. [DOI] [PubMed] [Google Scholar]
- 55.City of Toronto. Street Needs Assessment Results. Toronto, Ontario, Canada: Shelter, Support, and Housing Administration, City of Toronto; 2009. [Google Scholar]
- 56.Althaus F, Paroz S, Hugli O et al. Effectiveness of interventions targeting frequent users of emergency departments: a systematic review. Ann Emerg Med. 2011;58(1):41–52. doi: 10.1016/j.annemergmed.2011.03.007. e42. [DOI] [PubMed] [Google Scholar]
- 57.Larimer ME, Malone DK, Garner MD et al. Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems. JAMA. 2009;301(13):1349–1357. doi: 10.1001/jama.2009.414. [DOI] [PubMed] [Google Scholar]
- 58.Martinez TE, Burt MR. Impact of permanent supportive housing on the use of acute care health services by homeless adults. Psychiatr Serv. 2006;57(7):992–999. doi: 10.1176/ps.2006.57.7.992. [DOI] [PubMed] [Google Scholar]
- 59.Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA. 2009;301(17):1771–1778. doi: 10.1001/jama.2009.561. [DOI] [PubMed] [Google Scholar]
- 60.Kertesz SG, Weiner SJ. Housing the chronically homeless: high hopes, complex realities. JAMA. 2009;301(17):1822–1824. doi: 10.1001/jama.2009.596. [DOI] [PubMed] [Google Scholar]
- 61.Raven MC. What we don’t know may hurt us: interventions for frequent emergency department users. Ann Emerg Med. 2011;58(1):53–55. doi: 10.1016/j.annemergmed.2011.04.009. [DOI] [PubMed] [Google Scholar]