Abstract
Background
Several prospective studies have been conducted to examine the relationship between fruit juice intake and risk of incident type 2 diabetes, but results have been mixed. In the present study, we aimed to estimate the association between fruit juice intake and risk of type 2 diabetes.
Methods
PubMed and Embase databases were searched up to December 2013. All prospective cohort studies of fruit juice intake with risk of type 2 diabetes were included. The pooled relative risks (RRs) with 95% confidence intervals (CIs) for highest vs. lowest category of fruit juice intake were estimated using a random-effects model.
Results
A total of four studies (191,686 participants, including 12,375 with type 2 diabetes) investigated the association between sugar-sweetened fruit juice and risk of incident type 2 diabetes, and four studies (137,663 participants and 4,906 cases) investigated the association between 100% fruit juice and risk of incident type 2 diabetes. A higher intake of sugar-sweetened fruit juice was significantly associated with risk of type 2 diabetes (RR = 1.28, 95%CI = 1.04–1.59, p = 0.02), while intake of 100% fruit juice was not associated with risk of developing type 2 diabetes (RR = 1.03, 95% CI = 0.91–1.18, p = 0.62).
Conclusions
Our findings support dietary recommendations to limit sugar-sweetened beverages, such as fruit juice with added sugar, to prevent the development of type 2 diabetes.
Introduction
Type 2 diabetes, one of the main causes of morbidity and mortality, has significantly increased worldwide in recent years. Thus, it is important to identify modifiable factors to reduce the risk of developing type 2 diabetes. Although sugar-sweetened beverage (SSB) consumption decreased among youth and adults in the United States between 1999 and 2010 [1], an increased intake of these beverages was observed in Asians [2]. Since the consumption of SSBs has been associated with an increased risk of obesity [3] and type 2 diabetes [4], reduction of SSB intake should be a recommended strategy to promote optimal health. Fruit juice, different from SSBs, has been considered a healthier drink. However, to date, the findings of the association between fruit juice intake and risk of type 2 diabetes are mixed according to type of fruit juice [5]–[11]. Several prospective studies suggested that higher intake of sugar-sweetened fruit juice may increase the risk of developing type 2 diabetes [5], [10], while others showed no significant association for 100% fruit juice [6], [8], [9].
To our knowledge, no meta-analysis has been published to accurately estimate the strength of the effects of type of fruit juice (sugar-sweetened or 100%) on incidence of type 2 diabetes. Although all four studies included in this meta-analysis showed no significant association between 100% fruit juice and risk of developing type 2 diabetes, there was a positive trend for three [6], [8] of the four studies, and insufficient power may explain the non-significant study findings. Therefore, in this study, we conducted a systematic review and meta-analysis to address this issue.
Materials and Methods
Literature and search strategy
The PRISMA checklist is available as Checklist S1. The Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines were followed for the current study [12]. The literature databases including PubMed and Embase were searched. Search terms were “fruit juice” and “type 2 diabetes” or “T2DM”. The reference lists of retrieved articles were also screened. The literature search was limited to the English language. If more than one article was published on the same cohort, only the study with the largest sample size was included. The literature search was updated on December 10, 2013.
Inclusion criteria and data extraction
Studies included in the meta-analysis met the following inclusion criteria: (1) evaluation of the association between fruit juice intake and incidence of type 2 diabetes; (2) a prospective study design; and (3) covariate adjusted relative risks (RRs) or hazard ratios (HRs) with 95% confidence intervals (CIs) for highest vs. lowest category of fruit juice intake. The following information was extracted from each study: (1) name of the first author; (2) year of publication; (3) country of study; (4) number of incident cases and study population; (5) age distribution of the study population at baseline; (6) sex of the participants; (7) average duration of follow-up; (8) the covariates included in the regression models; and (9) RRs or HRs with 95% CIs for highest vs. lowest category of fruit juice intake. Two investigators (SL and ZL) independently assessed the articles for compliance with the inclusion/exclusion criteria and resolved disagreements through discussion.
The quality of each study was assessed by the Newcastle–Ottawa quality scale (NOS) [13], which is a validated scale for non-randomized studies in meta-analyses. This scale assigned a maximum of nine points for each study. Three broad perspectives were considered: the selection of the cohorts (4 points); the comparability of cohorts (2 points); and the ascertainment of the exposure and outcome of interest (3 points).
Statistical analysis
A random effects model [14] was used to calculate pooled RRs with 95% CIs for highest vs. lowest category of fruit juice intake. Heterogeneity was assessed by the Q test and the I 2 statistic [15]. The significance for the Q test was defined as p<0.10. The I 2 statistic represents the amount of total variation attributed to heterogeneity. Low, moderate, and high degrees of heterogeneity correspond to I 2 values of 25%, 50%, and 75%, respectively. Publication bias was assessed by Begg's test [16] and Egger's test [17] (p<0.05 was considered statistically significant). Statistical analysis was conducted using STATA version 11 (StataCorp LP, College Station, TX, USA).
Results
Study characteristics
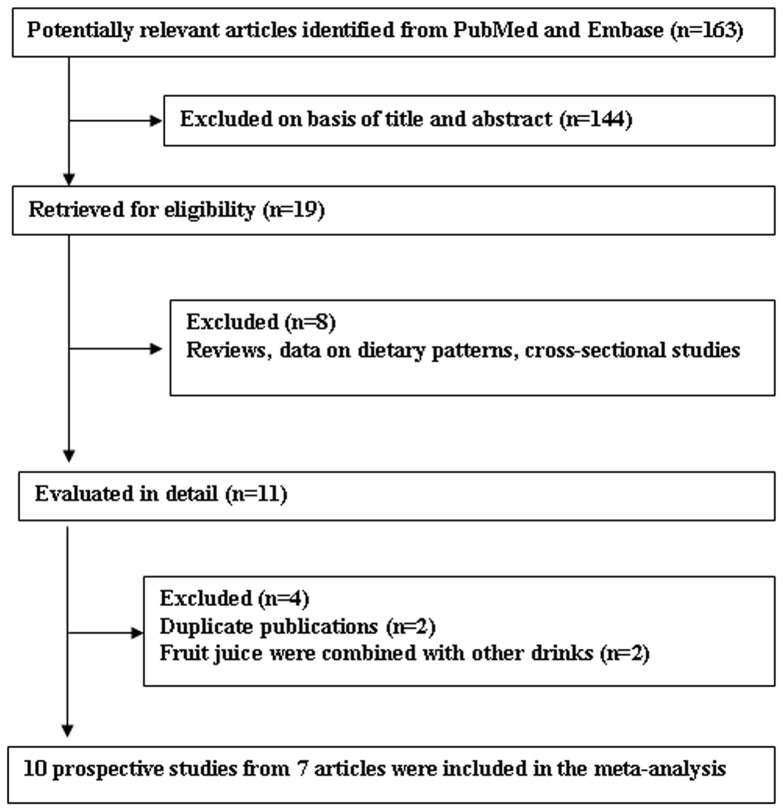
Figure 1 shows the process of study selection for the meta-analyses. It should be noted that two duplicate publications [18], [19] and two publications [20], [21] that combined fruit juices with other drinks were excluded. A total of 10 prospective studies from 7 publications were included in the meta-analysis of fruit juice intake and risk of developing type 2 diabetes [5]–[11]. In the publication by Eshak et al. [8], results were reported for each gender and were handled as two independent studies. In addition, the publication by Muraki et al. [10] contained three studies but provided pooled estimate based on them. The characteristics of the studies included in the meta-analyses are summarized in Table 1. Among all studies included in the meta-analysis, four studies examined sugar-sweetened fruit juice [5], [10], four studies examined 100% fruit juice [6], [8], [9], and two studies did not specify the type of fruit juice [7], [11]. Four studies were from the USA [6], [10], three from Europe [5], [9], and three from Asia [7], [8]; and the duration of follow-up ranged from 5.7 to 25 years.
Figure 1. Process of study selection.
Table 1. Characteristics of included studies on fruit juice intake and risk of type 2 diabetes.
| Study | Country | No. of cases/ participants | Sex | Age (years) | Follow-up (years) | Dietary assessment (juice type) | Diagnosis of type 2 diabetes | RR (95%CI) for highest vs. lowest intakes | Confounders' Adjustment | Study qualitya |
| Montonen et al, 2007 [5] | Finland | 177/4304 | Men and women | 40–60 | 12 | Dietary history interview (sugar-sweetened) | Confirmed via social insurance institutions register | 51 g/day vs. 0 g/day: 1.56 (1.08–2.26) | Age, sex, BMI, energy intake, smoking, geographic area, physical activity, family history of diabetes, prudent dietary pattern score, conservative pattern score, serum cholesterol, blood pressure, history of infarction, history of angina pectoris, and history of cardiac failure | 7 |
| Palmer et al, 2008 [6] | USA | 2713/43960 | Women | 38±10 | 10 | FFQ (100%) | Self-reported and validated in a random sample | ≥2 drinks/day vs. <1 drink/month: 1.11 (0.92–1.35) | Age, family history of diabetes, physical activity, cigarette smoking, years of education, each of the 2 other types of drinks, intake of red meat, processed meats, cereal fiber, and coffee, and glycemic index | 7 |
| Odegaard et al, 2010 [7] | Singapore | 2273/43580 | Women | 45–74 | 5.7 | FFQ (unknown) | Confirmed via hospital databases | 2–≥3 glasses/week vs. never: 1.24 (1.01– 1.53) | Age, sex, dialect, year of interview educational level, smoking status, alcohol use, physical activity, saturated fat intake, dietary fiber intake, dairy intake, juice or soft drink intake depending on model, coffee consumption,BMI, energy intake, weight gain | 7 |
| Eshak et al, 2013 [8] | Japan | 824/27585 | Men and women | 40–59 | 10 | FFQ (100%) | Self-reported and validated in a random sample | Men: 1 time/day vs. rarely: 1.17 (0.69–2.00) Women: 1 time/day vs. rarely: 1.37 (0.79–2.37) | Age, BMI, family history of diabetes mellitus, education, occupation, smoking status, alcohol intake, history of hypertension, leisure-time physical activity, consumption of coffee, consumption of green tea, energy-adjusted intakes of dietary magnesium, calcium, vitamin D, rice and total dietary fiber, and total energy intake | 7 |
| Fagherazzi et al, 2013 [9] | France | 1369/66118 | Women | 53±7 | 14 | FFQ (100%) | Confirmed via health insurance records and questionnaire | >967 ml/week vs. none: 0.93 (0.78–1.10) | Years of education, smoking status, physical activity; hypertension, hypercholesterolemia, use of hormone replacement therapy, family history of diabetes, self-reported use of antidiabetic drugs, alcohol intake,omega-3 fatty acid intake, carbohydrate intake, coffee, fruit and vegetables, processed-meat consumption, dietary pattern, total energy intake and BMI | 7 |
| Muraki et al, 2013 [10] | USA | NHS: 6358/66105 NHS II: 3153/85104 HPFS: 2687/36173 | Men and women | NHS: 52–77 NHS II: 35–52 HPFS: 40–75 | NHS: 25 NHS II: 9 HPFS: 23 | FFQ (sugar-sweetened) | Self-reported and validated in a random sample | ≥1 serving/day <1 serving/week: 1.21 (1.13–1.29) | Age, ethnicity, BMI, smoking status, multivitamin use, physical activity, family history of diabetes, menopausal status and post-menopausal hormone use, oral contraceptive use (for Nurses' Health Study II), total energy intake, fruit juice consumption and the modified alternate healthy eating index score | 8 |
| Mursu et al. 2013 [11] | Finland | 432/2332 | Men | 42–60 | 19.3 | Instructed 4–d food recording (unknown) | The National hospital discharge registry and Social Insurance Institution of Finland reimbursement registry | Q4 vs. Q1: 0.99 (0.74–1.31) | Age, examination years, BMI,waist-to-hip ratio, smoking, education, leisuretime physical activity, family history of diabetes, and intakes of energy and alcohol | 7 |
NHS, Nurses' Health Study; HPFS, Health Professionals Follow-up Study; FFQ, food-frequency questionnaire; BMI, body mass index.
The quality of each study was assessed by Newcastle–Ottawa quality scale.
Meta-analysis of fruit juice intake and risk of developing type 2 diabetes
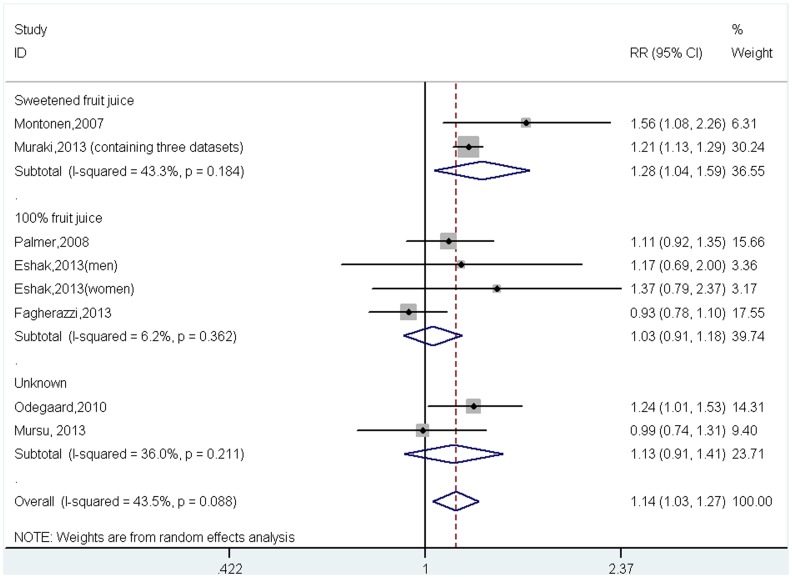
A total of 375,261 participants, including 19,986 with incident type 2 diabetes, were included in the meta-analysis. The pooled results indicate that individuals with a higher intake of fruit juice had a greater risk of developing type 2 diabetes (RR = 1.14, 95%CI = 1.03–1.27 p = 0.01, Figure 2), with modest evidence of between-study heterogeneity (I 2 = 43.5%, p = 0.09).
Figure 2. Relative risk for incident type 2 diabetes for highest versus lowest intake of fruit juice (by type of juice).
To determine if the risk of developing type 2 diabetes was different for fruit juice with added sugar than for 100% fruit juice, subgroup analyses were conducted stratified for sugar-sweetened fruit juice and 100% fruit juice. Four studies (191,686 participants, including 12,375 with type 2 diabetes) investigated the association between sugar-sweetened fruit juice and risk of developing type 2 diabetes, and four studies (137,663 participants and 4,906 cases) investigated the association between 100% fruit juice and risk of type 2 diabetes. Notably, higher intake of sugar-sweetened fruit juice was significantly associated with greater risk of incident type 2 diabetes (RR = 1.28, 95%CI = 1.04–1.59, p = 0.02, I 2 = 43.3%, p = 0.184, Figure 2), while there was no association between intake of 100% fruit juice and risk of incident type 2 diabetes (RR = 1.03, 95%CI = 0.91–1.18, p = 0.62, I 2 = 6.2%, p = 0.362, Figure 2).
Since the publication by Muraki et al. [10] did not provide the study-specific result for each of the three studies included in their meta-analysis, we were unable to assess the effects of the other characteristics of the participants in these studies, such as age, gender, origin of country, follow-up time, whether or not BMI was adjusted for the association between sugar-sweetened fruit juice and type 2 diabetes. But we did assess those variables for the other four studies for the association between 100% fruit juice and incident type 2 diabetes. As the age of the study population and follow-up time were similar between these four studies, we only assessed the effects of gender, origin of country, and whether or not BMI was adjusted. The results remained non-significant for 100% fruit juice in both sexes (men: RR = 1.17, 95%CI = 0.69–1.99; women: RR = 1.02, 95%CI = 0.90–1.16), in each country (USA: RR = 1.11, 95%CI = 0.92–1.34; Japan: RR = 1.26, 95%CI = 0.86–1.85; France: RR = 0.93, 95%CI = 0.78–1.10), and in both models with or without adjustment for BMI (without adjustment for BMI: RR = 1.11, 95%CI = 0.92–1.34; adjusted for BMI: RR = 0.98, 95%CI = 0.84–1.15).
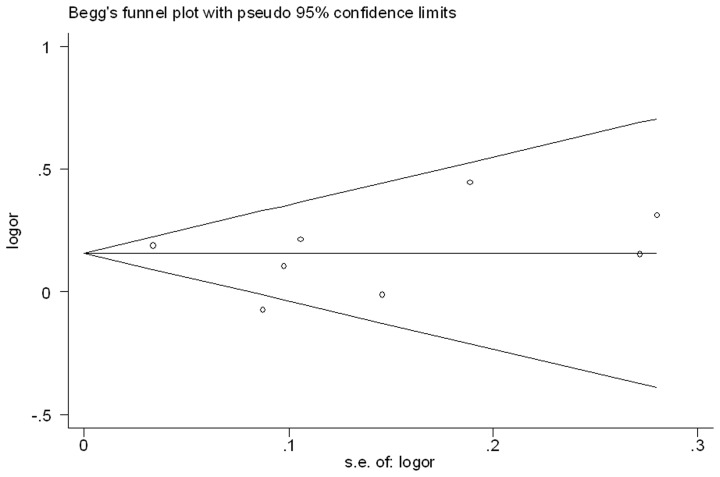
Potential publication bias
No publication bias was detected (p = 0.71 for Begg's test and p = 0.77 for Egger's test; Figure 3).
Figure 3. Funnel plot of the association between intake of fruit juice and incident type 2 diabetes.
Discussion
In the present study, we first performed a systematic meta-analysis to investigate the association between fruit juice intake and risk of incident type 2 diabetes. Results from our meta-analysis suggested that a greater intake of fruit juice was associated with a 14% higher risk of incident type 2 diabetes. However, in subgroup analyses, only sugar-sweetened fruit juice intake was associated with an increased risk of developing type 2 diabetes while 100% fruit juice had no effect.
Two previous meta-analyses showed no association between higher intake of whole fruit and incident type 2 diabetes [22], [23]. However, one recent publication including three large-scale prospective studies showed that a higher intake of whole fruit decreased risk of type 2 diabetes (≥3 servings/day vs.<4 servings/week: RR = 0.88, 95%CI = 0.81–0.96) [10]. An updated meta-analysis is warranted to clarify these inconsistent results.
In the Nurses' Health Study II, fruit punch, a sugar-sweetened fruit drink but different from fruit juice, was associated with a greater risk of incident type 2 diabetes [18]. Indeed, higher consumption of SSBs, including soft drinks, fruit drinks, iced tea, and energy and vitamin water drinks, was associated with development of type 2 diabetes in a previous meta-analysis [4]. Just recently, the relation between fruit juice intake and type 2 diabetes has received more attention. Based on our findings, sugar-sweetened fruit juice had a similar deleterious metabolic action as SSBs in the development of type 2 diabetes. First, the beneficial components of whole fruit, such as naturally occurring soluble fiber, vitamins, minerals and phytochemicals, might have been destroyed or diminished in processing. Second, the high glycemic load of added sugars in beverages may increase the risk of developing type 2 diabetes [24]. In addition, liquid calories may result in more rapid and larger changes in serum levels of glucose and insulin than whole fruit [10].
A previous systematic review reported no association between 100% fruit juice intake and risk of obesity in children and adolescents [25]. This finding is consistent with ours that 100% fruit juice had no effect on the risk of developing type 2 diabetes. The mechanism underlying this association is unclear but two points might explain the finding. First, for sugar-sweetened fruit juice, the healthy components of whole fruit may be destroyed during the processing stage; second, the naturally occurring sugars in 100% fruit juice may have different metabolic effects than added sugars [6], [18].
Our study has several strengths, including the prospective study design, large sample size, long follow-up duration, and relatively precise RRs (95%CIs) adjusted for potential confounders in the studies included in the current meta-analysis. However, several limitations should be considered. First, only several publications were included in the present meta-analysis. However, the total sample size for both sugar-sweetened fruit juice and 100% fruit juice subgroups was relatively large. Second, although most known confounding factors have been adjusted for, we cannot rule out the effect of residual confounding on the observed association. Third, all studies in the meta-analysis used fruit juice intake assessed at baseline; however, it is possible that individuals may have changed their intake of fruit juice during the follow-up period. However, the non-differential misclassification tends to attenuate the observed association towards the null. Fourth, we were unable to determine a dose-response association between fruit juice intake and incidence of type 2 diabetes since different units, e.g., kilogram, milliliter, glass, drink or time, were used to quantify the amount of juice intake. In addition, although we performed the meta-analysis of high intake of fruit juice compared with low intake, the quantities of high and low intakes among the studies may be different. Finally, potential publication bias might influence our results even though Begg's and Egger's tests were not significant.
In conclusion, the present meta-analysis showed that 100% fruit juice intake was not associated with the risk of developing type 2 diabetes; but, a higher intake of sugar-sweetened fruit juice was associated with an increased the risk of incident type 2 diabetes. Our findings have important public health implications. Sugar-sweetened fruit juice is not a healthy choice to replace SSBs, and individuals should limit their intake of sugar-sweetened fruit juice [26] to prevent the development of type 2 diabetes.
Supporting Information
Supporting PRISMA checklist.
(DOC)
Funding Statement
The authors have no funding or support to report.
References
- 1. Kit BK, Fakhouri TH, Park S, Nielsen SJ, Ogden CL (2013) Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999–2010.Am J Clin Nutr. 98: 180–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zenith International (2008) Report on Global Soft Drinks. Bath, United Kingdom: Zenith International, Ltd.
- 3. Kaiser KA, Shikany JM, Keating KD, Allison DB (2013) Will reducing sugar-sweetened beverage consumption reduce obesity? Evidence supporting conjecture is strong, but evidence when testing effect is weak. Obes Rev 14: 620–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Malik VS, Popkin BM, Bray GA, Després JP, Willett WC, et al. (2010) Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care 33: 2477–2483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Montonen J, Järvinen R, Knekt P, Heliövaara M, Reunanen A (2007) Consumption of sweetened beverages and intakes of fructose and glucose predict type 2 diabetes occurrence. J Nutr 137: 1447–1454. [DOI] [PubMed] [Google Scholar]
- 6. Palmer JR, Boggs DA, Krishnan S, Hu FB, Singer M, et al. (2008) Sugar-sweetened beverages and incidence of type 2 diabetes mellitus in African American women. Arch Intern Med 168: 1487–1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Odegaard AO, Koh WP, Arakawa K, Yu MC, Pereira MA (2010) Soft drink and juice consumption and risk of physician-diagnosed incident type 2 diabetes: the Singapore Chinese Health Study. Am J Epidemiol 171: 701–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eshak ES, Iso H, Mizoue T, Inoue M, Noda M, et al. (2013) Soft drink, 100% fruit juice, and vegetable juice intakes and risk of diabetes mellitus. Clin Nutr 32: 300–308. [DOI] [PubMed] [Google Scholar]
- 9. Fagherazzi G, Vilier A, Saes Sartorelli D, Lajous M, Balkau B, et al. (2013) Consumption of artificially and sugar-sweetened beverages and incident type 2 diabetes in the Etude Epidemiologique aupres des femmes de la Mutuelle Generale de l'Education Nationale-European Prospective Investigation into Cancer and Nutrition cohort. Am J Clin Nutr 97: 517–523. [DOI] [PubMed] [Google Scholar]
- 10. Muraki I, Imamura F, Manson JE, Hu FB, Willett WC, et al. (2013) Fruit consumption and risk of type 2 diabetes: results from three prospective longitudinal cohort studies. BMJ 347: f5001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mursu J, Virtanen JK, Tuomainen TP, Nurmi T, Voutilainen S (2013) Intake of fruit, berries, and vegetables and risk of type 2 diabetes in Finnish men: the Kuopio Ischaemic Heart Disease Risk Factor Study. Am J Clin Nutr [Epub ahead of print]. [DOI] [PubMed]
- 12. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, et al. (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283: 2008–2012. [DOI] [PubMed] [Google Scholar]
- 13.Wells GA, Shea B, O'connell D, Peterson J, Welch V, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed October 2013).
- 14. Mantel N, Haenszel W (1959) Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 22: 719–748. [PubMed] [Google Scholar]
- 15. Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50: 1088–1101. [PubMed] [Google Scholar]
- 17. Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315: 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schulze MB, Manson JE, Ludwig DS, Colditz GA, Stampfer MJ, et al. (2004) Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA 292: 927–934. [DOI] [PubMed] [Google Scholar]
- 19. Bazzano LA, Li TY, Joshipura KJ, Hu FB (2008) Intake of fruit, vegetables, and fruit juices and risk of diabetes in women. Diabetes Care 31: 1311–1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. InterAct consortium (2013) Consumption of sweet beverages and type 2 diabetes incidence in European adults: results from EPIC-InterAct. Diabetologia 56: 1520–1530. [DOI] [PubMed] [Google Scholar]
- 21. Paynter NP, Yeh HC, Voutilainen S, Schmidt MI, Heiss G, et al. (2006) Coffee and sweetened beverage consumption and the risk of type 2 diabetes mellitus: the atherosclerosis risk in communities study. Am J Epidemiol 164: 1075–1084. [DOI] [PubMed] [Google Scholar]
- 22. Hamer M, Chida Y (2007) Intake of fruit, vegetables, and antioxidants and risk of type 2 diabetes: systematic review and meta-analysis. J Hypertens 25: 2361–2369. [DOI] [PubMed] [Google Scholar]
- 23. Carter P, Gray LJ, Troughton J, Khunti K, Davies MJ (2010) Fruit and vegetable intake and incidence of type 2 diabetes mellitus: systematic review and meta-analysis. BMJ 341: c4229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Livesey G, Taylor R, Livesey H, Liu S (2013) Is there a dose-response relation of dietary glycemic load to risk of type 2 diabetes? Meta-analysis of prospective cohort studies. Am J Clin Nutr 97: 584–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. O'Neil Carol E, Nicklas Theresa A (2008) A Review of the Relationship Between 100% Fruit Juice Consumption and Weight in Children and Adolescents. AJLM 2: 315–354. [Google Scholar]
- 26. Davis MM, Gance-Cleveland B, Hassink S, Johnson R, Paradis G, et al. (2007) Recommendations for prevention of childhood obesity. Pediatrics 120: S229–S253. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting PRISMA checklist.
(DOC)