Abstract
Trauma exposure and PTSD are associated with poorer physical health. Psychological and behavioral mechanisms may help account for this relationship. In this study, we tested avoidant coping and alcohol use as mediators of the relationship between trauma exposure, PTSD, and self-reported physical health complaints in female drinkers. In 827 college women, we compared three groups: women with no trauma history, women with a sexual assault but no PTSD, and women with a sexual assault and PTSD, on avoidant coping, alcohol use, and physical health complaints. We found that PTSD was positively associated with alcohol use and that both PTSD and trauma exposure were associated with increased avoidant coping. We also found that avoidant coping mediated the relationship between trauma, PTSD and physical health complaints. Alcohol use did not predict physical health but was associated with PTSD. These results suggest that in female college students coping may be more critical in the PTSD/physical health relationship than alcohol and have implications for targeting coping in young trauma-exposed women to improve physical health.
Keywords: PTSD, trauma exposure, college students, physical health, alcohol, coping
Sexual assault is common on college campuses with lifetime prevalence rates for women ranging from 50–75% (cf. Abbey, Parkhill, & Koss, 2005). In addition, a substantial portion of individuals enter universities with a trauma history (Pereda, Guilera, Forns, & Gómez-Benito, 2009), and 7% of incoming freshman report a history of sexual assault (Read, Ouimette, White, Colder, & Farrow, 2011). Approximately 30% of college women exposed to unwanted sexual experiences develop posttraumatic stress disorder (PTSD; Read et al., 2011). Both adult and child sexual assault is associated with increased physical health problems including somatic complaints (e.g., Kimerling & Calhoun, 1994; Kimerling, Clum, & Wolfe, 2000), poorer overall health status (e.g., Cloutier, Martin, & Poole, 2002; Masho, Odor, & Adera, 2005), and increased utilization of medical health services (e.g., Stein, Golding, Siegel, Burnam, & Sorenson, 1988; Koss, Woodruff, & Koss, 1991). In addition, there is evidence suggesting that physical health complaints persist chronically after traumatic events (e.g., Kimerling & Calhoun, 1994; Sutker, Uddo, Brailey, Allain, & Errera, 1994). Taken together, this underscores the need for better understanding of the complex relationships among sexual assault, PTSD, and physical health.
Although college students are generally physically healthy, health modifying behaviors are often established in young adulthood (Gordon-Larsen, Nelson, & Popkin, 2004), and even relatively minor physical health complaints (e.g., headaches, stomach upset) can be associated with functional impairment such as decreased class attendance and poorer academic performance. College women report more physically unhealthy days compared to college men (Zahran, Zack, Vernon-Smiley, & Hertz, 2007). Moreover, university students’ stress, alcohol use, and mental health concerns have been associated with poorer health (e.g., Zinzow et al., 2011). Associations between PTSD and physical health concerns have been studied extensively in non-college populations (e.g., Amstadter et al., 2011; Kimerling et al., 2000), but few studies have examined these in college sexual assault victims. In the few studies with college students, PTSD has been found to predict poorer physical health (Flood, McDevitt-Murphy, Weathers, Eakin, & Benson, 2009; Lawler, Ouimette, & Dahlstedt, 2005), more health concerns (Zinzow et al., 2011), and a greater likelihood to seek medical treatment (Amstadter et al., 2010; Flood et al., 2009). An estimated 9% of college students meet criteria for PTSD, but rates of trauma exposure are as high as 66% and rates of sexual assault for college women are estimated at 11% (Read et al., 2011). Given that rates of trauma and sexual assault are relatively high among college women, but that many of these women do not develop PTSD, it is important to tease apart the relative importance of both the experience of trauma and the presence of PTSD in predicting physical health for college students.
Schnurr and colleagues (Schnurr & Green, 2004; Schnurr & Jankowski, 1999) have proposed a model to explain the relationship between PTSD and health outcomes, highlighting the roles of biological, psychological, attentional, and behavioral mechanisms. In this paper, we explore two of these proposed mechanisms: psychological and behavioral pathways. Avoidant coping, one potential psychological mechanism, generally refers to cognitive-behavioral strategies that function to emotionally disengage the individual from a subjectively stressful situation. It is theorized that avoidant coping may be related to physical health outcomes through its influence on behavior, such as decreased treatment seeking and decreased engagement in activities that promote physical health (Lazarus, 1991). A recent study (Rutter, Weatherill, Krill, Orazem, & Taft, 2013) found that exercise mediated the relationship between PTSD, depression and physical health in a sample of undergraduates. PTSD, in particular, is related to avoidant coping (e.g., Coffey, Leitenberg, Henning, Turner, & Bennet, 1996; Ullman, Filipas, Townsend, & Starzynski, 2007), and trauma-specific and health-specific avoidant coping both mediate the relationship between PTSD and health (Lawler et al., 2005). Thus, avoidant coping may be an important mechanism by which PTSD is associated with physical complaints.
In regards to theorized behavioral mechanisms, alcohol use is one potentially important behavior which may predict physical health. In adolescents and in college samples, alcohol consumption has been indirectly related to health problems as well as directly related to increased rates of injuries, obesity, and sedentary behavior (e.g., Hingson, Heeren, Zakocs, Kopstein, & Wechsler, 2002; Nelson, Kocos, Lytle, & Perry, 2009). Among adolescents, greater frequency and quantity of alcohol consumption has also been associated with poorer self-perceived health, especially for women (Johnson & Richter, 2002) and physical symptoms such as headaches, nausea, and vomiting are some of the most commonly endorsed negative consequences of alcohol use for college students (Perkins, 2002). In addition, heavy alcohol use has been linked to deleterious chronic health effects including decreased immune functioning, increased infection, nutritional deficiencies, and liver damage (e.g., Cook, 2008; Romeo et al., 2007). Furthermore, PTSD and alcohol abuse are highly comorbid (Kessler, Sonnega, Bromet, & Hughes, 1995), and there is evidence that alcohol use increases following sexual assault (e.g., Danielson et al., 2009; Gidycz, Hanson, & Layman, 1995). It is theorized that this is due to the use of alcohol as a self-medication strategy to deal with distress related to victimization (Saladin, Brady, Dansky, & Kilpatrick, 1995); although, it is important to note that college students drink for a myriad of reasons in addition to coping (e.g., Ham & Hope, 2003; Read, Wood, Kahler, Maddock, & Palfai, 2003) and that college students often do not endorse using alcohol to cope (Kuntsche, Knibbe, Gmel, & Engels, 2005). Therefore, although alcohol use may overlap with coping motives, looking independently at coping and alcohol use can help tease apart their relative importance to understanding the relationships between PTSD and health outcomes. While alcohol misuse may be important in the relationship between PTSD and poor physical health (Rheingold, Acierno, & Resnick, 2004), findings on substance use as a mediator between PTSD and health concerns are mixed (Del Gaizo, Elhai, & Weaver, 2011; Flood et al., 2009). It is possible that alcohol use associated with PTSD contributes to poor health, alcohol use has an independent association with negative health outcomes in trauma-exposed populations, or that PTSD is predominantly responsible for elevated health concerns among trauma exposed populations.
In this study we investigated potential mediators of the relationship between sexual assault, PTSD, and physical health in female college students. This study extends previous literature by examining both psychological (avoidant coping) and behavioral risk (alcohol use) mechanisms. Specifically, by comparing three groups of women (those with no trauma history, those with a sexual assault history but no symptoms of PTSD, and those with current PTSD from a sexual assault) we investigated sexual assault exposure and PTSD as unique predictors of physical health complaints. We also evaluated avoidant coping and alcohol use as mediators between trauma and physical health. We hypothesized that PTSD would predict increased physical complaints, with the PTSD group reporting the most health complaints. We also hypothesized that both avoidant coping and alcohol use would predict increased health complaints and significantly mediate the relationship between PTSD and health. By focusing on women with varying degrees of episodic drinking we were able to focus on an at risk sample.
Method
Participants & Procedures
This study was part of a larger study on trauma exposure, alcohol use, and other health behaviors in college women. Contact information for a random sample of 11,544 female students was obtained from the Registrar’s Office at a large northwestern university. Participants were invited by mail and email between fall of 2008 and spring of 2010 to complete an online screening survey. The response rate (37.6%) was similar to other large scale studies in this population (e.g., Marlatt et al., 1998). Trauma history was assessed via the Sexual Experiences Survey (SES; Koss & Oros, 1982), the Childhood Victimization Questionnaire (CVQ; Finkelhor, 1979), and Traumatic Life Experiences Questionnaire (TLEQ; Kubany et al., 2000). Eligibility criteria included: age 18 and older, a history of at least one unwanted sexual experience, and at least some heavy episodic drinking (4+ drinks on at least two occasions in the past month).
Following screening, eligible participants who reported a history of sexual assault (n = 722) were directed to the online baseline survey to determine PTSD prevalence and severity and we assessed membership in one of two groups: sexual assault but no PTSD (PTSDNEG; n = 580), and sexual assault with PTSD (PTSDPOS; n = 142). A random sample of women with no past exposure to DSM-IV PTSD Criterion A traumatic events as measured by the TLEQ at screening (NOTR; n = 105) was also selected to complete the baseline survey. The sexual assault groups (PTSDNEG, PTSDPOS) reported, in response to the SES and CVQ, at least one experience of childhood or adult sexual victimizatioin that was not within the past 3 months. The PTSDPOS group also endorsed a minimum of one Criteria B re-experiencing symptom, three Criteria C avoidance symptoms, two Criteria D hyperarousal symptoms, and at least one area of functional impairment as a result of the above symptoms (e.g., interference with relationships) consistent with DSM-IV diagnostic criteria (American Psychiatric Association, 1994). Thus, all three groups (PTSDNEG, PTSDPOS, NOTR) reported some current drinking but varied in terms of trauma exposure and PTSD diagnostic status. Means and percentages for demographic and outcome variables are presented in Table 1. Participants were paid $10 for screening and $35 for baseline. All study procedures were approved by the university’s institutional review board.
Table 1.
Demographic information and main study measures by group
| PTSDPOS | PTSDNEG | NOTR | |
|---|---|---|---|
| (n = 142) | (n = 580) | (n = 105) | |
| M (SD) | M (SD) | M (SD) | |
| Age | 20.43 (2.16) | 20.41 (1.81) | 20.20 (1.50) |
| Racial Identity (%)* | |||
| Caucasian | 64.0 | 73.2 | 67.6 |
| Black | 3.6 | 0.9 | 0.0 |
| Asian/Pacific Islander | 17.3 | 15.1 | 24.8 |
| Native American/Alaskan Native | 1.4 | 0.7 | 0.0 |
| Multi-ethnic | 10.1 | 8.3 | 7.6 |
| Other | 3.6 | 1.9 | 0.0 |
| Ethnic Identity (%) | |||
| Hispanic | 7.1 | 5.1 | 5.7 |
| Sexual Orientation (%) | |||
| Heterosexual | 92.3 | 92.9 | 98.1 |
| Lesbian | 2.8 | 0.7 | 0.0 |
| Bisexual | 4.2 | 3.8 | 1.9 |
| Questioning | 0.7 | 2.6 | 0.0 |
| Class Standing | |||
| Freshman | 14.1 | 15.4 | 21.9 |
| Sophomore | 23.2 | 18.8 | 15.2 |
| Junior | 31.7 | 29.7 | 26.7 |
| Senior | 31.0 | 36.1 | 36.2 |
| Avoidant coping*** | 2.28 (.53)a | 1.83 (.49)b | 1.62 (.51)c |
| Drinks per week** | 12.83 (9.28)a | 11.02 (7.22)b | 9.97 (4.98)b |
| Drinks per peak occasion | 7.60 (3.44) | 7.68 (3.03) | 6.92 (2.61) |
| Physical health complaints*** | 24.59 (10.08)a | 18.18 (9.58)b | 12.88 (8.61)c |
Note.
Groups differ at the p< .05 level.
Groups differ at the p< .01 level
Groups differ at the p< .001 level.
Means in the same row that do not share subscripts significantly differ.
NOTR = no trauma exposure; PTSDNEG = reported childhood or adult sexual assault but no PTSD diagnosis; PTSDPOS = reported sexual assault and met criteria for PTSD diagnosis.
Measures
Total drinks per week was assessed using the Daily Drinking Questionnaire (Collins, Parks, & Marlatt, 1985), a measure of daily typical consumption. Responses were summed across all seven days of “a typical week in the past 3 months,” range = 0–66 drinks, M(SD) = 11.21(7.43).
Peak drinks on a single occasion was measured by an item on the Quantity Frequency questionnaire (Marlatt et al., 1998), with response options from 0 to 25+ drinks, range = 1–25, M(SD) = 7.58(3.06).
PTSD diagnosis and severity was assessed by the Posttraumatic Diagnostic Scale (Foa, Cashman, Jaycox, & Perry, 1997). Focusing on their worst unwanted sexual experience (PTSDPOS and PTSDNEG groups) or most stressful life experience (NOTR group), participants were asked to report their degree of distress over the last month for the 17 PTSD symptoms. Response options ranged from 0 (not at all) to 3 (very much). Nine additional dichotomous items (yes/no) were used to determine life impairment, and were included to determine diagnosis.
Avoidant coping was evaluated using the 28-item Brief Cope (Carver, 1997). Participants are asked to rate statements indicative of coping strategies from 1 (I haven’t been doing this at all) to 4 (I’ve been doing this a lot). Based on past literature (Schnider, Elhai, & Gray, 2007) we created a composite avoidant coping scale (α = .77) of the means from the self-distraction (e.g., “I’ve been turning to work or other activities to take my mind off things”), denial (e.g., “I’ve been refusing to believe that it has happened”), behavioral disengagement (e.g., “I’ve been giving up trying to deal with it”), and self-blame (e.g., “I’ve been criticizing myself”) subscales, which are items that represent behaviors that serve to disengage the individual from problems. We excluded the substance use items due to our inclusion of alcohol use separately in the analyses.
Physical health complaints were assessed by the Pennebaker Inventory of Limbic Languidness (Pennebaker, 1982), which asked participants to rate their experience of 54 somatic complaints on a 5-point scale. Consistent with prior studies (Kaysen et al., 2008), complaints were dichotomously coded (present/absent) and then summed to create a continuous count variable indicating total number of physical health complaints endorsed, range = 0–46; M(SD) = 18.61(10.07). Individuals who endorse more complaints on the PILL are more aware of unpleasant physical and somatic sensations than those who endorse fewer complaints.
Statistical Analyses
Prior to mediation analyses, differences between assault groupings (NOTR, PTSDNEG, PTSDPOS) on avoidant coping, alcohol use, and physical symptoms were assessed with analyses of variance (ANOVAs). The proposed mediators were examined for significant correlations before they were included in further analysis. SPSS macros for bootstrapping multiple mediation effects (Preacher & Hayes, 2008) were used to test the mediation models. The bootstrap method, an alternative approach to the causal steps of mediation testing of Baron and Kenny (1986), is a nonparametric resampling procedure that involves repeatedly sampling from the data set to generate a sampling distribution. This distribution is used to calculate confidence intervals (CIs) and bootstrap-estimated standard errors of the mediated effect (Shrout & Bolger, 2002).
For these analyses, 5,000 bootstrap resamples were used to generate 95% CIs per recommendations (Hayes, 2009). Given our categorical independent variable with three levels (NOTR, PTSDNEG, PTSDPOS), we created two dummy variables and ran two pairwise comparison models, using one dummy variable as the independent variable and the other as a covariate in each model. The PTSDNEG served as our reference group. Thus, in our first model we compared the NOTR group to the PTSDNEG group, and in our second model we compared the PTSDPOS group to the PTSDNEG group. In both cases, avoidant coping and alcohol use served as the mediators, while physical symptoms served as the outcome variable.
Results
Preliminary Analyses
Means and standard deviations for all outcome variables are presented in Table 1. Bivariate and point-biserial correlations (see Table 2) illustrated significant, positive associations between alcohol variables (total drinks per week and peak drinks). Avoidant coping was generally not associated with alcohol use. Additionally, although avoidant coping and total drinks per week were significantly correlated with assault, peak drinks were not. This was further demonstrated by an ANOVA in which differences in peak drinks was only marginally significant by assault group, p = .07. Assault group was significantly correlated with the remaining mediators (avoidant coping and total drinks per week). ANOVAs with assault group as the independent variable further demonstrated these significant effects, ps < .01. Specifically, Tukey’s post-hoc tests showed that the PTSDPOS group scored highest on avoidance coping, followed by PTSDNEG, followed by NOTR, all pairwise comparisons ps < .01 (see Table 2). With respect to alcohol consumption, the PTSDPOS group consumed significantly more drinks per week than the other two groups. Thus, in order to be parsimonious total drinks per week was used as the index of drinking consumption in meditational analyses, as it showed the stronger relationship with assault.
Table 2.
Correlations for Main Study Variables
| Variable | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. Trauma | — | |||
| 2. Avoidant coping | .34*** | — | ||
| 3. Drinks per week | .11** | .08* | — | |
| 4. Drinks per occasion | .05 | .02 | .56*** | — |
| 5. Physical complaints | .32*** | .35*** | .08* | .07* |
Note. Trauma defined as 1 = NOTR (no trauma exposure); 2 = PTSDNEG (reported childhood or adult sexual assault but no PTSD diagnosis); 3 = PTSDPOS (reported sexual assault and met criteria for PTSD diagnosis) and a point-biserial correlation was used due to the trauma variable being categorical.
p< .05
p< .01
p< .001.
The most common physical complaints are displayed in Table 3. An ANOVA followed by Tukey’s post-hoc tests showed that the PTSDPOS group scored highest on physical symptom severity, followed by PTSDNEG, followed by NOTR, all pair-wise comparisons ps < .001.
Table 3.
Most Common Physical Health Complaints in the Past Month as Indicated by the PILL
| Variable | N | Percentage Endorsed |
|---|---|---|
| 1. Acne or pimples on the face | 590 | 70.7% |
| 2. Headaches | 572 | 68.6% |
| 3. Upset stomach | 501 | 60.1% |
| 4. Eyes watering | 487 | 60.6% |
| 5. Itchy eyes or skin | 484 | 58% |
| 6. Back pain | 458 | 54.9% |
| 7. Heartburn or gas | 454 | 54.4% |
| 8. Sore muscles | 447 | 53.6% |
| 9. Insomnia or difficulty sleeping | 438 | 52.4% |
| 9. Stiff or sore muscles | 438 | 52.4% |
| 10. Running nose | 433 | 51.9% |
Note. The PILL was scored as a total sum of complaints endorsed as present. Shown in the Table are the frequencies for common complaints endorsed as present.
Mediation Effect Analyses
Bootstrapping for multiple mediation used listwise deletion, excluding 43 participants due to missing data on main study variables (final N in models = 784). A series of t-tests and chi-square analyses demonstrated that these participants did not significantly differ from those included in mediation analyses on any completed main study or demographic variables at the p < .05 level.
A multiple mediation analysis was tested in two path models (Figures 1 and 2), where assault group was the independent variable. The direct effect of NOTR versus PTSDNEG and indirect effects via the proposed mediators of avoidant coping and weekly alcohol use are presented in Figure 1. As shown here and in Table 4, sexual assault had a significant direct effect (“a” paths) on avoidant coping but not on alcohol use. Furthermore, avoidant coping but not alcohol use had a significant direct effect (“b” paths) on physical complaints. Regarding effects of assault on physical complaints, the difference between the total (β = −5.21, SE = 1.04) and direct effect (β = −4.01, SE = 1.01) is the total indirect effect exerted through the two mediators, with a point estimate of β = −1.19 and 95% CI of −1.92–.59. An examination of the indirect effects (Table 4) indicated that only avoidant coping was a significant mediator.
Figure 1.
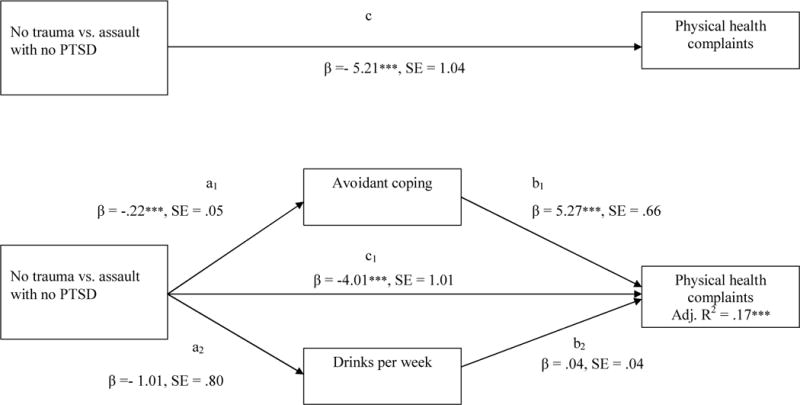
Multiple mediation model of the relationship between assault grouping (no trauma vs. assault with no PTSD) and physical symptoms. All coefficients represent unstandardized regression coefficients.
*p< .05. **p< .01. ***p< .001.
Figure 2.
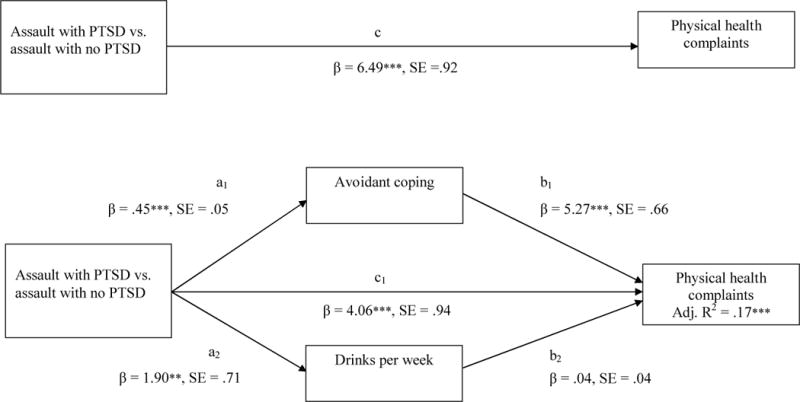
Multiple mediation model of the relationship between assault grouping (assault with PTSD versus assault with no PTSD) and physical symptoms. All coefficients represent unstandardized regression coefficients.
*p< .05. **p< .01. ***p< .001.
Table 4.
Mediation of the Effect of Trauma Group on Physical Health Complaints through Avoidant Coping and Drinks per Weeka
| Bootstrap Results for Mediation Effects
|
|||
|---|---|---|---|
| 95% Confidence Interval (CI)
|
|||
| Model | Mediation Effect (SE) | Lower | Upper |
| No trauma vs. trauma no PTSD | |||
|
| |||
| Indirect Effects | |||
| Avoidant coping | −1.15 (.33) | −1.88 | −.56 |
| Drinks per week | −.04 (.05) | −.19 | .04 |
| Total indirect | −1.19 (.33) | −1.91 | −.59 |
| Contrasts | |||
| Avoidant coping vs. drinks per week | 1.12 (.33) | .51 | 1.85 |
|
| |||
| Trauma with PTSD vs. trauma no PTSD | |||
|
| |||
| Indirect Effects | |||
| Avoidant coping | 2.36 (.40) | 1.65 | 3.22 |
| Drinks per week | .07 (.10) | −.06 | .35 |
| Total indirect | 2.43 (.41) | 1.71 | 3.32 |
| Contrasts | |||
| Avoidant coping vs. drinks per week | −2.29 (.41) | −3.18 | −1.55 |
Note. SE = standard error; CI = confidence interval. N = 784. Boldface type highlights a significant effect as determined by the 95% bias corrected and accelerated confidence interval (95% CI).
In the second path model (Figure 2), PTSDPOS was compared to PTSDNEG. PTSD had significant and direct effects (“a” paths) on avoidant coping and alcohol, but only coping had a significant direct effect (“b” path) on physical complaints. The total indirect effect of PTSD on health through the two mediators was significant, with a point estimate of β = 2.43 and 95% CI of 1.71–3.32. Specific indirect effects indicated that only coping was a significant mediator.
Discussion
This study is one of the few to examine the independent effect of behavioral (alcohol use) and psychological (avoidant coping) mechanisms on the relationship between PTSD and health, two of the four pathways proposed in Schnurr’s theoretical model of PTSD and health (e.g., Schnurr et al., 2004). Findings suggest both sexual assault and PTSD are predictive of greater avoidant coping and physical complaints. Our findings are consistent with the model by Schnurr and colleagues (Schnurr & Green, 2004; Schnurr & Jankowski, 1999), such that the relationship between trauma and physical health may be due to the effects of PTSD more so than trauma exposure. Moreover, the effect of PTSD on physical health complaints was partially mediated by avoidant coping, but not alcohol use, in this relatively young and physically healthy sample. These findings expand on previous findings that trauma specific and health specific avoidant coping predicts physical health in trauma exposed college students (Lawler et al., 2005) by suggesting that a general avoidant coping style also predicts increased physical health complaints. Taken together, this suggests that how people cope with stressors has an important impact on perceptions of their physical health.
Avoidant coping may also lead to other behaviors that decrease health and perceptions of well-being. For example, PTSD has been associated with reduced exercise, increased sedentary behavior, higher obesity, and higher perception of pain (e.g., Engel, 2004), although these factors have just begun being examined in college women with PTSD. The one study that looked at exercise in college students with PTSD found that it mediated the relationship between PTSD and physical health symptoms (Rutter et al., 2013). The current study builds upon these findings in suggesting that decreased engagement in active coping strategies is generally related to increased physical health complaints. It is possible that those who do not employ avoidant strategies, like distraction or denial, are better able to manage their PTSD symptoms and less likely to present somatically. Our finding that avoidant coping partially explains the relationship between both assault and PTSD with physical health complaints suggests that this general tendency is important in addition to trauma specific avoidance. The finding that increased endorsement of items indicative of general avoidance coping is related to physical health symptoms over and above PTSD suggests that it is not just PTSD-related avoidance symptoms that are important to consider in the trauma-health relationship but that broader avoidance tendencies also play a critical role. Given that college is a time of development and maturation these findings point to the importance of decreasing a tendency to cope with stressors by disengaging from the problem, as over time these perceptions and related behaviors may actually lead to demonstrably poorer health outcomes.
In contrast to the model proposed by Schnurr and colleagues (2004), alcohol use did not mediate relationships between sexual assault with or without PTSD and physical health complaints, although we did find relationships between presence of PTSD and higher alcohol consumption. Although prior research has demonstrated that trauma exposure and PTSD are associated with increased alcohol use (e.g., Kessler et al., 1995), which is in turn associated with negative physical health (Rehm et al., 2003), this relationship may have been complicated in the current sample by developmental factors. Although Flood and colleagues (2009) found a relationship between alcohol consequences and physical health in college students, most studies of alcohol-health associations have focused on older samples, more chronic health conditions, or factors such as violence associated with alcohol consumption (e.g., Rehm et al., 2003). Our sample was too young to manifest more chronic health conditions and the measure selected, general health concerns, may not have captured alcohol-related health consequences specifically. In regards to our hypothesis that alcohol would predict poorer health, one limitation of this study is that we did not include non-drinkers. Specifically, students were selected for the study if they endorsed some heavy episodic drinking; however, a range of alcohol use behavior was evident at baseline, with some participants reporting no drinking over the study, making this variable suitable to include in mediation analyses. Our method of sample selection may help explain why we did not find a relationship between drinking and health concerns. Future studies should include a broader range of drinking in order to better generalize to all college students. However, most research has not focused on relationships between PTSD, avoidant coping, alcohol and health within those who may be more at risk due to their general pattern of drinking.
We did not find meaningful associations between avoidant coping and alcohol use. In past research avoidant coping has been positively associated with alcohol use (Hruska, Fallon, Spoonster, Sledjeski, & Delahanty, 2011), suggesting that in our sample alcohol may be serving a function unique from coping. College students drink for many reasons, including social facilitation and positive reinforcement (Kuntsche et al., 2005; Read et al., 2003), and coping motives are relatively infrequently endorsed. Even in a trauma exposed sample, students may be drinking for reasons other than managing negative affect. In addition, we used a general coping measure, rather than one focused on drinking to cope, which may also explain differing findings. Future research that is able to prospectively explore relationships between trauma, different types of coping including alcohol-specific, trauma-specific, and more general coping, and drinking behavior is needed to elucidate more clearly the directional pathways between trauma and physical health complaints.
Individuals with PTSD are at increased risk for serious health problems and increased health care utilization over time. Even in a young and relatively healthy sample, individuals with PTSD endorsed experiencing more physical complaints than trauma exposed individuals without PTSD, though assault itself also increased physical distress. These findings suggest that avoidant coping may help explain this relationship and may be an important avenue for intervention. Avoidance of trauma related thoughts, feelings, and situations are a prominent part of PTSD, and these results suggest that a tendency to avoid more generally may also be important to trauma related symptoms and health. Adequate treatment of PTSD is associated with improvements in physical health (Galovski, Monson, Bruce, & Resick, 2009). Thus, increased screening for trauma exposure and PTSD and improved integration of PTSD treatments in college health clinics may improve both emotional and physical health in college students (Lawler et al., 2005). It is also possible that teaching skills oriented toward active problem solving could prevent more chronic health conditions from developing in trauma-exposed and non-trauma-exposed students. Finally, avoidant coping is only one potentially important psychological factor and others, such as experiences of general distress or symptoms of depression or anxiety, are also important to consider in the relationship between trauma exposure, PTSD and physical health. In particular, depression is often accompanied by somatic symptoms, especially in women (e.g., Silverstein, 2002). Looking at depression, PTSD, and coping can help us better understand complex relationships between mental health, adjustment, and physical health. Similarly, alcohol use is one of several potential behaviors that might mediate the relationship between trauma and physical complaints and future studies should consider additional mechanisms, such as exercise and health service utilization, along with alcohol use to get a clearer picture of the pathways between trauma and physical functioning.
Additional limitations of the current study should be noted. Our response rate to our initial screening invitation was somewhat low (~38%). This may be due to the tendency to avoid in a sample characterized by sexual assault and alcohol use, and thus our sample may be biased to those individuals with somewhat less severe PTSD symptoms. Moreover, this study utilized a sample of female college students, that by definition may be relatively high functioning and unlikely to have chronic mental or physical problems. Generalizability of these results are thus limited to similar samples; though, young adults are an important target for preventative health efforts and are at particularly high risk for sexual assault. In addition, similar to much of the work on this topic, this data was cross-sectional, retrospective in nature, and collected via self-report. Thus, conclusions drawn from mediation analyses are limited and we cannot state that either avoidant coping or alcohol use (our mediators) are causal links in the relationship between PTSD, trauma exposure and physical health (Kraemer, Stice, Kazdin, Offord, & Kupfer, 2001; Maxwell & Cole, 2007). Our measure of health concerns was solely self-report and did not include assessment of health costs, student health center visits, or chart review. In addition, we used a relatively liberal definition of physical health complaints to ensure that we captured the broad range of physical distress experienced by relatively healthy college students. However, the diverse and broad physical symptoms reported in this sample may overlap with more general somatic complaints associated with distress or depressive symptomatology. Although looking specifically at depression was outside the scope of this paper, additional research should consider its role in impacting physical health in trauma exposed samples. Finally, the measures used in this study assessed general alcohol use and coping strategies. Therefore, although the use of general measures minimized the overlap between PTSD and proposed mediators these findings cannot comment on the importance of trauma-specific coping strategies or particular drinking motives. Future investigations should investigate these factors to draw more specific conclusions on mechanisms that put assault victims at risk for physical health problems.
This study builds on the existing literature on assault, PTSD, avoidant coping, and health complaints. We examined two pathways in a high-risk group for whom the consequences of sexual assault on physical health have been relatively unexamined. The pattern of results suggest that targeting general coping strategies may be one way to improve health complaints, especially for young women with history of assault and/or PTSD. In addition, findings suggest that in this population avoidant coping may be an important mechanism of physical health.
Acknowledgments
This research was funded in part by grants from the National Institute of Alcohol Abuse and Alcoholism R21 AA016211 (PI: Kaysen) and F32 AA18609 (PI: Bedard-Gilligan). NIAAA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
References
- Abbey A, Parkhill MR, Koss MP. The effects of frame of reference on responses to questions about sexual assault victimization and perpetration. Psychology of Women Quarterly. 2005;29:364–373. doi: 10.1111/j.1471-6402.2005.00236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC US: American Psychiatric Press; 1994. [Google Scholar]
- Amstadter AB, Elwood LS, Begle A, Gudmundsdottir B, Smith DW, Resnick HS, Kilpatrick DG. Predictors of physical assault victimization: Findings from the National Survey of Adolescents. Addictive Behaviors. 2011;36:814–820. doi: 10.1016/j.addbeh.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amstadter AB, Zinzow HM, McCauley JL, Strachan M, Ruggiero KJ, Resnick HS, Kilpatrick DG. Prevalence and correlates of service utilization and help seeking in a national college sample of female rape victims. Journal of Anxiety Disorders. 2010;24:900–902. doi: 10.1016/j.janxdis.2010.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Biondi M, Picardi A. Psychological stress and neuroendocrine function in humans: The last two decades if research. Psychotherapy and Psychosomatization. 1999;68:114–50. doi: 10.1159/000012323. [DOI] [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol’s too long: Consider the Brief COPE. International Journal of Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Cloutier SS, Martin SL, Poole CC. Sexual assault among North Carolina women: Prevalence and health risk factors. Journal of Epidemiology and Community Health. 2002;56:265–271. doi: 10.1136/jech.56.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins R, Parks GA, Marlatt G. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53:189–200. doi: 10.1037/0022-006X.53.2.189. [DOI] [PubMed] [Google Scholar]
- Coffey P, Leitenberg H, Henning K, Turner T, Bennett RT. The relation between methods of coping during adulthood with a history of childhood sexual abuse and current psychological adjustment. Journal of Consulting and Clinical Psychology. 1996;64:1090–1093. doi: 10.1037/0022-006X.64.5.1090. [DOI] [PubMed] [Google Scholar]
- Cook RT. Alcohol abuse, alcoholism, and damage to the immune system—a review. Alcoholism: Clinical and Experimental Research. 1998;22(9):1927–1942. [PubMed] [Google Scholar]
- Danielson C, Amstadter AB, Dangelmaier RE, Resnick HS, Saunders BE, Kilpatrick DG. Trauma-related risk factors for substance abuse among male versus female young adults. Addictive Behaviors. 2009;34:395–399. doi: 10.1016/j.addbeh.2008.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Gaizo AL, Elhai JD, Weaver TL. Posttraumatic stress disorder, poor physical health and substance use behaviors in a national trauma-exposed sample. Psychiatry Research. 2011;188:390–395. doi: 10.1016/j.psychres.2011.03.016. [DOI] [PubMed] [Google Scholar]
- Engel CR. Somatization and multiple idiopathic physical symptoms: Relationship to traumatic events and posttraumatic stress disorder. In: Schnurr PP, Green BL, editors. Trauma and health: Physical health consequences of exposure to extreme stress. Washington, DC US: American Psychological Association; 2004. pp. 191–215. [DOI] [Google Scholar]
- Finkelhor D. What’s wrong with sex between adults and children? Ethics and the problem of sexual abuse. American Journal of Orthopsychiatry. 1979;49:692–697. doi: 10.1111/j.1939-0025.1979.tb02654.x. [DOI] [PubMed] [Google Scholar]
- Flood AM, McDevitt-Murphy ME, Weathers FW, Eakin DE, Benson TA. Substance use behaviors as a mediator between posttraumatic stress disorder and physical health in trauma-exposed college students. Journal of Behavioral Medicine. 2009;32:234–243. doi: 10.1007/s10865-008-9195-y. [DOI] [PubMed] [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment. 1997;9:445–451. doi: 10.1037/1040-3590.9.4.445. [DOI] [Google Scholar]
- Galovski TE, Monson C, Bruce SE, Resick PA. Does cognitive-behavioral therapy for PTSD improve perceived health and sleep impairment? Journal of Traumatic Stress. 2009;22:197–204. doi: 10.1002/jts.20418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gidycz CA, Hanson K, Layman MJ. A prospective analysis of the relationships among sexual assault experiences: An extension of previous findings. Psychology of Women Quarterly. 1995;19:5–29. doi: 10.1111/j.1471-6402.1995.tb00276.x. [DOI] [Google Scholar]
- Gordon-Larsen P, Nelson MC, Popkin BM. Longitudinal physical activity and sedentary behavior trends: Adolescence to adulthood. American Journal of Preventative Medicine. 2004;27:277–283. doi: 10.1016/j.amepre.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Ham LS, Hope DA. College students and problematic drinking: A review of the literature. Clinical Psychology Review. 2003;23:719–759. doi: 10.1016/S0272-7358(03)00071-0. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76:408–420. [Google Scholar]
- Hingson R, Heeren T, Zakocs R, Kopstein A, Wechsler H. Magnitude of alcohol-related mortality and morbidity among U.S. college students ages 18–24. Journal of Studies on Alcohol. 2002;63:136–44. doi: 10.15288/jsa.2002.63.136. [DOI] [PubMed] [Google Scholar]
- Hruska B, Fallon W, Spoonster E, Sledjeski EM, Delahanty DL. Alcohol use disorder history moderates the relationship between avoidance coping and posttraumatic stress symptoms. Psychology of Addictive Behaviors. 2011;25:405–414. doi: 10.1037/a0022439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson PB, Richter L. The relationship between smoking, drinking, and adolescents’ self-perceived health and frequency of hospitalization: Analyses from the 1997 National Household Survey on Drug Abuse. Journal of Adolescent Health. 2002;30:175–183. doi: 10.1016/S1054-139X(01)00317-2. [DOI] [PubMed] [Google Scholar]
- Kaysen D, Pantalone DW, Chawla N, Lindgren KP, Clum GA, Lee C, Resick PA. Posttraumatic stress disorder, alcohol use, and physical health concerns. Journal of Behavioral Medicine. 2008;31(2):115–125. doi: 10.1007/s10865-007-9140-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kimerling R, Calhoun KS. Somatic symptoms, social support, and treatment seeking among sexual assault victims. Journal of Consulting and Clinical Psychology. 1994;62:333–340. doi: 10.1037/0022-006X.62.2.333. [DOI] [PubMed] [Google Scholar]
- Kimerling R, Clum GA, Wolfe J. Relationships among trauma exposure, chronic posttraumatic stress disorder symptoms, and self-reported health in women: Replication and extension. Journal of Traumatic Stress. 2000;13:115–128. doi: 10.1023/A:1007729116133. [DOI] [PubMed] [Google Scholar]
- Koss MP, Woodruff WJ, Koss PG. Criminal victimization among primary care medical patients: Prevalence, incidence, and physician usage. Behavioral Sciences and the Law. 1991;9:85–96. doi: 10.1002/bsl.2370090110. [DOI] [PubMed] [Google Scholar]
- Koss MP, Oros CJ. Sexual Experiences Survey: A research instrument investigating sexual aggression and victimization. Journal of Consulting and Clinical Psychology. 1982;50:455–457. doi: 10.1037/0022-006X.50.3.455. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry. 2001;158:848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Leisen M, Kaplan AS, Watson SB, Haynes SN, Owens JA, Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment. 2000;12:210–224. doi: 10.1037/1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R. Why do young people drink? A review of drinking motives. Clinical Psychology Review. 2005;25:841–861. doi: 10.1016/j.cpr.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Lawler C, Ouimette P, Dahlstedt D. Posttraumatic Stress symptoms, coping, and physical health status among university students seeking health care. Journal of Traumatic Stress. 2005;18:741–750. doi: 10.1002/jts.20082. [DOI] [PubMed] [Google Scholar]
- Lazarus RS. Progress on a cognitive-motivational-relational theory of emotion. American Psychologist. 1991;46:819–834. doi: 10.1037/0003-066X.46.8.819. [DOI] [PubMed] [Google Scholar]
- Marlatt G, Baer JS, Kivlahan DR, Dimeff LA, Larimer ME, Quigley LA, Williams E. Screening and brief intervention for high-risk college student drinkers: Results from a 2-year follow-up assessment. Journal of Consulting and Clinical Psychology. 1998;66:604–615. doi: 10.1037/0022-006X.66.4.604. [DOI] [PubMed] [Google Scholar]
- Masho SW, Odor RK, Adera T. Sexual assault in Virginia: A population-based study. Women’s Health Issues. 2005;15:157–166. doi: 10.1016/j.whi.2005.04.001. [DOI] [PubMed] [Google Scholar]
- Maxwell SE, Cole DA. Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods. 2007;12:23–44. doi: 10.1037/1082-989X.12.1.23. [DOI] [PubMed] [Google Scholar]
- Nelson MC, Kocos R, Lytle LA, Perry CL. Understanding the perceived determinants of weight-related behaviors in late adolescence: A qualitative analysis among college youth. Journal of Nutrition Education and Behavior. 2009;41:287–292. doi: 10.1016/j.jneb.2008.05.005. [DOI] [PubMed] [Google Scholar]
- Pennebaker JW. The psychology of physical symptoms. New York, NY US: Springer Verlag, Inc; 1982. [Google Scholar]
- Pereda N, Guilera G, Forns M, Gómez-Benito J. The prevalence of child sexual abuse in community and student samples: A meta-analysis. Clinical Psychology Review. 2009;29:328–338. doi: 10.1016/j.cpr.2009.02.007. [DOI] [PubMed] [Google Scholar]
- Perkins HW. Surveying the Damage: A Review of Research on Consequences of Alcohol Misuse in College Populations. Journal of Studies on Alcohol. 2002;(Supplement No. 14):91–100. doi: 10.15288/jsas.2002.s14.91. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- Read JP, Ouimette P, White J, Colder C, Farrow S. Rates of DSM–IV–TR trauma exposure and posttraumatic stress disorder among newly matriculated college students. Psychological Trauma: Theory, Research, Practice, and Policy. 2011;3:148–156. doi: 10.1037/a0021260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Wood MD, Kahler CW, Maddock JE, Palfai TP. Examining the role of drinking motives in college student alcohol use and problems. Psychology Of Addictive Behaviors. 2003;17:13–23. doi: 10.1037/0893-164X.17.1.13. [DOI] [PubMed] [Google Scholar]
- Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos CT. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: An overview. Addiction. 2003;98:1209–1228. doi: 10.1046/j.1360-0443.2003.00467.x. [DOI] [PubMed] [Google Scholar]
- Rheingold AA, Acierno R, Resnick HS. Trauma, posttraumatic stress disorder, and health risk behaviors. In: Schnurr PP, Green BL, editors. Trauma and health: Physical health consequences of exposure to extreme stress. Washington, DC US: American Psychological Association; 2004. pp. 217–243. [DOI] [Google Scholar]
- Romeo J, Wärnberg J, Nova E, Díaz LE, Gómez-Martinez S, Marcos A. Moderate alcohol consumption and the immune system: a review. British Journal of Nutrition. 2007;98(S1):S111–S115. doi: 10.1017/S0007114507838049. [DOI] [PubMed] [Google Scholar]
- Saladin ME, Brady KT, Dansky BS, Kilpatrick DG. Understanding comorbidity between PTSD and substance use disorder: Two preliminary investigations. Addictive Behaviors. 1995;20:643–655. doi: 10.1016/0306-4603(95)00024-7. [DOI] [PubMed] [Google Scholar]
- Schnider KR, Elhai JD, Gray MJ. Coping style use predicts posttraumatic stress and complicated grief symptom severity among college students reporting a traumatic loss. Journal of Counseling Psychology. 2007;54:344–350. [Google Scholar]
- Schnurr P, Green B. Trauma and health: Physical health consequences of exposure to extreme stress. Washington, DC US: American Psychological Association; 2004. [DOI] [Google Scholar]
- Schnurr PP, Jankowski MK. Physical health and post-traumatic stress disorder: Review and synthesis. Seminar in Clinical Neuropsychiatry. 1999;4:295–304. doi: 10.153/SCNP00400295. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7:422–445. doi: 10.1037/1082-989X.7.4.422. [DOI] [PubMed] [Google Scholar]
- Silverstein B. Gender differences in the prevalence of somatic versus pure depression: a replication. American Journal of Psychiatry. 2002;159(6):1051–1052. doi: 10.1176/appi.ajp.159.6.1051. [DOI] [PubMed] [Google Scholar]
- Stein JA, Golding JM, Siegel JM, Burnam MA, Sorenson SB. Long term psychological sequelae of child sexual abuse: The Los Angeles Epidemiologic Catchment area study. In: Wyatt GE, Powell GJ, editors. Lasting effects of child sexual abuse. Newbury Park, CA US: Sage Publications; 1988. pp. 135–154. [Google Scholar]
- Sutker PB, Uddo M, Brailey K, Allain AN, Errera P. Psychological symptoms and psychiatric diagnoses in Operation Desert Storm troops serving graves registration duty. Journal of Traumatic Stress. 1994;7:159–171. doi: 10.1007/BF02102942. [DOI] [PubMed] [Google Scholar]
- Ullman SE, Filipas HH, Townsend SM, Starzynski LL. Psychosocial correlates of PTSD symptom severity in sexual assault survivors. Journal of Traumatic Stress. 2007;20:821–831. doi: 10.1002/jts.20290. [DOI] [PubMed] [Google Scholar]
- Zahran HS, Zack MM, Vernon-Smiley ME, Hertz MF. Health-related quality of life and behaviors risky to health among adults aged 18–24 years in secondary or higher education–United States, 2003–2005. Journal of Adolescent Health. 2007;41:389–397. doi: 10.1016/j.jadohealth.2007.05.011. [DOI] [PubMed] [Google Scholar]
- Zinzow HM, Amstadter AB, McCauley JL, Ruggiero KJ, Resnick HS, Kilpatrick DG. Self-rated health in relation to rape and mental health disorders in a national sample of college women. Journal of American College Health. 2011;59:588–594. doi: 10.1080/07448481.2010.520175. [DOI] [PMC free article] [PubMed] [Google Scholar]


