Abstract
Background
Although a series of meta-analysis demonstrated neuromuscular training (NMT) is an effective intervention to reduce anterior cruciate ligament (ACL) injury in female athletes, the potential existence of a dosage effect remains unknown.
Objective
To systematically review previously published clinical trials and evaluate potential dosage effects of NMT for ACL injury reduction in female athletes.
Design
Meta- and Sub-group analyses
Setting
The key words “knee”, “anterior cruciate ligament”, “ACL”, “prospective”, “neuromuscular”, “training”, “female”, and “prevention” were utilized in PubMed and EBSCO host for studies published between 1995 and May 2012.
Participants
Inclusion criteria set for studies in the current analysis were: 1) recruited female athletes as subjects, 2) documented the number of ACL injuries, 3) employed a NMT intervention aimed to reduce ACL injuries, 4) had a control group, 5) used a prospective control trial design and 6) provided NMT session duration and frequency information.
Main outcome measures
The number of ACL injuries and female athletes in each group (control and intervention) were compared based on duration, frequency, and volume of NMT through odds ratio (OR).
Results
A total of 14 studies were reviewed. Analyses that compared the number of ACL injuries with short versus long NMT duration showed greater ACL injury reduction in female athletes who were in the long NMT duration (OR:0.35, 95%CI: 0.23, 0.53, p=0.001) than the short NMT duration (OR: 0.61, 95%CI: 0.41, 0.90, p=0.013) group. Analysis that compared single versus multi NMT frequency indicated greater ACL injury reduction in multi NMT frequency (OR: 0.35, 95%CI: 0.23, 0.53, p=0.001) compared to single NMT frequency (OR: 0.62, 95%CI:0.41, 0.94, p=0.024). Combining the duration and frequency of NMT programs, an inverse dose-response association emerged among low (OR: 0.66, 95%CI: 0.43, 0.99, p=0.045), moderate (OR: 0.46, 95%CI: 0.21, 1.03, p=0.059), and high (OR:0.32, 95%CI: 0.19, 0.52, p=0.001) NMT volume categories.
Conclusions
The inverse dose-response association observed in the subgroup analysis suggests that the higher NMT volume, the greater prophylactic effectiveness of the NMT program and increased benefit in ACL injury reduction among female athletes.
1. INTRODUCTION
Since inception of Title IX of The Educational Assistance Act in 1972, the number of female athletes at high school level has increased more than 11 fold (from 0.3 to 3.2 million) whereas the increase in male athletes has been approximately 1.2 fold (from 3.7 to 4.5 million) in the United States.47 Along with the increase in number of female athletic participants, the number of resultant athletic injuries among female athletes has also increased rapidly. Among many types of debilitating injuries, female athletes have shown susceptibility to knee joint injury, especially anterior cruciate ligament (ACL) injury. In high school basketball, it is reported that rate of one in every 81 female athletes suffered an ACL injury1,2 and the total number of ACL injuries among female athletes was estimated to be approximately 38,000 annually in the United States as of 2001.3 The similar trend has also been reported in the college level as date through the National Collegiate Athletic Association (NCAA) from 1989 to 1998, which demonstrated female soccer and basketball players have 2.4 times and 4.1 times higher risk for suffering an ACL injury compared to their male counterparts in the same sports at college level, respectively4.
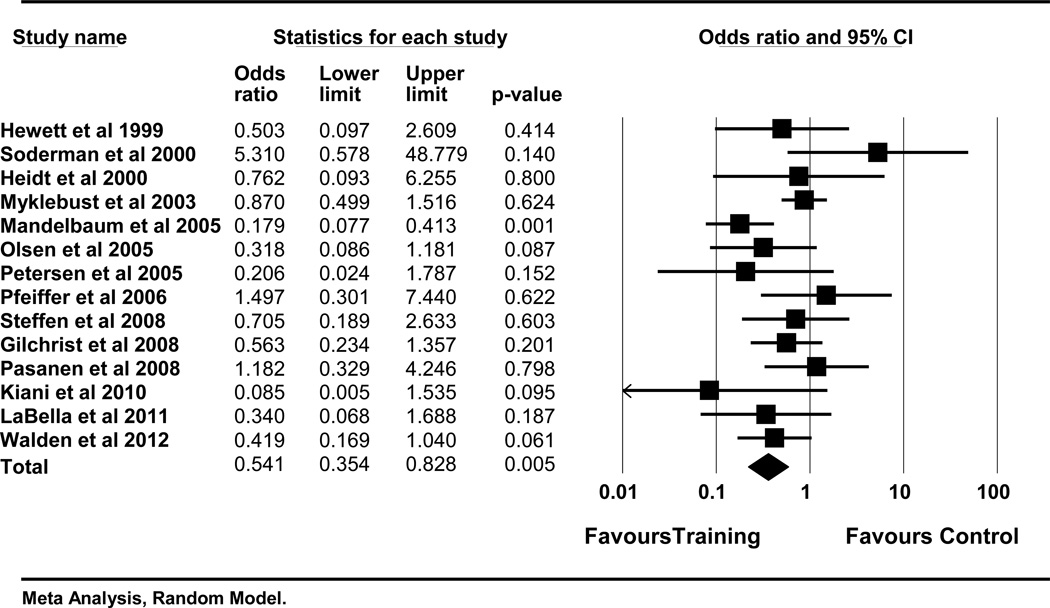
The disproportionately higher ACL injury risk in female athletes compared to their male counterparts is considered multi-factorial in nature and often discussed from anatomical, hormonal, and biomechanical standpoints.5,6 Several biomechanical studies found elevated knee abduction, limited knee flexion, asymmetrical landing patterns, higher ground reaction force, and poor trunk control are predictors for future ACL injuries in young female athletes.7–9 Consequently, a few intervention studies examined the effectiveness of neuromuscular training (NMT) through alteration of the biomechanical ACL risk factors, and a majority of the studies demonstrated prophylactically favorable alteration.10–13 However, findings from the laboratory do not seem to have translated as well to clinical environments. In fact, the ACL injury rate continues to rise annually.14 One of the reasons may be related to inconsistent findings within the previous ACL prevention clinical trials. A few clinical trials that used NMT as an intervention demonstrated a significant ACL injury reduction.15–17 Conversely, several NMT clinical trials did not show ACL injury reduction.18,19 For instance, using a specialized NMT called “prevent injury and enhance performance,” one study demonstrated 88% of ACL injury reduction in intervention group,17 but conversely, another actually recorded greater number of ACL injuries in intervention group compared to the control group.18 To determine the evidence whether or not NMT is an effective intervention for ACL injury reduction in female athletes, a meta-analysis was conducted and demonstrated effectiveness of NMT as an intervention on ACL injury reduction in female athletes.20 (Figure 1)
Figure 1.
A meta-analysis of 14 clinical trials – ACL injury
Although the most recent meta-analysis report20 and other studies21,22 identified NMT programs as useful interventions to reduce ACL injuries in female population, there is no clear answer for the heterogeneity of the ACL injury reduction differences within the clinical trials.15–19 One potential reason to explain the disparity of injury reduction rate may be related to the dosage of the NMT programs. When an unrelated study evaluating the effectiveness of neck rehabilitation, the study demonstrated that the rehabilitation exercises were effective when performed three times per week, but not when performed two times per week.23 Additionally, one of the recent clinical trials that utilized NMT as an intervention for female athletes to reduce ACL injury concluded that the NMT effect is “likely dose related.”24 Several clinical trials that aimed to reduce ACL injuries stated that too few number of NMT sessions performed is a limitation and may be a reason why desirable treatment effects were not obtained.25,26 Since previous meta-analysis confirmed effectiveness of NMT intervention to reduce ACL injury in young female athletes (Figure 1), the current project was designed to examine dosage effects of NMT, which was analyzed based on duration and frequency of NMT sessions. Therefore, the purpose of the current analysis was to systematically review previously published NMT intervention clinical trials that aimed to reduce ACL injury in female athletes and evaluate whether or not higher NMT dosage enhanced the prophylactic effectiveness of NMT on ACL injury in young female athletes.
2. METHODS
2.1. Literature Search and Criteria
A literature search was performed using the PubMed and EBSCO host (CINAHL, MEDLINE, and SPORTDiscus) from 1995 to 2012 in May 31, 2012. The key words searched were performed by applying a combination of the following words: “knee”, “anterior cruciate ligament”, “ACL”, “prospective”, “neuromuscular”, “training”, “female”, and “prevention” (Table 1). Language was limited to English, and subjects were all human. The following criteria were examined by the two independent reviewers to meet inclusion: 1) the number of ACL injury incidents were reported, 2) a NMT intervention that aimed to reduce ACL incidence was applied, 3) a control group was used, 4) a prospective controlled trial study design was employed, 5) females were included as subjects, and 6) NMT duration and frequency information were provided. Abstracts, posters, and unpublished data were not included in the final analysis. During this process, discrepancies in inclusion and exclusion of studies such as holding very similar characteristics of the above inclusionary criteria were discussed among authors. (Primary author (DS) and second author (GDM)) Egger’s regression was used to examine a potential risk of publication bias.
Table 1.
Stepped PubMed/EBSCOhost Search Strategy With the Number of Studies
| Step | Strategy | PubMed | EBSCO |
|---|---|---|---|
| #17 | Search (#11) AND (#16) | 402 | 76 |
| #16 | Search (#12) OR (#13) OR (#14) OR (#15) | 24897 | 41136 |
| #15 | Search “preventing” [TIAB] | 5101 | 1122 |
| #14 | Search “preventive” [TIAB] | 2496 | 2348 |
| #13 | Search “prevent” [TIAB] | 8551 | 2003 |
| #12 | Search “prevention” [TIAB] | 13521 | 14814 |
| #11 | Search (#5) AND (#10) | 4377 | 3616 |
| #10 | Search (#6) OR (#7) OR (#8) OR (#9) | 76185 | 75651 |
| #9 | Search “female” [TIAB] | 15605 | 25488 |
| #8 | Search “training” [TIAB] | 10336 | 26450 |
| #7 | Search “neuromuscular” [TIAB] | 1455 | 2646 |
| #6 | Search “prospective” [TIAB] | 52817 | 21939 |
| #5 | Search (#1) OR (#2) OR (#3) OR (#4) | 13050 | 60968 |
| #4 | Search “ACL” [TIAB] | 438 | 1104 |
| #3 | Search “anterior cruciate ligament” [TIAB] | 565 | 4330 |
| #2 | Search “knee” [TIAB] | 5074 | 18321 |
| #1 | Search “injury” [TIAB] | 8156 | 39322 |
Abbreviations: TIAB, title and abstract. Date was limited from January 1, 1995 to May 31, 2012.
Language was limited in English. Species were limited in humans. Sex was limited in female. MEDLINE was used for a journal category selection for the PubMEd. CINAHL, MEDLINE, and SPORTDiscus were included in the EBSCO search.
2.2. Quality of Methodology Evaluation Method
The Physiotherapy Evidence Database (PEDro) scale was used to analyze methodological quality of the included studies. The PEDro scale is a widely utilized measurement tool to rate the methodological quality of the randomized clinical intervention trials. The PEDro scale of the study reviewed was reported in the previous study.20
2.3. Level of Evidence and Strength of Recommendation Assessment Method
To evaluate the quality of the current analysis, the Strength of Recommendation Taxonomy (SORT) was implemented.27 The SORT is used to evaluate quality of the included studies and strength of recommendation, which facilitates generating a grade of strength of recommendation for the current analyses.
2.4. Data Extraction
The number of ACL injuries in each group (control and intervention) and the number of subjects in each group (control and intervention) were extracted for data analysis by the primary author. The number of ACL injuries was carefully reviewed and extracted. To examine the dosage effect, the time used for each NMT session (NMT session) and the number of NMT sessions per week (NMT frequency) were also reviewed and extracted from each study. In the scenario that the necessary information for the analysis was not documented in the published manuscript, an email was sent to the corresponding author listed in the original paper and a request for NMT duration and frequency information was completed.
2.5. Operational Definitions
To examine the dosage effects, reviewed trials were dichotomized based on status of the extracted NMT duration and NMT frequency. For the NMT duration, short and long periods were defined as follows:
-
1
short NMT duration = Less than 20 minutes of NMT per session
-
2
long NMT duration = More than 20 minutes of NMT per session
Likewise, the NMT frequency was defined as either single or multi using following definitions:
-
3
single NMT frequency = One session of NMT per week during in-season
-
4
multi NMT frequency = At least two sessions of NMT per week during in-season
Finally, the session length and session frequency were combined and defined as NMT volume.
Following definitions were used for low, moderate and high NMT volume:
-
5
low NMT volume = Up to 15 minutes per week was spent for NMT during in-season
-
6
moderate NMT volume = 15 to 30 minutes per week was spent for NMT during in-season
-
7
high NMT volume = More than 30 minutes per week was spent for NMT during in-season
2.6. Data Analysis
To evaluate NMT effectiveness and the potential dosage effects, a series of subgroup analyses with 95% confidence interval (CI) were employed. The NMT duration was examined based on short vs. long NMT duration. Likewise, single vs. multi NMT frequency was analyzed for assessing potential dosage effects of NMT frequency. Lastly, NMT volume was compared with low, moderate, and high NMT volume.
To compare a ratio of ACL injuries in subjects between intervention and control groups, an odds ratio (OR) was used. Because it was assumed that effect size of each study is different, random-effects model was chosen to minimize variability among the included studies. I2 statistics were calculated to express total variation across studies due to heterogeneity as opposed to random chance. The significance level of the heterogeneity was set at 0.05 a priori. Egger’s regression and trim and fill plot were used to examine potential risks of publication bias assessment. I2 statistics were employed to check heterogeneity of the sub-group analyses. The alpha level of the I2 was set at <0.05 priori. All analyses were performed by comprehensive meta-analysis software (Biostat, Englewood, NJ, USA).
3. RESULTS
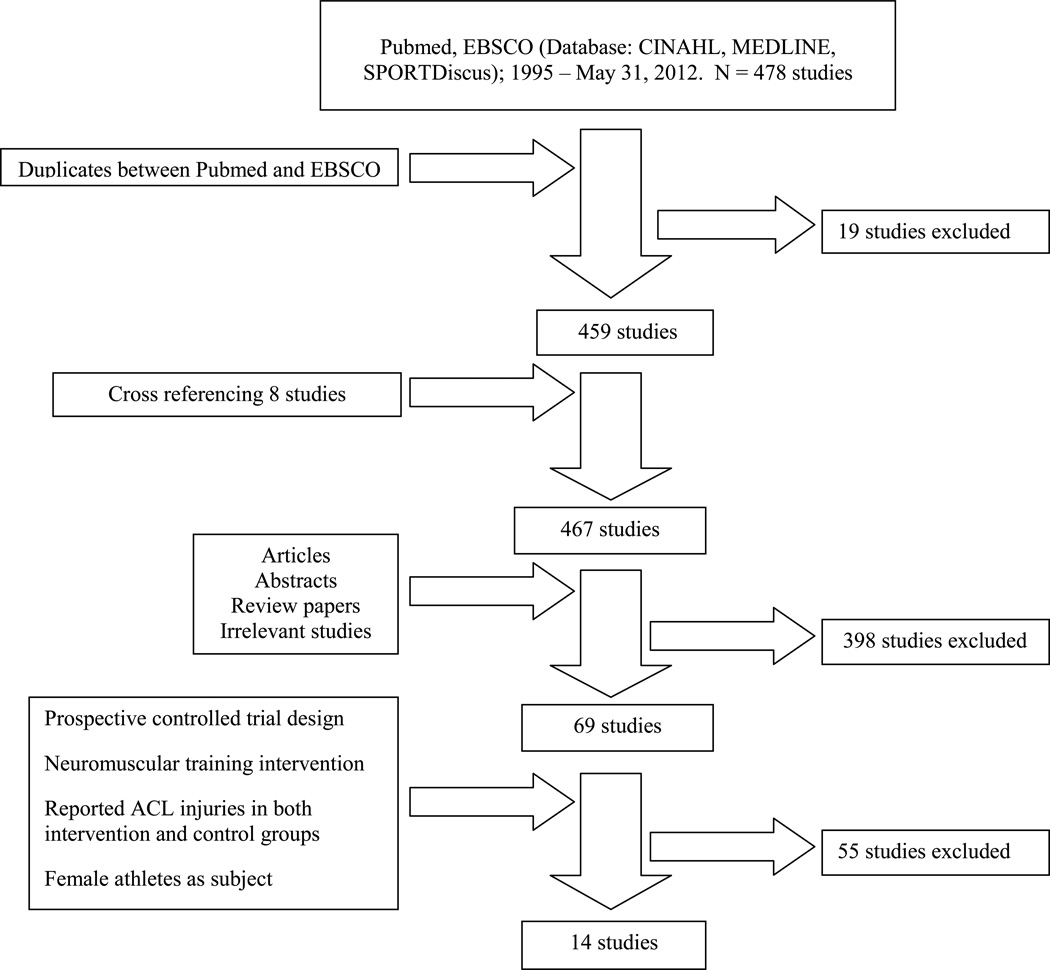
A total of 459 original studies were collected including cross-referenced studies resulting in, and 13 clinical trials that met the inclusion criteria of the current analyses. One study25 that did not completely fulfill the inclusion criteria because of an absence of control group due to the study design (cross-over design) was actually included since the study fulfilled the rest of the inclusion criteria and met the purpose of current project. Thus, a total of 14 studies15–19,24–26,28–33 were included in the current analyses (Figure 2). The quality of each study, number of ACL injuries, length and frequency of each NMT program and other related information are summarized in Table 2. The relevant methodological quality as evaluated by the PEDro scores was reported in the previously published study.20
Figure 2.
A flow chart of literature review
Table 2.
Summary of studies included in the review.
| Reference (Year) |
Study design |
Level of evidence |
Sports | Number of teams |
Age (mean±SD)f |
Type | Length | Frequency | Weekly time spent during in-season |
|---|---|---|---|---|---|---|---|---|---|
| Hewett et al. (1999) | Prospective non-randomized cohort | II | Soccer Volley ball Basket ball | 15 teams (C) 15 teams (I) |
14 – 18 yr (range) | Stretching, plyometrics, Weight training | 60 – 90 minutes | 3 days per week in pre-season | N/Ae |
| Soderman et al. (2000)a | Prospective randomized control | II | Soccer | 6 teams (C) 7 teams (I) |
C:20.4±5.4 yr I: 20.4 ±4.6 yr |
Balance with balance boards | 10 – 15 minutes | Each day for 30 days. 3 days per week rest of the season | 10–15 min |
| Heidt et al. (2000)b | Prospective randomized control | I | Soccer | 258 individuals (C) 42 individuals (I) |
14 – 18 yr (range) | Cardiovascular, Plyometrics, Strength, flexibility, agility, and sports specific drills | 75 minutes | 3 days per week in pre-season | N/Ae |
| Myklebust et al. (2003) | Prospective non-randomized cross over | II | Handball | 60 teams (1st yr) 58 teams (2nd yr) 52 teams (3rd yr) |
21–22 yr | Balance with mats and wobble boards | 15 minutes | 3 days per week for 5–7 weeks. Once a week for rest of the season | 15 min |
| Mandelbaum et al. (2005) | Prospective non-randomized cohort | II | Soccer | 207 teams (C) 97 teams (I) |
14–18 yr (range) | Basic warm-up, stretching, strengthening, plyometrics, and agility | 20 minutes | 2–3 times per week in in-season | 40–60 min |
| Olsen et al. (2005) | Prospective cluster randomized controlled | I | Handball | 59 teams (C) 61 teams (I) |
16–17 yr | Warm-up, technique, balance, strength and power | 15–20 minutes | 15 consecutive sessions. Once a week for rest of the season | 15–20 min |
| Petersen et al. (2005)c | Prospective matched cohort | II | Handball | 10 teams (C) 10 teams (I) |
C:19.8 I: 19.4 yr |
Education, balance-board exercise, jump training | 10 minutes | 3 times per week in pre-season. Once per week for rest of the season | 10 min |
| Pfeiffer et al. (2006) | Prospective non-randomized cohort | II | Soccer Volley ball Basket ball | 69 teams (C) 43 teams (I) |
14–18 yr (range) | Plyometrics | 20 minutes | 2 times per week in in-season | 40 min |
| Steffen et al. (2008) | Prospective block randomized controlled | I | Soccer | 51 teams (C) 58 teams (I) |
15.4 yr | Core stability, balance, plyometrics | 15 minutes | 15 consecutive sessions. Once a week for rest of the season | 15 min |
| Gilchrist et al. (2008) | Prospective cluster randomized controlled | I | Soccer | 35 teams (C) 26 teams (I) |
C:19.9 yr I: 19.9 yr |
Basic warm-up, stretching, strengthening, plyometrics, and agility | 20 minutes | 3 times per week in in-season | 60 min |
| Pasanen et al. (2008) | Prospective cluster randomized controlled | I | Floorball | 14 teams (C) 14 teams (I) |
24 yr | Running techniques, balance and body control, plyometrics, strengthening | 20–30 minutes | 2–3 times per week for pre-season (intensive training period) and once a week in in-season (maintenance period) | 40–90 min |
| Kiani et al. (2010)d | Prospective cluster non-randomized cohort | II | Soccer | 49 teams (C) 48 teams (I) |
C: 15.0 I: 14.7 yr |
Core strengthening, balance | 20–25 minutes | 2 days per week for 2 months. Once a week for rest of the season | 20–25 min |
| LaBella et al. (2011) | Prospective cluster randomized controlled | I | Soccer Basket ball | 53 teams (C) 53 teams (I) |
C: 16.2 I: 16.2 yr |
Strengthening, plyometrics, balance, agility | 20 minutes | 3 times per week in pre-and in-season | 60 min |
| Walden et al. (2012) | Prospective cluster randomized controlled | I | Soccer | 109 teams (C) 121 teams (I) |
C: 14.1 I: 14.0 yr |
Core stability, balance, jump-landing with knee alignment feedback | 15 minutes | 2 times per week. | 30 min |
Although the study was a randomized controlled design, the follow-up rate was low (51.2%). Therefore, the level of evidence was rated as II.
For the analysis purpose, data from 1st year intervention year was only used.
Although there was no specific statement, the neuromuscular training indicated plyometric components.
Although there were jump-landing maneuvers, repeated stretch-shortening cycle were not employed in the training.
The NMT was performed only during a pre-season. N/A stands for Not Applicable.
Unless otherwise indicated.
“C” stands for control group. “I” stands for Intervention group.
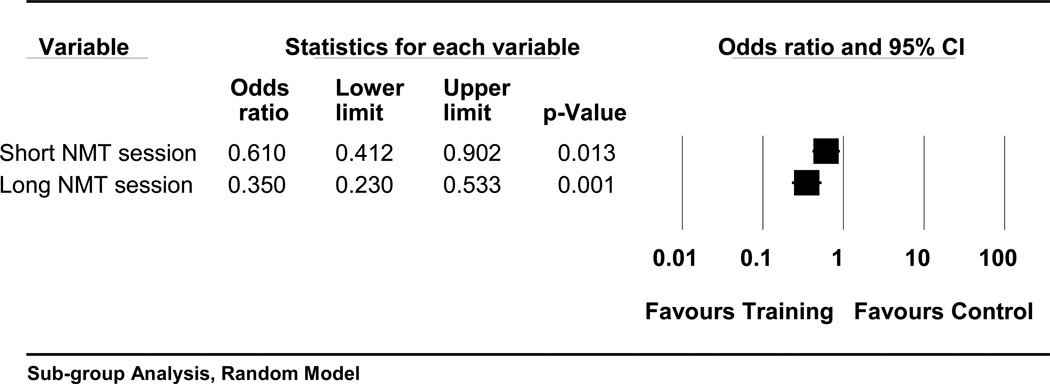
3.1. ACL injury: NMT Duration of 14 Clinical Trials
The sub-group analysis that compared the number of ACL injuries with short vs. long NMT duration within the 14 reviewed clinical trials15–19,24–26,28–33 indicated greater ACL injury reduction in the long NMT session (OR: 0.35, 95% CI: 0.23, 0.53, p=0.001) compared to the short (OR: 0.61, 95% CI: 0.41, 0.90, p=0.013) NMT session. (Figure 3)
Figure 3.
Subgroup analysis of neuromuscular training (NMT) duration and anterior cruciate ligament injury in 14 clinical trials.
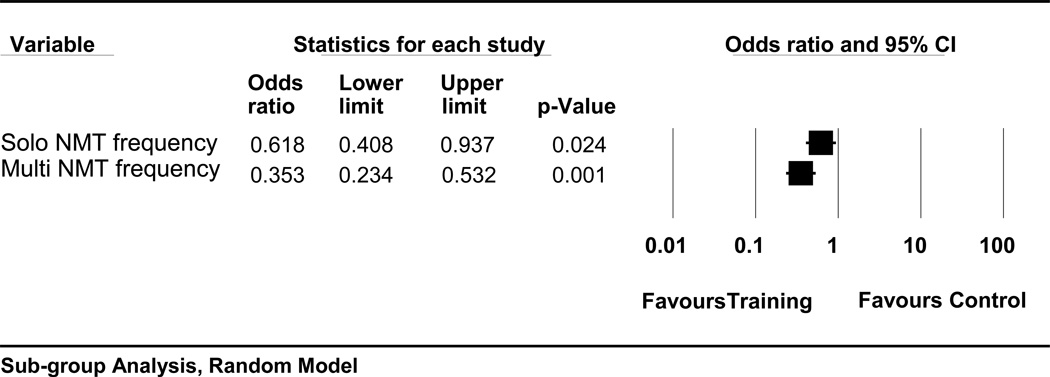
3.2. ACL injury: NMT Frequency of 12 Clinical Trials
Two clinical trials15,28 were removed from this analysis since they were pre-season programs and the reminder of the clinical trials had in-season NMT components; thus, the two clinical trials15,28 were not comparable. Comparison of the number of ACL injuries with single vs. multi NMT frequency with 12 reviewed clinical trials16–19,24–26,29–33 demonstrated greater ACL injury reduction in the multi NMT frequency groups (OR: 0.35, 95% CI: 0.23, 0.53, p=0.001) compared to the single (OR: 0.62, 95% CI: 0.41, 0.94, p=0.024) (Figure 4)
Figure 4.
Subgroup analysis of neuromuscular training (NMT) frequency and anterior cruciate ligament injury in 12 clinical trials.
3.3.ACL injury: NMT Volume of 12 Clinical Trials
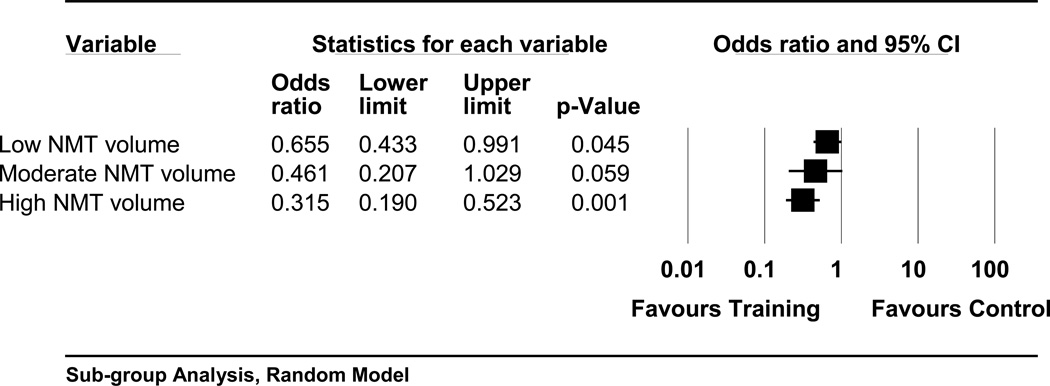
The aforementioned two clinical trials15,28 were removed from this analysis because they were implemented as pre-season NMT programs and the reminder of the clinical trials were in-season NMT programs; thus, the two clinical trials15,28 did not match with three categories for this analysis. The number of ACL injuries was evaluated based on low vs. moderate vs. high NMT volume classification with a total of 12 clinical trials.16–19,24–26,29–33 The analysis showed the greatest ACL injury reduction in the high NMT volume (OR: 0.32, 95% CI: 0.19, 0.52, p=0.001), then, the moderate (OR: 0.46, 95% CI: 0.21, 1.03, p=0.059) and the low (OR: 0.66, 95% CI: 0.43, 0.99, p=0.045) NMT volume programs. (Figure 5)
Figure 5.
Subgroup analysis of neuromuscular training (NMT) volume and anterior cruciage ligament injury in 12 clinical trials.
3.4. Evidence Synthesis
The SORT level of evidence of each clinical trial was listed in the Table 2. The SORT level of evidence can further generate a grade of strength of recommendation based on the level of consistent evidence, composed of A to C. In the current analysis, seven of the included clinical trials24,26,28,29,31–33 were rated as level I (high quality individual randomized control trial), while seven clinical trials15–19,25,30 were rated as level II (lower quality clinical trial and cohort study). Although the number of level I and II clinical trials are equivalent, the current meta-analysis supports consistency of evidence since 11 of the 14 reviewed clinical trials demonstrated fewer ACL injuries in the NMT intervention group compared to control groups. In addition, a summary effect of the meta-analysis (Figure 1) supports the evidence consistency. Based on the consistency of the results from included clinical trials, the strength of recommendation grade for the current evidence is A (recommendation based on consistent and good quality patient-oriented evidence).
3.5. Heterogeneity
The I2 statistics of the subgroup NMT analysis for duration, frequency, and volume indicated p-value greater than 0.05 (p = 0.06 for duration, p = 0.06 for frequency, and p = 0.09 for volume). Since the p-value did not find a statistical significance, the heterogeneity effects were considered minimal.
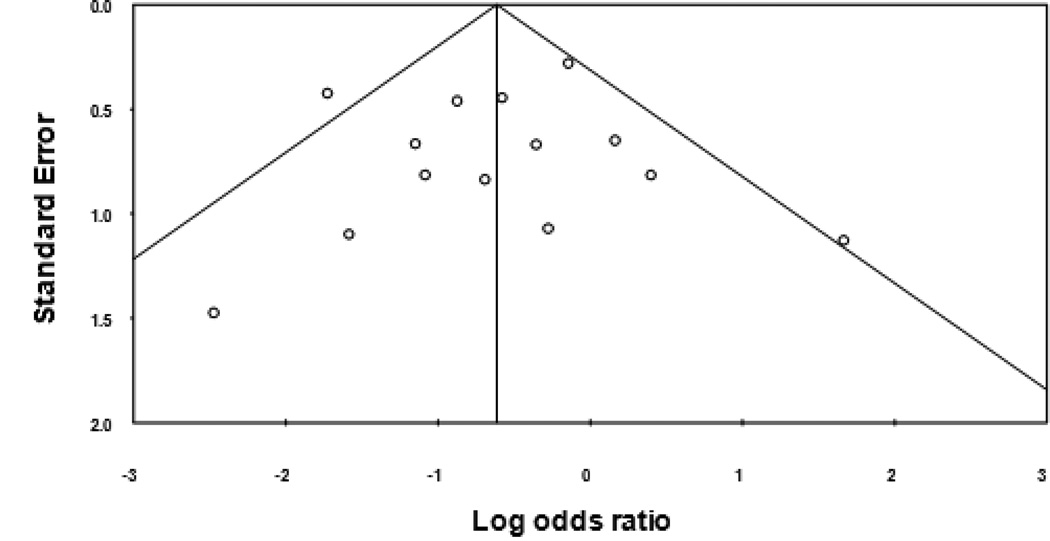
3.6. Bias assessment
Egger’s regression for the publication bias for the 14 reviewed clinical trials showed an interception −0.17 (95% CI: −1.93, 1.59, p=0.41, one tailed), indicating no publication bias in the current analysis, and the trim and fill plot also displayed no publication bias (Figure 6)
Figure 6.
A trim and fill plot for testing publication bias.
4. DISCUSSION
The previously performed meta-analysis generated an OR 0.54 (95% CI: 0.35, 0.83, p=0.05; Figure 1) ensuring effectiveness of NMT as an intervention demonstrating 46% of risk reduction for suffering an ACL injury compared to those who did not perform NMT. Although the reviewed NMT clinical trials were fairly diverse (Table 2), closely examining NMT programs from a dosage standpoint, several key NMT elements appear to link with greater ACL injury reduction: NMT duration, frequency and volume. Relative to dosage effect, the two dichotomized sub-group analyses (short vs. long NMT duration and single vs. multi NMT frequency analyses) resulted in more significant prophylactic effects in the long NMT duration and multi NMT frequency groups compared to the short NMT duration and single NMT session groups. The two dichotomized sub-group analyses demonstrated dosage effects between duration and frequency of NMT programs and number of ACL injuries in young female athletes. It implies that longer and more frequent NMT programs demonstrated greater NMT prophylactic effects. Comparing the risk difference between the long and short NMT session, the long NMT session clinical trial groups showed 26% lower risk. Similarly, the multi NMT frequency group demonstrated 27% lower risk compared to the single NMT frequency group. In fact, one of the reviewed clinical trials compared the ACL injury rate based on compliance, and more compliant athletes demonstrated significantly less ACL injury risk compared to those who were less compliant.33 Similarly, another clinical trial reviewed in this analysis also documented lower risk of noncontact lower leg injury in the high compliant group.32 The results of these studies thus support longer duration and more frequent NMT interventions for increased prophylactic effect.
4.1. Neuromuscular Training Duration
Breaking down the NMT volume with sub-components including duration (short vs.long) and frequency (single vs. multi), it appeared that fewer types of NMT exercises were prescribed in the short NMT session studies.18,25 This can simply be interpreted that it is difficult to perform many types of NMT exercises in the limited amount of NMT session time, which might have impacted reducing the prophylactic effects of NMT. However, the long NMT session raises a question with regard to practicality. The longer the NMT session duration is, the more difficult to implement a NMT program. Two studies that had the longest NMT durations were pre-season programs15,28, which may indicate a difficulty of implementing a long NMT program, especially during the in-season schedule. A NMT implementation requires understanding and support from coaching staff, and they may not be supportive for implementing a long NMT program because the long NMT session often results in decreasing actual practice time. The same issue is applied to the NMT frequency, which may result in a reduction in compliance.
4.2. Neuromuscular Training Frequency
The current data regarding NMT frequency needs to be interpreted cautiously. All clinical trials that had the single NMT session during in-season frequently had NMT sessions in the protocols during pre-season. For instance, two clinical trials26,29 had athletes perform preventive NMT 15 consecutive times in the beginning of the season and decreased the NMT frequency to once a week during in-season. Similarly, two other clinical trials employed NMT three times per week during pre-season and reduced the NMT frequency to once a week during the in-season.25,30 Therefore, although the current analyses suggested performing preventive NMT interventions less than 20 minutes per session once a week during in-season can reduce 38–39% of ACL injury risk (Figure 3 and 4), practicing one NMT session per week during the in-season without frequent pre-season NMT workouts is less likely to demonstrate the prophylactic effects on ACL injury reduction. Another meta-analysis that evaluated effectiveness of NMT programs to lower ACL incidence in female athletes reported that the combined pre-and in-season NMT intervention is the most effective process to reduce ACL incidence rather than either pre- or in-season NMT programs alone.34
Potential benefits of performing pre-and in-season NMT interventions were evidenced by two clinical trials reviewed in this project. A clinical trial with a cluster randomized controlled design performed by Gilchrist et al. recorded similar ACL injury rates between athletes in intervention and control groups in the first half of the soccer season. However, during the second half of the season, no ACL injury was observed among athletes in the intervention group, but five ACL injuries were noted in the control group.31 Similarly, in a clinical trial conducted by LaBella et al, no ACL injury was documented in basketball athletes in the intervention group during second half of the regular season.24 These studies support that it takes a certain amount of time for athletes to adopt the patterns of NMT performance. Physiologically, muscle activation enhancement was not observable after three weeks of physical training, but was seen after six weeks.35 More interestingly, one study reported that strength gains to trunk and lower extremity is slower compared to upper extremity.36 In addition to the physiological alteration, motor skill adaptations and transformations in actual performance during practice and game situations may require a longer time period. Thus, considering the necessary time for athletes to attain the neuromuscular training skills, it is logical to provide NMT during the pre-season.
4.3. Neuromuscular Training Volume
The NMT volume analysis, which consists of low, moderate and high volume categorizations and is a combination of NMT session and NMT frequency during in-season, also supports the inverse dose-response association. The observed inverse dose-response association is that: the greater the NMT volume, the greater the prophylactic effect. The statistically greater prophylactic effects were found in the higher NMT volume group compared to the lower NMT volume group. The high NMT volume group may reduce ACL injury risk by 68%, whereas the risk reduction of the moderate and low NMT volume groups were 54% and 44% respectively. The 24% risk reduction differences between the high and low NMT volume groups can be attributed to dosage (NMT duration and frequency) difference. The results of the NMT volume analysis provide a meaningful clinical implication. The current analysis suggests that 68% of non-contact ACL injuries can be avoided if a preventive NMT program of more than 20 minutes duration and multiple per week sessions is employed in female athletes (Figure 5).37–4
A majority of those who suffer ACL rupture undergo reconstructive surgery, but still experience early osteoarthritis (OA) changes within eight to15 years after the reconstruction surgery.42–45 Researchers have reported knee related quality of life in these individuals,43 and if a female athlete has an ACL injury during her middle teens, pre-mature OA may be present at age of 30 or even earlier. Hence, performing NMT may provide substantial future health benefits for females. Female athletes can potentially reduce risk for those negative consequences, which, in turn, hold more opportunities to maintain a physically active lifestyle.
Several recent studies reported significance of NMT dosage using a compliance measurement. Using a prospective cluster randomized controlled design, Soligard et al. examined an association between NMT compliance and soccer related injuries.46 Comparing the acute and overall soccer injuries to compliance rates with tertile fashion (high, intermediate, and low), high compliance rate athletes showed 35% lower risks compared to intermediate compliance rate athletes in overall soccer related injuries. Similarly, in terms of acute soccer injuries, high compliance rate athletes experienced a 39% risk reduction in relation to athletes with intermediate compliance rate. In addition, the high NMT compliance rates and low injury risks were also reported by Sugimoto et al.48 The authors also categorized the compliance rates in tertile method (high, moderate, and low) and examined the association with ACL injury rates of six clinical trials. The analysis identified that the moderate NMT compliance clinical trials had 3.1 times greater risk of suffering from ACL injuries compared to high compliance clinical trials. Similarly, the low compliance clinical trials demonstrated 4.9 times greater ACL injury risk compared to high compliance clinical trials. Both analyses documented impact of the NMT dosage through compliance assessment in relation to athletic injuries, which support the result of the current subgroup analysis.
4.4. Limitations
For the subgroup analysis for the dosage effect, the length of the NMT programs was considered as a variable. However, the NMT length within each clinical trial demonstrated a significant diversity ranging between six to eight weeks15,28,30 to four to seven months.16–19,24–26,29–33 Thus, the current project could not find a meaningful cut-off point for the NMT length subgroup analysis. However, most clinical trials16–19,24–26,29–33 used the NMT as a warm-up and the number of ACL injuries were counted during the competitive athletic seasons. Therefore, the longer the length of NMT and competitive seasons were, the more numbers of ACL injuries were likely to be recorded. Hence, the current project focused on aspects within the NMT length within each clinical trial.
In the NMT volume analysis, the moderate NMT group demonstrated fairly wide CIs compared to high and low NMT volume categorizations. (Figure 5) This is mainly explained by a small number of subjects in this group compared to the other two groups. The other two groups had more than 3,500 subjects in both intervention and control groups, but the number of subjects in the moderate NMT group in each arm did not reach 2,000, likely accounting for the wide CIs.
In the total of 14 included clinical trials, seven clinical trials24,26,28,29,31–33 were rated as level I (high quality individual randomized control trial), and the remaining seven clinical trials15–19,25,30 were rated as level II (lower quality clinical trial and cohort study). Randomization is known as an effective method to reduce potential bias. Therefore, if more clinical trials were performed with randomized manners, outcome of each cohort clinical trial might have differed, and the evidence would be more substantial. Thus, increased trials of this nature would be valuable. However, in order to present the best available evidence, the presented meta-analysis (Figure 1) was performed based on clinical trials found under a comprehensive and systematic literature search.
Although subject population were homogenous (young female athletes), diversity was observed in the sports: soccer, handball, basketball and floorball. In addition to the different type of sports, subjects’ ages and given NMT programs varied among clinical studies. It was challenging to differentiate the reviewed clinical trials further based on the sports, ages, and types of NMT. Thus, the prophylactic effects demonstrated by the current analyses may vary by sports, ages, and given NMT programs.
5. CONCLUSION
In order to find potential aspects to enhance prophylactic effectiveness of NMT, a series of subgroup analyses were performed, which found an inverse dose-response effect: The higher NMT volume, the greater the prophylactic effectiveness of the NMT program and more benefit for female athletes in ACL injury reduction. Specifically, about 70% of ACL injury was avoided if preventive NMT was performed a total of more than 30 minutes per week during the in-season. Since implementation of NMT requires coaching staff’s understanding and cooperation, it may be more realistic and applicable to perform NMT multiple times per week instead of one 30 minute session a week, especially during in-season. The current analysis suggests that the NMT duration is desirably longer than 20 minutes per session. In addition, a few reviewed clinical trials incorporated a substantial amount of NMT sessions during pre-season rather than just during in-season. Also, several clinical trials noted more ACL injuries in the beginning of competitive seasons. Because of these two factors, performing preventive NMT both during pre- and in-seasons is suggested. The current analysis was rated as an evidence level A in the SORT evidence category. Hence, the results of this report encourage healthcare practitioners to apply preventive NMT to female athletes to minimize the likelihood of an ACL injury, which should promote a physically active and healthy lifestyle in young females’ lives.
Acknowledgements
The authors would like to acknowledge funding support from National Institutes of Health/NIAMS Grants R01-AR049735, R01-AR055563 and R01-AR056259. We would also like to thank the Sports Medicine Biodynamics teams at Cincinnati Children’s, the University of Kentucky and The Ohio State University for all their helpful input and support. The figure 1 was adapted from “The Influence of Age on the Effectiveness of Neuromuscular Training to Reduce Anterior Cruciate Ligament in Female Athletes” written by Myer GD et al. The permission was obtained from Myer GD.
Footnotes
The authors have no potential conflicts of interest that are directly relevant to the content of this study.
REFERENCES
- 1.Messina DF, Farney WC, DeLee JC. The incidence of injury in Texas high school basketball. A prospective study among male and female athletes. Am J of Sports Med. 1999;27:294–299. doi: 10.1177/03635465990270030401. [DOI] [PubMed] [Google Scholar]
- 2.Gomez E, DeLee JC, Farney WC. Incidence of injury in Texas girls' high school basketball. Am J Sports Med. 1996;24:684–687. doi: 10.1177/036354659602400521. [DOI] [PubMed] [Google Scholar]
- 3.Toth AP, Cordasco FA. Anterior cruciate ligament injuries in the female athlete. J Gend Specif Med. 2001;4:25–34. [PubMed] [Google Scholar]
- 4.Arendt EA, Agel J, Dick R. Anterior cruciate ligament injury patterns among collegiate men and women. J Athl Train. 1999;34:86–92. [PMC free article] [PubMed] [Google Scholar]
- 5.Griffin LY, Albohm MJ, Arendt EA, et al. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am J Sports Med. 2006;34:1512–1532. doi: 10.1177/0363546506286866. [DOI] [PubMed] [Google Scholar]
- 6.Hewett TE, Ford KR, Myer GD. Anterior cruciate ligament injuries in female athletes: Part 2, a meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med. 2006;34:490–498. doi: 10.1177/0363546505282619. [DOI] [PubMed] [Google Scholar]
- 7.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33:492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 8.Hewett TE, Torg JS, Boden BP. Video analysis o f trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med. 2009;43:417–422. doi: 10.1136/bjsm.2009.059162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zazulak BT, Hewett TE, Reeves NP, et al. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med. 2007;35:1123–1130. doi: 10.1177/0363546507301585. [DOI] [PubMed] [Google Scholar]
- 10.de Marche Baldon R, Lobato DF, Carvalho LP, et al. Effect of Functional Stabilization Training on Lower Limb Biomechanics in Women. Med Sci Sports Exerc. 2012:44135–44142. doi: 10.1249/MSS.0b013e31822a51bb. [DOI] [PubMed] [Google Scholar]
- 11.Lephart SM, Abt JP, Ferris CM, et al. Neuromuscular and biomechanical characteristic changes in high school athletes: a plyometric versus basic resistance program. Br J Sports Med. 2005;39:932–938. doi: 10.1136/bjsm.2005.019083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Myer GD, Ford KR, Brent JL, et al. Differential neuromuscular training effects on ACL injury risk factors in "high-risk" versus "low-risk" athletes. BMC musculoskeletal disorders. 2007;8:39. doi: 10.1186/1471-2474-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Myer GD, Brent JL, Ford KR, et al. A pilot study to determine the effect of trunk and hip focused neuromuscular training on hip and knee isokinetic strength. Br J Sports Med. 2008;42:614–619. doi: 10.1136/bjsm.2007.046086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007 Apr-Jun;42:311–319. [PMC free article] [PubMed] [Google Scholar]
- 15.Hewett TE, Lindenfeld TN, Riccobene JV, et al. The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Am J Sports Med. 1999;27:699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 16.Kiani A, Hellquist E, Ahlqvist K, et al. Prevention of soccer-related knee injuries in teenaged girls. Arch Intern Med. 2010 Jan 11;170:43–49. doi: 10.1001/archinternmed.2009.289. [DOI] [PubMed] [Google Scholar]
- 17.Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33:1003–1010. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 18.Soderman K, Werner S, Pietila T, et al. Balance board training: prevention of traumatic injuries of the lower extremities in female soccer players? A prospective randomized intervention study. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA. 2000;8:356–363. doi: 10.1007/s001670000147. [DOI] [PubMed] [Google Scholar]
- 19.Pfeiffer RP, Shea KG, Roberts D, et al. Lack of effect of a knee ligament injury prevention program on the incidence of noncontact anterior cruciate ligament injury. J Bone Joint Surg Am. 2006;88:1769–1774. doi: 10.2106/JBJS.E.00616. [DOI] [PubMed] [Google Scholar]
- 20.Myer GD, Sugimoto D, Thomas S, et al. The influence of age on the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a meta-analysis. Am Journal Sports Med. 2012;41:216–224. doi: 10.1177/0363546512460637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gagnier JJ, Morgenstern H, Chess L. Interventions designed to prevent anterior cruciate ligament injuries in adolescents and adults: a systematic review and meta-analysis. Am J Sports Med. 2013;41:1952–1962. doi: 10.1177/0363546512458227. [DOI] [PubMed] [Google Scholar]
- 22.Sadoghi P, von Keudell A, Vavken P. Effectiveness of anterior cruciate ligament injury prevention training programs. J Bone Joint Surg Am. 2012;94:769–776. doi: 10.2106/JBJS.K.00467. [DOI] [PubMed] [Google Scholar]
- 23.Nikander R, Malkia E, Parkkari J, et al. Dose-response relationship of specific training to reduce chronic neck pain and disability. Med Sci Sports Exerc. 2006;38:2068–2074. doi: 10.1249/01.mss.0000229105.16274.4b. [DOI] [PubMed] [Google Scholar]
- 24.LaBella CR, Huxford MR, Grissom J, et al. Effect of neuromuscular warm-up on injuries in female soccer and basketball athletes in urban public high schools: cluster randomized controlled trial. Arch Pediatr Adolesc Med. 2011;165:1033–1040. doi: 10.1001/archpediatrics.2011.168. [DOI] [PubMed] [Google Scholar]
- 25.Myklebust G, Engebretsen L, Braekken IH, et al. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. 2003;13:71–78. doi: 10.1097/00042752-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Steffen K, Myklebust G, Olsen OE, et al. Preventing injuries in female youth football--a cluster-randomized controlled trial. Scand J Med & Sci in Sports. 2008;18:605–614. doi: 10.1111/j.1600-0838.2007.00703.x. [DOI] [PubMed] [Google Scholar]
- 27.Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. J American Board of Family Practice. 2004;17:59–67. doi: 10.3122/jabfm.17.1.59. [DOI] [PubMed] [Google Scholar]
- 28.Heidt RS, Jr, Sweeterman LM, Carlonas RL, et al. Avoidance of soccer injuries with preseason conditioning. Am J Sports Med. 2000;28:659–662. doi: 10.1177/03635465000280050601. [DOI] [PubMed] [Google Scholar]
- 29.Olsen OE, Myklebust G, Engebretsen L, et al. Exercises to prevent lower limb injuries in youth sports: cluster randomised controlled trial. BMJ (Clinical research ed) 2005;330(7489):449. doi: 10.1136/bmj.38330.632801.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Petersen W, Braun C, Bock W, et al. A controlled prospective case control study of a prevention training program in female team handball players: the German experience. Arch Orthop Trauma Surg. 2005;125:614–621. doi: 10.1007/s00402-005-0793-7. [DOI] [PubMed] [Google Scholar]
- 31.Gilchrist J, Mandelbaum BR, Melancon H, et al. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med. 2008;36:1476–1483. doi: 10.1177/0363546508318188. [DOI] [PubMed] [Google Scholar]
- 32.Pasanen K, Parkkari J, Pasanen M, et al. Effect of a neuromuscular warm-up programme on muscle power, balance, speed and agility: a randomised controlled study. Br J Sports Med. 2009;43:1073–1078. doi: 10.1136/bjsm.2009.061747. [DOI] [PubMed] [Google Scholar]
- 33.Walden M, Atroshi I, Magnusson H, et al. Prevention of acute knee injuries in adolescent female football players: cluster randomised controlled trial. BMJ (Clinical research ed) 2012;344:e3042. doi: 10.1136/bmj.e3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yoo JH, Lim BO, Ha M, et al. A meta-analysis of the effect of neuromuscular training on the prevention of the anterior cruciate ligament injury in female athletes. Knee Surg Sports Traumatol Arthr. 2010;18:824–830. doi: 10.1007/s00167-009-0901-2. [DOI] [PubMed] [Google Scholar]
- 35.Vila-Cha C, Falla D, Farina D. Motor unit behavior during submaximal contractions following six weeks of either endurance or strength training. J Appl Physiol. 2010;109:1455–1466. doi: 10.1152/japplphysiol.01213.2009. [DOI] [PubMed] [Google Scholar]
- 36.Chilibeck PD, Calder AW, Sale DG, et al. A comparison of strength and muscle mass increases during resistance training in young women. Eur J Appl Physiol Occup Physiol. 1998;77:170–175. doi: 10.1007/s004210050316. [DOI] [PubMed] [Google Scholar]
- 37.Agel J, Arendt EA, Bershadsky B. Anterior cruciate ligament injury in national collegiate athletic association basketball and soccer: a 13-year review. Am J Sports Med. 2005;33:524–530. doi: 10.1177/0363546504269937. [DOI] [PubMed] [Google Scholar]
- 38.Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. Am J Sports Med. 1995;23:694–701. doi: 10.1177/036354659502300611. [DOI] [PubMed] [Google Scholar]
- 39.Boden BP, Dean GS, Feagin JA, Jr, et al. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23:573–578. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 40.Myklebust G, Maehlum S, Engebretsen L, et al. Registration of cruciate ligament injuries in Norwegian top level team handball. A prospective study covering two seasons. Scand J Med & Sci in Sports. 1997;7:289–292. doi: 10.1111/j.1600-0838.1997.tb00155.x. [DOI] [PubMed] [Google Scholar]
- 41.Walden M, Hagglund M, Werner J, et al. The epidemiology of anterior cruciate ligament injury in football (soccer): a review of the literature from a gender-related perspective. Knee Surg Sports Traumatol Arthrosc. 2011;19:3–10. doi: 10.1007/s00167-010-1172-7. [DOI] [PubMed] [Google Scholar]
- 42.Li RT, Lorenz S, Xu Y, et al. Predictors of radiographic knee osteoarthritis after anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39:2595–2603. doi: 10.1177/0363546511424720. [DOI] [PubMed] [Google Scholar]
- 43.Lohmander LS, Ostenberg A, Englund M, et al. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50:3145–3152. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 44.Oiestad BE, Holm I, Aune AK, et al. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med. 2010;38:2201–2210. doi: 10.1177/0363546510373876. [DOI] [PubMed] [Google Scholar]
- 45.Oiestad BE, Holm I, Engebretsen L, et al. The association between radiographic knee osteoarthritis and knee symptoms, function and quality of life 10–15 years after anterior cruciate ligament reconstruction. Br J Sports Med. 2011;45:583–588. doi: 10.1136/bjsm.2010.073130. [DOI] [PubMed] [Google Scholar]
- 46.Soligard T, Nilstad A, Steffen K, et al. Compliance with a comprehensive warm-up programme to prevent injuries in youth football. Br J Sports Med. 2010;44:787–793. doi: 10.1136/bjsm.2009.070672. [DOI] [PubMed] [Google Scholar]
- 47.National Federation of State High School Associations. 2010 High School Participation Survey. Indianapolis, Ind.: National Federation of State High School Associations; 2002. [Google Scholar]
- 48.Sugimoto D, Myer GD, Bush HM, et al. Compliance with neuromuscular training and anterior cruciate ligament injury risk reducion in female atheltes: A meta-analysis. J Athl Train. 2012;47:714–723. doi: 10.4085/1062-6050-47.6.10. [DOI] [PMC free article] [PubMed] [Google Scholar]