Abstract
Despite efforts to reduce morbidity and mortality in breast cancer, Latinas continue to have lower 5-year survival rates than their non-Latina white counterparts. All along the cancer continuum from screening to follow-up of abnormal screening to diagnosis and treatment to survivorship, Latinas fare poorer than non-Latina whites. To close this gap, a number of research projects across the continuum have attempted to improve breast cancer outcomes. In this review, we examine studies that have been carried out in breast cancer along the cancer continuum. We focus not only on randomized, controlled trials, but also on quasi-experimental, and pre- and post-test studies that provided interventions for positive breast cancer outcomes. We examine not only the intervention outcomes, but also the type of intervention targets and type of intervention implementation. In future breast cancer research among Latinas, more emphasis should be placed on the steps in detection and treatment that occur after screening.
Keywords: breast cancer, breast cancer disparities, cancer control continuum, interventions Latinas
Breast cancer in Latinas in the USA presents a complicated picture. On the one hand, a lower incidence of breast cancer exists for Latinas compared with non-Latino whites (NLWs) [1], although highly acculturated Latinas are likely to have breast cancer rates that are consistent with those of NLWs [2]. On the other hand, breast cancer is the most common cancer among Latinas [101]; Latinas have lower 5-year survival rates than NLWs [1,3,102]. Furthermore, unlike NLWs who are experiencing a drop in mortality rates, Latina mortality rates are remaining stable [103]. Finally, Latinas experience lower rates of 5-year cancer-specific survival [104].
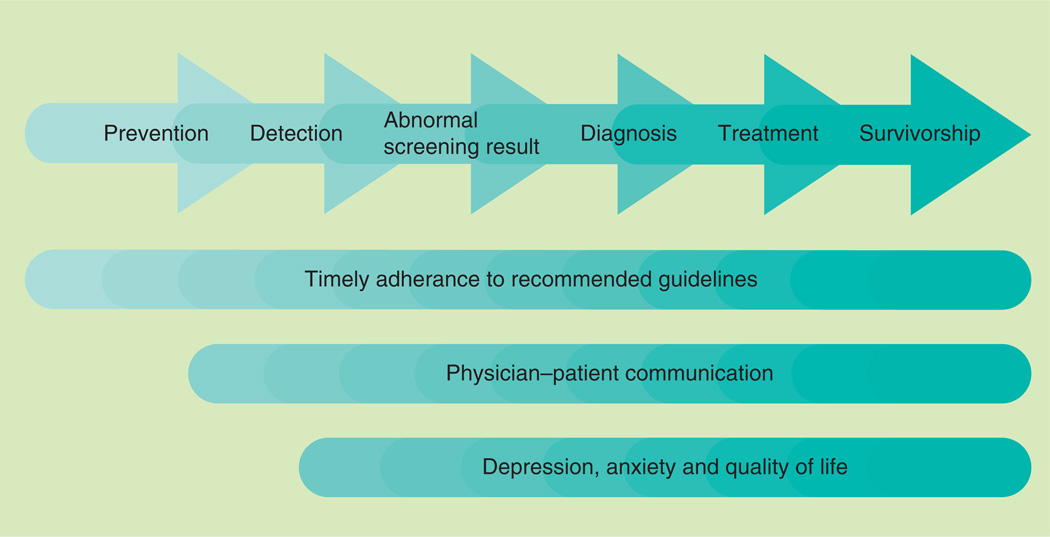
Ethnically-based disparities between the US NLWs and Latinas in breast cancer prevention and control have been documented at every stage of the cancer continuum: screening, follow-up of abnormal screening results, cancer diagnosis/treatment, survivorship and end of life. Multiple biophysiological factors contribute to differences in breast cancer between Latina and NLW women. For example, Latinas are at higher risk for the BRCA gene; furthermore, Latinas are at greater risk for estrogen- and progesterone-negative tumors, for which there are fewer treatment options, a higher chance of recurrence and lower odds of survival [4,5]. Moreover, Latinas are more likely to present with breast cancer that has metastasized at younger ages [6]. Comorbidities additionally influence breast cancer risk: Latinas are also at greater risk for obesity relative to NLW [7], which has been associated with increased breast cancer risk of various tumor types [8] and mortality [9]. Finally, disparities in behavioral, communication and psychosocial factors have been thought to contribute to an overall negative breast cancer involvement among Latinas, culminating with the observed difference in rates of breast cancer mortality between Latinas and NLWs [10,101]. The majority of interventions dedicated to improve the breast health of US-based Latinas have focused on the latter components. Consequently, this review focuses on these aspects of breast cancer. Figure 1 demonstrates the disparities in these aspects of cancer across multiple stages of the continuum that are described below.
Figure 1.
Outcomes of interest across the cancer continuum for interventions improving Latinas’ breast health.
Behavioral factors and timely adherence to recommended guidelines in particular, may serve as an important contributor to differences in breast cancer survival. In terms of prevention, diet and physical activity have been linked to breast cancer risk and differences exist between Latina and NLW women [11]. Timely adherence to recommended screening guidelines is an important disparity that has been thought to be integral to early-stage detection and survival. Specifically, there are higher rates of nonadherence to screening recommendations for clinical breast examinations (CBEs) and mammograms for Latinas relative to NLWs [12]. There are also lower rates of adherence to follow-up for abnormal screening, and greater times to diagnostic resolution [13,14], which have been linked to disparities in late-stage detection [15,105]. In addition, Latinas experience greater delays in initiation of treatment [16,17]. Disparities also exist among breast cancer survivors, in which their Latina breast cancer survivors have been documented to be less adherent to adjuvant therapy than their NLW counterparts.
Communication inequalities may also contribute to negative experiences across the breast cancer continuum and potentially breast cancer mortality. A growing body of research has documented communication inequalities across multiple stages. With regard to screening, providers appear to be less likely to recommend mammography screening to Latinas compared with NLWs [18]. Simultaneously, Latinas are less likely to comprehend recommended follow-up care, as well as being less likely to accurately report the follow-up care they have received after receipt of an abnormal mammogram result, potentially owing to linguistic barriers and health literacy levels [19–22]. During diagnosis and treatment, Latinas experience elevated levels of dissatisfaction concerning treatment decisions [23,24], and report more patient–physician communication problems, partially as a consequence of linguistic barriers and acculturation [25]. Inadequate interactions with providers may be related to subsequent reliance on family and social networks in the decision-making process for Latinas with regard to treatment [25]. Communication problems may be particularly relevant for less acculturated Latinas, who report more unmet information and care support needs than other women [26]. Such communication issues may contribute to inequalities in treatment options; for example, Latinas are more likely to experience ‘substandard’ treatment options [3,27–29]. Communication inequalities have also been documented to continue following treatment; for example, some research has indicated that Latinas have less information regarding reconstruction and express greater decisional dissatisfaction regarding breast reconstruction surgery after a mastectomy [30].
Finally, breast cancer disparities exist in relation to psychosocial experiences associated with cancer, including depression, anxiety and quality of life. Differences have been well documented with regard to later stages of the cancer continuum. For example, Latinas appear to experience particularly high levels of anxiety following receipt of an abnormal mammogram, which has been linked to diagnostic delays [19,31]. After a breast cancer diagnosis, Latinas experience poorer quality of life as patients and as breast cancer survivors [32]. In particular, studies have documented that lower acculturated Latinas express a lower quality of life and elevated levels of worry of recurrence [33,34].
In an effort to reduce cancer health disparities, intervention studies have been conducted at each stage of the cancer continuum. Many studies have been conducted with the aim of increasing timely adherence and to increase breast cancer screening in Latinas in particular. Other studies have examined discrepancies in follow-up to abnormal screening and treatment, while others attempted interventions to enhance initiation of treatment. Interventions have additionally sought to address communication inequalities and disparities in quality of life, as well as psychosocial experiences to a lesser extent. As a group, there are at least two modes of intervention, systemic or cultural, that have been used to improve breast cancer outcomes in Latinas.
Systemic barriers include the obstacles that exist in the US healthcare system, where healthcare is closely tied to insurance status. Latinas have lower rates of any kind of insurance (public or private) than NLWs [35]. Furthermore, many government-funded insurance programs pose additional problems for Latinas (e.g., being undocumented). A second systemic barrier is the thoroughness or quality of care that is available to Latinas. For example, Latinas who are monolingual Spanish speakers are less likely to navigate the complexities of the US healthcare system than English-speaking women [36,37]. As a result, they may not receive all the services to which they are entitled [38–40].
Cultural barriers may account for some of the individual reluctance to seek screening or treatment. These factors may underlie the heightened disadvantage unacculturated Latinas experience if diagnosed with breast cancer, in terms of communication difficulties and quality of life [30,33,34,41]. Indeed, a woman’s health needs and decisions may depend on her self-perception relative to the needs and interests of others (e.g., children and spouses) as a matter of cultural socialization. This is particularly relevant for Latina populations, in which there is a strong emphasis on warm, interpersonal relationships (e.g., personalismo and familismo), and norms may correspond to taking care of one’s family first and themselves second (e.g., marianismo [42]). Other cultural values and practices relevant to breast health prevention and treatment include views of fatalism [43–46], and the belief that a woman requires symptoms before seeing a physician [47]. All of these factors may contribute to timely adherence of recommended guidelines. For example, Latinas may be more likely to delay screening mammography since they prioritize healthcare for family members over themselves. Furthermore, cultural competence in care may also prevent Latinas from receiving adequate screening and treatment. This is likely to occur when providers view a woman as more able to understand and follow through on recommendations than is actually the case, resulting in communication barriers and misunderstanding concerning recommended guidelines [48]. Indeed, communication efforts to increase adherence may be best framed in the context of warmth between providers and patients, as well as the perceived benefits of decisions to a woman’s family and social network.
A number of interventions have attempted to address the various systemic and cultural factors that provide barriers for Latinas in breast cancer screening and treatment, with fewer focusing on cancer survivorship and mortality. These interventions appear to address cultural barriers to screening through the use of lay health educators (promotores) and community-wide activities [49–51]. Promotores are often used as bridges between communities and their health systems, given their in-depth understanding of cultural values, norms and behaviors. They may be better conduits to deliver and disseminate health knowledge. Activities held in communal areas, such as churches, health fairs and community centers, have have been shown to be effective in improving health promotion outcomes, but have often been used in tandem with peer and lay health educators.
By contrast, interventions addressing the systemic aspect of Latina breast cancer care have primarily focused on enhancing access and navigation of care [52]. For instance, several studies have addressed financial and transportation barriers, whereas others have employed patient navigators to assist with the coordination of care [28,53].
Existing reviews concerning Latina breast cancer interventions, however, have focused primarily on one stage of the continuum (i.e., mammography [49]), assessed one type of study design (i.e., randomized controlled trials [RCT]) [2] or have not focused specifically on Latinas [51,52]. Furthermore, no review to date has assessed the scope of interventions in terms of the nature of the intervention target (cultural vs systemic).
The purpose of this review is to gain a perspective on the entire scope of interventions that attempted to increase positive breast health outcomes among Latinas across the cancer continuum. Unlike a systematic review that may include meta-analysis, the authors examined and classified interventions of all types, from a RCT to one sample pre- and post-tests. Our goal in gathering such an all-encompassing list of studies was to develop an understanding of the type of breast cancer research that has been conducted in Latinas across the breast cancer continuum. This approach offers the opportunity to identify gaps, strengths and weaknesses in this body of literature. In addition to this goal, in this review, we sought to characterize the interventions by their emphases: cultural, systemic or both. Our work provides a springboard from which we may gain insight into heterogeneities in methodology and thereby better understand the implications of existing interventions to addressing cancer health disparities among US Latinas with breast cancer.
Methods
The authors conducted literature searches using Google Scholar, PubMed, Medline, Science-Direct and Web of Knowledge to identify breast cancer interventions for Latina women. In order to be considered for this review, articles describing interventions had to meet the following eligibility criteria: be published between 1990 and 2012; have a sample in which at least 25% of participants were identified as Latina; and the manuscript had to be written in English. Finally, in line with Figure 1, we considered intervention studies that addressed the following outcomes of interest for Latinas across one or multiple stages of the cancer continuum: timely adherence to recommended guidelines (screening practices [46,53–70], time to follow-up [15,71–74] and initiation of treatment [72]); physician–patient communication [75]; and psychosocial measures (depression/anxiety [76–78] and quality of life [30,41,79]). Exclusion criteria included interventions concerning breast cancer knowledge, intentions/expectations to obtain a mammogram and breast self-examination, as breast cancer knowledge and mammography intentions do not necessarily result in obtaining screening and breast self-examination has not been found to be an effective early detection strategy [80].
Within each stage of the cancer continuum, studies were categorized by four foci: study design, the type of intervention, who implemented the intervention and study outcomes. Studies were considered pre-/post-test design if all participants received the intervention and were tested before and after they received the intervention, and there was no control group. Occasionally, only a post-test was reported. Quasi-experimental designs included nonrandom assignment of individuals or sites/census tracts into conditions. Studies were labeled as RCTs if randomization occurred at the level of the individual and/or sites/census tracts. Interventions were further described in terms of their use of lay health workers (e.g., community health workers [CHWs], promotoras and peer navigators), community wide activities (e.g., health fairs and churches) and/or healthcare professionals (e.g., general practitioners and nurse navigators) to administer the intervention. Finally, we identified the focus of intervention on cultural and/or systemic targets. If interventions did not focus on either factor, we labeled them as ‘neither’.
Results
A total of 31 studies met the eligibility criteria for this review. Of these 31 studies, 30 provided percentages/counts and have been described here. In-depth detail regarding each of these studies are provided in Table 1. A total of 22 studies addressed solely Latina participant samples, approximately a third of the articles focused on Mexican/Mexican–American populations (n = 10; 32%) [46,53,56,58–60,63–65,81], and a similar proportion focused on populations residing on the west coast of the USA (n = 11; 35%) [53,54,57,60–63,66,67,73,77]. In terms of study design, we identified 13 RCTs, ten quasi-experimental studies and eight pre-/post-test studies. The majority of these studies focused on detection/screening practices (n = 19). Fewer studies were found on the topics of receipt of an abnormal screening (n = 5), treatment (n = 6) and survivorship (n = 1) (Table 1). No interventions that addressed metastatic breast cancer or end of life for Latinas were identified.
Table 1.
List of interventions and their outcomes by phase of the cancer continuum.
| Study (year) | Latina (%) |
Type of study design |
Type of intervention target |
Type of intervention implementation |
Outcomes | Ref. | |
|---|---|---|---|---|---|---|---|
| Control group/pre-test (%) | Intervention group/post-test (%) | ||||||
| Screening | |||||||
| Zapka et al. (1993) | 100 | Pre-/post-test | Systemic | Professionals | <50 years*†: 66 51–65 years*†: 78 >65 years†: 68 <50 years*‡: 13 51–65 years*‡: 19 >65 years*‡: 14 |
<50 years*†: 56 51–65 years*†: 56 >65 years*†: 52 <50 years*‡: 44 51–65 years*‡: 60 >65 years*‡: 56 |
[70] |
| Skaer et al. (1996) | 100 | RCT | Systemic | Professionals | 17.5*‡ | 87*‡ | [53] |
| Suarez et al. (1997) | 100 | Quasi-experimental | Cultural | Community-based activities | 17‡ | 19‡ | [46] |
| Fox et al. (1998) | 100 | Quasi-experimental | Cultural | Community-based activities/professionals | 1*‡ | 15*‡ | [57] |
| Mishra et al. (1998) | 100 | Quasi-experimental | Cultural | Professionals | 35† 11‡ |
43† 10‡ |
[61] |
| Navarro et al. (1998) | 100 | RCT | Cultural | Community health workers | 7*‡ | 21.4*‡ | [63] |
| Valdez et al. (2001) | 100 | RCT | Cultural | Professionals | 35‡ N/A | [67] | |
| Fernandez-Esquer et al. (2003) | 100 | Quasi-experimental | Cultural | Community-based activities/community health workers | 31‡ | 35‡ | [56] |
| Hansen et al. (2005) | 100 | Pre-/post-test | Cultural | Community health workers | 19‡ N/A | [58] | |
| Warren et al. (2006) | 100 | Pre-/post-test | Cultural/systemic | Community-based activities/community health workers/professionals | 53‡ N/A | [68] | |
| Thompson et al. (2006) | 55 | RCT | Cultural | Community-based activities | 40–49 years‡: 88.3 50+ years‡: 73.5 |
40–49 years‡: 80.6 50+ years‡: 73.35 |
[66] |
| Navarro et al. (2007) | 100 | Pre-/post-test | Cultural | Community health workers | 83.5*† 63.35‡ |
94.4*† 70.05‡ |
[62] |
| Sauaia et al. (2007) | 100 | Quasi-experimental§ | Cultural | Community health workers |
Promotora-based: 2*‡ Printed materials: 1*‡ |
[65] | |
| Fernandez et al. (2009) | 100 | RCT | Cultural | Community health workers | 29.9*‡ | 40.8*‡ | [55] |
| Livaudais et al. (2010) | 100 | Pre-/post-test | Cultural | Community health workers | 83*‡ | 91*‡ | [60] |
| Calderon et al. (2010) | 100 | Quasi-experimental§ | Cultural | Professionals | Discussion group: 41*‡ Discussion group plus media: 49*‡ |
Discussion group: 72*‡ Discussion group plus media: 58*‡ |
[54] |
| Nuno et al. (2011) | 100 | RCT | Cultural | Community health workers | 58‡ | 73*‡ | [64] |
| Larkey et al. (2012) | 100 | RCT§ | Cultural | Community health workers | 33.9‡ | 22.5‡ | [59] |
| White et al. (2012) | 100 | Pre-/post-test | Cultural | Community health workers | 62‡ N/A | [69] | |
| Abnormal screening result | |||||||
| Ell et al. (2006) | 85 | RCT | Systemic | Professionals | 77*¶ | 90*¶ | [73] |
| Ferrante et al. (2007) | 28 | RCT | Systemic | Professionals | 43 days*¶ | 25 days*¶ | [74] |
| Burhansstipanov et al. (2010) Dudley et al. (2012) |
45 46 |
Quasi-experimental Quasi-experimental |
Systemic Cultural/systemic |
Professionals Professionals/community health workers |
2*¶ 47.5*¶ |
54.9*¶ 62.6*¶ |
[71] [72] |
| Ramirez et al. (2013) | 100 | Quasi-experimental | Cultural/systemic | Professionals | 44.6 days*¶ | 32.5 days*¶ | [15] |
| Diagnosis/treatment | |||||||
| Moadel et al. (2007) | 31 | RCT | Neither cultural nor systemic | Professionals | 4.46*# | 1.26*# | [88] |
| Ell et al. (2008) | 87.9 | RCT | Neither cultural nor systemic | Professionals | 6-month follow-up: 41.74*†† 12-month follow-up: 43.46†† |
6-month follow-up: 44.49*†† 12-month follow-up: 45.65†† |
[77] |
| Sheppard et al. (2008) | 100 | Pre-/post-test | Cultural | Community health workers | 93‡‡ N/A | [75] | |
| Changrani et al. (2008) | 100 | RCT | Cultural | Community health workers | 64.1# 15.8†† |
67.3# 16.6†† |
[78] |
| Ell et al. (2011) | 93 | RCT | Neither cultural nor systemic | Professionals | 6-month follow-up: 50†† 12-month follow-up: 60*†† 18-month follow-up: 55*†† 24-month follow-up: 37*†† |
6-month follow-up: 61†† 12-month follow-up: 72*†† 18-month follow-up: 69*†† 24-month follow-up: 54*†† |
[76] |
| Dudley et al. (2012) | 46 | Quasi-experimental | cultural/systemic | Professionals/community health workers | 56.30*§§ | 80%*§§ | [72] |
| Survivorship | |||||||
| Hughes et al. (2008) | 100 | Pre-/post-test | Cultural | Professionals | Physical wellbeing: 47.41 ± 7.75#¶¶ Mental wellbeing: 47.33 ± 9.33¶¶ General stress: 23.39 ± 5.68*¶¶ |
Physical wellbeing: 49.40 ± 8.24#¶¶ Mental wellbeing: 50.06 ± 7.66¶¶ General stress: 20.88 ± 6.95*¶¶ |
[79] |
Measures related to clinical breast examination practices, including proportion of women receiving clinical breast examinations, as well as clinical breast examination rate per 100 eligible years.
Measures related to mammography practices, including percentage of women obtaining a mammogram at the end of the study, change in percentage of women reporting a mammogram and mammogram rates per 100 eligible years.
Study included two interventions.
Measures related to behaviors following receipt of an abnormal mammogram, including percentage of women who adhered to follow-up guidelines and days in diagnostic interval.
Quality-of-life measures.
Measures related to percentage change in depression/anxiety scores.
Measures related to improvement in and satisfaction with physician–patient communication measures.
Percentage of women who began treatment within 60 days of diagnosis.
Values represent mean ± standard deviation.
Statistically significant differences between control/intervention groups and pre-/post-test designs at p < 0.05.
N/A: No data collected at baseline or for the control group, as applicable; RCT: Randomized controlled trial.
Detection
Interventions addressed increases or decreases in CBE and mammography practices, although two-thirds focused solely on screening mammography. The authors found seven RCTs, six quasi-experimental and six pre-/post-test designs in the screening area.
The majority of screening interventions implemented cultural factors, as well as cultural values to promote screening CBE and mammography rates among Latinas. The primary mode of delivery was by CHWs or promotores who were members of the targeted communities. Specifically, CHW interventions included four RCTs, two quasi-experimental studies and five pre-/post-test study designs. Cultural norms and factors also were used in terms of community contexts. For example, messages about screening were introduced within local health activities, church-based programs and in local media outreach programs (e.g., print and TV). Notably, studies employing professionals or medical technologies (e.g., kiosks in healthcare settings) as modes of delivery were, in general, noted as bicultural and were linguistically matched to meet the needs of their local populations of women. Health professionals participating in screening interventions included nurses, general practitioners and health educators.
Fewer interventions addressed systemic barriers – that is, studies that attempted to decrease structural barriers, such as access to care. Two studies attempted to influence financial barriers (i.e., by providing vouchers), peer support in navigation of the US healthcare system (using patient navigators) and cultural competency training for healthcare providers. Other projects did not address access to care, but focused on logistical barriers to participation in interventions, for example, a few CHWs facilitated access to resources, such as transportation and child care needs.
Ten of the 19 screening interventions reported significant differences related to participation in interventions (e.g., postintervention or in the intervention compared with the control group). Of those that reported significant differences, approximately 44.4% (four out of nine) were RCTs, 22% (two out of nine) were quasi-experimental and 33% (three out of nine) were pre-/post-test study designs. Among the different modes of delivery, 50% of those that employed CHWs, 25% of those that employed community activities and 33% of those that used health professionals reported significant outcomes for increased screening behavior. Although two out of three systemic interventions had significant differences in reporting increased CBE and mammography rates, similar patterns were less discernible among interventions focusing primarily on cultural barriers. Only eight out of the 17 in that category reported significant intervention effects. It should be noted, however, that four interventions did not provide sufficient data to indicate intervention effects (e.g., no control group and no preintervention data).
Abnormal screening result
Of the five interventions dedicated to improving time to diagnostic resolution after a woman received notice of an abnormal screening result, three research efforts were quasi-experimental and two utilized RCT designs. These studies primarily incorporated professional patient navigation designs and measured the percentage of women who adhered to the follow-up recommendations, as well as days to diagnostic resolution.
In this type of intervention target, culture was addressed in terms of bilingualism – that is, the patient navigators spoke both Spanish and English. In addition, referrals for care were made to community services such a local clinics or hospitals. Despite this community referral, only one of these intervention activities appeared to be in partnership with a local community organization or venue; thus, it was not clear whether the patient navigation continued after the woman sought out a biopsy. The primary focus of abnormal screening results interventions addressed the systemic factors that prevented follow-up, such as repeated attempts to contact women with an abnormal screening test and referrals to programs that would pay for a repeat mammogram or a biopsy. A few also incorporated responses to specific barriers such as scheduling appointments.
The quasi-experimental and RCT studies in this category reported significant improvements in participants compared with pre-assessment or control groups. In two studies that looked at time to resolution of an abnormal test, both significantly reduced the time to follow-up, by 18 days [74] and by 12.1 days (increasing mammographic adherence), respectviely [15]. A third study saw time to resolution actually increase [72].
Diagnosis/treatment
The six interventions related to cancer diagnosis/treatment were varied in their outcomes of interest and addressed diverse needs of cancer patients, specifically, days to treatment initiation (n = 1), physician–patient communication (n = 1), depression (n = 3) and quality of life (n = 2). Approximately half of the projects relied on the use of professionals (n = 3) compared with the use of CHWs alone (n = 2) or in combination with a CHW (n = 1). Four out of the five interventions implemented interactions with professionals, including mental health specialists and professional patient navigators; the other intervention attempted to improve quality of life through physical activity/yoga.
Approximately 50% (n = 3) of the interventions addressed both systemic and cultural factors. Systemic factors (n = 1) were addressed through patient navigation to initiate treatment. Cultural factors were addressed through use of bilingual and bicultural CHWs (n = 3). In addition, individual factors influencing quality of life and depression were addressed through yoga instruction (n = 1) and use of mental health specialists (n = 2).
Four interventions indicated significant differences in time to treatment initiation and quality of life as a result of participation in the intervention; notably, one of the other two interventions did not provide information to indicate changes or effects of participation.
Survivorship
Only one intervention met the eligibility criteria for this review. The one published study used a 10-week physical activity intervention tailored to the physical abilities of each participant to reduce distress and improve quality of life. The physical activity prescriptions were developed for each participant by healthcare professionals and participants were responsible for following the prescription.
Cultural factors were addressed with the use of bilingual survey assessment of distress, quality of life and physical instruction materials. Significantly improved levels of distress were observed and, although not significant, a trend toward improved quality of life was observed. Physical activity was not significantly improved.
Discussion
In this review of breast cancer interventions conducted with Latinas, the authors identified 19 interventions that focused on screening, five that focused on addressing abnormal follow-ups, six that examined time to treatment or treatment outcomes and one that was concerned with survivorship. Of these, however, only 13 were RCTs. Of the remainder, ten were quasi-experimental and eight were pre-/post-test or post-test only. In many cases, attempts were made to make the interventions culturally relevant; such attempts ranged from ensuring the use of bilingual materials to the use of CHWs as promotores or patient navigators.
Overall, trials that had a systemic intervention target appeared to do better than those that focused primarily on cultural adaptation. The systemic factors assessed often emphasized increased access to care; therefore, it is not surprising that they are strong motivators of behavior change [78,82]. These included reducing the costs for Latinas to be screened by providing vouchers to defray expenses, as well as patient navigation that provided information and activities to support resolution of an abnormal screening test and initiate treatment.
Some interventions that included only cultural factors were also successful. The extent to which an intervention was culturally appropriate was not always clear and it may be that minimal efforts (e.g., bilingual materials only) might not be as effective as more in-depth cultural appropriateness. Future studies may wish to test these different circumstances. On the other hand, it has become part of the prevailing conceptual models to recognize the importance of making an intervention as culturally pertinent as possible to better engage the targeted population [83].
Importantly, there were some interventions that did not address cultural or systemic factors, but focused on individual-level factors involved in wellbeing along the cancer continuum. It is worthwhile to consider that these three interventions occurred during diagnosis and treatment and pertained to depression/anxiety and quality of life for cancer patients. Altogether, the existence of interventions for predominantly Latina samples that do not focus on cultural or systemic factors speak to the particularly challenging experiences faced by cancer patients in general.
The type of intervention implementation showed a trend over time, going from an emphasis on professional delivery of intervention to CHW delivery of intervention, especially with regard to early detection. In recent years, the use of lay health workers, or promotores in Latino culture, has become a well-established method of delivery of interventions [84]. Given the strong emphasis and value Latino culture places on interpersonal relationships, it is not surprising that many CHW-driven interventions also incorporated support for and participation from families and friends. Throughout later stages of treatment, interventions still relied heavily on the focus of professionals, which may be more helpful with regard to systemic barriers (e.g., patient navigators). Future interventions concerning these stages in the continuum may seek to incorporate a cultural perspective into designs regarding quality of life and mental health status, especially given the underutilization of existing interventions and programs for cancer patients and survivors by Latinas [85]. This literature has indicated the potential benefits of incorporating family support into support programs [85]. Simultaneously, for cancer patients, literature has indicated the importance of family in treatment decisions [42]; given this, future interventions to improve outcomes at the diagnosis/treatment stage may seek to include these cultural values and norms into interventions.
Interestingly, interventions with healthcare providers also paid attention to language barriers; only one of the healthcare provider interventions did not mention the importance of bilingual resources or the bicultural nature of healthcare providers or navigators. What was missing, however, was the extent to which information was written or presented in an understandable manner. This is especially important for Latinas who have fewer years of schooling or have difficulty with health literacy [86]. These issues were rarely addressed.
As is the case with all reviews of Latina activities, there is considerable heterogeneity in Latina populations. It is known that screening varies considerably by type of Latina; for example, Mexican Latinas have the lowest rates of screening mammography and CBEs compared with other groups of Latinas [12].
It is not surprising that the majority of the breast cancer intervention research identified in this review has been on attempts to increase early detection (screening). Screening is typically the first step in early detection as it identifies cancers at the earliest stage. However, given that Latinas are more likely to have advanced stage at diagnosis and lower 5-year survival rates, it is also necessary to focus on the intervening steps. It is clear that delay of following-up or ignoring an abnormal screening test is probably linked to stage of diagnosis. Furthermore, delay in seeking treatment for an abnormal finding will have implications for treatment and stage at diagnosis. Finally, survivorship data indicate that Latinas are less likely to survive for 5 years compared with their NLW counterparts, suggesting that efforts to address post-treatment sequelae are important [1,3,101].
In reviewing the outcomes, it should be noted that the studies presented varied by degree of scientific rigor, with RCTs having the highest degree of rigor, followed generally by quasi-experimental designs, and then followed further by the pre-/post-test designs (and the post-test only designs). A further caveat is that the units of randomization varied so that some research focused on individual women, while others focused on larger units of randomization, such as churches [57,65] and even communities [46,66]. For the purposes of this review, we desired a complete accounting of Latinas and breast cancer interventions; thus, the authors included all designs. Nevertheless, caution should be used in interpreting the results.
This review adds to the existing literature on Latinas and breast cancer. It is an area that will benefit from ongoing updates as Latina rates of breast cancer are not decreasing, and are increasing in some age groups (i.e., the 40–49-year-old group) [83]. Furthermore, as the proportion of Hispanics in the USA continue to increase, we may expect to see higher rates of breast cancer in this group owing to environmental exposures, ranging from chemicals to psychosocial exposures [87,106].
Conclusion & future perspective
In conclusion, this review demonstrates that in both rigorous randomized trials and quasi-experimental approaches, much has been achieved in increasing breast cancer screening, time to follow-up and time to treatment among Latinas. Furthermore, there is some evidence that survivorship intervention can improve Latina quality of life and mental status after treatment for the disease. Addressing all stages of the cancer continuum holds hope for Latinas who are diagnosed with breast cancer. Systemic interventions appear to be effective, whereas greater work remains to be completed for interventions targeting cultural factors. Future intervention projects that are warranted include comparison of different approaches to culturally pertinent interventions; implementation and evaluation of interventions dedicated to cultural factors in later stages of the continuum (e.g., diagnosis, treatment and survivorship), and specifically in relation to communication and psychosocial outcomes; and a greater number of RCTs to gain robust support for the benefit culturally pertinent interventions.
Learning objectives.
Upon completion of this activity, participants should be able to:
Analyze the epidemiology and impact of breast cancer among Latinas
Distinguish disparities in the detection and management of breast cancer faced by Latinas
Evaluate interventions to improve breast cancer detection among Latinas
Compare cultural and systematic interventions to improve breast cancer outcomes among Latinas
Executive summary.
Background
Although Latinas have a lower incidence of breast cancer than non-Latina whites, breast cancer is the major cancer killer of Latinas.
Despite the lower incidence of breast cancer, Latinas are more likely to die of the disease than their non-Latina white counterparts; reasons for this range from biological differences to screening and treatment differences.
Intervention studies to ameliorate the consequences of the disease are found along the cancer continuum – that is, Latinas are less likely to be screened, less likely to follow-up abnormal screening tests, less likely to be treated, and have poorer survivorship than non-Latina whites.
The purpose of this review is to gain a perspective on the entire scope of interventions along the breast cancer care continuum.
Methods
The authors examined diverse interventions on breast cancer among Latinas.
The authors were comprehensive in the approach and included randomized controlled trials, quasi-experimental and pre-/post-test interventions.
Results
A total of 31 studies met the criteria for inclusion.
The screening subgroup of interventions focused on cultural interventions and approximately half had significant results in increasing breast cancer screening by Latinas.
For abnormal screening, patient navigation was a primary focus that contributed to reduced time to follow-up.
In the diagnosis/treatment category, the interventions focused on healthcare professionals.
Only one study emphasized survivorship.
Discussion
Systematic interventions that reduced costs and other barriers to screening did better at increasing breast cancer screening than cultural interventions.
Over time, there was an increased focus on the use of promotores or community health workers in terms of responding to all parts of the breast cancer care continuum.
Many studies noted that language barriers are important to address when changing behavior of Latinas.
Future perspective
It is important to continue to make progress in Latinas and breast cancer incidence, mortality and survivorship.
There is increasing attention on Latina survivorship and it is likely that a focus on survivorship will develop.
It is especially important to examine interventions at all phases of the cancer continuum as Latinas ‘fall out’ at all stages of the continuum.
As the Affordable Care Act becomes implemented, more work will be devoted to systemic breast cancer interventions.
Footnotes
Financial & competing interests disclosure
CME Author
Charles P Vega, MD, Associate Professor and Residency Director, Department of Family Medicine, University of California, Irvine, CA, USA
Disclosure: Charles P Vega has disclosed no relevant financial relationships.
Authors & Credentials
Yamile Molina, PhD, Fred Hutchinson Cancer Research Center, 1100 Fairview Avenue N, M3-B232, PO Box 19024, Seattle, WA 98109, USA; and University of Illinois at Chicago, 700 S Halsted Street Number 2029 Chicago, IL 60607, USA
Disclosure: Yamile Molina has disclosed no relevant financial relationships.
Beti Thompson, PhD, Fred Hutchinson Cancer Research Center, 1100 Fairview Avenue N, M3-B232, PO Box 19024, Seattle, WA 98109, USA; and University of Washington, School of Public Health, Box 357230, Seattle, WA 98195, USA
Disclosure: Beti Thompson has disclosed no relevant financial relationships.
Noah Espinoza, MPH, Fred Hutchinson Cancer Research Center, 1100 Fairview Avenue N, M3-B232, PO Box 19024, Seattle, WA 98109, USA
Disclosure: Noah Espinoza has disclosed no relevant financial relationships.
Rachel Ceballos, PhD, Fred Hutchinson Cancer Research Center, 1100 Fairview Avenue N, M3-B232, PO Box 19024, Seattle, WA 98109, USA; and University of Washington, School of Public Health, PO Box 357230, Seattle, WA 98195, USA
Disclosure: Rachel Ceballos has disclosed no relevant financial relationships.
Editor
Elisa Manzotti, Publisher, Future Science Group
Disclosure: Elisa Manzotti has disclosed no relevant financial relationships.
References
- 1.DeSantis C, Siegel R, Bandi P, Jemal A. Breast cancer statistics, 2011. CA Cancer J. Clin. 2011;61(6):408–418. doi: 10.3322/caac.20134. [DOI] [PubMed] [Google Scholar]
- 2.John EM, Phipps AI, Davis A, Koo J. Migration history, acculturation, and breast cancer risk in hispanic women. Cancer Epidemiol. Biomarkers Prevent. 2005;14(12):2905–2913. doi: 10.1158/1055-9965.EPI-05-0483. [DOI] [PubMed] [Google Scholar]
- 3.Li CI, Malone KE, Daling JR. Differences in breast cancer stage, treatment, and survival by race and ethnicity. Arch. Intern. Med. 2003;163(1):49–56. doi: 10.1001/archinte.163.1.49. [DOI] [PubMed] [Google Scholar]
- 4.Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V. Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype. Cancer. 2007;109(9):1721–1728. doi: 10.1002/cncr.22618. [DOI] [PubMed] [Google Scholar]
- 5.Lara-Medina F, Pérez-Sánchez V, Saavedra-Pérez D, et al. Triple-negative breast cancer in Hispanic patients. Cancer. 2011;117(16):3658–3669. doi: 10.1002/cncr.25961. [DOI] [PubMed] [Google Scholar]
- 6.Wray CJ, Phatak UR, Robinson EK, et al. The effect of age on race-related breast cancer survival disparities. Anna. Surg. Oncol. 2013 doi: 10.1245/s10434-013-2913-x. (Epub ahead of print). [DOI] [PubMed] [Google Scholar]
- 7.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among us adults, 1999–2010. JAMA. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 8.White KK, Park SY, Kolonel LN, Henderson BE, Wilkens LR. Body size and breast cancer risk: the multiethnic cohort. Int. J. Cancer. 2012;131(5):E705–E716. doi: 10.1002/ijc.27373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N. Engl. J. Med. 2003;348(17):1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 10.Jemal A, Clegg LX, Ward E, et al. Annual report to the nation on the status of cancer, 1975–2001, with a special feature regarding survival. Cancer. 2004;101(1):3–27. doi: 10.1002/cncr.20288. [DOI] [PubMed] [Google Scholar]
- 11.Kushi LH, Byers T, Doyle C, et al. American Cancer Society guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J. Clin. 2006;56(5):254–281. doi: 10.3322/canjclin.56.5.254. [DOI] [PubMed] [Google Scholar]
- 12.Miranda PY, Tarraf W, González P, Johnson-Jennings M, González HM. Breast cancer screening trends in the United States and ethnicity. Cancer Epidemiol. Biomarkers Prev. 2012;21(2):351–357. doi: 10.1158/1055-9965.EPI-11-0873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elmore JG, Nakano CY, Linden HM, Reisch LM, Ayanian JZ, Larson EB. Racial inequities in the timing of breast cancer detection, diagnosis, and initiation of treatment. Med. Care. 2005;43(2):141–148. doi: 10.1097/00005650-200502000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Press R, Carrasquillo O, Sciacca RR, Giardina EG. Racial/ethnic disparities in time to follow-up after an abnormal mammogram. J. Women’s Health. 2008;17(6):923–930. doi: 10.1089/jwh.2007.0402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ramirez AG, Pérez-Stable EJ, Penedo FJ, et al. Navigating Latinas with breast screen abnormalities to diagnosis: the Six Cities Study. Cancer. 2013;119(7):1298–1305. doi: 10.1002/cncr.27912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bickell NA, Wang JJ, Oluwole S, et al. Missed opportunities: racial disparities in adjuvant breast cancer treatment. J. Clin. Oncol. 2006;24(9):1357–1362. doi: 10.1200/JCO.2005.04.5799. [DOI] [PubMed] [Google Scholar]
- 17.Fedewa SA, Ward EM, Stewart AK, Edge SB. Delays in adjuvant chemotherapy treatment among patients with breast cancer are more likely in African American and Hispanic populations: a national cohort study 2004–2006. J. Clin. Oncol. 2010;28(27):4135–4141. doi: 10.1200/JCO.2009.27.2427. [DOI] [PubMed] [Google Scholar]
- 18.Blackman DJ, Masi CM. Racial and ethnic disparities in breast cancer mortality: are we doing enough to address the root causes? J. Clin. Oncol. 2006;24(14):2170–2178. doi: 10.1200/JCO.2005.05.4734. [DOI] [PubMed] [Google Scholar]
- 19.Allen JD, Shelton RC, Harden E, Goldman RE. Follow-up of abnormal screening mammograms among low-income ethnically diverse women: findings from a qualitative study. Patient Educ. Couns. 2008;72(2):283–292. doi: 10.1016/j.pec.2008.03.024. [DOI] [PubMed] [Google Scholar]
- 20.Karliner LS, Ma L, Hofmann M, Kerlikowske K. Language barriers, location of care, and delays in follow-up of abnormal mammograms. Med. Care. 2012;50(2):171–178. doi: 10.1097/MLR.0b013e31822dcf2d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mojica CM, Bastani R. Receipt of diagnostic tests for breast cancer: validity of self-reports among low-income, mostly Latina, indigent women. Eval. Health Prof. 2010;33(4):437–451. doi: 10.1177/0163278710367802. [DOI] [PubMed] [Google Scholar]
- 22.Mojica CM, Bastani R, Ponce NA, Boscardin WJ. Latinas with abnormal breast findings: patient predictors of timely diagnostic resolution. J. Womens Health. 2007;16(10):1468–1477. doi: 10.1089/jwh.2006.0324. [DOI] [PubMed] [Google Scholar]
- 23.Campesino M, Koithan M, Ruiz E, et al. Surgical treatment differences among Latina and African American breast cancer survivors. Oncol. Nurs. Forum. 2012;39(4):E324–E331. doi: 10.1188/12.ONF.E324-E331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hawley ST, Janz NK, Hamilton A, et al. Latina patient perspectives about informed treatment decision making for breast cancer. Patient Educ. Couns. 2008;73(2):363–370. doi: 10.1016/j.pec.2008.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maly RC, Umezawa Y, Ratliff CT, Leake B. Racial/ethnic group differences in treatment decision-making and treatment received among older breast carcinoma patients. Cancer. 2006;106(4):957–965. doi: 10.1002/cncr.21680. [DOI] [PubMed] [Google Scholar]
- 26.Janz NK, Mujahid MS, Hawley ST, Griggs JJ, Hamilton AS, Katz SJ. Racial/ethnic differences in adequacy of information and support for women with breast cancer. Cancer. 2008;113(5):1058–1067. doi: 10.1002/cncr.23660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Freedman RA, Virgo KS, He Y, et al. The association of race/ethnicity, insurance status, and socioeconomic factors with breast cancer care. Cancer. 2011;117(1):180–189. doi: 10.1002/cncr.25542. [DOI] [PubMed] [Google Scholar]
- 28.Freeman H. Patient navigation: a community based strategy to reduce cancer disparities. J. Urban Health. 2006;83(2):139–141. doi: 10.1007/s11524-006-9030-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Livaudais J, Hershman D, Habel L, et al. Racial/ethnic differences in initiation of adjuvant hormonal therapy among women with hormone receptor-positive breast cancer. Breast Cancer Res. Treat. 2012;131(2):607–617. doi: 10.1007/s10549-011-1762-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alderman A, Hawley S, Janz N, et al. Racial and ethnic disparities in the use of postmastectomy breast reconstruction: results from a population-based study. J. Clin. Oncol. 2009;27(32):5325–5330. doi: 10.1200/JCO.2009.22.2455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ashing-Giwa KT, Gonzalez P, Lim JW, et al. Diagnostic and therapeutic delays among a multiethnic sample of breast and cervical cancer survivors. Cancer. 2010;116(13):3195–3204. doi: 10.1002/cncr.25060. [DOI] [PubMed] [Google Scholar]
- 32.Yanez B, Thompson E, Stanton A. Quality of life among Latina breast cancer patients: a systematic review of the literature. J. Cancer Surv. 2011;5(2):191–207. doi: 10.1007/s11764-011-0171-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Janz N, Mujahid M, Hawley S, et al. Racial/ethnic differences in quality of life after diagnosis of breast cancer. J. Cancer Surv. 2009;3(4):212–222. doi: 10.1007/s11764-009-0097-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Janz NK, Hawley ST, Mujahid MS, et al. Correlates of worry about recurrence in a multiethnic population-based sample of women with breast cancer. Cancer. 2011;117(9):1827–1836. doi: 10.1002/cncr.25740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.DeNavas-Walt C, Proctor BD, Smith JC. Income, poverty, and health insurance coverage in the United States: 2009. In: Harrington C, Estes CL, editors. Health Policy: Crisis and Reform. MA, USA: Jones and Bartlett Publishers; 2012. pp. 267–280. [Google Scholar]
- 36.Timmins CL. The impact of language barriers on the health care of Latinos in the United States: a review of the literature and guidelines for practice. J. Midwifery Womens Health. 2002;47(2):80–96. doi: 10.1016/s1526-9523(02)00218-0. [DOI] [PubMed] [Google Scholar]
- 37.Marcus E, Koru-Sengul T, Miao F, Yepes M, Sanders L. How do breast imaging centers communicate results to women with limited english proficiency and other barriers to care? J. Immigr. Minor. Health. 2013 doi: 10.1007/s10903-012-9771-7. (Epub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Diaz E, Prigerson H, Desai R, Rosenheck R. Perceived needs and service use of Spanish speaking monolingual patients followed at a Hispanic clinic. Commun. Ment. Health J. 2001;37(4):335–346. doi: 10.1023/a:1017552608517. [DOI] [PubMed] [Google Scholar]
- 39.Gresenz CR, Rogowski J, Escarce JJ. Community demographics and access to health care among U.S. Hispanics. Health Serv. Res. 2009;44(5 Pt 1):1542–1562. doi: 10.1111/j.1475-6773.2009.00997.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Perez-Stable EJ. Language access and Latino health care disparities. Med. Care. 2007;45(11):1009–1011. doi: 10.1097/MLR.0b013e31815b9440. [DOI] [PubMed] [Google Scholar]
- 41.Janz N, Mujahid M, Hawley S, Griggs J, Hamilton A, Katz S. Racial/ethnic differences in adequacy of information and support for women with breast cancer. Cancer. 2008;113(5):1058–1067. doi: 10.1002/cncr.23660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Arredondo P, Santiago-Rivera AL, Gallardo-Cooper M. Counseling Latinos and la familia: a practical guide. In: Arredondo P, Santiago-Rivera AL, Gallardo-Cooper M, editors. Multicultural Aspects of Counseling Series. CA, USA: Sage Publications, Incorporated; 2001. pp. 49–51. [Google Scholar]
- 43.Flórez K, Aguirre A, Viladrich A, Céspedes A, De La Cruz A, Abraído-Lanza A. Fatalism or destiny? A qualitative study and interpretative framework on dominican women’s breast cancer beliefs. J. Immigr. Minor. Health. 2009;11(4):291–301. doi: 10.1007/s10903-008-9118-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Laws MB, Mayo S. The Latina breast cancer control study, year one: factors predicting screening mammography utilization by urban Latina women in Massachusetts. J. Commun. Health. 1998;23(4):251–267. doi: 10.1023/a:1018776704683. [DOI] [PubMed] [Google Scholar]
- 45.McMullin JM, Alba ID, Chávez LR, Hubbell FA. Influence of beliefs about cervical cancer etiology on pap smear use among Latina immigrants. Ethnic Health. 2005;10(1):3–18. doi: 10.1080/1355785052000323001. [DOI] [PubMed] [Google Scholar]
- 46.Suarez L, Roche RA, Nichols D, Simpson DM. Knowledge, behavior, and fears concerning breast and cervical cancer among older low-income Mexican–American women. Am. J. Prev. Med. 1997;13(2):137–142. [PubMed] [Google Scholar]
- 47.Ogedegbe G, Cassells AN, Robinson CM, et al. Perceptions of barriers and facilitators of cancer early detection among low-income minority women in community health centers. J. Natl Med. Assoc. 2005;97(2):162. [PMC free article] [PubMed] [Google Scholar]
- 48.Davis SW, Diaz-Mendez M, Garcia MT. Barriers to seeking cancer information among Spanish-speaking cancer survivors. J. Cancer Educ. 2009;24(3):167–171. doi: 10.1080/08858190902873053. [DOI] [PubMed] [Google Scholar]
- 49.Corcoran J, Dattalo P, Crowley M. Interventions to increase mammography rates among U.S. Latinas: a systematic review. J. Women’s Health. 2010;19(7):1281–1288. doi: 10.1089/jwh.2009.1621. [DOI] [PubMed] [Google Scholar]
- 50.Nelson A, Lewy R, Dovydaitis T, Ricardo F, Kugel C. Promotores as researchers: expanding the promotor role in communitybased research. Health Promot. Pract. 2011;12(5):681–688. doi: 10.1177/1524839910380849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.O’Malley AS, Gonzalez RM, Sheppard VB, Huerta E, Mandelblatt J. Primary care cancer control interventions including Latinos: a review. Am. J. Prev. Med. 2003;25(3):264–271. doi: 10.1016/s0749-3797(03)00190-9. [DOI] [PubMed] [Google Scholar]
- 52.Legler J, Meissner HI, Coyne C, Breen N, Chollette V, Rimer BK. The effectiveness of interventions to promote mammography among women with historically lower rates of screening. Cancer Epidemiol. Biomarkers Prev. 2002;11(1):59–71. [PubMed] [Google Scholar]
- 53.Skaer TL, Robison LM, Sclar DA, Harding GH. Cancer-screening determinants among Hispanic women using migrant health clinics. J. Health Care Poor Underserved. 1996;7(4):338–354. doi: 10.1353/hpu.2010.0465. [DOI] [PubMed] [Google Scholar]
- 54.Calderon JL, Bazargan M, Sangasubana N, Hays RD, Hardigan P, Baker RS. A comparison of two educational methods on immigrant Latinas breast cancer knowledge and screening behaviors. J. Health Care Poor Underserved. 2010;21(Suppl. 3):S76–S90. doi: 10.1353/hpu.0.0364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fernandez ME, Gonzales A, Tortolero-Luna G, et al. Effectiveness of cultivando la salud: a breast and cervical cancer screening promotion program for low-income Hispanic women. Am. J. Public Health. 2009;99(5):936–943. doi: 10.2105/AJPH.2008.136713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fernandez-Esquer ME, Espinoza P, Torres I, Ramirez AG, McAlister AL. A su salud: a quasi-experimental study among Mexican American women. Am. J. Public Health Behav. 2003;27(5):536–545. doi: 10.5993/ajhb.27.5.5. [DOI] [PubMed] [Google Scholar]
- 57.Fox SA, Stein JA, Gonzalez RE, Farrenkopf M, Dellinger A. A trial to increase mammography utilization among Los Angeles Hispanic women. J. Health Care Poor Underserved. 1998;9(3):309–321. doi: 10.1353/hpu.2010.0218. [DOI] [PubMed] [Google Scholar]
- 58.Hansen LK, Feigl P, Modiano MR, et al. An educational program to increase cervical and breast cancer screening in Hispanic women: a Southwest Oncology Group study. Cancer Nurs. 2005;28(1):47–53. doi: 10.1097/00002820-200501000-00007. [DOI] [PubMed] [Google Scholar]
- 59.Larkey LK, Herman PM, Roe DJ, et al. A cancer screening intervention for underserved Latina women by lay educators. J. Women’s Health. 2012;21(5):557–566. doi: 10.1089/jwh.2011.3087. [DOI] [PubMed] [Google Scholar]
- 60.Livaudais JC, Coronado GD, Espinoza N, Islas I, Ibarra G, Thompson B. Educating Hispanic women about breast cancer prevention: evaluation of a home-based promotora-led intervention. J. Women’s Health. 2010;19(11):2049–2056. doi: 10.1089/jwh.2009.1733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mishra SI, Chavez LR, Magana JR, Nava P, Burciaga Valdez R, Hubbell FA. Improving breast cancer control among Latinas: evaluation of a theory-based educational program. Health Educ. Behav. 1998;25(5):653–670. doi: 10.1177/109019819802500511. [DOI] [PubMed] [Google Scholar]
- 62.Navarro AM, Raman R, McNicholas LJ, Loza O. Diffusion of cancer education information through a Latino community health advisor program. Prev. Med. 2007;45(2–3):135–138. doi: 10.1016/j.ypmed.2007.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Navarro AM, Senn KL, McNicholas LJ, Kaplan RM, Roppe B, Campo MC. Por La Vida model intervention enhances use of cancer screening tests among Latinas. Am. J. Prev. Med. 1998;15(1):32–41. doi: 10.1016/s0749-3797(98)00023-3. [DOI] [PubMed] [Google Scholar]
- 64.Nuno T, Martinez ME, Harris R, Garcia F. A promotora-administered group education intervention to promote breast and cervical cancer screening in a rural community along the U.S.–Mexico border: a randomized controlled trial. Cancer Causes Control. 2011;22(3):367–374. doi: 10.1007/s10552-010-9705-4. [DOI] [PubMed] [Google Scholar]
- 65.Sauaia A, Min SJ, Lack D, et al. Church-based breast cancer screening education: impact of two approaches on Latinas enrolled in public and private health insurance plans. Prev. Chronic Dis. 2007;4(4):A99. [PMC free article] [PubMed] [Google Scholar]
- 66.Thompson B, Coronado G, Chen L, Islas I. Celebremos la salud! A community randomized trial of cancer prevention (United States) Cancer Causes Control. 2006;17(5):733–746. doi: 10.1007/s10552-006-0006-x. [DOI] [PubMed] [Google Scholar]
- 67.Valdez A, Banerjee K, Fernandez M, Ackerson L. Impact of a multimedia breast cancer education intervention on use of mammography by low-income Latinas. J. Cancer Educ. 2001;16(4):221–224. doi: 10.1080/08858190109528777. [DOI] [PubMed] [Google Scholar]
- 68.Warren AG, Londoño GE, Wessel LA, Warren RD. Breaking down barriers to breast and cervical cancer screening: a university-based prevention program for Latinas. J. Health Care Poor Underserved. 2006;17(3):512–521. doi: 10.1353/hpu.2006.0114. [DOI] [PubMed] [Google Scholar]
- 69.White K, Garces IC, Bandura L, McGuire AA, Scarinci IC. Design and evaluation of a theory-based, culturally relevant outreach model for breast and cervical cancer screening for Latina immigrants. Ethnic Dis. 2012;22(3):274–280. [PMC free article] [PubMed] [Google Scholar]
- 70.Zapka JG, Harris DR, Hosmer D, Costanza ME, Mas E, Barth R. Effect of a community health center intervention on breast cancer screening among Hispanic American women. Health Serv. Res. 1993;28(2):223–235. [PMC free article] [PubMed] [Google Scholar]
- 71.Burhansstipanov L, Dignan MB, Schumacher A, Krebs LU, Alfonsi G, Apodaca CC. Breast screening navigator programs within three settings that assist underserved women. J. Cancer Educ. 2010;25(2):247–252. doi: 10.1007/s13187-010-0071-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dudley DJ, Drake J, Quinlan J, et al. Beneficial effects of a combined navigator/promotora approach for Hispanic women diagnosed with breast abnormalities. Cancer Epidemiol. Biomarkers Prev. 2012;21(10):1639–1644. doi: 10.1158/1055-9965.EPI-12-0538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ell K, Vourlekis B, Lee PJ, Xie B. Patient navigation and case management following an abnormal mammogram: a randomized clinical trial. Prev. Med. 2006;44(1):26–33. doi: 10.1016/j.ypmed.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 74.Ferrante JM, Chen PH, Kim S. The effect of patient navigation on time to diagnosis, anxiety, and satisfaction in urban minority women with abnormal mammograms: a randomized controlled trial. J. Urban Health. 2007;85(1):114–124. doi: 10.1007/s11524-007-9228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sheppard VB, Figueiredo M, Canar J, et al. Latina a Latina: developing a breast cancer decision support intervention. Psychooncology. 2008;17(4):383–391. doi: 10.1002/pon.1239. [DOI] [PubMed] [Google Scholar]
- 76.Ell K, Xie B, Kapetanovic S, et al. One-year follow-up of collaborative depression care for low-income, predominantly Hispanic patients with cancer. Psychiatr. Serv. 2011;62(2):162–170. doi: 10.1176/ps.62.2.pss6202_0162. [DOI] [PubMed] [Google Scholar]
- 77.Ell K, Xie B, Quon B, Quinn DI, Dwight-Johnson M, Lee PJ. Randomized controlled trial of collaborative care management of depression among low-income patients with cancer. J. Clin. Oncol. 2008;26(27):4488–4496. doi: 10.1200/JCO.2008.16.6371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Changrani J, Lieberman M, Golant M, Rios P, Damman J, Gany F. Online cancer support groups: experiences with underserved immigrant Latinas. Primary Psychiatry. 2008;15(10):55–62. [Google Scholar]
- 79.Hughes DC, Leung P, Naus MJ. Using single-system analyses to assess the effectiveness of an exercise intervention on quality of life for Hispanic breast cancer survivors: a pilot study. Soc. Work Health Care. 2008;47(1):73–91. doi: 10.1080/00981380801970871. [DOI] [PubMed] [Google Scholar]
- 80.Schueler KM, Chu PW, Smith-Bindman R. Factors associated with mammography utilization: a systematic quantitative review of the literature. J. Women’s Health. 2008;17(9):1477–1498. doi: 10.1089/jwh.2007.0603. [DOI] [PubMed] [Google Scholar]
- 81.Lopez VA, Castro FG. Participation and program outcomes in a church-based cancer prevention program for Hispanic women. J. Commun. Health. 2006;31(4):343–362. doi: 10.1007/s10900-006-9016-6. [DOI] [PubMed] [Google Scholar]
- 82.Klassen AC, Smith ALM, Meissner HI, Zabora J, Curbow B, Mandelblatt J. If we gave away mammograms, who would get them? A neighborhood evaluation of a no-cost breast cancer screening program. Prev. Med. 2002;34(1):13–21. doi: 10.1006/pmed.2001.0956. [DOI] [PubMed] [Google Scholar]
- 83.Brach C, Fraserirector I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Med. Care Res. Rev. 2000;57(Suppl. 4):S181–S217. doi: 10.1177/1077558700057001S09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rhodes SD, Foley KL, Zometa CS, Bloom FR. Lay health advisor interventions among Hispanics/Latinos: a qualitative systematic review. Am. J. Prev. Med. 2007;33(5):418–427. doi: 10.1016/j.amepre.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 85.Nápoles-Springer A, Ortíz C, O’Brien H, Díaz-Méndez M, Pérez-Stable E. Use of cancer support groups among Latina breast cancer survivors. J. Cancer Surviv. 2007;1(3):193–204. doi: 10.1007/s11764-007-0029-7. [DOI] [PubMed] [Google Scholar]
- 86.Bennett IM, Chen J, Soroui JS, White S. The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. Ann. Fam. Med. 2009;7(3):204–211. doi: 10.1370/afm.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Macon M, Fenton S. Endocrine disruptors and the breast: early life effects and later life disease. J. Mammary Gland Biol. Neoplasia. 2013;18(1):43–61. doi: 10.1007/s10911-013-9275-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Moadel AB, Shah C, Wylie-Rosett J, et al. Randomized controlled trial of yoga among a multiethnic sample of breast cancer patients: effects on quality of life. J. Clin. Oncol. 2007;25(28):4387–4395. doi: 10.1200/JCO.2006.06.6027. [DOI] [PubMed] [Google Scholar]
Websites
- 101.American Cancer Society. Cancer facts and figures for Hispanics/Latinos: 2009–2011 PDF brochure. [Accessed 7 February 2012]; www.cancer.org/Research/Cancer Facts Figures/Cancer Facts Figures for Hispanics Latinos/ff-hispanics-latinos-2009–2011-pdf.
- 102.American Cancer Society. Breast cancer facts and figures: 2011–2012 – PDF Brochure. [Accessed 5 February 2012]; www.cancer.org/Research/Cancer Facts Figures/Breast Cancer Facts Figures/ACSPC-030975.
- 103.Altekruse SF, Kosary CL, Krapcho M, et al. SEER cancer statistics review, 1975–2007. [Accessed 15 February 2013];2010 http://seer.cancer.gov/csr/1975_2010.
- 104.American Cancer Society. Cancer facts and figures for African–Americans 2011–2012. [Accessed 27 February 2012]; www.cancer.org/acs/groups/content/@epidemiology surveilance/ documents/document/acspc-027765.pdf.
- 105.Barry M, Gemignani ML. Follow-up for women with abnormal mammograms. [Accessed 14 June 2013];Journal Watch Specialties. http://womens-health.jwatch.org/cgi/content/full/2011/414/1.
- 106.Williams DR. Distinguished visiting scholars. [Accessed 7 February 2013];Identifying gaps in breast cancer research: addressing disparities and the roles of the physical and social environment. www.cbcrp.org/sri/reports/identifyinggaps.