Abstract
In humans, infection with Hymenolepis diminuta is usually uncommon but has been reported from various areas of the world. Parasitization rates ranging between 0.001% and 5.5% have been reported according to different surveys. We report a rare case of H. diminuta infection in a 10-year-old female from the rural area of Kendrapada district of Odisha. The patient came to our pediatrics outpatient department with the chief complain of intermittent abdominal pain, anal pruritus and nocturnal restlessness. She responded well to praziquantel therapy.
Keywords: Hymenolepis diminuta, praziquantel, rat tapeworm
INTRODUCTION
Hymenolepis diminuta is a rat tapeworm that occurs throughout the world in temperate to tropical conditions of poor sanitation.[1] Basically, it is a parasite of rats and infections in human beings are reported on rare occasions. In humans, infections caused by H. nana are much more common than those caused by H. diminuta. Parasitization rates according to different surveys range between 0.001% and 5.5%.[2] Its principal definitive hosts are rodents. Ingestion of infected arthropod containing cysticercoids infects human beings accidentally. Adult worms are found in the small intestine of human beings, and it passes eggs in the stool. Infections in human beings are usually indicated by noting the presence of eggs in the stool.[3] Cases have been reported from the western and southern parts of India, but there is no case reported from this part of India. To the best of our knowledge, this is the first documented case from the eastern part of India.
CASE REPORT
A 10-year-old female belonging to a rural area of Kendrapada district of Odisha came to our pediatrics outpatient department with a chief complaint of intermittent abdominal pain, anal pruritus and nocturnal restlessness since the last 2-3 weeks. On physical examination, there were no positive clinical findings. No abnormal readings were found in the blood and urine analyses. Her height was 130 cm and weight was 29 kg. Examination of the stool samples revealed spherical eggs 70 µm in diameter, yellow-colored, thick-shelled eggs that contained six central hooklets but no polar filaments [Figure 1]. These were identified as H. diminuta eggs and were differentiated from H. nana eggs, which have a similar appearance but are smaller in size and have two evident polar thickenings, from each of which four to eight polar filaments arise.[4] Further confirmation was done by examination of another stool sample by the concentration method. Again, the same findings were noted. The patient was successfully treated with praziquantel (10 mg/kg body weight) for 7 days.
Figure 1.
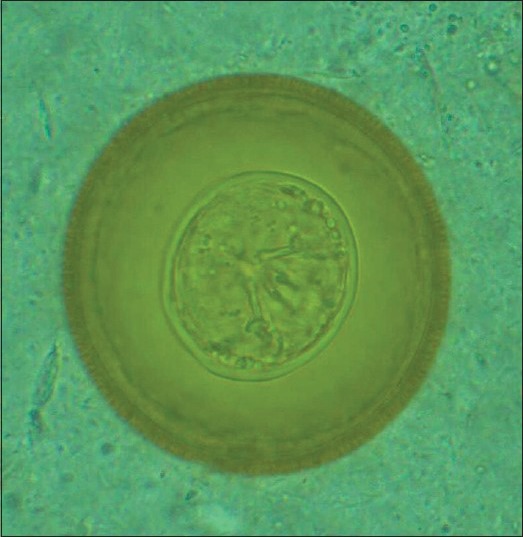
Showing the egg of Hymenolepis diminuta containing six central hooklets (×100)
DISCUSSION
H. diminuta is a rodent parasite for which the arthropod acts as intermediate host. Rodents become infected by ingesting the arthropod containing cysticercoid larvae. Human beings, usually children, can be accidentally infected by the ingestion of infected arthropod.[4] In humans, infections with H. nana are much more common than those by H. diminuta, as its transmission does not require any intermediate host. It can be spread directly from person to person. Although H. diminuta infection in humans is uncommon, few hundred cases (till now <500) have been reported worldwide.[2,5,6,7,8] In India also during a survey done by Chandler,[9] 20 cases of H. diminuta were found after examination of more than 8,000 stool samples. Apart from this, few other isolated cases were also reported from India.[3,10]
The human form of H. diminuta infection is often asymptomatic, but abdominal pain, irritability, itching and eosinophilia have been reported. Our patient also had similar findings, but eosinophilia was not evident. Praziquantel is the drug of choice for the treatment of H. diminuta infection.[2] Our patient was treated with praziquantel (10 mg/kg body weight) for 7 days. After completion of therapy, her stool was examined for the presence of H. diminuta eggs on three occasions (on the 8th, 9th and 10th days), and it was found to be negative. We suggest that in order to improve our knowledge of the epidemiology, mode of transmission and treatment protocol of this rare infection, any case of H. diminuta infection should be reported and analyzed.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.McMillan B, Kelly A, Walker JC. Prevalence of Hymenolepis diminuta infection in man in the New Guinea highlands. Trop Geogr Med. 1971;23:390–2. [PubMed] [Google Scholar]
- 2.Tena D, Pérez Simón M, Gimeno M, Pérez Pomata MT, Illescas S, Amondarain I, et al. Human infection with Hymenolepis diminuta: Case report from Spain. J Clin Microbiol. 1998;36:2375–6. doi: 10.1128/jcm.36.8.2375-2376.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Watwe S, Dardi CK. Hymenolepis diminuta in a child from rural area. Indian J Path Microbiol. 2008;51:149–50. doi: 10.4103/0377-4929.40431. [DOI] [PubMed] [Google Scholar]
- 4.Marangi M, Zechini B, Fileti A, Quaranta G, Aceti A. Hymenolepis diminuta infection in a child living in the urban area of Rome, Italy. J Clin Microbiol. 2003;41:3994–5. doi: 10.1128/JCM.41.8.3994-3995.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Foresi C. Data on the epidemiology of hymenolepiasis in Italy. I. Arch Ital Sci Med Trop Parassitol. 1967;48:251–62. [PubMed] [Google Scholar]
- 6.Cohen IP. A case report of Hymenolepis diminuta infection in a child in St James Parish, Jamaica. J La State Med Soc. 1989;141:23–4. [PubMed] [Google Scholar]
- 7.Tesjaroen S, Chareonlarp K, Yoolek A, Mai-iam W, Lertlaituan P. Fifth and sixth discoveries of Hymenolepis diminuta infections in Thai people. J Med Assoc Thai. 1987;70:49–50. [PubMed] [Google Scholar]
- 8.Stafford E, Sudomo M, Marsi S, Brown RJ. Human parasitosis in Bali, Indonesia. Southeast Asian J Trop Med Public Health. 1980;11:319–23. [PubMed] [Google Scholar]
- 9.Chandler AC. The distribution of H. diminuta infection in India and discussion of its epidemiological significance. Indian J Med Res. 1927;14:973–94. [Google Scholar]
- 10.Sane SY, Irani S, Jain N, Shah KN. Hymenolepis diminuta a rare zoonotic infection report of a case. Indian J Pediatr. 1984;51:743–5. doi: 10.1007/BF02776395. [DOI] [PubMed] [Google Scholar]


