Abstract
Background:
There are sporadic reports on detection of extended-spectrum beta-lactamases (ESBL) producers from Karnataka; hence, this is a first multicentric study across Karnataka state to determine the prevalence of ESBL production among clinical isolates of Escherichia coli and Klebsiella pneumoniae.
Aims and objectives:
To determine the prevalence of ESBL producing clinical isolates of E. coli and K. pneumoniae from five geographically distributed centers across Karnataka, to study the susceptibility of ESBL producing isolates to other beta-lactam and beta-lactam-beta-lactamase inhibitors and to demonstrate transferability of plasmids coding for ESBL phenotype.
Materials and Methods:
Two hundred isolates of E. coli and K. pneumoniae each were collected from each of the five centers (Bellary, Dharwad, Davangere, Kolar and Mangalore). They were screened for resistance to screening agents (ceftazidime, cefotaxime, ceftriaxone, aztreonam) and positive isolates were confirmed for ESBL production by test described by Clinical and Laboratory Standards Institute. Co-production of ESBL and AmpC beta-lactamase was identified by using amino-phenylboronic acid disk method. Susceptibility of ESBL producers to beta-lactam antibiotics and beta-lactamase inhibitors was performed. Transferability of plasmids was performed by conjugation experiment.
Results:
Overall prevalence of ESBL production among E. coli and K. pneumoniae across five centers of the state was 57.5%. ESBL production was found to be 61.4% among E. coli and 46.2% among K. pneumoniae. ESBL production was significantly more among E. coli than K. pneumoniae. Significant variations in distribution of ESBL across the state was observed among E. coli isolates, but not among K. pneumoniae isolates. All ESBL producers demonstrated minimum inhibitory concentration levels ≥2 μg/ml towards cefotaxime, ceftazidime and ceftriaxone.
Conclusion:
Overall prevalence of ESBL production among clinical isolates of E. coli and K. pneumoniae across Karnataka state was high. The prevalence of ESBL production was significantly higher with E. coli than K. pneumoniae isolates. Higher rates of resistance to ceftriaxone and cefotaxime than to ceftazidime suggests the possibility of presence of CTX-M type ESBLs. Of all the beta-lactam/beta-lactamase inhibitor combinations tested, cefepime-tazobactam demonstrated highest in-vitro activity against ESBL producers. There was no statistical difference in the transferability of plasmids among E. coli and K. pneumoniae.
Keywords: Beta-lactamase, beta-lactamase inhibitor, extended-spectrum beta-lactamases
INTRODUCTION
Treatment of infections caused by Gram-negative bacilli is becoming increasingly difficult because of antibiotic resistance. Various mechanisms such as enzymatic inactivation of antibiotics, altered target sites, decreased porin permeability and active efflux pumps are known to produce drug resistance. One such mechanism is the production of extended-spectrum beta-lactamase (ESBL) enzymes by these bacteria. ESBLs are known to hydrolyze all penicillins, early cephalosporins, oxyimino-cephalosporins and monobactams, but they lack hydrolytic activity on cephamycins and carbapenems. ESBLs are inhibited by beta-lactamase inhibitors such as clavulanic acid, tazobactam and sulbactam.[1] Treatment failures after instituting beta-lactam antibiotic therapy for infections caused by ESBL producing Gram-negative bacilli have been reported.[2] ESBL producing bacteria have been isolated from healthy subjects, health care workers, food of animal origin, animals, hospital environment, vegetation and sewage.[3,4,5] As the genes coding for ESBLs are mainly plasmid borne, ESBLs have rapidly disseminated among the bacterial communities, within and across the species. ESBL producing Escherichia coli and Klebsiella pneumoniae have known to cause outbreaks in hospital settings.[6]
Although there are a few reports of ESBL producing bacteria from Karnataka, data from multiple centers across the state is currently lacking. Hence, this is the first multi-centric study that was conducted with the following objectives: (a) To determine the prevalence of ESBL producing clinical isolates of E. coli and K. pneumoniae from five geographically distributed centers across Karnataka (b) to study the susceptibility of ESBL producing isolates to other beta-lactam and beta-lactam-beta-lactamase inhibitors and (c) to demonstrate transferability of plasmids coding for ESBL phenotype.
MATERIALS AND METHODS
Collection of specimen
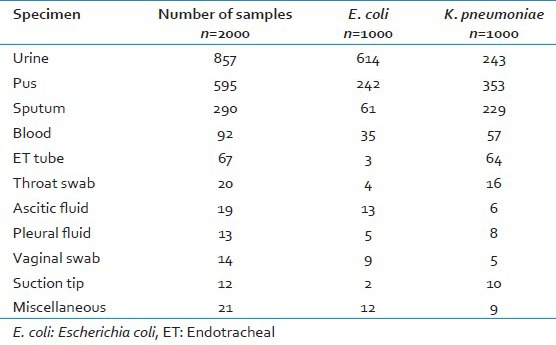
Between May 2009 and September 2012, 2000 clinical isolates comprising of 1000 isolates each of E. coli and K. pneumoniae were collected from hospitals attached to Medical Colleges at Davangere (DVG), Kolar (KOL), Mangalore (MNG), Dharwad (DWD) and Bellary (BEL). 200 isolates each of E. coli and K. pneumoniae from each center were randomly collected over a period of 3 years and 3 months. The samples yielding these isolates were as follows: Urine-857, pus-595, sputum-290, blood-92, endotracheal tube-67, throat swab-20, ascitic fluid-19, vaginal swab-14, pleural fluid-13, suction tip-12, rectal swab-8, cervical swab-6, gastric lavage-3 and two each from cerebrospinal fluid and bronchoalveolar lavage samples. Isolation of E. coli and K. pneumoniae from these samples is shown in Table 1. Ethical clearance was obtained from the Institutional Ethical Committee.
Table 1.
Isolation of E. coli and K. pneumoniae from various clinical samples
Screening for resistance to oxyimino-cephalosporins
Isolates were screened for resistance to three oxyimino-cephalosporins: Ceftazidime (30 μg), cefotaxime (30 μg), ceftriaxone (30 μg) and the monobactam: Aztreonam (30 μg) by disk diffusion test. Isolates that displayed resistance to one or more of these were considered positive for screening test.
Phenotypic detection of ESBL production
Presence of ESBL among isolates positive on screening was confirmed by using both ceftazidime/ceftazidime-clavulanic acid (CAZ/CAC) (30/10 μg) and ceftotaxime/cefotaxime-clavulanic acid (CTX/CEC) (30/10 μg) disks according to phenotypic confirmatory test (PCT). An increase in zone diameter by ≥5 mm around disks with cephalosporin and clavulanic acid versus disks with cephalosporin alone was interpreted as positive as per Clinical and Laboratory Standards Institute (CLSI) 2010 guidelines.[7]
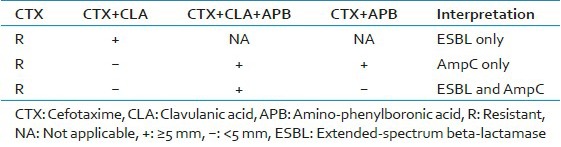
Detection of ESBL in the presence of AmpC
Isolates that were positive upon screening but negative by PCT were tested for co-production of ESBL and AmpC enzymes by using amino-phenylboronic acid (APB) disk method as described earlier.[8] Briefly, 400 μg/ml APB acid was added to disks containing cefotaxime/clavulanic acid (30/10 μg) and cefotaxime (30 μg). Plain disks with APB acid were used as controls. Interpretation of the test was made as shown in Table 2.
Table 2.
Interpretation of amino-phenylboronic acid disk method for co-production of ESBL and AmpC beta-lactamase
Determination of Minimum inhibitory concentration values
The MIC values for cefoxitin, ceftazidime, cefotaxime and ceftriaxone against isolates identified as ESBL producers were obtained by agar dilution method using a dilution range of 128-0.25 μg/ml on Mueller Hinton agar. K. pneumoniae ATCC 700603 and E. coli ATCC 25922 were used as controls.
Additional susceptibility testing
ESBL producing isolates were further tested for susceptibility to cefepime (30 μg), cefepime-tazobactam (30/10 μg), cefepime-clavulanic acid (30/10 μg) and imipenem (10 μg) by disk diffusion method.
Transfer of resistance by conjugation
Isolates phenotypically identified as ESBL producers were tested for transferability of the plasmid by conjugation (mating) experiment as described earlier.[9] Test strains and the recipient strain were grown overnight separately in Luria Bertani broth at 37°C. Cultures of test strain and recipient strains were mixed in a separate tube at 1:10 ratio and incubated at 37°C overnight. A volume of 50 μl of the mixture was placed on Mueller Hinton agar with 2 μg/ml cefotaxime and 200 μg/ml sodium azide and incubated at 37°C for up to 48 h. Growth on this medium was interpreted as successful conjugation and such colonies were confirmed for ESBL production by PCT. The recipient strain (E. coli J53 AzR) was kindly provided by George Jacoby.
Statistical methods applied
Using an approximate prevalence rate of 50%, confidence interval of 95%, precision of 5% and using the formula n = (Z1-α)2(P (1 − P)/D2), a sample size of 385 was calculated. It was rounded off to 400 samples per center including 200 of E. coli and 200 of K. pneumoniae. The power of study was set at 80%. Categorical data was analyzed by Chi-square test whereas z test for proportion was used to determine the relationship between groups. P ≤ 0.05 was considered to be statistically significant.
Culture media, antibiotic disks, APB acid, dimethylsulphoxide, ATCC strains were procured from Hi-Media laboratories, Mumbai, India. Pure antibiotic powders for MIC determination were procured from Sigma-Aldrich, Bangalore, India.
RESULTS
Screening test
A total of 1276 isolates were considered as screen positive. Of the 1,000 E. coli isolates, 740 (74%) were found resistant to one or more the screening agents. Among them 738 (99.7%) were resistant to all the four screening agents. Of the 1,000 K. pneumoniae isolates, 536 (53.6%) were found resistant to one or more the screening agents. Among them 529 (98.7%) were resistant to all the four screening agents.
Phenotypic detection of ESBL
Of the 1276 isolates that were positive in the screening test, ESBL production was confirmed by PCT in 1076 (84.3%) isolates, which included 614 (61.4%) E. coli and 462 (46.2%) K. pneumoniae, indicating that the prevalence of ESBL production is 61.4% in E. coli (ESBL-EC) and 46.2% in K. pneumoniae (ESBL-KP) across Karnataka. Co-production of ESBL and AmpC beta-lactamase were detected in 58 (2.9%) isolates, which included 56 (5.6%) E. coli and 2 (0.2%) K. pneumoniae. AmpC production was noted in 35 (3.5%) isolates of E. coli and 9 (0.9%) isolates of K. pneumoniae. Neither AmpC nor ESBL production could be accounted for cephalosporin resistance in the remaining 35 isolates of E. coli and 63 isolates of K. pneumoniae.
Distribution of ESBL producers across the state
The distribution of ESBL producing E. coli and K. pneumoniae from various centers is as shown in Table 3 and Figure 1. The prevalence of ESBL-EC was noticed to be highest from Bellary center (83.5%) followed by Mangalore and Davangere (63.5% each) and lesser from Dharwad (49.5%) and Kolar (47%) centers. Differences in the prevalence of ESBL-EC across Karnataka was significant (P < 0.001); on the other hand, the prevalence of ESBL-KP across Karnataka was not significant (P = 0.2).
Table 3.
Distribution of ESBL producing EC and KP from various centers
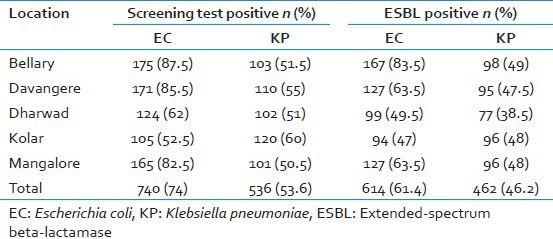
Figure 1.
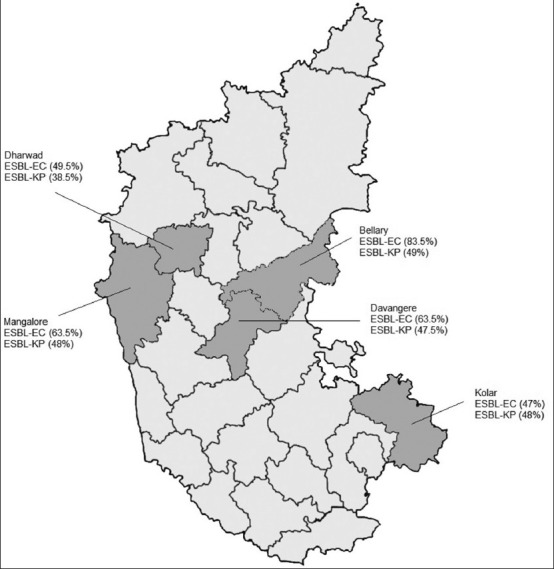
Distribution of extended-spectrum beta-lactamase producers from five centers across Karnataka
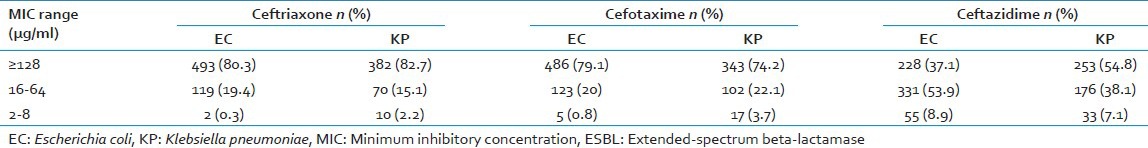
MIC values of ESBL producers
MIC values of ESBL-EC and ESBL-KP isolates to ceftazidime, cefotaxime and ceftriaxone are displayed in Table 4. All the ESBL producers had MIC levels of ≥2 μg/ml to each of the third generation cephalosporin tested, thus confirming resistance. At the concentration of ≥128 μg/ml of ceftriaxone and cefotaxime, 493 (80.3%) and 486 (79.1%) isolates of ESBL-EC respectively were resistant; however at a similar concentration of ceftazidime only 228 (37.1%) isolates of ESBL-EC showed resistance. These differences in resistance pattern at the concentration ≥128 μg/ml were statistically significant (P < 0.001). This observation was also true with ESBL-KP. At the concentration of ≥128 μg/ml of ceftriaxone and cefotaxime, 382 (82.7%) and 343 (74.2%) isolates of ESBL-KP respectively were resistant; however at a similar concentration of ceftazidime only 253 (54.8%) of ESBL-KP showed resistance.
Table 4.
MIC values of ESBL producers to ceftazidime, cefotaxime and ceftriaxone
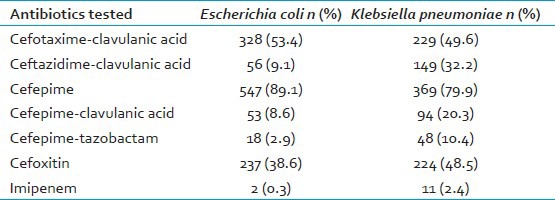
Resistance pattern to other beta-lactams, beta-lactam-beta-lactamase inhibitors
Table 5 presents resistance pattern of the ESBL producing isolates to certain beta-lactam antibiotics other than those used for testing and beta-lactam/beta-lactamase inhibitor combinations. Resistance to the combination of cefotaxime and clavulanic acid was almost the same in case of ESBL-EC (53.4%) and ESBL-KP (49.6%); however, 32.2% ESBL-KP and 9.1% of ESBL-EC were resistant to the combination of ceftazidime and clavulanic acid. This difference was found to be significant (P < 0.001). It was observed that 89.1% of ESBL-EC and 79.9% of ESBL-KP were resistant to cefepime. This resistance was reduced considerably (from 89.1% to 2.9%) when cefepime was combined with tazobactam or clavulanic acid. Of all the combinations of beta-lactam/beta-lactamase inhibitor tested, cefepime-tazobactam had the least resistance. Cefoxitin resistance was observed both in ESBL-EC (38.6%) and ESBL-KP (48.5%). Only 2 (0.3%) ESBL-EC and 11 (2.4%) ESBL-KP were found resistant to imipenem.
Table 5.
Antibiotic resistance to other betalactam antibiotics and beta-lactamase inhibitors
Plasmid transfer by conjugation
Plasmid mediated resistance transfer was successfully demonstrated in 362/614 (59%) isolates of ESBL-EC and 249/462 (53.9%) isolates of ESBL-KP.
DISCUSSION
In a multi-centric study conducted as part of India SENTRY surveillance, the prevalence of ESBL production was reported to be 84%.[10] Here we found that 61.4% of E. coli and 46.2% of K. pneumoniae isolates collected across five centers of Karnataka were ESBL producers. The prevalence of ESBL-EC was significantly more (P < 0.001) than ESBL-KP.
ESBL production among Enterobacteriaceae members vary widely from region to region and sometimes within the state. We found that the prevalence of ESBL producing bacteria varied across Karnataka with respect to E. coli but not with K. pneumoniae. In the case of E. coli it was highest at Bellary (87.5%) and lowest at Kolar (52.5%). However, it was almost the same with respect to K. pneumoniae expect from Dharwad. These differences could be due to varied degree exposure of these organisms to beta-lactam antibiotics or due to varied transferability of plasmids in nature among them. However, our plasmid transmission studies conducted in the laboratory did not reveal a significant difference (P = 0.09) in the transferability of plasmid in ESBL-EC and ESBL-KP.
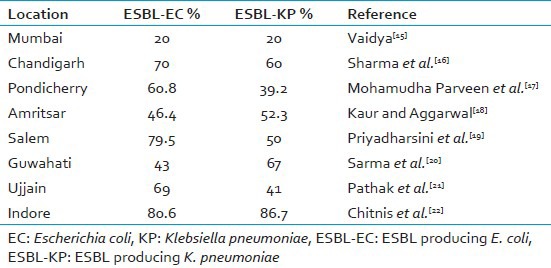
Earlier studies from Karnataka found that the detection rates of ESBL-EC has varied from 23.6% (Raichur) to 86.7% (Shimoga). The detection rates of ESBL-KP from different studies across Karnataka has been reported to vary from 9.6% (Bangalore) to 81.8% (Mangalore).[11,12,13,14] Reports of ESBL detection among clinical isolates of E. coli range between 20% and 80.6% and those among K. pneumoniae ranges between 20% and 86.7% across the country; these findings are summarized in Table 6. The variation in the detection rates within and across the states could be due to the differences in the methodology used in these studies. We made our study stringent by using four beta-lactam antibiotics for screening and two beta-lactam and beta-lactamase inhibitor combination disks for confirmation of ESBL as per the CLSI guidelines, thus, bringing uniformity in testing.
Table 6.
Reports of ESBL production in EC and KP across the country
Co-production of AmpC beta-lactamase and ESBL among the isolates in this study has been only minimal (2.9%), but was observed to be higher among E. coli (5.6%) isolates than K. pneumoniae (0.2%) isolates. Our findings contrasts with that reported from Bangalore and Manipal. The study from Manipal reported a co-production rate of 58.5% among E. coli; a study from Bangalore reported a co-production rate of 30.1% for E. coli and 30.3% for Klebsiella sps.[23,24] These variations could be due to differences in the methodologies adopted.
In the present study reported, none of the ESBL producing bacteria had MIC of <2 μg/ml towards ceftazidime, cefotaxime or ceftriaxone. The ESBL producers exhibited significantly higher MIC levels (≥128 μg/ml) to cefotaxime and ceftriaxone than to ceftazidime. This difference suggests the presence of CTX-M type ESBLs that hydrolyse cefotaxime and ceftriaxone more efficiently than ceftazidime.[25]
Cefoxitin, which is a cephamycin is not hydrolyzed by ESBLs, but in our study we have observed resistance in both E. coli (38.5%) and K. pneumoniae (48.5%) isolates. Earlier studies have suggested that cefoxitin resistance could be due to altered membrane porins.[26] Cefepime resistance among the ESBL producers was also found to be high among both E. coli (89.1%) and K. pneumoniae (79.9%). Similarly, high resistance to the tune 97.4% was observed among ESBL-EC isolates from Bangalore.[23] Resistance to cefepime could be attributed to the high prevalence of CTX-M type ESBLs in these isolates, some of which are capable of hydrolyzing cefepime.[27] Cefepime-tazobactam combination was found to be more effective than cefepime-clavulanic acid combination against ESBL producing isolates.
Although all ESBL producing isolates were resistant to ceftazidime and cefotaxime in the screening test, addition of clavulanic acid did not render all the isolates susceptible to the cephalosporins. Ceftazidime-clavulanic acid combination had better inhibitory effect on ESBL-EC and ESBL-KP than cefotaxime-clavulanic acid. This difference in susceptibilities also highlights the possible presence of CTX-M type enzymes in these isolates. ESBLs have no hydrolytic activity on imipenem, but resistance was noted in two E. coli and 11 K. pneumoniae isolates. Presence of other beta-lactamases or alterations in porin channels might account for this resistance.[28] As the co-resistance to imipenem in ESBL producers is low, it continues to be effective in treating diseases caused by them.
Presence of ESBL genes on plasmids was demonstrated successfully by mating experiment in 56.8% isolates. E. coli isolates were found to readily transfer the plasmids than K. pneumoniae, although this observation was statistically not significant. Presence of bla gene on non-transmissible plasmids can account for failure in conjugation experiments. Recently, a study was conducted at Mumbai, which evaluated horizontal transfer rates of ESBL carrying plasmids by conjugation. The author reported transfer of resistance under laboratory and environmental conditions at a frequency of 3-4 × 10−5, which is high.[15] The promiscuity of the isolates in transferring the plasmid containing bla gene does not seem to be very high in our study.
CONCLUSION
Prevalence of ESBL production among E. coli was 61.4% and 46.2% among K. pneumoniae across Karnataka state. The prevalence of ESBL production was significantly higher with E. coli than K. pneumoniae isolates. There was significant variation in the distribution of ESBL-EC across Karnataka, but not so with ESBL-KP. Isolates that co-produced ESBL and AmpC enzymes were marginally low in both the species. All ESBL producers had MIC levels ≥2 μg/ml toward cefotaxime, ceftriaxone and ceftazidime. High level resistance was more apparent with cefotaxime and ceftriaxone than with ceftazidime. Susceptibility pattern indicates possible presence of CTX-M type ESBLs amongst ESBL producers. Cefepime-tazobactam has highest in-vitro activity against ESBL producers than cefotaxime-clavulanic acid, ceftazidime-clavulanic acid or cefepime-clavulanic acid. This study, which has shown conjugation rate of 58.8% indicates that conjugation is perhaps only moderate but not rampant.
Strength and weakness of the study
This is the first study to undertake a multi-centric study on prevalence of ESBL-EC and ESBL-KP across Karnataka, which has also demonstrated unusually high levels of resistance to cefoxitin and cefepime. A state-wide surveillance not only reveals the prevalence and the extent of distribution of ESBLs among E. coli and K. pneumoniae but also helps in monitoring degree of resistances to beta-lactam antibiotics and beta-lactam inhibitor combinations. Although other combinations of beta-lactams and beta-lactamase inhibitors were tested, other antimicrobials like aminoglycosides, fluoroquinolones were not tested since it was beyond the scope of this study. Genotypic study on beta-lactamase gene using polymerase chain reaction would have given better picture on the prevalent ESBL type. Even though, samples were from five geographically distinct location, the results cannot be applied to the entire state.
ACKNOWLEDGMENTS
Dr. RD Kulkarni, professor, Department of Microbiology, SDMCMSH, Dharwad, Dr. Beena PM, professor, Department of Microbiology, SDUMC, Kolar and Dr. George Jacoby, Lahey Clinic, Massachusetts, USA.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Giske CG, Sundsfjord AS, Kahlmeter G, Woodford N, Nordmann P, Paterson DL, et al. Redefining extended-spectrum beta-lactamases: Balancing science and clinical need. J Antimicrob Chemother. 2009;63:1–4. doi: 10.1093/jac/dkn444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Karas JA, Pillay DG, Muckart D, Sturm AW. Treatment failure due to extended spectrum beta-lactamase. J Antimicrob Chemother. 1996;37:203–4. doi: 10.1093/jac/37.1.203. [DOI] [PubMed] [Google Scholar]
- 3.Calbo E, Freixas N, Xercavins M, Riera M, Nicolás C, Monistrol O, et al. Foodborne nosocomial outbreak of SHV1 and CTX-M-15-producing Klebsiella pneumoniae: Epidemiology and control. Clin Infect Dis. 2011;52:743–9. doi: 10.1093/cid/ciq238. [DOI] [PubMed] [Google Scholar]
- 4.Doi Y, Paterson DL, Egea P, Pascual A, López-Cerero L, Navarro MD, et al. Extended-spectrum and CMY-type beta-lactamase-producing Escherichia coli in clinical samples and retail meat from Pittsburgh, USA and Seville, Spain. Clin Microbiol Infect. 2010;16:33–8. doi: 10.1111/j.1469-0691.2009.03001.x. [DOI] [PubMed] [Google Scholar]
- 5.Shaheen BW, Nayak R, Foley SL, Kweon O, Deck J, Park M, et al. Molecular characterization of resistance to extended-spectrum cephalosporins in clinical Escherichia coli isolates from companion animals in the United States. Antimicrob Agents Chemother. 2011;55:5666–75. doi: 10.1128/AAC.00656-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Webster DP, Young BC, Morton R, Collyer D, Batchelor B, Turton JF, et al. Impact of a clonal outbreak of extended-spectrum β-lactamase-producing Klebsiella pneumoniae in the development and evolution of bloodstream infections by Klebsiella pneumoniae and Escherichia coli: An 11 year experience in Oxfordshire, UK. J Antimicrob Chemother. 2011;66:2126–35. doi: 10.1093/jac/dkr246. [DOI] [PubMed] [Google Scholar]
- 7.Clinical and Laboratory Standards Institute. Vol. 30. Wayne, PA: CLSI; 2010. Performance Standards for Antimicrobial Susceptibility Testing: Twenty-First Informational Supplement M100-S20; p. 46. [Google Scholar]
- 8.Robberts FJ, Kohner PC, Patel R. Unreliable extended-spectrum beta-lactamase detection in the presence of plasmid-mediated AmpC in Escherichia coli clinical isolates. J Clin Microbiol. 2009;47:358–61. doi: 10.1128/JCM.01687-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park YJ, Park SY, Oh EJ, Park JJ, Lee KY, Woo GJ, et al. Occurrence of extended-spectrum beta-lactamases among chromosomal AmpC-producing Enterobacter cloacae, Citrobacter freundii, and Serratia marcescens in Korea and investigation of screening criteria. Diagn Microbiol Infect Dis. 2005;51:265–9. doi: 10.1016/j.diagmicrobio.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Manoharan A, Premalatha K, Chatterjee S, Mathai D SARI Study Group. Correlation of TEM, SHV and CTX-M extended-spectrum beta lactamases among Enterobacteriaceae with their in vitro antimicrobial susceptibility. Indian J Med Microbiol. 2011;29:161–4. doi: 10.4103/0255-0857.81799. [DOI] [PubMed] [Google Scholar]
- 11.Harwalkar A, Sataraddi J, Gupta S, Yoganand R, Rao A, Srinivasa H. The detection of ESBL-producing Escherichia coli in patients with symptomatic urinary tract infections using different diffusion methods in a rural setting. J Infect Public Health. 2013;6:108–14. doi: 10.1016/j.jiph.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 12.Bhat PV, Sarkar A. Emergence and control of multidrug resistant organisms in small cities in India: A wake up call. Indian J Med Sci. 2011;65:337–43. [PubMed] [Google Scholar]
- 13.Eshwarappa M, Dosegowda R, Aprameya IV, Khan MW, Kumar PS, Kempegowda P. Clinico-microbiological profile of urinary tract infection in south India. Indian J Nephrol. 2011;21:30–6. doi: 10.4103/0971-4065.75226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kamath S, Mallaya S, Shenoy S. Nosocomial infections in neonatal intensive care units: Profile, risk factor assessment and antibiogram. Indian J Pediatr. 2010;77:37–9. doi: 10.1007/s12098-010-0005-5. [DOI] [PubMed] [Google Scholar]
- 15.Vaidya VK. Horizontal transfer of antimicrobial resistance by extended-spectrum β lactamase-producing enterobacteriaceae. J Lab Physicians. 2011;3:37–42. doi: 10.4103/0974-2727.78563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sharma J, Sharma M, Ray P. Detection of TEM and SHV genes in Escherichia coli and Klebsiella pneumoniae isolates in a tertiary care hospital from India. Indian J Med Res. 2010;132:332–6. [PubMed] [Google Scholar]
- 17.Mohamudha Parveen R, Manivannan S, Harish BN, Parija SC. Study of CTX-M type of extended spectrum β-lactamase among nosocomial isolates of Escherichia coli and Klebsiella pneumoniae in South India. Indian J Microbiol. 2012;52:35–40. doi: 10.1007/s12088-011-0140-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaur M, Aggarwal A. Occurrence of the CTX-M, SHV and the TEM genes among the extended spectrum β-lactamase producing isolates of enterobacteriaceae in a Tertiary Care Hospital of North India. J Clin Diagn Res. 2013;7:642–5. doi: 10.7860/JCDR/2013/5081.2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Priyadharsini RI, Kavitha A, Rajan R, Mathavi S, Rajesh KR. Prevalence of bla (CTX M) extended spectrum beta lactamase gene in enterobacteriaceae from critical care patients. J Lab Physicians. 2011;3:80–3. doi: 10.4103/0974-2727.86838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sarma JB, Bhattacharya PK, Kalita D, Rajbangshi M. Multidrug-resistant Enterobacteriaceae including metallo-β-lactamase producers are predominant pathogens of healthcare-associated infections in an Indian teaching hospital. Indian J Med Microbiol. 2011;29:22–7. doi: 10.4103/0255-0857.76519. [DOI] [PubMed] [Google Scholar]
- 21.Pathak A, Marothi Y, Kekre V, Mahadik K, Macaden R, Lundborg CS. High prevalence of extended-spectrum β-lactamase-producing pathogens: Results of a surveillance study in two hospitals in Ujjain, India. Infect Drug Resist. 2012;5:65–73. doi: 10.2147/IDR.S30043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chitnis S, Katara G, Hemvani N, Chitnis DS. Augmentation in zone of inhibition of cefoperazone/cefoperazone+sulbactum compares well with the clinical laboratory standard institute standard extended spectrum beta-lactamase detection method as well as the polymerase chain reaction method. Curr Drug Saf. 2011;6:155–8. doi: 10.2174/157488611797579294. [DOI] [PubMed] [Google Scholar]
- 23.Rudresh SM, Nagarathnamma T. Extended spectrum β-lactamase producing Enterobacteriaceae and antibiotic co-resistance. Indian J Med Res. 2011;133:116–8. [PMC free article] [PubMed] [Google Scholar]
- 24.Shobha KL, Ramachandra L, Rao G, Majumder S, Rao SP. Extended spectrum beta-lactamases (ESBL) in gram negative bacilli at a Tertiary Care Hospital. J Clin Diagn Res. 2009;3:1307–12. [Google Scholar]
- 25.Tzouvelekis LS, Tzelepi E, Tassios PT, Legakis NJ. CTX-M-type beta-lactamases: An emerging group of extended-spectrum enzymes. Int J Antimicrob Agents. 2000;14:137–42. doi: 10.1016/s0924-8579(99)00165-x. [DOI] [PubMed] [Google Scholar]
- 26.Ananthan S, Subha A. Cefoxitin resistance mediated by loss of a porin in clinical strains of Klebsiella pneumoniae and Escherichia coli. Indian J Med Microbiol. 2005;23:20–3. doi: 10.4103/0255-0857.13867. [DOI] [PubMed] [Google Scholar]
- 27.Yu WL, Pfaller MA, Winokur PL, Jones RN. Cefepime MIC as a predictor of the extended-spectrum beta-lactamase type in Klebsiella pneumoniae, Taiwan. Emerg Infect Dis. 2002;8:522–4. doi: 10.3201/eid0805.010346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oteo J, Delgado-Iribarren A, Vega D, Bautista V, Rodríguez MC, Velasco M, et al. Emergence of imipenem resistance in clinical Escherichia coli during therapy. Int J Antimicrob Agents. 2008;32:534–7. doi: 10.1016/j.ijantimicag.2008.06.012. [DOI] [PubMed] [Google Scholar]


