Abstract
Background:
Periorbital hyperpigmentation (POH) is one of the most commonly encountered conditions in routine dermatology practice. There are only few published studies about its prevalence, classification, and pathogenesis but none showing its association with habits, and other medical conditions in Indian patients.
Aims:
To determine prevalence and type of POH, common causative factors, and its association with personal habits and other disorders within various age and sex groups.
Materials and Methods:
Two hundred patients attending the dermatology OPD were included in study and were subjected to detailed history, careful clinical and Wood's lamp examination, eyelid stretch test and laboratory investigations. Clinical photographs of all patients were taken.
Results:
POH was most prevalent in 16-25 years age group (47.50%) and in females (81%) of which majority were housewives (45.50%). Commonest form of POH was constitutional (51.50%) followed by post inflammatory (22.50%). Lower eyelids were involved in 72.50%. Grade 2 POH was seen in 58%. Wood's lamp examination showed POH to be dermal in 60.50%. Faulty habits were observed viz. lack of adequate sleep (40%), frequent cosmetic use (36.50%), frequent eye rubbing (32.50%), and lack of correction for errors of refraction like myopia in 12% patients. Strong association of POH with stress (71%), atopy (33%) and family history (63%) was noted.
Conclusions:
Periorbital hyperpigmentation is a multi-factorial entity. It is absolutely essential to classify the type of POH and determine underlying causative factors in order to direct appropriate measures for better and successful outcome in future.
Keywords: Dark circles, habits, infraorbital hyperpigmentation, periorbital
Introduction
What was known?
Periorbital hyperpigmentation is extremely common yet unexplored aesthetic condition in Indian patients.
Aesthetic facial concerns have been the main reason for dermatological consults in the last few years.[1] Among which there is one that is called “periorbital hyperpigmentation” (POH) or “dark circles under the eyes” (DC). Periorbital hyperpigmentation is defined as bilateral, homogeneous hyperchromic macules and patches primarily involving the lower eyelids but also sometimes extending towards the upper eyelids, eyebrows, malar regions, temporal regions and lateral nasal root. The age of onset is usually after puberty or in early adulthood (16-25 years). It is more pronounced in certain ethnic groups and is also frequently seen in multiple members of the same family.[1]
Although considered a phenomenon within the limit of physiology, patients, especially women are really bothered and concerned about it, even relating the presence of dark circles with significant impairment on their quality of life. Although not rare in males, females are affected more owing to the hormonal factors.[2]
DC are caused by multiple etiologic factors that include genetic/constitutional,[3] dermal melanin deposition, post inflammatory hyperpigmentation, secondary to atopic or allergic contact dermatitis, anemia, stress, faulty habits, periorbital edema, superficial location of vasculature, and shadowing due to skin laxity, etc.[4]
While there are not much statistics giving the frequency of its occurrence, judging from the amount of advertising of cosmetics marketed to treat it, dark circles are a cosmetic concern for large number of individuals.[5,6]
However, there is lack of published studies concerning POH in Indian patients. So this study was conducted to explore the condition in Indian patients.
Our aims of the study were to determine the prevalence and type of periorbital hyperpigmentation within various age and sex groups in patients attending dermatology OPD at tertiary care hospital and to find out etiology of periorbital hyperpigmentation and its association with habits and other disorders.
Materials and Methods
This was single centre, cross-sectional, descriptive, anonymous study conducted in patients attending the skin OPD of the teaching hospital from November 2009 to July 2011 with approval of Institutional Ethical Committee (Human). Two hundred new patients from skin OPD having age between 16-45 years and Fitzpatrick skin type I to IV were included in study. Informed consent of each volunteer was taken. Detailed history was taken including duration of the condition, family history, history of atopy or drug intake, associated faulty habit or lifestyle, use of cosmetics, precipitating factor such as photosensitivity, allergies, seasonal variations, presence of associated pigmentation in other areas of the face and the body and presence of any concomitant illness such as anemia, gastrointestinal diseases, hepato-biliary diseases, renal diseases, thyroid diseases, etc.
This was followed by careful physical examination to detect involvement of upper or lower or both eyelids and extension beyond the periorbital region, colour of hyperpigmented areas (Light brown/Dark brown/Red/Blue), presence of any dermatological disease or scar in periorbital region, presence of any visible bulging, shadow effect, superficial visible vasculature (i.e., capillaries or veins) in the infraorbital region, pallor in palpebral conjunctiva, face, nails and palms; any cosmetics applied over face, presence of pigmentation in other areas of face e.g., melasma, freckles, etc.
Diagnosis of periorbital hyperpigmentation was done clinically and the patients were classified according to the classification proposed by Ranu et al.[7] as follows:
Constitutional – The presence of a curved band of brownish to black pigmentation on the skin of the lower eyelids approximating the shape of the orbital rim with frequent involvement of upper eyelids.
Post inflammatory – Presence of irregular patches of brownish or grey pigmentation on the skin on the upper, lower or both eyelids with features of lichenification, accentuation of skin creases, and eczematous papules or patches in the surrounding areas. Personal and/or family history of atopy may or may not be present.
Vascular – Presence of erythema predominantly involving the inner aspect of lower eyelids, with prominent capillaries or telangiectasia (capillaries) or the presence of bluish discoloration of the lower eyelid and visible bluish veins that becomes more prominent when the overlying skin is stretched. This type of dark circle appears to be due to a combination of transparency of the overlying skin and dermal vascularity.
Shadow effect – Presence of a dark shadow under an overhanging tarsal muscle, eye bags, or the presence of a deep tear trough over the medial aspect of inferior orbital rim that disappear with direct lighting.
Others – POH from other causes including anemia, hormonal disturbances, nutritional deficiencies, acanthosis nigricans, skin laxity, associated chronic illness, habits, etc.
Grading of POH was done in comparison to surrounding skin as follows: 0 – skin colour comparable to other facial skin areas, 1 – faint pigmentation of infraorbital fold, 2 – pigmentation more pronounced, 3 – deep dark colour, all four lids involved, 4 – grade 3+ pigmentation spreading beyond infraorbital fold. Wood's lamp[1,4,8,9] examination was done to determine whether pigmentation is epidermal or dermal. If there is no accentuation of pigment, then it is due to dermal pigmentation or vascularity. If there is accentuation of pigment, then it is due to superficial pigmentation. Eyelid stretch test[1,4,8,9] was done in which if the dark circles improves, then it is because of skin laxity. If dark circles worsen, then it is because of subdermal vascularity. If there is no change in dark circles, then it is due to epidermal and/or dermal pigmentation. Direct lighting was used to identify the dark circles due to shadow effect. Clinical photographs of the patients were taken under standard conditions. Following baseline investigations were carried out in each patient: Complete blood count, serum TSH, SGPT, serum cholesterol, random blood sugar.
While history and physical examination are usually sufficient to determine the primary cause of periorbital hyperpigmentation, confirmation by histologic examination may rarely be necessary.[8] Histopathology examinations were not performed due to esthetic concerns.
Statistical analysis
Data were statistically described in frequencies (number of cases) and percentages (%) when appropriate. Association between POH and other variables was tested using multinomial logistic regression. P < 0.05 was considered statistically significant. All statistical calculations were done using computer programs Microsoft Excel 2010 and IBM SPSS (Statistical Package for the Social Science) version 20 for Microsoft Windows.
Results
Demographic characteristics are shown in Table 1. The mean age was 21.31 years (range 16-45). Majority of the patient were housewives (n = 91, 45.5%) (P = 0.0001).
Table 1.
Demographic features of the patients
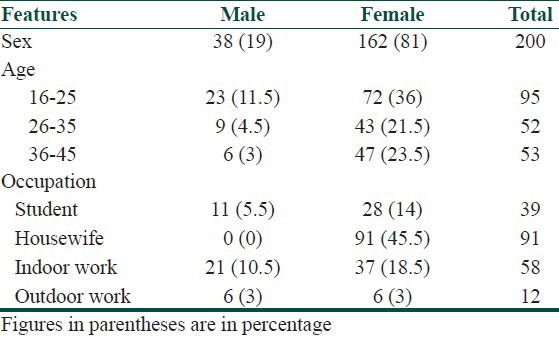
The commonest form of POH observed was constitutional type (n = 103, 51.5%) followed by post inflammatory type (n = 45, 22.5%) [Table 2]. Various types of POH observed in our study are shown in Figures 1 to 4. In our study, the most common site involved were lower eyelids (n = 134, 67%) followed by involvement of both upper and lower eyelids (n = 41, 20.5%). Patients having grade 1 to grade 4 type of POH as observed in our study are shown in Figure 5 to 8. Majority of the patients were having POH of grade 2 (n = 115, 57.5%). One hundred twenty six (63%) patients had a positive family history of POH (P = 0.03). On Wood's lamp examination, 121 (60.50%) patients had dermal pigmentation (P = 0.0001). A summary of these findings is displayed in Table 3.
Table 2.
Classification of POH
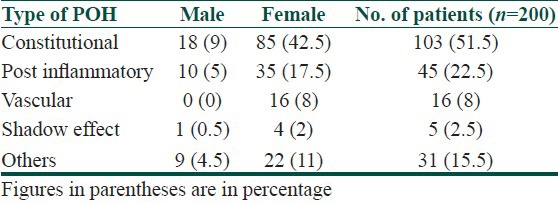
Figure 1.

Constitutional type of periorbital hyperpigmentation
Figure 4.

Shadow effect type of periorbital hyperpigmentation
Figure 5.

Grade 1 type of periorbital hyperpigmentation
Figure 8.

Grade 4 type of periorbital hyperpigmentation
Table 3.
Distribution of patients according to various parameters
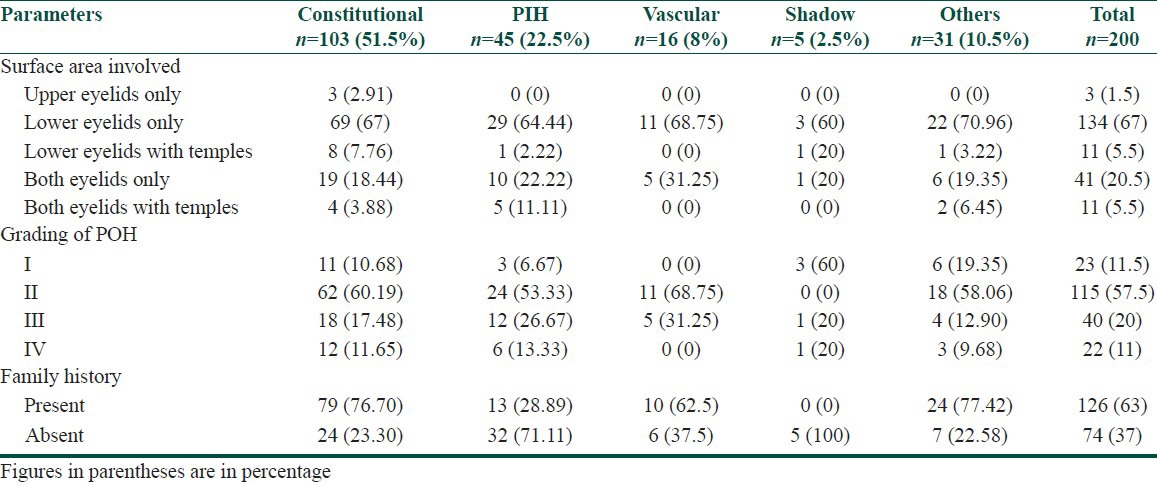
Figure 2.

Post inflammatory type of periorbital hyperpigmentation
Figure 3.

Vascular type of periorbital hyperpigmentation
Figure 6.

Grade 2 type of periorbital hyperpigmentation
Figure 7.

Grade 3 type of periorbital hyperpigmentation
Multinomial logistic regression shows that the model showing association of POH with different variables is very good (Chi square value 419.515, df = 57, P = 0.0001 and Cox and Snell Pseudo R- square value = 0.877). As regards with habits, the multinomial logistic regression of POH with variables like lack of correction for myopia (P = 0.02) and lack of adequate sleep i.e., 6-8 hours per night regularly (P = 0.01) were statistically significant, both of which signifying strain on eyelid muscles. Association of POH with other habits and eye diseases was not statistically significant (P > 0.05).
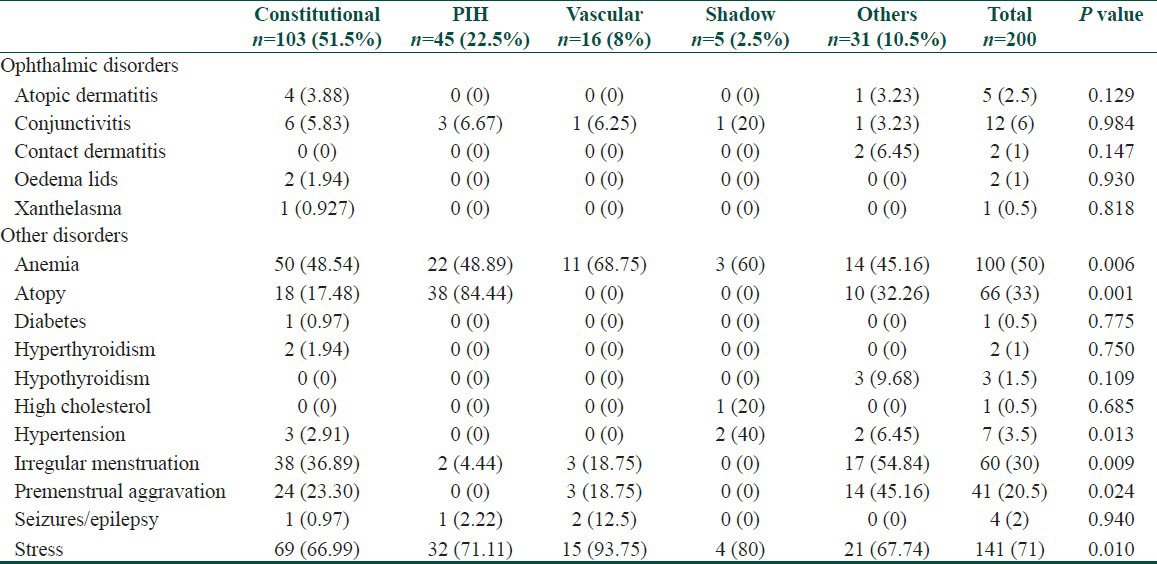
Multinomial logistic regression of POH with atopy (P = 0.001) and irregular menstruation (P = 0.009), premenstrual aggravation (P = 0.024), stress (P = 0.010) and anemia (P = 0.006) was highly significant. Laboratory investigations revealed anemia in 100 (50%) patients, raised blood sugar in 1 (0.5%) patient, serum TSH was raised in 3 (1.5%) patients, while it was decreased in 2 (1%) patients and serum cholesterol was raised in 1 (0.5%) patient. SGPT values were within normal range in all the patients. A comprehensive summary of findings can be found in Tables 4 and 5.
Table 4.
Association of POH with personal habits and lifestyle
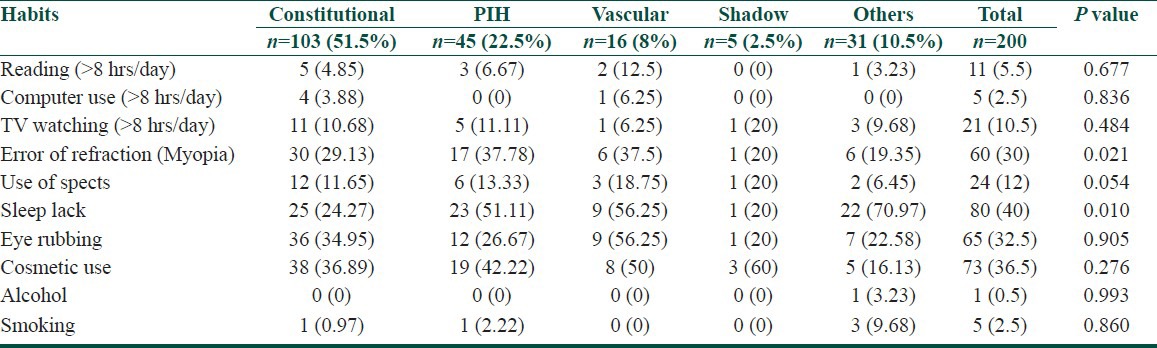
Table 5.
Association of POH with ophthalmic and other disorders
Discussion
Prevalence of POH was estimated to be 30.76%. Present study shows that most common age group was 16-25 years and that POH has higher preponderance for females over males (1:4.2).
Strachan et al.[10] has stated that genetic conditions are not necessarily congenital (present at birth). The genotype is fixed at conception, but the phenotype may not manifest until adult life. In such cases the penetrance is age-related, which supports that age of onset of POH in majority of the patients in our study was in early adulthood, i.e., 16-25 years.
Seasonal variation was seen in only 15% patients having aggravation of their condition in winter showing that seasonal change has got a little impact on POH (P > 0.05).
Our results are in agreement with findings of Ranu et al.[7] regarding the commonest type of POH in Indian patients to be of constitutional type. Present study shows that 51.50% of the patients were having constitutional type of POH, while Ranu et al.[7] had reported that in their study on Chinese, Malay and Indian patients, the commonest form of POH observed was vascular (41.8%), followed by constitutional (38.6%), post inflammatory type (12%), and shadow effect (11.4%). The constitutional type of POH was more commonly seen in Malays (65%) and Indians (94%).
In PIH type of POH, 33% patients had history of atopy in our study while it was 55.4% in study conducted by Ranu et al.[7]
Sarma et al.[11] have proposed that all the described PDLs on face including PDL-F,G,H actually represent the margins of pigmentary patches which closely conforms with Blaschko's lines on face and have proposed that mosaicism may play a role in development of PDL. Malakar et al. [12] have defined periorbital melanosis as an extension of pigmentary demarcation line F of the face which was observed in 22 (11%) patients in our study [Figure 9]. Only one patient (0.5%) was having pigmentary demarcation line G.
Figure 9.

Periorbital hyperpigmentation with pigmentary demarcation line F
In our study, 126 (63%) patients had positive family history of POH. Goodman et al.[3] has reported POH to be an autosomal dominant trait which usually runs in the families, which is reflected in our study, as out of 103 patients of constitutional type of POH, 79 (76.69%) patients had positive family history of POH, which reflects its genetic transmission. Out of 16 patients of vascular type, 10 (62.5%) patients had positive family history of POH, which may be due to thin skin of periorbital region which is an inherited trait. Ranu et al.[7] reported 42.2% patients had a positive family history of POH.
Watanabe et al.[5] reported that out of 12 patients of dark circles included in their study; all the 12 patients (100%) revealed dermal melanin deposition by histopathological examination. In contrast to that our study showed 60.50% patients had dermal pigmentation, 38% patients had epidermal pigmentation, while 1.5% patients had mixed type of pigmentation on Wood's lamp examination.
In the present study, 40% patients reported lack of adequate sleep. In a study by Ranu et al.,[7] 94 (51.1%) and 83 (41.5%) patients reported sleep deprivation and insomnia respectively.
All the patients who were using different cosmetics in periorbital area (n = 65, 36.5%) gave history of frequent eye rubbing and scratching in periorbital area which implies that there may be some ingredient in it that causes allergic contact dermatitis and on resolution leaves post inflammatory hyperpigmentation in periorbital area. However, this needs further evaluation by a separate scientific study as the results were not statistically significant in our study.
Thirty percent patients had error of refraction i.e., myopia, out of which only 12% patients were regularly using the spectacles or contact lenses thereby causing exhaustion of periorbital muscles. According to Gathers[8] exhaustion of periorbital muscles may play a significant role in causation of POH.
Majority of these patients had aggravation of dark circles during periods of stress. It may be due to effect of increased MSH secretion via HPA axis in response to stress which creates a vicious cycle and it is very difficult to differentiate whether stress increases POH or vice versa but once dark circles appear, it definitely increases stress regarding their aesthetic appearance. In our study, 71% patients of gave positive history of stress due to dark circles under the eyes which shows that it is a major esthetic concern and having significant impact on quality of life. According to Gathers[8] fatigue, stress, emotional liability and aging all may play a significant role in development of POH.
In the present study, 50% patients of POH had associated iron deficiency anemia. Many patients reported improvement of dark circles on correction of anemia. In these patients POH may be either because enough oxygen is not reaching the periorbital tissues or due to facial pallor which makes the periorbital region look comparatively darker.
Thirty percent patients of POH had menstrual disturbances like irregular menstruation for longer periods (>1.5-2 years). Eighteen percent patients were taking oral contraceptive pills which reflects the hormones to be one of the factors involved in causation or exacerbation of POH. According to Gathers,[8] chronic use of some drugs including oral contraceptives, hormone-replacement therapy, antipsychotics, gold, chemotherapeutic compounds can lead to periorbital hyperpigmentation.
In our study, patients of POH having either present or past positive history of systemic diseases like diabetes, hyperthyroidism, hypothyroidism, high cholesterol, hypertension, seizures constituted only 9% which was not statistically significant (P > 0.05).
Gendler et al.[2] stated that some medical problems that may contribute to dark circles include disorders of heart, thyroid, kidney or liver, Vitamin K deficiency, Addison's disease, etc., However, statistical data was not shown in this literature. According to Boxrud et al.[13] systemic conditions that can lead to pigmentation of periorbital area include metabolic and endocrine disorders, but no statistical data have been shown.
Considering its multifactorial etiology and increasing cosmetic concerns, we look forward to larger studies to further enlighten our knowledge over this condition.
Limitations of the study
Assessment of pigment depth by Wood's lamp in Indian skin may be unreliable.
Clinico-histopathological correlation was not done.
Conclusion
Periorbital hyperpigmentation is a multi-factorial entity. It is absolutely essential to classify the type of POH, determine underlying causative factors and correction of faulty habits in order to direct the appropriate treatment for better and successful outcome in future.
What is new?
This is a unique study showing prevalence, classification and association of periorbital hyperpigmentation with habits and other disorders in Indian patients, which will help to explore and direct appropriate measures for treatment of this aesthetic condition.
Acknowledgment
The authors express their gratitude to Dr. Saket J. Thaker, Department of Clinical Pharmacology, 2nd floor New M.S. Building, Seth G.S. Medical College and K.E.M.H., Parel, Mumbai - 400 012, Maharashtra, India for statistical analysis and constant support throughout the study. We are also thankful to Dr. Janak Dharsandiya, Dr. Jayshree Savalia and Dr. Deep Joshipura, C.U. Shah Medical College and Hospital, Surendranagar for their invaluable help during the study.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Freitag FM, Cestari TF. What causes dark circles under the eyes? J Cosmet Dermatol. 2007;6:211–5. doi: 10.1111/j.1473-2165.2007.00324.x. [DOI] [PubMed] [Google Scholar]
- 2.Gendler EC. Treatment of periorbital hyperpigmentation. Aesthet Surg J. 2005;25:618–24. doi: 10.1016/j.asj.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 3.Goodman RM, Belcher RW. Periorbital hyperpigmentation. An overlooked genetic disorder of pigmentation. Arch Dermatol. 1969;100:169–74. doi: 10.1001/archderm.100.2.169. [DOI] [PubMed] [Google Scholar]
- 4.Roh MR, Chung KY. Infraorbital dark circles: Definition, causes, and treatment options. Dermatol Surg. 2009;35:1163–71. doi: 10.1111/j.1524-4725.2009.01213.x. [DOI] [PubMed] [Google Scholar]
- 5.Watanabe S, Nakai K, Ohnishi T. Condition known as “dark rings under the eyes” in the Japanese population is a kind of dermal melanocytosis which can be successfully treated by Q-swithched ruby laser. Dermatol Surg. 2006;32:785–9. doi: 10.1111/j.1524-4725.2006.32161.x. [DOI] [PubMed] [Google Scholar]
- 6.Epstein JS. Management of infraorbital dark circles. A significant cosmetic concern. Arch Facial Plast Surg. 1999;1:303–7. doi: 10.1001/archfaci.1.4.303. [DOI] [PubMed] [Google Scholar]
- 7.Ranu H, Thng S, Goh BK, Burger A, Goh CL. Periorbital hyperpigmentation in Asians: An epidemiologic study and a proposed classification. Dermatol Surg. 2011;37:1297–303. doi: 10.1111/j.1524-4725.2011.02065.x. [DOI] [PubMed] [Google Scholar]
- 8.Gathers RC. Periorbital hypermelanosis. In: Paul KA, editor. Dermatology for Skin of Color. 1st ed. New York: McGraw Hill; 2009. pp. 341–3. [Google Scholar]
- 9.Dhepe N. Dark circles: Causes and treatments. The Aestheticians Journal. 2011;3:14–20. [Google Scholar]
- 10.Strachan T, Read AP. Genes in pedigrees and population. In: Strachan T, editor. Human Molecular Genetics. 3rd ed. New York: Garland Science; 2003. pp. 106–7. [Google Scholar]
- 11.Sarma N, Chakraborty S, Bhattacharya SR. Acquired, Idiopathic, Patterned Facial Pigmentation (AIPFP) including periorbital pigmentation and pigmentary demarcation lines on face follows the Lines of Blaschko on face. Indian J Dermatol. 2014;59:41–48. doi: 10.4103/0019-5154.123492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malakar S, Lahiri K, Banerjee U, Mondal S, Sarangi S. Periorbital melanosis is an extension of pigmentary demarcation line-F on face. Indian J Dermatol Venereol Leprol. 2007;73:323–5. doi: 10.4103/0378-6323.34009. [DOI] [PubMed] [Google Scholar]
- 13.Boxrud CA, Sylvester DA. Infraorbital discoloration: Dark circles-an anatomic analysis and treatment. In: Mauriello JA, editor. Techniques in Cosmetic Eyelid Surgery: A Case Study Approach. 1st ed. Philadelphia: Lippincott Williams and Wilkins; 2004. pp. 291–305. [Google Scholar]


