Abstract
Background:
The search for alternative and effective forms of training simulation is needed due to ethical and medico-legal aspects involved in training surgical skills on living patients, human cadavers and living animals.
Aims:
To evaluate if the bench model fidelity interferes in the acquisition of elliptical excision skills by novice medical students.
Materials and Methods:
Forty novice medical students were randomly assigned to 5 practice conditions with instructor-directed elliptical excision skills’ training (n = 8): didactic materials (control); organic bench model (low-fidelity); ethylene-vinyl acetate bench model (low-fidelity); chicken legs’ skin bench model (high-fidelity); or pig foot skin bench model (high-fidelity). Pre- and post-tests were applied. Global rating scale, effect size, and self-perceived confidence based on Likert scale were used to evaluate all elliptical excision performances.
Results:
The analysis showed that after training, the students practicing on bench models had better performance based on Global rating scale (all P < 0.0000) and felt more confident to perform elliptical excision skills (all P < 0.0000) when compared to the control. There was no significant difference (all P > 0.05) between the groups that trained on bench models. The magnitude of the effect (basic cutaneous surgery skills’ training) was considered large (>0.80) in all measurements.
Conclusion:
The acquisition of elliptical excision skills after instructor-directed training on low-fidelity bench models was similar to the training on high-fidelity bench models; and there was a more substantial increase in elliptical excision performances of students that trained on all simulators compared to the learning on didactic materials.
Keywords: Cutaneous surgery, elliptical excision, excisional biopsy, medical education, medical student, teaching
Introduction
What was known?
Simulation-based surgical training in graduate medical education has gained widespread acceptance;
Several high-fidelity and low-fidelity bench models have been described for elliptical excision-skill training;
These bench models are educational, simple, versatile, portable, easy-to-assemble, and inexpensive tools; however, so far, none of them is complete.
Primary health care practitioners are routinely confronted with pathological process that demands performance of simple cutaneous surgical procedures.[1,2] However, as most of the general practitioners performing minor surgical procedures do not have any formal surgical training,[3] and the basic surgical fundaments are not acquired by a large percentage of medical students,[4] the teaching and learning of cutaneous surgical principles (e.g., excision of skin lesion, closure of skin incision, and others) become an important component of the formation of both undergraduates and newly graduates.[3,5]
Given that the basic cutaneous skills’ training on live patients can neglect ethical and medico-legal aspects, the learning of technical skills on inanimate bench models is becoming widely used in medical education.[6,7] These inanimate bench models vary widely regarding their level of fidelity (or “realism”) to living human patients.[7] High-fidelity bench models such as parts of postmortem animals (e.g., ox tongue, cattle digits, and pig, rat and chicken skins[8,9,10,11,12,13]) are limited by high costs, low availability, potential for transmission of infectious disease, and ethical concerns[7]; and lower-fidelity bench models such as synthetic or organic materials (e.g., polyurethane foam sheet, synthetic ethylene-vinyl acetate, fruits and vegetables[9,14,15,16,17,18,19,20]) sacrifice “realism” for portability, lower costs, and potential for repetitive use.[7]
Despite the intuitive belief that “the more realistic is the better”,[21] in surgical simulation this cannot be based only on subjectivity[22]; and so far, few studies have directly compared the effectiveness of low-fidelity bench models versus high-fidelity postmortem animal bench models on the acquisition of elliptical excision skills in medical education. Therefore, the purpose of this study was to assess objectively if the fidelity of bench models interferes in the acquisition of elliptical excision skills by novice medical students, using the comparison among four inanimate simulators (two considered of low-fidelity and two of high-fidelity) by means of a randomized controlled blinded study.
Materials and Methods
Subjects
The protocol consisted of 40 first- and second-year medical students with no surgical skills background (novices) from a single academic center that volunteered to take part in the study; they were enrolled upon a consent form signed by them, in accordance with the Helsinki Declaration of 1975, as amended in 1983. Local institutional research ethics board approval was obtained.
Study design
It was a randomized controlled study with blinded expert examiners, including a pre-test, a 1-h practice phase, and a post-test [Figure 1]. The pre- and post-test were identical and consisted in the performance of an elliptical excision (marking of safety margins forming an ellipse, incision and excision of the tissue) for the diagnosis and treatment of a non-melanoma skin cancer measuring 1 cm in diameter simulated on ox tongue. Each student was tested individually and had a total of 12 min to complete the task.[23] No verbal feedback was provided during pre- and post-tests.
Figure 1.
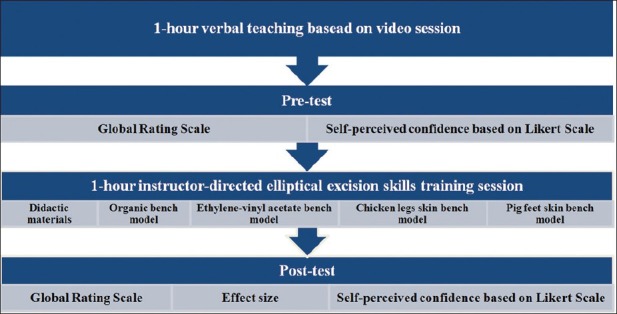
Study design
Pre testing
Since the elliptical excisional technique was required, on the day of the experiment, all participants were taught how to use surgical instruments by means of an instructional video[24] presentation that was repeated and commented during one hour (verbal teaching based on video).[25,26] Next, all participants underwent a pre-test.
Group assignment and training phase
Immediately after pre-test, all students were randomly assigned, via a computer generated process, to 1 of 5 groups (n = 8) to receive instructor-directed elliptical excision skill training. All 5 groups remained in separate rooms so they were unable to communicate with each other. In Group 1 (control), students were given a training based on didactic materials (textbooks, online texts, and online expert narrated demonstration videos).[26] The remaining participants in trained elliptical excision skills in a repetitive deliberate form on low-fidelity organic bench model (Group 2), on low-fidelity synthetic ethylene-vinyl acetate bench model (Group 3) [Figure 2], on high-fidelity chicken legs’ skin bench model (Group 4), or on high-fidelity pig foot skin bench model (Group 5) [Figure 3]. This stage lasted one hour[25,26] for all five groups.
Figure 2.
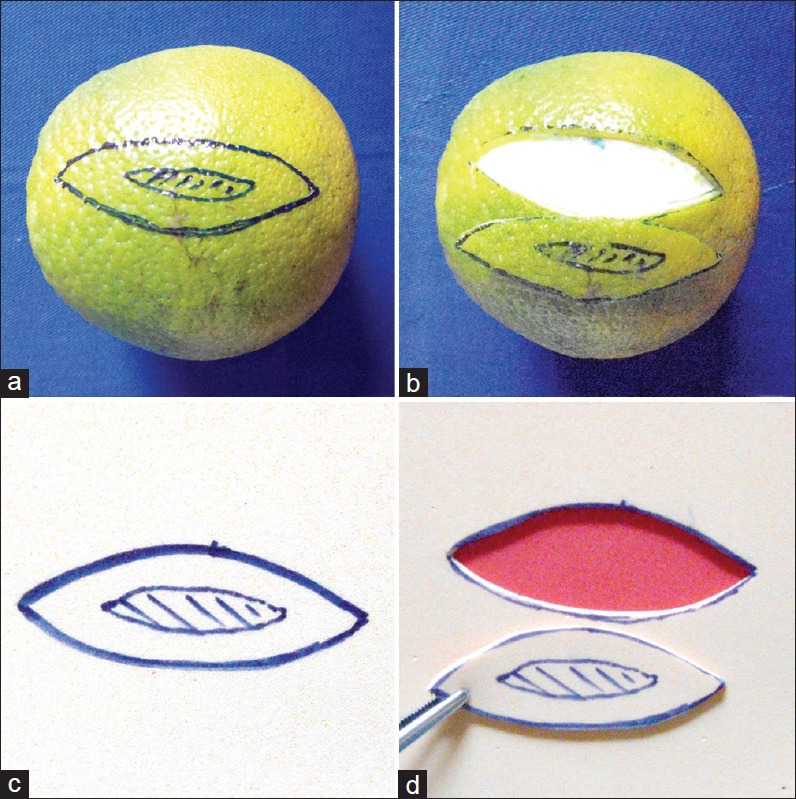
Low-fidelity bench models simulating a non-melanoma skin cancer and an elliptical excision. (a and b) Organic bench model. (c and d) Synthetic ethylene-vinyl acetate bench model
Figure 3.
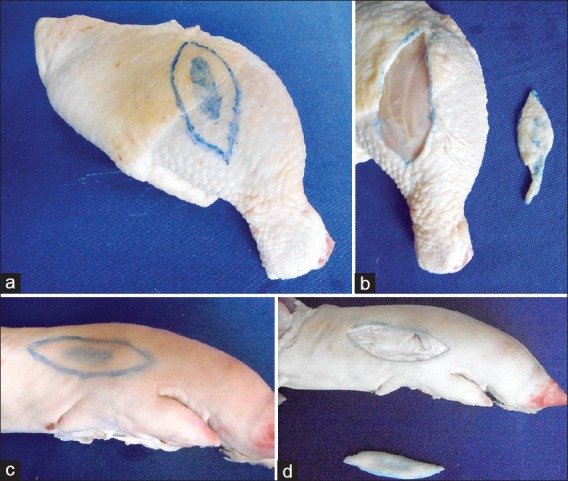
High-fidelity bench models simulating a non-melanoma skin cancer and an elliptical excision. (a and b) Chicken legs’ skin bench model. (c and d) Pig foot skin bench model
Apparatus for hands-on training
The whole teaching process, learning and training of elliptical excision skills given to the students that received hands-on training (groups 2 to 5) was performed on three-dimensional inanimate bench models. The adoption of oranges (organic bench model) and many sheets of ethylene-vinyl acetate glued together as low-fidelity simulation platforms during the training phase was carried out according to some principles previously described by our group[16,19,20] and by others.[17,18] Chicken legs and pig feet were used as high-fidelity simulation platforms according to some characteristics described by Khalil et al.[11] and by Purim,[12] respectively. The training also took some additional materials such as No. 15 surgical blade with scalpel handle, tooth rat tweezers and marking pen.
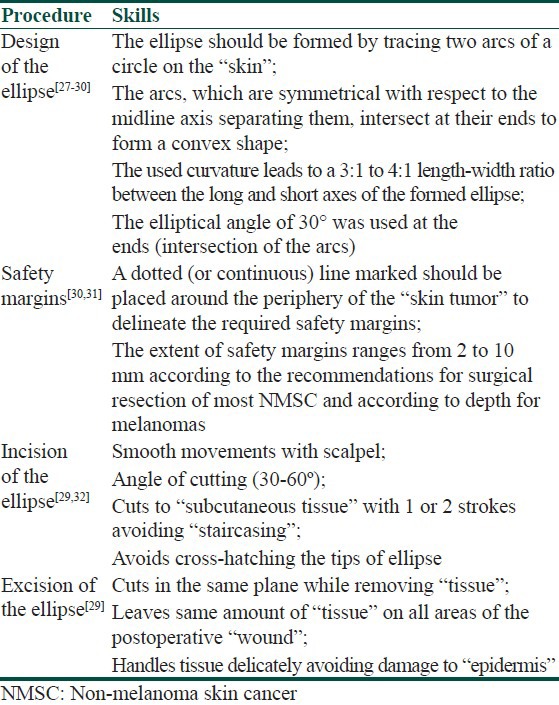
Instructors, feedback and elliptical excision technique
All five groups received concurrent and summary feedback from instructors. In order to standardize the teaching and learning, one instructor was randomly allocated via a computer generated process to one of the semi-groups with 4 students each.[25] Faculty surgeons with long experience in teaching basic and advanced surgical skills to medical students and residents were chosen to be instructors. They are not co-authors of the present study and they did not participate in the blind evaluation process of surgical maneuvers performed during pre- and post-training. On standardized didactic seminar, all instructors were told to teach the elliptical excision technique using the same method [Table 1].[27,28,29,30,31,32]
Table 1.
Standardization of teaching and learning of the elliptical excision technique
Post testing
Immediately after the training phase, all medical students were randomly assigned to post-test via a computer generated process.
Study blinding
All 80 pre- and post-tests maneuvers were recorded (images focusing only on hand movements) and saved. These digital videos were archived for later analysis and codified by one of the investigators through the use of randomly assigned numbers. All digital videos were independently evaluated in a blinded fashion by two experienced surgical specialists that had no prior knowledge about the groups and did not take part in the training processes. The evaluators were able to fast-forward the tapes, a procedure which, while shortening evaluation time, has been shown to be as effective as viewing the entire skill at its natural pace.[33]
Outcome measures
All 40 study participants completed pre- and post-training questionnaires in order to measure self-perceived confidence in performing elliptical excision; they rated their confidence on a 5-point Likert scale[15] with the lowest rating (very unconfident) being 1 and the highest rating being 5 (very confident).
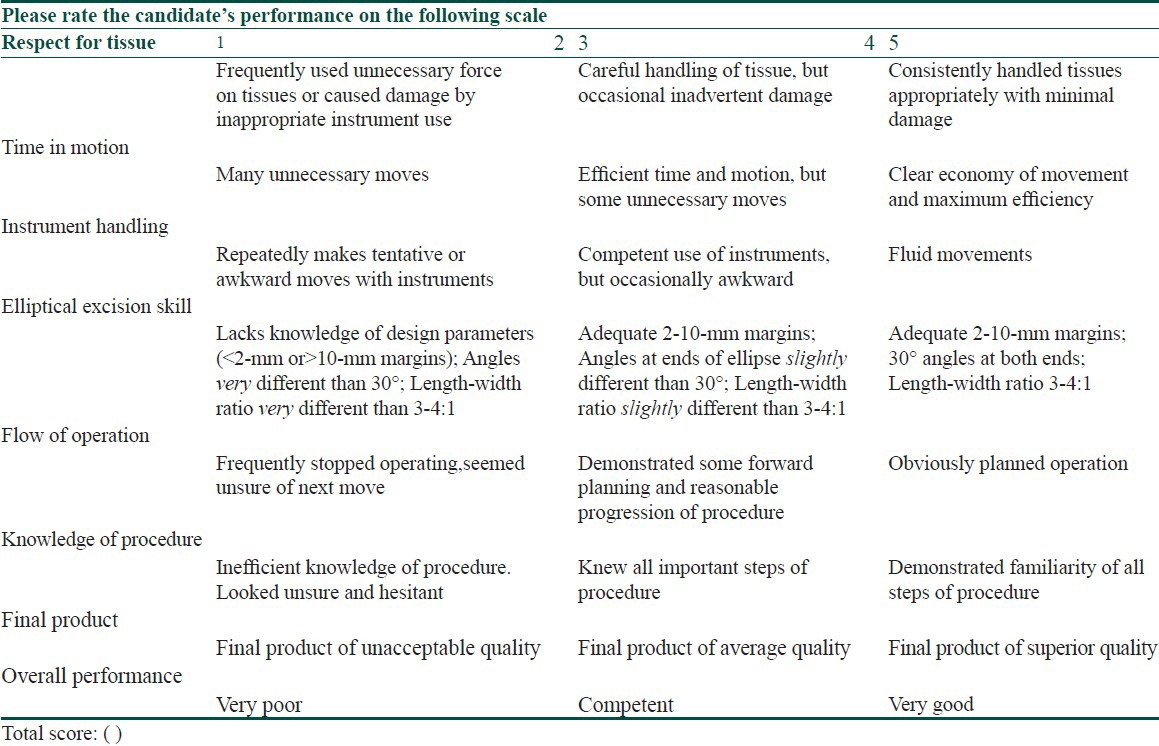
The Global Rating Scale [Table 2][34,35] adapted for elliptical excision evaluation[29] was used to objectively evaluate (qualitative assessment) elliptical excision performances of each student in eight main areas, each of which was rated in a behaviorally anchored 5-point scale with 1 being the minimum score (unsatisfactory performance) and 5 the maximum score (outstanding performance) for a total maximum score of 40.
Table 2.
Global rating scale[34,35] adapted for evaluation of biopsy techniques[29] used to assess qualitatively and objectively all elliptical excision performances
Statistical analysis
In the descriptive analysis, data were summarized as means, medians, standard deviations, 1st and 3rd quartiles, minimum and maximum values. Bioestat® for Windows, version 5.0, was used in the statistical analyses. Student's T-test was used for measurable variables. Values were considered significant for a confidence interval of 95% (P < 0.05). Effect sizes were also calculated in order to identify the magnitude of the effect of the intervention regardless of the sample size; effect sizes exceeding 0.80 were considered large.[36]
Results
Qualitative and objective elliptical excision skills evaluation based on global rating scale
In the blinded evaluations of all maneuvers performed during pre- and post-training, no inter-observer difference was detected between the examiners regarding the qualitative evaluation of means in all five groups (all P > 0.05).
The objective analysis of the elliptical excision pre-training performances showed that the five groups were similar (all P > 0.05) in group-to-group comparisons. The post-training analysis demonstrated that groups 2, 3, 4 and 5 presented superior performance (all P = 0.0000) when compared to Group 1. There was no difference (all P > 0.05) in the comparison of groups 2, 3, 4 and 5. Comparing pre-test and post-test, there was a better performance (all P = 0.0000) of all five groups in the post-training [Table 3 and Figure 4].
Table 3.
Mean of the objective and qualitative assessments based on global rating scale pre-and post-training and the effect size. (biopsy training) of elliptical excision
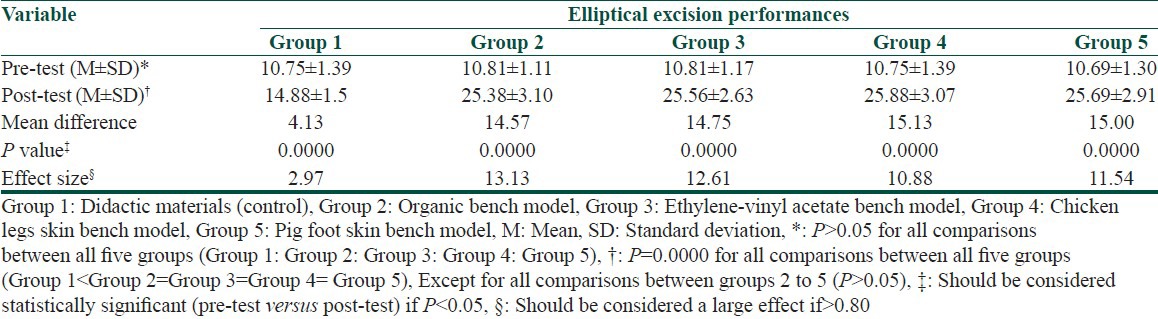
Figure 4.
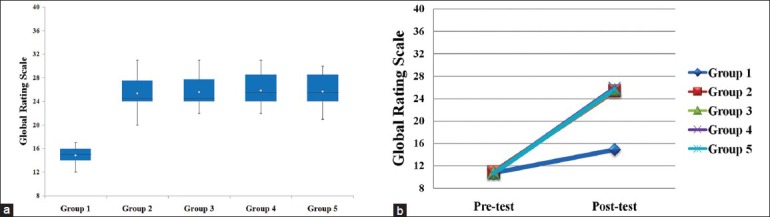
(a) Boxplot showing the dispersion of the mean values of all elliptical excision performances post-training based on Global Rating Scale. Groups 2 to 5 were similar to each other (all P > 0.05), but presented a significantly better performance (all P = 0.0000) than control Group 1. The diamond symbol represents the mean value. The heavy line is the median. The bars represent the data range. (b) Mean of all elliptical excision performances in pre- and post-tests based on Global Rating Scale. Groups 2 to 5 were similar to each other (all P > 0.05), but improved their qualitative performance significantly more (all P = 0.0000) than control Group 1
Effect sizes
The evaluation of the intervention magnitude (elliptical excision training) was considered large (≥0.80) in all performed measurements [Table 3].
Self-perceived confidence based on likert scale
Regarding students’ perceptions about their confidence to perform pre-training elliptical excisions, there were no differences in the group-to-group comparisons made among all the five groups (all P > 0.05). After training, although students from groups 2, 3, 4 and 5 were similar among themselves (all P > 0.05), they felt more confident (all P = 0.0000) to perform elliptical excisions when compared to the trainees from Group 1. In the comparison of pre- and post-training, there was increased confidence (all P < 0.05) in all five groups after training [Table 4 and Figure 5].
Table 4.
Students’ perception on their confidence to perform elliptical excision pre-and post-training based on 5-point Likert scale
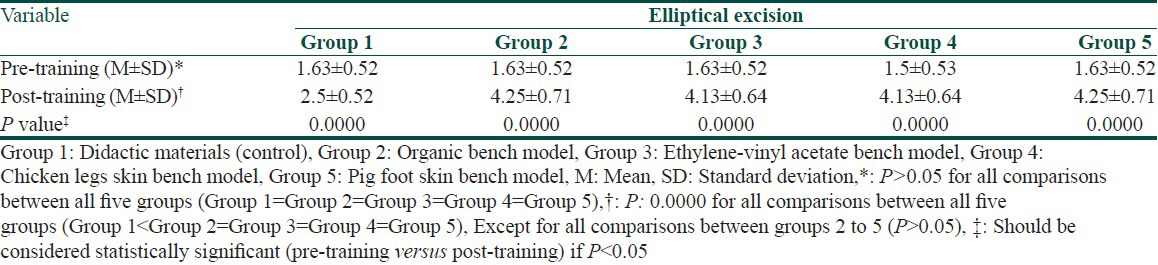
Figure 5.
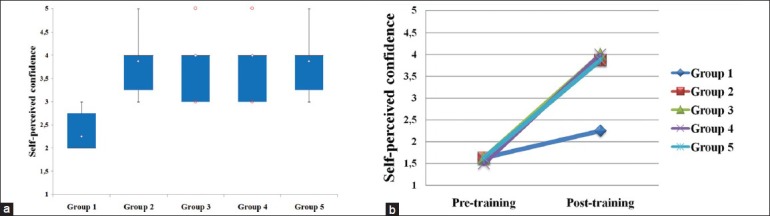
(a) Boxplot showing the dispersion of the mean values of students’ perceptions about their confidence to perform elliptical excision post-training based on 5-point Likert scale. Groups 2 to 5 were similar to each other (all P > 0.05), but presented a significantly better confidence (all P = 0.0000) than control Group 1. The diamond symbol represents the mean value. The heavy line is the median. The bars represent the data range. The symbols “o” indicates the outliers. (b) Mean of students’ perceptions, of all five groups, on their confidence to perform elliptical excision pre- and post-training based on 5-point Likert scale. Groups 2 to 5 were similar to each other (all P > 0.05), but improved their confidence significantly more (all P = 0.0000) than control Group 1
Discussion
Since surgical excision with pre-determined safety margins (excisional biopsy) has been described as the therapeutic modality of choice for several dermatologic conditions, such as precancerous and malignant lesions,[31] and the number of cutaneous lesions has been increasing,[1,2] this basic technical skill (excision biopsy techniques) that is considered as a cornerstone of cutaneous surgical practice[30] should be part of the cutaneous surgical armamentarium.[28]
However, some studies[1,2,37,38] have shown that the rate of incomplete excision of skin tumors is higher among general practitioners than among specialized doctors (e.g. general surgeons, plastic surgeons, and dermatologists). Therefore, great efforts should be concentrated to train general practitioners[1,2,37,38] and medical students[3,5] in the art of proper surgical excision of skin tumors to further improve health outcomes.
Currently, it is recommended to acquire basic surgical skills outside the operating environment (simulation-based training) prior to procedures on live patients.[6] However, as the practice on fresh human cadavers and on live animals is associated with high costs, risks of infections, need of specialized facilities, and legal/ethical aspects, and the use of virtual reality simulators is hampered by the high costs and lack of access,[7] several low- and high-fidelity bench models have been described as teaching and learning tools.[8,9,10,11,12,13,14,15,16,17,18,19,20]
Although, several reports[3,8,9,13,15,26,39,40,41,42,43,44] in the surgical literature have assessed relevant aspects of the surgical skills’ training, including basic cutaneous surgery principles on several bench models, to the best of our knowledge, this is one of the few studies that objectively evaluated the acquisition of elliptical excision skills by novice medical students by comparing low-fidelity bench models and high-fidelity bench models. An extensive English literature review (Medline, Scopus, Web of Science, EBSCO, and Embase databases) showed no relevant reports demonstrating the superiority of high-fidelity simulator over low-fidelity simulator (or the superiority of low-fidelity simulator over another low-fidelity simulator) for teaching elliptical excision skills to novice medical students, although there are similar reports on the teaching of biopsy techniques to internists and residents.[27,43]
As observed in other studies,[45,46] the students that trained on simulators (groups 2 to 5) showed a qualitative increase in elliptical excision performances when compared to the didactic training group (control), regardless of the bench model fidelity.
In the present study, the effect sizes (elliptical excision training) were large, indicating that the significant improvement was most likely related to the intervention and not to the sample size.[36] The evaluations of all elliptical excision performances, carried out by two independent and blinded evaluators, reduced the possibility that this increase in performances was a result of rater bias or of expectations from the non-blinded surgeon raters.[15]
This study also showed that after a 1-h training session there was an increase in confidence levels for the performance of the skills taught, similar to what was observed by others.[47] Furthermore, the present results confirm that the acquisition of technical skills on bench models (hands-on training) is more effective than the non-simulated learning.[48]
Based on similar results found in this study (training on low-fidelity simulators was similar to training on high-fidelity simulators), and on the description that a combination of self-directed training with expert-administered feedback distributed intermittently during a pre-determined period (weeks or months) is an excellent method to teach basic technical skills,[42] the authors believe that in some situations the four bench models that were studied could be complementary and, consequently, enhance the teaching and learning already established. In those training programs that use pig or chicken skins,[11,12] in laboratories of surgical technique, the plates of ethylene-vinyl acetate[16,17] or organic materials[19] can be adopted as an alternative complementary tool for training sessions at home. Thus, students can train under supervision of instructors in classrooms (concurrent feedback) and they can also practice at home, bringing the ethylene-vinyl acetate plates or organic material with them to resolve doubts with the instructor (summary feedback). In both instances, important aspects to promote good wound healing and cosmesis (e.g., manual dexterity, safe handling of instruments, respect for tissues, and others) can be assessed and taught again to the student; and as a consequence, there is a gain of skills over time.
The present study assessed only one basic skill of cutaneous surgery (elliptical excision training), not meeting all the needs of medical students in training; and it should include the acquisition of other skills (e.g., complex tasks such as anastomosis and others) that can also be trained in simulation environments.[42,49] Further studies are required to measure the retention of biopsy skills taught over time, the transferability to surgical practice, and also to access if trainees in other training levels (e.g., final year medical students and residents) also acquire excision elliptical skills on bench models, regardless of the fidelity of the material.
Conclusion
In summary, the present study demonstrated that the acquisition of elliptical excisional skills on low-fidelity bench models by novice medical students, after 1-h training, was similar to the training on high-fidelity bench models; and the qualitative increase of elliptical excisional performances of participants that received hands-on training was superior to the learning on didactic materials.
What is new?
Both high-fidelity and low-fidelity bench models allow novice medical students to practice elliptical excision skills in a safe, controlled, risk-free setting;
These bench models allow novice medical students to acquire elliptical excision skills without compromising the qualitative and objective results.
This data has an impact on the possibility of using any of these bench models according to the institutional availability.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Murchie P, Delaney EK, Thompson WD, Lee AJ. Excising basal cell carcinomas: Comparing the performance of general practitioners, hospital skin specialists and other hospital specialists. Clin Exp Dermatol. 2008;33:565–71. doi: 10.1111/j.1365-2230.2008.02710.x. [DOI] [PubMed] [Google Scholar]
- 2.Hansen C, Wilkinson D, Hansen M, Soyer HP. Factors contributing to incomplete excision of nonmelanoma skin cancer by Australian general practitioners. Arch Dermatol. 2009;145:1253–60. doi: 10.1001/archdermatol.2009.270. [DOI] [PubMed] [Google Scholar]
- 3.Collins AM, Ridgway PF, Hassan MS, Chou CW, Hill AD, Kneafsey B. Surgical instruction for general practitioners: How, who and how often? J Plast Reconstr Aesthet Surg. 2010;63:1156–62. doi: 10.1016/j.bjps.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 4.Forbes SS, Fitzgerald PG, Birch DW. Undergraduate surgical training: Variations in program objectives and curriculum implementation across Canada. Can J Surg. 2006;49:46–50. [PMC free article] [PubMed] [Google Scholar]
- 5.Friedlich M, Wood T, Regehr G, Hurst C, Shamji F. Structured assessment of minor surgical skills (SAMSS) for clinical clerks. Acad Med. 2002;77:S39–41. doi: 10.1097/00001888-200210001-00013. [DOI] [PubMed] [Google Scholar]
- 6.Hammond I, Karthigasu K. Training, assessment and competency in gynaecologic surgery. Best Pract Res Clin Obstet Gynaecol. 2006;20:173–87. doi: 10.1016/j.bpobgyn.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 7.Hammoud MM, Nuthalapaty FS, Goepfert AR, Casey PM, Emmons S, Espey EL, et al. Association of Professors of Gynecology and Obstetrics Undergraduate Medical Education Committee. To the point: Medical education review of the role of simulators in surgical training. Am J Obstet Gynecol. 2008;199:338–43. doi: 10.1016/j.ajog.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 8.Altinyazar HC, Hosnuter M, Unalacak M, Koca R, Babucçu O. A training model for cutaneous surgery. Dermatol Surg. 2003;29:1122–4. doi: 10.1046/j.1524-4725.2003.29350.x. [DOI] [PubMed] [Google Scholar]
- 9.Tokuhara KG, Boldt DW, Yamamoto LG. Teaching suturing in a workshop setting: A comparison of several models. Hawaii Med J. 2004;63:258–9. [PubMed] [Google Scholar]
- 10.Camelo-Nunes JM, Hiratsuka J, Yoshida MM, Beltrani-Filho CA, Oliveira LS, Nagae AC. Ox tongue: An alternative model for surgical training. Plast Reconstr Surg. 2005;116:352–4. doi: 10.1097/01.prs.0000173550.42201.b5. [DOI] [PubMed] [Google Scholar]
- 11.Khalil PN, Siebeck M, Mutschler W, Kanz KG. The use of chicken legs for teaching wound closure skills. Eur J Med Res. 2009;14:459–60. doi: 10.1186/2047-783X-14-10-459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Purim KS. Cutaneous surgery workshop. Rev Col Bras Cir. 2010;37:303–5. doi: 10.1590/s0100-69912010000400012. [DOI] [PubMed] [Google Scholar]
- 13.Khalil PN, Kanz KG, Siebeck M, Mutschler W. Teaching advanced wound closure techniques using cattle digits. Dermatol Surg. 2011;37:325–30. doi: 10.1111/j.1524-4725.2011.01881.x. [DOI] [PubMed] [Google Scholar]
- 14.Bjellerup M. Novel method for training skin flap surgery: Polyurethane foam dressing used as a skin equivalent. Dermatol Surg. 2005;31:1107–11. doi: 10.1097/00042728-200509000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Taché S, Mbembati N, Marshall N, Tendick F, Mkony C, O’Sullivan P. Addressing gaps in surgical skills training by means of low-cost simulation at Muhimbili University in Tanzania. Hum Resour Health. 2009;7:64. doi: 10.1186/1478-4491-7-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bastos EM, Silva RD. Proposal of a synthetic ethylene-vinyl acetate bench model for surgical foundations learning. Suture training. Acta Cir Bras. 2011;26:149–52. doi: 10.1590/s0102-86502011000200014. [DOI] [PubMed] [Google Scholar]
- 17.Gutiérrez-Mendoza D, Narro-Llorente R, Contreras-Barrera ME, Fonte-Ávalos V, Domíguez-Cherit J. Ethylene vinyl acetate (Foam): An inexpensive and useful tool for teaching suture techniques in dermatologic surgery. Dermatol Surg. 2011;37:1353–7. doi: 10.1111/j.1524-4725.2011.02033.x. [DOI] [PubMed] [Google Scholar]
- 18.Whallett EJ, McGregor JC. An alternative model for teaching basic principles and surgical skills in plastic surgery. J Plast Reconstr Aesthet Surg. 2011;64:272–4. doi: 10.1016/j.bjps.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 19.Denadai R, Souto LR. Organic bench model to complement the teaching and learning on basic surgical skills. Acta Cir Bras. 2012;27:88–94. doi: 10.1590/s0102-86502012000100015. [DOI] [PubMed] [Google Scholar]
- 20.Denadai R, Bastos EM. Letter: The synthetic ethylene-vinyl acetate bench model. Dermatol Surg. 2012;38:288–9. doi: 10.1111/j.1524-4725.2011.02260.x. [DOI] [PubMed] [Google Scholar]
- 21.Grober ED, Hamstra SJ, Wanzel KR, Reznick RK, Matsumoto ED, Sidhu RS, et al. The educational impact of bench model fidelity on the acquisition of technical skill: The use of clinically relevant outcome measures. Ann Surg. 2004;240:374–81. doi: 10.1097/01.sla.0000133346.07434.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Darzi A, Datta V, Mackay S. The challenge of objective assessment of surgical skill. Am J Surg. 2001;181:484–6. doi: 10.1016/s0002-9610(01)00624-9. [DOI] [PubMed] [Google Scholar]
- 23.Dorman K, Satterthwaite L, Howard A, Woodrow S, Derbew M, Reznick R, et al. Addressing the severe shortage of health care providers in Ethiopia: Bench model teaching of technical skills. Med Educ. 2009;43:621–7. doi: 10.1111/j.1365-2923.2009.03381.x. [DOI] [PubMed] [Google Scholar]
- 24.Czarnowski C, Ponka D, Rughani R, Geoffrion P. Elliptical excision: Minor surgery video series. Can Fam Physician. 2008;54:1144. [PMC free article] [PubMed] [Google Scholar]
- 25.Dubrowski A, MacRae H. Randomised, controlled study investigating the optimal instructor: Student ratios for teaching suturing skills. Med Educ. 2006;40:59–63. doi: 10.1111/j.1365-2929.2005.02347.x. [DOI] [PubMed] [Google Scholar]
- 26.Xeroulis GJ, Park J, Moulton CA, Reznick RK, Leblanc V, Dubrowski A. Teaching suturing and knot-tying skills to medical students: A randomized controlled study comparing computer-based video instruction and (concurrent and summary) expert feedback. Surgery. 2007;141:442–9. doi: 10.1016/j.surg.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 27.Alguire PC, Mathes BM. Skin biopsy techniques for the internist. J Gen Intern Med. 1998;13:46–54. doi: 10.1046/j.1525-1497.1998.00009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goldberg LH, Alam M. Elliptical excisions: Variations and the eccentric parallelogram. Arch Dermatol. 2004;140:176–80. doi: 10.1001/archderm.140.2.176. [DOI] [PubMed] [Google Scholar]
- 29.Garcia C, Neuburg M, Carlson-Sweet K. A model to teach elliptical excision and basic suturing techniques. Arch Dermatol. 2006;142:526. doi: 10.1001/archderm.142.4.526. [DOI] [PubMed] [Google Scholar]
- 30.Hussain W, Mortimer NJ, Salmon PJ. Optimizing technique in elliptical excisional surgery: Some pearls for practice. Br J Dermatol. 2009;161:697–8. doi: 10.1111/j.1365-2133.2009.09312.x. [DOI] [PubMed] [Google Scholar]
- 31.Silva RD, Souto LR. Evaluation of the diagnosis and treatment of non-melanoma skin cancer and its impacts on the prevention habits in a specific population of southeastern Brazil. Eur J Gen Med. 2011;8:291–301. [Google Scholar]
- 32.Vujevich JJ, Kimyai-Asadi A, Goldberg LH. The four angles of cutting. Dermatol Surg. 2008;34:1082–4. doi: 10.1111/j.1524-4725.2008.34212.x. [DOI] [PubMed] [Google Scholar]
- 33.Dath D, Regehr G, Birch D, Schlachta C, Poulin E, Mamazza J, et al. Toward reliable operative assessment: The reliability and feasibility of videotaped assessment of laparoscopic technical skills. Surg Endosc. 2004;18:1800–4. doi: 10.1007/s00464-003-8157-2. [DOI] [PubMed] [Google Scholar]
- 34.Faulkner H, Regehr G, Martin J, Reznick R. Validation of an objective structured assessment of technical skill for surgical residents. Acad Med. 1996;71:1363–5. doi: 10.1097/00001888-199612000-00023. [DOI] [PubMed] [Google Scholar]
- 35.Reznick R, Regehr G, MacRae H, Martin J, McCulloch W. Testing technical skill via an innovative “bench station” examination. Am J Surg. 1997;173:226–30. doi: 10.1016/s0002-9610(97)89597-9. [DOI] [PubMed] [Google Scholar]
- 36.Hojat M, Xu G. A visitor's guide to effect sizes: Statistical significance versus practical (clinical) importance of research findings. Adv Health Sci Educ Theory Pract. 2004;9:241–9. doi: 10.1023/B:AHSE.0000038173.00909.f6. [DOI] [PubMed] [Google Scholar]
- 37.McWilliam LJ, Knox F, Wilkinson N, Oogarah P. Performance of skin biopsies by general practitioners. BMJ. 1991;303:1177–9. doi: 10.1136/bmj.303.6811.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bhatti AZ, Asif S, Alwan M. Factors affecting incomplete excision of nonmelanoma skin cancers in New Zealand. Ann Plast Surg. 2006;57:513–6. doi: 10.1097/01.sap.0000226934.45093.30. [DOI] [PubMed] [Google Scholar]
- 39.van Hove PD, Tuijthof GJ, Verdaasdonk EG, Stassen LP, Dankelman J. Objective assessment of technical surgical skills. Br J Surg. 2010;97:972–87. doi: 10.1002/bjs.7115. [DOI] [PubMed] [Google Scholar]
- 40.Porte MC, Xeroulis G, Reznick RK, Dubrowski A. Verbal feedback from an expert is more effective than self-accessed feedback about motion efficiency in learning new surgical skills. Am J Surg. 2007;193:105–10. doi: 10.1016/j.amjsurg.2006.03.016. [DOI] [PubMed] [Google Scholar]
- 41.Nousiainen M, Brydges R, Backstein D, Dubrowski A. Comparison of expert instruction and computer-based video training in teaching fundamental surgical skills to medical students. Surgery. 2008;143:539–44. doi: 10.1016/j.surg.2007.10.022. [DOI] [PubMed] [Google Scholar]
- 42.Jensen AR, Wright AS, Levy AE, McIntyre LK, Foy HM, Pellegrini CA, et al. Acquiring basic surgical skills: Is a faculty mentor really needed? Am J Surg. 2009;197:82–8. doi: 10.1016/j.amjsurg.2008.06.039. [DOI] [PubMed] [Google Scholar]
- 43.Capperauld I, Hargraves J. Surgical simulation for general practitioners. Ann R Coll Surg Engl. 1991;73:273–5. [PMC free article] [PubMed] [Google Scholar]
- 44.Moulton CA, Dubrowski A, Macrae H, Graham B, Grober E, Reznick R. Teaching surgical skills: What kind of practice makes perfect?: A randomized, controlled trial. Ann Surg. 2006;244:400–9. doi: 10.1097/01.sla.0000234808.85789.6a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Matsumoto ED, Hamstra SJ, Radomski SB, Cusimano MD. The effect of bench model fidelity on endourological skills: A randomized controlled study. J Urol. 2002;167:1243–7. [PubMed] [Google Scholar]
- 46.Grober ED, Hamstra SJ, Wanzel KR, Reznick RK, Matsumoto ED, Sidhu RS, et al. Laboratory based training in urological microsurgery with bench model simulators: A randomized controlled trial evaluating the durability of technical skill. J Urol. 2004;172:378–81. doi: 10.1097/01.ju.0000123824.74075.9c. [DOI] [PubMed] [Google Scholar]
- 47.Kim MJ, Boehler ML, Ketchum JK, Bueno R, Jr, Williams RG, Dunnington GL. Skills coaches as part of the educational team: A randomized controlled trial of teaching of a basic surgical skill in the laboratory setting. Am J Surg. 2010;199:94–8. doi: 10.1016/j.amjsurg.2009.08.016. [DOI] [PubMed] [Google Scholar]
- 48.Lynagh M, Burton R, Sanson-Fisher R. A systematic review of medical skills laboratory training: Where to from here? Med Educ. 2007;41:879–87. doi: 10.1111/j.1365-2923.2007.02821.x. [DOI] [PubMed] [Google Scholar]
- 49.Klingensmith ME, Brunt LM. Focused surgical skills training for senior medical students and interns. Surg Clin North Am. 2010;90:505–18. doi: 10.1016/j.suc.2010.02.004. [DOI] [PubMed] [Google Scholar]


